Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Lower Gi Bleed NG
Caricato da
bocah_britpopTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Lower Gi Bleed NG
Caricato da
bocah_britpopCopyright:
Formati disponibili
LOWER GI BLEEDNG
CLINICAL PRESENTATION
A 68 yrs old presents to the ER with BRBPR. He has several
episodes, beginning on the evening before presentation.
He describes the bleeding as profuse and filling the toilet, he felt
light headed and almost passed out while sitting on the toilet.
PMHx: htn
Meds: amlodipine
P.Ex: B.P. =86/42mm hg, pulse = 134/min,
pt. is orthostatic.
Abdominal examination reveals slight abdominal distention
with hyperactive bowel sounds.
Rectal exam shows gross blood
Wbc-10
Hct-28 %
Plt-180
Lytes wnl
Coagulation profile wnl
LFTs wnl
Estimation of blood loss
Estimated Fluid and Blood Losses in Shock
Class 1 Class 2 Class 3 Class 4
Blood Loss,
mL
Up to 750 750-1500 1500-2000 >2000
Blood Loss,%
blood volume
Up to 15% 15-30% 30-40% >40%
Pulse Rate,
bpm
<100 >100 >120 >140
Blood
Pressure
Normal Normal Decreased Decreased
Respiratory
Rate
Normal or
Increased
Decreased Decreased Decreased
Urine
Output,
mL/h
14-20 20-30 30-40 >35
CNS/Mental
Status
Slightly
anxious
Mildly
anxious
Anxious,
confused
Confused,
lethargic
Fluid
Replacement,
3-for-1 rule
Crystalloid Crystalloid
Crystalloid
and blood
Crystalloid
and blood
Initial steps in the management of upper gastrointestinal bleeding
Airway protection
Airway monitoring
Endotracheal intubation (if indicated)
Hemodynamic stabilization
Large bore intravenous access
Intravenous fluids
Red cell transfusion (for symptomatic anemia)
Fresh-frozen plasma, platelets (if indicated)
Consider erythropoeitin
Nasogastric oral administration
Large bore orogastric tube/lavage
Clinical and laboratory monitoring
Serial vital signs
Serial hemograms, coagulation profiles, and chemistries (as clinically indicated)
Electrocardiographic monitoring
Hemodynamic monitoring (if indicated in high-risk patients)
Endoscopic examination and therapy
RESUSCITATION
High-risk patients (eg, those who are elderly or who have severe co
morbid illnesses such as coronary disease or cirrhosis) should
receive packed red blood cell transfusions to maintain the
hematocrit above 30 percent.
Patients who are elderly or have known cardiovascular disease are
at increased risk for a myocardial infarction and should thus be
monitored appropriately; consideration should be given to ruling
out a myocardial infarction.
Young and otherwise healthy patients should be transfused to
maintain their hematocrit above 20 percent.
Patients with active bleeding and a coagulopathy (prolonged
prothrombin time with INR >1.5) or low platelet count
(<50,000/microL) should also be transfused with fresh frozen
plasma and platelets, respectively.
Lower GI bleeding
Next step
Risk stratification
Initial Emergency Department Risk Stratification for Patients with Gastrointestinal
Bleeding
Low Risk Moderate Risk High Risk
Age <60 Age >60
Initial SBP 100 mm
Hg
Initial SBP <100 mm
Hg
Persistent SBP <100 mm Hg
Normal vitals for 1 hr Mild ongoing
tachycardia for 1 hr
Persistent moderate/severe
tachycardia
No transfusion
requirement
Transfusions required
4 U
Transfusion required >4 U
No active major
comorbid diseases
Stable major comorbid
diseases
Unstable major comorbid diseases
No liver disease Mild liver diseasePT
normal or near-normal
Decompensated liver diseasei.e.,
coagulopathy, ascites,
encephalopathy
No moderate-risk or
high-risk clinical
features
No high-risk clinical
features
Risk stratification
Strate and colleagues retrospectively collected data on 24
clinical variables available in the first 4 hours of
evaluation in 252 consecutive patients.
