Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Adult Urethral Disease (Aug 2014)
Caricato da
mvannierCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Adult Urethral Disease (Aug 2014)
Caricato da
mvannierCopyright:
Formati disponibili
Adult Urethral Disease
1
2
Case #1
What is this?
Case #2
Dysuria and occasional hematuria.
Case #3
5
Case #4
Diagnosis?
6
Case #5
Two similar trauma cases. Whats different?
7
Case #6
What is it?
8
Case #7
Diagnosis?
9
Outline
Anatomy
Imaging Modalities
Retrograde
Cystoscopy
CT
US
MR
Trauma
Bladder Urethra
Classification scheme
Strictures
Diverticula
Urethral Stones
Malignancies
Whats not included:
Embryology
Congenital abnormalities other
than PUV
10
Anterior and Posterior Male Urethra
Anterior urethra-
Inferior aspect of the
urogenital diaphragm to
external meatus (14-15 cm)
Bulbar urethra
Pendulous Urethra
Posterior urethra-
Membranous urethra is 1 to
1.5 cm long within urogenital
diaphragm
Prostatic urethra-more
proximally located and
continues to bladder neck
11
Urethral Anatomy
12
Normal CT anatomy
13
Normal CT anatomy (cont)
14
15
Retrograde Urethrography
Technique
Insert 10 to 18 F Foley
catheter with tip at fossa
navicularis (just deep to
external urethral orifice)
without lubricant
Inflate balloon 1-1.5 ml
Patient in supine oblique
position - penis over thigh
with moderate traction
Infuse 20-30 mls contrast
Slow gentle pressure to
overcome spasm of EUS
Indications
Initial study for evaluating
urethral injuries, strictures
and fistulas in males
Often in trauma situation, if
blood visible from meatus,
RUG should be performed
Best to evaluate anterior
urethra
Retrograde Urethrography
Anatomy-
Importance of patient positioning
16
17
Voiding Cystourethrography
(VCUG)
Technique
Fill bladder with contrast
material
Obtain images in a 20-30
degree oblique position
During active voiding,
viewed under fluoroscopy,
bladder neck opens
In males, anterior urethra
not fully distended
Indications
Evaluation of the female
urethra and posterior male
urethra
Evaluation of urinary
complaints secondary to
central or peripheral
neurological disorders
18
Ultrasonography
Technique
Posterior urethra- high
frequency endorectal
probes with patient urinating
Anterior urethra- high
frequency linear probes.
Saline solution injected into
urethra for contrast
Indications
Decreased radiation but
limited view
Some evidence of detection
of spongiofibrosis
19
MR Imaging
Technique
Not currently widely used
Urethra distended with
saline solution through foley
catheter
Use small surface coil with
small FOV
Contrast can be used to
evaluate degree of active
inflammation
Indications
Detection of spongiofibrosis
associated with
inflammatory urethral
stenosis
Evaluation of tunica
albuginea in penile fracture
Normal T2 MR
20
Normal Anatomy
Male urethra
Anterior and posterior portions
Each portion subdivided into 2
parts
Anterior urethra
Penile and bulbar
Posterior urethra
Prostatic and membranous
Posterior
Urethra
Anterior
Urethra
Prostatic
Membranous
Bulbar
Penile
Posterior Urethra
Prostatic Urethra
Extends from bladder neck
through prostate gland and ends
at superior aspect of UG
diaphragm
Longitudinal ridge of smooth
muscle along posterior wall
extends from bladder neck
membranous urethra swells into
a 1 cm mound called the
verumontanum (colliculus)
Continuous with bladder mucosa
and consists of transitional cells
Prostatic
Urethra
Utricle
Ejaculatoy
duct
Opening of
prostatic
ducts
Posterior Urethra
Utricle
Ejaculatoy
duct
Opening of
prostatic
ducts
Passes through UG diaphragm
Narrowest portion of the urethra
Begins at distal end of
verumontanum and ends at tip
of the cone of the bulbous
urethra
Membranous Urethra
Membranous
Urethra
Anterior Urethra
Bulbous Urethra
Begins at inferior aspect of
UG diaphragm and extends
to penoscrotal junction
Has a conical shape
proximally
2 ducts draining Cowpers
glands empty into the
proximal to midbulbous
urethra
Anterior Urethra
Penile Urethra
Extends from penoscrotal
junction to the meatus
Distal 2 cm is dilated
fossa navicularis
Lined by glands of Littre
(as is bulbous urethra)
Kim et al. Seminars in Ultrasound CT and MRI, 28:258-273, 2007.
