Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Urothelial Tumors of The Upper Urinary Tract Fix
Caricato da
Agung Indra0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
18 visualizzazioni25 pagineutuc
Titolo originale
Urothelial Tumors of the Upper Urinary Tract Fix
Copyright
© © All Rights Reserved
Formati disponibili
PPTX, PDF, TXT o leggi online da Scribd
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoutuc
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato PPTX, PDF, TXT o leggi online su Scribd
0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
18 visualizzazioni25 pagineUrothelial Tumors of The Upper Urinary Tract Fix
Caricato da
Agung Indrautuc
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato PPTX, PDF, TXT o leggi online su Scribd
Sei sulla pagina 1di 25
Urothelial Tumors of the Upper
Urinary Tract and Ureter
CAMPBELL 11 TH EDITION
Agung Adhitya
Management of Positive Upper Tract Urinary Cytology
or Carcinoma in Situ
• urinary cytology (+) presence of urothelial
carcinoma. Most cases are from a bladder
• extravesical sites may be involved, upper
urinary tracts and the prostatic urethra in men
• Diagnosis is difficult limitations of radiographic
evaluation of upper tracts and the complexity
of upper tract endoscopy compared with the
bladder.
Management of Positive Upper Tract
Urinary Cytology or Carcinoma in Situ
Management of Positive Upper Tract
Urinary Cytology or Carcinoma in Situ
• repeat the cytology
• upper tracts CT urography
• bladder evaluation biopsies and tumor
resection if tumor is present
• Bladder (+) intravesical therapy and/or tumor
resection voided urinary cytologies
• Cytology (+) selective cytologies each upper
urinary tract URS non contamination specimen
from bladder or urethra + prostatic urethra
specimen in men resection of a representative
specimen of the prostatic urethra
Carcinoma in Situ of the Upper Urinary Tracts
• diagnosis of CIS difficult inability to
evaluate the urothelium of the upper tracts
with adequate tissue samples
• most cases persistent positive selective
cytology absence of any ureteroscopic or
radiographic findings.
• Radical nephroureterectomy unilateral
cytologic abnormality of upper tract to
eliminate presumed CIS. not recommended
Carcinoma in Situ of the
Upper Urinary Tracts
Carcinoma in Situ of the
Upper Urinary Tracts
• Upper tract cytology same limitations in
specificity as does bladder cytology
• upper tract samples are of limited volume and
cell count compared with bladder
• Inflammation UTI or calculus false-
positive result
Carcinoma in Situ of the Upper Urinary
Tracts
• topical therapy nephrostomy tube reliable
delivery system initially with surgical
intervention absence of any histologic,
radiographic, or endoscopic finding cytology
false-positive results and the high risk for bilateral
disease in the future
• segmental resection not effective because
multifocality of the disease.
• Nephroureterectomy indicated
radiographically or endoscopically more than
just surface disease
Carcinoma in Situ of the
Upper Urinary Tracts
Carcinoma in Situ of the Upper Urinary
Tracts
• Re evaluation urinalysis
– Selective cytology
– cystoscopy every 3 months
– retrograde pyelography or ureteropyeloscopy every 6
months
– 1 to 2 years
• CIS of ureteral margins during radical cystectomy
serial endoscopy and found that recurrences
were found at the site of the margin but also at
other sites
Adjuvant Therapy.
After Organ-Sparing Therapy
• Extirpative surgery has a higher local recurrence to
minimize these risks instillation of immunotherapeutic
or chemotherapeutic and brachytherapy of nephrostomy
tract
• Instillation therapy
– primary treatment for CIS and as adjuvant therapy after
endoscopic or organ sparing therapy
– antegrade through a nephrostomy tube and retrograde directly
into a ureteral catheter or with iatrogenically created
vesicoureteral reflux
– instillation ureteral catheter placed suprapubically, but given
over tumor implantation rarely used.
– low pressure and absence active infection to minimize sepsis
Adjuvant Therapy.
After Organ-Sparing Therapy
• mytomicin and BCG same agents used to treat
urothelial carcinoma of the bladder same with to
treat tumors of the upper urinary tract
• Gemcitabine alternative to BCG with fewer
side effects
– insufficient clinical significance rarity of the disease
– UTUC have a tumor biology different with bladder
tumor
– inadequate delivery system upper tract have an
adequate dwell time to enable a clinical response.
Adjuvant Therapy.