Seven independent predictors of severity in acute
LGIB
hypotension
tachycardia,
syncope,
nontender abdominal exam,
bleeding within 4 hours of presentation,
aspirin use, and
more than two comorbid diseases
Risk stratification
Based on these factors, patients could be
stratified into three risk groups:
Patients with more than three risk factors
had an 84% risk of severe bleeding,
One to three risk factors a 43% risk, and
No risk factors a 9% risk.
In another study clinical predictors in the
first hour of evaluation in patients with
severe LGIB included
initial hematocrit of no more than 35%,
presence of abnormal vital signs 1 hour
after initial medical evaluation, and
gross blood on initial rectal examination.
Next step
localization
An upper gastrointestinal source of bleeding is detected in 10% to
15% of patients presenting with severe hematochezia .
Patients with hemodynamic compromise and hematochezia should
have a nasogastric tube placed.
I f bile is present, an upper source is unlikely.
I f the aspirate is nondiagnostic (no blood or bile), or if there is
a strong suspicion of an upper bleeding source (i.e., history of
previous peptic ulcer disease or frequent NSAID use), then an
upper endoscopy should be performed before examining the colon
.
An upper endoscopy should be performed if no source of bleeding is
identified during colonoscopy.
LOCALIZATION
The duration, frequency, and color of blood passed per rectum
may help discern the severity and location of bleeding.
Characteristically, melena or black, tarry stool, indicates bleeding
from an upper gastrointestinal or small bowel source,
Maroon color suggests rt. Sided lesion
whereas bright red blood per rectum signifies bleeding from the
left colon or rectum. However, patient and physician reports of
stool color are often inaccurate and inconsistent
In addition, even with objectively defined bright red bleeding,
significant proximal lesions can be found on colonoscopy
LOCALIZATION
past medical history may also help to elucidate a specific bleeding source.
antecedent constipation or diarrhea (hemorrhoids, colitis),
the presence of diverticulosis (diverticular bleeding),
receipt of radiation therapy (radiation enteritis),
recent polypectomy (postpolypectomy bleeding), and
vascular disease/hypotension (ischemic colitis).
A family history of colon cancer increases the likelihood of a colorectal
neoplasm and generally calls for a complete colonic examination in
patients with hematochezia.
Nonetheless, even after a detailed history, physicians cannot reliably
predict which patients with hematochezia will have significant pathology
and a history of bleeding from one source does not eliminate the
possibility of bleeding from a different source.
LOCALIZATION
Multiple factors make the identification of a precise
bleeding source in LGIB challenging.
The diversity of potential sources,
The length of bowel involved,
The need for colon cleansing, and
The intermittent nature of bleeding.
In up to 40% of patients with LGIB, more than one
potential bleeding source will be noted and
Stigmata of recent bleeding in LGIB are infrequently
identified
As a result, no definitive source will be found in a large
percentage of patients
Clinical scenarios
Pt. continued to bleed with hypotension
and tachycardia. Patient requires 2 units
of PRBCs
Pt. stopped bleeding. Vitals normalizes
Options to diagnose and control
the bleeding
RBC scan, requires 0.5-1 ml/min bleeding
Mesenteric angiography, requires 1-1.5
ml/min bleeding
Colonoscopy
Surgery
Meckels scan
Scenario one-
Pt. continues to bleed
and is unstable.
Rbc scan vs colonoscopy
COLONOSCOPY
Colonoscopy is undoubtedly the best test for confirming the source
of LGIB and for excluding ominous diagnoses, such as
malignancy.
The diagnostic yield of colonoscopy ranges from 45% to 95%
Perform after golytely prep(w/in 12-24h)
Identifies lesion in 75 % or more
Can provide endoscopic therapy
Early colonoscopy associated with reduced stay
Complications 0.5-1 %
most patients undergoing radiographic evaluation for LGIB
regardless of findings and interventions will subsequently require
a colonoscopy to establish the cause of bleeding.
