Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
PREGNANCY
Caricato da
rj0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
56 visualizzazioni64 pagineTitolo originale
PREGNANCY.pptx
Copyright
© © All Rights Reserved
Formati disponibili
PPTX, PDF, TXT o leggi online da Scribd
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
© All Rights Reserved
Formati disponibili
Scarica in formato PPTX, PDF, TXT o leggi online su Scribd
0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
56 visualizzazioni64 paginePREGNANCY
Caricato da
rjCopyright:
© All Rights Reserved
Formati disponibili
Scarica in formato PPTX, PDF, TXT o leggi online su Scribd
Sei sulla pagina 1di 64
PREGNANCY
BY: RHODEVA JOY BRAGA, RN
What is the difference between
growth and development?
Increase in BMR by 25%
Tendency to retain water
Constipation- 3rd tri
Hormonal changes
Weight gain
Inc plasma volume
Production of simple
glycosuria
RECOMMENDED WEIGHT GAIN
DURING PREGNANCY
• A weight gain of 11.2 to 15.9 kg (25 to 35 lb) is recommended as an
average weight gain in pregnancy
PRE-PREGNANT WEIGHT RECOMMENDED
WEIGHT GAIN
UNDERWEIGHT BMI <18.5 28-40 lbs
HEALTHY BMI <18.5-24.9 25-35 lbs
OVERWEIGHT BMI <25-29.9 15-25 lbs
OBESE BMI >30 15 lbs
WEIGHT GAIN
• 0.4 kg (1 lb) per month during the first trimester
• 0.4 kg (1 lb) per week during the last two trimesters (3-12-12)
• As a general rule, in the average woman, weight gain is considered
excessive if it is more than 3 kg (6.6 lb) a month during the second
and third trimesters; it is less than usual if it is less than 1 kg (2.2 lb)
per month during the second and third trimesters.
• You can encourage women pregnant with multiple fetuses to gain at
least 1 lb per week for a total of 40 to 45 lb
ENERGY (CALORIE)
NEEDS
CARBOHYDRATES
• An inadequate intake of carbohydrates can lead to protein breakdown
for energy, depriving a fetus of essential protein, and possibly
resulting in ketoacidosis, a possible cause of fetal and neurologic
disorders.
• The DRI of calories for women of childbearing age is 2200.
• An additional 300 calories, or a total caloric intake of 2500
calories, is recommended to meet the increased needs of pregnancy.
• In addition to supplying energy for a fetus, this increase provides
calories to sustain an elevated metabolic rate in the woman from
increased thyroid function and an increased workload from the extra
weight she must carry.
• obese women should never consume fewer than 1500 calories
per day.
Advise women to obtain calories from complex
carbohydrates (cereals and grains) rather than simple
carbohydrates (sugar and fruits).
Do not recommend sugar substitutes for women during
pregnancy, because a pregnant woman needs sugar to
maintain glucose levels
When helping a woman plan an increased caloric intake,
consider her lifestyle.
EXAMPLE: many women commonly skip meals, have erratic
eating patterns, or rely on fast and convenience foods. For
pregnancy, a woman needs to add calories by eating foods
rich in protein, iron, and other essential nutrients rather than
eating more fast-food, empty-calorie foods such as pretzels
and doughnuts.
SUGGESTION: prepare snacks such as carrot sticks or cheese
and crackers early in the day when fatigue is usually less.
The easiest method for determining if a
woman’s caloric intake is adequate is assessing
the weight she is gaining.
PROTEIN NEEDS
ADEQUATE PROTEIN INTAKE
to build a body framework
also help prevent complications of pregnancy such as pregnancy-
induced hypertension or preterm birth
NOTE:
Be careful when nutrition counseling not to make general statements
such as, “Eat high-protein foods.” Food in the supermarket, after all, is
not labeled “high-protein.” Instead, provide advice in more specific
terms: “Eat three servings of some type of meat or fish every day.”
• The DRI for protein in women is 46 g/d.
• During pregnancy, the need for protein increases to 71
g daily.
