Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Pancreatic FTSVVV
Caricato da
vabukpanthiTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Pancreatic FTSVVV
Caricato da
vabukpanthiCopyright:
Formati disponibili
The functional unit of pancreas is acinus & its draining ductule.
The duct epithelium extends into the lumen of the acinus with centroacinar cell located b/w ductal epithelium and the acinus. The centroacinar cell secretes ions & water.
The acinus synthesizes,stores,secretes digestive enzymes. On the basolateral membrane lies receptors for hormones& neurotransmitters that stimulate secretion of the enzymes. The duct epithelium consists of cuboidal cells and rich in mitochondria for ion transport. The duct cells & centroacinar cells contain carbonic anhydrase,to secrete bicarbonate.
Inorganic constituents: Water,sodium,chlorides,potassium,bicarbona te. Water& ions deliver digestive enzymes to intestinal lumen and help to neutralise gastric acid. Pancreatic fluid is colourless,clear,alkaline. The total daily volume is 2.5 lts.
Organic components: The pancreas synthesize digestive enzymes. They are proteolytic,amylolytic,lipolytic & nuclease digestive enzymes. These enzymes are in inactive precursor forms .
Activation of these enzymes takes in lumen of intestine where a brush border glyco protein peptidases,enterokinases,activate trypsinogen by removing a N-Terminal hexa peptide fragment of molecule. The active trypsin catalyzes the activation of other inactive proenzymes.
In addition to digestive enzymes the acinar cells secrete Pancreatic Secretory Trypsin Inhibitor(PSTI). It inactivates trypsins that are autocatalytically formed in the pancreas that prevents pancreatitis
Amylase: Digests starch & glycogen in the diet. The amylase hydrolyses 1,4-glycosidic linkages at every other junction b/w carbon 1& O2. The hydrolytic products are maltose ,maltriose& alpha dextrins. The brush border enzymes complete hydrolysis to give glucose.
Lipases:three lipases lipase,phospholipaseA2,carboxylesterase. Most important is salivary,pancreatic,gastric lipase for fat digestion. Pancreatic lipase digests a triglyceride to two fatty acids & a monoglyceride.
PhospholipaseA2 catalyses the hydrolysis of fatty acid ester linkage at carbon 2 of phosphatidylcholine to form free fatty acid & lysophosphadidylcholine. Carboxylesterase cleaves cholesterol esters ,fat soluble vitamin esters,tri,di,monoglycerides.
Proteases : Pancreas secrete variety of proteases that are activated in the duodenum. The activated forms are trypsin,chymotrypsin,&elastases. These endopeptidases cleave specific peptide bonds adjacent to specific amino acids. Also present are carboxypeptidases,exopeptidases.
The combined action of proteases & pepsin result in release of oligopeptides ,free amino acids. These amino acids have effect on stimulating pancreatic secretion,inhibiting gastric secretion,regulating small bowel motility causing satiety.
The first line laboratory tests include estimation of serum levels of pancreatic lipase & amylase. It is easy to diagnose pancreatic insufficiency in presence of clinical triad of diabetes,pancreatic calcification & steatorrhea.
Most pancreatic disease remain clinically silent until 90% of gland is destroyed. Early recognition of pancreatic dysfunction may improve the management of the patients disease and his / her quality of life . The pancreatic function tests are divided into Direct & Indirect.
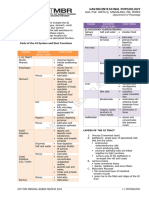
It requires oro duodenal tube that aspirates pancreatic secretion from duodenum near Ampulla of Vater The stimulants used are secretin , cholecystokinin and lundh test meal The collection period varies from 45 125 minutes Direct evaluation of pancreatic fluid may include measurement of total volume , conc of HCO3- / enzymes
This requires pancreatic stimulation by secretin stimulation followed by CCK stimulation
It assess the response of pancreas to endogenous secretin and pancreozymin in response to test meal of 5% protein 6% fat 15% carbohydrate and 74% non nutrient fibre. the conc of trypsin and volume of secretin are measured in the duodenal aspirate in 10 20 minute interval over a period of 2 hrs It is simple test , virtually abnormal in pancreatic insufficiency Abnormal result occur when small bowel , liver and biliary tree disease.
