Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
PROBLEM 4A - Varla
Caricato da
varlavarleyDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
PROBLEM 4A - Varla
Caricato da
varlavarleyCopyright:
Formati disponibili
By: Varla S.
G (405090215)
The abrupt (acute) onset of abdominal pain.
A potential medical emergency, an acute
abdomen may reflect a major problem with
one of the organs in the abdomen such as the
appendix (being inflamed =appendicitis), the
gallbladder (inflamed = cholecystitis), the
intestine (an ulcer that has perforated), the
spleen (that has ruptured), etc.
Ileus occurs from hypomotility of the
gastrointestinal tract in the absence of
mechanical bowel obstruction.
Presumably, the muscle of the bowel wall is
transiently impaired and fails to transport
intestinal contents.
This lack of coordinated propulsive action
leads to the accumulation of gas and fluids
within the bowel.
Postoperative ileus
after an open
cholecystectomy.
Ogilvie pseudo-
obstruction in a
septic elderly
patient.
Note the massive
dilatation of the
colon, especially the
right colon and
cecum.
According to some hypotheses, postoperative
ileus is mediated via activation of inhibitory
spinal reflex arcs.
Anatomically, 3 distinct reflexes are involved:
ultrashort reflexes confined to the bowel wall,
short reflexes involving prevertebral ganglia,
and long reflexes involving the spinal cord.
The surgical stress response leads to systemic
generation of endocrine and inflammatory
mediators that also promote the development
of ileus.
Rat models have shown that laparotomy,
eventration, and bowel compression lead to
increased numbers of macrophages, monocytes,
dendritic cells, T cells, natural killer cells, and mast
cells, as demonstrated by immunohistochemistry .
Macrophages residing in the muscularis externa and
mast cells are probably the key players in this
inflammatory cascade
Calcitonin generelated peptide, nitric oxide,
vasoactive intestinal peptide, and substance P
function as inhibitory neurotransmitters in the bowel
nervous system.
Postoperative ileus occurs in approximately
50% of patients who undergo major
abdominal surgery
Patients with ileus typically have vague, mild
abdominal pain and bloating.
They may report nausea, vomiting, and
poor appetite.
Abdominal cramping is usually not present.
Patients may or may not continue to pass
flatus and stool.
The abdomen may be distended and
tympanic, depending on the degree of
abdominal and bowel distention, and may be
tender.
A distinguishing feature is absent or
hypoactive bowel sounds, in contrast to the
high-pitched sound of obstruction.
The silent abdomen of ileus reveals no
discernible peristalsis or succussion splash.
Most cases of ileus occur after intra-abdominal
operations.
Normal resumption of bowel activity after
abdominal surgery follows a predictable pattern:
the small bowel typically regains function within
hours; the stomach regains activity in 1-2 days;
and the colon regains activity in 3-5 days.
Serial abdominal radiographs mapping the
distribution of radiopaque markers have shown
that the colonic gradient for resolution of
postoperative ileus is proximal to distal.
Other causes of adynamic ileus are as follows:
Sepsis
Drugs (eg, opioids, antacids, warfarin, amitriptyline,
chlorpromazine)
Metabolic (eg, low potassium, magnesium, or sodium
levels; anemia; hyposmolality)
Myocardial infarction
Pneumonia
Trauma (eg, fractured ribs, fractured spine)
Biliary colic and renal colic
Head injury and neurosurgical procedures
Intra-abdominal inflammation and peritonitis
Retroperitoneal hematomas
The common differentials for ileus are
pseudo-obstruction, also referred to as
Ogilvie syndrome, and mechanical bowel
obstruction.
Mechanical
bowel
obstruction due
to a left colon
carcinoma.
Note the
paucity of bowel
gas throughout
the colon.
Contrast study, in
the same patient as
in Media File 3,
showing the classic
"apple-core" lesion
of colon carcinoma.
Laboratory studies and blood work should focus
on evaluations for infectious, electrolytic, and
metabolic derangements.
On plain abdominal radiographs, ileus appears
as copious gas dilatation of the small intestine
and colon.
With enteroclysis, the contrast medium in
patients with paralytic ileus should reach the
cecum within 4 hours; if the contrast medium
remains stationary for longer than 4 hours,
mechanical obstruction is suggested
Patients should receive intravenous
hydration.
For patients with vomiting and distention,
use of a nasogastric tube provides
symptomatic relief; however, no studies in
the literature support the use of nasogastric
tubes to facilitate resolution of ileus.
For patients with protracted ileus, mechanical
obstruction must be excluded with contrast
studies.
In one study, the amount of morphine
administered directly correlated with the time
elapsed before the return of bowel sounds and
the passage of flatus and stool.
The use of postoperative narcotics can be
diminished by supplementation with
nonsteroidal anti-inflammatory drugs (NSAIDs).
In addition to permitting lower narcotic doses by
providing pain relief, NSAIDS may improve
ileus by reducing local inflammation.
The clinician must assess the overall status
of the patient and evaluate for adequate
oral intake and good bowel function.
A patient's report of flatus, bowel sounds, or
stool passage may prove misleading;
therefore, clinicians must not rely solely on
self-reporting.
The presence of ileus does not preclude enteral
feeding.
Postpyloric feeding into the small bowel can be
cautiously performed.
Start feeds at one-quarter or one-half strength
at a slow rate and gradually advance.
Having patients chew gum has been advocated
as a means of promoting recovery from
postoperative ileus.
Chewing gum may constitute a form of sham
feeding that stimulates gastrointestinal motility.
Meta-analyses have shown that gum
chewing can reduce the time to first flatus
and passage of feces, and marginally
decrease the length of hospital stay after
intestinal surgery.
Conventional wisdom and wide practice
foster the notion that ambulation stimulates
bowel function and improves postoperative
ileus, although this has not been shown in
the literature.
Postoperative ambulation remains beneficial
in preventing the formation of
atelectasis, deep vein thrombosis, and
pneumonia but has no role in treating ileus.
Studies have shown that combinations of thoracic
epidurals containing bupivacaine alone or in
combination with opioids improve postoperative
ileus.
Continuous intravenous administration of lidocaine
during and after abdominal surgery may decrease
the duration of postoperative ileus.
Peripherally selective opioid antagonists are an
option for the treatment of postoperative ileus.
Methylnaltrexone (Relistor) and alvimopan
(Entereg) are approved by the Food and Drug
Administration
Erythromycin, a motilin receptor agonist,
has been used for postoperative gastric
paresis but has not been shown to be
beneficial for ileus.
Metoclopramide (Reglan), a dopaminergic
antagonist, has antiemetic and prokinetic
activities, but data have shown that the drug
may actually worsen ileus.
