Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
08&09 Oral Hypoglycemics-Level 11
Caricato da
Usman Ali Akbar0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
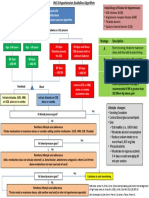
41 visualizzazioni48 pagineThis document discusses the classification, mechanisms of action, pharmacokinetics, clinical uses, and side effects of various classes of oral hypoglycemic drugs used to treat type 2 diabetes. It covers insulin secretagogues like sulfonylureas and meglitinides, insulin sensitizers like biguanides and thiazolidinediones, alpha-glucosidase inhibitors, incretin mimetics, and dipeptidyl peptidase-4 inhibitors. The goal is for students to understand how each class of drug works to lower blood glucose levels and their proper uses and adverse effect profiles.
Descrizione originale:
ORal
Titolo originale
08&09 Oral Hypoglycemics-level 11
Copyright
© © All Rights Reserved
Formati disponibili
PPT, PDF, TXT o leggi online da Scribd
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoThis document discusses the classification, mechanisms of action, pharmacokinetics, clinical uses, and side effects of various classes of oral hypoglycemic drugs used to treat type 2 diabetes. It covers insulin secretagogues like sulfonylureas and meglitinides, insulin sensitizers like biguanides and thiazolidinediones, alpha-glucosidase inhibitors, incretin mimetics, and dipeptidyl peptidase-4 inhibitors. The goal is for students to understand how each class of drug works to lower blood glucose levels and their proper uses and adverse effect profiles.
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato PPT, PDF, TXT o leggi online su Scribd
0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
41 visualizzazioni48 pagine08&09 Oral Hypoglycemics-Level 11
Caricato da
Usman Ali AkbarThis document discusses the classification, mechanisms of action, pharmacokinetics, clinical uses, and side effects of various classes of oral hypoglycemic drugs used to treat type 2 diabetes. It covers insulin secretagogues like sulfonylureas and meglitinides, insulin sensitizers like biguanides and thiazolidinediones, alpha-glucosidase inhibitors, incretin mimetics, and dipeptidyl peptidase-4 inhibitors. The goal is for students to understand how each class of drug works to lower blood glucose levels and their proper uses and adverse effect profiles.
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato PPT, PDF, TXT o leggi online su Scribd
Sei sulla pagina 1di 48
Objectives
By the end of this lecture, students should be able to:
Classify different categories of oral hypoglycemic drugs.
Identify mechanism of action, pharmacokinetics and
pharmacodynamics of each class oral hypoglycemic drugs.
Identify the clinical uses of hypoglycemic drugs
Know the side effects, contraindications of each class of
oral hypoglycemic drugs.
Types of diabetes mellitus
Type I
due to autoimmune or viral diseases
Type II
due to obesity, genetic factors
Pts with Type 11 diabetes have
two physiological defects:
1. Abnormal insulin secretion.
2. Resistance to insulin action in target
tissues associated with decreased
number of insulin receptors.
Drugs used for treatment of
Type-2 diabetes
1. Sulfonylurea drugs
2. Meglitinide analogues
3. Biguanides
4. Thiazolidinediones.
5.Alpha-glucosidase inhibitors.
6. Dipeptidyl peptidase-4(DPP-4) inhibitors
Insulin secretagogues
Sulfonylurea drugs
Meglitinide analogues
Insulin sensitizers
Biguanides
Thiazolidinediones
Oral hypoglycemic drugs
Others
Alpha glucosidase inhibitors
Dipeptidyl peptidase-4(DPP-4)
inhibitors
Insulin secretagogues
Are drugs which increase the amount of
insulin secreted by the pancreas
Include:
Sulfonylureas
Meglitinides
Classification of sulfonylureas
Tolbutamide
Acetohexamide
Tolazamide
Chlorpropamide
Glipizide
Glyburide
(Glibenclamide)
Glimepiride
First generation
Long
acting
Short
acting
second generation
Short
acting
Intermediate
acting
Long
acting
Stimulate insulin release from functioning B cells
by blocking of ATP-sensitive K channels resulting
in depolarization and calcium influx(Hence, not
effective in totally insulin-deficient pts type-1).
