Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Atrial Fibrillation
Caricato da
varun_swm0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
190 visualizzazioni50 pagineAtrial fibrillation (AF) is the most common sustained arrhythmia affecting humans.
A detailed discussion of etiology,pathogenesis ,evaluation and treatment of atrial fibrillation.
Copyright
© © All Rights Reserved
Formati disponibili
PPTX, PDF, TXT o leggi online da Scribd
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoAtrial fibrillation (AF) is the most common sustained arrhythmia affecting humans.
A detailed discussion of etiology,pathogenesis ,evaluation and treatment of atrial fibrillation.
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato PPTX, PDF, TXT o leggi online su Scribd
0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
190 visualizzazioni50 pagineAtrial Fibrillation
Caricato da
varun_swmAtrial fibrillation (AF) is the most common sustained arrhythmia affecting humans.
A detailed discussion of etiology,pathogenesis ,evaluation and treatment of atrial fibrillation.
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato PPTX, PDF, TXT o leggi online su Scribd
Sei sulla pagina 1di 50
Annamalai University
Department of General Medicine
ATRIAL FIBRILLATION
Moderator Dr S.Sudharshan
Presentor-Dr M.Arun & Dr Varun s (M 5)
Date-2/8/2012
Introduction
An arrhythmia is a problem with the rate or rhythm of the
heartbeat.
Atrial fibrillation (AF) is the most common sustained
arrhythmia affecting humans.
It is marked by disorganized, rapid, and irregular atrial
activation
Classification
Paroxysmal - AF that terminates
spontaneously within 7 days
Persistent AF that present continuously for
more than 7 days
Longstanding - AF persistent for more than 1
year
Permanent - AF refractory to cardioversion
Lone - AF that occurs in patients younger
than 60 years who do not have
hypertension or any evidence of
structural heart disease
Causes
Hypertension
Coronary heart disease
Cardiomyopathy
Dilated
Hypertrophic
Mitral valve disease
Stenosis
Regurgitation
Thyrotoxicosis
Sick sinus syndrome
Congenital heart disease
Atrial septal defect
Ebstein's anomaly
Cardiac surgery
Pericarditis
Tumors
Alcohol
Lung disease
Neurogenic
Electric shock
Lone (idiopathic)
Causes
Paroxysmal Pericarditis, Alcohol, Cardiac surgery
Persistent - Coronary heart disease, Cardiomyopathy,
Mitral valve disease, Congenital heart disease
Permanent Cardiomyopathy, Mitral valve disease,
Congenital heart disease
Mechanism of AF
Initiating event - a premature atrial or
ventricular complex.
Sustaining substrate - one or more Reentrant circuits or
Automatic Focus .
The initiating event and sustaining substrate may be all due to
automaticity or reentry circuit.
Automatic Focus
The drivers appear to originate predominantly from
the atrialized musculature that enters the pulmonary
veins and represent either focal abnormal
automaticity or triggered firing
Microreentry Circuits
Sustained forms of microreentry as drivers
also have been documented
around the orifice of pulmonary veins;
nonpulmonary vein drivers also have
been demonstrated.
Symptoms of Atrial Fibrillation
The symptoms of AF vary widely between patients,
ranging from none to severe and functionally
disabling symptoms
The most common symptoms of AF are palpitations,
fatigue, dyspnea, effort intolerance, and
lightheadedness. Polyuria can occur because of
release of atrial natriuretic hormone.
Syncope is an uncommon symptom of AF, most often
caused by a long sinus pause on termination of AF in
a patient with the sick sinus syndrome.
Asymptomatic or minimally symptomatic AF patients
are not prompted to seek medical care and can
present with a complication of AF such as stroke or
CCF.
Physical examination
The hallmark of AF on physical examination is an irregularly
irregular pulse.
Short R-R intervals during AF do not allow adequate time for
left ventricular diastolic filling, resulting in a low stroke
volume and the absence of palpable peripheral pulse. This
results in a pulse deficit, during which the peripheral pulse is
not as rapid as the apical rate.
Other manifestations of AF on the physical examination are
irregular jugular venous pulsations and variable intensity of
the first heart sound.