Urethral Sphincters
Consists of 3 sphincters
Internal sphincter (sm)
Around bladder neck
Primary muscle of passive
continence
Intrinsic sphincter (sm)
Below verumontanum and
surrounding membranous urethra
External sphincter (striated)
Peripheral to extrinsic
Active urinary continence
Urethrographic Technique
External meatus prepared in standard sterile fashion
12 14 Fr Foley catheter (already flushed) inserted
until deflated balloon disappears just beyond meautus
1-2 ml used to inflate balloon within fossa navicularis
Retrograde Urethrography
Technique
Inflation until mild traction does not remove catheter from
urethra
Patient placed in supine 45 oblique position with dependent
hip flexed
Urethra positioned so it projects over soft tissues of the thigh
~20-30 mL of iodinated contrast injected under fluoroscopic
guidance
verumontanum
membranous
urethra
penoscrotal
junction
bulbous urethra
prostatic urethra
penile urethra
Muscular Compressor Nudae
(MCN)
Voiding Cystourethrography
Evaluation of male posterior urethra and female urethra
Bladder filled with contrast via transurethral or suprapubic
catheter
Patient voids under fluoroscopic observation
Voiding Cystourethrogram
Verumontanum
becomes elongated
Membranous
urethra becomes
dilated (still remains
narrowest portion)
Anterior urethra
does not optimally
distend
34
Bladder Trauma
May be a result of blunt, penetrating, or iatrogenic trauma
Up to 85% of patients with pelvic fractures have bladder
injuries
Although 25% of intraperitoneal ruptures occur in absence of
fracture
Degree of distension of bladder with urine determines shape and
injury
Relatively minor trauma may rupture a fully distended bladder, whereas the empty
bladder is seldom injured
10-25% of pts with posterior urethral injury have
associated bladder rupture
Bladder Trauma
ACR Appropriateness Criteria
Bladder Trauma
ACR Appropriateness Criteria
Indications for Imaging
Absolute indication
Blunt trauma Gross hematuria
with association pelvic fracture
Penetrating trauma Any
hematuria
Relative indications
Blunt trauma with:
Gross hematuria without fracture
Pelvic fracture with microhematuria
Isolated microhematuria
Clinical Indicators
Suprapubic pain
Inability to void
Clots in urine
Preexisting bladder disease
Technique
Retrograde cystography
300-400 ml of dilute contrast
instilled into bladder via Foley
Radiographs in AP, oblique,
lateral positions obtained
Postdrainage view obtained
Small amt of contrast can be
hidden behind full bladder (10%
of cases)
CT cystogram
~300 of dilute contrast
instilled into bladder
15 ml of Omnipaque 350
mixed with 500 ml of saline
Postdrainage CT not
required
Assessment of bladder filled
with contrast via excretion is
not adequate to exclude
injury
Bladder Trauma
Consensus Panel of the
International Society of Urology
4 categories of bladder injury
Type 1: Contusion
Type 2: Intraperitoneal Rupture
Type 3: Extraperitoneal Rupture
Type 4: Combined Injury
Bladder Injury
Type 1
Bladder contusion
Partial mucosal tear
Most common injury (not considered a major injury)
Diagnosis of exclusion hematuria in patients with
blunt trauma for which no other cause is found
Bladder Injury
Type 2
Intraperitoneal rupture
(10-20% of major
bladder injuries)
Sudden rise in
intravesicle pressure as
a result of a direct blow
to distended bladder
Weak point is dome,
which ruptures into
peritoneum
Occurs in 25% of
patients without pelvic
fracture
Type 2 injury
Intraperitoneal
contrast
around bowel
loops and
mesenteric
folds and in
paracolic
gutters
Bladder
hematoma
Type 3 Injury
Extraperitoneal Rupture (60% of
major injuries)
Associated with fractures of the
pubic rami or diastasis of the
symphisis
Simple
Confined to pelvic extraperitoneal
space
Complex
Extends beyond perivesical space
to thigh, scrotum, perineum
Type 3 (Simple)
Type 3 (complex)
Type 4
Combined
extraperitoneal and
intraperitoneal
Occurs in ~5% of
ruptures
Management
Type 1
Indwelling urethral catheter
Type 2 (extraperitoneal)
If bony spicule protrudes into bladder, or bladder neck injury
surgery
Indwelling catheter otherwise, repeat cysto in 10d
Type 3 (intraperitoneal)
Usually open surgical repair, suprapubic catheter, repeat cysto in
7-10 d
49
Urethral Trauma
Two Main Mechanisms:
Fractures of the anterior pelvic arch (pubic rami and
symphysis)
Some form of urethral injury occurs in ~5% of males with pelvic
fracture
Usually involves membranous urethra
Straddle injuries
Direct blow to the perineum
Compresses corpus spongiosa and urethra against pubic
symphysis
Usually involves bulbous urethra
Clinical Features
Gross hematuria
Blood at the meatus
Perineal, penile, scrotal hematoma
High-riding prostate on physical exam
ACR Appropriateness Criteria
Classification of Urethral Injuries
Skippage, Patel. Radiographics 2008.