Potentiation of insulin action on target tissues.
Reduction of serum glucagon concentration.
Mechanism of action of sulfonylureas:
Mechanisms of Insulin Release
Pharmacokinetics of sulfonylureas:
Orally, well absorbed.
Reach peak concentration after 2-4 hr.
All are highly bound to plasma proteins.
Duration of action is variable.
Second generation has longer duration than
first generation.
Metabolized in liver
excreted in urine
Cross placenta, stimulate fetal B cells to release
insulin hypoglycemia at birth.
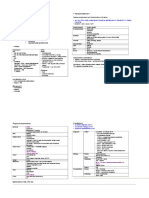
Tolbutamid
short-
acting
Acetohexamide
intermediate-
acting
Tolazamide
intermediate
-acting
Chlorpropa
mide
long- acting
Absorption Well Well Slow Well
Metabolism Yes Yes Yes Yes
Metabolites Inactive Active Active Inactive
Half-life 4 - 5 hrs 6 8 hrs 7 hrs 24 40 hrs
Duration of
action
Short
(6 8 hrs)
Intermediate
(12 20 hrs)
Intermediate
(12 18 hrs)
Long
( 20 60
hrs)
Excretion Urine Urine Urine Urine
First generation sulfonylurea
Tolbutamide:
safe for old diabetic patients or pts with
renal impairment.
First generation sulfonylureas
Glipizide Glibenclamide
(Glyburide)
Glimepiride
Absorption Well Well Well
Metabolism Yes Yes Yes
Metabolites Inactive Moderate activity Moderate activity
Half-life 2 4 hrs Less than 3 hrs 5 - 9 hrs
Duration of 10 16 hrs 12 24 hrs 12 24 hrs
action short long long
Doses Divided doses
30 min before
meals
Single dose Single dose
1 mg
Excretion Urine Urine Urine
SECOND GENERATION SULPHONYLUREA
Type II diabetes:
monotherapy or in combination with other
antidiabetic drugs.
Uses of sulfonylureas
Unwanted Effects:
1. Hyperinsulinemia & Hypoglycemia:
2. Weight gain due to increase in appetite
e.g. Repaglinide
Rapidly acting insulin secretagogues
Meglitinide analogues
Mechanism of Action:
Insulin secretagogue as sulfonylureas.
Pharmacokinetics of Meglitinides
Orally, well absorbed.
Very fast onset of action, peak 1 h.
short duration of action (4 h).
Metabolized in the liver & excreted in
bile.
Type II diabetes:
monotherapy or combined with other
antidiabetic drugs.
Patients allergic to sulfonylurea
Uses of Meglitinides
Hypoglycemia
Weight gain.
Adverse effects of Meglitinides
1. Biguanides, e.g. Metformin
2. Thiazolidinediones, e.g. pioglitazone
Insulin sensitizers
BIGUANIDES
E.g. Metformin
Does not stimulate insulin release.
Increases liver ,muscle &adipose tissues
sensitivity to insulin & increase peripheral
glucose utilization.
Inhibits gluconeogenesis.
Impairs glucose absorption from GIT.
Mechanism of action of metformin
orally.
Not bound to serum protein.
Not metabolized.
t 3 hours.
Excreted unchanged in urine
Pharmacokinetics of metformin
Obese patients with type II diabetes
Monotherapy or in combination.
Advantages:
No risk of hyperinsulinemia or hypoglycemia
or weight gain (anorexia).
Uses of metformin
Metallic taste in the mouth
GIT disturbances: nausea, vomiting, diarrhea
Lactic acidosis
Long term use interferes with vitamin B
12
absorption.
Adverse effects of metformin
Pregnancy.
Renal disease.
Liver disease.
Alcoholism.
Heart failure
Contraindications of metformin
Insulin sensitizers
Thiazolidinediones (glitazones)
Pioglitazone
Mechanism of action
Increase sensitivity of target tissues to insulin.
Increase glucose uptake and utilization in
muscle and adipose tissue.
Pharmacokinetics of pioglitazone
Orally (once daily dose).