Appendicular abscess is the localized
collection of pus in the peri-appendicular area
(right iliac fossa) following appendicitis and
its perforation.
An inflammatory mass occurs either as
phlegmon or abscess in 2% to 6% patients
with appendicitis.
History of pain in right iliac fossa and mass
formation over few days is always present.
Rarely it may present without prolonged history
which may happen in deep and retrocaecal
appendicitis.
The common presenting features are :
Pain
Pain is usually present in the right iliac fossa.
It is not very severe to start with.
It is continuous and gets worse gradually.
The pain becomes throbbing and unbearable as the abscess
formation occurs.
Mass right iliac fossa
There is mass formation in the right iliac fossa which is tender to
touch.
Over lying skin is usually normal.
The local temperature may or may not be raised.
The mass may increase in size and become more painful than
before
Fever
Fever is present in association with other symptoms.
It is continuous and is not responsive to antibiotics.
It has a typical pattern showing progressive rise in the peak of
temperature.
In fact the appendicular abscess is diagnosed with reasonable
certainty when the patient with appendicular mass starts running
high grade temperature regularly.
Tenderness
The mass in the right iliac fossa becomes tender not
only to touch but to respiratory movements as well.
On examination even gentle palpation is very painful.
Paralytic ileus
Mostly these patients are already diagnosed cases of
appendicular mass and are on conservative treatment
when they develop paralytic ileus.
Patients may present with paralytic ileus which may
be due to appendicular abscess.
Patient may present with difficulty in
micturition, frequency of micturition, acute
retention of urine and haematuria.
The symptoms are due to presence of
abscess and inflammatory mass near right
lower ureter and bladder.
Urine examination
It is a simple investigation which helps to exclude the
renal causes of urological symptoms in patients with
appendicular abscess.
Blood examination
Haemoglobin percentage is decreased.
Leukocyte count is raised.
Polymorphonucleo-leukocytosis is present.
Sedimentation rate is raised.
Radiological examination
Plain X-ray of the abdomen.
It may show loops of distended small gut around the
abscess area (sentinel loops)
Ultrasound scan
The differentiation between appendicular mass and abscess is
easily done with the ultrasound scan.
The abdominal ultrasound scan shows a solid mass in the right
iliac fossa as hypo epoic area (fluid collection).
The amount of fluid collection varies with the amount of pus
present.
The shadow of adherent and distended loops of bowel is also
seen.
Percutaneous drainage under ultrasound guidance is
minimally invasive.
CT scan
It can reliably distinguish phlegmonous inflammation from a
liquified abscess.
It can delineate the full extent of such inflammatory mass.
Percutaneous drainage under CT control is safe, effective
and carries low morbidity.
The treatment of appendicular abscess has
following components:
Ultrasound guided drainage of abscess
Emergency surgery
Laparoscopic drainage
Expectant treatment
Delayed surgery
When the appendicular abscess is diagnosed
by sonography.
It can be aspirated with the help of a wide
bore needle under ultrasound control.
It is simple, safe and effective.
It may be repeated if the abscess collects.
In fact, the drainage is a better option than
the aspiration.
It is required when abscess fails to resolve or
recurs.
It is also required when the general condition of
patient deteriorates inspite of conservative
management.
Incision and drainage of the abscess is
performed.
The appendix, its debris or inflammatory mass is
also removed if safely possible at the same
operation, otherwise, it is left for later stage to
be removed as elective operation.
It is less traumatic and less invasive procedure but it should better be avoided as the
risk of spread of infection into the peritoneal cavity is too high.
If the patient is haemodynamically stable, the
patient is observed and treated
symptomatically and conservatively.
It is safe and effective alternative to immediate
surgery.
It is monitored with ultrasound and CT scan .
Initial expectant treatment has following
components:
Fluid and electrolytes
Nil orally
Parenteral antibiotics
Appropriate antibiotics are started as soon
as the condition is diagnosed.
Triple regimen of antibiotics is usually used.
It is a combination of drugs against gram
negative, gram positive and anaerobic
organisms.
Commonly used drugs are amino glycosides,
ampicillin, and metronidazole.
Interval appendicectomy is performed
about six to eight weeks afterwards.
This is performed to prevent recurrent
attacks and will provide definitive diagnosis.
Recently there is growing evidence against
routinely performing interval
appendicectomy as the risk of recurrent
attack is only 14% and most of it occurs in
first three months.
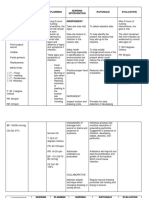
Appendicular mass leading to abscess formation
Parenteral antibiotics
Fluid replacement
Nil orally
Serial ultrasound
No abcess
Abcess
formation
Percutaneous
drainage
Mass resolves
Persistent
recurrent abcess
Delayed surgery
(appendicectomy)
Age >40 years barium
enema colonoscopy
Open drainage surgery
Following complications may be seen in
patients with appendicular abscess:
Peritonitis.
Pelvic abscess.
Subphrenic abscess.
Paralytic ileus.
Adhesion formation.
Intestinal obstruction.
Septicaemia.
Pelvic inflammatory disease is a general term
for infection of the uterus lining, fallopian
tubes, or ovaries.
Most cases of pelvic inflammatory disease are
caused by bacteria that move from the vagina
or cervix into the uterus, fallopian tubes,
ovaries, or pelvis.
The most common cause of PID is sexual contact
without using a condom or other protection.
This is called a sexually transmitted disease
(STD).
Chlamydia and gonorrhea are the two bacteria
that cause most cases of PID.
However, bacteria may also enter the body
during some surgical or office procedures,
such as:
Childbirth
Endometrial biopsy
Insertion of an intrauterine device (IUD)
Miscarriage
Therapeutic or elective abortion
In the United States, nearly 1 million women
develop PID each year.
About 1 in 8 sexually active adolescent girls
will develop PID before age 20.
Male sexual partner with gonorrhea or
chlamydia
Multiple sexual partners
Past history of any sexually transmitted
disease
Past history of PID
Recent insertion of an IUD
Sexual activity during adolescence
The most common symptoms of PID include:
Fever (not always present; may come and go)
Pain or tenderness in the pelvis, lower abdomen, or sometimes the lower back
Vaginal discharge with abnormal color, texture, or smell
Other symptoms that may occur with PID:
Bleeding after intercourse
Chills
Fatigue
Frequent or painful urination
Increased menstrual cramping
Irregular menstrual bleeding or spotting
Lack of appetite
Nausea, with or without vomiting
No menstruation
Painful sexual intercourse
Note: There may be no symptoms. People who experience an ectopic
pregnancy or infertility often have had silent PID, which is usually caused
by chlamydia infection.
You may have a fever and abdominal tenderness.
