Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Referat Bronkopneumonia Jul
Caricato da
juliand hidayatTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Referat Bronkopneumonia Jul
Caricato da
juliand hidayatCopyright:
Formati disponibili
REFERAT
BRONKOPNEUMONIA
Oleh :
Juliand Hidayat
030.13.104
Dokter Pembimbing:
dr. Andri Firdaus, Sp.A
Kepaniteraan Klinik Ilmu Kesehatan Anak
Rumah Sakit Umum Daerah Karawang
Universitas Trisakti
2019
BRONKOPNEUMONIA
• Bronchopneumonia can occur at any age, but those who are
more susceptible are children less than 5 years old.
• Various microorganisms can cause bronchopneumonia,
including viruses, fungi and bacteria.
• Steptococcus pneumoniae is the most common
• In Indonesia, pneumonia is also the second leading cause of
death in children under five after diarrhea, which is estimated at
922,000 children.
Kepaniteraan Klinik Ilmu Kesehatan Anak
Rumah Sakitt Umum Daerah Karawang
Universitas Trisakti 2019
Definition
Bronchopneumonia refers to lung inflammation that is focused on the
bronchiole area and alveolus, triggers the production of mucopurulent
exudates which causes small caliber respiratory tracts and causes even
consolidation into adjacent lobules.
Bronchopneumonia more commonly found in infants and children
Kepaniteraan Klinik Ilmu Kesehatan Anak
Rumah Sakitt Umum Daerah Karawang
Universitas Trisakti 2019
Etiology Microorganisms that cause pneumonia by age group:
Usia Etiologi yang sering Etiologi yang jarang
Bakteri Bakteri
E.coli Bakteri anaerob
Streptococcus group B Streptococcus group D
Listeria monocytogenes Haemophilus influenza
Lahir – 20 hari Streptococcus pneumoniae
Ureaplasma urealyticum
• Pneumonia is caused Virus
Virus sitomegalo
by infections of Bakteri
Virus herpes simpleks
Bakteri
microorganisms, Chlamidia trachomatis Bordetella pertusis
Streptococcus pneumoniae Haemophilus influenza tipe
especially viruses and B
3 minggu – 3 bulan Virus Moraxella catharalis
bacteria. Virus adeno Staphylococcus aureus
• Age is an important Virus influenza
Virus parainfluenza
Ureaplasma urealyticum
Virus
factor in the difference Respiratorysyncytial virus Virus sitomegalo
Bakteri Bakteri
in pneumonia in Chlamidia pneumoniae Haemophilus influenza tipe
children. Mycoplasma pneumoniae
B
Moraxella catharalis
Streptococcus pneumonia Neisseria meningitidis
4 bulan – 5 tahun Virus Staphylococcus aureus
Virus adeno Virus
Virus influenza Virus varicella-zoster
Virus parainfluenza
Virus rino
RespiratorySyncytial Virus
Kepaniteraan Klinik Ilmu Kesehatan Anak
Rumah Sakitt Umum Daerah Karawang
Universitas Trisakti 2019
Risk factor
Exposure to cigarette smoke Malnutrition
not exclusive breastfeeding
low economic status low birth weight
Kepaniteraan Klinik Ilmu Kesehatan Anak
Rumah Sakitt Umum Daerah Karawang
Universitas Trisakti 2019
Classification
Infection Predilection Community Pneumonia
Nosocomial Pneumonia
Recurent Pneumonia
Aspiration Pneumonia
Immunocomoramised
Pneumonia
Kepaniteraan Klinik Ilmu Kesehatan Anak
Rumah Sakitt Umum Daerah Karawang
Universitas Trisakti 2019
Classification Pneumonia classification based on WHO:
Baby less than 2 months Children aged 2 months - 5 years
• Severe pneumonia: rapid • Mild pneumonia: rapid
breathing or severe retraction breathing> 50x / minute (2
• Very severe pneumonia: do not months - 1 year) or> 40x /
want to suck / drink, convulsions, minute (> 1-5 years), given oral
lethargy, fever or hypothermia, antibiotics
bradycardia or irregular • Severe pneumonia: retraction,
breathing. shortness of breath