Highly bound to plasma albumins (99%)
Slow onset of activity
Half life 3-4 h
Metabolized in the liver
Excreted in urine 64% & bile
Type II diabetes with insulin resistance.
Used either alone or combined with
sulfonylurea, biguanides or insulin.
No risk of hypoglycemia when used alone
Uses of pioglitazone
Hepatotoxicity ?? (liver function tests for
1st year of therapy).
Fluid retention (Edema).
Precipitate congestive heart failure
Mild weight gain.
Adverse effects of pioglitazone
E.g. Acarbose, Meglitol
Reversible inhibitors of intestinal -
glucosidases in intestinal brush border
responsible for degradation of
oligosaccharides to monosaccharides.
-Glucosidase inhibitors
decrease carbohydrate digestion and
absorption in small intestine.
Decrease postprandial hyperglycemia.
Taken just before meals.
No hypoglycemia if used alone.
-Glucosidase inhibitors
37
-GLUCOSIDASE INHIBITORS (Contd.)
MECHANISM OF ACTION
Acarbose
Given orally, poorly absorbed.
Metabolized by intestinal bacteria.
Excreted in stool and urine.
Kinetics of -glucosidase inhibitors
GIT: Flatulence, diarrhea, abdominal
pain.
No hypoglycemia if used alone.
Adverse effects of -glucosidase
inhibitors
Incretin mimetics
e.g. Exenatide(GLP-1)
Incretins are GI hormones secreted in
response to food, carried through circulation
to the beta cells to stimulate insulin secretion
& decrease glucagon secretion.
Incretins
Two main Incretin hormones:
GLP-1 (glucagon-like peptide-1)
GIP (gastric inhibitory peptide or glucose-
dependent insulinotropic peptide)
Both are inactivated by dipeptidyl peptidase-4
(DPP-4).
Incretin mimetics
Exenatide
is glucagon-like peptide-1 (GLP-1) agonist.
given s.c. once or twice daily
Therapy of patients with type 2 diabetes
who are not controlled with oral medicine.
Adverse efects
Nausea & vomiting(most common)
Dipeptidyl peptidase-4 (DPP- 4 )
inhibitors
e.g. Sitagliptin
Orally
Given once daily
half life 8-14 h
Dose is reduced in pts with renal
impairment
Mechanism of action of sitagliptin
Inhibit DPP-4 enzyme and leads to an
increase in incretin hormones level.
This results in an increase in insulin
secretion & decrease in glucagon secretion.
Mechanism of
action
Clinical uses
Type 2 DM as an adjunct to diet &
exercise as a monotherapy or in
combination with other antidiabetic drugs.
Adverse effects
Nausea, abdominal pain, diarrhea
Nasopharyngitis
Potrebbero piacerti anche
- National Leaflet About CKD and eGFR For GPs (Updated September 2007)Documento2 pagineNational Leaflet About CKD and eGFR For GPs (Updated September 2007)Dhika ArdiansyahNessuna valutazione finora
- DR Colbert Keto Diet PDFDocumento11 pagineDR Colbert Keto Diet PDFHamilton Durant100% (1)
- MYP Biology 10 Worksheet: Diet, Insulin and Blood GlucoseDocumento3 pagineMYP Biology 10 Worksheet: Diet, Insulin and Blood GlucoseLizzy AnthonyNessuna valutazione finora
- 7.8 Collect Data & Come Up With Plan For Day & Nursing Diagnosis Pre-Conference 8-9 Vitals Then Chart, AM Care, StartDocumento2 pagine7.8 Collect Data & Come Up With Plan For Day & Nursing Diagnosis Pre-Conference 8-9 Vitals Then Chart, AM Care, StartSade' CovingtonNessuna valutazione finora
- CD Im PrimerDocumento28 pagineCD Im PrimerTiagogiesteiraNessuna valutazione finora
- Third-Year OSCE Manual 2019-2020Documento17 pagineThird-Year OSCE Manual 2019-2020Agleema AhmedNessuna valutazione finora