A pelvic examination may show:
A cervix that bleeds easily
Cervical discharge
Pain with movement of the cervix
Tenderness in the uterus or ovaries
Lab tests that look for signs of infection are:
C-reactive protein (CRP)
Erythrocyte sedimentation rate (ESR)
WBC count
Other tests include:
Culture of your vagina or cervix to look for gonorrhea, chlamydia, or other
causes of PID
Pelvic ultrasound or CT scan to look for other causes of your symptoms, such
as appendicitis or pregnancy, and to look forabscesses or pockets of infection
around the tubes and ovaries
Serum HCG (pregnancy test)
Your doctor will often start you on antibiotics while
waiting for your test results.
If you are diagnosed with milder PID, you will usually be
given an antibiotic injection or shot, and then sent
home with antibiotic pills to take for up to 2 weeks.
More severe cases of PID may require you to stay in the
hospital.
Antibiotics are first given by IV, and then later by mouth.
Sexual partners must be treated to prevent passing the
infection back and forth.
Use condoms until you both have finished taking your
antibiotics.
Complicated cases that do not improve with antibiotics
may need surgery.
PID infections can cause scarring of the pelvic
organs, possibly leading to:
Chronic pelvic pain
Ectopic pregnancy
Infertility
Preventive measures include:
Get prompt treatment for sexually transmitted diseases.
Practice safer sex behaviors. The only absolute way to
prevent an STD is to not have sex (abstinence). Having a
sexual relationship with only one person (monogamous)
can reduce the risk. Use a condom every time you have
sex.
You can reduce the risk of PID by getting regular STD
screening exams. Couples can be tested for STDs before
starting to have sex. Testing can detect STDs that may not
be producing symptoms yet.
All sexually active women ages 20 - 25 and younger should
be screened each year for chlamydia and gonorrhea. All
women with new sexual partners or multiple partners
should also be screened.
Appendicitis is defined as an inflammation of
the inner lining of the vermiform appendix
that spreads to its other parts.
This condition is a common and urgent surgical
illness with protean manifestations, generous
overlap with other clinical syndromes, and
significant morbidity, which increases with
diagnostic delay .
In fact, despite diagnostic and therapeutic
advancement in medicine, appendicitis remains
a clinical emergency and is one of the more
common causes of acute abdominal pain.
The appendix is a wormlike extension of the
cecum and, for this reason, has been called
the vermiform appendix.
The average length of the appendix is 8-10
cm (ranging from 2-20 cm).
The appendix appears during the fifth
month of gestation, and several lymphoid
follicles are scattered in its mucosa.
Such follicles increase in number when
individuals are aged 8-20 years.
PROLIFERASI BAKTERI & SEKRESI MUKUS
YANG BERKELANJUTAN DI LUMEN
APENDIKS, PEMBESARAN FOLIKEL
SUBMUKOSA LIMFOID (AKIBAT INFEKSI
MIKROBA)
TEKANAN
INTRALUMINAL
EDEMA & KONGESTI
VENA dan LIMFATIK
PERFUSI ARTERIAL
YANG DIRUSAK
ISKEMIA PADA
DINDING
APENDIKS
INVASI BAKTERI DENGAN INFILTRAT
INFLAMASI PADA LAMINA DINDING
APENDIKS & NEKROSIS
APENDIKITIS
SEDERHANA
APENDIKITIS
GANGRENOSA
APENDIKITIS
PERFORASI
APENDIKITIS
ABSES
Appendicitis is caused by obstruction of the
appendiceal lumen from a variety of causes.
Obstruction is believed to cause an increase in
pressure within the lumen.
At the same time, intestinal bacteria within the
appendix multiply, leading to the recruitment of
white blood cells and the formation of pus and
subsequent higher intraluminal pressure.
If appendiceal obstruction persists, intraluminal
pressure rises ultimately above that of the
appendiceal veins, leading to venous outflow
obstruction
As a consequence, appendiceal wall ischemia
begins, resulting in a loss of epithelial
integrity and allowing bacterial invasion of
the appendiceal wall.
Within a few hours, this localized condition
may worsen because of thrombosis of the
appendicular artery and veins, leading to
perforation and gangrene of the appendix.
As this process continues, a periappendicular
abscess or peritonitis may occur.
Appendicitis is caused by obstruction of the appendiceal lumen.
The most common causes of luminal obstruction include lymphoid
hyperplasia secondary to inflammatory bowel disease (IBD) or infections
(more common during childhood and in young adults), fecal stasis and
fecaliths (more common in elderly patients), parasites (especially in
Eastern countries), or, more rarely, foreign bodies and neoplasms.
Fecaliths form when calcium salts and fecal debris become layered
around a nidus of inspissated fecal material located within the appendix.
Lymphoid hyperplasia is associated with various inflammatory and
infectious disorders including Crohn disease, gastroenteritis,
amebiasis, respiratory infections, measles, and mononucleosis
Obstruction of the appendiceal lumen has less commonly been
associated with bacteria (Yersinia species, adenovirus, cytomegalovirus,
actinomycosis,Mycobacteria species, Histoplasma species), parasites
(eg, Schistosomesspecies, pinworms, Strongyloides stercoralis), foreign
material (eg, shotgun pellet, intrauterine device, tongue stud, activated
charcoal), tuberculosis, and tumors.
In the United States, 250,000 cases of appendicitis are
reported annually, representing 1 million patient-days
of admission.
The incidence of acute appendicitis has been declining
steadily since the late 1940s, and the current annual
incidence is 10 cases per 100,000 population.
Appendicitis occurs in 7% of the US population, with
an incidence of 1.1 cases per 1000 people per year.
Some familial predisposition exists.
In Asian and African countries, the incidence of
acute appendicitis is probably lower because of the
dietary habits of the inhabitants of these geographic
areas.
There is a slight male preponderance of 3:2 in teenagers
and young adults; in adults, the incidence of appendicitis is
approximately 1.4 times greater in men than in women.
The incidence of primary appendectomy is approximately
equal in both sexes.
The incidence of appendicitis gradually rises from birth,
peaks in the late teen years, and gradually declines in the
geriatric years.
The mean age when appendicitis occurs in the pediatric
population is 6-10 years.
Lymphoid hyperplasia is observed more often among infants
and adults and is responsible for the increased incidence of
appendicitis in these age groups.
Younger children have a higher rate of perforation, with
reported rates of 50-85%.
The median age at appendectomy is 22 years.
Although rare, neonatal and even prenatal appendicitis have
been reported.
Clinicians must maintain a high index of suspicion in all age
groups.
Appendectomy carries a complication rate of 4-15%, as well as
associated costs and the discomfort of hospitalization and surgery.
Delayed diagnosis and treatment account for much of the mortality
and morbidity associated with appendicitis.
