Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Problem 3 - Varla
Caricato da
varlavarley0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
44 visualizzazioni75 pagineFewer than 400 cases of typhoid fever are reported in the u.s. Each year. Most cases are brought in from countries where typhid fever is common. A few people can become carriers of the bacteria and continue to release the bacteria in their stools for years.
Descrizione originale:
Titolo originale
PROBLEM 3 -VARLA.pptx
Copyright
© © All Rights Reserved
Formati disponibili
PPTX, PDF, TXT o leggi online da Scribd
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoFewer than 400 cases of typhoid fever are reported in the u.s. Each year. Most cases are brought in from countries where typhid fever is common. A few people can become carriers of the bacteria and continue to release the bacteria in their stools for years.
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato PPTX, PDF, TXT o leggi online su Scribd
0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
44 visualizzazioni75 pagineProblem 3 - Varla
Caricato da
varlavarleyFewer than 400 cases of typhoid fever are reported in the u.s. Each year. Most cases are brought in from countries where typhid fever is common. A few people can become carriers of the bacteria and continue to release the bacteria in their stools for years.
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato PPTX, PDF, TXT o leggi online su Scribd
Sei sulla pagina 1di 75
PROBLEM 3
By: Varla Septrinidya Gharatri - 405090215
TYPHOID FEVER
DEFINITION
Acute enteric infectious disease
Caused by Salmonella typhi (S.Typhi) and
S.parathypi (a,b), S.chloreaesuis
Prolonged fever, relative bradycardia, apathetic facial
expressions, roseola, splenomegaly, hepatomegaly,
leukopenia.
intestinal perforation, intestinal hemorrhage
EPIDEMIOLOGY
Affected patients' age in Indonesia between
3-19 years to reach 91% of cases.
Typhoid fever is common in developing
countries, but fewer than 400 cases are
reported in the U.S. each year.
Most cases in the U.S. are brought in from
other countries where typhoid fever is
common.
ETIOLOGY
The bacteria that cause typhoid fever -- S.
typhi -- spread through contaminated food,
drink, or water.
If you eat or drink something that is
contaminated, the bacteria enter your body.
They travel into your intestines bloodstream
lymph nodes, gallbladder, liver, spleen, and
other parts of the body.
A few people can become carriers of S.
typhi and continue to release the bacteria in
their stools for years, spreading the disease.
Structure of salmonella
Gram negative, no spore, anaerob
fakultative
Have flagel peritrich for movement
Endure to frozen water in long period
Endure to chemical like sodium
deoxycholate, briliant green, saodium
tetrathionate. This chemical for inhibit growth
of other enteric bacteria
Fermentation glucosa (+), manosa (+), no
fermentation lactosa and sukrosa
TSIA: -/+, H2S (+)
Structure antigen
3 major antigen:
Ag flagel H:
destroy in 60
0
C,
alchohol, acid, Ab IgG
Ag O:
endure to 100
0
C,
alcholol, acid. Ab IgM
Ag Vi:
upper Ag O,
as a capsul, prevent fagositosis/ demage of intracellular
membran bacteria
Destroy 60
0
C within 1 hour
Transmission
S typhi has no nonhuman vectors. The
following are modes of transmission:
Oral transmission via food or beverages handled by
an individual who chronically sheds the bacteria
through stool or, less commonly, urine
Hand-to-mouth transmission after using a
contaminated toilet and neglecting hand hygiene
Oral transmission via sewage-contaminated water
or shellfish (especially in the developing world)
LIFE CYCLE OF S.Typhii
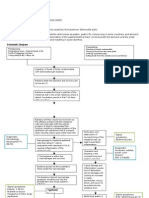
Pathophysiology
intestine
IgA immune
response is less well
Salmunella breed
Food
contaminated with
Salmonella
Penetrate the
epithelial cells and
proliferate in the
lamina propia
macrofag
DIE
Survive
Plaque
payers
KGB
mecent
erica
Tora
sikus
duct
bacteremia
Orga
n RE
Leaving
the
phagocyt
e cells
Pathophysiology
phagocytes
cell
Breed in the
extracellular
organ
Bakteriremia
II
Liver
gall
bladder
Intestinal
lumen
feces
Penetrate more
and reactions as
previously
Macrofag
already
activated
hypera
ctive
Releasing cytokines Symptoms
Reaction hiperplasi plaque peyeri
Hyperplasia or
necrosis
hypersensitivity
reactions
Erosion of blood vessels
The process continues
GI bleeding
Perforation
Penetrate the mucosa and
muscle layer
Accumulation in
inflammatory bowel
mononuclear
Clinical Manifestation
Salmonella
thypi
infection
per oral
patients went to the doctor yet
Incubation period 10-14 days
No
symptoms
Symptoms
begin
week 1:
prodormal symptoms:
fever
anorexia
nausea, vomiting
constipation
myalgia
second week and
next:
relative bradikardi
thypoid tongue
oeganomegali
delirium
patient went to the doctor
Week 1 second week
and next
Symptoms
First week of illness
Fever, often as high as 103 or 104 F (39.4 or 40 C)
Headache
Weakness and fatigue
Sore throat
Abdominal pain
Diarrhea or constipation
Rash
Second week of illness
Continuing high fever
Either diarrhea that has the color and consistency of pea
soup, or severe constipation
Considerable weight loss
Extremely distended abdomen
Third week of illness
Become delirious
Lie motionless and exhausted with your eyes half-
closed in what's known as the typhoid state
Life-threatening complications often develop at this
time.
