Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Neurofibromatosis
Caricato da
Kristin Lorenc HenningDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Neurofibromatosis
Caricato da
Kristin Lorenc HenningCopyright:
Formati disponibili
26y male known with NF2, presenting with new onset seizures seen at C15 and discharged 2 days
ys previously, now readmitted with decreasing LOC now GCS ~ 10/15
Multiple intracranial schwannomas Cervical spine ependymoma at C4/5 Multiple spinal schwannomas and/or meningiomas large schwannoma involving left L5 nerve root Multiple enhancing subcutaneous scalp lesions
NF first described by von Recklinghausen in late 1800s series of patients - combination of cutaneous lesions and peripheral and central nervous system tumours NF2 only recognised in early 20th C and only truly distinguished from NF2 in 1981 NF1 and NF2 are two very different diseases with a few overlapping features longstanding misunderstanding/confusion The term neurobromatosis is a misnomer, because the primary tumour types in NF2 are schwannoma and meningioma
3 subtypes:
Neurofibromas (NF1) Schwannomas (NF2) Malignant peripheral nerve sheath tumours
(MPNSTs) (NF1)
Neurofibromas: mixture of proliferated Schwann cells, as well as fibroblasts and pericytes Schwannomas: composed entirely of neoplastic Schwann cells
Source: Yohay, K.: Neurofibromatosis Types 1 and 2 in The Neurologist Volume 12, Number 2, March 2006
Neurofibromas are rarely found in NF2 which has led some to propose that the disease be termed schwannomatosis or MISME syndrome: Multiple intracranial schwannomas Meningiomas Ependymomas
NF2 is present in a person who has either of the following: 1. Bilateral eighth nerve masses seen with appropriate imaging techniques (eg MRI or CT) 2. A rst degree relative with NF2 AND either unilateral eighth nerve mass or 2 of the following: Glioma Meningioma Schwannoma Neurobroma Juvenile posterior subcapsular lenticular opacity
Unilateral VS < 30 years plus at least 1 of the following: meningioma, glioma, schwannoma, juvenile posterior subcapsular lenticular opacities OR Multiple meningiomas (2) plus unilateral VS < 30 years OR 1 of the following: glioma, schwannoma, juvenile posterior subcapsular lenticular opacities
Gutmann DH, et al. The diagnostic evaluation and multidisciplinary management of neurofibromatosis 1 and neurofibromatosis 2. JAMA. Jul 2 1997;278(1):51-7. in Wagner, AL.
Cardinal feature of NF2 can arise from the cranial nerves (particularly the 8th cranial nerve), spinal roots, or any nerve distal to the spinal cord Vestibular schwannomas:
typically slow growing gradual deterioration
in hearing Balance and other cranial nerve functions may become impaired Brainstem compression and obstructive hydrocephalus can occur
Vestibular schwannomas
CT: Strongly but heterogenously enhancing
CPA masses that extend from the IAC MRI: often have heterogeneous signals, but they are typically isointense to hypointense on T1-weighted images and hyperintense on T2-weighted images; enhance avidly but often heterogenously
Spinal schwannomas
Arise from dorsal spinal roots Present in >80% of pts with NF2 Usually small and asymptomatic but can
cause spinal cord compression dumbbell-shaped enhancing masses extending out the neural foramina or intradural extramedullary masses in the spinal canal Can be radiologically indistinguishable from neurofibromas arising from spinal roots in NF1
Peripheral schwannomas can arise from any nerve, superficial or deep
Subcutaneous nodules Slighly raised, well-circumscribed cutaneous
lesions
Cutaneous schwannomas are seen in up to half of NF2 patients, but are generally a fairly minor component of the disorder.
