Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Caesarean Section
Caricato da
Muriel CardosoCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Caesarean Section
Caricato da
Muriel CardosoCopyright:
Formati disponibili
Caesarean Section
Clinical Guideline 13
RCOG APRIL 2004.
Caesarean Section
Doctor, I Would like a Caesarean
Section!
Making the Decision
Caesarean Section
Carrying Out the Procedure
How we can Decrease Morbidity
Regional Anaesthesia
Antibiotic Cover
Thromboprophylaxis
Anti-emetics
Timing-at 39 weeks
Caesarean Section
Reducing the likelihood of C Section
ECV-except in labour, ut scar , abn, foetal
compromise, ROM, blding, med condn.
Support During Labour
IOL AT 41 weeks
Partogram
Consultant involvement
EFM and FBS
Caesarean Section
INCIDENCE: 1 IN 5!
Common Indications
PRIMARY SECTION
Failure to progress 25%
Presumed foetal compromise 28%
Breech 14%
Caesarean Section
REPEAT SECTIONS
Previous Section 44%
Maternal request 12%
Failure to progress 10%
Presumed foetal Compromise 9%
Breech 3%
Caesarean Section
Provision of Information
EVIDENCE BASED
Indication
What the procedure involves.
Associated risks and benefits
Implications for future pregnancy
and birth after CS.
Caesarean Section
CONSENT
Risks v/s Benefits
Right to Refuse
Record Indication in order of Influencing
Factor
Caesarean Section
EMERGENCY LSCSHOW URGENT
Immediate threat to life of mother/foetus.
Maternal/foetal compromise-not
immediately life threatening
No maternal/foetal compromise but needs
early delivery.
Delivery timed to suit woman and staff.
Caesarean Section
PLANNED CS
1. Breech- ECV Failed OR CI
2. Multiple pregnancy-1 AND 2 TW.
3. Preterm birth- Not routinely
4. Small for Gestational Age- Not routinely
5. Placenta praevia Gr 3,4.
6. Predicting CS for CPD in labour -NO
7. Mother to Child Transmission- HIV,HepB
Hep C, HSV
Caesarean Section
Maternal Request
NOT an indication on its own.
Discuss Risks v/s Benefits
Is she afraid of childbirth-counsel.
Clinician has a right to refuse.
Respect her decision and offer referral.
Caesarean Section
Factors which DONT affect CS Rates
Walking
Position during labour
Epidural
Food and drink
Water Birthing
Caesarean Section
TIMING OF CAESAREAN SECTION
39 WEEKS
30 MINUTES FROM DECISION-TO-
DELIVERY
Caesarean Section
NECESSARY
HB (blood loss >1 litre
occurs in 4-8%)
NOT NECESSARY
ADVANCE BB3
CROSSMATCH
CLOTTING PROFILE
USG FOR PLACENTA
Caesarean Section
Anaesthesia
Regional-safer even in placenta praevia.
Rapid Sequence Induction
Antacid, H2 receptor antag, PPI
Antiemetic
Table tilt
Caesarean Section
SURGICAL TECHNIQUES
Double Glove for HIV
Joel Cohen- LESSPAIN, BETTER COSMETIC.
FASTER, LESS FEBRILE MORB.
Blunt extension of uterine incision-LESS BLD
LOSS
Placenta CCT
Dont exteriorize IT ONLY PAINS
Dont close peritoneum.-QUICK, LESS
ANALGESIA
Caesarean section
Suture in 2 layers (Bujold 2002, 3%v/s
0.5% risk of rupture with single layer)
Subcutaneous stitch only if >2cm.
Effects of suture materials unclear.
Antibiotics,prophylactic
Thromboprophylaxis
Caesarean Section
Care of the Baby
Paediatrician
Temperature maintenance
Skin to skin contact
BF support
Caesarean Section
Care of the woman
Monitoring-Half hourly for 2 hrs, then hrly.
Opioids- pca, intrathecal,NSAIDS
Food and Drink
Bladder care
Opportunity to Discuss
Hospital Stay
Caesarean Section
RECOVERY
Pain Relief
Wound care- DRESSING,S/O INFECTION
UTI
SUI (4%)
UT Injury (1 in 1000)
Resume activities
Caesarean Section
VBAC
Maternal Preferences and Priorities
Risks and Benefits
Risk of Rupture
Risk of perinatal and maternal Mortality
and Morbidity.