Blunt Urethral Trauma
Generally classified as posterior or anterior
Goldman proposed adaptation of Colapinto and
McCallum classification -system. This
expanded types I-III to I-V to include bladder
base and straddle-type anterior urethral injuries
These injuries classically evaluated by
retrograde urethrography. However, in setting
of trauma, CT often obtained prior to RUG and
some signs important to recognize on CT
54
Classification of urethral traumatic
injuries- Type I
55
Type 1 injury
Stretching or
elongation of an intact
posterior urethra
Mechanism
Puboprostatic
ligament rupture
Hematoma forms and
dislocates bladder
base out of pelvis
Posterior urethra
stretched
Moore et al. Clinically
Oriented Anatomy
2009.
Type I injury on CT
57
Type I injury on CT
58
Elevation of the prostatic apex
above the UGD
At the level of the UGD - no prostatic apex,
hematoma
CT image 2 cm cranial,
prostate with hematoma
Classification of urethral traumatic
injuries (cont) Type II
Type II- Membranous
urethra torn above
an intact UGD (15%)
59
Type II injury
60
Type 2 Injury
Normal cone of
the bulbous
urethra
Contrast flows through prostatic urethra, incomplete tear
No contrast flows into bladder, complete tear
Type 2 Injury
Partial or complete tear of membranous urethra above the
UG diaphragm
Intact UG diaphragm prevents contrast from extending into
perineum
~15% of urethral injuries as a result of pelvic fracture
Type II injury
63
Type II injury
64
RUG shows extravasated contrast,
contrast tracked into the prevesical space
(arrowheads)
Extravasated contrast above the UGD.
Foley balloon is present
Classification of urethral traumatic
injuries- Type III
Type III (Most Common)-
Membranous urethra ruptured
and urogenital diaphragm
lacerated causing extension of
injury into proximal bulbous
urethra
Type II and III may result in
pie in the sky bladder on
excretory urography
Both Type II and III can result
in incontinence because of
damage to external sphincter
65
Pie In the Sky Bladder
66
Type III 2 examples
67
Type III 2 examples
68
Contrast material extends below UGD
and surrounds proximal bulbous urethra
Axial CT shows contrast extrav
below UGD
Distortion of the UGD fat plane CT
69
Distortion of the UGD fat plane CT
70
Distortion of the UGD fat plane
is associated with urethral injury
Type II urethral injury
disrupted L fat plane,
normal R fat plane
Normal fat planes are
preserved bilaterally
Preservation of fat plane
Despite fracture of
superior pelvic rami,
maintenance of
normal fat planes
surrounding the
prostate
Subsequent
retrograde
urethrogram was
normal
71
Type 3 injury
Most common form
Type 2 injury (torn membranous portion) with extension into
proximal bulbous urethra
Combined anterior/posterior injury
Contrast extends below UG diaphragm into perineum
Partial Complete
Compare with type 2 (normal
cone of the bulbous urethra)
Type 4
Injury of the bladder base
extending into the neck
and proximal urethra
May lead to incontinence
as it involves primary
continence mechanism
(internal urethral
sphincter)
Type 4A resembles type
4 radiographically,
actually are base of
bladder injuries that do
not extend into proximal
urethra
Normal
Type 4
Type 4A
Classification of urethral traumatic
injuries (cont)
Type IV
76
Type IV involves base of bladder and bladder neck, with extraperitoneal
contrast extrav, pear shaped bladder d/t perivesical hematoma
and extrav at bladder neck (arrow)
Classification of urethral traumatic
injuries (cont)
Type IVa
77
Extraperitoneal extrav extends from
elevated bladder base.
