Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Tatalaksana Hiponatremia, Hiperkalemia, Hipomagnesiemia
Caricato da
Udyani AgustinaDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Tatalaksana Hiponatremia, Hiperkalemia, Hipomagnesiemia
Caricato da
Udyani AgustinaCopyright:
Formati disponibili
Tatalaksana hiponatremia,
hiperkalemia, hipomagnesiemia
HIPONATREMIA
Hyponatremia (serum sodium less than 135 mEq/L) has
been reported in
50% of hospitalized patients with neurologic disorders ,
40% of hospitalized patients with acquired
immunodeficiency syndrome ,
5% of hospitalized elderly patients and
1% of postoperative patients .
Hyponatremic patients can have twice the mortality
rate of patients with a normal plasma sodium, but a
causal link is unproven
The management of hyponatremia is determined
by the state of the ECV (i.e., low, normal, or high)
and by the presence or absence of neurological
symptoms. Symptomatic hyponatremia requires
more aggressive corrective therapy than
asymptomatic hyponatremia. However, to limit
the risk of a demyelinating encephalopathy, the
rate of rise in plasma sodium should not exceed
0.5 mEq/L per hour and the final plasma sodium
concentration should not exceed 130 mEq/L .
The general management strategies based on the ECV are
as follows:
Low ECV: Infuse hypertonic saline (3% NaCl) in
symptomatic patients, and isotonic saline in
asymptomatic patients.
Normal ECV: Combine furosemide diuresis with
infusion of hypertonic saline in symptomatic patients,
or isotonic saline in asymptomatic patients.
High ECV: Use furosemide-induced diuresis in
asymptomatic patients. In symptomatic patients,
combine furosemide diuresis with judicious use of
hypertonic saline.
Sodium Replacement
When corrective therapy requires the infusion of isotonic
saline or hypertonic saline, the replacement therapy can be
guided by the calculated sodium deficit. This is determined
as follows (using a plasma sodium of 130 mEq/L as the
desired end-point of replacement therapy):
The normal TBW (in liters) is 60% of the lean body weight
(in kg) in men, and 50% of the lean body weight in women.
Thus, for a 60 kg woman with a plasma sodium of 120
mEq/L, the sodium deficit will be 0.5 60 (130 - 120)
= 300 mEq.
Because 3% sodium chloride contains 513 mEq of
sodium per liter, the volume of hypertonic saline
needed to correct a sodium deficit of 300 mEq will be
300/513 = 585 mL. Using a maximum rate of rise of 0.5
mEq/L per hour for the plasma sodium (to limit the risk
of a demyelinating encephalopathy), the sodium
concentration deficit of 10 mEq/L in the previous
example should be corrected over at least 20 hours.
Thus, the maximum rate of hypertonic fluid
administration will be 585/20 = 29 mL/hour. If isotonic
saline is used for sodium replacement, the
replacement volume will be 3.3 times the replacement
volume of the hypertonic 3% saline solution.
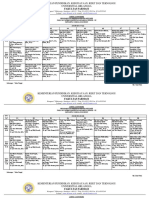
Tatalaksana hiperkalemia
Pemberian kalsium glukonas memiliki efek
meningkatkan kalsium ion, sehingga potensial
ambang terjadinya eksitasi listrik jantung
semakin negatif dan menghambat depolarisasi
yang ditimbulkan oleh hiperkalemia
(menstabilkan membran sel jantung). Cara
pemberiannya intravena secara perlahan
dengan monitor elektrokardiografi (EKG),
karena mempunyai efek kardiotoksik.
Pemberian insulin mempunyai efek
memindahkan kalium ekstrasel ke dalam sel,
sehingga menimbulkan gradien potensial
transmembran yang lebih fisiologis
(mendorong glukosa bersama kalium masuk
ke dalam sel). Pemberiannya bersamaan atau
tanpa glukosa harus dimonitor untuk
memantau terjadinya
hiperglikemia/hipoglikemia.
Pemberian 2 agonis melalui nebulizer (albuterol,
salbutamol) juga menimbulkan kemampuan
pengambilan kalium oleh sel.
Alkalinisasi cairan ekstraselular dengan natrium
bikarbonat juga dapat menimbulkan ambilan
kalium oleh sel (menurunkan ion hidrogen serum,
sehingga ion hidrogen keluar dari sel dan ion
kalium masuk ke dalam sel). Saat ini tidak terlalu
sering digunakan, kecuali jika terjadi asidosis
metabolik yang berperan dalam hiperkalemia.