The overall mortality rate of 0.2-0.8% is attributable to complications of
the disease rather than to surgical intervention.
The mortality rate in children ranges from 0.1% to 1%; in patients
older than 70 years, the rate rises above 20%, primarily because of
diagnostic and therapeutic delay.
Appendiceal perforation is associated with increased morbidity and
mortality compared with nonperforating appendicitis.
The mortality risk of acute but not gangrenous appendicitis is less
than 0.1%, but the risk rises to 0.6% in gangrenous appendicitis.
The rate of perforation varies from 16% to 40%, with a higher frequency
occurring in younger age groups (40-57%) and in patients older than 50
years (55-70%), in whom misdiagnosis and delayed diagnosis are
common.
Complications occur in 1-5% of patients with appendicitis, and
postoperative wound infections account for almost one third of the
associated morbidity.
The classic history of anorexia and periumbilical pain
followed by nausea, right lower quadrant (RLQ)
pain, and vomiting occurs in only 50% of cases.
Diarrhea or constipation is noted in as many as 18%
of patients and should not be used to discard the
possibility of appendicitis.
The most common symptom of appendicitis
is abdominal pain.
Typically, symptoms begin as periumbilical or
epigastric pain migrating to the right lower
quadrant (RLQ) of the abdomen.
Patients usually lie down, flex their hips, and draw
their knees up to reduce movements and to avoid
worsening their pain.
Usually, a fever is not present at this stage.
The duration of symptoms is less than 48 hours in
approximately 80% of adults but tends to be longer in elderly
persons and in those with perforation.
Approximately 2% of patients report duration of pain in excess of
2 weeks.
A history of similar pain is reported in as many as 23% of cases,
but this history of similar pain, in and of itself, should not be used
to rule out the possibility of appendicitis.
In addition to recording the history of the abdominal pain, obtain
a complete summary of the recent personal history surrounding
gastroenterologic, genitourinary, and pneumologic conditions, as
well as consider gynecologic history in female patients.
An inflamed appendix near the urinary bladder or ureter can
cause irritative voiding symptoms and hematuria or pyuria.
Cystitis in male patients is rare in the absence of instrumentation.
Consider the possibility of an inflamed pelvic appendix in male
patients with apparent cystitis.
Also consider the possibility of appendicitis in pediatric or adult
patients who present with acute urinary retention
Rupture appendix a child will feel pain
in some hours
A small child can not show the pain
location correctly
Vomiting with or without nausea
Fever 38,9
0
C
Do not want to eat
Crying
It is important to remember that the position of the appendix is
variable.
Of 100 patients undergoing 3-dimensional (3-D) multidetector
computed tomography (MDCT) scanning, the base of the
appendix was located at the McBurney point in only 4% of
patients; in 36%, the base was within 3 cm of the point; in 28%, it
was 3-5 cm from that point; and, in 36% of patients, the base of
the appendix was more than 5 cm from the McBurney point.
The most specific physical findings in appendicitis are rebound
tenderness, pain on percussion, rigidity, and guarding.
Rarely, left lower quadrant (LLQ) tenderness has been the major
manifestation in patients with situs inversus or in patients with a
lengthy appendix that extends into the LLQ.
Tenderness on palpation in the RLQ over the McBurney point is
the most important sign in these patients.
In a minority of patients with acute appendicitis, some other signs may
be noted.
However, their absence never should be used to rule out appendiceal
inflammation.
The Rovsing sign (RLQ pain with palpation of the LLQ) suggests
peritoneal irritation in the RLQ precipitated by palpation at a remote
location.
The obturator sign (RLQ pain with internal and external rotation of the
flexed right hip) suggests that the inflamed appendix is located deep in
the right hemipelvis.
The psoas sign (RLQ pain with extension of the right hip or with flexion
of the right hip against resistance) suggests that an inflamed appendix is
located along the course of the right psoas muscle.
The Dunphy sign (sharp pain in the RLQ elicited by a voluntary cough)
may be helpful in making the clinical diagnosis of localized peritonitis.
The Markle sign, pain elicited in a certain area of the abdomen when the
standing patient drops from standing on toes to the heels with a jarring
landing, was studied in 190 patients undergoing appendectomy and
found to have a sensitivity of 74%
There is no evidence in the medical literature
that the digital rectal examination (DRE)
provides useful information in the evaluation
of patients with suspected appendicitis;
however, failure to perform a rectal examination
is frequently cited in successful malpractice
claims.
In 2008, Sedlak et al studied 577 patients who
underwent DRE as part of an evaluation for
suspected appendicitis and found no value as a
means of distinguishing patients with and
without appendicitis
The incidence of appendicitis is unchanged in pregnancy
relative to the general population, but the clinical
presentation is more variable than at other times.
During pregnancy, the appendix migrates in a
counterclockwise direction toward the right kidney, rising
above the iliac crest at about 4.5 months' gestation.
RLQ pain and tenderness dominate in the first
trimester, but in the latter half of pregnancy, right upper
quadrant (RUQ) or right flank pain must be considered a
possible sign of appendiceal inflammation.
Nausea, vomiting, and anorexia are common in
uncomplicated first trimester pregnancies, but their
reappearance later in gestation should be viewed with
suspicion.
In these systems, a finite number of clinical
variables is elicited from the patient and each is
given a numeric value; then, the sum of these
values is used.
The best known of these scoring systems is the
MANTRELS score, which tabulates migration of
pain, anorexia, nausea and/or vomiting,
tenderness in the RLQ, rebound tenderness,
elevated temperature, leukocytosis, and shift to
the left.
Clinical scoring systems are attractive because of their simplicity; however,
none has been shown prospectively to improve on the clinician's judgment
in the subset of patients evaluated in the emergency department (ED) for
abdominal pain suggestive of appendicitis.
The MANTRELS score, in fact, was based on a population of patients
hospitalized for suspected appendicitis, which differs markedly from the
population seen in the ED.
In reviewing the records of 150 ED patients who underwent
abdominopelvic computed tomography (CT) scanning to rule out
appendicitis, McKay and Shepherd suggested that patients with an
MANTRELS score of 0-3 could be discharged without imaging, that
those with scores of 7 or above receive surgical consultation, and those
with scores of 4-6 undergo CT evaluation.
The investigators found that patients with a MANTRELS score of 3 or
lower had a 3.6% incidence of appendicitis, patients with scores of 4-6
had a 32% incidence of appendicitis, and patients with scores of 7-10 had a
78% incidence of appendicitis.
In another study, Schneider et al concluded that the MANTRELS score was
not sufficiently accurate to be used as the sole method for determining
the need for appendectomy in the pediatric population.
These investigators, studied 588 patients aged 3-21 years and found that a
MANTRELS score of 7 or greater had a positive predictive value of 65%
and a negative predictive value of 85%.
