Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Clostridium Difficile Epidemiology
Caricato da
Isha BhattDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Clostridium Difficile Epidemiology
Caricato da
Isha BhattCopyright:
Formati disponibili
Clostridium difficile
I SHA BHATT
DEPARTMENT OF EPI DEMI OLOGY AND BI OSTATISTICS
DREXEL UNI VERSI TY SCHOOL OF PUBLI C HEALTH
MAY, 2014
Overview
Clinical context and terminology
Microbiology
Pathogenesis and reservoirs
Disease definition, syndromes , outcomes
Diagnosis and treatment
Surveillance and prevention strategies
Impact
History :
First cases of C.diff infections reported as far back as 1890s
First isolated in the stools of infants and described by Hall and
OToole in 1935 as Bacillus difficile.
In 1978, Bartlett et al, demonstrated a link between C.diff toxins and
cases of pseudomembranous colitis after antibiotic use.
The years 2003 2005 saw several outbreaks in Canada and United
Kingdom
2004 First International Clostridium difficile symposium(FICDS)
Microbiolo
gy
Gram positive
Motile ,obligate
anaerobe
Spore and Toxin
producing
Normal gut flora
especially in
infants and
elderly
Multiple strains
Also known as
C.diff
Source: http://www.bioquell.com/technology/microbiology/clostridium-difficile/
Culture : Isolation Media
CCFA: first proposed
BA with lysed horse blood:
Opaque grey-white colonies
TCCFA: Enhances sporulation
CDMN Selective Agar: C.
difficile grows better
Buchanens broth
Terminology:
Antibiotic-associated diarrhea : C.diff is only one of the etiologic
factors (10%-25%). Others include MRSA, Klebsiella, E.coli infections
Clostridium difficile infections (CDI) : diarrhea associated with
positive stool culture and toxin assays
Clostridium difficile associated diarrhea (CDAD): used
interchangeably with CDI.
Pseudomembranous colitis: fulminant CDI, severe and often fatal.
Confirmed endoscopically
Toxic megacolon: also diagnosed by CT and endoscopy. May lead to
perforation and death
Reservoir :
~2% normal adult gut flora
10 70% colonization in newborns and infants (50%)
Exogenous reservoir : animals feces
Spores : highly resistant to destruction and disinfection
Most acquired disease causing strains are in hospital settings and
through HCW hands
Increased colonization rates in hospitalized patients or those in long-
term care facilities after antibiotic exposure (10- 25 %)
Risk Factors :
Patients in hospitals and long-term care facilities
Exposure to antibiotics
Elderly
Children >1 year
Peripartum women
History of Inflammatory bowel diseases
Antibiotics implicated :
High Frequency Medium frequency Low Frequency
Ampicillin Erythromycin Chloramphenicol
Amoxicillin Other macrolides Metronidazole
Clindamycin Sulphonamides Rifampin
Fluoroquinolones Tetracyclines
Cephalosporins Vancomycin
Transmission:
Primary mode of transmission:
Fecal-Oral route
Direct contact: Hands of health
care workers
Patient to patient transmission
Family and/or visitor introduction
Asymptomatic carriers
Indirect transmission via fomites
Procedural transmission:
through improperly sterilized
rectal thermometers and
endoscopic tubes and intubation
CDI : Symptoms
CDI have a wide range of clinical presentation
Ingestion of C.diff may lead to excretion or asymptomatic
colonization of healthy individuals
Manifested disease may be mild, moderate to severe with
life-threatening consequences
Relapses are not uncommon in healthcare settings
Mild to Moderate cases Severe cases
Fever Pain, fever, diarrhea, increased WBCs
Abdominal pain Blood in stool
Diarrhea (>10 bowel movements
per day)
Electrolyte imbalance
Increased WBCs Paralytic ileus
Dehydration Toxic megacolon
Pseudomembranous colitis
Perforation
Death
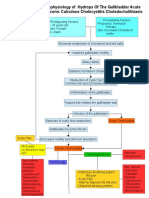
Pathogenesis:
Disruption of normal protective gut flora
Ingestion of spores and colonization of C.diff
Toxin production A and B
Damage to the cytoskeletal structures, loss of tight
junctions leading to mucosal injury , inflammation,
increased fluid secretion
Colitis and diarrhea
Onset and Progression :
Source: http://www.cdc.gov/HAI/pdfs/cdiff/Cohen-IDSA-SHEA-CDI-guidelines-2010.pdf
Course :
Onset usually >3 days - ~7 days
Latent period difficult to determine due to
asymptomatic carriers
Acute infection lasts for more than 10 days and
continues depending on severity and extent of
mucosal damage
Infection may progress to complete resolution ,
recurrence or in severe cases coma or death
Case definition: Incident
Presence of symptoms (usually diarrhea i.e >10 bowl
movements per day)
AND
Either Stool test result positive for C. difcile toxins or toxigenic
C. difcile
OR
or colonoscopic evidence of pseudomembranous colitis.