Diagnostic Evaluation
Electrocardiographic Features
- Low-amplitude baseline oscillations (fibrillatory
or f waves)
- The f waves have a rate of 300 to 600 beats/min and
are variable in amplitude, shape, and timing.
- Irregularly irregular ventricular rhythm
- Atrial flutter (rate of 250 to 350 beats/min and are
constant in timing and morphology)
Comparison between the f waves of AF (top panel) and the
flutter waves of atrial flutter (bottom panel). f waves are variable
in rate, shape, and amplitude, whereas flutter waves are constant
in rate and all aspects of morphology.
A recording of AF with a rapid ventricular rate of 160 beats/min.
Shown are leads V
1
, II, and V
5
. On quick review, there may
appear to be a regular rate consistent with paroxysmal
supraventricular tachycardia. On closer inspection, it is clear that
the rate is irregularly irregular.
Holter recording
Patient who describes rapid palpitations suggestive of
paroxysmal AF, ambulatory monitoring is useful to
document whether AF is responsible for the symptoms
Echocardiography
Evaluate atrial size and left ventricular function and to
look for left ventricular hypertrophy, congenital heart
disease & valvular heart disease
A stress test
Appropriate for evaluation of ischemic heart disease in
at-risk patients
Laboratory testing should include thyroid function tests, liver
function tests.
Therapy of Atrial Fibrillation: General
Principles
Three potential therapeutic goals of treatment
- Restoration and maintenance of sinus rhythm,
- Rate control during AF,
- Prevention of thromboembolism
Restore sinus rhythm or Ventricular rate
control ?
Decision should be individual to each patient, based on
analysis of the risk benefit ratio for that individual.
Factors to consider are
- Severity of symptoms,
- Left atrial size,
- Patient age,
- Presence of cardiovascular disease or other medical
conditions,
- Pharmacologic and nonpharmacologic options
Severity of symptoms
- If patient is hemodynamically unstable or is in
severe cardiac failure, immediate
DC cardioversion aimed at restoring sinus rhythm
must be tried.
Left atrial size
- Patients with dilated left atrium are more prone to AF,
and these patients are more likely to remain in AF than
those with normal LA dimensions
- In these patients rate control is ideal
Patient age
For example, an elderly patient with minimal symptoms
and years of persistent AF is an ideal candidate for a
rate control and anticoagulation treatment strategy.
Alternatively, a young patient with very symptomatic
episodes of paroxysmal AF should be considered
initially for a rhythm control treatment strategy
Presence of cardiovascular disease or other medical
conditions
In patients with Permanent AF(Cardiomyopathy,
Mitral valve disease, Congenital heart disease) rate
control is preferred
AFFIRM TRIAL
The Atrial Fibrillation Follow-Up Investigation of Rhythm
Management (AFFIRM) trial was the largest trial which
compared difference in mortality between the rhythm and
rate control strategies in AF.
The mean follow-up in AFFIRM was 3.5 years; thus, only
short-term follow-up data are available.
There was no difference in mortality between the rhythm
and rate control strategies.
Thus, clinicians should individualize their approach and
select the treatment strategy that is best for each patient.
One important observation is that in patients at high risk for
stroke, long-term anticoagulation is required regardless of
whether a rhythm or rate control strategy is selected.
Two important decisions in acute AF
If cardioversion is decided on for a hemodynamically
stable patient who presents with AF that does not
appear to be self-limited, there are two management
decisions to be made: early versus delayed
cardioversion and pharmacologic versus electrical
cardioversion.
Early or Delayed Cardioversion ?
Duration of AF
Duration < 48 hrs
- Less chance of thromboembolism
- No need for anticoagulant before
cardioversion(chemical or DC) to restore sinus rhythm
Duration > 48 hrs
- Transesophagial echocardiography to rule out
Atrial thrombus.
- If thrombus present- anticoagulant for 3 weeks
before Cardioversion (chemical or DC) and
4 weeks following cardioversion.
Chemical cardioversion or DC cardioversion
for restoring rhythm ?
Pharmacologic cardioversion has these advantage
- Does not requiring general anesthesia or deep
sedation.
Disadvantages of pharmacological cardioversion
- Associated with the risk of adverse drug effects
- Not as effective as electrical cardioversion.