Mekanisme
kerja
Obat dosis Cara pemberian Onset kerja Lama kerja
antagonis Kalsium
glukonas 10%
100mg/kg/x
(=1ml/kg/x)
Intravena dalam
3-5 menit
1-3 menit 30 menit
redistribusi Glukosa (25%)
(insulin)
0,5g/kg (=2
ml/kg) (regular
insulin, 0,1U/kg)
Iv dlm 15-30 mnt 30 mnt 2-4 jam
Albuterol (0,5%) 0,1-0,3 mg/kg
utk < 12 thn
Nebulisasi dlm
10 mnt
Dlm 30 mnt 4-6 jam
bicnat 1-2 mEq/jg Iv dlm 5-10 mnt 10-30 mnt 2 jam
Pembuangan furosemid 1-2 mg/kg Iv/im 15-30 mnt 4-6 jam
Natrium
poistiren
sulfonat resin
0,5-1 g/kg Oral/rektal 60-120 mnt 4-6 jam
HIPOMAGNESEMIA
Mild, Asymptomatic Hypomagnesemia
The following guidelines can be used for patients with
mild hypomagnesemia and no apparent complications :
Assume a total magnesium deficit of 1 to 2 mEq/kg.
Because 50% of the infused magnesium can be lost in
the urine, assume that the total magnesium
requirement is twice the magnesium deficit.
Replace 1 mEq/kg for the first 24 hours, and 0.5
mEq/kg daily for the next 3 to 5 days.
If the serum magnesium is greater than 1 mEq/L, oral
magnesium can be used for replacement therapy.
Moderate Hypomagnesemia
The following therapy is intended for patients
with a serum magnesium level less than 1 mEq/L
or when hypomagnesemia is accompanied by
other electrolyte abnormalities:
Add 6 g MgSO
4
(48 mEq Mg) to 250 or 500 mL
isotonic saline and infuse over 3 hours.
Follow with 5 g MgSO
4
(40 mEq Mg) in 250 or 500
mL isotonic saline infused over the next 6 hours.
Continue with 5 g MgSO
4
every 12 hours (by
continuous infusion) for the next 5 days
Life-Threatening Hypomagnesemia
When hypomagnesemia is associated with
serious cardiac arrhythmias (e.g., torsades de
pointes) or generalized seizures, do the following:
Infuse 2 g MgSO
4
(16 mEq Mg) intravenously over
25 minutes.
Follow with 5 g MgSO
4
(40 mEq Mg) in 250 or 500
mL isotonic saline infused over the next 6 hours.
Continue with 5 g MgSO
4
every 12 hours (by
continuous infusion) for the next 5 days.
Preparation Elemental Magnesium
Oral preparations:
Magnesium chloride enteric coated
tablets
64 mg (5.3 mEq)
Magnesium oxide tablets (400 mg) 241 mg (19.8 mEq)
Magnesium oxide tablets (140 mg) 85 mg (6.9 mEq)
Magnesium gluconate tablets (500 mg) 27 mg (2.3 mEq)
Parenteral solutions:
Magnesium sulfate (50%)* 500 mg/mL (4 mEq/mL)
Magnesium sulfate (12.5%) 120 mg/mL (1 mEq/mL)
*Should be diluted to a 20% solution for intravenous injection.
Potrebbero piacerti anche
- Practise Questions Keith & Moore 5th Edition - Should ReadDocumento113 paginePractise Questions Keith & Moore 5th Edition - Should ReadAmirsalar Eslami83% (6)
- Business Plan MriDocumento17 pagineBusiness Plan Mriapi-298975236100% (1)
- Perhitungan - Nutrisi Parenteral SortedDocumento50 paginePerhitungan - Nutrisi Parenteral Sortedtyazk100% (6)
- 3rd Annocement Mukernas Hisfarsi REV 181021Documento15 pagine3rd Annocement Mukernas Hisfarsi REV 181021ANA 1992100% (1)
- Klasifikasi Asma Gina 2015Documento34 pagineKlasifikasi Asma Gina 2015Roni Ardian100% (1)
- Perioperative Management OF Brain Trauma: Tatang Bisri Konsultan Neuroanestesi IDSAIDocumento52 paginePerioperative Management OF Brain Trauma: Tatang Bisri Konsultan Neuroanestesi IDSAIKimbek BuangkeNessuna valutazione finora
- Pomr (Problem Oriented Medical Record) : Cue and Clue PL Idx PDX PTX Pmo&EdDocumento4 paginePomr (Problem Oriented Medical Record) : Cue and Clue PL Idx PDX PTX Pmo&EdDoctoRides 46Nessuna valutazione finora
- 2016 10 12 Members Letter-HHS OCR Organ Transplant DiscriminationDocumento4 pagine2016 10 12 Members Letter-HHS OCR Organ Transplant DiscriminationMike Honda100% (2)