Source : http://www.cdc.gov/HAI/pdfs/cdiff/Cohen-IDSA-SHEA-CDI-guidelines-2010.pdf
Probable case: prompt to isolate
and test
Consider presumptive isolation for patients with > 3 unformed stools
within 24 hours
Send specimen for testing and presumptively isolate patient pending
results
Positive predictive value of testing will also be optimized if focused on
patients with >3 unformed stools within 24 hours
Exception: patient with possible recurrent CDI (isolate and test following
first unformed stool)
Source : CDC SHEA Guildelines, 2012
Diagnosis : Laboratory
Testing
Tissue Culture Cytotoxin Assay : Gold standard to identify toxin in fecal
samples in Vero cells
Toxigenic Culture
4-6 isolates to CMC
24 hr. filtrate for toxin detection ( fast )
Enzyme Immunoassay for toxin detection ( Toxin A and B )
Glutamate dehydrogenase detection : characteristic enzyme produced
by C.diff
PCR toxin gene detection, greater sensitivity and specificity
Limitations to Laboratory
testing:
Cytotoxin assays have low sensitivity and specificity
Stool culture time-consuming
GDH : risk of cross reaction
Recommendation for best predictive outcome :
-Screening for GDH
-Followed by culture for C.diff or EIA toxin assay
Radiologic testing : CT
Accordion Sign
evidence of
Pseudomembranous
colitis
Endoscopic Testing :
Colonoscopy
Evidence suggestive
of PMC
Treatment :
Discontinue the offending agent stop the antimicrobial
treatment !!
Start supportive treatment simultaneously : Fluid and
symptomatic treatment
If not resolved with conservative therapy Start oral
metronidazole for 10 days or Vancomycin
When both vancomycin and metronidazole fail : antibiotic
combination therapy
Newer treatment modalities
:
Probiotics efficacy undetermined
Fecal micro biota transplant : risk of transplanting
other pathogens
IV immunoglobulins passive immunization
especially for Immunocompromised
Surgical approach : in severe fulminant cases
resection of necrotic colon to prevent sepsis
New Antibiotic: Fidaxomycin
Prevention: Core
strategies
Judicious use of high potency antibiotics
Contact Precautions for duration of diarrhea
Hand hygiene in compliance with CDC/WHO
Cleaning and disinfection of equipment and environment
Laboratory-based alert system for immediate notification
of positive test results
Educate about CDI: HCP, housekeeping, administration,
patients, families
Source: http://www.cdc.gov/ncidod/dhqp/id_CdiffFAQ_HCP.html
Dubberke et al. Infect Control Hosp Epidemiol 2008;29:S81-92
Prevention: Supplemental
strategies
Extend use of Contact Precautions beyond duration of diarrhea (e.g.,
48 hours)
Presumptive isolation for symptomatic patients pending
confirmation of CDI
Evaluate and optimize testing for CDI : for faster and accurate
diagnosis
Implement soap and water for hand hygiene before exiting room of a
patient with CDI
Implement universal glove use on units with high CDI rates
Use sodium hypochlorite (bleach) for spores
CDI : Incidence and Epidemiology
(US)
Increased incidence (2.7 cases per
1,000 discharges in 1997 to 6.8 cases
per 1,000 discharges in 2001)
Increased severity (0.15 to 0.60 cases
per 1,000 discharges) of CDI
23% annual increase in CDI-related
hospitalizations between 2000 and
2005, associated with an increased
age-adjusted, annual case-fatality rate
of 0.2% over the study period
Changing trends and
causes:
The proportion of children with toxin-positive stool tests
increased from 46% in 2001 to 64% in 2006.