After Organ-Sparing Therapy
• BCG via a nephrostomy for CIS 55 patients
57% 5-year recurrence-free survival
• adjuvant after endoscopic ablation had
inferior results
• mitomycin C smaller numbers of patients
and variable no definite conclusions
reached
• intrarenal perfusion of BCG 50% (5 of 10)
recurrence 50.9 months
Adjuvant Therapy.
After Organ-Sparing Therapy
• Agent-specific complications ramifications
of systemic absorption of the agent
• Brachytherapy to nephrostomy tract through
iridium wire by Patel and coworkers (1996)
– No instances of tract recurrences in this series
– major complication cutaneous fistula formation
requiring nephroureterectomy.
Adjuvant Therapy.
After Organ-Sparing Therapy
After Complete Excision
• stage T3, T4, & N+ radiation therapy after radical
surgery decrease risk of local relapse
• 41 patients decreased local recurrence but no effect
on distant relapse or survival
• 26 patients 46 Gy
• Tumor stage was T2, T3, and N+ in 42%, 58%, and 35% of cases
• 5-year survival was 49%,with 30% remaining disease free
• 252 patients
• T3 : overall 5-year survival rates with or without adjuvant 41%
and 28%
• T4 : survival 6 months with or without adjuvant 45% and 40%
• relapse occurred in 9%
After Complete Excision
• adjuvant radiation isolated local relapse
without distant metastases 10% (T3) and 4%
(T4)
• radical nephroureterectomy high rate of
local control.
• combined radiation chemotherapy
advanced disease evidence supporting this
is small and retrospective
After Complete Excision
• Chemotherapy many patients have baseline
chronic kidney disease worsens after
nephroureterectomy ineligible to receive full
dose cisplatinum
• 15 patients T2-T4
– MVAC (methotrexate, vinblastine, Adriamycin, and cisplatin)
– MEC (methotrexate, etoposide, and cisplatin)
– MVEC (methotrexate, vinblastine, epirubicin, and cisplatin)
– before nephroureterectomy 13% complete
responses and 40% partial responses
After Complete Excision
• 27 patients T3 16 patient received platinum
based therapy after nephroureterectomy
no significant difference in recurrence free
and disease specific survival 40 months
• lack of controlled trials that establish the
efficacy neoadjuvant or adjuvant
chemotherapy in UTUC
Treatment of Metastatic Disease
• chemotherapy in metastatic UTUC decline in
renal function after nephroureterectomy
compromise ability to administer effective
postoperative chemotherapy
• lymph node (+) initial chemotherapy surgery
withheld until a complete radiographic response
• MVAC highest response toxicity prohibits
optimal dosage and duration complete
responses rare in the metastatic overall
survival of 12 to 24 months
Treatment of Metastatic Disease
• Carboplatin is frequently substituted for cisplatin
limitations of renal function or concerns over
toxicity results remain inferior
• randomized phase III study
• paclitaxel, cisplatin, and gemcitabine (PCG) VS.
gemcitabine and cisplatin (GC)
• metastatic and locally advanced urothelial cancer
• follow-up of 4.6 years
• overall survival 15.8 months vs. 12.7 months
• overall response rate 55.5% vs. 43.6%
• The inhibitor of MET and VEGF pathways, in
patients in whom previous chemotherapy has
failed.
• phase I trials in metastatic urothelial
carcinoma Targeting inhibitory surface
receptor PD-1, activation of which by PD-L1
ligand confers inhibition of T-cell proliferation
and cytokine production
• ongoing phase II and III trials
Treatment of Metastatic Disease
EAU, 2016
summary
• UTUC like bladder cancer, is chemosensitive
chemotherapy are toxic and lack sustained
response.
