Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Shock
Caricato da
may_hisolerDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Shock
Caricato da
may_hisolerCopyright:
Formati disponibili
4/23/12
SHOC K
-
A complex clinical syndrome that may occur at any time and in any place. Inadequate blood flow to body organs and tissue causing lifethreatening cellular dysfunction. A syndrome not an illness nor a disease. A syndrome in which there is circulation perfusion compromise. tissue perfusion. Their is a cellular anoxia, if not prevented leads to tissue death. Homeostasis just to restore the patency of the blood. Inadequate tissue perfusion. Oxygen in the blood. Serious life threatening condition.
Click to edit Master subtitle style
Classificatio n
4/23/12
Shock is commonly divided into three major classifications: SHOCK
1. HYPOVOLEMIC
2. CARDIOGENIC
3. DISTRIBUTIVE
Hemorrhage Anaphylactic Burns Neurogenic Dehydration
MI Obstructive condition other causes Septic
4/23/12
1. Hypovolemia
Reduced
intravascular blood volume causing circulatory dysfunction and inadequate tissue perfusion resulting from loss of blood, plasma, or fluids. loss of fluid in our body. life threatening.
Massive
Potentially
4/23/12
Pathophysiology
CAUSES:
Hemorrhage Burns Dehydration ( as from excessive perspiration, severe diarrhea, protracted vomiting, diabetes insipidus, diuresis, or inadequate fluid intake)
When fluid is lost from the intravascular space ( venous return to the heart is reduced )
This decreases ventricular filling ( which leads to a drop in stroke volume.)
Cardiac output falls (causing reduced perfusion to tissues and organs.)
Tissue anoxia prompts a shift in cellular metabolism from aerobic to anaerobic pathways.
This produces an accumulation of lactic acid, resulting in metabolic acidosis.
HYPOVOLEMIA
4/23/12
ASSESSMENT
FINDINGS
Preexisting disorders or conditions that reduced blood volume, such as GI hemorrhage, trauma, and severe diarrhea and vomiting. Some anginal pain in patients with cardiac disease ( because of decreased myocardial perfusion and oxygenation.) Physical symptoms consistent with reduced
4/23/12
TREATMENT
In severe cases, an intra-aortic balloon pump, ventricular assist device, or pneumatic anti shock garment ( rare, only when unstable fractures involved) Oxygen administration Bleeding control by direct application of pressure and related measures Possible parenteral nutrition or tube feedings Bed rest Prompt and vigorous blood and fluid replacement Positive inotropes Possibly diuretics Possible surgery to correct underlying problem
4/23/12
NURSING
MANAGEMENT
Check for a patient airway and adequate circulation. ( if blood pressure and heart rate are absent, start cardiopulmonary resuscitation. Obtain type and cross match as ordered. Administer prescribed I.V solutions or blood products. Insert an indwelling urinary catheter. Administer prescribed oxygen. Provide emotional support to the patient and his family. Used modified Trendelenburgs position. Monitor Vital signs and peripheral pulses Cardiac rhythm
Coagulation studies for signs of impending coagulopathy Complete blood count and electrolyte measurements Arterial blood gas level Intake and output Hemodynamics
Monitor the patient for such complications as:
4/23/12
2. CARDIOGENIC SHOCK
condition of diminished cardiac output that severely impairs tissue perfusion ( myocardial damage of more than 40% of the left ventricle most common) of the heart to pump blood adequately to meet oxygenation needs of the body. lethal form of shock.
Failure
Most
4/23/12
pathophysiology
Left ventricular dysfunction initiates as series of compensatory mechanisms that attempt to increase cardiac output.