Prior to 1990, predominant strain was toxinotype
0/ribotype 001
Now: ribotype 027 (BI/NAP1/027) is associated with
increased virulence, mortality and morbidity
Increase incidence in previously considered non-high risk
groups
Surveillance :
To layout case definitions for Healthcare facility
acquired CDI and community acquired CDI
Use these as universal guidelines to survey the
disease in populations across the country and the
world
Devise prevention strategies to curb the epidemic
Surveillance and
reporting :
EIP : Emerging Infections program - surveillance
representative of the whole country.
NHSN : National Healthcare Safety Network data
entered from hospitals
HHS Action Plan : targets towards reducing HAIs
including CDI
Impact on Health care :
CDI may have resulted in $4.8 billion in
excess costs in US acute-care facilities
Per person cost increases by $2000- $7000
due to prolonged hospital stay and
additional testing
Increased risk of recurrence
Global impact
New MRSA
Similar increase in CDI worldwide across North America,
Europe and Asia
New strain in Asia O17 in addition to O27
Globally difficult surveillance : no universal case
definitions, diagnostic gold standards, inadequate data
reporting ad collection
Ongoing research and cumulative efforts to combat CDI
References :
Bartlett, J. G., & Gerding, D. N. (2008). Clinical recognition and diagnosis of clostridium difficile
infection. Clinical Infectious Diseases, 46(Supplement 1), S12-S18. doi:10.1086/521863
Centers for Disease Control and Prevention (CDC). (2012). Vital signs: Preventing clostridium difficile
infections.MMWR.Morbidity and Mortality Weekly Report, 61(9), 157-162. doi:mm6109a3 [pii]
Cohen, S. H., Gerding, D. N., Johnson, S., Kelly, C. P., Loo, V. G., L Clifford McDonald, M., . . . Wilcox, M.
H. (2010). Clinical practice guidelines for clostridium difficile infection in adults: 2010 update by the
society for healthcare epidemiology of america (SHEA) and the infectious diseases society of america
(IDSA).Infection Control and Hospital Epidemiology, 31(5), 431-455.
HALL, I. C., & O'TOOLE, E. (1935). Intestinal flora in new-born infantswith a description of a new
pathogenic anaerobe, bacillus difficilis. American Journal of Diseases of Children,49(2), 390-402.
Kelly, C. P., & LaMont, J. T. (2008). Clostridium difficilemore difficult than ever. New England Journal
of Medicine, 359(18), 1932-1940.
L Clifford McDonald, M., Coignard, B., Dubberke, E., Song, X., Horan, T., Kutty, P. K., & Ad Hoc
Clostridium difficile Surveillance Working Group. (2007). Recommendations for surveillance of
clostridium difficileassociated disease.Infection Control and Hospital Epidemiology, 28(2), 140-145.