Fourth week of illness
Improvement may come slowly during the fourth
week. Your fever is likely to decrease gradually until
your temperature returns to normal in another week
to 10 days. But signs and symptoms can return up to
two weeks after your fever has subsided.
Laboratory Studies
Culture
Polymerase chain reaction (PCR)
Specific serologic tests
Assays that identify Salmonella antibodies or antigens support the
diagnosis of typhoid fever, but these results should be confirmed with
cultures or DNA evidence.
Widal test
Indirect hemagglutination, indirect fluorescent Vi antibody, and indirect
enzyme-linked immunosorbent assay (ELISA) for immunoglobulin M
(IgM) and IgG antibodies to S typhi polysaccharide
Other nonspecific laboratory studies
Serological tests (Widal test):
Five types of antigens:
somatic antigen (O), flagella (H) antigen, and paratyphoid
fever flagella (A,B,C) antigen.
Antibody reaction appear during first week
70% positive in 3~4 weeks and can prolong to several
months
In some cases, antibodies appear slowly, or remain at a low
level,
some(10~30%) not appear at all.
Examination
Blood test:
Hb
Leukocyte
trombocyte
Leukopenia
Mild Thrombocytopenia
SGPT/SGOT
Liver
function:
SGOT
SGPT
THYPHOID
Widal Test
Culture +
Definitive Diagnosis
Aglutination
Antigen
Antibodi
Get + 6 months-1 year
POST THYPOID
BLOOD
CULTURE
BILE
CULTURE
TREATMENT
Fluids and electrolytes may be given through
a vein (intravenously), or you may be asked to
drink uncontaminated water with electrolyte
packets.
Appropriate antibiotics are given to kill the
bacteria. There are increasing rates of
antibiotic resistance throughout the world, so
your health care provider will check current
recommendations before choosing an
antibiotic.
Antibiotic Therapy For Enteric Fever in
Adults
Indication Agent Dosage (Route)
Duration
, Days
Empirical
Treatment
Ceftriaxone
Azithromycin
1-2 g/d (IV)
1 g/d (PO)
7-14
5
Fully Susceptible
Ciprofloxacin(1
st
line)
Amoxicilin (2
nd
line)
Chloramphenicol
Trimethoprim-
Sulfamethoxazole
500mg bid (PO) or
400mg q12h(IV)
1g tid (PO) or 2 g q6h
(IV)
25mg/kg tid (PO/IV)
160/800mg bid (PO)
5-7
14
14-21
14
Source : Harrison
Indication Agent Dosage (Route) Duration, Days
Multidrug-
Resistant
Ciprofloxacin
Ceftriaxone
Azithromycin
500 mg bid (PO) or
400 mg q12h (IV)
2-3 g/d (IV)
1 g/d (PO)
5-7
7-14
5
Nalidixic Acid-
Resitant
Ceftriaxone
Azithromycin
High-dose
ciprofloxacin
1-2 g/d (IV)
1 g/d (PO)
750 mg bid (PO) or
400mg q8h (IV)
7-14
5
10-14
Source : Harrison
Management
Non pharmacology
Bed rest and treatment to prevent complication and make healing faster
Bed rest , having meal, drink, take a bath, stools
Once in the care need ,should taking care of cleanliness of the bed, clothes,
and equipment in use
Diet and supporting therapy
Some researchers show that solved food (rice with side dish low cellulose) is
safe for patient
Surgical Care
Surgery is usually indicated in intestinal perforation cases.
Most surgeons prefer simple closure of the perforation with drainage of the
peritoneum.
Small-bowel resection is indicated for patients with multiple perforations.
PROGNOSIS
Symptoms usually improve in 2 to 4 weeks
with treatment.
The outcome is likely to be good with early
treatment, but becomes poor if complications
develop.
Symptoms may return if the treatment has not
completely cured the infection.
Complication Intestinal
Intestine bleeding
Perforation small intestine
Illeus paralitic
Complication Extraintestinal
Hematology thrombocytopenia, hypofibrinogenemia,
increase prothrombin time, increase partial
thromboplastin time, increase fibrin degradation
products, DIC
Hepatitis typhosa
Myocarditis
Neuropsychiatric parkinson rigidity
PREVENTION
Vaccines are recommended for travel outside of the
U.S., Canada, northern Europe, Australia, and New
Zealand, and during epidemic outbreaks.
If you are traveling to an area where there is typhoid
fever, ask your health care provider if you should bring
electrolyte packets in case you get sick.
Immunization is not always completely effective and
at-risk travelers should drink only boiled or bottled
water and eat well-cooked food. Studies of an oral
live attenuated typhoid vaccine are now under way
and appear promising.
Water treatment, waste disposal, and protecting
the food supply from contamination are important
public health measures. Carriers of typhoid must not
be allowed to work as food handlers.
DYSENTRY BACILLI
DEFINITION
A condition characterized by diarrhea, with the
consistency of stool is usually soft,
accompanied by inflammatory exudate
containing polymorphonuclear leukocytes and
blood.
