Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Ectopic Pregnancy
Caricato da
Rima Hajjar0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
9 visualizzazioni26 pagineCopyright
© © All Rights Reserved
Formati disponibili
PPTX, PDF, TXT o leggi online da Scribd
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
© All Rights Reserved
Formati disponibili
Scarica in formato PPTX, PDF, TXT o leggi online su Scribd
0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
9 visualizzazioni26 pagineEctopic Pregnancy
Caricato da
Rima HajjarCopyright:
© All Rights Reserved
Formati disponibili
Scarica in formato PPTX, PDF, TXT o leggi online su Scribd
Sei sulla pagina 1di 26
Ectopic Pregnancy
Rima Hajjar PGY1
Definition
An ectopic or extrauterine
pregnancy is one in which the
blastocyst implants anywhere other
than the endometrial lining of the
uterine cavity.
Location
Heterotopic Pregnancy
Epidemiology
Epidemiology
2.7% of all pregnancy-related deaths
The prevalence of ectopic pregnancy among
women presenting with first-trimester
vaginal bleeding, or abdominal pain, or both,
is as high as 18%
Risk factors
50% Unknown
Prior ectopic pregnancy ( 10% recurrence for 1 prior , 25% if more)
PID
Tubal surgery
Infertility
ART
IUD?
Diagnostic tools
Every sexually active, reproductive-aged woman presenting with
abdominal pain or vaginal bleeding should be screened for pregnancy,
regardless of whether she is currently using contraception
Ultrasound
Gestational sac = 4.5 -5 weeks
Yolk Sac = 5-6 weeks
Fetal pole with cardiac activity =5.5-6 weeks
US can definitively diagnose an ectopic pregnancy when a gestational
sac with a yolk sac, or embryo, or both, is noted in the adnexa
however, most ectopic pregnancies do not progress to this stage
Therefore, findings of a mass that is separate from the ovary should
raise suspicion for the presence of an ectopic pregnancy.
Ultrasound
US limitations
PPV only 80% because findings can be confused with pelvic structures,
such as a paratubal cyst, corpus luteum, hydrosalpinx, endometrioma,
or bowel
Although an early intrauterine gestational sac may be visualized as
early as 5 weeks of gestation, definitive intrauterine pregnancy includes
visualization of a gestational sac with a yolk sac or embryo
Visualization of a definitive intrauterine pregnancy eliminates ectopic
pregnancy except in the rare case of a heterotopic pregnancy
Although a hypoechoic “sac-like” structure) in the uterus likely
represents an intrauterine gestation, it also may represent a
pseudogestational sac, which is a collection of fluid or blood in the
uterine cavity that is sometimes visualized with ultrasonography in
women with an ectopic pregnancy
B-HCG
Surrogate for gestational age
Discriminatory Level : “ hCG value above which the landmarks of a
normal intrauterine gestation should be visible on ultrasonography. ”
The absence of a possible gestational sac on ultrasound in the
presence of a hCG measurement above the discriminatory level strongly
suggests a nonviable gestation (an early pregnancy loss or an ectopic
pregnancy)
Trends of Serial Serum Human
Chorionic Gonadotropin
A single hCG concentration measurement cannot diagnose viability or
location of a gestation.
Serial hCG concentration measurements are used to differentiate
normal from abnormal pregnancies
A second hCG value measurement is recommended 2 days after the
initial measurement to assess for an increase or decrease
Medical Management
Medical management with methotrexate can be considered for women
with a confirmed or high clinical suspicion of ectopic pregnancy who are
hemodynamically stable, who have an unruptured mass ,and who do
not have absolute contraindications to methotrexate administration.
These patients generally also are candidates for surgical management.
Methotraxate
Contraindications
Different protocols
three published protocols for the administration of methotrexate to
treat ectopic pregnancy:
1) a single-dose protocol
2) a two-dose protocol
3) a fixed multiple-dose protocol
No consensus regarding the best protocol.