Lessa, F. C., Gould, C. V., & McDonald, L. C. (2012). Current status of clostridium difficile infection
epidemiology. Clinical Infectious Diseases : An Official Publication of the Infectious Diseases Society of
America, 55 Suppl 2, S65-70. doi:10.1093/cid/cis319 [doi]
Thank you
Potrebbero piacerti anche
- Blood CultureDocumento22 pagineBlood CulturepawchanNessuna valutazione finora
- How To Treat: Septic ShockDocumento6 pagineHow To Treat: Septic ShockmeeandsoeNessuna valutazione finora
- Incidence and Prevalence PDFDocumento9 pagineIncidence and Prevalence PDFSreya SanilNessuna valutazione finora
- Retinopathy of PrematurityDocumento27 pagineRetinopathy of PrematurityTeoness JoyNessuna valutazione finora
- Standards of Care in Diabetes - 2024Documento9 pagineStandards of Care in Diabetes - 2024josueraulbalandranNessuna valutazione finora
- Secondary ImmunodeficiencyDocumento13 pagineSecondary ImmunodeficiencytanyagargNessuna valutazione finora
- Bladder and Bowel ManagementsDocumento26 pagineBladder and Bowel ManagementsDRKNessuna valutazione finora
- Pathophysiology of CholecystitisDocumento2 paginePathophysiology of CholecystitisAnonymous gDp7y3Cl82% (22)
- Hodgkin's DiseaseDocumento58 pagineHodgkin's Diseasealibayaty1Nessuna valutazione finora
- Stem Cell TransplantationDocumento13 pagineStem Cell TransplantationMylls MondejarNessuna valutazione finora
- Nosocomial Infections: Dr. Tjatur Winarsanto SPPD RST Ciremai CirebonDocumento48 pagineNosocomial Infections: Dr. Tjatur Winarsanto SPPD RST Ciremai CirebonNovita Trilianty MagdalenaNessuna valutazione finora
- Normal Values - CBCDocumento4 pagineNormal Values - CBCMohammad Salah D. MacapantonNessuna valutazione finora
- Management of Tuberculosis: A guide for clinicians (eBook edition)Da EverandManagement of Tuberculosis: A guide for clinicians (eBook edition)Nessuna valutazione finora
- Acute Lymphocytic Leukemia: A Case Presentation by Nollen LaquianDocumento43 pagineAcute Lymphocytic Leukemia: A Case Presentation by Nollen LaquianMonica MoralesNessuna valutazione finora
- Bone Marrow TransplantDocumento8 pagineBone Marrow TransplantPSRI hospitalNessuna valutazione finora
- Pancytopenia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDa EverandPancytopenia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNessuna valutazione finora
- Collection of SpecimenDocumento35 pagineCollection of SpecimenRona Palomo100% (1)
- Case Study - HivDocumento10 pagineCase Study - HivJoycee BurtanogNessuna valutazione finora
- CholangitisDocumento15 pagineCholangitisFaye TanNessuna valutazione finora
- Dimension of Development: Health Awareness: Nstp-Cwts Chapter 6Documento8 pagineDimension of Development: Health Awareness: Nstp-Cwts Chapter 6Rika Mae100% (3)
- Transfusion Reaction and Coombs Test: Moderator:-Dr Sanjay Agrwal Presenter: - DR Pratima Singh PG Jr-1Documento33 pagineTransfusion Reaction and Coombs Test: Moderator:-Dr Sanjay Agrwal Presenter: - DR Pratima Singh PG Jr-1UmikaguptaNessuna valutazione finora
- Pathophysiology Septic ShockDocumento26 paginePathophysiology Septic ShockTinea Sycillia100% (1)
- Brain InfectionDocumento61 pagineBrain Infectionmanisha paikarayNessuna valutazione finora
- Hematologic SystemDocumento81 pagineHematologic Systemseigelystic100% (23)
- Transfusion Medicine All by Manno 2002Documento23 pagineTransfusion Medicine All by Manno 2002we445Nessuna valutazione finora
- Week1 - Intro-Infectious Disease EpidemiologyDocumento42 pagineWeek1 - Intro-Infectious Disease EpidemiologyLee da Don100% (1)
- Acinetobacter BaumanniiDocumento53 pagineAcinetobacter BaumanniiLaboratorium BorromeusNessuna valutazione finora
- MDRO PPT MarcDocumento24 pagineMDRO PPT MarcMarc Andrew100% (1)