• Pneumonia must be treated and • Very severe pneumonia: can not
given antibiotics: rapid breathing eat / drink, seizures, letargis,
(> 60x / minute), retraction malnutrition
• Not pneumonia: no rapid • Not pneumonia: there is no rapid
breathing, enough symptomatic breathing, only symptomatic
treatment treatment such as fever reducing
Kepaniteraan Klinik Ilmu Kesehatan Anak
Rumah Sakitt Umum Daerah Karawang
Universitas Trisakti 2019
Patofisiology
defense mechanism
virulensi organisme me↑
disturbed
virus
bacteria
Invasion of microorganisms into Me↓ integrity structural
the lower airway (inhalation or sel alveolar tipe II dan i
commensal floral aspiration) surfactan production
Inflammatory response leukocyte formed hyaline membrane
migration to the focus of infection, and pulmonary edema
release of toxic substances, activation of
the complement cascade Dispnea
Kepaniteraan Klinik Ilmu Kesehatan Anak
Rumah Sakitt Umum Daerah Karawang
Universitas Trisakti 2019
Patofisiology
1. Congestion Stadium 2. Red hepatization
(First 4-12 hours) stadium (48 hours later)
4 Stadium
3. Gray Hepatization
4. Resolution Stadium
Stadium
(8-11 days)
(3-8 days)
Kepaniteraan Klinik Ilmu Kesehatan Anak
Rumah Sakitt Umum Daerah Karawang
Universitas Trisakti 2019
Sign & Symptomps
• General infection • Respiration disorders
First upper respiratory tract infection Dispneu
Temperature: 390-400C Nasal lobe breathing
Restless Cyanosis around the nose and
mouth
Headache
Cough
Malaise Chest retraction (intercostal,
Decreased appetite subcostal, and suprasternal)
Gastrointestinal Disorders Tachypnea
Chest pain Tachycardia
Kepaniteraan Klinik Ilmu Kesehatan Anak
Rumah Sakitt Umum Daerah Karawang
Universitas Trisakti 2019
Diagnosis
ANAMNESIS PEMERIKSAAN FISIK PEMERIKSAAN PENUNJANG
• Continual high fever Temperature ≥ 39c Darah tepi:
• Shivering (in children) Dispnue Thrombocytopenia,
• Cough Takipnu leukocytosis with count
Chest wall retraction
• Restless shifted to the left
Nasal lobe breathing
• Fussy Cyanosis
• Out of breath Movement of the thoracic Foto thorax: alveolar
• cyanosis around the wall decreases in the infiltrates that can be
mouth affected area found throughout the
• Seizures (in infants) Normal / poor percussion lung fields
• Chest pain Vf decreases
• Children prefer lying on Decreased breathing sound
Auscultation: weak breath
the affected side
sounds, soft wet crackles in
the affected lung
Kepaniteraan Klinik Ilmu Kesehatan Anak
Rumah Sakitt Umum Daerah Karawang
Universitas Trisakti 2019
Kriteria Diagnosis
The diagnosis is made if 3 of the following 5 symptoms are found:
1. Shortness of breath accompanied by nasal lobe breathing and chest
wall pull
2. Body heat
3. Wet Ronkhi is loud (crackles)
4. Chest radiographs diffuse Infiltrate images
5. Leukocytosis (in viral infections not exceeding 20,000 / mm3 with
predominant lymphocytes, and predominant 15,000-40,000 / mm3
bacterial neutrophils)
Kepaniteraan Klinik Ilmu Kesehatan Anak
Rumah Sakitt Umum Daerah Karawang
Universitas Trisakti 2019
Tatalaksana
The management of pneumonia patients includes supportive therapy
and etiologic therapy.
Supportive therapy given to people with pneumonia is:
Giving oxygen 2-4 L / min through a nasal catheter or nasopharynx. If
the disease is severe and means are available, breathing aids may be
needed especially within 24-48 hours
Providing adequate fluids and nutrients. The liquid given contains
enough sugar and electrolytes.
Correction of electrolyte or metabolic abnormalities that occur.
