Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
NCP On Dengue Risk For Bleeding
Caricato da
Cazze Sunio100%(4)Il 100% ha trovato utile questo documento (4 voti)
6K visualizzazioni13 pagineMaternity Case presentation
Titolo originale
NCP on Dengue Risk for Bleeding
Copyright
© © All Rights Reserved
Formati disponibili
PPTX, PDF, TXT o leggi online da Scribd
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoMaternity Case presentation
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato PPTX, PDF, TXT o leggi online su Scribd
100%(4)Il 100% ha trovato utile questo documento (4 voti)
6K visualizzazioni13 pagineNCP On Dengue Risk For Bleeding
Caricato da
Cazze SunioMaternity Case presentation
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato PPTX, PDF, TXT o leggi online su Scribd
Sei sulla pagina 1di 13
Nursing Care Plan
On Risk for Bleeding
By: Cazze Lynn Sunio
BSN 2B
Name of Patient : R.C.
Age/Sex : 20/Female
Rm. Bed # : DR4-3
Reason For Admission: Fever and Rashes
Attending Physicians: Dr. Garado, Dr. Arao, Dr.
Nazareno
Diagnosis: G-1, AOG: 29 1/7
Date and Time: August 20, 2014 @ 9 am
CUES:
Subjective: Miss paki-tawag daw si Doc. Akung
kugmo lagi kay puro dugo.
Objective:
withCC of fever and rashes.
With associate headache andjoint pain.
With pink palpebral conjunctiva.
With (+) loss of appetite.
With observed weakness / restlessness
With observed flushing of face, cheeks and lips.
With hemoglobin count of 104 (normal: 120-
160)
With WBC count of 18.1 (normal: 5.0-10.0)
With platelet count of 17
With (+) Uterine contractions every 15 mins.
With VS of:
T=35.8 degree celcius
CR=107 bpm
PR=100 bpm
RR=33 bpm
BP=90/70 mmhg
FHT=126 bpm
Need:
Health Perception-Health Management Pattern
Nursing Diagnosis:
Injury, risk for bleeding r/t altered clotting
factor aeb decreased platelet and hemoglobin
count secondary to dengue hemmorhagic fever.
R: this disease is manifested by a sudden onset
of fever, headache, joint/muscle pain, nausea
and vommiting and decreased in appetite.
Rashes and ecchymosis can be seen in the acute
phase. There may also be gastritis and bleeding
because of altered clotting factors due to low
platelet count (thrombocypenia) that may lead
to worsening cases of DHF.
Objective of Care:
After 6 hrs. of nursing interventions, the pt. will
be able to demonstrate behaviors that reduces
the risk for bleeding aeb:
a. Gaining good appetite
b. Increase in fluid intake
c. Avoidane of dark colored foods/fluids and
eating food rich in vit. C
d. Eradication of weakness/restlessness
Nursing Interventions:
1. Establish rapport and good working condition
with the patient. R: to gain patients trust and
cooperation.
2. Assess for signs and symptoms of G.I. bleeding
/nosebleeding. Note for color of stool,
vomitus and urine. R: the G.I. track (esophagus
& rectum) is the most usual source of bleeding
due to its mucosal fragility.
3. Observe for presence of petechiae, ecchymosis,
bleeding from one or more sites. R: Sub-acute
disseminated intravascular coagulation (DIC) may
develop sec. to altered clotting factors.
4. Monitor VS especially Pulse and BP. R: an increase
in pulse with decreased blood pressure can indicate
loss of circulating blood volume.
5. Encourage use of soft toothbrush, avoid straining for
stool, and forceful nose blowing. R: in the presence of
clotting factor disturbances, minimal trauma can cause
mucosal bleeding.
6. Avoid dark colored foods/fluids. R: dark colored
foods/fluids may mask bleeding.
7. Encourage patient to eat food rich in vit. C. R: to boost
body resistance to infections that may lead to further
complications.