- Final Exam 2013 Sample Epidemiology of Infectious DiseasesDocumento7 pagineFinal Exam 2013 Sample Epidemiology of Infectious DiseasesIsha Bhatt100% (1)
- Blood Transfusion Guidelines PDFDocumento21 pagineBlood Transfusion Guidelines PDFEmhemed Amer Tabib100% (2)
- Clostridium DifficileDocumento52 pagineClostridium DifficileAndrés Menéndez RojasNessuna valutazione finora
- Safe Handling Chemotherapy DrugsDocumento62 pagineSafe Handling Chemotherapy DrugsKaterina Georgiadi KalogianniNessuna valutazione finora
- Hanson Infectious Diseases - Anamneza I StatusDocumento33 pagineHanson Infectious Diseases - Anamneza I StatusSilvia KesegNessuna valutazione finora
- Group 1 Apolonio, Leizel, R. Corpuz Rolyn Mañalac Joelle Anne Señeres Loui AnneDocumento33 pagineGroup 1 Apolonio, Leizel, R. Corpuz Rolyn Mañalac Joelle Anne Señeres Loui AnneLeizel ApolonioNessuna valutazione finora
- Laboratory Hematology PracticeDa EverandLaboratory Hematology PracticeKandice Kottke-MarchantValutazione: 5 su 5 stelle5/5 (1)
- Nosocomial Infections - Dr. LindaDocumento30 pagineNosocomial Infections - Dr. LindaGeorge C. KasondaNessuna valutazione finora
- Haemophilus SPPDocumento109 pagineHaemophilus SPPJamie CañebaNessuna valutazione finora
- Nosocomial InfectionDocumento26 pagineNosocomial InfectionAhmad MohamedNessuna valutazione finora
- Concepts of Infection ControlDocumento61 pagineConcepts of Infection Controltummalapalli venkateswara rao100% (1)
- Nosocomial InfectionDocumento13 pagineNosocomial InfectionwabalyNessuna valutazione finora
- Acinetobacter BaumanniiDocumento12 pagineAcinetobacter BaumanniiGIST (Gujarat Institute of Science & Technology)Nessuna valutazione finora
- Problems in Bone Marrow PathologyDocumento29 pagineProblems in Bone Marrow PathologymaurocznNessuna valutazione finora
- Cep Halo SporinsDocumento19 pagineCep Halo SporinsStarlet Rhonadez Bito-onon OrielNessuna valutazione finora
- Blood Transfusion - Indications, Administration and Adverse Reactions PDFDocumento9 pagineBlood Transfusion - Indications, Administration and Adverse Reactions PDFStacey WoodsNessuna valutazione finora
- Viral Hepatitis PDFDocumento4 pagineViral Hepatitis PDFNina BracyNessuna valutazione finora
- Ethics in Healthcare Case ScenariosDocumento1 paginaEthics in Healthcare Case ScenariosA CNessuna valutazione finora
- Systemic Lupus Erythematosus (SLE)Documento39 pagineSystemic Lupus Erythematosus (SLE)Nadya SabrinaNessuna valutazione finora
- Leukemia (Partly)Documento9 pagineLeukemia (Partly)rukipatNessuna valutazione finora
- WHO Guidline On Development of Haemovigilance SystemDocumento19 pagineWHO Guidline On Development of Haemovigilance SystemRustiannaTumanggorNessuna valutazione finora
- Complications of CABGDocumento38 pagineComplications of CABGpriyathasanNessuna valutazione finora
- Tumor MarkersDocumento14 pagineTumor MarkersPatrick LizarondoNessuna valutazione finora
- Status Asthmaticus: Triwahju AstutiDocumento41 pagineStatus Asthmaticus: Triwahju AstutirianiNessuna valutazione finora
- In The Clinic - Acute PancreatitisDocumento16 pagineIn The Clinic - Acute PancreatitisSurapon Nochaiwong100% (1)
- Acute Lymphoid LeukemiaDocumento41 pagineAcute Lymphoid Leukemiaummi ulfahNessuna valutazione finora
- Febrile Neutropenia: Nontapak ThiangpakDocumento53 pagineFebrile Neutropenia: Nontapak ThiangpakRapid MedicineNessuna valutazione finora
- Pharmacology of The GITDocumento31 paginePharmacology of The GITmarviecute22Nessuna valutazione finora
- Questions For OSCE Exam - Model AnswersDocumento9 pagineQuestions For OSCE Exam - Model AnswersFarah FarahNessuna valutazione finora
- Oncologic EmergenciesDocumento32 pagineOncologic EmergenciesColleen BernilNessuna valutazione finora
- 12 Lower Female Genital Tract InfectionsDocumento42 pagine12 Lower Female Genital Tract InfectionsAwal Sher khanNessuna valutazione finora