• If protein needs are met, overall nutritional needs are
likely to be met as well(with the possible exceptions of
vitamins C, A, and D) because of the high
incorporation of other nutrients with protein foods.
• A woman with a family history of high cholesterol levels
(hypercholesterolemia) probably should not eat more than
two or three eggs per week because of the high cholesterol
content of eggs.
• Encourage such women to eat lean meat, to cook with olive
oil instead of lard or butter, and to remove the skin from
poultry to reduce its fat content.
• She also should not eat lunch meats such as bologna or
salami as food staples, because their protein content may
not be high and their fat content is invariably exceptionally
high.
Milk is a rich source of protein.
Nonfat milk supplies the same protein and half the calories
as regular milk and is very low in fat.
Yogurt or cheese may also be substituted for milk, or milk
may be incorporated into custards, eggnogs, or cream soups.
Women who are lactose intolerant can add a lactase
supplement, buy lactose-free milk, or take a calcium
supplement.
FAT NEEDS
• Only linoleic acid, an essential fatty acid necessary for new cell
growth, cannot be manufactured in the body from other sources.
• Using vegetable oils (e.g., safflower, corn, olive, peanut, and
cottonseed) that have a low cholesterol content rather than
animal oils (butter) is recommended for all adults as a means of
preventing hypercholesterolemia and coronary heart disease.
• Women should also try and ingest omega-3 oils, found primarily in
fish, omega-3–fortified eggs, and the newer omega-3–fortified
spreads.
VITAMIN NEEDS
VITAMIN DEFICIENCY
VITAMIN D-can begin to diminish both fetal and maternal mineral
bone density.
Lack of vitamin A results in tender gums and poor night vision.
Women who were taking oral contraceptives before they became
pregnant should be certain to include good sources of vitamins A and
B and folic acid in early pregnancy.
VITAMIN DEFICIENCY
Counsel women not to use mineral oil as a laxative.
If a woman is housebound, be certain that she is taking a prenatal
vitamin containing vitamin D because she is probably not receiving
as much sun exposure as normally
Megadoses of vitamin C may cause withdrawal scurvy in the infant at
birth.
excessive vitamin A intake and fetal malformation. It is well
documented that the intake of excessive vitamin A in the form of
isotretinoin (Accutane), a medication prescribed for acne, causes
congenital anomalies
VITAMIN DEFICIENCY
FOLIC ACID- Found predominantly in fresh fruits and vegetables.
Necessary for red blood cell formation.
Without adequate folic acid, a megaloblastic anemia (large but
ineffective red blood cells) may develop.
important in preventing neural tube defects.
Take prenatal vitamins that contains a folic acid supplement of 0.4 to
1.0 mg
MINERAL NEEDS
CALCIUM AND PHOSPHORUS
• 8th week- Tooth formation begins
• 12th week- Bones begin to calcify
• The recommended amount of calcium during
pregnancy is 1300 mg
• Most foods high in protein are also high in
phosphorus, so by eating high-protein foods, women
receive enough phosphorus, also important for bone
growth.
IODINE
• Iodine is essential for the formation of thyroxine and,
therefore, for the proper functioning of the thyroid gland.
• If iodine deficiency occurs, it can cause hypothyroidism and
thyroid enlargement (goiter) in a woman.
• Thyroid enlargement in a fetus at birth is serious because the
increased pressure of the enlarged gland on the airway. If
not discovered at birth, hypothyroidism may lead to the
infant’s being cognitively challenged.
IODINE
• The DRI for iodine is 220 g daily during pregnancy.
Seafood is the best source of iodine. In areas where the
water and soil are known to be deficient in iodine, it is
suggested that women use iodized salt rather than plain salt
to ensure a healthy iodine intake.
IRON
• A fetus at term has a hemoglobin level of 17 to 21 g per
100 mL of blood
• Iron is needed to build this high level of hemoglobin.
• After week 20 of pregnancy fetus begins to store iron in
the liver to last through the first 3 months of life
• A woman needs iron to build an increased red cell volume
for herself and to protect against iron lost in blood at birth.