URGENT COLONOSCOPY
Jensen et al
Reduced rate of rebleeding and emergency surgery
from diverticular bleed when compared to historical
controls
Green et al
100 randomized to urgent (w/in 8hrs) colonoscopy
to standard care
Definitive source more common in urgent group
No difference in multiple clinical outcomes
Issue is still not resolved
CLINICAL SCENARIO
Patient continues to bleed
RBC scan is positive on the left side?
How much true this information is??
What to do next? surgery, ?angio with
embolization?
RADIONUCLIDE SCAN
radionuclide scanning has variable accuracy, cannot confirm the
source of bleeding, and may delay other diagnostic and therapeutic
procedures.
Correct localization rate is 41-100%
Accuracy appears to be best when the scan becomes positive within a
short period of time
In one study, 42% of patients underwent an incorrect surgical
procedure based on scintigraphy results. In addition, several studies
have found that regardless of accuracy, scintigraphy did not affect
surgical management
Predictors of positive response
-hemodynamic instability= 62% vs. 21%
->2units transfused within 24 hrs= 64% vs. 32%
CLINICAL SCENARIO
Patient underwent angiogram with
embolization
Vitals improved
What are the chances that pt. will
rebleed?
Colonoscopy?
MESENTERIC ANGIOGRAM
Selective embolization initially controls
hemorrhage in up to 100% of patients, but
rebleeding rates are 15% to 40%
Advantages:
-Precise localization
-Can provide therapy with intra-arterial
vasopressin or coil embolization
-Procedure of choice in briskly bleeding pts
-Minor complication rate of 9% and a 0%
major complication rate
Disadvantages:
-Invasive
-Less sensitive in detecting venous
bleeding
-Can cause ischemia, contrast
reactions, arterial injury
Advantages and disadvantages of common diagnostic procedures used in the evaluation of lower
gastrointestinal bleeding
Procedure Advantages Disadvantages
Colonoscopy Therapeutic possibilities Bowel preparation required
Diagnostic for all sources of
bleeding
Can be difficult to orchestrate without on-
call endoscopy facilities or staff
Needed to confirm diagnosis in
most patients regardless of initial
testing
Invasive
Efficient/cost-effective
Angiography No bowel preparation needed Requires active bleeding at the time of the
exam
Therapeutic possibilities Less sensitive to venous bleeding
May be superior for patients with
severe bleeding
Diagnosis must be confirmed with
endoscopy/surgery
Serious complications are possible
Radionuclide
scintigraphy
Noninvasive Variable accuracy (false positives)
Sensitive to low rates of bleeding Not therapeutic
No bowel preparation May delay therapeutic intervention
Easily repeated if bleeding recurs Diagnosis must be confirmed with
endoscopy/surgery
Flexible
sigmoidoscopy
Diagnostic and therapeutic Visualizes only the left colon
Minimal bowel preparation Colonoscopy or other test usually
necessary to rule out right-sided lesions
Easy to perform
Pt. under went colonoscopy for definitive
diagnosis.
In how many patients there will be more
than one potential diagnosis?
In how many patients there will be no
diagnosis found?
ETIOLOGY
Differential Diagnosis of Lower Gastrointestinal Hemorrhage
COLONIC BLEEDING (95%) % SMALL BOWEL BLEEDING (5%)
Diverticular disease 30-40 Angiodysplasias
Ischemia 5-10 Erosions or ulcers (potassium, NSAIDs)
Anorectal disease 5-15 Crohn's disease
Neoplasia 5-10 Radiation
Infectious colitis 3-8 Meckel's diverticulum
Postpolypectomy 3-7 Neoplasia
Inflammatory bowel disease 3-4 Aortoenteric fistula
Angiodysplasia 3
Radiation colitis/proctitis 1-3
Other 1-5
Unknown 10-25
DIAGNOSTIC DIFFICULTIES
When compared with EGD for upper GI bleeding, the diagnostic
modalities for lower GI bleeding are not as sensitive or specific in making
an accurate diagnosis.