Chemical and cytological evaluation are performed on actual secretions Cytological evaluation can establish the presence/ suspicion of neoplasm although precise localization of primary organ of involvement is not possible Because of advances in imaging techniques stimulation tests are used less often
Combined stimulation of Secretin / CCK allows simultaneous estimation of both HCO3 and trypsin. The test is performed after 6 hr/over night fast . Pancreas is stimulated by iv administration of secretin 0.25 to 1U/kg followed by CCK administration. The aspiratescollected at 20,60,80 min interval.
The pH,fluid volume,enzyme activities,HCO3 conc are determined. Decreased pancreatic flow is associated with pancreatic obstruction.
Low concentration of HCO3 and enzymes are associated with cystic fibrosis,chronic pancreatitis,cysts,calcification and edema.
ORAL FUNCTIONAL TEST
Bentiromide test Pancreolauryl test Shilling test
Bentiromide is a compound attached to PABA It is hydrolysed by pancreatic chymotrypsin in the duodenum It is useful to distinguish patients with pancreatic steatorrhea from those with normal fat absorption Chymotrypsin hydrolysis of bentiromide liberates PABA which is absorbed in the proximal small bowel and conjugated in the liver.
The PABA conjugates are excreted in the urine . Urine output of PABA reflects duodenal chymotrypsin activity. Excretion of less than 50% of ingested dose in 6hrs indicates pancreatic insufficiency False results occur in intestinal mucosal , hepatic or renal disease
A tablet containing fluorescein dilaurate is taken on day 1 and urine is collected for 10 hours. On day two, a tablet containing fluorescein alone is given and urine collected again for 10 hours. Fluorescein dilaurate is hydrolysed by cholesterol ester hydrolase, present in pancreatic juice.
Fluorescein is absorbed by the intestine, conjugated in the liver, and excreted in the urine where its fluorescence can be measured.
Results are expressed as the ratio of fluorescein excreted after fluorescein dilaurate and after free fluorescein. A ratio < 20% is considered abnormal. It detects severe pancreatic insufficiency. It is a rarely used test.
Principle Oral administration of radio active cobolt 57 labelled vitamin B12 Followed by IV cold B12 to wash out the absorbed vitamin in urine
Excretion of radio activity in urine is a measure of absorption of vitamin B12 from intestine . Hence it is a function of duodenal pancreatic enzyme activity. Chronic pancreatitis gives rise to abnormal shilling test .
A) Trypsinogen proteolytic proenzyme produced exclusively in the pancreas It is detected by radio immuno assay Elevated levels are seen in acute pancreatitis or renal failure Decrease levels are seen in severe pancreatic insufficiency , cystic fibrosis and type I DM
Is produced and released from salivary glands , pancreas , intestine and Genito Urinary Tract is particuarly useful in diagnosis of acute pancreatitis for which the sensitivity is 75 % It starts rising in the serum within few hrs of onset of disease, reaches a peak in 24 hrs and returns to normal in three to five days with increased renal clearance
In healthy individuals amylase clearance parallearance
But in acute pancreatitis amylase clearance increases as opposed to creatinine clearance Normal amylase serum level is 50-120 IU/L Macroamylasemia persistent elevation of serum amylase activity with no apparent clinical symptoms of pancreatic disease It is an early marker A rapid rise and fall in serum amylase in patient with acute abdomen suggests passage of stone through ampulla of vater
Acute pancreatitis Diabetic keto acidosis Burns Renal failure Perforated duodenal ulcer Malignany Gall stones Ovarian cysts and ruptured ectopics
The increased renal clearance of amylase is reflected in increase levels of amylase in urine Urinary amylase is more sensitive indicator than serum amylase Determination of renal clearance of amylase is in detecting minor or intermittent increase in serum concentration of this enzyme
amylase clearance % creatinine clearance serum creatinine X
urinary amylase
=
serum amylase
x 100 urinary creatinine Normal range: 1.0 -3.1% Acute pancreatitis: 4.0-12%
Hydrolyses neutral fat to fatty acids and monoglycerides . In acute pancreatitis lipase levels are very high ( 2 -5 times the normal amount ). There is a rapid rise of lipase level in blood after attack and persists for 7 14 days.