• population chronic kidney disease
worsens after nephroureterectomy
• novel targeted therapies and experimentation
with new chemotherapeutic optimize
treatment of metastatic UTUC
Potrebbero piacerti anche
- Bladder CancerDa EverandBladder CancerJa Hyeon KuNessuna valutazione finora
- Radiotherapy of Liver CancerDa EverandRadiotherapy of Liver CancerJinsil SeongNessuna valutazione finora
- Urology Sample Osce Exam e PDFDocumento8 pagineUrology Sample Osce Exam e PDFLana LocoNessuna valutazione finora
- Non Metastatic Bladder CancerDocumento57 pagineNon Metastatic Bladder CancerAsim ArshadNessuna valutazione finora
- Testicular Tumors Part4Documento52 pagineTesticular Tumors Part4Ramesh ReddyNessuna valutazione finora
- UTUCDocumento39 pagineUTUCShalini shreeNessuna valutazione finora
- BladderDocumento36 pagineBladderdrsumitavaNessuna valutazione finora
- Locally Advanced Breast CarcinomaDocumento31 pagineLocally Advanced Breast Carcinomaapi-3701915100% (1)
- The Emergence of Liver Transplantation For Hilar CholangiocarcinomaDocumento109 pagineThe Emergence of Liver Transplantation For Hilar CholangiocarcinomatasarimkutusuNessuna valutazione finora
- Radical Cystectomy: History of The ProcedureDocumento6 pagineRadical Cystectomy: History of The ProcedureIvy MinaNessuna valutazione finora
- RT Urothelial Carcinomas Radu MitricaDocumento37 pagineRT Urothelial Carcinomas Radu MitricaStirNessuna valutazione finora
- Gall Bladder CarcinomaDocumento29 pagineGall Bladder CarcinomaUsman FarooqNessuna valutazione finora
- Urinary Tract Ca, Neurogenic Bladder-Rasha Khashan and Rima Saker-19156Documento49 pagineUrinary Tract Ca, Neurogenic Bladder-Rasha Khashan and Rima Saker-19156huso20Nessuna valutazione finora
- Testicular Tumors The EndDocumento67 pagineTesticular Tumors The EndRamesh ReddyNessuna valutazione finora
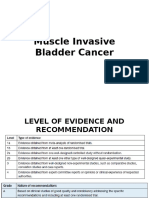
- Muscle Invasive Bladder CancerDocumento39 pagineMuscle Invasive Bladder CancerBernardNessuna valutazione finora
- Case Based Teaching - Urology: Haematuria & Renal TransplantDocumento21 pagineCase Based Teaching - Urology: Haematuria & Renal Transplantamoody95Nessuna valutazione finora
- Pancreaticcancer 150917114601 Lva1 App6891Documento25 paginePancreaticcancer 150917114601 Lva1 App6891enam professorNessuna valutazione finora
- Pancreaticcancer 150917114601 Lva1 App6891Documento30 paginePancreaticcancer 150917114601 Lva1 App6891enam professorNessuna valutazione finora
- Microhematuria Case Study: Medical Student Case-Based LearningDocumento30 pagineMicrohematuria Case Study: Medical Student Case-Based LearningjenegneNessuna valutazione finora
- Carcinomagallbladder PDFDocumento61 pagineCarcinomagallbladder PDFZaki DhiifNessuna valutazione finora
- Bladder CancerDocumento43 pagineBladder CancerIsaac MwangiNessuna valutazione finora
- OncologyDocumento7 pagineOncologyKit NameKoNessuna valutazione finora
- Urinary Bladder Neoplasm: DR Rikesh Jung Karkee Assitant Professor Urology Division Surgery DepartmentDocumento60 pagineUrinary Bladder Neoplasm: DR Rikesh Jung Karkee Assitant Professor Urology Division Surgery DepartmentAashish YadavNessuna valutazione finora
- Breast MassesDocumento25 pagineBreast MassesRima HajjarNessuna valutazione finora
- Esophageal CarcinomaDocumento34 pagineEsophageal Carcinomaapi-19916399100% (1)
- Testicular TumorsDocumento35 pagineTesticular TumorsHafizur RashidNessuna valutazione finora
- Role of Radiotherapy For Hepatocellular CarcinomaDocumento37 pagineRole of Radiotherapy For Hepatocellular CarcinomabahtiarhabibiNessuna valutazione finora
- Practice Essentials: Essential Update: Pancreatoduodenectomy May Be Done Without Biopsy Proof in Select CasesDocumento3 paginePractice Essentials: Essential Update: Pancreatoduodenectomy May Be Done Without Biopsy Proof in Select CasesSheila AnisaNessuna valutazione finora