8. Encourage the patient to rest more. R: rest promotes
body recovery from aches and pains.
9. Increase in fluid intake as indicated. R: body needs 3-
3.5L of water daily as the body has sensible & insensible
water losses. More water intake surely aids in the
recovery of the patient and prevents dehydration.
10. Monitor Hb, Hct, WBC and platelet count every 12
hrs. R: These are indicators of anemia, active
bleeding/impending complications.
Evaluation:
August 20, 2014@3pm.
Goal partially met. After 6 hrs. of nursing interventions,
the patient was able to demonstrate behavior that
reduced the risk for bleeding aeb:
a. The patient was still observed to have loss of
appetite.
b. The patients total fluid intake @ the end of the shift
is 1,260 cc
c. The patient only eats rice & soup, only drinks water
and apple juice.
d. The patient was able to rest/sleep.
Potrebbero piacerti anche
- Dengue NCP (Risk For Bleeding)Documento5 pagineDengue NCP (Risk For Bleeding)Bernadette Malamug50% (6)
- Planning (Nursing Care Plans)Documento10 paginePlanning (Nursing Care Plans)Kier Jucar de GuzmanNessuna valutazione finora
- NCP - Fluid RetentionDocumento3 pagineNCP - Fluid RetentionMichelle Teodoro100% (1)
- DengueDocumento14 pagineDengueKarenn Joy Concepcion OctubreNessuna valutazione finora
- Risk For Fluid Volume Deficit For DengueDocumento3 pagineRisk For Fluid Volume Deficit For DengueRose Cua33% (3)
- 3 Nursing Care Plans For Dengue Hemorrhagic FeverDocumento8 pagine3 Nursing Care Plans For Dengue Hemorrhagic FeverCarren Wingwash100% (3)
- Nursing Care Plan For RabiesDocumento1 paginaNursing Care Plan For RabiesAngel VillamorNessuna valutazione finora
- NCP DengueDocumento3 pagineNCP DengueYeana Alon50% (4)
- NCP Ineffective TissueDocumento2 pagineNCP Ineffective TissueFhel AragonNessuna valutazione finora
- NCP DengueDocumento3 pagineNCP DengueRichmund Earl Geron100% (1)
- NCP DengueDocumento4 pagineNCP DengueJanna Carrel Isabedra Rodio100% (2)
- Dengue Hemorrhagic Fever PathophysiologyDocumento4 pagineDengue Hemorrhagic Fever Pathophysiologyteddydeclines1483% (18)
- Nursing Care Plan For Dengue Hemmorrhagic FeverDocumento6 pagineNursing Care Plan For Dengue Hemmorrhagic FeverMean Elepaño100% (1)
- Dengue NCPDocumento3 pagineDengue NCPnj_pink08179456% (9)
- Dengue Fever Nursing Care Plan-High Risk For Fluid Volume DeficitDocumento1 paginaDengue Fever Nursing Care Plan-High Risk For Fluid Volume Deficitemman_abz100% (5)
- NCP Risk For Bleeding Related To Decreased Platelet CountDocumento2 pagineNCP Risk For Bleeding Related To Decreased Platelet CountKC Ignacio83% (23)
- Ncp-Ineffective Tissue Perfusion (Aortic Stenosis)Documento2 pagineNcp-Ineffective Tissue Perfusion (Aortic Stenosis)Daniel Vergara Arce67% (3)
- NCP - Altered Tissue PerfusionDocumento2 pagineNCP - Altered Tissue PerfusionLeigh Kristel Andrion0% (1)
- Ineffective Tissue PerfusionDocumento2 pagineIneffective Tissue PerfusionClaidelyn De Leyola100% (1)
- Dengue Hemorrhagic Fever Pathophysiology DiagramDocumento4 pagineDengue Hemorrhagic Fever Pathophysiology DiagramGuia Rose Sibayan0% (1)