Cant distinguish this from type IV
Type 5 Injury
Occurs as a result of
straddle injury
Most commonly
occurs when a male
patient falls astride a
hard object such as
the crossbar of a
bicycleor the edge
of a manhole cover
Pure anterior urethra
injury
Classification of urethral traumatic
injuries (cont)
Type V
79
Clinical Management
Generally 2 schools of thought
Primary vs. delayed repair
Delayed repair
Suprapubic catheter inserted for drainage
Stricture 100% of the time
Urethroplasty ~3 mos later
Primary repair
Higher incidence of impotence, incontinence, and
recurrent stricture
Newer techniques minimize damage to neurovascular
bundle and the internal urethra sphincter
Penetrating Urethral Injuries
Generally occur to
anterior urethra
Urethrography
indicated for penile
injury as 50% have
urethral injury
84
Rupture of the corpus
cavernosum
(penile fracture)
Rupture of CC during
injury to erect penis
Associated with
urethral injury in 38%
MRI often obtained to
evaluate cavernosum
Cavernosography can
identify tunica
albunigea tear
85
86
Strictures
Urethral stricture
Refers to anterior urethral scarring
process involving corpus spongiosum
(spongiofibrosis)
Can be secondary to:
Inflammation
Trauma
Iatrogenic
Congenital
Posterior stricture
Usually a result of distraction injury or
post-surgical (TURP or prostatectomy)
Inflammatory Strictures
Gonococcal Stricture
Decreasing prevalence secondary to early
antibiotic treatment
Mechanism
Ascends urethra, infects mucosal cells and submucosal
glands of Littre
Cells desquamate and slough, granulation tissue
develops, scarring occurs
Occurs most often in bulbous urethra secondary to less
effective urinary flushing/high number of glands of Littre
Normal
Glands of Littre
Cowpers Duct
Glands of Littre
Cowpers Duct
s = stricture
cb = cone of the
bulbar urethra
mu = membranous urethra
v = verumontanum
Proximal
bulbar
stricture
Stricture
Cone of the bulbous
urethra
Scarring can extend proximally and distally, producing
softer scars (not as much hard fibrous tissue)
Distorted
cone of
bulbous
urethra from
soft scar
Postvoid
dilation
of soft
scar
Pseudodiverticula
from periurethral
abscess
Reflux into the
prostate gland
Reflux into the
ejaculatory ducts
Glands of Littre opacified
Periurethral
abscess
Tuberculosis and Schistosomiasis
In TB, urethral involvement is
rare.
Generally, stricturing is followed
by periurethral abscess
Anterior urethral stricture
associated with
prostatocutaneous and
urethrocutaneous fistulae and
blind ending sinus tracts
Schistosomiasis has similar
appearance, except fistulae
precede stricture formation
Contrast
entering
urethra
Iatrogenic
Injury
Usually results from
pressure necrosis/scar
formation at 2 main sites
Penoscrotal junction
Membranous urethra
Most commonly from
transurethral resection of
prostate (TURP)
Stricture at
penoscrotal
junction
Tight stricture of
bulbous urethra at
junction with
membranous
urethra
Iatrogenic stricture
Indwelling catheters
Long-term indwelling
catheters cause diffuse
urethritis
Infection spreads across
urethra and involves glands
of Littre
Long irregular stricture, with
visualization of glands on
urethrography
Markedly narrowed penile and
distal bulbous urethra
Urethral Strictures
Can be classified either by etiology or position
Etiology:
Post-Infectious
Post-Traumatic
Post-Surgical
Posterior
Usually results at anastomosis after surgery
RUG still exam of choice but may be inaccurate in determining length of
stricture. Therefore VCUG or sonography may be performed
Anterior
Inflammatory- infectious, balantitis xerotica obliterans
Traumatic-straddle injury or post instrumentation
Congenital
97
Posterior Urethral Stenoses
Vesical neck obstructive syndrome
Evident during urination
Etiologies: hypertrophied bladder neck muscle,
hyperplasia paraurethral glands, neurogenic
bladder with detrusor-bladder neck dyssynergia
Post-prostatectomy stenosis
Can occur at bladder neck or along cavity of
prostate
Long narrow stricture in prostatic bed or enlarged
urethra in prostatic bed with stenosis at distal
portion
98
Bladder Neck Obstruction
99
Post-prostatectomy stenosis
100
Post-Traumatic
Stricture
If delayed repair is chosen,
stricture occurs in majority
of cases
Length of stricture depends
on mechanism of trauma
Type 2 strictures are usually
very short because torn
ends of membranous urethra
are approximated when
pelvic hematoma is resorbed
Post Type 3
Injury
Anterior Stricture
Post-traumatic/Post surgical
Stenosis where trauma located
Stenosis due to pelvic fracture usually at membranous
urethra
Post Inflammatory
VCUG and RUG performed to evaluate extent before
surgery
VCUG gives dynamic imaging and more easily defines
anatomy proximal to stenosis
Sonography allows evaluation of periurethral spongy
tissue. Also has been reported to be more accurate
for detecting full length of stricture
MR with contrast allows evaluation of active
inflammation (hyperintense on T1)
102
Gonococcal Urethral Stricture
Gonococcal infections ascend, proliferating on
columnar epithelium
Clinically present with purulent urethral discharge
Bulbous urethra most common site of stricture due to
presence of periurethral glands in this region.