Acute infection terminal ileum and colon
caused by bacteria of the genus Shigella
EPIDEMIOLOGI
Shigella infection easily occur in densely
populated, poor sanitation, lack of water,
and low levels of personal hygiene.
Shigella infection in endemic area is 10-15%
cause of diarrhea in children.
Number of bacteria to cause disease are
relatively few, it ranged between 10-100
germs.
Therefore it is very easy transmission is
fecal-oral route, either by direct contact or
due to contaminated food and drink
MICROBIOLOGY
Shigella including enterobacteriaceae group,
which is gram negative, facultative anaerobes
and very similar to eschericia coli.
Several properties that distinguish the bacteria
with E. coli are bacteria do not stir it active, do
not produce gas in glucose media and in
general negative lactose.
Known 4 shigella species with different
serotypes namely: S. dysenteriae (12 serotypes),
S. flexneri (14 serotypes), S. boydii (15
serotypes), and S. sonnei (1 serotypes)
PATHOPHISIOLOGY
After passing through the stomach and small
intestine the bacteria invade the colonic
mucosal epithelial cells and proliferate in it.
Expansion of the invasion of bacteria into the
surrounding cells through a mechanism of cell-to-
cell transfer
Although the initial lession occurs in the epithelial
layer but the local inflammatory response that
accompanies severe enough, involving PMN
leukocytes and macrophages.
It causes edema, mikroabses, loss of goblet cells,
damage to tissue architecture and mucosal
ulceration.
CLINICAL SYMPTOMS
The shoots ranged from 7 hours to 7 days.
7-day average duration symptoms in adults, but
can take up to 4 weeks.
In the early phase of patients complained of
lower abdominal pain, rectal burning
sensation, diarrhea accompanied by fever
which can reach 40 C.
Further reduced but the stool was diarrhea
containing blood and mucus, tenesmus, and
decreased apetite.
In children may get a high fever with or without
convulsions, delirium, headache, stiff neck,
and lethargy.
DIAGNOSE
Microscopic examination of feces showed
eritrocytes and PMN leukocytes.
To confirm the diagnosis made from the
material culture of fresh feces or anal
swab.
Sigmoidoscopy can confirm the diagnosis of
colitis, but the examination generally not
necessary, because it causes the patient to
feel very uncomfortable.
In the acute phase of shigella infection,
serology test are not useful.
DIFFERENTIAL DIAGNOSE
Salmonellosis
Enterotoxin diarrhea syndrome due to E. coli
Cholera
Colitis ulserosa
COMPLICATIONS
Intestinal
Toxic megacolon
Intestinal perforation
Dehydration
Hypovolemic shock
Malnutrition
Extraintestinal
Coughs
Colds
Pneumonia
Meningismus
Seizures
Peripheral neuropathy
Hemolytic uremic
syndrome
Thrombocytopenia
Leukemoid reaction
Arthritis
TREATMENT
Address the balance of fluid and electrolyte
disturbances
The majority of patients with dysentery can be treated with
oral rehydration.
In patients with severe diarrhea with dehydration and
patients with excessive vomiting that cannot be performed
by oral rehydration, intravenous rehydration should be
done.
Antibiotics
Making use of antibiotics based on severity of the disease
entirely, in which patients with moderate to severe
symptoms of dysentery with persistent diarrhea.
Some types of antibiotics that are recommended are:
Ampicilin 500 mg 4 times per day
Cotrimoxazole 2 times 2 tablets per day
Tetracycline 500 mg 4 times per day for 5 days
Narcotic drugs and derivates
Avoid drugs that can inhibit intestinal motility such
as narcotics and its derivates, because it can
reduce the elimination of bacteria, and provoke
toxic megacolon.
Symptomatic treatment
Are given to according to the patient analgesic-
antipiretic and anticonvulsant
CHOLERA
DEFINITION
Cholera is an infection of the small intestine
that causes a large amount of watery diarrhea.
CAUSES, INCIDENCE, RISK
FACTORS
Cholera is caused by the bacterium Vibrio cholerae.
The bacteria releases a toxin that causes increased release of water in the
intestines, which produces severe diarrhea.
Cholera occurs in places with poor sanitation, crowding, war, and
famine.
Common locations for cholera include:
Africa
Asia
India
Mexico
South and Central America
People get the infection by eating or drinking contaminated food or
water.
A type of vibrio bacteria also has been associated with shellfish, especially
raw oysters.
Risk factors include:
Exposure to contaminated or untreated drinking water
Living in or traveling to areas where there is cholera
SYMPTOMS
Abdominal cramps
Dry mucus membranes or mouth
Dry skin
Excessive thirst
Glassy or sunken eyes
Lack of tears
Lethargy
Low urine output
Nausea
Rapid dehydration
Rapid pulse (heart rate)
Sunken "soft spots" (fontanelles) in infants
Unusual sleepiness or tiredness
Vomiting
Watery diarrhea that starts suddenly and has a "fishy" odor
Note: Symptoms can vary from mild to severe.
SIGNS AND TESTS
Tests that may be done include:
Blood culture
Stool culture
TREATMENT
The objective of treatment is to replace fluid
and electrolytes lost through diarrhea.
Depending on your condition, you may be
given fluids by mouth or through a vein
(intravenous).