Computer-aided diagnosis consists of using retrospective
data of clinical features of patients with appendicitis and
other causes of abdominal pain and then prospectively
assessing the risk of appendicitis.
Computer-aided diagnosis can achieve a sensitivity
greater than 90% while reducing rates of perforation
and negative laparotomy by as much as 50%.
However, the principle disadvantages to this method are
that each institution must generate its own database to
reflect characteristics of its local population, and
specialized equipment and significant initiation time are
required.
In addition, computer-aided diagnosis is not widely
available in US EDs.
The stages of appendicitis can be divided into
early, suppurative, gangrenous, perforated,
phlegmonous, spontaneous resolving,
recurrent, and chronic.
Early stage appendicitis
In the early stage of appendicitis, obstruction of the
appendiceal lumen leads to mucosal edema, mucosal
ulceration, bacterial diapedesis, appendiceal
distention due to accumulated fluid, and increasing
intraluminal pressure.
The visceral afferent nerve fibers are stimulated, and
the patient perceives mild visceral periumbilical or
epigastric pain, which usually lasts 4-6 hours
Suppurative appendicitis
Increasing intraluminal pressures eventually exceed capillary
perfusion pressure, which is associated with obstructed
lymphatic and venous drainage and allows bacterial and
inflammatory fluid invasion of the tense appendiceal wall.
Transmural spread of bacteria causes acute suppurative
appendicitis.
When the inflamed serosa of the appendix comes in contact
with the parietal peritoneum, patients typically experience the
classic shift of pain from the periumbilicus to the right lower
abdominal quadrant (RLQ), which is continuous and more severe
than the early visceral pain.
Gangrenous appendicitis
Intramural venous and arterial thromboses ensue, resulting in
gangrenous appendicitis.
Perforated appendicitis
Persisting tissue ischemia results in appendiceal infarction
and perforation.
Perforation can cause localized or generalized
peritonitis.
Phlegmonous appendicitis or abscess
An inflamed or perforated appendix can be walled off by
the adjacent greater omentum or small-bowel loops,
resulting in phlegmonous appendicitis or focal abscess.
Spontaneously resolving appendicitis
If the obstruction of the appendiceal lumen is relieved,
acute appendicitis may resolve spontaneously.
This occurs if the cause of the symptoms is lymphoid
hyperplasia or when a fecalith is expelled from the
lumen.
Recurrent appendicitis
The incidence of recurrent appendicitis is 10%.
The diagnosis is accepted as such if the patient underwent
similar occurrences of RLQ pain at different times that, after
appendectomy, were histopathologically proven to be the result
of an inflamed appendix.
Chronic appendicitis
Chronic appendicitis occurs with an incidence of 1% and is defined
by the following: (1) the patient has a history of RLQ pain of at
least 3 weeks duration without an alternative diagnosis; (2)
after appendectomy, the patient experiences complete relief of
symptoms; (3) histopathologically, the symptoms were proven
to be the result of chronic active inflammation of the
appendiceal wall or fibrosis of the appendix.
The overall accuracy for diagnosing acute
appendicitis is approximately 80%, which
corresponds to a mean false-negative appendectomy
rate of 20%.
Diagnostic accuracy varies by sex, with a range of
78-92% in male patients and 58-85% in female
patients.
The classic history of anorexia and periumbilical pain
followed by nausea, right lower quadrant (RLQ)
pain, and vomiting occurs in only 50% of cases.
Vomiting that precedes pain is suggestive of intestinal
obstruction, and the diagnosis of appendicitis should
be reconsidered.
The differential diagnosis of appendicitis is often a clinical challenge because
appendicitis can mimic several abdominal conditions (see Differentials).
Patients with many other disorders present with symptoms similar to those of
appendicitis, such as the following:
Pelvic inflammatory disease (PID) or tubo-ovarian abscess
Endometriosis
Ovarian cyst or torsion
Ureterolithiasis and renal colic
Degenerating uterine leiomyomata
Diverticulitis
Crohn disease
Colonic carcinoma
Rectus sheath hematoma
Cholecystitis
Bacterial enteritis
Mesenteric adenitis and ischemia
Omental torsion
Biliary colic
Renal colic
Urinary tract infection (UTI)
Gastroenteritis
Enterocolitis
Pancreatitis
Perforated duodenal ulcer
Other problems that should be considered in a patient with suspected
appendicitis include appendiceal stump appendicitis, typhlitis, epiploic
appendagitis, psoas abscess, and yersiniosis.
Misdiagnosis in women of childbearing age
Appendicitis is misdiagnosed in 33% of nonpregnant women of childbearing
age.
The most frequent misdiagnoses are PID, followed by gastroenteritis and
urinary tract infection.
In distinguishing appendiceal pain from that of PID, anorexia and onset of pain
more than 14 days after menses suggests appendicitis.
Previous PID, vaginal discharge, or urinary symptoms indicates PID.
On physical examination, tenderness outside the RLQ, cervical motion
tenderness, vaginal discharge, and positive urinalysis support the diagnosis of
PID.
Although negative appendectomy does not appear to adversely affect
maternal or fetal health, diagnostic delay with perforation does increase fetal
and maternal morbidity.
The level of urinary betahuman chorionic gonadotropin (beta-hCG) is useful in
differentiating appendicitis from early ectopic pregnancy.
However, with regard to the WBC count, physiologic leukocytosis during
pregnancy makes this study less useful in the diagnosis than at other times,
and no reliable distinguishing WBC parameters are cited in the literature.
Misdiagnosis in children
Appendicitis is misdiagnosed in 25-30% of children, and the rate of initial
misdiagnosis is inversely related to the age of the patient.
The most common misdiagnosis is gastroenteritis, followed by upper
respiratory infection and lower respiratory infection.
Children with misdiagnosed appendicitis are more likely than their
counterparts to have vomiting before pain onset, diarrhea, constipation,
dysuria, signs and symptoms of upper respiratory infection, and lethargy
or irritability.
Physical findings less likely to be documented in children with a
misdiagnosis than in others include bowel sounds; peritoneal signs;
rectal findings; and ear, nose, and throat findings.
Considerations in elderly patients
Appendicitis in patients older than 60 years accounts for 10% of all
appendectomies.
The incidence of misdiagnosis is increased in elderly patients.
Older patients tend to seek medical attention later in the course of
illness; therefore, a duration of symptoms in excess of 24-48 hours should
not dissuade the clinician from the diagnosis.
In patients with comorbid conditions, diagnostic delay is correlated with
increased morbidity and mortality.