- Approach: A. How The Kidney Handle The Proteins?Documento9 pagineApproach: A. How The Kidney Handle The Proteins?Rashed ShatnawiNessuna valutazione finora
- Mo Intern Handbook - FinalDocumento37 pagineMo Intern Handbook - FinalGideon K. MutaiNessuna valutazione finora
- Stroke - Final ReportDocumento16 pagineStroke - Final ReportgolokipokNessuna valutazione finora
- Year 6 Clerkship - Welcome & Curriculum Class 2020 (Revised 25.04.2019)Documento190 pagineYear 6 Clerkship - Welcome & Curriculum Class 2020 (Revised 25.04.2019)Ali SemajNessuna valutazione finora
- Problem-based Approach to Gastroenterology and HepatologyDa EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisNessuna valutazione finora
- Exercise PrescriptionDocumento87 pagineExercise PrescriptionDianne Faye ManabatNessuna valutazione finora
- Introduction To Internal Medicine - PPTMDocumento30 pagineIntroduction To Internal Medicine - PPTMAddyNessuna valutazione finora
- Diabetes and Complications: When Documenting Diabetes, It's Important To Note The FollowingDocumento2 pagineDiabetes and Complications: When Documenting Diabetes, It's Important To Note The Followingmeikaizen100% (1)
- Nutritionalanemia25thmarch2021 210403063057Documento29 pagineNutritionalanemia25thmarch2021 210403063057najeebNessuna valutazione finora
- Organophosphate PoisoningDocumento23 pagineOrganophosphate PoisoningUsman Ali AkbarNessuna valutazione finora
- Obstetrics OBDocumento65 pagineObstetrics OBVicviclookTheking100% (1)
- Gestational Diabetes MellitusDocumento16 pagineGestational Diabetes Mellitusarjunr19910% (1)
- Pass 2010 ScheduleDocumento1 paginaPass 2010 SchedulewldcrdNessuna valutazione finora
- DiabetesMellitusMasterclass MedmasteryHandbookDocumento88 pagineDiabetesMellitusMasterclass MedmasteryHandbookDeenissa Van GawaranNessuna valutazione finora
- Preventive Health: Based On The USPSTF 2014Documento42 paginePreventive Health: Based On The USPSTF 2014Louella CarpioNessuna valutazione finora
- Pharma PrelimDocumento8 paginePharma PrelimNom NomNessuna valutazione finora
- Practical Gastroenterology and Hepatology Board Review ToolkitDa EverandPractical Gastroenterology and Hepatology Board Review ToolkitKenneth R. DeVaultNessuna valutazione finora
- Mood Disorders: Advanced Practice Education AssociatesDocumento11 pagineMood Disorders: Advanced Practice Education AssociatesAndrea100% (1)
- Read MeDocumento1 paginaRead MeJack GuccioneNessuna valutazione finora
- Case Study - DM Type 2-Presentation On DIAMICRONDocumento37 pagineCase Study - DM Type 2-Presentation On DIAMICRONdrnasim20088171Nessuna valutazione finora
- Alarm Symptoms of Hematoonco in Pediatrics: Dr. Cece Alfalah, M.Biomed, Sp.A (K) Pediatric Hematology and OncologyDocumento22 pagineAlarm Symptoms of Hematoonco in Pediatrics: Dr. Cece Alfalah, M.Biomed, Sp.A (K) Pediatric Hematology and OncologyMuhammad ArifNessuna valutazione finora
- Glucose Oxidase MethodDocumento5 pagineGlucose Oxidase MethodMayara MeloNessuna valutazione finora
- Treatment of Resistant and Refractory HypertensionDocumento21 pagineTreatment of Resistant and Refractory HypertensionLuis Rodriguez100% (1)
- Diabetic FootDocumento22 pagineDiabetic FootNaikko80100% (2)
- DiabeticcasestudyDocumento7 pagineDiabeticcasestudyapi-272773859Nessuna valutazione finora
- Drug StudyDocumento14 pagineDrug StudyLovely Saad TubañaNessuna valutazione finora