Antibiotics may shorten the time you feel ill.
The World Health Organization (WHO) has
developed an oral rehydration solution that
is cheaper and easier to use than the
typical intravenous fluid.
This solution of sugar and electrolytes is
now being used internationally.
PROGNOSIS
Severe dehydration can cause death.
Given adequate fluids, most people will make
a full recovery.
COMPLICATIONS
Severe dehydration
Death
PREVENTION
The U.S. Centers for Disease Control and
Prevention does not recommend cholera
vaccines for most travelers. (Such a vaccine
is not available in the United States.)
Travelers should always take precautions
with food and drinking water, even if
vaccinated.
When outbreaks of cholera occur, efforts
should be directed toward establishing clean
water, food, and sanitation, because
vaccination is not very effective in managing
outbreaks.
GASTROENTERITIS
DEFINITION
Gastroenteritis is a condition that causes
irritation and inflammation of the stomach
and intestines (the gastrointestinal tract).
An infection may be caused by bacteria or
parasites in spoiled food or unclean water.
The severity of infectious gastroenteritis
depends on your immune systems ability to
resist the infection.
Electrolytes (these include essential elements
of sodium and potassium) may be lost as you
vomit and experience diarrhea.
CAUSES
Viruses and bacteria are the most common.
Viruses and bacteria are very contagious and can
spread through contaminated food or water.
Gastroenteritis caused by viruses may last 1-2 days.
On the other hand, bacterial cases can last a week
or more.
Bacteria:
Escherichia coli - Travelers diarrhea, food poisoning,
dysentery, colitis, or uremic syndrome
Salmonella - Typhoid fever; handling poultry or
reptiles such as turtles that carry the germs
Campylobacter - Undercooked meat, unpasteurized
milk
Shigella - Dysentery
Viruses:
Viral outbreaks (30-40% of cases in children) can
spread rapidly through close contact among
children in day care and schools.
Poor handwashing habits can spread viruses.
Common viral causes include the following:
Adenoviruses
Rotaviruses
Caliciviruses
Astroviruses
Norovirus (formerly called Norwalk-like virus or
NLV) and Norwalk virus
Parasites and protozoans:
These tiny organisms are less frequently
responsible for intestinal irritation.
You may pick up one of these by drinking
contaminated water.
Swimming pools are common places to come in
contact with these parasites.
Common parasites include these:
Giardia - The most frequent cause of waterborne
diarrhea causing giardiasis
Cryptosporidium - Affects mostly people with
weakened immune systems, causes watery
diarrhea
Giardia Lamblia
Other common causes:
Chemical toxins most often found in seafood, food allergies, heavy
metals, antibiotics, and other medications also may be responsible for
bouts of gastroenteritis that are not infectious to others.
Medications
Aspirin
Nonsteroidal anti-inflammatory medicines (such as Motrin or Advil)
Antibiotics
Caffeine
Steroids - Excessive use or a sudden change in frequency or dosage
Laxatives
Inability to tolerate the sugar lactose in milk and milk
products such as cheese and ice cream
Exposure to heavy metals sometimes present in drinking
water
Arsenic
Lead
Mercury
SYMPTOMS
Gastroenteritis may affect both the stomach and the
intestines, resulting in one or more of the following
symptoms:
Common symptoms:
Low grade fever (99F)
Nausea with or without vomiting
Mild-to-moderate diarrhea: May range from 2-4 loose stools per day
for adolescents and adults to stools that run out of the diaper in
infants.
Crampy painful bloating
Vomiting: May or may not accompany diarrhea.
More serious symptoms
Blood in vomit or stool
Vomiting more than 48 hours
Fever higher than 101F
Swollen abdomen or abdominal pain coming from the right lower side
Dehydration - Little to no urination, extreme thirst, lack of tears,
and dry mouth (dry diapers in infants)
EXAMS AND TESTS
Anamnese
Checking electrolytes, blood, and stool.
Normal stain of stool sample looking for ova, parasites, and
leukocytes.
Image courtesy of Alexis Carter, MD, Department of Pathology and Laboratory Medicine, East Carolina University.
SELF CARE AT HOME
Dehydration in children:
Children should be given oral rehydration solutions such
as Pedialyte, Rehydrate, Resol, and Rice-Lyte.
Cola, tea, fruit juice, and sports drinks will not correctly replace
fluid or electrolytes lost from diarrhea or vomiting.
After each loose stool, children younger than 2 years should
be given 1-3 ounces of any of the rehydration solutions. Older
children should be asked to drink 3-8 ounces. Adults should
drink as much as possible.
In underdeveloped nations or regions without available
commercial pediatric drinks, the World Health Organization
has established a field recipe for fluid rehydration: Mix 2
tablespoons of sugar (or honey) with teaspoon of table salt
and teaspoon of baking soda. (Baking soda may be
substituted with teaspoon of table salt.) Mix in 1 liter (1 qt) of
clean or previously boiled water.
You will need solid foods eventually to help end the diarrhea.
After 24 hours, begin to offer bland foods with the BRAT
dietbananas, rice, applesauce without sugar, toast, pasta, or
potatoes.
Dehydration in adults:
Although adults and adolescents have a larger
electrolyte reserve than children, electrolyte
imbalance and dehydration may still occur as fluid
is lost through vomiting and diarrhea.