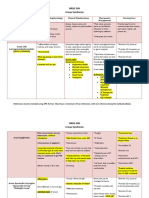
Terapi Antibiotik
Kategori Usia Patogen Rawat Jalan Rawat Inap
(7-10 hari) (10-14 hari)
Neonatus (<1 month) Streptococcus Grup B It should not be done as Ampicillin +
E.Coli an outpatient aminoglycoside added
Streptococcus with anti-staphylococcal
pneumonia preparations if S. aureus
Haemophiluz influenza infection is suspected
(type b)
< 2 month parainfluenza virus, It is not recommended sefotaksim ditambah
influenza virus, to do outpatient dng nafsilin atau
adaenovirus), S. treatment at the oksasilin
Pneumonia, Haemopilus beginning
influenza (type b)
2 month - 5 years (parainfluenza virus, Amoksisilin, eritromisin, beta laktam+amoksisillin
influenza virus, azitromisin/ amoksisillin-amoksisillin
adaenovirus), klaritomisin klavulanat
S.pneumonia, golongan sefalosporin
H.influenza (tipe b), kotrimoksazol
M.pneumonia, makrolid (eritromisin)
Clamydophilia
pneumonia, S. Aureus,
Streptococcus Grup A
Tatalaksana
*Alternative: Seftriakson chloramphenicol added
Drug of choice for (80-100 mg/kgbb IM atau (25 mg / kgbb / times IV
suspected germs IV sekali sehari
or IM every 8 hours)
when no one is suspected increasingly severe illness
• ` no improvement
initial antibiotics ampicillin /
amoxicillin (25-50 mg / kgbb / times monitor at least 24 hours
Iv or IM every 6 hours) according to until the 3rd day
age group (trial & error)
Prognosis
• In general, children with uncomplicated bronchopneumonia can
show a good therapeutic response from the start of appropriate and
adequate antibiotic therapy early on
• And also the prognosis is good if quickly treated or quickly given the
right antibiotics. But the prognosis will be bad if there is leukopenia
Kepaniteraan Klinik Ilmu Kesehatan Anak
Rumah Sakitt Umum Daerah Karawang
Universitas Trisakti 2019
1. Bennett NJ. Pediatric Pneumonia. Accessed on [2019 August 28]. Available at
http://emedicine.medscape.com/article/967822-overview#a5.
2. Kemenkes RI. Profil Kesehatan Indonesia 2015: Pneumonia. Jakarta: Pusdatin.2016; p.172-74
3. Zec LS, Selmanovic K, Andrijic NL, Kadic A, Zecevic L, Zunic L. Evaluation of Drug Treatment of
Bronchopneumonia at the Pediatric Clinic in Sarajevo. Med Arch. 2016 Jun;70(3):177-181.
4. Anwar A, Dharmayanti I. Pneumonia pada Anak Balita di Indonesia. Jakarta: Jurnal Kesehatan
Masyarakat Nasional.2014;8(8):359-65
5. Pudjiadi A, Hegar B, Handryastuti S, Idris NS, Gandaputra EP, Harmoniati ED. Pedoman Pelayanan Medis
Ikatan Dokter Anak Indonesia. Jakarta: Ikatan Dokter Anak Indonesia; 2009.p.250-4.
6. Pabary R, Balfour-Lynn IM. Complicated pneumonia in children. Breathe. March 2013;9(3):211-22.
7. Paks M. Bronchopneumonia. Accessed on [2019 August 28]. Available at
https://radiopaedia.org/articles/bronchopneumonia.
8. Kliegman RM, Stanton BF, St Geme JW, Schor NF, Behrman RE. Nelson Textbook of Pediatrics. 20th ed.
Philadelphia; 2016.p.2088-94.
9. Rahajoe NN, Supriyatno B, Setyanto DB. Buku Ajar Respirologi Anak. 1st ed. Jakarta: Ikatan Dokter Anak
Indonesia; 2013.p.350-64.
Kepaniteraan Klinik Ilmu Kesehatan Anak
Rumah Sakitt Umum Daerah Karawang
Universitas Trisakti 2019
THANK YOU!