Therefore lipase estimation has advantage over amylase estimation
Elevated lipase levels are also seen in peptic ulcer , malignancy, renal failureand salivary gland inflammation
Lipase levels are also used in diagnosis and follow up of cystic fibrosis ,coeliac disease and crohnsdisease. Low lipase levels indicate pancreatic destruction and associated with DM Lipase deficient people have high cholesteryl triglycerides , high blood pressure , difficulty losing weight and varicose veins .
Sensitivity of amylase and lipase test for detection of acute pancreatitis is 91 and 94% respectively. Normal lipase levels: 50-175 IU/L.
It involves 72 hr fecal fat determination. Individuals on lipid free diet excrete 1-4gm lipid in 24 hr period. Even with lipid rich diet, fecal fat will not exceed 7 gms in 24 hr period. The pt is placed on 100gm/day fat diet and stool is collected daily for 3 days. Individual with normal pancreatic fn excrete < 7 % of total fat ingested while in pancreatic insufficiency, pts excrete > 20 % of fat.
Although steatorrhoea occurs in mucosal malabsorption it is not as great as that encountered in pancreatic insufficiency. Qualitative test :- Visualisation of fat droplets / free fatty acids under the microscope using fat stains. Normal feces have 40-50 neutral lipid droplets/HPF. Steatorrhoea is characterised by increase in numb & size of droplets.
Quantitative:- Confirmatory test for Steatorrhoea. The pt is put on high fat diet atleast 2 days prior to fecal collection & stools are collected for 72 hrs. The fecal fat is analysed by Titrimetric & Gravimetric methods. Titrimetric Method involves saponification of fecal lipids with hydroxide and then conversion of salts of FA to FFA with acid treatment.
Gravimetric method:- involves extraction of total fecal lipids in organic solvent followed by their physical measurement by sensitive balance.
FE is increasingly being used as a noninvasive first line test to diagnose exocrine pancreatic insufficiency. Faecal Elastase is a proteolytic enzyme secreted by the acinar cells of the pancreas.
Elastase-1 is not degraded during intestinal transit, so the stool conc. reflects exocrine pancreatic function. Values > 200 g elastase/g stool indicate normal exocrine pancreatic function. Values < 200 g elastase/g stool indicate exocrine pancreatic insufficiency.
Estimation of sweat and skin electrolytes is helpful in the diagnosis of cystic fibrosis. Two to five fold increase in sweat sodium,chloride are diagnostic. No other condition will cause increase of sweat chloride,Na above 80 mEq/L. Sweat potassium is also increased but less significant.
The Pancreatic Malabsorption has to be differentiated from GI Malabsorption. Among the absorption tests Starch Tolerance & D- Xylose test provide useful information Starch Tolerance test:- Pancreatic Amylase deficiency in intestine should compromise the hydrolysis of carbohydrates and hence after oral ingestion of starch.There is rise in Bl.Glucose, which is lower than normal individuals.
Pts with Pancreatic Malabsorption show flatter STT curve. D-Xylose Test:- D-Xylose is valuable in differientiating malabsorption 25gm of d-xylose in water is ingested orally &amount excreted over 5hr period in urine is determined. If amount excreted is <3gm% the diagnosis is mostly enterogenous malabsorption.
Because pancreatic enzymes are not required for absorption of xylose. Accuracy of this test depends on rate of absorption & rate of excretion.
Faecal nitrogen: In pancreatic disease with diminished secretion of protein splitting enzymes the faecal nitrogen may be increased
Fecal Chymotrypsin & Elastase 1: Chymotrypsin in stool is an indirect test to establish pancreatic insufficiency in pts with Cystic Fibrosis. Measurement of pancratic elastase 1 in stool using Monoclonal antibody against human elastase 1 has received significant interest. But this test is not sensitive in detecting mild to moderate disease.
Other indirect tests that have been used are Triglyceride & Cholestryl breath test , H2 & CO2 breath test, plasma measurement of pancreatic polypeptide & Amino acids. Measurement of Leucine aminopeptidase is elevated in Ca Pancreas.Other tumour markers include CEA,AFP,Pancreatic onco fetal antigen. However these tests prove less sensitive than other indirect tests.