Diagnostic evaluation is further complicated by the observation that, in up
to 40% of patients with lower GI bleeding, more than one potential source
of hemorrhage is identified.
If more than one source is identified, it is critical to confirm the
responsible lesion before initiating aggressive therapy.
This approach may occasionally require a period of observation with
several episodes of bleeding before a definitive diagnosis can be made.
In fact, in up to 25% of patients with lower GI hemorrhage, the bleeding
source is never accurately identified.
CLINICAL SCENARIO
COLONOSCOPY SHOWED
old and BRB in mid colon
tics seen throughout
Dx= probably diverticular beed
Pt was d/c home
CLINICAL SCENARIO
2 wks later readmitted with rebleed and
syncope
Hct 32--- 24
Urgent tagged RBC scan neg
Deep mid AC diverticulum with clot that
could not be removed
What is the next step
SURGERY
Surgery usually is employed for hemorrhage in two settings:
massive or recurrent bleeding.
It is required in 15% to 25% of patients who have diverticular
bleeding and is recommended for patients with a high transfusion
requirement (generally more than four units within a 24-hour
period or greater than 10 units total)
Recurrent bleeding from diverticula occurs in 20% to 40% of
patients and generally is considered an indication for surgery
In patients with serious comorbid medical conditions and without
exsanguinating hemorrhage, this decision should be made
carefully.
Great effort should be made to accurately localize the site of
bleeding preoperatively so that segmental rather than subtotal
colectomy can be performed Operative mortality is 10% even with
accurate localization and up to 57% with blind subtotal colectomy.
Potrebbero piacerti anche
- 09 - Monitoring and Complications of Parenteral NutritionDocumento14 pagine09 - Monitoring and Complications of Parenteral Nutritionbocah_britpopNessuna valutazione finora
- 03 - Nutritional Screening and Assessment PDFDocumento8 pagine03 - Nutritional Screening and Assessment PDFbocah_britpop100% (1)
- 17 - Enhanced Recovery PrinciplesDocumento7 pagine17 - Enhanced Recovery Principlesbocah_britpopNessuna valutazione finora
- 17 - Enhanced Recovery PrinciplesDocumento7 pagine17 - Enhanced Recovery Principlesbocah_britpopNessuna valutazione finora
- Materi PerioperatifDocumento11 pagineMateri PerioperatifSyahdat NurkholiqNessuna valutazione finora
- 17 - The Traumatized PatientDocumento7 pagine17 - The Traumatized Patientbocah_britpopNessuna valutazione finora
- 03 - Energy BalanceDocumento8 pagine03 - Energy Balancebocah_britpopNessuna valutazione finora
- 09 - Compounding and Ready-To-use Preparation of PN Pharmaceutical Aspects. Compatibility and Stability Consideration DrugDocumento21 pagine09 - Compounding and Ready-To-use Preparation of PN Pharmaceutical Aspects. Compatibility and Stability Consideration Drugbocah_britpopNessuna valutazione finora
- 08 - Oral and Sip FeedingDocumento11 pagine08 - Oral and Sip Feedingbocah_britpopNessuna valutazione finora
- Interaction of Bone and Vascular Disease in CKDDocumento7 pagineInteraction of Bone and Vascular Disease in CKDbocah_britpopNessuna valutazione finora
- 08 - Oral and Sip FeedingDocumento11 pagine08 - Oral and Sip Feedingbocah_britpopNessuna valutazione finora