Caesarean Section
Pregnancy and Childbirth following C S
Rupture
Planned CS 12 /10000
Planned VBAC 35 /10000
Induced-non PG 80/ 10000
Induced-PG 240/10000
Caesarean Section
Pregnancy and Childbirth following C S
Risk of Foetal Intrapartum Death
VBAC 10 /10000
ERCS -- 1/10000
Caesarean Section
VBAC
Continuous EFM
Immediate access to CS
Immediate access to blood transfusion.
Better success if prior vaginal delivery
reduced
CAESAREAN VAGINAL
Perineal pain 2% 5%
U Incontinence
At 3 months
4.5% 7.3%
Prolapse Overall----------- 5%
Increased
CAESAREAN VAGINAL
Abdominal pain 9% 5%
Bladder Injury 0.1% 0.003%
Ureteric Injury 0.03% 0.001%
Further surgery 0.5% 0.03%
Hysterectomy 0.8% 0.01%
ICU Care 0.9% 0.1%
Thrombo-e Overall 0.04 --- To 0.16%
Increased
CAESAREAN VAGINAL
Hospital Stay 3-4 days 1-2 days
Readmission 5.3% 2.2%
Maternal Death 82.3/million 16.9/million
No more childrn 42% 29%
Placenta previa 0.7% 0.5%
Future rupture 0.4% 0.01%
Future SB 0.4% 0.2%
Resp morbidity 3.5% 0.5%
Not DIFFERENT
CAESAREAN VAGINAL
Haemorrhage 0.5% 0.7%
Infection 6.4% 4.9%
Gen tr Injury 0.6% 0.8%
Faecal Incont 0.8% 1.5%
Back Pain 11.3% 12.2%
No Difference
CAESAREAN VAGINAL
PND 10.1% 10.8%
Dyspareunia 17% 18.7%
Neonatal MORT 0.1% 0.1%
ICH 0.04% 0.03%
Br Plexus Injury Overall----------- 0.05%
CPalsy Overall----------- 0.02%
Potrebbero piacerti anche
- Cesarean Section: Associate Professor Ph.D. E.A. EinyshDocumento33 pagineCesarean Section: Associate Professor Ph.D. E.A. EinyshPrerit Aggarwal100% (1)
- Placenta IsuogDocumento40 paginePlacenta IsuogKARINA BASTIDAS IBARRA100% (1)
- Absolute Obstetric Anesthesia Review: The Complete Study Guide for Certification and RecertificationDa EverandAbsolute Obstetric Anesthesia Review: The Complete Study Guide for Certification and RecertificationNessuna valutazione finora
- Cervical DystociaDocumento22 pagineCervical DystociaBaldau TiwariNessuna valutazione finora
- Ectopic Pregnancy ADocumento37 pagineEctopic Pregnancy AJervhen Sky Adolfo Dalisan100% (1)
- Vbac FinDocumento15 pagineVbac FinCindy AgustinNessuna valutazione finora
- Antepartum HemorrhageDocumento48 pagineAntepartum HemorrhageJoshua EvansNessuna valutazione finora
- C-S & VbacDocumento54 pagineC-S & VbacDagnachew kasayeNessuna valutazione finora
- Ectopic PregDocumento6 pagineEctopic PregYwagar Ywagar0% (1)
- Vaginal Birth After Caesarean (Vbac) : Max Brinsmead MB Bs PHD December 2015Documento36 pagineVaginal Birth After Caesarean (Vbac) : Max Brinsmead MB Bs PHD December 2015kikyNessuna valutazione finora
- Final Thesis Copy - Gonzales, ADocumento114 pagineFinal Thesis Copy - Gonzales, ADONNABELLE ALIWALAS100% (1)
- Sectio CaesareaDocumento13 pagineSectio CaesareaDavid ZamrilNessuna valutazione finora
- CPG Intrapartum and Immediate Postpartum Care PDFDocumento52 pagineCPG Intrapartum and Immediate Postpartum Care PDFAngela SaldajenoNessuna valutazione finora
- Cesarean SectionDocumento42 pagineCesarean SectionP Kasikrishnaraja100% (1)
- Maternal and Child Health Nursing TestDocumento21 pagineMaternal and Child Health Nursing TestAt Day's Ward50% (2)
- Trial of ScarDocumento12 pagineTrial of Scarnyangara50% (2)
- High Risk Pregnancy NewDocumento16 pagineHigh Risk Pregnancy NewSurya SasidharanNessuna valutazione finora