IRON
• The DRI for iron for pregnant women is 27 mg.
• An average diet supplies about 6 mg of iron per 1000
calories.
• If a woman eats a 2500-calorie diet daily, her daily intake,
therefore, is about 15 mg iron. Because only 10% to 20% of
dietary iron is absorbed, she is actually taking in less than
this amount (closer to 1.5 to 3 mg).
• Therefore, dietary supplementation with 15 mg iron per day
helps ensure that adequate iron is ingested and absorbed.
IRON
• Oral iron compounds turn stools black or blackish green.
• The compounds can be irritating to the stomach or cause
constipation in some women.
INTERVENTION:
increase fluid intake or fiber to relieve the constipation.
Some may need a prescribed stool softener such as
docusate sodium (Colace)
FLUORIDE
Because fluoride aids in the formation of sound
teeth, a pregnant woman should drink fluoridated
water.
Fluoride in large amounts causes brown-stained
teeth, so a woman should not take the supplement
more often than prescribed or if tap water in her area
is already fluoridated.
SODIUM
Sodium is the major electrolyte that acts to maintain fluid in the body
Retaining enough fluid during pregnancy in the maternal circulation is
important to ensure a pressure gradient to allow optimal exchange of
nutrients across the placenta.
Too much salt could result in retention of excessive amounts of fluid,
putting a strain on the heart as blood volume doubles.
ZINC
Zinc is necessary for the synthesis of DNA and RNA.
Although not proved, zinc deficiency may be associated with preterm
birth.
The DRI for zinc during pregnancy is 12 mg, or an increase of 3 mg
over pre-pregnancy needs.
Most people who take in adequate protein also take in adequate zinc
because zinc is contained in foods such as meat, liver, eggs, and
seafood. It is also a component of prenatal vitamins to help ensure an
adequate intake.
FLUID NEEDS
Two or three glasses of fluid daily over and above the
three servings of milk recommended by the food
pyramid is a common recommendation during
pregnancy (a total of six to eight glasses daily).
FIBER NEEDS
Eating fiber-rich foods, foods consisting of parts of
the plant cell wall resistant to normal digestive
enzymes such as broccoli and asparagus, are a natural
way of preventing constipation, because the bulk of
the fiber left in the intestine aids evacuation.
Fiber also has the advantage of lowering cholesterol
levels and may remove carcinogenic contaminants
from the intestine.
Dietary Reference Intakes for
Pregnant and Nonpregnant Women
FOODS TO AVOID OR LIMIT IN
PREGNANCY
EXCESS SEAFOODS
• Women should eat up to 12 ounces (2 to 3 meals) of seafood or shellfish a
week for their omega-3 and iodine content.
• Fish such as shark, swordfish, king mackerel or tilefish are high in mercury
contamination, however, so should be avoided.
• Five types of fish that are low in mercury:
1. Shrimp
2. canned light tuna
3. Salmon
4. Pollock
5. catfish.
FOODS WITH CAFFEINE
• Caffeine a central nervous system stimulant capable of increasing
heart rate, urine production in the kidney, and secretion of acid in the
stomach.
• A daily intake of caffeine of two or three cups of coffee has not been
associated with low birth weight, but drinking over three cups is
associated with an increased rate of early miscarriage (Applebee,
2008).
• To limit their caffeine intake, women may need to limit not only the
amount of coffee they drink but also other sources of caffeine such as
chocolate, soft drinks, and tea.
FOODS WITH CAFFEINE
• Decaffeinated coffee, as the name implies, contains almost no caffeine. The
longer tea brews, the greater is the caffeine content.
• Green tea has less caffeine than black tea. Both herbal teas and
decaffeinated tea are readily available.
• The cocoa bean that is used to make chocolate and cocoa is yet another
natural source of caffeine.
• Chocolate sources tend to be low in caffeine, however, compared with
coffee. A cup of coffee contains approximately 120 mg of caffeine, whereas a
cup of hot chocolate contains only 10 mg.
• Baking chocolate, used for cake frostings and glazes, is proportionately higher,
containing about 35 mg of caffeine per ounce.
