Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Trachy 121106090823 Phpapp02
Caricato da
Saya Menang0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
36 visualizzazioni46 pagineent
Titolo originale
trachy-121106090823-phpapp02
Copyright
© © All Rights Reserved
Formati disponibili
PPTX, PDF, TXT o leggi online da Scribd
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoent
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato PPTX, PDF, TXT o leggi online su Scribd
0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
36 visualizzazioni46 pagineTrachy 121106090823 Phpapp02
Caricato da
Saya Menangent
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato PPTX, PDF, TXT o leggi online su Scribd
Sei sulla pagina 1di 46
Tracheostomy
Upper and Lower Respiratory System
What is a tracheotomy?
its involves surgical creation of an external
opening through the 2
nd
and 3
rd
or 3
rd
and 4
th
ring of the trachea
A Tracheostomy can be
- Temporary,
- Permanent or
- placed during Emergency.
Cricothyrotomy
is an emergency tracheotomy that may
also be performed when endotracheal
intubation is impossible
Indications for Tracheostomy :
1. Airway Obstruction
Congenital
Ex: larynx hemangioma
Ex: Sub glottic or tracheal
stenosis,
Foreign body aspiration
Ex: Swallowed or inhaled
object lodged in upper airway
Infection
Ex: Acute epiglottitis,
It is an infection of the
epiglottis and
supraglottic
structures.
2. Airway Clearance:
clears the secretions that cannot be cleared due to
weakness and conditions requiring long term airway
support, like progressive neurological conditions such as:
Severe brain injury .ect
3.Long Term Intubation:
Long Term What is considered
Intubation for an adult and pediatric
patient???
Adult: Intubated more than two weeks.
Pediatric: Intubated more than 3-4 weeks.
4. Elective/Prophylactic
1- During major head and neck surgery
2- Radiation treatment
What physiological changes occur
with a tracheostomy???
temporary voice loss.
filtration, loss of the airborne particle
action of warming and humidification
. the nose
potential impairment of swallowing.
Mucociliary transport and cough
mechanisms are impaired.
IN 2 WAYS :
1-SURGICAL {OPEN (ST)}
(ENT) SURGEON, OR A THORACIC SURGEON.
2- PERCUTANEOUS PERCUTANEOUS DILATATION
TRACHEOSTOMY (PDT) IS DONE USING PERCUTANEOUS DILATATION
TECHNIQUE.
How is a Tracheostomy performed?
Surgical tracheostomy performed in
patients with:
1. Tumors of the upper airway
2. Previously failed/difficult percutaneous procedure
3. Major vascular structures at risk
4. Anatomical abnormality (e.g. goiters)
5. Short neck
6. Morbid obesity
7. Emergency airway
Goiters is a swelling of the thyroid gland, which can lead to a swelling of the neck or larynx (voice box)
Nursing Considerations
In (ST), the pt may come back with stay sutures
around the tube - to hold or manipulate the operating area.
In ST sutures are removed after the first
tracheostomy tube change - 5-7 days of the
insertion, while the stoma is forming or as
ordered by the operating surgeon.
stay sutures done:
to prevint accedint accidentally
dislodged.
Percutaneous
insertion:
The first tube change should
not be performed before 2
weeks of the initial insertion??
because the stoma is very tight
and the risk of the tracheotomy
collapsing is high.
Holistic Nursing Considerations
During the first 2-3 daysthe patient is
uncomfortable due to
trauma of surgery, pain of a fresh incision,
choking, presence of a foreign object in his
trachea and inability to communicate through
speech.
keep in mind .. the
patient is more than a
trach tube!
1- pain management.
2- reassurance.
3- education
What are the risks involved in
tracheostomy?
1-Reactions to medication and
anesthesia.
2-Uncontrollable bleeding.
3-Respiratory problems.
4-Possibility of cardiac arrest.
What are the complications of a
Tracheostomy?
Early ( Life-threatening ) Late
Infection :
1- stoma site
2- chest-
50-60% of tracheostomy patients may
develop nosocomial pneumonia
Skin breakdown
Tracheal stenosis
Tracheo-esophageal fistula :
1- Abdominal distention
2- Liquid food suctioned through
tracheostomy tube.