- Mosegor, Nacl, Nahco 3, Fondaparinux, RamiprilDocumento2 pagineMosegor, Nacl, Nahco 3, Fondaparinux, RamiprilSandrine Barredo100% (2)
- NCP GunshotDocumento13 pagineNCP GunshotMichael John F. Natividad0% (1)
- NCP Near DrowningDocumento1 paginaNCP Near Drowningchristine louise bernardoNessuna valutazione finora
- NCP-Dengue Hemorrhagic FeverDocumento8 pagineNCP-Dengue Hemorrhagic Feverjunrey1990Nessuna valutazione finora
- NCP Risk For BleedingDocumento1 paginaNCP Risk For BleedingJen Garzo75% (4)
- Dengue Discharge PlanDocumento6 pagineDengue Discharge PlanChayliu Bugo75% (4)
- NCP DengueDocumento4 pagineNCP Denguesarzlasco0980% (5)
- NCP For Dengue Hemorrhagic FeverDocumento14 pagineNCP For Dengue Hemorrhagic FeverKim Celeste Matulac100% (3)
- NCP Deficient Fluid Volume Related To Fluid Loss DHNDocumento2 pagineNCP Deficient Fluid Volume Related To Fluid Loss DHNMa. Elaine Carla Tating38% (8)
- Risk For Deficient Fluid Volume - NCPDocumento2 pagineRisk For Deficient Fluid Volume - NCPAyla Mar100% (1)
- NCP in ER Acute Pain RT DengueDocumento1 paginaNCP in ER Acute Pain RT DengueWhoo CaresNessuna valutazione finora
- NCP-risk For BleedingDocumento3 pagineNCP-risk For BleedingAce Dioso Tubasco100% (2)
- Pediatrics Care Plan Kawasaki Disease Final Draft and CorrectedDocumento9 paginePediatrics Care Plan Kawasaki Disease Final Draft and CorrectedValencia Vickers50% (4)
- Ncp-Readiness For Enhanced Knowledge Related To Preoperative CareDocumento1 paginaNcp-Readiness For Enhanced Knowledge Related To Preoperative CareAce Dioso Tubasco50% (2)
- NCP Dengue FeverDocumento3 pagineNCP Dengue Feveralfonselay63% (8)
- Kawasaki Disease NCPDocumento2 pagineKawasaki Disease NCPRay Jhunel Cemine Pascual100% (2)
- NCP Leptospirosis - NewDocumento5 pagineNCP Leptospirosis - Newglaiza_requintoNessuna valutazione finora
- Ineffective Protection NCPDocumento2 pagineIneffective Protection NCPTerry Mae Atilazal Sarcia83% (6)
- Discharge PlanningDocumento5 pagineDischarge PlanningNoora KhalidNessuna valutazione finora
- Risk For BleedingDocumento2 pagineRisk For Bleedingmikebry72% (25)
- Nursing Care Plan Process Analysis Planning and ImplementationDocumento2 pagineNursing Care Plan Process Analysis Planning and ImplementationVanessa Prieto100% (2)
- NCP For DengueDocumento6 pagineNCP For DenguePamela Ann Perez79% (33)
- HCVD NCPDocumento5 pagineHCVD NCPCee Sanchez100% (1)
- Sickle Cell Anemia Nursing Care PlanDocumento6 pagineSickle Cell Anemia Nursing Care PlanArisa Vijungco100% (4)
- NCP DMDocumento21 pagineNCP DMKate ManalastasNessuna valutazione finora
- Nursing Care of The Patient With Dengue HaemorrhagicDocumento19 pagineNursing Care of The Patient With Dengue HaemorrhagicTharu LakshaniNessuna valutazione finora
- Case Presentation YayaDocumento26 pagineCase Presentation Yayayusufharkian100% (1)
- Ugib Case StudyDocumento33 pagineUgib Case StudyRosemarie Cunanan Grifoni100% (1)
- SAMDocumento108 pagineSAMAlimyon Abilar MontoloNessuna valutazione finora