Initially, adults should eat ice chips and clear,
noncaffeinated, nondairy liquids such as
Gatorade, ginger ale, fruit juices, and Kool-Aid or
other commercial drink mixes.
After 24 hours of fluid diet without vomiting, begin
a soft-bland solid diet such as the BRAT diet.
MEDICAL TREATMENT
Rehydration
Antibiotics may be given for certain bacteria,
specifically Campylobacter, Shigella,
and Vibrio cholerae
Antiemetics for adults
Avoid antidiarrheal medications for all age
groups if they suspect the infection is caused
by a toxin
PREVENTION
With most infectious germs, the key is to block
the spread of the organism.
Always wash your hands.
Eat properly prepared and stored food.
Bleach soiled laundry.
Vaccinations for Salmonella typhi, Vibrio cholerae,
and rotavirus have been developed.
For lactose intolerance, supplementary enzymes are
available over-the-counter for adolescents and adults
to aid digestion of milk sugars.
Soy formulas and other lactose-free products are
available from most grocery stores for formula-feeding
infants.
DENGUE HEMORRHAGIC
FEVER
DEFINITION
Dengue hemorrhagic fever is a severe,
potentially deadly infection spread by certain
species of mosquitoes (Aedes aegypti).
CAUSE, INCIDENCE, RISK
FACTORS
Four different dengue viruses are known to cause dengue
hemorrhagic fever.
Dengue hemorrhagic fever occurs when a person catches a
different type dengue virus after being infected by another one
sometime before.
Prior immunity to a different dengue virus type plays an important
role in this severe disease.
Worldwide, more than 100 million cases of dengue fever occur
every year.
A small number of these develop into dengue hemorrhagic fever.
Most infections in the United States are brought in from other
countries.
It is possible, but uncommon, for a traveler who has returned to the
United States to pass the infection to someone who has not
traveled.
Risk factors for dengue hemorrhagic fever include having
antibodies to dengue virus from prior infection and being younger
than 12, female, or Caucasian.
SYMPTOMS
Early symptoms include:
Decreased appetite
Fever
Headache
Joint aches
Malaise
Muscle aches
Vomiting
Acute phase symptoms include:
Restlessness followed by:
Ecchymosis
Generalized rash
Petechiae
Worsening of earlier symptoms
Shock-like state
Cold, clammy extremities
Sweatiness (diaphoretic)
SIGNS AND TESTS
A physical examination may reveal:
Enlarged liver (hepatomegaly)
Low blood pressure
Rash
Red eyes
Red throat
Swollen glands
Weak, rapid pulse
Tests may include:
Arterial blood gases
Coagulation studies
Electrolytes
Hematocrit
Liver enzymes
Platelet count
Serologic studies (demonstrate antibodies to Dengue viruses)
Serum studies from samples taken during acute illness and convalescence (increase
in titer to Dengue antigen)
Tourniquet test (causes petechiae to form below the tourniquet)
X-ray of the chest (may demonstrate pleural effusion)
TREATMENT
Because Dengue hemorrhagic fever is caused by
a virus for which there is no known cure or
vaccine, the only treatment is to treat the
symptoms.
A transfusion of fresh blood or platelets can
correct bleeding problems
Intravenous (IV) fluids and electrolytes are also
used to correct electrolyte imbalances
Oxygen therapy may be needed to treat
abnormally low blood oxygen
Rehydration with intravenous (IV) fluids is
often necessary to treat dehydration
Supportive care in an intensive care
unit/environment
PROGNOSIS
With early and aggressive care, most patients
recover from dengue hemorrhagic fever.
However, half of untreated patients who go
into shock do not survive.
COMPLICATIONS
Encephalopathy
Liver damage
Residual brain damage
Seizures
Shock
PREVENTION
There is no vaccine available to prevent
dengue fever.
Use personal protection such as full-coverage
clothing, netting, mosquito repellent containing
DEET, and if possible, travel during periods of
minimal mosquito activity.
Mosquito abatement programs can also
reduce the risk of infection.
Viral infection
Such as upper respiratory tract infection. Abrupt onset
with fever, headache, leucopenia, sore throat, cough,
coryza.
No rose spots, no enlargement of liver & spleen.
The course of illness no more than 2 weeks.
Differential diagnosis depends on typical manifestations
and blood culture.
Malaria
History of exposure to malaria.
Paroxysms(often periodic) of sequential chill,high fever
and sweating.
Headache, anorexia, splenomegaly, anemia,
leukopenia
Characteristic parasites in erythrocytes,identified in
thick or thin blood smears.