- Carcinoma of UnknownDocumento31 pagineCarcinoma of Unknownsamer falconNessuna valutazione finora
- Case Presentation: by DR SaleemDocumento61 pagineCase Presentation: by DR SaleemsandeepNessuna valutazione finora
- Preliminary Information About Intraperitoneal Hypertermic Chemoterapy (Iphc) in Abdominal CancerDocumento29 paginePreliminary Information About Intraperitoneal Hypertermic Chemoterapy (Iphc) in Abdominal CancerViorica StoianNessuna valutazione finora
- Palliative CystectomyDocumento20 paginePalliative CystectomymostafaNessuna valutazione finora
- Eva Bolton Haematuria Presentation WebDocumento52 pagineEva Bolton Haematuria Presentation WebereczkieNessuna valutazione finora
- HIPECDocumento34 pagineHIPECBimlesh thakurNessuna valutazione finora
- Seminar Obgyn Chemotheraphy in GynaecologyDocumento38 pagineSeminar Obgyn Chemotheraphy in GynaecologyRoshandiep GillNessuna valutazione finora
- Management of Lung Cancer by DR Abdul-AzizDocumento89 pagineManagement of Lung Cancer by DR Abdul-AzizAbdulaziz HassenNessuna valutazione finora
- Epithelial Ovarian TumorDocumento62 pagineEpithelial Ovarian TumorChristopher EnikeNessuna valutazione finora
- 17-09-2019 Lower GI FINALDocumento32 pagine17-09-2019 Lower GI FINALNaima HabibNessuna valutazione finora
- Carcinoma Penis Management: Dr. Lilamani Rajthala MS Resident Moderator: Dr. Samir ShresthaDocumento63 pagineCarcinoma Penis Management: Dr. Lilamani Rajthala MS Resident Moderator: Dr. Samir ShresthaBibek GhimireNessuna valutazione finora
- Malignant Tumors of Uterus: DR Tahira RizwanDocumento52 pagineMalignant Tumors of Uterus: DR Tahira RizwanSadia YousafNessuna valutazione finora
- Uterine Cancer: Pedro T. Ramirez, M.DDocumento46 pagineUterine Cancer: Pedro T. Ramirez, M.DIsabel Barredo Del MundoNessuna valutazione finora
- Soal 20112020Documento21 pagineSoal 20112020Derri HafaNessuna valutazione finora
- Biliary Tumors: Cholangiocarcinoma and Cancer of The Gall BladderDocumento34 pagineBiliary Tumors: Cholangiocarcinoma and Cancer of The Gall BladderSahirNessuna valutazione finora
- Brachytherapy in The Treatment of Cervical CancerDocumento10 pagineBrachytherapy in The Treatment of Cervical CancervchendilNessuna valutazione finora
- Debulking (Cytoreductive) SurgeryDocumento23 pagineDebulking (Cytoreductive) Surgerytsega tilahunNessuna valutazione finora
- Wilms' Tumor 2014Documento18 pagineWilms' Tumor 2014api-282060573Nessuna valutazione finora
- ARTSCANIIIDocumento61 pagineARTSCANIIIKishoreChandraKoradaNessuna valutazione finora
- Cancer Cervix: BY Ahmed Magdy ElmohandesDocumento34 pagineCancer Cervix: BY Ahmed Magdy ElmohandesAhmed ElmohandesNessuna valutazione finora
- Rectal CancerDocumento6 pagineRectal CancerIqra FatemahNessuna valutazione finora
- Bladder CancerDocumento19 pagineBladder Cancervishnu100% (1)
- Faculty of Medicine NR - Ii Department of Surgery NR - Ii: Diseases of The Biliary TractDocumento40 pagineFaculty of Medicine NR - Ii Department of Surgery NR - Ii: Diseases of The Biliary TractGalina LozovanuNessuna valutazione finora
- Urinary Tract Infection: UpdateDocumento42 pagineUrinary Tract Infection: UpdateakNessuna valutazione finora
- MalarDocumento41 pagineMalarமணிகண்டன் ராஜேந்திரன்Nessuna valutazione finora
- 20.MBBS Pancreatic CancerDocumento52 pagine20.MBBS Pancreatic Cancermrajah95Nessuna valutazione finora
- C122 Early Post TURB Instillational Treatment in Ta, T1 Bladder CancersDocumento1 paginaC122 Early Post TURB Instillational Treatment in Ta, T1 Bladder CancersOkki Masitah Syahfitri NasutionNessuna valutazione finora
- Pointer Trial Long Term FinalDocumento43 paginePointer Trial Long Term FinalHarsha VardhanNessuna valutazione finora
- Nodul Tiroidian Engleza PPT 2016Documento36 pagineNodul Tiroidian Engleza PPT 2016Stefi GrNessuna valutazione finora