Initial
Decreased myocardial contractility
Decreased stroke volume
Decreased left ventricular emptying
Increased heart rate
Left ventricular dilation and back up of blood Increased preload
Decreased coronary artery perfusion and collateral blood flow. Myocardial Hypoxia
Pulmonary Congestion
Decreased cardiac output
Compensation
Decompensation and DEATH
CAUSES
Acute mitral or aortic insufficiency End- stage cardiomyopathy Myocardial infarction (MI);myocardial damage of more than 40% of the left ventricle most common Myocardial Ischemia Myocarditis Papillary muscle dysfunction Ventricular aneurysm Ventricular septal defect
4/23/12
ASSESSMENT FINDINGS
Determination of existing disorder, such as MI or cadiomyopathy that severely decreases left ventricular function. Anginal pain Urine output less than 20ml/hr Pale, cold, clammy skin Decreased sensorium Rapid, shallow respirations Rapid, thready pulse Mean arterial pressure of less than 60 mm Hg in adults Gallop rhythm, faint heart sounds, and possibly, a holosystolic murmur
4/23/12
TEST RESULTS
Serum enzyme measurements show elevated levels of creatine kinase, lactate dehydrogenase, aspartate aminotransferase and alanine amino transferase. Troponin level is elevated. Cardiac catherterization and echocardiography may reveal other conditions that can lead to pump dysfunction and failure ( cardiac tamponade, papillary muscle infarct or rupture, ventricular septal rupture, pulmonary emboli, venous pooling, and hypovolemia) Pulmonary artery pressure monitoring reveals increased pulmonary artery pressure and pulmonary artery wedge pressure, reflecting an increase in left ventricular end-diastolic pressure (preload) and heightened resistance to left ventricular emptying (afterload) caused by ineffective pumping and increased peripheral vascular resistance. Invasive arterial pressure monitoring shows systolic arterial pressure less than 80mm Hg ,caused by impaired ventricular ejection. Arterial blood gas (ABG) analysis may show metabolic and respiratory acidosis and hypoxia. Electrocardiography demonstrates possible evidence of acute MI , ischemia, or ventricular aneurysm.
4/23/12
TREATMENT
Intra aortic balloon pump (IABP) Vasopressors, inotropics, and vasoconstrictors Oxygen Osmotic diuretics Vasodilators Analgesics, sedatives Bed rest Possible parenteral nutrition or tube feedings Possible ventricular assist device Possible heart transplant.
4/23/12
NURSING INTERVENTION
Administer prescribed oxygen Follow IABP protocols and policies. ( When a patient is receiving treatment with an IABP, sitting position higher than 45 degrees (including for chest x-rays) because the balloon may tear through the aorta and cause immediate death. Monitor the patient continuously for cardiac arrhythmias. Monitor ABG levels (acid-base balance) and pulse oximetry. Evaluate complete blood count and electrolyte levels. Obtain vital signs and peripheral pulses. Monitor hemodynamic parameters. Measure and record urine output every hour from indwelling catheter, and fluid intake. Monitor heart and breath sounds. Evaluate LOC Be alert to adverse responses to drug therapy Plan care to allow frequent rest periods, and provide as much privacy as possible. Provide explanations and reassurance for the patient and his family as appropriate. Prepare the patient and his family for a possibly fatal outcome , and help them find effective coping strategies. Monitor the patient for possible multiple organ dysfunction.
4/23/12
3. Distributive shock
v v
Problem is in vascular area Is due to changes in blood vessel tone that increase the size of the vascular space without an increase in the circulating blood volume. also called as Vasogenic Shock
Distributive Shock is divided into three types :
Anaphylactic Shock Neurogenic Shock Septic Shock
Potrebbero piacerti anche
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5795)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1091)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Chapter End Stop SignsDocumento4 pagineChapter End Stop Signsapi-307327939Nessuna valutazione finora
- Breast UltrasoundDocumento57 pagineBreast UltrasoundYoungFanjiensNessuna valutazione finora
- Goodbye HachikoDocumento6 pagineGoodbye HachikoAbraham LizardoNessuna valutazione finora
- Etiology and Pathophysiology Breast CancerDocumento1 paginaEtiology and Pathophysiology Breast Cancermay_hisolerNessuna valutazione finora