- Weekly Patient Report FormDocumento8 pagineWeekly Patient Report FormOsama FrancisNessuna valutazione finora
- Informatics HYPERLINK Gypsy Kaye PinedaDocumento73 pagineInformatics HYPERLINK Gypsy Kaye PinedaRaquel JavierNessuna valutazione finora
- Drug StudyDocumento17 pagineDrug Studyjlg513Nessuna valutazione finora
- Case StudyDocumento7 pagineCase StudyMicah Jonah ElicañoNessuna valutazione finora
- Exposure To Toxic SubstancesDocumento21 pagineExposure To Toxic SubstancesDavid VillanuevaNessuna valutazione finora
- Medicine Ward NCPDocumento11 pagineMedicine Ward NCPKimsha ConcepcionNessuna valutazione finora
- NCPDocumento14 pagineNCPclaidelynNessuna valutazione finora
- Exposure To Toxic SubstancesDocumento21 pagineExposure To Toxic SubstancesDavid VillanuevaNessuna valutazione finora
- Practice Exam - HematologyDocumento2 paginePractice Exam - HematologyrlinaoNessuna valutazione finora
- Nursing Care PlanDocumento2 pagineNursing Care PlanManena BalagtasNessuna valutazione finora
- PEDIA - TachypneaDocumento12 paginePEDIA - TachypneaAlvin Germo PasuquinNessuna valutazione finora
- Oxygenation - NCPDocumento5 pagineOxygenation - NCPCazze SunioNessuna valutazione finora
- Diabetes Mellitus NCPDocumento5 pagineDiabetes Mellitus NCPCazze SunioNessuna valutazione finora
- NCP Anxiety and PainDocumento12 pagineNCP Anxiety and PainCazze Sunio100% (1)
- NCP Risk For InfectionDocumento6 pagineNCP Risk For InfectionCazze SunioNessuna valutazione finora
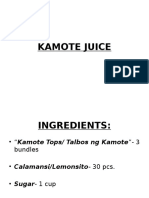
- How To Make Kamote JuiceDocumento6 pagineHow To Make Kamote JuiceCazze SunioNessuna valutazione finora
- NCP Hydrocephalus-Delayed Growth and DevelopmentDocumento4 pagineNCP Hydrocephalus-Delayed Growth and DevelopmentCazze Sunio100% (3)
- Diabetes Mellitus NCPDocumento5 pagineDiabetes Mellitus NCPCazze SunioNessuna valutazione finora
- NCP HydrocephalusDocumento3 pagineNCP HydrocephalusCazze SunioNessuna valutazione finora
- Practice Paper Pre Board Xii Biology 2023-24-1Documento6 paginePractice Paper Pre Board Xii Biology 2023-24-1salamnaseema14Nessuna valutazione finora
- Math 10 Week 3-4Documento2 pagineMath 10 Week 3-4Rustom Torio QuilloyNessuna valutazione finora
- Industrial Automation Using PLCDocumento29 pagineIndustrial Automation Using PLCAditya JagannathanNessuna valutazione finora
- Lords of ChaosDocumento249 pagineLords of ChaosBill Anderson67% (3)
- Poster PresentationDocumento3 paginePoster PresentationNipun RavalNessuna valutazione finora
- Richard IIIDocumento36 pagineRichard IIIXuan Mai Nguyen ThiNessuna valutazione finora
- Good Manufacturing Practices in Postharvest and Minimal Processing of Fruits and VegetablesDocumento40 pagineGood Manufacturing Practices in Postharvest and Minimal Processing of Fruits and Vegetablesmaya janiNessuna valutazione finora
- The Role of IT in TQM L'Oreal Case StudyDocumento9 pagineThe Role of IT in TQM L'Oreal Case StudyUdrea RoxanaNessuna valutazione finora
- R07 SET-1: Code No: 07A6EC04Documento4 pagineR07 SET-1: Code No: 07A6EC04Jithesh VNessuna valutazione finora