Potrebbero piacerti anche
- Essential Treatment Guidelines for BronchopneumoniaDocumento67 pagineEssential Treatment Guidelines for BronchopneumoniaVerra AnindyaNessuna valutazione finora
- Bronkopneumonia Pada Pasien PediatrikDocumento5 pagineBronkopneumonia Pada Pasien PediatrikCecilia Evangelista NiluhNessuna valutazione finora
- CASE REPORT 4: PNEUMONIA DEXTRA SUSPECT COVID-19 + ACUTE GASTRITISDocumento17 pagineCASE REPORT 4: PNEUMONIA DEXTRA SUSPECT COVID-19 + ACUTE GASTRITISdianarahimmNessuna valutazione finora
- Bunga Rampai Infeksi Dengue AnakDocumento67 pagineBunga Rampai Infeksi Dengue AnakSatrio PrimaesoNessuna valutazione finora
- Pertanyaan Jurnal ReadingDocumento5 paginePertanyaan Jurnal ReadingMohammad AlmuhaiminNessuna valutazione finora
- Case Report on Pulmonary TuberculosisDocumento38 pagineCase Report on Pulmonary TuberculosisBunga Listia ParamitaNessuna valutazione finora
- Case Report BronkopneumoniaDocumento25 pagineCase Report BronkopneumoniaBintang TrianaNessuna valutazione finora
- Myelodisplastic SyndromeDocumento9 pagineMyelodisplastic SyndromeEni JiantiNessuna valutazione finora
- Print PneumoniaDocumento24 paginePrint Pneumoniavandhani79Nessuna valutazione finora
- Demam TifoidDocumento106 pagineDemam TifoidMasYurahNharaBarusNessuna valutazione finora
- Typhoid Fever Case ReportDocumento32 pagineTyphoid Fever Case ReportAlvin PratamaNessuna valutazione finora
- Continuing Professional Development: The Role of Exogenous Surfactants in Treating Premature Infant Respiratory Distress SyndromeDocumento4 pagineContinuing Professional Development: The Role of Exogenous Surfactants in Treating Premature Infant Respiratory Distress Syndromelaudya100% (1)
- Lapsus Bangsal 1Documento20 pagineLapsus Bangsal 1Ira M RNessuna valutazione finora
- Tuberculous Meningitis Case ReportDocumento34 pagineTuberculous Meningitis Case ReportDippos Theofilus HNessuna valutazione finora
- Case Report Melita Aditya Sari 12-058Documento51 pagineCase Report Melita Aditya Sari 12-058Firda Diah UtamiNessuna valutazione finora
- Case Report Kejang DemamDocumento48 pagineCase Report Kejang DemamRahmatNessuna valutazione finora
- Case Report - Cutaneous Larva MigransDocumento15 pagineCase Report - Cutaneous Larva MigransDira Adhitya100% (1)
- Hypertension Treatment and GoalsDocumento41 pagineHypertension Treatment and GoalsSemestaNessuna valutazione finora
- Congenital GlaucomaDocumento27 pagineCongenital Glaucomaanon_373532435Nessuna valutazione finora
- Borang LohhDocumento22 pagineBorang LohhRezki RamadhanNessuna valutazione finora
- Otitis Media AkutDocumento31 pagineOtitis Media AkutNin DuskNessuna valutazione finora
- Abdominal Pain in Children - Dr. Hermanto SP - BaDocumento41 pagineAbdominal Pain in Children - Dr. Hermanto SP - Bajimmy_junNessuna valutazione finora
- MeningoencephalitisDocumento58 pagineMeningoencephalitisShillea Olimpia Melyta100% (1)
- Dr. Ago Harlim - MikosisDocumento50 pagineDr. Ago Harlim - MikosisBrian Pasa NababanNessuna valutazione finora
- Chronic Cephalgia and Hemiparese due to Brain TumorDocumento5 pagineChronic Cephalgia and Hemiparese due to Brain TumorrivienaNessuna valutazione finora
- Laporan Kasus CHFDocumento27 pagineLaporan Kasus CHFBerka Phillia NingrumNessuna valutazione finora
- Dermatological Infection Management UpdateDocumento29 pagineDermatological Infection Management UpdateyheyenNessuna valutazione finora
- Paederus Dermatitis Karthikeyan K, Kumar A - Indian J Dermatol Venereol LeprolDocumento11 paginePaederus Dermatitis Karthikeyan K, Kumar A - Indian J Dermatol Venereol Leprolalmas prawoto100% (1)