- Unlikely to be effective if the duration of AF is longer
than 7 days
AF
Hemodynamically
unstable
DC cardioversion
Hemodynamically
stable
Rhythm control
Rate control
< 48 hrs > 48 hrs
Rate control
drugs
Cardiovert
without
anticoagulant
TEE
Thrombus
present
Thromus
absent
3 weeks
anticoagulation
before cardioversion
Start anticoagulant
and cardiovert
Intravenous Agents to Restore Sinus Rhythm
Commonly used drugs are Ibutalide(60-70%),
Amiodarone (40-50%), procainamide(30-40%).
To minimize the risk of QT prolongation and polymorphic
ventricular tachycardia (torsades de pointes ), the use of
ibutilide should be limited to patients with an ejection fraction
>35%
Other drugs which can be also used are flecainide,
propafenone, and sotalol.
Oral Antiarrhythmic Agents for Restoration of
sinus rhythm
Acute pharmacologic cardioversion of AF also can be
attempted with orally administered drugs in patients without
structural heart disease.
The most commonly used oral agents for acute conversion of
AF are propafenone (300 to 600 mg) and flecainide (100 to
200 mg).
Oral agents for Maintenance of Sinus Rhythm
All of the available drugs except amiodarone have similar
efficacy and are associated with a 50% to 60% reduction in the
odds of recurrent AF during 1 year of treatment
Lone AF or minimal heart disease - flecainide, propafenone,
sotalol, and dronedarone are reasonable first-line drugs, and
amiodarone and dofetilide can be considered if the first-line
agents are ineffective or not tolerated.
In patients with substantial left ventricular hypertrophy, the
hypertrophy may heighten the risk of ventricular
proarrhythmia, and the safest choice for drug therapy is
amiodarone.
In patients with coronary artery disease, the safest first-line
options are dofetilide, sotalol, and dronedarone, with
amiodarone reserved for use as a second-line agent.
In patients with heart failure, several antiarrhythmic drugs
have been associated with increased mortality, and the only
two drugs known to have a neutral effect on survival are
amiodarone and dofetilide.
Drug having higher efficacy than the others is amiodarone.
However, because of the risk of organ toxicity, amiodarone is
not appropriate first-line drug therapy for most categories of
patients with AF.
Risk factors for proarrhythmia in patients on these drugs
include female gender, left ventricular dysfunction, and
hypokalemia.
Use of Drug Therapy to Control Ventricular
Rate
Drugs used to decrease conduction in the AV node are useful
in controlling ventricular rate in patients who have AF
It is very important to control ventricular rate, not only to
decrease symptoms, but also to prevent tachycardia-mediated
ventricular cardiomyopathy
Commenly used drugs are digitalis, beta blockers, calcium
channel antagonists, and amiodarone.
Beta blocker & Calcium channel blocker
-The first-line agents for rate control
- Preferred over digoxin for rate control in patients who
have not experienced heart failure.
- Adrenergic blockers are also recommended in
situations in which sympathetic tone is increased,
such as thyrotoxicosis
Digitalis
- Adequately control the rate at rest but often does not
provide adequate rate control during exertion.
- Its use is appropriate in patients with systolic heart
failure.
Amiodarone
- Less frequently used for rate control than the other
agents because of the risk of organ toxicity
associated with long-term therapy.
- Amiodarone may be an appropriate choice for rate
control if the other agents are not tolerated or are
ineffective.
Rate control in WPW syndrome
Use of agents that depress conduction over the accessory
pathway.
In the acute setting, intravenous procainamide and ibutilide
are the treatments of choice, unless the patient is unstable and
requires urgent electrical cardioversion.
The use of drugs such as digoxin, calcium channel blockers,
adrenergic blockers, and adenosine are contraindicated in this
situation as they do not block conduction over the accessory
pathway and may accelerate the ventricular response
Transthoracic Electrical Cardioversion
Many patient who has AF may be a candidate for transthoracic
DC cardioversion.
Certain characteristics predict poor success in maintenance of
sinus rhythm
- Mitral valve disease
- Very large left atrium
- Patients who have AF of relatively long duration
Antiarrhythmic drugs are frequently used to maintain sinus
rhythm in patients undergoing transthoracic direct current
(DC) cardioversion.