- BacteriaDocumento168 pagineBacteriadenekeNessuna valutazione finora
- Blood Cell CountDocumento27 pagineBlood Cell CountDiane-Richie PezLoNessuna valutazione finora
- Culture and IdentificationDocumento4 pagineCulture and IdentificationDewa Denis100% (1)
- Cancer Risk FactorsDocumento44 pagineCancer Risk FactorsSalomo Galih NugrohoNessuna valutazione finora
- Guideline Antibiotic RationalDocumento35 pagineGuideline Antibiotic RationalIstianah EsNessuna valutazione finora
- Safe Blood: Purifying the Nations Blood Supply in the Age of ADa EverandSafe Blood: Purifying the Nations Blood Supply in the Age of ANessuna valutazione finora
- PBHL 625 Longitudinal Data Analysis - Fall 2014Documento3 paginePBHL 625 Longitudinal Data Analysis - Fall 2014Isha BhattNessuna valutazione finora
- Sasrtf For LDADocumento6 pagineSasrtf For LDAIsha BhattNessuna valutazione finora
- 02 ImmunizationDocumento4 pagine02 ImmunizationIsha BhattNessuna valutazione finora
- Contoh Soal Uji Kompetensi Keperawatan KomunitasDocumento39 pagineContoh Soal Uji Kompetensi Keperawatan KomunitasUmairohSetengahTiga67% (3)
- Doh DC 2018-0142Documento2 pagineDoh DC 2018-0142vanceNessuna valutazione finora
- Epidemiology Computational ModelsDocumento16 pagineEpidemiology Computational ModelsIbrahim Jynx FalamaNessuna valutazione finora
- Typhoid Fever: Presented by Sharlin MacalintalDocumento18 pagineTyphoid Fever: Presented by Sharlin MacalintalPaul JacksonNessuna valutazione finora
- TestresultDocumento2 pagineTestresultaasirNessuna valutazione finora
- New First Aid With BLS PresentationDocumento115 pagineNew First Aid With BLS PresentationSheena Mae MahinayNessuna valutazione finora
- Epidemiology AssignmentDocumento12 pagineEpidemiology AssignmentSagar ParajuliNessuna valutazione finora
- Chickenpox (Varicella) : Questions and Answers: Information About The Disease and VaccinesDocumento3 pagineChickenpox (Varicella) : Questions and Answers: Information About The Disease and VaccinesKailash NagarNessuna valutazione finora
- Innocent ResearchDocumento31 pagineInnocent ResearchInnocent njogopaNessuna valutazione finora
- Lung CarcinomaDocumento29 pagineLung Carcinomavinoedhnaidu_rajagopalNessuna valutazione finora
- Nutrients 11 00655Documento20 pagineNutrients 11 00655Ibtidau NiamilahNessuna valutazione finora
- Pengembangan Aplikasi Monitoring Penyakit Hipertensi Dan Diabetes Mellitus TerintegrasiDocumento15 paginePengembangan Aplikasi Monitoring Penyakit Hipertensi Dan Diabetes Mellitus TerintegrasiberiNessuna valutazione finora
- Anaerobic Bacteria QuizletDocumento6 pagineAnaerobic Bacteria QuizletReca Marie FRIASNessuna valutazione finora
- Evaluation of Microscopic HematuriaDocumento15 pagineEvaluation of Microscopic HematuriaAndi SusiloNessuna valutazione finora
- Framingham Heart Study PDFDocumento5 pagineFramingham Heart Study PDFCarlos Fernando RíosNessuna valutazione finora
- Dik Sakit PDFDocumento117 pagineDik Sakit PDFrisky royatinNessuna valutazione finora
- Sba #4 - STDSDocumento6 pagineSba #4 - STDSlucyNessuna valutazione finora
- NCP Knowledge DeficitDocumento2 pagineNCP Knowledge DeficitRainier IbarretaNessuna valutazione finora
- 5 Pengkajian Awal Medis & Keperawatan (RI)Documento2 pagine5 Pengkajian Awal Medis & Keperawatan (RI)nurkholilaNessuna valutazione finora
- Vaccine and ImmunityDocumento32 pagineVaccine and ImmunityAlona SangamNessuna valutazione finora
- Internal Medicine II II MidtermDocumento11 pagineInternal Medicine II II MidtermJerin XavierNessuna valutazione finora
- Tut 202 2018 S1Documento23 pagineTut 202 2018 S1Feroza AngamiaNessuna valutazione finora
- What Is DracunculiasisDocumento1 paginaWhat Is DracunculiasisSiti SyahirahNessuna valutazione finora
- CuesDocumento8 pagineCuesFloyd SevillaNessuna valutazione finora