- Vitamin D Levels and Recurrent Tonsillitis in ChildrenDocumento14 pagineVitamin D Levels and Recurrent Tonsillitis in ChildrenMyarNessuna valutazione finora
- PPT Case NephrolithiasisDocumento45 paginePPT Case NephrolithiasisRifka Anisa0% (1)
- Trantornos Anorrectales Adquiridos PDFDocumento7 pagineTrantornos Anorrectales Adquiridos PDFIván Castellares RojasNessuna valutazione finora
- Kuliah TETANUSDocumento30 pagineKuliah TETANUSAraa AsukaNessuna valutazione finora
- Demam Tifoid: Etiologi, Gejala, Diagnosis dan PenatalaksanaanDocumento30 pagineDemam Tifoid: Etiologi, Gejala, Diagnosis dan PenatalaksanaanRaihan LuthfiNessuna valutazione finora
- Fix Case Report TifoidDocumento24 pagineFix Case Report Tifoidanggun nur auliaNessuna valutazione finora
- Pediatri Essensial 3Documento86 paginePediatri Essensial 3Gregorius WahyudiNessuna valutazione finora
- 10 - 258sepsis Neonatorum Awitan DiniDocumento4 pagine10 - 258sepsis Neonatorum Awitan DiniIrenaNessuna valutazione finora
- REFERAT - Meassles - FirdaDocumento19 pagineREFERAT - Meassles - FirdaEriza LuthfansyahNessuna valutazione finora
- Otitis MediaDocumento48 pagineOtitis MediaRaisah_Ridwan382Nessuna valutazione finora
- PertusisDocumento28 paginePertusiswenyinriantoNessuna valutazione finora
- Batu Saluran Kemih: Dr. Suhaemi, SPPD, FinasimDocumento57 pagineBatu Saluran Kemih: Dr. Suhaemi, SPPD, FinasimAfri AdiNessuna valutazione finora
- Sindrom Nefritik DebDocumento2 pagineSindrom Nefritik DebrchristevenNessuna valutazione finora
- Causes, Symptoms and Treatment of ChorioretinitisDocumento13 pagineCauses, Symptoms and Treatment of Chorioretinitisrada tri rosi kurniaNessuna valutazione finora
- Chorioretinitis: By. Bimo Nugroho SaktiDocumento14 pagineChorioretinitis: By. Bimo Nugroho SaktiSalman AlkomaNessuna valutazione finora
- Radiologi - Tambahan SsDocumento91 pagineRadiologi - Tambahan SsShifa TifarinNessuna valutazione finora
- Tutorial Kasus: AppendisitisDocumento50 pagineTutorial Kasus: Appendisitiseruza hiwatariNessuna valutazione finora
- Journal Reading THT - OMADocumento15 pagineJournal Reading THT - OMAIndira MaycellaNessuna valutazione finora
- NRSG 206 Croup SyndromeDocumento3 pagineNRSG 206 Croup SyndromeGirlwithnonameNessuna valutazione finora
- Pityriasis Rosea PatogenesisDocumento4 paginePityriasis Rosea PatogenesisAdrian KuswantoNessuna valutazione finora
- KERATITISDocumento12 pagineKERATITISfaridasylvia100% (1)
- Patient Medical RecordsDocumento50 paginePatient Medical Recordscamila anisNessuna valutazione finora
- Kista Ovarium 21906150Documento43 pagineKista Ovarium 21906150NUR ATHIFAHNessuna valutazione finora
- FIXED DRUG ERUPTION PrintDocumento17 pagineFIXED DRUG ERUPTION PrintnajwaNessuna valutazione finora
- Skull Cervical X-RayDocumento15 pagineSkull Cervical X-RayPuji Yunisyah RahayuNessuna valutazione finora
- PDF Borang Ukm Advokasi CompressDocumento8 paginePDF Borang Ukm Advokasi CompressJeffry HertantoNessuna valutazione finora
- Pneumonia in Children - Causes, Signs, SymptomsDocumento63 paginePneumonia in Children - Causes, Signs, SymptomsAbraham AnaelyNessuna valutazione finora
- Pneumonia Minggu GMEDocumento42 paginePneumonia Minggu GMEEkaNessuna valutazione finora
- Acquired PneumoniaeDocumento20 pagineAcquired PneumoniaeVivi DeviyanaNessuna valutazione finora
- Causes of Neonatal Pneumonia by Route - UpToDateDocumento2 pagineCauses of Neonatal Pneumonia by Route - UpToDateThảo Nguyên Phan NguyễnNessuna valutazione finora
- Bacteri Pathology&pathogenesisDocumento22 pagineBacteri Pathology&pathogenesisAsem AlhazmiNessuna valutazione finora