Drug therapy should be considered before use of
cardioversion in patients with long-standing AF (e.g., >3
months), to lessen the chance of early recurrence of AF in the
first few days after cardioversion
Prevention of Thromboembolism
Prevention of stroke is key to the management of the condition
of patients with AF
warfarin is highly effective in reducing the incidence of
ischemic stroke among patients with AF . Overall, a combined
risk reduction of 68% is seen.
Aspirin does not prevent thromboembolic complications as
effectively as warfarin in patients with AF
Catheter Ablation
Success rates of more than 95% are attainable when the
arrhythmia substrate is well defined, localized, and temporally
stable.
In contrast, the arrhythmia substrate of AF as yet is not well
understood, usually is widespread, is variable between patients,
and may be progressive.
AF may recur more than 2 or 3 years after an initially
successful ablation procedure.
Indications for catheter ablation
- Young patients(< 35 yrs) with symptomatic AF that is
affecting quality of life and that has not adequately
responded to drug therapy.
- The ideal candidate has lone AF or only minimal
structural heart disease(such as normal left atrial size)
- Patients with sinus node dysfunction in whom
antiarrhythmic drug therapy is likely to create the need
for a permanent pacemaker.
Surgical Approaches to Atrial Fibrillation
The most effective surgical procedure for AF is the cut-and-
sew maze procedure developed by Cox in 1987.
This operation involves 12 atrial incisions to isolate the
pulmonary veins and to create lines of block in the left atrium
and right atrium.
In addition, the left and right atria are excised.
Long-term freedom from AF after the Cox maze procedure has
been reported to range from 70% to 95%, but 10% to 35% of
patients still require antiarrhythmic drug therapy
The Cox maze procedure has not been widely performed
because it requires cardiopulmonary bypass, is technically
difficult, and is associated with a mortality risk of
approximately 1% to 2%.
References
Braunwald's Heart Disease, 9th Edition.
Topol Textbook of Cardiovascular Medicine, 3rd Edition.
Harrison's Principles of Internal Medicine, 18th Edition.
Annamalai university
Potrebbero piacerti anche
- BCSC Reading Schedule 2019-2020Documento11 pagineBCSC Reading Schedule 2019-2020Mari Martinez100% (1)
- DYSRHYTHMIAS (A.k.a. Arrhythmias) Disorders in TheDocumento3 pagineDYSRHYTHMIAS (A.k.a. Arrhythmias) Disorders in TheDarell M. Book100% (1)
- Innovation - Edipeel Prolongs Fruit Shelf Life, Reduces SpoilageDocumento5 pagineInnovation - Edipeel Prolongs Fruit Shelf Life, Reduces SpoilageahosfhaofahfouaNessuna valutazione finora
- Acute k9 Pain ScaleDocumento1 paginaAcute k9 Pain Scaleapi-367949035Nessuna valutazione finora
- En Anerkennung Abschluesse FinalDocumento2 pagineEn Anerkennung Abschluesse FinalKasim ButkovicNessuna valutazione finora
- Atrial Fibrillation HandoutDocumento5 pagineAtrial Fibrillation HandoutAlfa AlfinNessuna valutazione finora
- Mitral Valve Regurgitation, A Simple Guide To The Condition, Treatment And Related ConditionsDa EverandMitral Valve Regurgitation, A Simple Guide To The Condition, Treatment And Related ConditionsNessuna valutazione finora
- Update On (Approach To) Anemia1 (Changes)Documento39 pagineUpdate On (Approach To) Anemia1 (Changes)Balchand KukrejaNessuna valutazione finora
- Atrial Fibrillation: Presented by ShehzadiDocumento17 pagineAtrial Fibrillation: Presented by ShehzadisamNessuna valutazione finora