- Indications, Contraindications and Monitoring of Enteral NutritionDocumento13 pagineIndications, Contraindications and Monitoring of Enteral Nutritionbocah_britpopNessuna valutazione finora
- 17 - Enhanced Recovery PrinciplesDocumento7 pagine17 - Enhanced Recovery Principlesbocah_britpopNessuna valutazione finora
- 17 - The Traumatized PatientDocumento7 pagine17 - The Traumatized Patientbocah_britpopNessuna valutazione finora
- 08 - Complications and Monitoring of enDocumento7 pagine08 - Complications and Monitoring of enbocah_britpopNessuna valutazione finora
- Weekly ChartDocumento7 pagineWeekly Chartbocah_britpopNessuna valutazione finora
- m84 PDFDocumento14 paginem84 PDFMico Ga Bisa GendutNessuna valutazione finora
- 08 - Techniques of Enteral NutritionDocumento16 pagine08 - Techniques of Enteral Nutritionbocah_britpopNessuna valutazione finora
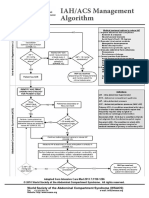
- IAH/ACS Management Algorithm Adapted from Intensive Care MedDocumento1 paginaIAH/ACS Management Algorithm Adapted from Intensive Care Medbocah_britpopNessuna valutazione finora
- 09 - Compounding and Ready-To-use Preparation of PN Pharmaceutical Aspects. Compatibility and Stability Consideration DrugDocumento21 pagine09 - Compounding and Ready-To-use Preparation of PN Pharmaceutical Aspects. Compatibility and Stability Consideration Drugbocah_britpopNessuna valutazione finora
- Materi PerioperatifDocumento11 pagineMateri PerioperatifSyahdat NurkholiqNessuna valutazione finora
- Case Disc RadioDocumento29 pagineCase Disc Radiobocah_britpopNessuna valutazione finora
- Intraabdominal Pressure MonitoringDocumento10 pagineIntraabdominal Pressure Monitoringbocah_britpopNessuna valutazione finora
- Presentation 1Documento2 paginePresentation 1bocah_britpopNessuna valutazione finora
- ACS SabistonDocumento10 pagineACS Sabistonbocah_britpopNessuna valutazione finora
- Interaction of Bone and Vascular Disease in CKDDocumento7 pagineInteraction of Bone and Vascular Disease in CKDbocah_britpopNessuna valutazione finora
- IAH ACS Medical Management 2014Documento1 paginaIAH ACS Medical Management 2014bocah_britpopNessuna valutazione finora
- University of Colorado NICHE Practice Survey SummaryDocumento48 pagineUniversity of Colorado NICHE Practice Survey Summarybocah_britpopNessuna valutazione finora
- Upper Abdominal Pain Case ReportDocumento2 pagineUpper Abdominal Pain Case Reportbocah_britpopNessuna valutazione finora
- HydrocephalusDocumento51 pagineHydrocephalusbocah_britpopNessuna valutazione finora
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (587)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (265)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (119)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- HPS STGDocumento33 pagineHPS STGDJGGNessuna valutazione finora
- Billroth ii procedure explainedDocumento2 pagineBillroth ii procedure explainedJasmin MirandaNessuna valutazione finora
- 4 2 - 181 182 PDFDocumento2 pagine4 2 - 181 182 PDFNam LeNessuna valutazione finora
- MCN Test DrillsDocumento20 pagineMCN Test DrillsFamily PlanningNessuna valutazione finora
- QuestionsDocumento26 pagineQuestionsLyka Mae Imbat - PacnisNessuna valutazione finora
- Clinical Gynaecology: Juta - Co.za/pdf/23698Documento3 pagineClinical Gynaecology: Juta - Co.za/pdf/23698Thato MotaungNessuna valutazione finora