Accidental tube displacement
Blocked tracheostomy tube
Damage during surgery - possible
hemorrhage.
Sx emphysema
Trauma
Pneumothorax
What are the parts of the
tracheostomy tube?
Parts of Tracheostomy Tube
Main features Part
Main body of the tube Outer canula
A balloon at the distal end of the tube, provide
seal between the rachea & tube
cuff
External balloon connected to the inflation line to
the internal cuff ( vice versa)
Pilot balloon
Support the main tube structure.
Tube type, size & coude
Flange/ neck plate
Bevel, smooth rounded dilating tip tipped placed
inside the inner canula of the tube during insertion.
( reduce the risk of trauma ) removed once the
tube in correct placement
Introducer/ obturator
Allow attachment to ventilation equipment/ ambu-
bag
15 mm adaptor
Types of tracheostomy tubes
Single lumen:
- Larger inner diameter than double lumen
tube.
- Absence of removable inner cannula.
Double lumen:
- Removable inner cannula (twist-lock
connection ) prevent build up of secretion.
Cuffed t.t
contraindication indication
Child < 12 years old Risk of aspiration
Risk of tracheal tissue damage from cuff Newly formed stoma ( adult )
PPV
Unstable condition
Indication
cuffless cuff
No risk for aspiration Minemiz aspiration
Pt no longer need PPV Allow PPV ( one way valve )
Pt still need airway access Close system ( upper & lower airway )
Minemiz emphysema
Indication Close Suction System:
- Pt regyuireing Highy PEEP, Fio2
- TB, ARDS
- To Avoiding dramatic drop in oxygen.
Fenestration:
Single or multiple holes in the superior
curvature of the shaft of outer and inner
cannula.
Indication:
- Improve speech & swallowing function.
Occlusion cap:
Soolid piece of plasticc can be placed
on the end of a 15mm hub.
Indication :
Blocks all air flow via tracheostomy
(end stage weaning )
Humidification:
1- pt requiring oxygen with excessive
secretion/bedridden ( continuous \ ATM ) with need
to be labeled, dated and changed as per PP.
2- alert mobiles pt with minimal secretion ( HME )
change Q 24hr.
3- buchannan bib ( contains a special foam
(hydrolox) which act as filter & HME. Shoud by
Change/washed up to 3 uses only.
Nursing Considerations..
Condition of tracheostomy dressing wet/dry
Stoma site should be observed for:
- Bleeding
- Increase stoma size
- Appearance of stoma edges and tissue
( e.g. maceration, cellulites)
- Evidence of infection (purulent discharge, pain,
offensive odor, tenderness
- Allergic reaction to dressing product
- Tube secured to skin, ties are appropriately tight
- Patient on oxygen: TM T-piece, humidification
method.
Suctioning
Indications for Suctioning
if pt have one or more of the following :
Excessive secretions
Decreased oxygen saturations
Tachypnea , bradypnea or tachycardia
Restlessness, increased use of intercostal
muscles, or sweating
Noisy breath sounds/decreased breath
sound
Poor ineffective cough
Change in skin color from baseline
Reduced expired air flow from tube
during expiration
Collection of sputum specimens
Prior to section:
- hyperventelation
- hyperoxygenation
to Reduse Hypoxemia.
Caution:
COPD: patients should
only have 20% increase
of oxygenation.
Hyperventelation , will
be used for non-
spontaneous breather,
as it may have significant
adverse effects .
Ex: Reduced venous
return and barotraumas
Potential Complications of
Suctioning:
- Hypoxemia
- Hypotension
- Increased intracranial pressure
- Hyper/Hypoventilation
- Cardiac arrhythmias
- Increased work of breathing
- Bronchospasm
- Infection
- Accidental extubation/decannulation
- Cardiac Arrest
Famous People who was
tracheostomies
King Fahd bin Abdul Aziz Al Saud
(king of SA)
John Fitzgerald Kennedy (U.S. President)
Thank you
done by :
Marwah M.Ibrahim
Any Question
: References
- American Journal of Critical Care.