Occur in ~ one half of patients with NF2 Most are intracranial, however spinal meningiomas can occur Intracranial:
CT - enhancing extra-axial masses often with
internal calcifications and adjacent hyperostosis - best visualized with bone windows MRI typically isointense with gray matter on all sequences and, when small, can be difficult to detect without contrast; signal intensity can vary; gadolinium: intense and generally homogeneous enhancement
Spinal
intradural extramedullary masses usually thoracic spine occasionally, extend into neural foramina
and appear as dumbbell-shaped masses with widening of the neural foramina difficult to distinguish from schwannomas or neurofibromas, although the schwannoma should be brighter on T2-weighted images
Usually spinal but can be intracranial seen most frequently in cervical cord and conus Cord tumors are well-marginated, enhancing (CT & MRI) lesions, frequently associated with cyst formation and haemorrhage. May be iso- or hypointense relative to spinal cord on T1 and always bright on T2 Conus ependymomas are more often large tumors that can fill entire spinal canal with heterogeneous signal and enhancement
T1, post contrast
T1, post contrast
NF is a complex genetic disease with a very variable presentation It is always a diagnostic possibility that should be borne in mind in unusual clinical and radiological presentations
Evans, D.G.R.: Neurofibromatosis 2 in Genetics in Medicine Volume 11, Number 9, September 2009 Khan, N., van der Werke, I. et al: Neurofibromatosis Revisited: A Pictorial Review in SA Journal of Radiology, March 2010 Wagner, A.L.: Neurofibromatosis Type 2 in http://emedicine.medscape.com/article/342667 Yohay, K.: Neurofibromatosis Types 1 and 2 in The Neurologist Volume 12, Number 2, March 2006
Potrebbero piacerti anche
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (119)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (587)
- Autism AssessmentDocumento37 pagineAutism AssessmentRafael Martins94% (16)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2219)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (894)
- The Encyclopedia of Sexually Transmitted DiseasesDocumento353 pagineThe Encyclopedia of Sexually Transmitted DiseasesLaura ZabiskyFlorestaNessuna valutazione finora
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- MCQ1FULLDocumento176 pagineMCQ1FULLtheintrov100% (11)
- Two Mechanisms of Hypertensive NephrosclerosisDocumento2 pagineTwo Mechanisms of Hypertensive NephrosclerosisJessica Damasen Caballero0% (1)
- Organization of NICU ServicesDocumento45 pagineOrganization of NICU ServicesMonika Bagchi84% (64)
- Approach To Neurologic Infections.4 PDFDocumento18 pagineApproach To Neurologic Infections.4 PDFosmarfalboreshotmail.comNessuna valutazione finora
- Nursing Care of a Patient with AppendicitisDocumento3 pagineNursing Care of a Patient with AppendicitisKeisha BartolataNessuna valutazione finora
- OutputDocumento1 paginaOutputmsenthamizharasaNessuna valutazione finora
- Child Abuse and NeglectDocumento89 pagineChild Abuse and NeglectdrvarshaNessuna valutazione finora
- Chapter 38 - Pediatric and Geriatric HematologyDocumento3 pagineChapter 38 - Pediatric and Geriatric HematologyNathaniel Sim100% (2)
- Impact of Estrogen Type On Cardiovascular Safety of Combined OralDocumento12 pagineImpact of Estrogen Type On Cardiovascular Safety of Combined OralMary SuescaNessuna valutazione finora
- Family Nursing Care PlanDocumento26 pagineFamily Nursing Care PlanAmira Fatmah QuilapioNessuna valutazione finora
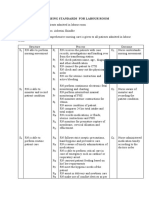
- Nursing Standards for Labour RoomDocumento3 pagineNursing Standards for Labour RoomRenita ChrisNessuna valutazione finora
- Atopic Dermatitis - The Epidemiology, Causes and Prevention of Atopic Eczema (PDFDrive)Documento289 pagineAtopic Dermatitis - The Epidemiology, Causes and Prevention of Atopic Eczema (PDFDrive)NguyenDinh NinhNessuna valutazione finora
- Human DrugsDocumento1.620 pagineHuman DrugsMohamed GameelNessuna valutazione finora
- Barge Clinic Visit Report SummaryDocumento42 pagineBarge Clinic Visit Report SummaryNicoMichaelNessuna valutazione finora
- Amazing Health Benefits of Coconut by The Coconut Research CenterDocumento6 pagineAmazing Health Benefits of Coconut by The Coconut Research CenterEuwan Tyrone PriasNessuna valutazione finora
- Lowering Blood Pressure GuideDocumento11 pagineLowering Blood Pressure GuideHilma NadzifaNessuna valutazione finora
- Microchem Non GLP ASTM E1052 Study Report NG14797Documento6 pagineMicrochem Non GLP ASTM E1052 Study Report NG14797MaryDianne RamosNessuna valutazione finora
- Designed To Enhance From The Inside Out: Apd TherapyDocumento7 pagineDesigned To Enhance From The Inside Out: Apd TherapyNumael Alfonso Serrato AlvaradoNessuna valutazione finora
- FUJIFILM's Antibacterial Technology - HYDRO AG'Documento3 pagineFUJIFILM's Antibacterial Technology - HYDRO AG'Colin BrownNessuna valutazione finora
- Jawaban UASDocumento3 pagineJawaban UASJaclin Awuy SalembaNessuna valutazione finora
- Antepartum Haemorrhage: Women's & Children's ServicesDocumento4 pagineAntepartum Haemorrhage: Women's & Children's ServicesYwagar YwagarNessuna valutazione finora
- Medical Design BriefsDocumento62 pagineMedical Design Briefsneto512Nessuna valutazione finora
- Varicella and Herpes ZosterDocumento20 pagineVaricella and Herpes ZosterzakiNessuna valutazione finora
- Yaotao Liu-ReDocumento2 pagineYaotao Liu-Reapi-489732973Nessuna valutazione finora
- Psik Soal UtsDocumento1 paginaPsik Soal UtsNaurahSalsabil / 20Nessuna valutazione finora
- Methods For The Euthanasia of Dogs and Cats - EnglishDocumento28 pagineMethods For The Euthanasia of Dogs and Cats - Englishapi-266985430Nessuna valutazione finora
- Geistlich Bio-Oss Collagen and Geistlich Bio-Gide in Extraction SocketsDocumento6 pagineGeistlich Bio-Oss Collagen and Geistlich Bio-Gide in Extraction SocketsErdeli StefaniaNessuna valutazione finora
- Case Digest 01Documento4 pagineCase Digest 01Jazz SolisNessuna valutazione finora