- 42 - Circulation and Gas ExchangeDocumento97 pagine42 - Circulation and Gas ExchangeTrisha SantillanNessuna valutazione finora
- Dysphagia Lusoria: A Comprehensive ReviewDocumento6 pagineDysphagia Lusoria: A Comprehensive ReviewDante ChavezNessuna valutazione finora
- Abdominal wall anatomy and common abdominal incisionsDocumento42 pagineAbdominal wall anatomy and common abdominal incisionsSamar AhmadNessuna valutazione finora
- Children's dental health: Retention of teethDocumento4 pagineChildren's dental health: Retention of teethKandiwapaNessuna valutazione finora
- Easy Pharyngeal Anesthesia with Lidocaine LozengesDocumento6 pagineEasy Pharyngeal Anesthesia with Lidocaine LozengespaulaNessuna valutazione finora
- AUTHORIZED HOSPITALS LIST CPRI GOI CGHSDocumento11 pagineAUTHORIZED HOSPITALS LIST CPRI GOI CGHSNaveenkumar PalanisamyNessuna valutazione finora
- Right Flank AbomasopexyDocumento24 pagineRight Flank Abomasopexy7candlesburningNessuna valutazione finora
- Unicompartmental Knee ArthroplastyDocumento10 pagineUnicompartmental Knee Arthroplastycronoss21Nessuna valutazione finora
- Balloon PumpDocumento1 paginaBalloon PumpRaghavendra PrasadNessuna valutazione finora
- Imaging Evaluation of Tracheobronchial InjuriesDocumento14 pagineImaging Evaluation of Tracheobronchial InjuriesSantiago TapiaNessuna valutazione finora
- Colleen J. Rutherford - Differentiating Surgical Instruments (With CDROM) - F. A. Davis Company (First Published March 7th 2005) (2011)Documento211 pagineColleen J. Rutherford - Differentiating Surgical Instruments (With CDROM) - F. A. Davis Company (First Published March 7th 2005) (2011)Amra Fejzic100% (1)
- L1) Oral Cavity, Palate and TongueDocumento39 pagineL1) Oral Cavity, Palate and Tongue3amroooni.a.aNessuna valutazione finora
- Bio Data Name: Prof. Dr. Vinod Kapoor Date/ Place of Birth Educational QualificationsDocumento6 pagineBio Data Name: Prof. Dr. Vinod Kapoor Date/ Place of Birth Educational Qualificationsayub_008Nessuna valutazione finora
- F3 C3 Human Blood Circulatory System ExerciseDocumento3 pagineF3 C3 Human Blood Circulatory System ExerciseCharvini SreeNessuna valutazione finora
- Newborn Capillary Blood CollectionDocumento3 pagineNewborn Capillary Blood CollectionYwagar YwagarNessuna valutazione finora
- Cog Thread LiftDocumento5 pagineCog Thread Liftemilly vidya71% (7)
- Carotid and Vertebral Ultrasonography - Dr. DanielDocumento74 pagineCarotid and Vertebral Ultrasonography - Dr. DanielSuci Rahayu Evasha100% (1)
- GH-ZOLL-Autopulse Quick Case-Instruction ManualDocumento80 pagineGH-ZOLL-Autopulse Quick Case-Instruction ManualjillNessuna valutazione finora
- Medetomidine-Buprenorphine Combo Reduces Isoflurane Needs in CatsDocumento9 pagineMedetomidine-Buprenorphine Combo Reduces Isoflurane Needs in CatsDaniela MartínezNessuna valutazione finora
- Medical Emergency ProcedureDocumento2 pagineMedical Emergency ProcedureAmeena HarisNessuna valutazione finora
- PEMASANGAN ECG 3 LEAD DAN 5 LEADDocumento3 paginePEMASANGAN ECG 3 LEAD DAN 5 LEADPrio Si IyoNessuna valutazione finora
- WelcomeDocumento74 pagineWelcomeSagarRathodNessuna valutazione finora
- Complete IssueDocumento212 pagineComplete IssueAmril MukminNessuna valutazione finora
- V-Gel Cleaning & User GuideDocumento3 pagineV-Gel Cleaning & User GuideInstrulife OostkampNessuna valutazione finora