- Feto Pelvic DisproportionDocumento10 pagineFeto Pelvic DisproportionIsrael WoseneNessuna valutazione finora
- Managing Women With Previous CS2Documento27 pagineManaging Women With Previous CS2zynal20038222Nessuna valutazione finora
- L1 Vbac PDFDocumento16 pagineL1 Vbac PDFMuhammad HaziqNessuna valutazione finora
- Cesarean Delivery - 090818183733Documento27 pagineCesarean Delivery - 090818183733Yared TJNessuna valutazione finora
- Materi VBAC Lovamil 202Documento30 pagineMateri VBAC Lovamil 202Zoeva VirdiniaNessuna valutazione finora
- Cesarean Section HennawyDocumento89 pagineCesarean Section Hennawykhadzx100% (2)
- Breech Presentation and Delivery AlarmDocumento43 pagineBreech Presentation and Delivery AlarmAshley Chloé UyNessuna valutazione finora
- Vbac - YurDocumento20 pagineVbac - YurkikiNessuna valutazione finora
- Acute AbdomenDocumento71 pagineAcute AbdomenariNessuna valutazione finora
- Malpresentation: Presented By: Dr. Nico Poundra Mulia Moderator: Dr. Fatmah Oktaviani, SpogDocumento28 pagineMalpresentation: Presented By: Dr. Nico Poundra Mulia Moderator: Dr. Fatmah Oktaviani, SpogaispoundraNessuna valutazione finora
- Vaginal Birth After Caesarean Section (Vbac)Documento16 pagineVaginal Birth After Caesarean Section (Vbac)api-370504650% (2)
- Preterm LaborDocumento29 paginePreterm LaborBer AnneNessuna valutazione finora
- Cervical Ripening & Induction of Labour: Obstetric Guideline 1Documento10 pagineCervical Ripening & Induction of Labour: Obstetric Guideline 1Maizura Syahirah MohtadaNessuna valutazione finora
- Caesarean Delivery: Basliel E M.DDocumento13 pagineCaesarean Delivery: Basliel E M.DAsteway MesfinNessuna valutazione finora
- Normal Pregnancy, Caesarean Section and Breech PresentationDocumento8 pagineNormal Pregnancy, Caesarean Section and Breech PresentationAmisha VastaniNessuna valutazione finora
- First Trimester BleedingDocumento48 pagineFirst Trimester BleedingEliana ArshidNessuna valutazione finora
- Case# 5 Obstetrical Hemorrhage Placental AbnormalitiesDocumento64 pagineCase# 5 Obstetrical Hemorrhage Placental Abnormalitiesrona liza faustinoNessuna valutazione finora
- Kehamilan Dengan Bekas Sectio Cecar: Disusun Oleh: Heru Maranata Nababan Pembimbing: Dr. Dr. Donel S, Spog (K)Documento36 pagineKehamilan Dengan Bekas Sectio Cecar: Disusun Oleh: Heru Maranata Nababan Pembimbing: Dr. Dr. Donel S, Spog (K)Heru Maranata Nababan100% (1)
- Ectopic Pregnancy BWDocumento28 pagineEctopic Pregnancy BWZiya AkhtarNessuna valutazione finora
- EctopicDocumento42 pagineEctopicSafana NazeerNessuna valutazione finora
- C-Obs 38 Planned Vaginal Birth After C-Section New Jul 10Documento7 pagineC-Obs 38 Planned Vaginal Birth After C-Section New Jul 10Aris SugiatnoNessuna valutazione finora
- Abortion, Anc, and CS: Focus+ Lecture SeriesDocumento24 pagineAbortion, Anc, and CS: Focus+ Lecture SeriesTianah davisNessuna valutazione finora
- Third Trimester Bleeding and ManagementDocumento43 pagineThird Trimester Bleeding and ManagementAndrada CatrinoiuNessuna valutazione finora
- 3&4 MiscarraigeDocumento90 pagine3&4 MiscarraigeAbdullah GadNessuna valutazione finora
- By Dr. Malleswar Rao Kasina, MD, Dgo. Hod & CSS, Dept. of Gynobs, Esi Hospital, Sanathnagar, Hyderabad, Ap, IndiaDocumento102 pagineBy Dr. Malleswar Rao Kasina, MD, Dgo. Hod & CSS, Dept. of Gynobs, Esi Hospital, Sanathnagar, Hyderabad, Ap, IndiaHerry SasukeNessuna valutazione finora