Abdominal Abscess
Cholecystitis and Biliary Colic
Constipation
Crohn Disease
Diverticular Disease
Ectopic Pregnancy
Endometriosis
Gastroenteritis
Gastroenteritis, Bacterial
Inflammatory Bowel Disease
Meckel Diverticulum
Mesenteric Ischemia
Mesenteric Lymphadenitis
Omental Torsion
Ovarian Cysts
Ovarian Torsion
Pediatrics, Intussusception
Pelvic Inflammatory Disease
Renal Calculi
Spider Envenomations, Widow
Urinary Tract Infection, Female
Urinary Tract Infection, Male
Patients with appendicitis may not have the reported classic
clinical picture 37-45% of the time, especially when the appendix
is located in an unusual place (see Anatomy).
In such cases, imaging studies may be important but not always
available.
However, patients with appendicitis usually have accessory signs
that may be helpful for diagnosis.
For example, the obturator sign is present when the internal
rotation of the thigh elicits pain (ie, pelvic appendicitis), and the
psoas sign is present when the extension of the right thigh elicits
pain (ie, retroperitoneal or retrocecal appendicitis).
Laboratory tests are not specific for appendicitis, but they may
be helpful to confirm diagnosis in patients with an atypical
presentation.
CBC Count
C-Reactive Protein
Liver and pancreatic function tests
Urinalysis
Urinary beta-HCG
Urinary 5-HIAA
CT scanning
Ultrasonography
Abdominal radiography
Barium enema study
Radionuclide scanning
MRI
Gross and microscopic evaluation
Studies consistently show that 80-85% of adults with
appendicitis have a white blood cell (WBC) count
greater than 10,500 cells/L.
Neutrophilia greater than 75% occurs in 78% of
patients.
Less than 4% of patients with appendicitis have a
WBC count less than 10,500 cells/L and
neutrophilia less than 75%.
Dueholm et al further delineated the relationship
between the WBC count and the likelihood of
appendicitis by calculating likelihood ratios for
defined intervals of the WBC count.
CBC tests are inexpensive, rapid, and
widely available; however, the findings are
nonspecific.
In infants and elderly patients, a WBC count is
especially unreliable because these patients
may not mount a normal response to
infection.
In pregnant women, the physiologic
leukocytosis renders the CBC count useless
for the diagnosis of appendicitis
C-reactive protein (CRP) is an acute-phase reactant synthesized by
the liver in response to infection or inflammation and rapidly
increases within the first 12 hours.
CRP has been reported to be useful in the diagnosis of
appendicitis; however, it lacks specificity and cannot be used to
distinguish between sites of infection.
CRP levels of greater than 1 mg/dL are commonly reported in
patients with appendicitis, but very high levels of CRP in patients
with appendicitis indicate gangrenous evolution of the disease,
especially if it is associated with leukocytosis and neutrophilia.
However, CRP normalization occurs 12 hours after onset of
symptoms.
Several prospective studies have shown that, in adults who have
had symptoms for longer than 24 hours, a normal CRP level has a
negative predictive value of 97-100% for appendicitis.
Thimsen et al noted that a normal CRP level after 12 hours of
symptoms was 100% predictive of benign, self-limited illness.
Liver and pancreatic function tests (eg,
transaminases, bilirubin, alkaline
phosphatase, serum lipase, amylase) may be
helpful to determine the diagnosis in patients
with an unclear presentation.
Urinalysis may be useful in differentiating appendicitis from
urinary tract conditions.
Mild pyuria may occur in patients with appendicitis because of the
relationship of the appendix with the right ureter.
Severe pyuria is a more common finding in urinary tract
infections (UTIs).
Proteinuria and hematuria suggest genitourinary diseases or
hemocoagulative disorders.
One study of 500 patients with acute appendicitis revealed that
approximately one third reported urinary symptoms, most
commonly dysuria or right flank pain.
One in 7 patients had pyuria greater than 10 WBCs per high power
field (hpf), and 1 in 6 patients had greater than 3 red blood cells
(RBCs) per hpf.
Thus, the diagnosis of appendicitis should not be dismissed due
to the presence of urologic symptoms or abnormal urinalysis
For women of childbearing age, the level of
urinary betahuman chorionic gonadotropin
(beta-hCG) is useful in differentiating
appendicitis from early ectopic pregnancy
According to a report by Bolandparvaz et al,
measurement of the urinary 5-hydroxyindoleacetic
acid (U-5-HIAA) levels could be an early marker of
appendicitis.
The rationale of such measurement is related to the
large amount of serotonin-secreting cells in the
appendix.
The investigators noted that U-5-HIAA levels
increased significantly in acute appendicitis,
decreasing when the inflammation shifted to necrosis
of the appendix.
Therefore, such decrease could be an early warning
sign of perforation of the appendix.
Computed tomography (CT) scanning with oral
contrast medium or rectal Gastrografin enema
has become the most important imaging study
in the evaluation of patients with atypical
presentations of appendicitis.
Intravenous contrast is usually not necessary.
Studies have found a decrease in negative
laparotomy rate and appendiceal perforation
rate when pelvic CT imaging was used in
selected patients with suspected appendicitis.
An enlarged appendix is shown in the CT below.
Because of concerns about patient exposure to radiation during CT
scans, ultrasonography has been suggested as a safer primary
diagnostic modality for appendicitis, with CT scanning used
secondarily when ultrasonograms are negative or inconclusive.
In pediatric patients, the ACEP 2010 clinical policy update
recommends using ultrasonography for confirmation, but not
exclusion, of acute appendicitis.
To definitively exclude acute appendicitis, CT is recommended.
[6, 7]
A healthy appendix usually cannot be viewed with
ultrasonography.
When appendicitis occurs, the ultrasonogram typically
demonstrates a noncompressible tubular structure of 7-9 mm in
diameter (see the images below).
Sagittal graded compression
transabdominal sonogram
shows an acutely inflamed
appendix.
The tubular structure is
noncompressible, lacks
peristalsis, and measures
greater than 6 mm in
diameter.
A thin rim of
periappendiceal fluid is
present.
Transverse graded
compression transabdominal
sonogram of an acutely
inflamed appendix.
Note the target like
appearance due to thickened
wall and surrounding
loculated fluid collection.
The kidneys-ureters-bladder (KUB) radiographic
view is typically used to visualize an
appendicolith in a patient with symptoms
consistent with appendicitis (see the following
image).
This finding is highly suggestive of appendicitis,
but appendicoliths also occur in fewer than 10%
of cases.
The consensus in the literature is that plain
radiographs are insensitive, nonspecific, and not
cost-effective.
Kidneys-ureters-bladder
(KUB) radiograph shows
an appendicolith in the
right lower quadrant.
An appendicolith is seen
in fewer than 10% of
patients with
appendicitis, but, when
present, it is essentially
pathognomonic.