However, can progress to membranous urethra,
which can lead to incontinence after surgical
correction
Early antibiotic therapy can control disease. If left
untreated can progress to fibrosis
15% of urethritis progress to stricture
103
Gonococcal Urethral Stricture
104
Cowpers duct
is opacified
Periurethral Abscess
Life threatening sequela
to gonococcal infection
Occurs after Littre gland
becomes obstructed
Infection tracks along
corpus spongiosum,
contained by Bucks
fascia
If no communication with
urethra, MR and CT can
evaluate complications
Treatment requires
debridement
105
Urethral Stenosis- MR and US
106
Sonography
Sonography
with power
doppler
T1 MR
T1 MR with
contrast
30 year old male presented with
dysuria and occasional hematuria.
Cowpers Duct Cyst
Cowpers glands - found in the urogenital diaphragm below the prostate
Drains into the bulbar urethra
Obstruction results in retention cysts
Cowper's gland cysts are probably secondary to trauma or infection
Large cysts can cause urinary obstruction, hematuria or infertility.
Treated by marsupialisation or endoscopic incision.
MRI of the pelvis demonstrated:
- a well defined cystic lesion on T1 and T2 (hyperintense )
- Midline lesion lies in close approximation to the bulbous urethra and
just inferior to the prostate.
110
Female Urethral Diverticula
Thought to be acquired due to inflammation of periurethral
glands abscess communication with urethra
pseudodiverticula. Therefore all contained within
periurethral fascia
1.5% associated with stress urinary incontinence in women
If proximal can have mass effect on bladder (female
prostate)
Clinically presents with 3 Ds- Dysuria, post void dribbling
and dyspareunia
May present with anterior wall mass which, when
compressed will give urethretic discharge
DDx includes vaginal cyst, ectopic ureterocele,
endometrioma and urethral tumor
111
Female Urethral Diverticula-
Detection
Usually diagnosed with VCUG or cross sectional
imaging
VCUG- accuracy of 65%.
Double balloon (positive pressure urethragraphy)
increases sensitivity as it can detect an ostium that does
not preferentially fill during voiding. Can be painful.
Delayed contrast enhanced CT
MR most sensitive. Can use endovaginal or
endorectal coils
Reports of transvaginal sonography- relatively
anechoic area adjacent to urethra
112
Acquired Pseudodiverticula- RUG
113
MR- Diverticula
114
Normal urethra
Urethral diverticulum posterior to
urethra
MR- Diverticula
115
Female Diverticulum
116
Urethral Calculi
Rare - generally migrate from the bladder to
urethra
Primary stones can occur from stasis secondary to
stenosis
Need to be distinguished from intraprostatic
calcifications or phleboliths
Can be evaluated with RUG, sonography
118
Urethral Calculi
119
Urethral Calculi
Passed stones may become lodged at membranous urethra or a urethral
stricture
Primary stone formation may be associated with urethral diverticula
121
Urethral Neoplasms
Transitional cell (15%)
Prostatic urethra
Adenocarcinoma (5%)
Glands of Littre
Cowpers glands
Squamous cell (80%)
Anterior urethra
Urethral Tumors
Transitional cell (15%)
Usually occurs in
prostatic urethra
May occur in isolation or
direct extension from
bladder neck
If occurs in anterior
urethra, may represent
drop metastases or
seeding from
instrumentation
Filling defect in
membranous
urethra
Urethral Tumors
Squamous cell carcinoma
(80%)
Previous urethral stricture in
75% of cases
Any condition that causes
stricture is a predisposing factor
Gonococcal urethritis, prolonged
stricture, trauma
Grossly irregular margins of
existing stricture
Focal stricture in bulbous
urethra with ulcerated mucosa
Scalloped margin to
bulbar stricture
with perineal fistula
Conydloma Acuminata
Viral infection (HPV)
May spread along urethra proximally to reach bladder
Multiple frondlike papillary filling defects in the area of involvement
Malignant degeneration of condyloma to squamous cell has been
reported
Urethral Tumors
Metastatic Disease
Bladder
Drop metastases
Instrumentation
Contiguous spread from
adjacent organs
Prostate
Rectum
Testes
127
Tumors- Male
Malignant-Male
<1% of all urologic cancers
Bulbomembranous (60%) >penile (30%)>prostatic (10%)
Vast majority squamous cell, except prostatic TCC
Associations include urethritis from STDs, >1/2 will have history
of stricture
Anterior better prognosis due to better surgical control
Can be diagnosed from RUG or MR. MR can help to
differentiate in tumor size, involvement of corpora cavernosa
Benign- Very rare
May be epithelial or mesenchymal
Biopsy usually necessary although MR can help to differentiate
128
RUG- Irregular stricture
due to SCCa
T2 MR- Mass in corpus
spongiosum
Tumors- Female
4:1 ratio of female to male, still <0.01% all female
malignancies
Associated with chronic irritation, UTI, urethral
caruncle = granlomatous overgrowth of external
meatus
Usually present with urethral bleeding
Surgical excision treatment of choice for anterior
lesions, tumor involving entire urethra general more
locally aggressive
Diagnosis usually clinical. MR used to evaluate local
invasion
MR findings: hypointense on T1 and hyperintense on
T2. Sagittal T2 most helpful
129
Tumors- Female
130
CT with contrast Sagittal CT same patient
131
Congenital Anomalies
Posterior Urethral Valves
Devastating congenital urethral anomaly that is life threatening in
the neonatal period as well as causing lifelong chronic problems
Campbell-Walsh Urology. 2007
PUV
Normally, the verumontanum continues inferiorly as inferior urethral
crest, which terminates into 2-4 plicae colliculi
Pass downward and end anteriorly, close to midline in membranous
urethra
Macpherson RI et al. Radiographics 1986.