• Soft drinks do not naturally contain caffeine; it is added to improve their
flavor. To limit the amount of caffeine consumed, encourage pregnant women
to choose caffeine free types
What if...
Tori Alarino states, “I love coffee. There’s always a pot
brewing where I work. And I love a cup of cappuccino
for lunch.” What suggestions could you make to help
her reduce her caffeine intake?
WEIGHT LOSS DIETS
• As a rule, weight reduction is not healthy during pregnancy. Liquid
reducing diets and/or diets that are combined with weight-reducing
drugs are particularly contraindicated during pregnancy because they
may lead to fetal ketoacidosis and poor growth. If women have been
following such diets before becoming pregnant, they may have few
nutritional stores, and additional vitamin supplementation may be
necessary
NUTRITIONAL RISK FACTORS
DURING PREGNANCY
AREAS TO BE ASSESSED FOR A
TOTAL NUTRITION HISTORY
PHYSICAL SIGNS AND SYMPTOMS
OF ADEQUATE PREGNANCY
NUTRITION
MANAGING COMMON PROBLEMS
AFFECTING NUTRITIONAL HEALTH
Nausea and Vomiting
CAUSES:
Sensitivity to the high level of chorionic gonadotropin hormone
produced by the trophoblast cells
High estrogen or progesterone levels
Lowered maternal blood sugar caused by the needs of the developing
embryo
Lack of pyridoxine
Diminished gastric motility
Nausea is aggravated by fatigue and may be aggravated by emotional
disturbance.
Nausea and Vomiting
Methods such as acupressure or avoiding fluid with meals are
effective for some women.
Mild-flavored ginger tea may be helpful
Increasing carbohydrate intake seems to relieve nausea better than
any other nutrition remedy.
The traditional solution is for women to keep dry crackers/saltines,
such as Saltines, by their bedside and eat a few before rising; sourball
candies may serve the same purpose.
A woman can then eat a light breakfast or delay breakfast until 10
or 11 AM, past the time her nausea seems to persist.
CRAVINGS
• During pregnancy, some women report an abnormal craving for nonfood
substances (termed pica from the Latin word for “magpie,” a bird that
is an indiscriminate eater).
• The most common form of pica in the past was a craving for laundry
starch.
Always ask women at prenatal visits if they crave any nonfood items, as
most women do not supply this information unless asked directly.
Encouraging a woman to stop eating the nonfood substance may not be
effective because the habit may be deeply ingrained. Because pica is a
symptom that often accompanies iron deficiency anemia, correcting this
underlying problem with an iron supplement may correct the pica.
At subsequent visits, be certain to assess if a woman’s hemoglobin is
increasing and ask if she notices any difference in her cravings.
HEARTBURN (PYROSIS)
Common suggestions to help prevent reflux into the esophagus are:
Eat small meals frequently rather than large meals.
Sleep on the left side with two pillows to elevate the upper torso.
Do not lie down immediately after eating; try and wait at least 2
hours.
Avoid fatty and fried foods, coffee, carbonated beverages, tomato
products, and citrus juices
Aluminum hydroxide (Amphojel, Alternagel) or a combination of
aluminum and magnesium hydroxide (Maalox) may be prescribed for
relief.