- EAU Pocket On Muscle Invasive and Metastatic Bladder Cancer 2022Documento17 pagineEAU Pocket On Muscle Invasive and Metastatic Bladder Cancer 2022Caio Vinicius SuartzNessuna valutazione finora
- Colo Rectal CarcinomaDocumento10 pagineColo Rectal CarcinomaA.R. MendozaNessuna valutazione finora
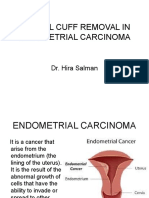
- Vaginal Cuff Removal in Endometrial Carcinoma: Dr. Hira SalmanDocumento38 pagineVaginal Cuff Removal in Endometrial Carcinoma: Dr. Hira SalmandrhirasalmanNessuna valutazione finora
- Suture Material: Mangkubumi Putra WijayaDocumento37 pagineSuture Material: Mangkubumi Putra WijayaAgung IndraNessuna valutazione finora
- MeatotomyDocumento11 pagineMeatotomyAgung Indra100% (1)
- PR NHL Dan HerniaDocumento23 paginePR NHL Dan HerniaAgung IndraNessuna valutazione finora
- Presentation 1Documento14 paginePresentation 1Agung IndraNessuna valutazione finora
- Meatotomy and Wound CareDocumento13 pagineMeatotomy and Wound CareAgung IndraNessuna valutazione finora
- PR Kateterisasi Pada TbiDocumento8 paginePR Kateterisasi Pada TbiAgung IndraNessuna valutazione finora
- SirkumDocumento22 pagineSirkumAgung IndraNessuna valutazione finora
- Wound CareDocumento13 pagineWound CareAgung IndraNessuna valutazione finora
- Orchidoscopy Journal Fix 2Documento24 pagineOrchidoscopy Journal Fix 2Agung IndraNessuna valutazione finora
- PR Kateterisasi Pada TbiDocumento8 paginePR Kateterisasi Pada TbiAgung IndraNessuna valutazione finora
- The Use of Medical Expulsive Therapy During Pregnancy: A Worldwide Perspective Among ExpertsDocumento18 pagineThe Use of Medical Expulsive Therapy During Pregnancy: A Worldwide Perspective Among ExpertsAgung IndraNessuna valutazione finora
- Inggris Chambel 2Documento33 pagineInggris Chambel 2Agung IndraNessuna valutazione finora
- Pap Smear Technique: VideoDocumento15 paginePap Smear Technique: VideoYuskamita KarsaeniNessuna valutazione finora
- Guildeline CA Penis KemoterapiDocumento18 pagineGuildeline CA Penis KemoterapiAgung IndraNessuna valutazione finora
- Case PresentationDocumento13 pagineCase PresentationAgung IndraNessuna valutazione finora
- Orchidoscopy Journal FixDocumento23 pagineOrchidoscopy Journal FixAgung IndraNessuna valutazione finora
- A Worldwide Perspective Among ExpertsDocumento17 pagineA Worldwide Perspective Among ExpertsAgung IndraNessuna valutazione finora
- AirwayTrauma FullRepDocumento62 pagineAirwayTrauma FullRepMuhammad Agung WNessuna valutazione finora
- Guildeline CA Penis KemoterapiDocumento18 pagineGuildeline CA Penis KemoterapiAgung IndraNessuna valutazione finora
- Jornal Reading Understanding The Ureter FixDocumento25 pagineJornal Reading Understanding The Ureter FixAgung IndraNessuna valutazione finora
- Cardiogenic ShockDocumento40 pagineCardiogenic ShockAgung IndraNessuna valutazione finora
- PujoDocumento4 paginePujoAgung IndraNessuna valutazione finora
- Abd Trauma - Cindy KinDocumento27 pagineAbd Trauma - Cindy KinAgung IndraNessuna valutazione finora
- Expert Lecture (Bleeding Disorders)Documento24 pagineExpert Lecture (Bleeding Disorders)Agung IndraNessuna valutazione finora
- Deep Vein Thrombosis: Faculty of Medicine University of BrawijayaDocumento59 pagineDeep Vein Thrombosis: Faculty of Medicine University of BrawijayaAgung IndraNessuna valutazione finora
- Deep Vein Thrombosis: Faculty of Medicine University of BrawijayaDocumento59 pagineDeep Vein Thrombosis: Faculty of Medicine University of BrawijayaAgung IndraNessuna valutazione finora
- Hasil Lab (18/6) Rentang Normal Rentang Normal Hematologi UrinalisisDocumento1 paginaHasil Lab (18/6) Rentang Normal Rentang Normal Hematologi UrinalisisAgung IndraNessuna valutazione finora
- Proses Diagnostik - KuliahDocumento52 pagineProses Diagnostik - KuliahAgung Indra100% (1)