- Antepartum & Postpartum Hemorrhage (APH &PPH) : Basim Abu-RafeaDocumento81 pagineAntepartum & Postpartum Hemorrhage (APH &PPH) : Basim Abu-RafeaSheilla ElfiraNessuna valutazione finora
- Third Trimester Bleeding 12Documento34 pagineThird Trimester Bleeding 12rayankemo31Nessuna valutazione finora
- CESAREAN SECTION BmsDocumento25 pagineCESAREAN SECTION BmsAhemigisha JamesNessuna valutazione finora
- Vaginal Birth After Cesarean Delivery (VBAC) Definition/AbbreviationDocumento3 pagineVaginal Birth After Cesarean Delivery (VBAC) Definition/AbbreviationCalvin TranNessuna valutazione finora
- AbortionDocumento30 pagineAbortionKIYANessuna valutazione finora
- Ob Procedures & Instruments - 2022-23 PDFDocumento48 pagineOb Procedures & Instruments - 2022-23 PDFZayNessuna valutazione finora
- 1091223產科晨會報告ver3Documento58 pagine1091223產科晨會報告ver3peipeipoorNessuna valutazione finora
- Antenatal CounsellingDocumento56 pagineAntenatal CounsellingDr. Prashant JainNessuna valutazione finora
- Normal Vaginal Delivery After One Lower Segment Caesarean Section Can Be Safe Option For Many Women But Not Right Choice For AllDocumento6 pagineNormal Vaginal Delivery After One Lower Segment Caesarean Section Can Be Safe Option For Many Women But Not Right Choice For AllRussel Cauton de JesusNessuna valutazione finora
- OBGYN Roisin Doubly UpdatedDocumento71 pagineOBGYN Roisin Doubly UpdatedDanny SchNessuna valutazione finora
- Student Unit 2 Topic 2.5 Jan 2018 TAYLORDocumento42 pagineStudent Unit 2 Topic 2.5 Jan 2018 TAYLORKrista KloseNessuna valutazione finora
- 06 SC AlarmDocumento34 pagine06 SC AlarmYosie Yulanda PutraNessuna valutazione finora
- Endometrial Case Presentation DoneDocumento24 pagineEndometrial Case Presentation Doneapi-278043011Nessuna valutazione finora
- Operatif DeliveryDocumento13 pagineOperatif DeliveryPepo AryabarjaNessuna valutazione finora
- Cesarean SectionDocumento110 pagineCesarean SectionyordiNessuna valutazione finora
- Post Date PregnancyDocumento18 paginePost Date Pregnancyscribdnotes123Nessuna valutazione finora
- Pre Term and Post Term Pregnancy ComplicationsDocumento8 paginePre Term and Post Term Pregnancy ComplicationsAbu YousufNessuna valutazione finora
- ATLS in WomanDocumento37 pagineATLS in WomanLukKaew Dhatchai CharoensilawathNessuna valutazione finora
- VBAC WebDocumento2 pagineVBAC WebNugroho AkbarNessuna valutazione finora
- Pregnancy Series I: All You Need to Know About Antenatal CareDa EverandPregnancy Series I: All You Need to Know About Antenatal CareNessuna valutazione finora
- Treatment Strategy for Unexplained Infertility and Recurrent MiscarriageDa EverandTreatment Strategy for Unexplained Infertility and Recurrent MiscarriageKeiji KurodaNessuna valutazione finora
- Lower Genital Tract Precancer: Colposcopy, Pathology and TreatmentDa EverandLower Genital Tract Precancer: Colposcopy, Pathology and TreatmentNessuna valutazione finora
- Nutrition For Late Preterm Babies What Should We Know.Documento25 pagineNutrition For Late Preterm Babies What Should We Know.IKA UNAIRNessuna valutazione finora
- Situation Analysis of Community Midwives ' Training in SindhDocumento107 pagineSituation Analysis of Community Midwives ' Training in Sindhmidwifepak100% (1)