PUV Type 1
3 types
Type 1
Most common
Valve leaflets extending
from distal
verumontanum to
urethral wall
Macpherson RI et al. Radiographics 1986.
PUV Type 2
Type 2
Mucosal folds extending from
verumontanum proximally to
the bladder neck
Rare, likely mucosal
redundancy secondary to
more distal obstruction
Macpherson RI et al. Radiographics 1986.
PUV Type 3
Type 3
Iris like membrane with
central pinhole orifice
Also rare
Macpherson RI et al. Radiographics 1986.
PUV
Clinical features
Most common cause of obstructive symptoms in male infants
Palpable kidneys, bladder, abdominal distention, inability to
void
Occasionally will present in young adults with mild obstruction
and infection
PUV - VCUG
Voiding
cystourethrography
Large capacity
bladder,
trabeculated,
diverticula
VUR
Dilated posterior
urethra with poor
distension of
membranous and
anterior urethra
Can occasionally
see valves
Normal
Trabeculated
bladder
Dilated
posterior
urethra
Thickened
Bladder
Neck
VUR
Diverticula
PUV
Diagnosis usually made on
antenatal ultrasound
Hydroureteronephrosis
Distended bladder with thick
wall
Dilated posterior urethra
Dilated bladder and posterior
urethra called keyhole sign
Thick
bladder
wall
Keyhole
appearance of
dilated
bladder and
posterior
urethra
Campbell-Walsh Urology. 2007
PUV
Management
Immediate urinary catheter drainage from bladder
Following drainage and medical stabilization, valves are ablated
Despite ablation, bladder and renal function usually unstable
throughout life
142
Take Home Points
While RUG is still procedure of choice for detecting
urethral injury after trauma, CT signs such as
distortion or obscuration of the urogenital
diaphragm fat plane are highly associated with
injury
MR is emerging technique for evaluating urethral
disease, especially in female diverticular disease,
stricture and malignancy
143
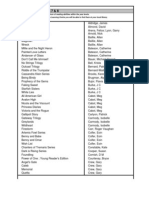
Modalities- Overview
Advantages Limitations Uses
Retrograde
urethrogram
Time proven External structures Urethral injury,
diverticula, stricture
Ultrasound
Non ionizing
Evaluate surrounding
structures, other ddx
Limited experience
in U.S.
Urethral stricture,
female diverticula
MR
Tissue resolution Expense, limits of
coils
Malignancy,
stricture,
CT
Quick, in trauma
situation being done
anyway
Tissue resolution,
for trauma pt
needs to be
voiding
TBD, but can aid
diagnosis in trauma
VCUG
Standard of care
Can only evaluate
within urethra and
bladder
Posterior urethral
injuries/ strictures
144
145
Case #1
What is this?
Seminal vesicle
filled retrograde
through the ejaculatory duct
Case #2
Pie in the Sky Bladder
Dysuria and occasional hematuria.
Case #3
Cowpers duct cyst
148
Case #4
Diagnosis?
Normal
149
Case #5
Two similar trauma cases. Whats different?
Two cases of Type 2 urethral trauma
Partial Complete
150
Case #6
What is it?
Urethral Diverticulum
151
Case #7
Diagnosis?
PUV
Bladder diverticula
Urethral reflux
References
Campbell-Walsh Urology. Edited by A. J. Wein, L. R. Kavoussi, A. C. Novick, A. W. Partin,
and C. A. Peters, 9th ed., 4592. Philadelphia, PA, Saunders-Elsevier, 2007.
Dunnick NR, Sandler CM, Newhouse JH, Amis SE. Textbook of Uroradiology, 4th edition.
Philidelphia PA, Lippincott Williams&Wilkins. 2008.
Kawashima A, Sandler CM, Wasseman NF, LeRoy AJ, King BF, Goldman SM. Imaging of
Urethral Disease: A Pictorial Review. Radiographics October 2004 24:S195-S216.