HYPERCHOLESTEROLEMIA
A woman who has had difficulty with hypercholesterolemia before
pregnancy may need to continue to eat only moderate amounts of fat during
pregnancy to prevent any increase in cholesterol. Helpful ways to reduce
cholesterol include:
• Exercising daily
• Eating oat cereal
• Broiling meat rather than frying it
• Using a minimum of salad oils
• Substituting new omega-3 products in place of butter
• Eating fish high in omega-3 oil, such as salmon or trout
Potrebbero piacerti anche
- GROUP 1 Nutrition in Pregnancy and LactationDocumento27 pagineGROUP 1 Nutrition in Pregnancy and LactationKaye NaigNessuna valutazione finora
- Nutrition For Pregnant WomanDocumento22 pagineNutrition For Pregnant WomanSukma PratiwiNessuna valutazione finora
- Pregnancy and Nutrition Lec M1Documento43 paginePregnancy and Nutrition Lec M1Judea PagedpedNessuna valutazione finora
- Nutrition In pregnancy Nourish yourself and your babyDa EverandNutrition In pregnancy Nourish yourself and your babyNessuna valutazione finora
- Breast Milk: Benefits & BarriersDocumento22 pagineBreast Milk: Benefits & BarriersNazia ArifNessuna valutazione finora
- Myths and Facts About InfertilityDocumento6 pagineMyths and Facts About Infertilityabha bhatt100% (2)
- FC - Lactation and Infant Feeding - Nov 1 - 2021Documento22 pagineFC - Lactation and Infant Feeding - Nov 1 - 2021Dorian HoussouNessuna valutazione finora
- Pregnancy Nutrition: Action Steps to Ensure a Healthy ChildDa EverandPregnancy Nutrition: Action Steps to Ensure a Healthy ChildNessuna valutazione finora
- Fanconi Anemia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDa EverandFanconi Anemia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNessuna valutazione finora
- Ovulation DR JRDocumento28 pagineOvulation DR JRtarajanejo100% (1)
- Radiology of Obstetrics and GynaecologyDocumento61 pagineRadiology of Obstetrics and GynaecologyMUBIRU SAMUEL EDWARDNessuna valutazione finora
- Diet During LactationDocumento4 pagineDiet During LactationVineetha Vineesh100% (1)
- Newer Insulin in Diabetic Pregnancy - PPT'Documento56 pagineNewer Insulin in Diabetic Pregnancy - PPT'Hemamalini100% (1)
- Thyroid Disorders in PregnancyDocumento17 pagineThyroid Disorders in PregnancyFemale calmNessuna valutazione finora
- 1st & 2nd Trimester Pregnancy LossDocumento48 pagine1st & 2nd Trimester Pregnancy LossAbdullah EssaNessuna valutazione finora
- Family Planning: What Are The Advantages of A Contraceptive Injection?Documento2 pagineFamily Planning: What Are The Advantages of A Contraceptive Injection?Adrian Clyde BautistaNessuna valutazione finora
- AED 2020-Gruidebook For Nutritionat Treatment of Eating DisordersDocumento63 pagineAED 2020-Gruidebook For Nutritionat Treatment of Eating DisordersNaiaraNessuna valutazione finora
- What Is Breastfeeding? Benefits of Breastfeeding?: Lessens The Risk of SIDSDocumento2 pagineWhat Is Breastfeeding? Benefits of Breastfeeding?: Lessens The Risk of SIDSGarmaine ApostolNessuna valutazione finora
- Breastfeeding Manual Jan 31 2023Documento43 pagineBreastfeeding Manual Jan 31 2023Aqsa Munir100% (1)
- Acute Fatty Liver Versus HELLPDocumento44 pagineAcute Fatty Liver Versus HELLPrainmaker77771121100% (1)
- Perineal Care ProcedureDocumento12 paginePerineal Care ProcedureShikarin KitaNessuna valutazione finora
- Tutorial 6Documento54 pagineTutorial 6ShenariNessuna valutazione finora
- Natural Fertility GuideDocumento29 pagineNatural Fertility GuideGabi100% (1)