- Valvular Heart Disease 2Documento46 pagineValvular Heart Disease 2Topea BogdanNessuna valutazione finora
- Acute Stroke Management by Carlos L Chua PDFDocumento61 pagineAcute Stroke Management by Carlos L Chua PDFHynne Jhea EchavezNessuna valutazione finora
- CardiopathophysiologyDocumento63 pagineCardiopathophysiologyapplesncoreNessuna valutazione finora
- Cardiac Output and Hemodynamic MeasurementDocumento29 pagineCardiac Output and Hemodynamic Measurementdeepa100% (1)
- Seizures in ChildrenDocumento21 pagineSeizures in ChildrenTera SurbaktiNessuna valutazione finora
- Congenital Heart Disease - Cynotic AcynoticDocumento34 pagineCongenital Heart Disease - Cynotic Acynoticvruttika parmarNessuna valutazione finora
- Nur 111 Session 6 Sas 1Documento12 pagineNur 111 Session 6 Sas 1Zzimply Tri Sha UmaliNessuna valutazione finora
- Arterial Lines in PACU: Presented by Autum Jacobs RN, BSNDocumento34 pagineArterial Lines in PACU: Presented by Autum Jacobs RN, BSNinuko1212Nessuna valutazione finora
- Intra Aortic Balloon PumpDocumento5 pagineIntra Aortic Balloon PumpZainal 'babeh' Arifin100% (1)
- Rapid Sequence InductionDocumento8 pagineRapid Sequence InductionAngela Mitchelle NyanganNessuna valutazione finora
- Assessment of Right Ventricular FunctionDocumento41 pagineAssessment of Right Ventricular FunctionAditya MadhavpeddiNessuna valutazione finora
- Cardio-Vascular Disease: Mitral Stenosis & Mitral RegurgitationDocumento25 pagineCardio-Vascular Disease: Mitral Stenosis & Mitral Regurgitationyulia silviNessuna valutazione finora
- Abdominal Swelling + AscitesDocumento29 pagineAbdominal Swelling + AscitesDevina CiayadiNessuna valutazione finora
- Hypertensive Crisis: Megat Mohd Azman Bin AdzmiDocumento34 pagineHypertensive Crisis: Megat Mohd Azman Bin AdzmiMegat Mohd Azman AdzmiNessuna valutazione finora
- Ekg Panum or OsceDocumento69 pagineEkg Panum or OsceGladish RindraNessuna valutazione finora
- Acute Coronary Syndrome: Dr. H.M. Saifullah Napu, SPJP, FihaDocumento47 pagineAcute Coronary Syndrome: Dr. H.M. Saifullah Napu, SPJP, FihaJual Beli Promosi100% (1)
- Procedure For Patent Ductus Arteriosus (PDA) Device ClosureDocumento13 pagineProcedure For Patent Ductus Arteriosus (PDA) Device ClosurejaganjaggiNessuna valutazione finora
- Acyanotic Congenital Heart Disease: Left-to-Right Shunt LesionsDocumento51 pagineAcyanotic Congenital Heart Disease: Left-to-Right Shunt Lesionselsa prima putri100% (2)
- Avnrt AvrtDocumento21 pagineAvnrt AvrtRima Rovanne Wenas100% (1)
- Carotid Artery Disease ManagementDocumento2 pagineCarotid Artery Disease ManagementWendy EscalanteNessuna valutazione finora
- ECG Master Class-3Documento97 pagineECG Master Class-3Shohag ID CenterNessuna valutazione finora
- Left Ventricular Non-CompactionDocumento20 pagineLeft Ventricular Non-CompactionlawlietNessuna valutazione finora
- Cardiac Nursing II Study GuideDocumento6 pagineCardiac Nursing II Study GuiderunnermnNessuna valutazione finora
- Electrical Activity of The HeartDocumento156 pagineElectrical Activity of The HeartNIRANJANA SHALININessuna valutazione finora
- Valvular Heart DiseaseDocumento2 pagineValvular Heart DiseaseAnonymous TVk12eX4Nessuna valutazione finora
- Manage Stroke with Tests, Treatments & PreventionDocumento27 pagineManage Stroke with Tests, Treatments & PreventionHanif SumonNessuna valutazione finora
- ECG Basics: NG Jit BengDocumento38 pagineECG Basics: NG Jit BengNur Atiqah ZainalNessuna valutazione finora