Kim B, Kawashima A, LeRoy A. Imaging of the Male Urethra. Seminars in Ultrasound CT
and MRI, 28:258-273, 2007.
Moore KL. Dalley AF, Agur AMR. Clinically Oriented Anatomy. 6th edition. Philadelphia PA
Lippincott Williams & Wilkins 2009.
Netter FH. Atlas of Human Anatomy (third ed.), Icon Learning Systems, New Jersey 2003.
Skippage PL. Patel U. Urethral Injuries after Pelvic Trauma: Evaluation with
Urethrography. Radiographics October 2008 28:1631-1643.
Steiner MS. The puboprostatic ligament and the male urethral suspensory mechanism: an
anatomic study. Urology 1994. Oct: 44 (4): 530-4.
Vaccaro JP, Brody J. CT Cystography in the Evaluation of Major Bladder Trauma.
Radiographics September 2000 20:1373-1381.
References -2
Ali, M et al. CT Signs of Urethral Injury. Radiographics 2003; 23:951-966.
Hahn Wy, Israel GM, Lee VS. MRI of female uethral and periurethral
disorders. AJR 2004; 182: 677-682.
Bircan MK, Sahin H, Korkmaz K. Diagnosis of urethral strictures: is
retrograde urethrography still necessary? Int Urol Nephrol 1996; 28: 01-
804.
Pavlica P et al. Imaging of the male urethra. Eur Radiol 2003 13:1583-
1596.
McCallum R. The Adult Male Urethra: Normal Anatomy, Pathology and
Method of Urethrography. Radiologic Clinics of North America. 17: 227-
244
Kawashima A et al. Imaging of Urethral Disease: A Pictorial Review.
Radiographics 2004; 24; S195-S216
Dyer et al. Classic Signs in Uroradiology Radiographics 2004 24:S247-
S280.
Keefe et al. Diverticula of the Female Urethra: Diagnosis by Endovaginal
and Transperineal Sonography. AJR 156:1195-1197, June 1991
153
154
Potrebbero piacerti anche
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- DIQUAD AnalyzerTM - Dentists' Users GuideDocumento2 pagineDIQUAD AnalyzerTM - Dentists' Users GuidemvannierNessuna valutazione finora
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- GE Discovery XR656 PRE-installationDocumento138 pagineGE Discovery XR656 PRE-installationmvannierNessuna valutazione finora
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Fortran IV CDC 6400 Program - Constructing Isometric DiagramsDocumento64 pagineFortran IV CDC 6400 Program - Constructing Isometric DiagramsmvannierNessuna valutazione finora
- Ti 82Documento34 pagineTi 82mvannierNessuna valutazione finora
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- (Bart M. Ter Haar Romeny) Front-End Vision and Multi-Scale Image Analysis - Multi-Scale Computer Vision Theory and Applications (2003)Documento470 pagine(Bart M. Ter Haar Romeny) Front-End Vision and Multi-Scale Image Analysis - Multi-Scale Computer Vision Theory and Applications (2003)mvannierNessuna valutazione finora
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Rotar BriefHistoryofCDC6600 Transcript FinalDocumento12 pagineRotar BriefHistoryofCDC6600 Transcript FinalmvannierNessuna valutazione finora
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Third generationAndWidebandHfRadioCommunications PDFDocumento254 pagineThird generationAndWidebandHfRadioCommunications PDFmvannierNessuna valutazione finora
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- UChicago IRS 990 (2012)Documento178 pagineUChicago IRS 990 (2012)mvannierNessuna valutazione finora
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- US Coast Guard Auxiliary Boat Crew Program Mentor GuideDocumento5 pagineUS Coast Guard Auxiliary Boat Crew Program Mentor GuidemvannierNessuna valutazione finora
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The Air AlmanacDocumento1 paginaThe Air AlmanacmvannierNessuna valutazione finora
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Chicago Area Net Directory (CAND)Documento3 pagineChicago Area Net Directory (CAND)mvannierNessuna valutazione finora
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Antune Build InstructionsDocumento4 pagineAntune Build InstructionsmvannierNessuna valutazione finora
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Health Impact of Electromagnetic Fields - 2005Documento394 pagineHealth Impact of Electromagnetic Fields - 2005mvannierNessuna valutazione finora
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- IARC Monograph On EMF Radiation - No 102Documento480 pagineIARC Monograph On EMF Radiation - No 102mvannierNessuna valutazione finora