In the past, barium enema examination was used to
diagnose appendicitis; in the era of ultrasonography
and CT scanning, barium enema study has essentially
no role in the diagnosis of acute appendicitis.
A single-contrast study can be performed on an
unprepared bowel.
Absent or incomplete filling of the appendix
coupled with pressure effect or spasm in the cecum
suggests appendicitis.
The typical radiologic sign of appendicitis is the
"reverse 3," which typically manifests as an
indentation of the cecum.
However, the appendix cannot be visualized in 50%
of healthy individuals; therefore, barium enema lacks
reliability.
Whole blood is withdrawn for radionuclide
scanning.
Neutrophils and macrophages are labeled
with technetium Tc 99m (
99m
Tc) albumin and
administered intravenously.
Then, images of the abdomen and pelvis are
obtained serially over 4 hours.
Localized uptake of tracer in the RLQ
suggests appendiceal inflammation.
Magnetic resonance imaging (MRI) plays a relatively
limited role in the evaluation of appendicitis because of
its high cost, long scan times, and limited availability.
However, the lack of ionizing radiation makes it an
attractive modality in pregnant patients.
In fact, Cobben et al showed that MRI is far superior to
transabdominal ultrasonography in evaluating pregnant
patients with suspected appendicitis
Nonetheless, when evaluating pregnant patients with
suspected appendicitis, graded compression
ultrasonography should be the imaging test of choice.
If ultrasonography demonstrates an inflamed appendix,
the patient should undergo appendectomy.
If graded compression ultrasonography is nondiagnostic,
the patient should undergo MRI of the abdomen and
pelvis.
In the early stages of appendicitis, the appendix
grossly appears edematous with dilation of the
serosal vessels.
Microscopy demonstrates neutrophil infiltrate of the
mucosal and muscularis layers extending into the
lumen.
As time passes, the appendiceal wall grossly
appears thickened, the lumen appears dilated, and
a serosal exudate (fibrinous or fibrinopurulent) may
be observed as granular roughening.
At this stage, mucosal necrosis may be observed
microscopically.
Appendectomy remains the only curative treatment of appendicitis, but
management of patients with an appendiceal mass can usually be divided
into the following 3 treatment categories:
Patients with a phlegmon or a small abscess: After intravenous (IV) antibiotic therapy, an
interval appendectomy can be performed 4-6 weeks later.
Patients with a larger well-defined abscess: After percutaneous drainage with IV antibiotics is
performed, the patient can be discharged with the catheter in place. Interval appendectomy
can be performed after the fistula is closed.
Patients with a multicompartmental abscess: These patients require early surgical drainage.
Although many controversies exist over the nonoperative management of acute
appendicitis, antibiotics have an important role in the treatment of patients
with this condition.
Antibiotics considered for patients with appendicitis must offer full aerobic and
anaerobic coverage.
According to several studies, antibiotic prophylaxis should be administered
before every appendectomy.
When the patient becomes afebrile and the white blood cell (WBC) count
normalizes, antibiotic treatment may be stopped.
Cefotetan and cefoxitin seem to be the best choices of antibiotics.
The emergency department (ED) clinician must evaluate the larger group
of patients who present to the ED with abdominal pain of all etiologies
with the goal of approaching 100% sensitivity for the diagnosis in a time-,
cost-, and consultation-efficient manner.
Establish IV access and administer aggressive crystalloid therapy to
patients with clinical signs of dehydration or septicemia.
Patients with suspected appendicitis should not receive anything by
mouth.
Administer parenteral analgesic and antiemetic as needed for patient
comfort.
The administration of analgesics to patients with acute undifferentiated
abdominal pain has historically been discouraged and criticized because
of concerns that they render the physical findings less reliable.
However, at least 8 randomized controlled studies have demonstrated
that administering opioid analgesic medications to adult and pediatric
patients with acute undifferentiated abdominal pain is safe; no study
has shown that analgesics adversely affect the accuracy of physical
examination
Anecdotal reports describe the success of IV
antibiotics in treating acute appendicitis in
patients without access to surgical intervention
(eg, submariners, individuals on ships at sea).
In a prospective study of 20 patients with
ultrasonography-proven appendicitis, symptoms
resolved in 95% of patients receiving antibiotics
alone, but 37% of these patients had recurrent
appendicitis within 14 months.
Preoperative antibiotics have demonstrated
efficacy in decreasing postoperative wound
infection rates in numerous prospective
controlled studies, and they should be
administered in conjunction with the surgical
consultant.
Broad-spectrum gram-negative and anaerobic
coverage is indicated.
Penicillin-allergic patients should avoid beta-
lactamase type antibiotics and cephalosporins.
Carbapenems are a good option in these
patients.
A retrospective study suggested that the risk of
appendiceal rupture is minimal in patients with less
than 24-36 hours of untreated symptoms,and
another retrospective study suggested that
appendectomy within 12-24 hours of presentation is
not associated with an increase in hospital length of
stay, operative time, advanced stages of appendicitis,
or complications compared with appendectomy
performed within 12 hours of presentation.
Additional studies are needed to demonstrate
whether initiation of antibiotic therapy followed by
urgent appendectomy is as effective as emergent
appendectomy for patients with unperforated
appendicitis.
Historically, immediate (emergent) appendectomy was recommended
for all patients with appendicitis, whether perforated or
unperforated.
More recent clinical experience suggests that patients with perforated
appendicitis with mild symptoms and localized abscess or phlegmon
on abdominopelvic computed tomography (CT) scans can be initially
treated with IV antibiotics and percutaneous or transrectal drainage
of any localized abscess.
If the patient's symptoms, WBC count, and fever satisfactorily resolve,
therapy can be changed to oral antibiotics and the patient can be
discharged home.
The above approach is successful in the vast majority of patients with
perforated appendicitis and localized symptoms.
Some have suggested that interval appendectomy is not necessary,
unless the patient presents with recurrent symptoms.
Further studies are needed to clarify not only whether routine interval
appendectomy is indicated but also to identify the optimal treatment
strategy in patients with perforated appendicitis
Initially performed in 1987, laparoscopic appendectomy has been
performed in thousands of patients and is successful in 90-94% of
attempts.
It has also been demonstrated that laparoscopic appendectomy is
successful in approximately 90% of cases of perforated
appendicitis.
However, this procedure is contraindicated in patients with
significant intra-abdominal adhesions.
According to the 2010 Society of American Gastrointestinal and
Endoscopic Surgeons (SAGES) guideline, the indications for
laparoscopic appendectomy are identical to those for open
appendectomy.