- Gestational Diabetes - On Broadening The DiagnosisDocumento2 pagineGestational Diabetes - On Broadening The DiagnosisWillians ReyesNessuna valutazione finora
- Breast Feeding FactsDocumento4 pagineBreast Feeding FactsJennifer VelascoNessuna valutazione finora
- Feto-Maternal Outcome of Ante-Natal Care Patients With Cord Around The Neck Finding in Term PregnancyDocumento5 pagineFeto-Maternal Outcome of Ante-Natal Care Patients With Cord Around The Neck Finding in Term PregnancyIJAR JOURNALNessuna valutazione finora
- Add 7 Days To The First Day of Last Menstrual PeriodDocumento16 pagineAdd 7 Days To The First Day of Last Menstrual PeriodRojean MartinezNessuna valutazione finora
- SKRIPSI CINDY SARI AGUSTIN TGL 27 Fix 1Documento119 pagineSKRIPSI CINDY SARI AGUSTIN TGL 27 Fix 1cindy agustinNessuna valutazione finora
- Bahan Utk VCDocumento58 pagineBahan Utk VCTias DiahNessuna valutazione finora
- Pengaruh Inisiasi Menyusu Dini Terhadap Waktu Pengeluaran Dan Perubahan Warna Mekonium Serta Kejadian Ikterik FisiologisDocumento8 paginePengaruh Inisiasi Menyusu Dini Terhadap Waktu Pengeluaran Dan Perubahan Warna Mekonium Serta Kejadian Ikterik FisiologisYESI NURMALA SARI SIANIPAR 1901015Nessuna valutazione finora
- Placenta Previa - MedscapeDocumento5 paginePlacenta Previa - MedscapeAnonymous jh87ryNessuna valutazione finora
- Clinic SchedDocumento3 pagineClinic SchedMyra MalabaguioNessuna valutazione finora
- Jurnal MaternitasDocumento11 pagineJurnal MaternitasamandyaNessuna valutazione finora
- Transverse LieDocumento32 pagineTransverse LieBharat ThapaNessuna valutazione finora
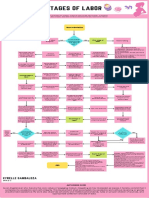
- Stages of Labor FlowchartDocumento1 paginaStages of Labor FlowchartXyrelle GambalozaNessuna valutazione finora
- Telegram Cloud Document 5 6274073709007339605Documento6 pagineTelegram Cloud Document 5 6274073709007339605IlhamNessuna valutazione finora
- Teenage PregnancyDocumento3 pagineTeenage PregnancyJhon Pol CailaoNessuna valutazione finora
- Identifying Client at RiskDocumento22 pagineIdentifying Client at RiskRon Ar IcaNessuna valutazione finora
- 3rd TrimesterDocumento37 pagine3rd TrimesterAparna MohanNessuna valutazione finora
- WHO Systematic Review of Maternal Mortality and Morbidity: The Prevalence of Uterine RuptureDocumento8 pagineWHO Systematic Review of Maternal Mortality and Morbidity: The Prevalence of Uterine RuptureThomas TombusNessuna valutazione finora
- TARIF BaruDocumento4 pagineTARIF Baruepelina hutagaolNessuna valutazione finora
- References For The Clinician - S Breastfeeding Triage Tool PDFDocumento19 pagineReferences For The Clinician - S Breastfeeding Triage Tool PDFValentina Rivas RamosNessuna valutazione finora
- Jadwal Pit (Fetomaternal Room)Documento3 pagineJadwal Pit (Fetomaternal Room)Dwi Adi NugrohoNessuna valutazione finora
- Breast Care and Assisting in BreastfeedingDocumento7 pagineBreast Care and Assisting in BreastfeedingBJ FernandezNessuna valutazione finora
- Treatment of Maternal Hypergalactia: Invited ReviewDocumento3 pagineTreatment of Maternal Hypergalactia: Invited ReviewMaria ChristodoulouNessuna valutazione finora
- MPDSR Training Workbook 17.10.30Documento29 pagineMPDSR Training Workbook 17.10.30Ebsa MohammedNessuna valutazione finora