- Pneumonia Lobaris PneumoniaDocumento34 paginePneumonia Lobaris PneumoniamoditiaraNessuna valutazione finora
- HEAD INJURY (Trauma Kepala) DR - AgusDocumento53 pagineHEAD INJURY (Trauma Kepala) DR - AgusSetyo RahmanNessuna valutazione finora
- 11.2 Gas Exchange in Humans Igcse Cie Biology Ext Theory MsDocumento3 pagine11.2 Gas Exchange in Humans Igcse Cie Biology Ext Theory MsRyan NishadNessuna valutazione finora
- Anatomy ProstateDocumento2 pagineAnatomy ProstatenavjavNessuna valutazione finora
- How Pandemics Spread and WebquestDocumento3 pagineHow Pandemics Spread and Webquestapi-405140390Nessuna valutazione finora
- Chapter 4 Integumentary SystemDocumento75 pagineChapter 4 Integumentary SystemAngel JuNessuna valutazione finora
- Acid Base Balance and Arterial Blood Gas AnalysisDocumento29 pagineAcid Base Balance and Arterial Blood Gas AnalysisPaulus LukmanNessuna valutazione finora
- Pubic Health SurvilanceDocumento28 paginePubic Health Survilanceteklay100% (1)
- Sample Research Plan2Documento9 pagineSample Research Plan2api-283862617Nessuna valutazione finora
- Alteration in Endocrine SystemDocumento215 pagineAlteration in Endocrine Systemyen1988100% (1)
- A Stag God Is Born Ch6-7Documento12 pagineA Stag God Is Born Ch6-7Eka KimNessuna valutazione finora
- Question Paper Unit f214 Communication Homeostasis and EnergyDocumento16 pagineQuestion Paper Unit f214 Communication Homeostasis and EnergyRobert EdwardsNessuna valutazione finora
- Acadsoc BookDocumento6 pagineAcadsoc Bookmarizon datuNessuna valutazione finora
- Asphyxia by SuffocationDocumento15 pagineAsphyxia by SuffocationBryan Christopher Co Lao100% (1)
- Arun Kumar RayDocumento15 pagineArun Kumar RayAnil GautamNessuna valutazione finora
- 04 Bahas Inggris Paket 4Documento9 pagine04 Bahas Inggris Paket 4Aji PangestuNessuna valutazione finora
- CCGL 9061 PosterDocumento1 paginaCCGL 9061 Posterchunpan tsangNessuna valutazione finora
- Pathogens 11 00715 v2Documento25 paginePathogens 11 00715 v2Hizrah Harianto SembiringNessuna valutazione finora
- Blood LecturesDocumento128 pagineBlood LecturessrhrenaissanceNessuna valutazione finora
- Anti-FTO Antibody (EPR6894) Ab126605: 6 ImagesDocumento4 pagineAnti-FTO Antibody (EPR6894) Ab126605: 6 Imageshorace35Nessuna valutazione finora
- Thoracic Trauma TreatmentDocumento77 pagineThoracic Trauma TreatmentAnonymous GsvDOlQuSNessuna valutazione finora
- Gynaecological NursingDocumento79 pagineGynaecological NursingGuruKPO100% (3)
- Livestock Superviser Job Description JB SDDocumento2 pagineLivestock Superviser Job Description JB SDSkyNessuna valutazione finora
- Many Sides of RizalDocumento11 pagineMany Sides of Rizaljulieanntipon100% (1)
- Body Condition Score Dog PDFDocumento1 paginaBody Condition Score Dog PDFJairo Alfonso Angulo NegreteNessuna valutazione finora
- 9 Pengaruh Therapi Tertawa Terhadap Penurunan Tekanan Darah Pada Lansia Penderita Hipertensi Di PSTW Puspakarma Mataram Ni Made SumartyawatiDocumento2 pagine9 Pengaruh Therapi Tertawa Terhadap Penurunan Tekanan Darah Pada Lansia Penderita Hipertensi Di PSTW Puspakarma Mataram Ni Made Sumartyawatikadek aryaNessuna valutazione finora
- Marketing AttractionDocumento16 pagineMarketing AttractionIka DinNessuna valutazione finora
- Of TheDocumento81 pagineOf Theayushy gupta100% (1)
- NatokinaseDocumento6 pagineNatokinasefabadioNessuna valutazione finora
- MD Curs Neuro 4Documento45 pagineMD Curs Neuro 4Andreea AlexaNessuna valutazione finora
- Benign Ovarian ConditionsDocumento31 pagineBenign Ovarian ConditionsNur Hanani KhanNessuna valutazione finora