Potrebbero piacerti anche
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Digestive ExamDocumento13 pagineDigestive Examapi-294622133Nessuna valutazione finora
- Small IntestineDocumento10 pagineSmall IntestineGaurav Singh100% (1)
- 5 Handouts - Ust MBR 2022 - Gi Physiology - Dr. SangalangDocumento23 pagine5 Handouts - Ust MBR 2022 - Gi Physiology - Dr. SangalangRhon Andrew RañesesNessuna valutazione finora
- Pre Test Grade 8-CHEMDocumento36 paginePre Test Grade 8-CHEMMaricel PenaNessuna valutazione finora
- NSO 2014 Set-B PDFDocumento8 pagineNSO 2014 Set-B PDFChirag JainNessuna valutazione finora
- Magnificent MagnesiumDocumento11 pagineMagnificent MagnesiumCesar Oliveira100% (1)
- Lesson 1Documento2 pagineLesson 1Marissa FontanilNessuna valutazione finora
- Candida Information Pack Amp DietDocumento13 pagineCandida Information Pack Amp DietCirjaliu Murgea MarinaNessuna valutazione finora
- Summary of Biomedical Treatments For Autism: by James B. Adams, PH.DDocumento28 pagineSummary of Biomedical Treatments For Autism: by James B. Adams, PH.DOtto F OttONessuna valutazione finora
- 1.biochemistry of Digestive SystemDocumento55 pagine1.biochemistry of Digestive SystemNor Izhharuddin Zainy60% (10)
- Unit 5: Digestive System Circle The Best Answer For The Following SentencesDocumento29 pagineUnit 5: Digestive System Circle The Best Answer For The Following Sentencesdty2257202010214Nessuna valutazione finora
- E12 Practice Test 14 Đáp ÁnDocumento7 pagineE12 Practice Test 14 Đáp Ánluuhangan18052000Nessuna valutazione finora
- Mps Public School: Annual Examination 2022Documento2 pagineMps Public School: Annual Examination 2022PRIYA KUMARINessuna valutazione finora
- Nutramine MenDocumento2 pagineNutramine MenCh Ashish PawaskarNessuna valutazione finora
- Apparent or True Digestibility: Protein Amino Acids Starch Glucose Fats Fatty Acids, MonoglyceridesDocumento13 pagineApparent or True Digestibility: Protein Amino Acids Starch Glucose Fats Fatty Acids, MonoglyceridesOyedotun TundeNessuna valutazione finora
- Lipid Digestion and AbsorptionDocumento72 pagineLipid Digestion and AbsorptionKavya GaneshNessuna valutazione finora
- Lipids or FatsDocumento8 pagineLipids or FatsbananakyuNessuna valutazione finora
- PhysioEx - DigestiveDocumento59 paginePhysioEx - DigestivemichelleNessuna valutazione finora
- 17 Digestion PointersDocumento2 pagine17 Digestion PointersInternet DeviceNessuna valutazione finora
- Utility of Banana PeelDocumento21 pagineUtility of Banana PeelkramadibrataNessuna valutazione finora
- Accelerated Syllabi of College PDFDocumento117 pagineAccelerated Syllabi of College PDFabottabad school system100% (1)
- THE DIGESTIVE SYSTEM 22 (Autosaved)Documento141 pagineTHE DIGESTIVE SYSTEM 22 (Autosaved)Jairus ChaloNessuna valutazione finora
- Masters ThesisDocumento61 pagineMasters ThesissampathdtNessuna valutazione finora
- Mammalian System-01 (Digestive System)Documento35 pagineMammalian System-01 (Digestive System)Saumya99Nessuna valutazione finora
- Digestive System of A FrogDocumento5 pagineDigestive System of A Frogkriss Wong100% (1)
- Feed Product ListDocumento2 pagineFeed Product ListBrian BobbyNessuna valutazione finora
- ProjectDocumento14 pagineProjectMonalisha Gujar100% (2)
- 9th Grade BiologyDocumento29 pagine9th Grade BiologyNarendran Sairam93% (27)
- Optimal Nutrition For ExerciseDocumento19 pagineOptimal Nutrition For ExerciseEashwar Prasad Meenakshi100% (2)
- Biology Special Notes (Question & Answer Format) - 2Documento180 pagineBiology Special Notes (Question & Answer Format) - 2Agola SimonNessuna valutazione finora