- F-15C Eagle SAC - February 1992Documento10 pagineF-15C Eagle SAC - February 1992mvannierNessuna valutazione finora
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- PANDA Electromagnetic Calorimeter (EMC)Documento199 paginePANDA Electromagnetic Calorimeter (EMC)mvannierNessuna valutazione finora
- Akhal-Teke (Horse)Documento11 pagineAkhal-Teke (Horse)Amy KlezanNessuna valutazione finora
- Birds of Van ViharDocumento8 pagineBirds of Van ViharDurgesh Kumar SinghNessuna valutazione finora
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- Wildlife Fact File - Birds - 11-20Documento20 pagineWildlife Fact File - Birds - 11-20ClearMind84Nessuna valutazione finora
- FleshLight Original FREE Stamina Training Unit Manual PDF EbookDocumento9 pagineFleshLight Original FREE Stamina Training Unit Manual PDF Ebookfleshlight100% (1)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- Leo GoatDocumento5 pagineLeo GoatIndre IndraniNessuna valutazione finora
- Examenes Happy CampersDocumento107 pagineExamenes Happy CampersCris MtzNessuna valutazione finora
- The Wardrobe, The White Witch Has Magical Powers That Children Fear. She Can TurnDocumento3 pagineThe Wardrobe, The White Witch Has Magical Powers That Children Fear. She Can Turnxxbbb ddssNessuna valutazione finora
- Graded Reading: Animals in The City (Level 3) - Exercises: PreparationDocumento2 pagineGraded Reading: Animals in The City (Level 3) - Exercises: Preparationestefania aranda jimenezNessuna valutazione finora
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Use Manual: 24k Golden Beauty Bar-Fashion Ideas Originate From JapanDocumento2 pagineUse Manual: 24k Golden Beauty Bar-Fashion Ideas Originate From JapanJayvee MirandaNessuna valutazione finora
- Gruber-Clay - 2016 - Pan ComparisonDocumento14 pagineGruber-Clay - 2016 - Pan ComparisonCarlos González LeónNessuna valutazione finora
- Best Books Years 7Documento7 pagineBest Books Years 7MagelicanNessuna valutazione finora
- The Use and Non-Use of Articles: From The Purdue University Online Writing Lab, Http://owl - English.purdue - EduDocumento2 pagineThe Use and Non-Use of Articles: From The Purdue University Online Writing Lab, Http://owl - English.purdue - EduprasanthaNessuna valutazione finora
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Bird Imagery in Portrait of The Artist As A Young ManDocumento2 pagineBird Imagery in Portrait of The Artist As A Young ManProfadeengleza8Nessuna valutazione finora
- Oasis: by Emily ReichDocumento5 pagineOasis: by Emily ReichcannibithobbalNessuna valutazione finora
- Quarter 4 - CompleteDocumento115 pagineQuarter 4 - Completemaria luisa mendozaNessuna valutazione finora
- SSC MTS Sen ImpDocumento7 pagineSSC MTS Sen ImpNaveen KasiNessuna valutazione finora
- AEOEDocumento900 pagineAEOEDolly BenitezNessuna valutazione finora
- Grade 7 TG SCIENCE 2nd QuarterDocumento60 pagineGrade 7 TG SCIENCE 2nd QuarterAilyn Soria Ecot100% (2)
- Ethical Issues in Conducting SIPDocumento60 pagineEthical Issues in Conducting SIPMavrichk100% (1)
- Case Taking FormatDocumento29 pagineCase Taking FormatmadhukarNessuna valutazione finora
- Fate of The Embryonic Germ LayersDocumento3 pagineFate of The Embryonic Germ Layersmalav1989Nessuna valutazione finora
- 1933 ConventionDocumento4 pagine1933 Conventionapi-301726216Nessuna valutazione finora
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- ITC HS Export Policy 2018 PDFDocumento392 pagineITC HS Export Policy 2018 PDFSachin AhujaNessuna valutazione finora
- Mam Level 2 FlashcardsDocumento38 pagineMam Level 2 FlashcardsAhmedSameh100% (1)
- Zoos, by H. L. Mencken (1918)Documento2 pagineZoos, by H. L. Mencken (1918)Nicolas MartinNessuna valutazione finora
- Caning Dictionary Jun 16Documento36 pagineCaning Dictionary Jun 16Hakki YazganNessuna valutazione finora
- Ineffective Airway ClearanceDocumento1 paginaIneffective Airway Clearancerozj0750% (2)
- Trans-Out Orders: NSVD Admitting Notes Postpartum OrdersDocumento7 pagineTrans-Out Orders: NSVD Admitting Notes Postpartum OrdersDre ValdezNessuna valutazione finora
- Radiological Features of BronchiectasisDocumento24 pagineRadiological Features of BronchiectasisOxana TurcuNessuna valutazione finora
- Describing How Muscles Work Activity SheetDocumento3 pagineDescribing How Muscles Work Activity SheetTasnim MbarkiNessuna valutazione finora