Choice should be guided by initial B-HCG
Adverse effects of
Methotraxate
Counseling
Risk of ectopic pregnancy rupture
Avoiding certain foods, supplements
folic acid supplements, foods that contain folic acid, and nonsteroidal
antiinflammatory drug ( Decreased efficacy )
narcotic analgesic medications, alcohol, and gas-producing foods (
Mask symptoms of rupture )
Abstain from sexual intercourse
Risk of rupture
Teratogenicity
How does methotrexate treatment
affect subsequent fertility?
No effect on subsequent fertility
No effect on ovarian reserve
Potrebbero piacerti anche
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- AWHONN High-Risk & Critical Care Obstetrics (2012)Documento440 pagineAWHONN High-Risk & Critical Care Obstetrics (2012)Rima Hajjar100% (2)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- In The Second Stage of LaborDocumento5 pagineIn The Second Stage of Laborravensclaw001Nessuna valutazione finora
- Obstetric Nursing RevisedDocumento345 pagineObstetric Nursing Revisedkarendelarosa06100% (1)
- Normal Abnormal LabourDocumento63 pagineNormal Abnormal LabourFelicianna Ashwinie StanleyNessuna valutazione finora
- Obstetrics and GynecologyDocumento4 pagineObstetrics and Gynecologychuppepay100% (3)
- Abnormalities of Amniotic FluidDocumento27 pagineAbnormalities of Amniotic FluidRukmini kakatikar0% (1)
- 3rd Stage of LabourDocumento22 pagine3rd Stage of Labourvarshasharma05100% (6)
- OB-2-SIR-KEN LDocumento5 pagineOB-2-SIR-KEN LLyrechel de GuzmanNessuna valutazione finora
- Premature Rupture of Membranes PromDocumento15 paginePremature Rupture of Membranes PromRima HajjarNessuna valutazione finora
- Case Report - PromDocumento16 pagineCase Report - PromFauziyyahrNessuna valutazione finora
- IncontinenceDocumento34 pagineIncontinenceRima HajjarNessuna valutazione finora
- Breast MassesDocumento25 pagineBreast MassesRima HajjarNessuna valutazione finora
- CREOG2Documento1 paginaCREOG2Rima HajjarNessuna valutazione finora
- STIDocumento53 pagineSTIRima HajjarNessuna valutazione finora
- Abnormal Uterine BleedingDocumento18 pagineAbnormal Uterine BleedingRima HajjarNessuna valutazione finora
- Preterm Labour (PTL) : Antenatal CareDocumento10 paginePreterm Labour (PTL) : Antenatal CareRima HajjarNessuna valutazione finora
- Obstetric Cholestasis (OC) : MaternalDocumento3 pagineObstetric Cholestasis (OC) : MaternalRima HajjarNessuna valutazione finora
- Pachychoroid PDFDocumento9 paginePachychoroid PDFRima HajjarNessuna valutazione finora
- Pre-Eclampsia PET and EclampsiaDocumento7 paginePre-Eclampsia PET and EclampsiaRima HajjarNessuna valutazione finora
- Gestational Diabetes Mellitus GDMDocumento4 pagineGestational Diabetes Mellitus GDMRima HajjarNessuna valutazione finora
- Antenatal CareDocumento7 pagineAntenatal CareRima HajjarNessuna valutazione finora
- Different Prostaglandin FunctionsDocumento1 paginaDifferent Prostaglandin FunctionsRima HajjarNessuna valutazione finora
- Case DISCUSSIONDocumento2 pagineCase DISCUSSIONRima HajjarNessuna valutazione finora
- Step 1 REVIEWDocumento140 pagineStep 1 REVIEWRima HajjarNessuna valutazione finora
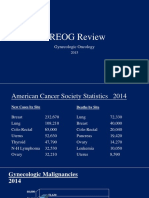
- CREOGGYNREVIEW PP PDFDocumento98 pagineCREOGGYNREVIEW PP PDFRima HajjarNessuna valutazione finora
- 2015 Oncology CREOG Review PDFDocumento76 pagine2015 Oncology CREOG Review PDFRima HajjarNessuna valutazione finora