- MVR CabgDocumento57 pagineMVR CabgRoshani sharmaNessuna valutazione finora
- Neonatal Meningitis Diagnosis and TreatmentDocumento10 pagineNeonatal Meningitis Diagnosis and TreatmentRana KhairunnisaNessuna valutazione finora
- Ventricular ArrhytmiaDocumento30 pagineVentricular ArrhytmiaIkhsan AmadeaNessuna valutazione finora
- Diabetic Ketoacidosis and Hyperosmolar Hyperglycaemic StateDocumento55 pagineDiabetic Ketoacidosis and Hyperosmolar Hyperglycaemic StateEva PrimanandaNessuna valutazione finora
- Myocardial Infarction Case Analysis: Symptoms, Causes, Diagnosis (MIDocumento76 pagineMyocardial Infarction Case Analysis: Symptoms, Causes, Diagnosis (MIIpeNessuna valutazione finora
- Unstable Angina, STEMI, NSTEMI Diagnosis and ManagementDocumento21 pagineUnstable Angina, STEMI, NSTEMI Diagnosis and ManagementNabil Mosharraf Hossain100% (2)
- CARDIOVASCULAR DISEASES: SIGNS, SYMPTOMS AND TREATMENT OF HEART FAILUREDocumento27 pagineCARDIOVASCULAR DISEASES: SIGNS, SYMPTOMS AND TREATMENT OF HEART FAILURESanthoshi Sadhanaa SankarNessuna valutazione finora
- Hypertrophic CardiomyopathyDocumento57 pagineHypertrophic CardiomyopathycynNessuna valutazione finora
- Cardiac MedicationsDocumento8 pagineCardiac Medicationsangeline totaram100% (2)
- A Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsDa EverandA Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsNessuna valutazione finora
- Aortic Regurgitation CaseDocumento38 pagineAortic Regurgitation CaseIka MagfirahNessuna valutazione finora
- Types and Management of Valvular Heart DiseaseDocumento60 pagineTypes and Management of Valvular Heart DiseaseIntan Kumalasari RambeNessuna valutazione finora
- Spectrum of Acute Coronary Syndrome: Milagros Estrada-Yamamoto, MDDocumento62 pagineSpectrum of Acute Coronary Syndrome: Milagros Estrada-Yamamoto, MDAnonymous HH3c17osNessuna valutazione finora
- Small Bowel Obstruction - Clinical Diagnosis and TreatmentDocumento11 pagineSmall Bowel Obstruction - Clinical Diagnosis and TreatmentVigariooNessuna valutazione finora
- Atrial Flutter: The Lancet Carotid Sinus MassageDocumento3 pagineAtrial Flutter: The Lancet Carotid Sinus Massageyosi rizalNessuna valutazione finora
- Acute Coronary SyndromeDocumento18 pagineAcute Coronary SyndromeKartika RahmawatiNessuna valutazione finora
- Chest X Ray Normal, Abnormal Views, and InterpretationDocumento57 pagineChest X Ray Normal, Abnormal Views, and InterpretationNina YuliNessuna valutazione finora
- Open Heart 2Documento11 pagineOpen Heart 2mohamedNessuna valutazione finora
- Esophageal Varices Week 4 T2T3Documento37 pagineEsophageal Varices Week 4 T2T3liewhuilianNessuna valutazione finora
- Rhythm Packet: Normal ECG CriteriaDocumento19 pagineRhythm Packet: Normal ECG CriteriaRegina MithaNessuna valutazione finora
- CCPACatheter Basics 07 MedicineDocumento44 pagineCCPACatheter Basics 07 MedicinerinbijoyNessuna valutazione finora
- Preload and AfterloadDocumento4 paginePreload and AfterloadNeranga SamaratungeNessuna valutazione finora
- SurgeryDocumento12 pagineSurgeryManusheeNessuna valutazione finora
- S1M3 Update Fluid Resuscitation Management in Emergency CasesDocumento70 pagineS1M3 Update Fluid Resuscitation Management in Emergency Casesgriya medicaNessuna valutazione finora
- Valvular Heart Disease To TW FinalDocumento13 pagineValvular Heart Disease To TW FinalMohammed ElSayedNessuna valutazione finora
- Shock ManagementDocumento26 pagineShock ManagementMuhammad Irfanuddin Bin IbrahimNessuna valutazione finora
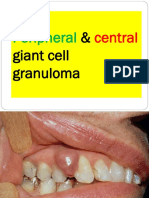