Dengue Fever
Sudden high fever day 1-3 (above 38,5
o
C), in day 3 or
day 4-5 increase but not very high (below 38,5
o
C)
Potrebbero piacerti anche
- 04 - Typhoid FeverDocumento35 pagine04 - Typhoid Feversoheil100% (1)
- TyphoidDocumento26 pagineTyphoidLiya Mary ThomasNessuna valutazione finora
- 04 - Typhoid FeverDocumento31 pagine04 - Typhoid FeverGloria MachariaNessuna valutazione finora
- Enteric FeverDocumento7 pagineEnteric FeverkudzaimuregidubeNessuna valutazione finora
- Typhoid Fever: Infectious DiseaseDocumento18 pagineTyphoid Fever: Infectious DiseaseSoumyadip PradhanNessuna valutazione finora
- Clinical Diagnosis and Management of Typhoid FeverDocumento68 pagineClinical Diagnosis and Management of Typhoid FeverPeriyent Liveryent VozzervodNessuna valutazione finora
- Communicable Diseases: Roberto M. Salvador Jr. R.N.,M.D. Infectious and Tropical Disease SpecialistDocumento846 pagineCommunicable Diseases: Roberto M. Salvador Jr. R.N.,M.D. Infectious and Tropical Disease SpecialistGrn Mynjrkxz100% (1)
- GASTROINTESTINAL DISORDERS AND POISONINGDocumento50 pagineGASTROINTESTINAL DISORDERS AND POISONINGEdelou Alegria JumawanNessuna valutazione finora
- TYPHOID FEVER: CAUSES, SYMPTOMS AND TREATMENTDocumento48 pagineTYPHOID FEVER: CAUSES, SYMPTOMS AND TREATMENTmanibharathiNessuna valutazione finora
- 1.3 Demam Tifoid Dan Kelainan HeparDocumento145 pagine1.3 Demam Tifoid Dan Kelainan HeparajikwaNessuna valutazione finora
- Thypoid - RPUDocumento22 pagineThypoid - RPUERONADIAULFAH SUGITONessuna valutazione finora
- Diarrhoea in TravellersDocumento5 pagineDiarrhoea in TravellersMazo KhanNessuna valutazione finora
- CHAPTER TWO Communicable DssDocumento36 pagineCHAPTER TWO Communicable DssAyro Business CenterNessuna valutazione finora
- Faeco-Oral DiseasesDocumento46 pagineFaeco-Oral DiseasesNatukunda DianahNessuna valutazione finora
- GastroenteritisDocumento4 pagineGastroenteritisArumDesiPratiwiNessuna valutazione finora
- Typhoid FeverDocumento5 pagineTyphoid FeverNaziha InaamNessuna valutazione finora
- Typhoid FeverDocumento9 pagineTyphoid FeverValerrie NgenoNessuna valutazione finora
- Demam Tifoid: Sigit Widyatmoko Fakultas Kedokteran Universitas Muhammadiyah SurakartaDocumento37 pagineDemam Tifoid: Sigit Widyatmoko Fakultas Kedokteran Universitas Muhammadiyah SurakartasakyaNessuna valutazione finora
- Typhoid Fever: by DR .. Magdi Elbaloola Ahmed Physcian & GastrohepatologistDocumento25 pagineTyphoid Fever: by DR .. Magdi Elbaloola Ahmed Physcian & GastrohepatologistÅbübâkêř Äbd-ëřhēēm BãřřîNessuna valutazione finora
- Feco-orally Transmitted DiseasesDocumento133 pagineFeco-orally Transmitted DiseasesTekletsadikNessuna valutazione finora
- Salmonella Infections: (Salmonelloses)Documento56 pagineSalmonella Infections: (Salmonelloses)andualemNessuna valutazione finora
- 伤寒英文教案 Typhoid Fever-应若素Documento36 pagine伤寒英文教案 Typhoid Fever-应若素Wai Kwong ChiuNessuna valutazione finora
- Causes, Signs and Symptoms of Dengue Fever and Typhoid FeverDocumento24 pagineCauses, Signs and Symptoms of Dengue Fever and Typhoid FeverrefkyjuliandriNessuna valutazione finora
- Diarrhea CaseDocumento8 pagineDiarrhea CaseStarr NewmanNessuna valutazione finora
- Understanding Typhoid Fever: Causes, Symptoms and DiagnosisDocumento22 pagineUnderstanding Typhoid Fever: Causes, Symptoms and DiagnosisUci MarleyNessuna valutazione finora
- Pemicu 3 GIT BudiDocumento67 paginePemicu 3 GIT BudiGrace KahonoNessuna valutazione finora
- Pemicu 3 GIT GraceDocumento67 paginePemicu 3 GIT GraceGrace KahonoNessuna valutazione finora
- Typhoid CompilationDocumento20 pagineTyphoid CompilationArc MuNessuna valutazione finora
- ACUTE GASTROENTERITIS GUIDEDocumento54 pagineACUTE GASTROENTERITIS GUIDEVincent LaranjoNessuna valutazione finora
- Typhoid Fever Pathogenesis and TreatmentDocumento71 pagineTyphoid Fever Pathogenesis and TreatmentDionisius KevinNessuna valutazione finora
- Gastroenteritis in Adults and Older Children: EpidemiologyDocumento4 pagineGastroenteritis in Adults and Older Children: Epidemiologyjotq19Nessuna valutazione finora
- 2 Feco-Oral DiseaseDocumento44 pagine2 Feco-Oral DiseaseAyro Business CenterNessuna valutazione finora
- Bibliography: NCERT - TextbookDocumento10 pagineBibliography: NCERT - TextbookjothiNessuna valutazione finora
- ShigellosisDocumento14 pagineShigellosisMuhammad GetsoNessuna valutazione finora