- NCP Ineffective Airway ClearanceDocumento1 paginaNCP Ineffective Airway ClearanceImation DataNessuna valutazione finora
- Jadwal Ujian Sidang Periode 112 TGL 26-27 Juni 2021 (Rev)Documento9 pagineJadwal Ujian Sidang Periode 112 TGL 26-27 Juni 2021 (Rev)Yohan Nafisa NetNessuna valutazione finora
- Diagnostik Dan Tatalaksana Stable CAD - CCSDocumento38 pagineDiagnostik Dan Tatalaksana Stable CAD - CCSIno HajrinNessuna valutazione finora
- Congestive Heart Failure (CHF) / Decompensation Cordis Functional Class (DCFCDocumento25 pagineCongestive Heart Failure (CHF) / Decompensation Cordis Functional Class (DCFCYUSRIL ZUMADINSYAHNessuna valutazione finora
- REFERAT Pendekatan Klinis PansitopeniaDocumento24 pagineREFERAT Pendekatan Klinis PansitopeniaYudhistira AdiNessuna valutazione finora
- Gambaran Histopatologi Hepatosit Tikus Putih Setelah Pemberian Jintan Hitam Dosis 500mgkgbb, 1000mgkgbb, Dan 1500mgkgbb Selama 21 Hari (Subkronik)Documento5 pagineGambaran Histopatologi Hepatosit Tikus Putih Setelah Pemberian Jintan Hitam Dosis 500mgkgbb, 1000mgkgbb, Dan 1500mgkgbb Selama 21 Hari (Subkronik)Mokhammad Faisol AbdullahNessuna valutazione finora
- Table Handling Obat IntravenaDocumento55 pagineTable Handling Obat IntravenaRegita AyuNessuna valutazione finora
- Informasi Obat Di Rumah SakitDocumento36 pagineInformasi Obat Di Rumah SakitSukeng Teazz50% (2)
- SPO High AlerTDocumento19 pagineSPO High AlerTHendraTriSaputroNessuna valutazione finora
- Daftar Obat High AlertDocumento3 pagineDaftar Obat High AlertLupus BoyssNessuna valutazione finora
- Obat Dan Kehamilan, Drugs, Aman Untuk Ibu Hamil, FarmasiDocumento13 pagineObat Dan Kehamilan, Drugs, Aman Untuk Ibu Hamil, FarmasifrankysukwendyNessuna valutazione finora
- Data Troli Depo FarmasiDocumento8 pagineData Troli Depo Farmasiizaura hanaNessuna valutazione finora
- Materi PP Aminofluid (Interna)Documento16 pagineMateri PP Aminofluid (Interna)ajieNessuna valutazione finora
- Adverse Drug ReactionDocumento4 pagineAdverse Drug ReactionRahmatulloh Al HusnaNessuna valutazione finora
- 10.preparasi TPN PDFDocumento36 pagine10.preparasi TPN PDFVini Insani RestuNessuna valutazione finora
- Farmakologi Obat Analgesik, Anti Piretik & Anti Inflamasi: Andri Tilaqza, M.Farm., AptDocumento45 pagineFarmakologi Obat Analgesik, Anti Piretik & Anti Inflamasi: Andri Tilaqza, M.Farm., AptDark BlueNessuna valutazione finora
- Diagnosis & Tata Laksana Cad / CcsDocumento40 pagineDiagnosis & Tata Laksana Cad / CcsIno HajrinNessuna valutazione finora
- Konsensus DM Perkeni 2006 PDFDocumento55 pagineKonsensus DM Perkeni 2006 PDFDenny LukasNessuna valutazione finora
- Farmakodinamik Obat Anti DiabetesDocumento24 pagineFarmakodinamik Obat Anti DiabetesAsma Somadayo100% (1)
- Pendekatan Evidence-Based Medicine Pada Manajemen Stroke Perdarahan IntraserebralDocumento6 paginePendekatan Evidence-Based Medicine Pada Manajemen Stroke Perdarahan IntraserebralArmiya MiaowNessuna valutazione finora
- Typhoid Management Guidelines - 2019 - MMIDSPDocumento14 pagineTyphoid Management Guidelines - 2019 - MMIDSPhasnah shintaNessuna valutazione finora
- Daftar Atc DDD Antibiotik Who 2018Documento12 pagineDaftar Atc DDD Antibiotik Who 2018APOTEKER RSUMMNessuna valutazione finora
- Daftar Harga Obat Asuransi 24Documento23 pagineDaftar Harga Obat Asuransi 24Widu Jalak SlpNessuna valutazione finora
- SP Sendo KF 122Documento5 pagineSP Sendo KF 122nurhadri azmiNessuna valutazione finora
- Asma Management 08 - 09 - 07Documento81 pagineAsma Management 08 - 09 - 07botolkecapNessuna valutazione finora