- Peripheral Central Giant Cell Granuloma NXPowerLiteDocumento18 paginePeripheral Central Giant Cell Granuloma NXPowerLiteAFREEN SADAF100% (1)
- The Effectiveness of Community-Based Rehabilitation Programs For Person Who Use Drugs (PWUD) : Perspectives of Rehabilitation Care Workers in IloiloDocumento27 pagineThe Effectiveness of Community-Based Rehabilitation Programs For Person Who Use Drugs (PWUD) : Perspectives of Rehabilitation Care Workers in IloiloErikah Eirah BeloriaNessuna valutazione finora
- Radiation Protection 2018Documento213 pagineRadiation Protection 2018Ricardo EdanoNessuna valutazione finora
- Kerry Washington. Family Secret.Documento3 pagineKerry Washington. Family Secret.yulya.shevchenko110Nessuna valutazione finora
- Antioxidant and Stability of Dragon Fruit Peel ColourDocumento3 pagineAntioxidant and Stability of Dragon Fruit Peel ColourPatricia VellanoNessuna valutazione finora
- Sendai Framework For Disaster Risk ReductionDocumento34 pagineSendai Framework For Disaster Risk ReductionDavid GarciaNessuna valutazione finora
- Hand Injuries & Their ManagementsDocumento78 pagineHand Injuries & Their ManagementsKuruNessuna valutazione finora
- EpididymitisDocumento8 pagineEpididymitisShafira WidiaNessuna valutazione finora
- Introduction To Psychology BrochureDocumento2 pagineIntroduction To Psychology BrochureErika JimenezNessuna valutazione finora
- Safety Data Sheet SummaryDocumento8 pagineSafety Data Sheet SummaryReffi Allifyanto Rizki DharmawamNessuna valutazione finora
- The Child Bipolar QuestionnaireDocumento10 pagineThe Child Bipolar QuestionnairefranciscatomiNessuna valutazione finora
- ManeuversDocumento16 pagineManeuversCezar-George BadaleNessuna valutazione finora
- Endocervical PolypDocumento2 pagineEndocervical PolypRez007Nessuna valutazione finora
- Penlon Prima 451 MRI Anaesthetic Machine: Anaesthesia SolutionsDocumento4 paginePenlon Prima 451 MRI Anaesthetic Machine: Anaesthesia SolutionsJuliana Jaramillo LedesNessuna valutazione finora
- Assessmen Ttool - Student AssessmentDocumento5 pagineAssessmen Ttool - Student AssessmentsachiNessuna valutazione finora
- Service Manual OPV-1500 NKDocumento109 pagineService Manual OPV-1500 NKIsabella Leal TobarNessuna valutazione finora
- Senior Counsel or Associate General Counsel or Assistant GeneralDocumento3 pagineSenior Counsel or Associate General Counsel or Assistant Generalapi-76922317Nessuna valutazione finora
- Nematode EggsDocumento5 pagineNematode EggsEmilia Antonia Salinas TapiaNessuna valutazione finora
- Kasaj2018 Definition of Gingival Recession and Anaromical ConsiderationsDocumento10 pagineKasaj2018 Definition of Gingival Recession and Anaromical ConsiderationsAna Maria Montoya GomezNessuna valutazione finora
- Phenol Hazards and PrecautionsDocumento3 paginePhenol Hazards and PrecautionsMarnel Roy MayorNessuna valutazione finora
- ESHRE IVF Labs Guideline 15122015 FINALDocumento30 pagineESHRE IVF Labs Guideline 15122015 FINALpolygone100% (1)
- Ayurveda Medical Officer 7.10.13Documento3 pagineAyurveda Medical Officer 7.10.13Kirankumar MutnaliNessuna valutazione finora
- Secrets of AntimonyDocumento9 pagineSecrets of AntimonyNCSASTRONessuna valutazione finora
- Dementia Rating ScaleDocumento2 pagineDementia Rating ScaleIqbal BaryarNessuna valutazione finora
- UntitledDocumento19 pagineUntitledAnna S. LatipNessuna valutazione finora
- Sulphonamides: A Pharmaceutical ReviewDocumento3 pagineSulphonamides: A Pharmaceutical ReviewinventionjournalsNessuna valutazione finora