- Cardiovascular System: by M. Rasjad IndraDocumento14 pagineCardiovascular System: by M. Rasjad IndraAgung IndraNessuna valutazione finora
- Surgical Epicrisis - TRANSDocumento1 paginaSurgical Epicrisis - TRANSlianaNessuna valutazione finora
- Breech & MalpositionDocumento41 pagineBreech & MalpositionAnuradha RoopchandNessuna valutazione finora
- New Born CareDocumento22 pagineNew Born Caredexter100% (8)
- Antenatal Assessment FormatDocumento9 pagineAntenatal Assessment FormatPalaniswami Palaniswami67% (3)
- Orlando S Arnold Palmer Hospital Founded in 1989 Specializes IDocumento1 paginaOrlando S Arnold Palmer Hospital Founded in 1989 Specializes IAmit PandeyNessuna valutazione finora
- Virchow's TriadDocumento3 pagineVirchow's TriadQuốc Vinh TrầnNessuna valutazione finora
- List of BIS Standards As On 07.9.2021Documento55 pagineList of BIS Standards As On 07.9.2021Subramani KarurNessuna valutazione finora
- PartographDocumento1 paginaPartographVraj SoniNessuna valutazione finora
- Open Access Textbook of General SurgeryDocumento7 pagineOpen Access Textbook of General SurgeryusamaNessuna valutazione finora
- NLRB Decision Regarding Cayuga Medical CenterDocumento58 pagineNLRB Decision Regarding Cayuga Medical CenterKelsey O'ConnorNessuna valutazione finora
- Multidisciplinary Approach To ProstatitisDocumento22 pagineMultidisciplinary Approach To ProstatitisGabrielAbarcaNessuna valutazione finora
- Paediatric Percutaneous Nephrolithotomy (P-PCNL) Reporting ChecklistDocumento6 paginePaediatric Percutaneous Nephrolithotomy (P-PCNL) Reporting ChecklistJad DegheiliNessuna valutazione finora
- BEmONC - Participant Workbook - v02Documento34 pagineBEmONC - Participant Workbook - v02lolemo kelbisoNessuna valutazione finora
- Hospital ListDocumento232 pagineHospital Listphone2hireNessuna valutazione finora
- Neg & ConsentDocumento6 pagineNeg & ConsentAnonymous NGLyy3hnNessuna valutazione finora
- Referat GaitDocumento32 pagineReferat GaitAsry WahidNessuna valutazione finora
- Postoperative Pain Control: Veerabhadram Garimella, MD, MRCS Christina Cellini, MDDocumento6 paginePostoperative Pain Control: Veerabhadram Garimella, MD, MRCS Christina Cellini, MDBani ZakiyahNessuna valutazione finora
- 4th LMDS List For Drug ShopDocumento59 pagine4th LMDS List For Drug ShopBirhaneNessuna valutazione finora
- Gynecology and ObstetricsDocumento147 pagineGynecology and ObstetricsMohammadAbuelhaija100% (4)
- Or and DR Instruments PDFDocumento59 pagineOr and DR Instruments PDFMayolianne Dumay100% (1)
- Developing SMART Objectives Case StudyDocumento3 pagineDeveloping SMART Objectives Case StudyVarun AchrejaNessuna valutazione finora
- Bihar HospitalDocumento4 pagineBihar Hospitalmahwish khanNessuna valutazione finora
- Maternal ResearchDocumento1 paginaMaternal ResearchAngela NeriNessuna valutazione finora
- HPLC Studies in HemoglobinopathiesDocumento6 pagineHPLC Studies in HemoglobinopathiesDevi SusantiNessuna valutazione finora
- © The Mechanism of Action of Anectine Involves What Appears To Be A "Persistent"Documento6 pagine© The Mechanism of Action of Anectine Involves What Appears To Be A "Persistent"kaye marie100% (1)
- IV Insulin Infusion ProtocolDocumento4 pagineIV Insulin Infusion ProtocolWeeranan Sueb-LaNessuna valutazione finora
- Step 2 NotesDocumento202 pagineStep 2 NotesNaved Rahman100% (2)
- A Speech About AbortionDocumento1 paginaA Speech About AbortionYusei FudoNessuna valutazione finora
- Healthcare Product Comparison System Titles ReportDocumento1 paginaHealthcare Product Comparison System Titles ReportHector AudelloNessuna valutazione finora
- Regurgitation, Rumination and The Rumination Syndromes: David R. Fleisher, MDDocumento5 pagineRegurgitation, Rumination and The Rumination Syndromes: David R. Fleisher, MDryselNessuna valutazione finora