- Alternate Dosing Protocol For Magnesium Sulfate In.18 PDFDocumento5 pagineAlternate Dosing Protocol For Magnesium Sulfate In.18 PDFRima HajjarNessuna valutazione finora
- Early Pregnancy LossDocumento20 pagineEarly Pregnancy LossRima HajjarNessuna valutazione finora
- Bleeding Dr. Sally Temraz - March 2, 2015Documento1 paginaBleeding Dr. Sally Temraz - March 2, 2015Rima HajjarNessuna valutazione finora
- The Autonomic Nervous System (ANS) : K, S & J, CH 47 HandoutDocumento27 pagineThe Autonomic Nervous System (ANS) : K, S & J, CH 47 HandoutRima HajjarNessuna valutazione finora
- Physiology of PuerperiumDocumento19 paginePhysiology of PuerperiumSunil RamchandaniNessuna valutazione finora
- Hipertensi Pada Ibu Hamil Trimester 3Documento8 pagineHipertensi Pada Ibu Hamil Trimester 3deskha putriNessuna valutazione finora
- How To Do An Abortion With PillsDocumento8 pagineHow To Do An Abortion With PillsGlenn Asuncion PagaduanNessuna valutazione finora
- Pa Rajshekar Specialist in Obg Al Bukariya General HospitalDocumento28 paginePa Rajshekar Specialist in Obg Al Bukariya General HospitalDedy Tesna AmijayaNessuna valutazione finora
- Formation of Twins Formation of Twins: Adawiyah - Athirah Humaira - Nur Ilham Syifa' - Marsya MunharDocumento7 pagineFormation of Twins Formation of Twins: Adawiyah - Athirah Humaira - Nur Ilham Syifa' - Marsya MunharnurfatihahNessuna valutazione finora
- Assessment of High-Risk PregnancyDocumento23 pagineAssessment of High-Risk PregnancyNiña Ricci MtflcoNessuna valutazione finora
- BMJ 2022 071653.fullDocumento16 pagineBMJ 2022 071653.fullANDREA LORENA GARZON LADINONessuna valutazione finora
- ObstetricsDocumento23 pagineObstetricsSundar MuneesNessuna valutazione finora
- BrochureDocumento3 pagineBrochureapi-218300213Nessuna valutazione finora
- A Rare Case Report - Syncephalus Conjoint TwinsDocumento3 pagineA Rare Case Report - Syncephalus Conjoint Twinsalifa9393Nessuna valutazione finora
- Hadlock ChartDocumento7 pagineHadlock Chartmasroork_2Nessuna valutazione finora
- Preeklampsia BeratDocumento5 paginePreeklampsia BeratmelatiigdNessuna valutazione finora
- Blighted OvumDocumento4 pagineBlighted Ovummaria50% (2)
- These Are The Documents Needed in Filing YourDocumento2 pagineThese Are The Documents Needed in Filing YourSuzanne Matuba SaetNessuna valutazione finora
- Fibroids in PregnancyDocumento1 paginaFibroids in PregnancyhanaddulNessuna valutazione finora
- Medical Report BHS InggrisDocumento15 pagineMedical Report BHS InggrisSyifa asqafNessuna valutazione finora
- Vaginal Birth After Caesarean Section (Vbac)Documento16 pagineVaginal Birth After Caesarean Section (Vbac)api-370504650% (2)
- Management of Placenta Previa During Pregnancy: M Hadyan Syahputra 71 2016 055Documento14 pagineManagement of Placenta Previa During Pregnancy: M Hadyan Syahputra 71 2016 055khaira_nNessuna valutazione finora
- Abnormal Labor and Dystocia: Dept. of Ob&Gyn, The First Affiliated Hospital He KeDocumento63 pagineAbnormal Labor and Dystocia: Dept. of Ob&Gyn, The First Affiliated Hospital He KeJoan LuisNessuna valutazione finora
- NFDN 2004 Prenatal Teaching Plan Version A V1.22.2Documento3 pagineNFDN 2004 Prenatal Teaching Plan Version A V1.22.2ᅮᅮAmalNessuna valutazione finora
- Rcog PpromDocumento7 pagineRcog PpromDevi SyamNessuna valutazione finora
- Case DR Priolapse - Preterm, Iufd, PromnDocumento15 pagineCase DR Priolapse - Preterm, Iufd, PromnAL-Neil AntonioNessuna valutazione finora