- Introspect Manual Lecture Eng (2004)Documento32 pagineIntrospect Manual Lecture Eng (2004)OBERON-INTROSPECT-BIOSPECT100% (8)
- Case History in PeriodonticsDocumento154 pagineCase History in Periodonticsrupali89% (9)
- Adult Electrolyte Replacement Protocol - MCLN 0006 J PDFDocumento1 paginaAdult Electrolyte Replacement Protocol - MCLN 0006 J PDFCraigNessuna valutazione finora
- 58 Cases History and Physical Exam BookDocumento102 pagine58 Cases History and Physical Exam BookeleazarmdNessuna valutazione finora
- Final GIT Case PresentationDocumento53 pagineFinal GIT Case PresentationRovan100% (1)
- Nephrology: Omar K MRCP IrelandDocumento54 pagineNephrology: Omar K MRCP IrelandManmeet SNessuna valutazione finora
- Clinical CasesDocumento12 pagineClinical CasesAndreea HanuNessuna valutazione finora
- Insulin and Oral Hypoglycemic DrugsDocumento30 pagineInsulin and Oral Hypoglycemic DrugsAngga NugrahaNessuna valutazione finora
- Practical Guidance On The Use of Premix Insulin - FinalDocumento14 paginePractical Guidance On The Use of Premix Insulin - FinalJonesius Eden ManoppoNessuna valutazione finora
- Article - Medical ErrorsDocumento4 pagineArticle - Medical ErrorsDavid S. ChouNessuna valutazione finora
- Peadiatric Guildlines For Malaysian House OfficerDocumento44 paginePeadiatric Guildlines For Malaysian House OfficerAlex MatthewNessuna valutazione finora
- Mock Record B-1-2-Well Child VisitsDocumento4 pagineMock Record B-1-2-Well Child VisitsaelteeNessuna valutazione finora
- Ectopic PregnancyDocumento76 pagineEctopic PregnancyVivian Jean TapayaNessuna valutazione finora
- Aquifer InternalMedicine11 - 45Documento8 pagineAquifer InternalMedicine11 - 45JulieNessuna valutazione finora
- Gastroenterology AscitesDocumento2 pagineGastroenterology AscitesNour SamadNessuna valutazione finora
- Family Medicine PresentationDocumento53 pagineFamily Medicine PresentationNancy BaggaNessuna valutazione finora
- Gyne Case COCDocumento37 pagineGyne Case COCLian BaylosisNessuna valutazione finora
- Pharmacology Exam4 ReviewDocumento8 paginePharmacology Exam4 ReviewNatalia BortellNessuna valutazione finora
- Reye's SyndromeDocumento11 pagineReye's SyndromeChristine Go100% (1)
- General Population (No Diabetes or CKD) Diabetes or CKD PresentDocumento1 paginaGeneral Population (No Diabetes or CKD) Diabetes or CKD PresentMuthia ArsilNessuna valutazione finora
- Step 1 REVIEWDocumento140 pagineStep 1 REVIEWRima HajjarNessuna valutazione finora
- Newborn NotesDocumento44 pagineNewborn NotesHaziq KamardinNessuna valutazione finora
- New Guidelines For The Diagnosis of Paediatric Coeliac DiseaseDocumento3 pagineNew Guidelines For The Diagnosis of Paediatric Coeliac DiseaseDiana NicaNessuna valutazione finora
- From This Age in What Patient Group? Start Screening For With Test FrequencyDocumento7 pagineFrom This Age in What Patient Group? Start Screening For With Test Frequencyphoenix24601Nessuna valutazione finora
- UTI On A Background of Obstructive NephropathyDocumento26 pagineUTI On A Background of Obstructive NephropathyAminath MeesanNessuna valutazione finora
- Personal Statement - FinalDocumento2 paginePersonal Statement - Finalapi-383932502Nessuna valutazione finora
- Turkey Book 03 Internal Medicine PDFDocumento47 pagineTurkey Book 03 Internal Medicine PDFPreaisNessuna valutazione finora
- USMLE Step 3 ER PDFDocumento12 pagineUSMLE Step 3 ER PDFlalaNessuna valutazione finora