- Drug Study Format Ready To PrintDocumento2 pagineDrug Study Format Ready To Printmay_hisolerNessuna valutazione finora
- AutoSPRINK12InstallationWalkthrough PDFDocumento2 pagineAutoSPRINK12InstallationWalkthrough PDFHai PhamNessuna valutazione finora
- Design Aeroleaf Wind Turbine PDFDocumento98 pagineDesign Aeroleaf Wind Turbine PDFananduNessuna valutazione finora
- Discharge Plan: MedicationDocumento2 pagineDischarge Plan: Medicationmay_hisolerNessuna valutazione finora
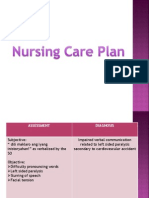
- NCP CvaDocumento7 pagineNCP Cvamay_hisolerNessuna valutazione finora
- Miyat PresentationDocumento73 pagineMiyat Presentationmay_hisolerNessuna valutazione finora
- Breast CompositionDocumento1 paginaBreast Compositionmay_hisolerNessuna valutazione finora
- Miyat PresentationDocumento73 pagineMiyat Presentationmay_hisolerNessuna valutazione finora
- CuesDocumento2 pagineCuesmay_hisolerNessuna valutazione finora
- Card It IsDocumento3 pagineCard It Ismay_hisolerNessuna valutazione finora
- Black Box Testing TechniquesDocumento28 pagineBlack Box Testing TechniquesAshish YadavNessuna valutazione finora
- 10th Triple Helix Conference 2012 University, Industry, and Government Partnership: Its Present and Future Challenges in IndonesiaDocumento10 pagine10th Triple Helix Conference 2012 University, Industry, and Government Partnership: Its Present and Future Challenges in IndonesiaMery Citra SondariNessuna valutazione finora
- System Analysis & Design: Structuring System Process RequirementsDocumento52 pagineSystem Analysis & Design: Structuring System Process RequirementsNusrat Jahan NafisaNessuna valutazione finora
- North West Karnataka Road Transport Corporation: (Application For Student Bus Pass)Documento3 pagineNorth West Karnataka Road Transport Corporation: (Application For Student Bus Pass)RasoolkhanNessuna valutazione finora
- Remote Digital Input (Rdi-32Xe / Rdi-32Axe) : Distributed Processing UnitsDocumento2 pagineRemote Digital Input (Rdi-32Xe / Rdi-32Axe) : Distributed Processing UnitsCHAIRMANNessuna valutazione finora
- Bending Tools RF-A English - OriginalDocumento116 pagineBending Tools RF-A English - OriginalGunnie PandherNessuna valutazione finora
- Fruit CakeDocumento3 pagineFruit CakeCynthia OnuigboNessuna valutazione finora
- Grandfather Tang Lesson PlanDocumento6 pagineGrandfather Tang Lesson PlanalyssamanningNessuna valutazione finora
- 4TH Quarter Grade 9 Pe Learning Activity Sheets Week 1 4 1Documento15 pagine4TH Quarter Grade 9 Pe Learning Activity Sheets Week 1 4 1Kelvin Pastor EncarnacionNessuna valutazione finora
- Talcott ParsonsDocumento20 pagineTalcott Parsonssyedarida fatimaNessuna valutazione finora
- Honeywell Question 1&2Documento6 pagineHoneywell Question 1&2anon_909027967Nessuna valutazione finora
- Black 2018 B Uploaded VersionDocumento46 pagineBlack 2018 B Uploaded VersionOwais AhmedNessuna valutazione finora
- EUCR-W 2009 - Captains PackDocumento9 pagineEUCR-W 2009 - Captains Packapi-16087835Nessuna valutazione finora
- SHPB2012 Barras de Cromsteel PDFDocumento24 pagineSHPB2012 Barras de Cromsteel PDFEdgar Rojas EspejoNessuna valutazione finora
- G Schock G-2210 ManualDocumento2 pagineG Schock G-2210 ManualcaquirinoNessuna valutazione finora
- CAF 8 AUD Autumn 2022Documento3 pagineCAF 8 AUD Autumn 2022Huma BashirNessuna valutazione finora
- Xtreet 250X 2017 Parts Catalogue 2016 08 16 1Documento32 pagineXtreet 250X 2017 Parts Catalogue 2016 08 16 1JeovannyAlexanderMatamorosSanchezNessuna valutazione finora
- Multiple Choice Quiz Chapter 5Documento4 pagineMultiple Choice Quiz Chapter 5gottwins05Nessuna valutazione finora
- Title 250706Documento556 pagineTitle 250706callmeasthaNessuna valutazione finora
- Paper171 I.banuDocumento6 paginePaper171 I.banuIoan-Viorel BanuNessuna valutazione finora
- R 2 KyDocumento3 pagineR 2 KyJorge AzurduyNessuna valutazione finora
- Autoplant TutorialDocumento404 pagineAutoplant TutorialManish Tukaram Deshpande100% (1)
- Comparison... Lesson PlanDocumento4 pagineComparison... Lesson PlanHicham EljarrariNessuna valutazione finora
- R2900G JLK01211 ConfigurationDocumento2 pagineR2900G JLK01211 Configurationjc villongcoNessuna valutazione finora
- Individual AssignmentDocumento17 pagineIndividual AssignmentYousef AboamaraNessuna valutazione finora