- Diet in PregnancyDocumento9 pagineDiet in PregnancyGERONA GABRYLE MARCNessuna valutazione finora
- Management of Pregnant PatientDocumento113 pagineManagement of Pregnant PatientWilliam BharathNessuna valutazione finora
- Self Study Module BreastfeedingDocumento151 pagineSelf Study Module BreastfeedingΕρη Ριρι100% (3)
- Lactation ManagementDocumento13 pagineLactation ManagementNadia Nur Salsabila50% (2)
- DHEA Final PresentationDocumento140 pagineDHEA Final PresentationSundar Narayanan100% (1)
- Nutr 304 Meal Planning ProjectDocumento45 pagineNutr 304 Meal Planning Projectapi-484988117Nessuna valutazione finora
- Judi Januadi Endjun: Gatot Soebroto Army Central Hospital/ Medical Faculty, University of Indonesia ISUOG, Bali, 2009Documento66 pagineJudi Januadi Endjun: Gatot Soebroto Army Central Hospital/ Medical Faculty, University of Indonesia ISUOG, Bali, 2009emilyakmanNessuna valutazione finora
- Maternal NutritionDocumento16 pagineMaternal NutritionAbdur RehmanNessuna valutazione finora
- ESHRE RPL Guideline - 28112017 - FINAL PDFDocumento154 pagineESHRE RPL Guideline - 28112017 - FINAL PDFAna MarianaNessuna valutazione finora
- 18 Colorectal Polyps and CarcinomaDocumento89 pagine18 Colorectal Polyps and Carcinomasuhaib ananzehNessuna valutazione finora
- Male Repro Problems 2022 With NotesDocumento65 pagineMale Repro Problems 2022 With NotesNikky Silvestre100% (1)
- Acute Abdomen in Pregnancy 2Documento54 pagineAcute Abdomen in Pregnancy 2jhobarryNessuna valutazione finora
- Summary of Product CharacteristicsDocumento15 pagineSummary of Product Characteristicsddandan_2Nessuna valutazione finora
- Benefits of Breast FeedingDocumento4 pagineBenefits of Breast FeedingAzAm KiOngNessuna valutazione finora
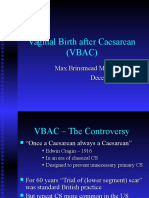
- Vaginal Birth After Caesarean (Vbac) : Max Brinsmead MB Bs PHD December 2015Documento36 pagineVaginal Birth After Caesarean (Vbac) : Max Brinsmead MB Bs PHD December 2015kikyNessuna valutazione finora
- DIsease, Compli, and DT in Obstetrics PDFDocumento549 pagineDIsease, Compli, and DT in Obstetrics PDFKiki Afifana100% (2)
- In Vitro Fertilisation Treatment and Factors Affecting SuccessDocumento12 pagineIn Vitro Fertilisation Treatment and Factors Affecting SuccessNguyễnHoàiNamNessuna valutazione finora
- Menstruation: Learning OutcomesDocumento87 pagineMenstruation: Learning OutcomesKimberly Whitfield (Kim)100% (2)
- Mother's Class ExerciseDocumento40 pagineMother's Class ExerciseRA TranceNessuna valutazione finora
- Prenatal Care: Williams ObstetricsDocumento43 paginePrenatal Care: Williams Obstetricsgayon09Nessuna valutazione finora
- Gastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDa EverandGastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNessuna valutazione finora
- Anemiain PregnancyDocumento4 pagineAnemiain PregnancyShalini ShanmugalingamNessuna valutazione finora
- A Complete Guide for First-Time Mommies: Healthy Pregnancy, Hospital Preparation, Post-Delivery CareDa EverandA Complete Guide for First-Time Mommies: Healthy Pregnancy, Hospital Preparation, Post-Delivery CareNessuna valutazione finora
- Detty S2 Gizi Nutrition PreconceptionDocumento25 pagineDetty S2 Gizi Nutrition PreconceptionyuniarsyNessuna valutazione finora
- Nutrition in PregnancyDocumento5 pagineNutrition in PregnancyCatalin SimionNessuna valutazione finora
- Iron Deficiency Anaemia in Toddlers: Learning PointsDocumento8 pagineIron Deficiency Anaemia in Toddlers: Learning PointsAfiqah So JasmiNessuna valutazione finora