- Victorias New ResumeDocumento2 pagineVictorias New Resumeapi-513192361Nessuna valutazione finora
- Nausea VomitingDocumento36 pagineNausea VomitingDian Fitri100% (1)
- Akd & CKDDocumento44 pagineAkd & CKDﻣﻠﻚ عيسىNessuna valutazione finora
- The Stages of Prevention - Primer On Public Health PopulationDocumento2 pagineThe Stages of Prevention - Primer On Public Health PopulationBSN 201450% (2)
- Grand Rounds - Pulmonary EmbolismDocumento25 pagineGrand Rounds - Pulmonary EmbolismAdrian CastroNessuna valutazione finora
- MGH/HMS Internal Medicine Comprehensive Review and Update Renal Cases - June 2021Documento49 pagineMGH/HMS Internal Medicine Comprehensive Review and Update Renal Cases - June 2021Churschmann SpiralNessuna valutazione finora
- Inborn Errors of Metabolism - Basics For Students (Iver Andreas Norbergs Kopi Som Er I Konflikt 2016-01-24)Documento4 pagineInborn Errors of Metabolism - Basics For Students (Iver Andreas Norbergs Kopi Som Er I Konflikt 2016-01-24)Wen Jie LauNessuna valutazione finora
- Breaking Bad News 1 PDFDocumento5 pagineBreaking Bad News 1 PDFSaeed HasanNessuna valutazione finora
- CCT - CCI Code of EthicsDocumento2 pagineCCT - CCI Code of EthicsAvanca LouisNessuna valutazione finora
- Ventricular Septal Defect, A Simple Guide To The Condition, Treatment And Related ConditionsDa EverandVentricular Septal Defect, A Simple Guide To The Condition, Treatment And Related ConditionsNessuna valutazione finora
- Urinary Tract Infection & PyelonephritisDocumento3 pagineUrinary Tract Infection & PyelonephritisUsman Ali AkbarNessuna valutazione finora
- Polycystic Kidneys: Adult PKD: ComplicationsDocumento1 paginaPolycystic Kidneys: Adult PKD: ComplicationsUsman Ali AkbarNessuna valutazione finora
- Chronic Renal Failure: Concise Long Case ApproachDocumento3 pagineChronic Renal Failure: Concise Long Case ApproachUsman Ali AkbarNessuna valutazione finora
- GI Bleeding Team Work - 2nd EditionDocumento9 pagineGI Bleeding Team Work - 2nd EditionUsman Ali AkbarNessuna valutazione finora
- Obstructive Airway Disease: Dr. Khalid Al-Mobaireek King Khalid University HospitalDocumento53 pagineObstructive Airway Disease: Dr. Khalid Al-Mobaireek King Khalid University HospitalUsman Ali AkbarNessuna valutazione finora
- Renal Tubular Acidosis Summary - AdjDocumento1 paginaRenal Tubular Acidosis Summary - AdjUsman Ali AkbarNessuna valutazione finora
- DialysisDocumento2 pagineDialysisUsman Ali AkbarNessuna valutazione finora
- Recurrent VomitingDocumento16 pagineRecurrent VomitingUsman Ali AkbarNessuna valutazione finora
- King Khalid University Hospital Department of Obstetrics & Gyncology Course 481Documento40 pagineKing Khalid University Hospital Department of Obstetrics & Gyncology Course 481Usman Ali AkbarNessuna valutazione finora
- DR Othman Alharbi, MBBS FRCPC Assistance Professor & Consultant Gastroenterology College of Medicine King Saud UniversityDocumento18 pagineDR Othman Alharbi, MBBS FRCPC Assistance Professor & Consultant Gastroenterology College of Medicine King Saud UniversityUsman Ali AkbarNessuna valutazione finora
- Anaemia in PregnancyDocumento13 pagineAnaemia in PregnancyUsman Ali AkbarNessuna valutazione finora
- Recurrent Nausea Andor VomitingDocumento8 pagineRecurrent Nausea Andor VomitingUsman Ali AkbarNessuna valutazione finora
- Cord ProlapseDocumento2 pagineCord ProlapseUsman Ali AkbarNessuna valutazione finora