The 2010 SAGES guideline lists the following conditions as
suitable for laparoscopic appendectomy:
Uncomplicated appendicitis
Appendicitis in pediatric patients
Suspected appendicitis in pregnant women
According to the SAGES guideline, laparoscopic appendectomy may be
the preferred approach in the following cases:
Perforated appendicitis
Appendicitis in elderly patients
Appendicitis in obese patients
The SAGES guideline states that the laparoscopic approach should be
preferred in women of childbearing age with presumed appendicitis.
Diagnostic laparoscopy may be useful in selected cases (eg, infants,
elderly patients, female patients) to confirm the diagnosis of appendicitis.
This procedure has been suggested for pregnant patients in the first
trimester with suspected appendicitis.
If findings are positive, such procedures should be followed by definitive
surgical treatment at the time of laparoscopy.
Although negative appendectomy does not appear to adversely affect
maternal or fetal hdiagnostic delay with perforation does increase fetal
and maternal morbidityealth,.
According to the SAGES guideline, if findings are negative (normal
appendix) on laparoscopic approach, removal should be considered based
on the patients clinical situation.
Advantages of laparoscopic appendectomy include increased cosmetic
satisfaction and a decrease in the postoperative wound-infection rate.
Some studies show that laparoscopic appendectomy shortens the hospital
stay and convalescent period compared with open appendectomy
Complications of appendicitis may include
wound infection, dehiscence, bowel
obstruction, abdominal/pelvic abscess,
and, rarely, death.
Stump appendicitis also occurs rarely;
however, at least 36 reported cases of
appendicitis in the surgical stump after
previous appendectomy exist
In cases of suspected appendicitis, consult a
general surgeon.
The surgeon's goals are to evaluate a
relatively small population of patients
referred for suspected appendicitis and to
minimize the negative appendectomy rate
without increasing the incidence of
perforation.
Potrebbero piacerti anche
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Problem 2: By: Varla S. G (405090215)Documento122 pagineProblem 2: By: Varla S. G (405090215)varlavarleyNessuna valutazione finora
- Non Fatty LiverDocumento3 pagineNon Fatty LivervarlavarleyNessuna valutazione finora
- Problem 3 - VarlaDocumento75 pagineProblem 3 - VarlavarlavarleyNessuna valutazione finora
- PROBLEM 2B - VarlaDocumento50 paginePROBLEM 2B - VarlavarlavarleyNessuna valutazione finora
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Methicillin-Resistant Staphylococcus Aureus (MRSA) in Adults: Treatment of Skin and Soft Tissue InfectionsDocumento23 pagineMethicillin-Resistant Staphylococcus Aureus (MRSA) in Adults: Treatment of Skin and Soft Tissue InfectionssadiaNessuna valutazione finora
- Abces SubfrenicDocumento2 pagineAbces SubfrenicAdrian NiţuNessuna valutazione finora
- Liver AbscessDocumento36 pagineLiver AbscessYuni PurwatiNessuna valutazione finora
- Sa CelulitisDocumento19 pagineSa CelulitisJulio Ramos EliasNessuna valutazione finora
- Jurnal Mediastinitis 1Documento3 pagineJurnal Mediastinitis 1Husnul KhatimahNessuna valutazione finora
- 2013-12 Editorial For The Month of December 2013 (Information Given in Repertory Is Not Always Gospel Truth)Documento3 pagine2013-12 Editorial For The Month of December 2013 (Information Given in Repertory Is Not Always Gospel Truth)Muhammad Ata Ul MustafaNessuna valutazione finora
- Abscess Case Pre FinalDocumento41 pagineAbscess Case Pre FinalDavid DueñasNessuna valutazione finora
- Swellings of The JawDocumento36 pagineSwellings of The JawSumaNessuna valutazione finora
- Treatment of Acute AppendicitisDocumento17 pagineTreatment of Acute Appendicitiszamir90Nessuna valutazione finora
- Biphasic CT Imaging of Deep Neck Infections (Dnis) : How Does Dual Injection Mode Helps in Differentiation Between Types of Collections?Documento11 pagineBiphasic CT Imaging of Deep Neck Infections (Dnis) : How Does Dual Injection Mode Helps in Differentiation Between Types of Collections?Muhammad Dody HermawanNessuna valutazione finora
- Animal Bite: DR - Alex. May 19, 2021Documento21 pagineAnimal Bite: DR - Alex. May 19, 2021Alex beharuNessuna valutazione finora
- Inflammation and RepairDocumento38 pagineInflammation and RepairIsaac Nsiah Acheampong100% (1)
- NCP - JaundiceDocumento5 pagineNCP - JaundiceQueen Shine0% (1)
- NCM 112 - Lower Respiratory InfectionsDocumento27 pagineNCM 112 - Lower Respiratory InfectionsLester LigutomNessuna valutazione finora
- 7 Osteomyelitis of JawsDocumento38 pagine7 Osteomyelitis of JawsDan 04Nessuna valutazione finora
- Crohns DiseaseDocumento42 pagineCrohns DiseaseFiraFurqaniNessuna valutazione finora
- 194 Surgical Cases PDFDocumento160 pagine194 Surgical Cases PDFkint100% (4)
- Surgical InfectionsDocumento54 pagineSurgical Infectionsmanish shresthaNessuna valutazione finora
- Surgical Site Infection: Intern Dr. Amit PoudelDocumento37 pagineSurgical Site Infection: Intern Dr. Amit PoudelShubham upadhyayNessuna valutazione finora
- Surgery MCQsDocumento24 pagineSurgery MCQsKiara Govender100% (2)
- Surgical Site InfectionDocumento35 pagineSurgical Site InfectionDetria Rahma GastiNessuna valutazione finora
- A-Z Family Medical EncyclopediaDocumento815 pagineA-Z Family Medical Encyclopediasunilas218408100% (7)
- Management of Odontogenic Infections and SepsisDocumento8 pagineManagement of Odontogenic Infections and Sepsismartha carolina vargas bernalNessuna valutazione finora
- Residual Limb Complications and Management StrategiesDocumento9 pagineResidual Limb Complications and Management StrategiesTarushi TanwarNessuna valutazione finora
- Contents 6Documento9 pagineContents 6Mitesh DabhiNessuna valutazione finora
- Surgical Site InfectionDocumento14 pagineSurgical Site InfectionSri AsmawatiNessuna valutazione finora
- Anal FistulaDocumento26 pagineAnal FistulaBeverly PagcaliwaganNessuna valutazione finora
- Lecture 16 Diseases of Bones and Joints (Co)Documento14 pagineLecture 16 Diseases of Bones and Joints (Co)Sara Abdul RahmanNessuna valutazione finora
- Mastitis 2Documento25 pagineMastitis 2Riana Pasca RoshianNessuna valutazione finora
- INFECTIONS Staphylococcal InfectionsDocumento48 pagineINFECTIONS Staphylococcal InfectionsDr.P.NatarajanNessuna valutazione finora