- Tracheostomy multiprofessional handbook (1ed
addition ).
- Critical Care Nurse.
- http://www.aurorahealthcare.org/yourhealth/health
gate/getcontent.asp?URLhealthgate=%2214874.html
%22
Potrebbero piacerti anche
- Physics PEKA Scoring Check ListDocumento2 paginePhysics PEKA Scoring Check ListSaya MenangNessuna valutazione finora
- Basketball Students Attendance List 2017 Dates Class 9/1 16/1 23/1 6/2 13/2 20/2 27/2 6/3 13/3 27/3 3/4 10/4 17/4 24/4Documento2 pagineBasketball Students Attendance List 2017 Dates Class 9/1 16/1 23/1 6/2 13/2 20/2 27/2 6/3 13/3 27/3 3/4 10/4 17/4 24/4Saya MenangNessuna valutazione finora
- Cerebellar ExaminationDocumento1 paginaCerebellar ExaminationSaya MenangNessuna valutazione finora
- Esa Waterpark D Weekday, Mon - Tue / Thu - Fri (Adult) : Ticket To Desa WaterparkDocumento1 paginaEsa Waterpark D Weekday, Mon - Tue / Thu - Fri (Adult) : Ticket To Desa WaterparkSaya MenangNessuna valutazione finora
- Rates of Reaction TestDocumento10 pagineRates of Reaction TestSaya MenangNessuna valutazione finora
- Sample Referral LetterDocumento2 pagineSample Referral LetterSaya Menang100% (1)
- Trial Terengganu SPM 2013 PHYSICS Ques - Scheme All PaperDocumento0 pagineTrial Terengganu SPM 2013 PHYSICS Ques - Scheme All PaperCikgu Faizal67% (3)
- Larynx (Anatomy, Laryngomalacia, Laryngeal Web)Documento12 pagineLarynx (Anatomy, Laryngomalacia, Laryngeal Web)Saya MenangNessuna valutazione finora
- ENT Short Cases Records & OSCE Questions: 1 EditionDocumento15 pagineENT Short Cases Records & OSCE Questions: 1 EditionSaya MenangNessuna valutazione finora
- Comprehensive Key For ENT Cases: CSOM Never Painful Except inDocumento21 pagineComprehensive Key For ENT Cases: CSOM Never Painful Except inSaya Menang100% (1)
- Cancer LaryncDocumento35 pagineCancer LaryncSaya MenangNessuna valutazione finora
- Sleep Apnea - Could It Be Robbing You of Rest?Documento4 pagineSleep Apnea - Could It Be Robbing You of Rest?Saya MenangNessuna valutazione finora
- Probability DistributionDocumento21 pagineProbability DistributionTee Pei LengNessuna valutazione finora
- Add Math Mid Year Exam Form 4 Paper 1Documento12 pagineAdd Math Mid Year Exam Form 4 Paper 1Rozaidi J-daiNessuna valutazione finora
- Bio 2011 PDF February 29 2012 1 51 Am 2 1 MegDocumento63 pagineBio 2011 PDF February 29 2012 1 51 Am 2 1 MegyatiNessuna valutazione finora
- Chapter 7 - ProbabilityDocumento12 pagineChapter 7 - ProbabilitySaya MenangNessuna valutazione finora
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Compare Visual Studio 2013 EditionsDocumento3 pagineCompare Visual Studio 2013 EditionsankurbhatiaNessuna valutazione finora
- Bakery Management SynopsisDocumento13 pagineBakery Management SynopsisSHiVaM KRNessuna valutazione finora
- DLL Week 7 MathDocumento7 pagineDLL Week 7 MathMitchz TrinosNessuna valutazione finora
- Adobe Scan Sep 06, 2023Documento1 paginaAdobe Scan Sep 06, 2023ANkit Singh MaanNessuna valutazione finora
- Alankit Assignments LTD.: Project Report ONDocumento84 pagineAlankit Assignments LTD.: Project Report ONmannuNessuna valutazione finora
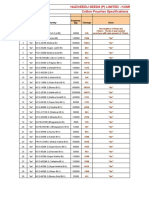