- Typhoid FeverDocumento15 pagineTyphoid FeverCherry Ann DomingoNessuna valutazione finora
- Gastroenteritis: Saima Alam AfridiDocumento23 pagineGastroenteritis: Saima Alam AfridiMahnoor ParvezNessuna valutazione finora
- L15 SalmonellaDocumento19 pagineL15 SalmonellaMohammed RedhaNessuna valutazione finora
- Typhoid Fever: Causes, Symptoms, Diagnosis and TreatmentDocumento5 pagineTyphoid Fever: Causes, Symptoms, Diagnosis and TreatmentElvisNessuna valutazione finora
- A Sacrifice to Become A Doctor: 18-Year-Old Student's Medical StruggleDocumento47 pagineA Sacrifice to Become A Doctor: 18-Year-Old Student's Medical StruggleEric RicardoNessuna valutazione finora
- Slide ThyphoidDocumento24 pagineSlide Thyphoidbanana boatNessuna valutazione finora
- Typhoid Fever: by Dr. Bambang SN, SP - PD Department of Internal Medicine, General Hospital of Dr. Soedarso, PontianakDocumento32 pagineTyphoid Fever: by Dr. Bambang SN, SP - PD Department of Internal Medicine, General Hospital of Dr. Soedarso, PontianakTriponiaNessuna valutazione finora
- Junior Intern Review - Oral Revalida 2016Documento170 pagineJunior Intern Review - Oral Revalida 2016Cyrus ZalameaNessuna valutazione finora
- Typhoid fever symptoms and treatmentDocumento13 pagineTyphoid fever symptoms and treatmentshazea shafiqNessuna valutazione finora
- Pa Tho Physiology of Typhoid Fever and Acute GastroenteritisDocumento4 paginePa Tho Physiology of Typhoid Fever and Acute GastroenteritisJade Fatima D. CaymoNessuna valutazione finora
- Top 10 leading causes of morbidity & mortality in the Philippines in 2007Documento7 pagineTop 10 leading causes of morbidity & mortality in the Philippines in 2007Raisa Robelle Quicho100% (1)
- Surgical Complication of Typhoid FeverDocumento10 pagineSurgical Complication of Typhoid FeverHelsa Eldatarina JNessuna valutazione finora
- Enteric Fever ADNAN SARWARDocumento36 pagineEnteric Fever ADNAN SARWARDr-Adnan Sarwar ChaudharyNessuna valutazione finora
- Typhoid Fever: Also Known As Enteric FeverDocumento3 pagineTyphoid Fever: Also Known As Enteric Feverchristian quiaoitNessuna valutazione finora
- Referat Demam TifoidDocumento30 pagineReferat Demam TifoidBening IrhamnaNessuna valutazione finora
- Acute Febrile IllnessesDocumento54 pagineAcute Febrile IllnessesfraolNessuna valutazione finora
- GERMAN MEASLES and HEPATITISDocumento51 pagineGERMAN MEASLES and HEPATITISatienza02Nessuna valutazione finora
- Epidemiology Case ReportDocumento5 pagineEpidemiology Case Reportbeia21Nessuna valutazione finora
- Gi InfectionDocumento28 pagineGi Infectionmohamed hanyNessuna valutazione finora
- Typhoid and Dengue PPT by Shefali RanaDocumento47 pagineTyphoid and Dengue PPT by Shefali RanariyaNessuna valutazione finora
- Typhoid FeverDocumento4 pagineTyphoid FeverBernice GyapongNessuna valutazione finora
- Typhoid Fever (Enteric Fever)Documento24 pagineTyphoid Fever (Enteric Fever)Liza Marie Cayetano AdarneNessuna valutazione finora
- Typhoid Fever Diagnosis and TreatmentDocumento52 pagineTyphoid Fever Diagnosis and TreatmentOsama HassanNessuna valutazione finora
- Canine Parvovirus: Everything You Need to KnowDa EverandCanine Parvovirus: Everything You Need to KnowNessuna valutazione finora
- Problem 2: By: Varla S. G (405090215)Documento122 pagineProblem 2: By: Varla S. G (405090215)varlavarleyNessuna valutazione finora
- DiareDocumento50 pagineDiarevarlavarleyNessuna valutazione finora
- Bradikardi, AcsDocumento101 pagineBradikardi, AcsvarlavarleyNessuna valutazione finora
- Status EpileptikusDocumento93 pagineStatus EpileptikusvarlavarleyNessuna valutazione finora
- AscitesDocumento16 pagineAscitessaowaneejing1580Nessuna valutazione finora
- Problem 3 - VarlaDocumento75 pagineProblem 3 - VarlavarlavarleyNessuna valutazione finora
- Bradikardi, AcsDocumento101 pagineBradikardi, AcsvarlavarleyNessuna valutazione finora
- Bradikardi, AcsDocumento101 pagineBradikardi, AcsvarlavarleyNessuna valutazione finora
- Non Fatty LiverDocumento3 pagineNon Fatty LivervarlavarleyNessuna valutazione finora
- PROBLEM 4A - VarlaDocumento126 paginePROBLEM 4A - VarlavarlavarleyNessuna valutazione finora
- Problem 5B - VarlaDocumento54 pagineProblem 5B - VarlavarlavarleyNessuna valutazione finora
- Problem 1a - VarlaDocumento121 pagineProblem 1a - VarlavarlavarleyNessuna valutazione finora