- Obat Wajib Apotek 1Documento4 pagineObat Wajib Apotek 1amelianuranti100% (1)
- Di, Siadh, CSW Tabel PerbedaanDocumento17 pagineDi, Siadh, CSW Tabel PerbedaanMichael Tambunan100% (1)
- 0812 Gelofusine PDFDocumento2 pagine0812 Gelofusine PDFMsglow WulanNessuna valutazione finora
- Daftar Obat ProlanisDocumento18 pagineDaftar Obat ProlanisMas EmNessuna valutazione finora
- SPGDT DISASTER MANAGEMENT PUSBANKES 118 (Compatibility Mode) PDFDocumento49 pagineSPGDT DISASTER MANAGEMENT PUSBANKES 118 (Compatibility Mode) PDFHari Mas KuncoroNessuna valutazione finora
- Daftar Persentase Obat TerdialisisDocumento1 paginaDaftar Persentase Obat Terdialisismazz.rianNessuna valutazione finora
- Hipertensi Emergensi (Herbesser)Documento41 pagineHipertensi Emergensi (Herbesser)riski novika100% (1)
- Ringkasan High Alert MedicationsDocumento8 pagineRingkasan High Alert MedicationsIsna MasrurohNessuna valutazione finora
- Rencana Distribusi Obat PuskesmasDocumento58 pagineRencana Distribusi Obat PuskesmasLita Rahma YulitaNessuna valutazione finora
- Protokol KemoDocumento13 pagineProtokol KemoVeysusanNessuna valutazione finora
- Target Range For Glycemic Control: 80-140 MG/DL (Generally 110 MG/DL)Documento3 pagineTarget Range For Glycemic Control: 80-140 MG/DL (Generally 110 MG/DL)Otchi Pudtrie Wijaya100% (1)
- Obat AntiaritmiaDocumento18 pagineObat AntiaritmiaWahyu JuliandaNessuna valutazione finora
- Kriteria Diagnosis RBBB - LBBBDocumento1 paginaKriteria Diagnosis RBBB - LBBBDwitya RiliantiNessuna valutazione finora
- Dosis Obat Igd PDFDocumento3 pagineDosis Obat Igd PDFRiyadila FajarizaNessuna valutazione finora
- Microgest InsertDocumento1 paginaMicrogest InsertChodhur BhodhurNessuna valutazione finora
- Dosis Ekuivalen Steroid PrednisoneDocumento2 pagineDosis Ekuivalen Steroid PrednisoneWisnu AdiputraNessuna valutazione finora
- Daun LeilemDocumento8 pagineDaun Leilemniken retnoNessuna valutazione finora
- Antibiotik Rasional Pada Demam TifoidDocumento35 pagineAntibiotik Rasional Pada Demam TifoidSelvi SulistianingsihNessuna valutazione finora
- CVP Guided Deresuscitation in Managing Overload in Icu PDFDocumento57 pagineCVP Guided Deresuscitation in Managing Overload in Icu PDFJonathan Hamm100% (1)
- Struma Nodulus Non ToksikDocumento32 pagineStruma Nodulus Non Toksikderahmat dedyNessuna valutazione finora
- Review Jurnal Interaksi Obat Antihipertensi - Radhwa Fauztina (20190350050)Documento13 pagineReview Jurnal Interaksi Obat Antihipertensi - Radhwa Fauztina (20190350050)Radhwa FauztinaNessuna valutazione finora
- Ensefalopati Uremikum Bu YantiDocumento16 pagineEnsefalopati Uremikum Bu YantiAnggi SetyariniNessuna valutazione finora
- Daftar Harga Buana Saraswati Bulan Agustus PDFDocumento57 pagineDaftar Harga Buana Saraswati Bulan Agustus PDFJasa Sunat JembranaNessuna valutazione finora
- NFCC. Chapter 8. ElectrolytesDocumento13 pagineNFCC. Chapter 8. ElectrolytesOsman fadilNessuna valutazione finora
- Magnesium Sulfa-WPS OfficeDocumento21 pagineMagnesium Sulfa-WPS OfficeNeha SinghNessuna valutazione finora
- Водно-электролитный балланс.Documento12 pagineВодно-электролитный балланс.misha202008Nessuna valutazione finora
- Management of Potassium Disorders 17706 ArticleDocumento4 pagineManagement of Potassium Disorders 17706 ArticlealeNessuna valutazione finora
- Potassium Disorders by AiyraDocumento25 paginePotassium Disorders by AiyraAnndrea IlhamNessuna valutazione finora
- HIPOMAGNESEMIADocumento11 pagineHIPOMAGNESEMIAInsan IlmanNessuna valutazione finora
- Anti Plate Let 2016Documento14 pagineAnti Plate Let 2016Desti Ratna PutriNessuna valutazione finora