- Sona Koyo Steering Systems Limited (SKSSL) Vendor ManagementDocumento21 pagineSona Koyo Steering Systems Limited (SKSSL) Vendor ManagementSiddharth UpadhyayNessuna valutazione finora
- Horgolás Minta - PulcsiDocumento5 pagineHorgolás Minta - PulcsiCagey Ice-RoyNessuna valutazione finora
- SATYAGRAHA 1906 TO PASSIVE RESISTANCE 1946-7 This Is An Overview of Events. It Attempts ...Documento55 pagineSATYAGRAHA 1906 TO PASSIVE RESISTANCE 1946-7 This Is An Overview of Events. It Attempts ...arquivoslivrosNessuna valutazione finora
- أثر البحث والتطوير على النمو الاقتصادي - دراسة قياسية لحالة الجزائر (1990 -2014)Documento17 pagineأثر البحث والتطوير على النمو الاقتصادي - دراسة قياسية لحالة الجزائر (1990 -2014)Star FleurNessuna valutazione finora
- E F Eng l1 l2 Si 011Documento2 pagineE F Eng l1 l2 Si 011Simona ButeNessuna valutazione finora
- January Payslip 2023.pdf - 1-2Documento1 paginaJanuary Payslip 2023.pdf - 1-2Arbaz KhanNessuna valutazione finora
- Send Me An AngelDocumento3 pagineSend Me An AngeldeezersamNessuna valutazione finora
- E-Governance Horizon Report 2007 PDFDocumento240 pagineE-Governance Horizon Report 2007 PDFtouhedurNessuna valutazione finora
- New Count The DotsDocumento1 paginaNew Count The Dotslin ee100% (1)
- Ancient Egyptian TimelineDocumento5 pagineAncient Egyptian TimelineMariz Miho100% (2)
- Cotton Pouches SpecificationsDocumento2 pagineCotton Pouches SpecificationspunnareddytNessuna valutazione finora
- HitchjikersGuide v1Documento126 pagineHitchjikersGuide v1ArushiNessuna valutazione finora
- Solution Document For Link LoadBalancerDocumento10 pagineSolution Document For Link LoadBalanceraralNessuna valutazione finora
- Company Profile RadioDocumento8 pagineCompany Profile RadioselviNessuna valutazione finora
- Hayat ProposalDocumento22 pagineHayat Proposalsebehadinahmed1992Nessuna valutazione finora
- Journal of The Folk Song Society No.8Documento82 pagineJournal of The Folk Song Society No.8jackmcfrenzieNessuna valutazione finora
- Problem Based LearningDocumento23 pagineProblem Based Learningapi-645777752Nessuna valutazione finora
- Detailed Award Sheet Government College University, FaisalabadDocumento1 paginaDetailed Award Sheet Government College University, FaisalabadAnayat KhetranNessuna valutazione finora
- Complete Cocker Spaniel Guide 009 PDFDocumento119 pagineComplete Cocker Spaniel Guide 009 PDFElmo RNessuna valutazione finora
- ZultaniteDocumento4 pagineZultaniteAcharya BalwantNessuna valutazione finora
- COSL Brochure 2023Documento18 pagineCOSL Brochure 2023DaniloNessuna valutazione finora
- AFI 90-901 Operational Risk ManagementDocumento7 pagineAFI 90-901 Operational Risk ManagementJohan Lai100% (1)
- Did Angels Have WingsDocumento14 pagineDid Angels Have WingsArnaldo Esteves HofileñaNessuna valutazione finora
- Visual Acuity: Opthalmology CEX StepsDocumento5 pagineVisual Acuity: Opthalmology CEX StepsVanessa HermioneNessuna valutazione finora
- 06 Ankit Jain - Current Scenario of Venture CapitalDocumento38 pagine06 Ankit Jain - Current Scenario of Venture CapitalSanjay KashyapNessuna valutazione finora