- Through The Strange WindsDocumento5 pagineThrough The Strange WindsUsman Ali AkbarNessuna valutazione finora
- Alas!! EmpytinessDocumento2 pagineAlas!! EmpytinessUsman Ali AkbarNessuna valutazione finora
- GRAM NEGATIVE RODS (5) Fastidious Organisms From Animal Sources (A)Documento1 paginaGRAM NEGATIVE RODS (5) Fastidious Organisms From Animal Sources (A)Usman Ali AkbarNessuna valutazione finora
- Subject: Permission For Badminton Court NID, Multan: TH THDocumento1 paginaSubject: Permission For Badminton Court NID, Multan: TH THUsman Ali AkbarNessuna valutazione finora
- Lect 1:: M2Pasysl21 Urinary SystemDocumento4 pagineLect 1:: M2Pasysl21 Urinary SystemUsman Ali AkbarNessuna valutazione finora
- Untold Stanza... : - Nasim Alam (N-61)Documento1 paginaUntold Stanza... : - Nasim Alam (N-61)Usman Ali AkbarNessuna valutazione finora
- Death and The Mother For MergeDocumento4 pagineDeath and The Mother For MergeUsman Ali AkbarNessuna valutazione finora
- When Hope DiesDocumento2 pagineWhen Hope DiesUsman Ali AkbarNessuna valutazione finora
- National Guidelines For GDMDocumento24 pagineNational Guidelines For GDMVijaya LakshmiNessuna valutazione finora
- Influence of Diabetes Mellitus On Orthodontic TreatmentDocumento30 pagineInfluence of Diabetes Mellitus On Orthodontic TreatmentSofie Lavida KadafiNessuna valutazione finora
- Pressure SoresDocumento43 paginePressure SoresArpanpatelNessuna valutazione finora
- ACR Albumin Creatinine Ratio To Be PRESENTED BY HMN TO THE NEW MED TECH TRAINEES IN JAHRA HEALTH CENTER Apr 23 2014Documento22 pagineACR Albumin Creatinine Ratio To Be PRESENTED BY HMN TO THE NEW MED TECH TRAINEES IN JAHRA HEALTH CENTER Apr 23 2014honorinanuguidNessuna valutazione finora
- Pta 2540 Case Study Amputation and Diabetes - Jade ClawsonDocumento3 paginePta 2540 Case Study Amputation and Diabetes - Jade Clawsonapi-317395769Nessuna valutazione finora
- Cancer Survivor DR Tom Wu1Documento6 pagineCancer Survivor DR Tom Wu1Tan CKNessuna valutazione finora
- Human Insulin Vs Insulin AnalogDocumento7 pagineHuman Insulin Vs Insulin AnalogWita Ferani Kartika100% (1)
- Health Promotion and Maintenance RationalesDocumento9 pagineHealth Promotion and Maintenance Rationalesrhymes2u100% (4)
- Metformin For GDMDocumento7 pagineMetformin For GDMRoro WidyastutiNessuna valutazione finora
- Reserach in PediaDocumento106 pagineReserach in Pediaraunak0% (1)
- The Diabetes and The BrainDocumento26 pagineThe Diabetes and The BrainPrecious SantayanaNessuna valutazione finora
- Clayton & Willihnganz: Basic Pharmacology For Nurses, 17th EditionDocumento4 pagineClayton & Willihnganz: Basic Pharmacology For Nurses, 17th EditionabsianoNessuna valutazione finora
- Nutrition Management of Diabetes During PregnancyDocumento31 pagineNutrition Management of Diabetes During PregnancyAbdelhamid ElbilbeisiNessuna valutazione finora
- Why Is Sleep ImportantDocumento5 pagineWhy Is Sleep ImportantaqilahaimanNessuna valutazione finora
- Form2midyear ExamDocumento11 pagineForm2midyear ExamBazilah HasanNessuna valutazione finora
- Anesthesia For LiposuctionDocumento26 pagineAnesthesia For Liposuctionjulissand10Nessuna valutazione finora
- Gudoy, Charies Jamille 12-WeierstrassDocumento4 pagineGudoy, Charies Jamille 12-WeierstrasschaNessuna valutazione finora
- Hierbas MexicoDocumento16 pagineHierbas MexicoSalomon AldanaNessuna valutazione finora