- Pharmacy Guidelines 3Documento2 paginePharmacy Guidelines 3Inas IbrahimNessuna valutazione finora
- K Burns Qualitative Research PosterDocumento1 paginaK Burns Qualitative Research Posterapi-257576036Nessuna valutazione finora
- Kidney Disease Fact Sheet 3Documento2 pagineKidney Disease Fact Sheet 3Kristine Claire DizonNessuna valutazione finora
- Treatments For OsteoporosisDocumento2 pagineTreatments For Osteoporosisawaw90Nessuna valutazione finora
- The Art and Science of Cytology and Cytopathology Has Been Implemented and Recognized As Early As The 18thDocumento3 pagineThe Art and Science of Cytology and Cytopathology Has Been Implemented and Recognized As Early As The 18thphysiosyedNessuna valutazione finora
- Lecture 35 PptsDocumento41 pagineLecture 35 PptsMuhammad Burhan UllahNessuna valutazione finora
- Arjo Bed ManualDocumento32 pagineArjo Bed ManualAmàr AqmarNessuna valutazione finora
- Poor and Rich CountriesDocumento5 paginePoor and Rich Countriestwentyeight28Nessuna valutazione finora
- Medical Surgical Nursing QuestionsDocumento7 pagineMedical Surgical Nursing Questionseloisa mae gementizaNessuna valutazione finora
- Calvert Cognitive Analytic TherapyDocumento25 pagineCalvert Cognitive Analytic TherapyldelblancodiezNessuna valutazione finora
- Active and Passive Range of Motion Exercises.Documento16 pagineActive and Passive Range of Motion Exercises.Attila Tamas100% (1)
- The Healing Center of AsklepionDocumento4 pagineThe Healing Center of AsklepionVolkan VVolkan100% (1)
- Medsurg QuestionsDocumento12 pagineMedsurg QuestionsPatziedawn GonzalvoNessuna valutazione finora
- Clinical Research Overview DownloadDocumento13 pagineClinical Research Overview DownloadWILLIAM RICARDO CASTAÑEDA VARGASNessuna valutazione finora
- Pharmacology - Principles and Applications, 3rd EditionDocumento657 paginePharmacology - Principles and Applications, 3rd Editionserenesh67% (3)
- First Aid and CPR Training Providing Company ProfileDocumento11 pagineFirst Aid and CPR Training Providing Company ProfilemedicalserviceNessuna valutazione finora
- Normal Values of Vital SignsDocumento3 pagineNormal Values of Vital SignsMela VincoNessuna valutazione finora
- VS Documentation FinalDocumento30 pagineVS Documentation FinalRoger ViloNessuna valutazione finora
- Autism-Mind, Emotion, and The Spectrum of Autism - Dr. Dan SiegelDocumento2 pagineAutism-Mind, Emotion, and The Spectrum of Autism - Dr. Dan Siegelcinfer75Nessuna valutazione finora
- Edh PDFDocumento4 pagineEdh PDFRiska Rahmawati PratAmaNessuna valutazione finora
- Teaching Plan Assignment Template Assessment (These Are Possible Assessment Elements)Documento4 pagineTeaching Plan Assignment Template Assessment (These Are Possible Assessment Elements)api-402048659Nessuna valutazione finora
- CFR Leaflet 2016Documento2 pagineCFR Leaflet 2016api-321221901Nessuna valutazione finora
- Role of Physiotherapist in Neuro-RehabilitationDocumento3 pagineRole of Physiotherapist in Neuro-RehabilitationMohammad AkheelNessuna valutazione finora
- Ar 2007-2008Documento36 pagineAr 2007-2008Osu OphthalmologyNessuna valutazione finora
- KaizenDocumento13 pagineKaizenVlado RadicNessuna valutazione finora
- The Baldrige Criteria 101Documento6 pagineThe Baldrige Criteria 101Chantich Charmtong100% (1)
- Head and Neck and Endocrine Surgery From Clinical Presentation To Treatment Success 1st Ed 2016Documento400 pagineHead and Neck and Endocrine Surgery From Clinical Presentation To Treatment Success 1st Ed 2016Luan MatosNessuna valutazione finora