- PROBLEM 2B - VarlaDocumento50 paginePROBLEM 2B - VarlavarlavarleyNessuna valutazione finora
- Salus Silver TSL2 - FormattedDocumento52 pagineSalus Silver TSL2 - Formattedhilajo1363Nessuna valutazione finora
- Case Conference: Pediatric Community Acquired PneumoniaDocumento46 pagineCase Conference: Pediatric Community Acquired PneumoniaElaine Francisse TampusNessuna valutazione finora
- MCCD Training ModuleDocumento90 pagineMCCD Training ModuleAashish PatniNessuna valutazione finora
- Nasima Akter, AMR Chowdhury NM KaziDocumento36 pagineNasima Akter, AMR Chowdhury NM KaziRoy Dip. SNessuna valutazione finora
- Innovation at 3M - Group 3 - B2BDocumento21 pagineInnovation at 3M - Group 3 - B2BRituraj BaruahNessuna valutazione finora
- Case of LeptospirosisDocumento60 pagineCase of LeptospirosisNoreen Cala-MayubayNessuna valutazione finora
- (Articulo) Epidemiologia - Modelling Plant Diseases EpidemicsDocumento14 pagine(Articulo) Epidemiologia - Modelling Plant Diseases EpidemicsFernanda PenagosNessuna valutazione finora
- The Math Behind The Virus' Dangerous Spread - Inquirer BusinessDocumento6 pagineThe Math Behind The Virus' Dangerous Spread - Inquirer BusinessFranchesca ValerioNessuna valutazione finora
- Contraindications To Air TravelDocumento15 pagineContraindications To Air TravelsDamnNessuna valutazione finora
- Poultry Diseases HandbookDocumento207 paginePoultry Diseases HandbookJose Ferreira100% (2)
- Causes and Prevention of Foodborne IllnessesDocumento1 paginaCauses and Prevention of Foodborne IllnessesSavior AlbertNessuna valutazione finora
- Gonorrhea Infection in Women: Prevalence, Effects, Screening, and ManagementDocumento12 pagineGonorrhea Infection in Women: Prevalence, Effects, Screening, and Managementilham hamkaNessuna valutazione finora
- Prevalence and Risk Factors of Puerperal Sepsisbamong Reproductive Aged Women at Jinja Regional Referral Hospital From January 2019 To June 2020Documento14 paginePrevalence and Risk Factors of Puerperal Sepsisbamong Reproductive Aged Women at Jinja Regional Referral Hospital From January 2019 To June 2020KIU PUBLICATION AND EXTENSIONNessuna valutazione finora
- Complications of Local AnaesthesiaDocumento35 pagineComplications of Local Anaesthesiaمحمد ربيعيNessuna valutazione finora
- 2017, 5 Anti Infeksi (Farmakologi Pada HIV-AIDS)Documento46 pagine2017, 5 Anti Infeksi (Farmakologi Pada HIV-AIDS)Jashmine RachlyNessuna valutazione finora
- COVID-19 Has Killed 5 Million People-And The Pandemic Is Far From OverDocumento16 pagineCOVID-19 Has Killed 5 Million People-And The Pandemic Is Far From OverLiar LiarNessuna valutazione finora
- GNM Nursing SyllabusDocumento97 pagineGNM Nursing SyllabusRavi RajanNessuna valutazione finora
- CytomegalovirusDocumento33 pagineCytomegalovirustummalapalli venkateswara raoNessuna valutazione finora
- Aseptic Technique in DentistryDocumento52 pagineAseptic Technique in Dentistrynew biee100% (1)
- Internal MedicineDocumento312 pagineInternal MedicineRoHIT ShowNessuna valutazione finora
- Diagnosing and Managing Tubercular MeningitisDocumento23 pagineDiagnosing and Managing Tubercular MeningitisAstie NomleniNessuna valutazione finora
- Desease Control On GoatsDocumento14 pagineDesease Control On Goats180006 RosmilahNessuna valutazione finora
- Treatment of Molluscum Contagiosum by Potassium Hy PDFDocumento12 pagineTreatment of Molluscum Contagiosum by Potassium Hy PDFKesuma YudhaNessuna valutazione finora
- Rapid Molecular Testing TBDocumento8 pagineRapid Molecular Testing TBNyonyo2ndlNessuna valutazione finora
- HowToFightCOVID19 DrAlexAndjaparidzeDocumento3 pagineHowToFightCOVID19 DrAlexAndjaparidzeAlex Andjaparidze100% (5)
- Detect Malaria ProtozoaDocumento81 pagineDetect Malaria ProtozoaMoses Tamba MomohNessuna valutazione finora
- WHO Health Definition 1JO Science ClassDocumento2 pagineWHO Health Definition 1JO Science ClassTCL SMART TVNessuna valutazione finora
- ECOLOGIC MODEL ANALYZES BRONCHIECTASISDocumento4 pagineECOLOGIC MODEL ANALYZES BRONCHIECTASISrodolfo opidoNessuna valutazione finora
- Infection Control BDADocumento15 pagineInfection Control BDAMariam WaseemNessuna valutazione finora
- Feline Calicivirus Upper Respiratory Disease DiagnosisDocumento2 pagineFeline Calicivirus Upper Respiratory Disease DiagnosisPetrisor GheorghiuNessuna valutazione finora