- Pelvic Organ Prolapse - Dr. QueDocumento55 paginePelvic Organ Prolapse - Dr. QueMenjale JulaoNessuna valutazione finora
- Up Dated Respectiful Maternity Care (RMC)Documento21 pagineUp Dated Respectiful Maternity Care (RMC)nyangaraNessuna valutazione finora
- Breast Feeding Is The Normal Way of Providing Young Infants With The Nutrients They Need For Healthy Growth and DevelopmentDocumento8 pagineBreast Feeding Is The Normal Way of Providing Young Infants With The Nutrients They Need For Healthy Growth and Developmentdanee しNessuna valutazione finora
- Progesterone in PregnancyDocumento59 pagineProgesterone in PregnancyKaruna Indoliya100% (2)
- BreastfeedingDocumento6 pagineBreastfeedingGreggy Francisco LaraNessuna valutazione finora
- Pcos 170123144542Documento86 paginePcos 170123144542Dewi Puspita Apsari100% (2)
- Micronutrients in PregnancyDocumento6 pagineMicronutrients in Pregnancykhalisah alhadarNessuna valutazione finora
- Epidemiology of Childhood Cancer in "Dharmais" Cancer HospitalDocumento16 pagineEpidemiology of Childhood Cancer in "Dharmais" Cancer HospitalIndonesian Journal of CancerNessuna valutazione finora
- CPG Intrapartum and Immediate Postpartum Care PDFDocumento52 pagineCPG Intrapartum and Immediate Postpartum Care PDFAngela SaldajenoNessuna valutazione finora
- Digital Photography Project RubricDocumento1 paginaDigital Photography Project Rubricrj100% (2)
- ENDORSEMENT FORM Converted MergedDocumento2 pagineENDORSEMENT FORM Converted MergedrjNessuna valutazione finora
- Lecture Basic Tools in NutritionDocumento47 pagineLecture Basic Tools in Nutritionrj100% (1)
- Diet For Pregnancy and Lactating WomenDocumento49 pagineDiet For Pregnancy and Lactating WomenrjNessuna valutazione finora
- ElderlyDocumento19 pagineElderlyrjNessuna valutazione finora
- Calendar Weekly PlannerDocumento12 pagineCalendar Weekly PlannerrjNessuna valutazione finora
- OILSDocumento12 pagineOILSrjNessuna valutazione finora
- Deficiency and ToxicityDocumento19 pagineDeficiency and ToxicityrjNessuna valutazione finora
- Calendar Weekly PlannerDocumento12 pagineCalendar Weekly PlannerrjNessuna valutazione finora
- By: Rhodeva Joy T. Braga, RN, MancDocumento17 pagineBy: Rhodeva Joy T. Braga, RN, MancrjNessuna valutazione finora
- Deficiency and ToxicityDocumento19 pagineDeficiency and ToxicityrjNessuna valutazione finora
- DOXYCYCLINEDocumento2 pagineDOXYCYCLINErj100% (1)
- Digital Photography RubricssssDocumento1 paginaDigital Photography RubricssssrjNessuna valutazione finora
- By: Rhodeva Joy T. Braga, RN, MancDocumento17 pagineBy: Rhodeva Joy T. Braga, RN, MancrjNessuna valutazione finora
- Drug StudyDocumento2 pagineDrug StudyrjNessuna valutazione finora
- Digital Photography Project RubricDocumento1 paginaDigital Photography Project RubricrjNessuna valutazione finora
- Subject EvaluationDocumento1 paginaSubject EvaluationrjNessuna valutazione finora
- PermutationDocumento5 paginePermutationrjNessuna valutazione finora
- Hypothesis ProblemsDocumento7 pagineHypothesis Problemsrj0% (1)
- MnemonicsDocumento15 pagineMnemonicsrj94% (18)
- SCHISTOSOMIASISDocumento2 pagineSCHISTOSOMIASISrjNessuna valutazione finora
- CeftriaxoneDocumento1 paginaCeftriaxonerjNessuna valutazione finora
- Sayyid DynastyDocumento19 pagineSayyid DynastyAdnanNessuna valutazione finora
- EDCA PresentationDocumento31 pagineEDCA PresentationToche DoceNessuna valutazione finora
- DHBVNDocumento13 pagineDHBVNnitishNessuna valutazione finora