- Curry PowderDocumento8 pagineCurry PowderMahendar Vanam100% (1)
- Kalitantra-Shava Sadhana - WikipediaDocumento5 pagineKalitantra-Shava Sadhana - WikipediaGiano BellonaNessuna valutazione finora
- The Path Vol 9 - William JudgeDocumento472 pagineThe Path Vol 9 - William JudgeMark R. JaquaNessuna valutazione finora
- Objective-C Succinctly PDFDocumento110 pagineObjective-C Succinctly PDFTKKNessuna valutazione finora
- Luxi User's GuideDocumento14 pagineLuxi User's GuidephilsouthNessuna valutazione finora
- Temperature Measurement: Temperature Assemblies and Transmitters For The Process IndustryDocumento32 pagineTemperature Measurement: Temperature Assemblies and Transmitters For The Process IndustryfotopredicNessuna valutazione finora
- JurnalDocumento12 pagineJurnalSandy Ronny PurbaNessuna valutazione finora
- Exchange 2010 UnderstandDocumento493 pagineExchange 2010 UnderstandSeKoFieNessuna valutazione finora
- Design of Ka-Band Low Noise Amplifier Using CMOS TechnologyDocumento6 pagineDesign of Ka-Band Low Noise Amplifier Using CMOS TechnologyEditor IJRITCCNessuna valutazione finora
- First Semester-NOTESDocumento182 pagineFirst Semester-NOTESkalpanaNessuna valutazione finora
- Sheridan Specialized Building Products LLC - Queue Solutions Commercial Proposal by SeQure TechnologiesDocumento6 pagineSheridan Specialized Building Products LLC - Queue Solutions Commercial Proposal by SeQure Technologiessailesh psNessuna valutazione finora
- 06.21.2010 - Historic Treasure of Jewish Life and Culture Gifted To UC BerkeleyDocumento2 pagine06.21.2010 - Historic Treasure of Jewish Life and Culture Gifted To UC BerkeleymagnesmuseumNessuna valutazione finora
- A Guide To Funeral Ceremonies and PrayersDocumento26 pagineA Guide To Funeral Ceremonies and PrayersJohn DoeNessuna valutazione finora
- Mod 2 MC - GSM, GPRSDocumento61 pagineMod 2 MC - GSM, GPRSIrene JosephNessuna valutazione finora
- American University of Beirut PSPA 210: Intro. To Political ThoughtDocumento4 pagineAmerican University of Beirut PSPA 210: Intro. To Political Thoughtcharles murrNessuna valutazione finora
- Job Stress InterventionsDocumento5 pagineJob Stress InterventionscocaralucamihaelaNessuna valutazione finora
- Competent Testing Requirements As Per Factory ActDocumento3 pagineCompetent Testing Requirements As Per Factory Actamit_lunia100% (1)
- DCNF Vs Hhs Nov 2020Documento302 pagineDCNF Vs Hhs Nov 2020SY LodhiNessuna valutazione finora
- How To Prepare Adjusting Entries - Step-By-Step (2023)Documento10 pagineHow To Prepare Adjusting Entries - Step-By-Step (2023)Yaseen GhulamNessuna valutazione finora
- Directorate of Indian Medicines & Homoeopathy, Orissa, Bhubaneswar Listof The Homoeopathic Dispensaries BhadrakDocumento1 paginaDirectorate of Indian Medicines & Homoeopathy, Orissa, Bhubaneswar Listof The Homoeopathic Dispensaries Bhadrakbiswajit mathematicsNessuna valutazione finora
- The Elder Scrolls V Skyrim - New Lands Mod TutorialDocumento1.175 pagineThe Elder Scrolls V Skyrim - New Lands Mod TutorialJonx0rNessuna valutazione finora