- Europe Landmarks Reading Comprehension Activity - Ver - 1Documento12 pagineEurope Landmarks Reading Comprehension Activity - Ver - 1Plamenna Pavlova100% (1)
- Syllabus Biomekanika Kerja 2012 1Documento2 pagineSyllabus Biomekanika Kerja 2012 1Lukman HakimNessuna valutazione finora
- EMI - Module 1 Downloadable Packet - Fall 2021Documento34 pagineEMI - Module 1 Downloadable Packet - Fall 2021Eucarlos MartinsNessuna valutazione finora
- JD For Library Interns Sep 2023Documento2 pagineJD For Library Interns Sep 2023Bharat AntilNessuna valutazione finora
- APA CitationsDocumento9 pagineAPA CitationsIslamNessuna valutazione finora
- SQ1 Mogas95Documento1 paginaSQ1 Mogas95Basant Kumar SaxenaNessuna valutazione finora
- People Vs Felipe Santiago - FCDocumento2 paginePeople Vs Felipe Santiago - FCBryle DrioNessuna valutazione finora
- Theo Hermans (Cáp. 3)Documento3 pagineTheo Hermans (Cáp. 3)cookinglike100% (1)
- Learner's Material: ScienceDocumento27 pagineLearner's Material: ScienceCarlz BrianNessuna valutazione finora
- Port of Surigao Guide To EntryDocumento1 paginaPort of Surigao Guide To EntryNole C. NusogNessuna valutazione finora
- Abramson, Glenda (Ed.) - Oxford Book of Hebrew Short Stories (Oxford, 1996) PDFDocumento424 pagineAbramson, Glenda (Ed.) - Oxford Book of Hebrew Short Stories (Oxford, 1996) PDFptalus100% (2)
- Kofax Cross Product Compatibility MatrixDocumento93 pagineKofax Cross Product Compatibility MatrixArsh RashaNessuna valutazione finora
- Science Project FOLIO About Density KSSM Form 1Documento22 pagineScience Project FOLIO About Density KSSM Form 1SarveesshNessuna valutazione finora
- Visual Images of America in The Sixteenth Century: Elaine BrennanDocumento24 pagineVisual Images of America in The Sixteenth Century: Elaine Brennanjoerg_spickerNessuna valutazione finora
- First Aid General PathologyDocumento8 pagineFirst Aid General PathologyHamza AshrafNessuna valutazione finora
- Monastery in Buddhist ArchitectureDocumento8 pagineMonastery in Buddhist ArchitectureabdulNessuna valutazione finora
- Animal Welfare in Bangladesh and The Role of Obhoyaronno CaseDocumento11 pagineAnimal Welfare in Bangladesh and The Role of Obhoyaronno CaseZarin Tanjim WoyshorjoNessuna valutazione finora
- 23 East 4Th Street NEW YORK, NY 10003 Orchard Enterprises Ny, IncDocumento2 pagine23 East 4Th Street NEW YORK, NY 10003 Orchard Enterprises Ny, IncPamelaNessuna valutazione finora
- Concept of HalalDocumento3 pagineConcept of HalalakNessuna valutazione finora
- 1986 Elektric M InfoDocumento1 pagina1986 Elektric M InfoDanielDiasNessuna valutazione finora
- Understanding SIP RE-INVITEDocumento6 pagineUnderstanding SIP RE-INVITESK_shivamNessuna valutazione finora
- Chain of CommandDocumento6 pagineChain of CommandDale NaughtonNessuna valutazione finora
- Pa Print Isang Beses LangDocumento11 paginePa Print Isang Beses LangGilbert JohnNessuna valutazione finora
- Harvard ReferencingDocumento7 pagineHarvard ReferencingSaw MichaelNessuna valutazione finora
- Outline - Criminal Law - RamirezDocumento28 pagineOutline - Criminal Law - RamirezgiannaNessuna valutazione finora
- 2017 - The Science and Technology of Flexible PackagingDocumento1 pagina2017 - The Science and Technology of Flexible PackagingDaryl ChianNessuna valutazione finora
- Hydraulics Experiment No 1 Specific Gravity of LiquidsDocumento3 pagineHydraulics Experiment No 1 Specific Gravity of LiquidsIpan DibaynNessuna valutazione finora