Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Chap11 13 Motor&Muscles
Caricato da
Natalie PedrajaCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Chap11 13 Motor&Muscles
Caricato da
Natalie PedrajaCopyright:
Formati disponibili
Review Organization of Nervous System
Brain Central
Spinal Cord
Sensory Neurons Motor Neurons
(afferents) (efferents)
Autonomic Somatic
neurons motor neurons
Sensory (somatic & visceral)
Receptors Sympathetic Parasympathetic
neurons neurons
Enteric
(GI)
Neurons
Smooth muscle
Cardiac muscle
Exocrine glands Skeletal muscle
Endocrine glands
Adipose Tissue
AUTONOMIC NERVOUS SYSTEM
The autonomic nervous system consists of
sympathetic and parasympathetic nerves to organs and
blood vessels. Specific groups of neurons in the central
nervous system (in the hypothalamus, medulla/pons, and
spinal cord) control the autonomic neurons, but actions of
these neurons are generally involuntary.
Parasympathetic and sympathetic nerves often innervate
the same organs and often have opposite effects on
these organs. For example, sympathetic nerves increase
heart rate and glycogen breakdown, and parasympathetic
nerves decrease heart rate and increase glycogen synthesis.
Note the anatomy of the parasympathetic and sympathetic
systems on the next slide.
Symp fibers red
Parasymp - blue
Pre-ganglionic
neurons originate in
the CNS (Parasymp
in medulla or sacral
cord; Symp in
thoracic or lumbar
cord)
Post-ganglionic
neurons originate in
ganglia (some
parasymp ganglia are
small and located so
close to the target
organ that they
cannot be seen).
Cervical
Thoracic
Lumbar
Sacral
Preganglionic nerves in both the sympathetic and
parasympathetic systems use acetylcholine as a
neurotransmitter, and the acetylcholine receptor
found on all autonomic ganglion cells is a nicotinic
receptor. The postganglionic parasympathetic nerve
also releases acetylcholine; therefore, the
parasympathetic system is strictly cholinergic.
Note that a preganglionic sympathetic
neuron goes directly to the adrenal medulla.
There is no post-ganglionic neuron to the adrenal.
The adrenal medulla is sometimes described as a
modified sympathetic ganglion because it
releases norepinephrine. Actually the adrenal
medulla releases epinephrine, norepinephrine,
and dopamine into the blood, not into a synapse.
No parasympathetic nerve to the adrenal
In the sympathetic nervous system, alpha and beta adrenergic
receptors may mediate similar actions or opposite actions.
Some target tissues have only one type of adrenergic receptor.
For example, the heart has only beta receptors for sympathetic
nerves. Remember that the heart also has muscarinic
receptors for parasympathetic nerves.
Signal transduction by alpha and beta receptors:
All beta-adrenergic receptors including the relatively rare
3
receptors, bind
to the Gs protein and mediate an increase in cAMP.
Sympathetic & Parasympathetic Actions
Sympathetic - Fight/Flight - Know the starred actions
Parasympathetic Digestion/Relaxation - Know the starred actions
Review Organization of Nervous System
Brain Central
Spinal Cord
Sensory Neurons Motor Neurons
(afferents) (efferents)
Autonomic Somatic
neurons motor neurons
Sensory (somatic & visceral)
Receptors Sympathetic Parasympathetic
neurons neurons
Enteric
(GI)
Neurons
Smooth muscle
Cardiac muscle
Exocrine glands Skeletal muscle
Endocrine glands
Adipose Tissue
Introduction to the Somatic Motor System:
Review the motor neurons in the ventral spinal cord that
send efferent signals to muscles. These are the neurons
that your text discusses at the end of Chapter 11.
Each somatic motor
neuron (ventral horn
neuron) sends an axon
that branches near the
muscle into many
terminal boutons that
form synapses on the
individual muscle fibers
making up a muscle. The
synapse is called the
neuromuscular junction.
The neurotransmitter of
the somatic motor neurons
is acetylcholine and the
postsynaptic membrane
on the skeletal muscle is
called the motor end
plate.
The acetylcholine receptors on the skeletal muscle membrane
are nicotinic receptors that are blocked by the snake venom
toxin -bungarotoxin, which causes paralysis.
Tonic stimulation by somatic motor neurons is needed to
maintain the strength and tone of skeletal muscles.
If the nerve dies or if neurotransmission is blocked for a
prolonged time, the muscle becomes weak and undergoes
atrophy (degenerative loss of weight and strength).
Myasthenia gravis: Auto-immune disease - antibodies attack
and destroy acetylcholine receptors on muscle cells;
eventually no response to nerves. Early Symptom muscle
weakness droopy eyelids = ptosis ; later symptom inability
to breathe (failure of diaphragm response to neural stimulation.
Summary of autonomic and somatic pathways. Explain
where nicotinic receptors are located in somatic and
autonomic pathways.
Chap 12 Muscles
Three types of muscle in human beings:
Smooth, Skeletal and Cardiac
Cardiac and Skeletal are Striated Smooth and Cardiac
have Gap junctions
Other classifications
of muscle:
Myogenic - Can
contract on its own
(Smooth and
Cardiac)
Neurogenic -
Depends on neural
control (Skeletal)
Skeletal muscle
Note examples of
flexors and
extensors
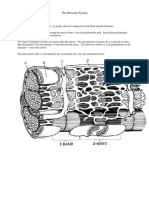
Muscle fiber = muscle cell
Thick
Filament = Myosin
Thin Filament =
Actin
Study the
Structure of
myofibrils on this
slide and the next.
Muscle fiber
The sarcomere is the smallest contractile unit in muscle.
Note the thin and thick filaments.
Titin and nebulin stabilize position of actin & myosin.
Titin = largest protein known. Titins elasticity returns a
resting muscle to its resting length.
Fig. 12-8 Sliding filament mechanism of contraction
Actin slides over myosin, which shortens the
sarcomere (Recall sarcomere = z to z region
Mechanism of Contraction in Skeletal Muscle
Note: prior to the events listed below, ATP must bind
to an ATPase site on myosin heads (myosin ATPase) The
ATP is needed to:
(1) break the attachment of the myosin head to actin
(2) energize the free myosin head so that it rotates and
pushes actin (See Figures in text)
1 Action potential in a motor neuron
2 A neuron releases acetylcholine (Ach)
(Botulinum toxin will block release)
3 Ach binds to receptors on muscle cell
(Curare or Bungarotoxin block receptors)
4 Voltage change in muscle membrane
= end plate potential (EPP)
5 Action potential in muscle membrane
6 Action potential conducted deep into muscle through
T-tubules
7 Action potential activates receptors in T-tubules to open
Ca++ channels
within sarcoplasmic reticulum (SR)
8 SR releases Ca++ into muscle sarcoplasm
[Ca++ is responsible for excitation contraction
coupling - Ca++ release is stimulated by an action
potential (excitation), Ca++ initiates mechanical
contraction by steps 9,10 below]
9 Ca++ binds to troponin-C troponin-C changes
conformation [troponin-C = Ca++ binding protein in
skeletal muscle]
10 Ca++/troponin-C changes position of tropomyosin to
expose binding sites on actin
11 Energy from ATP (myosin ATPase) permits myosin head to
rotate (energized myosin head rotates so can bind to actin
forming a cross-bridge)
12 release of phosphate from the myosin head permits
bending of the head in a powerstroke that pulls actin to
shorten the sarcomere
13 ADP is released from the myosin head to make room
for a new ATP
14 2 events necessary for Relaxation of the sarcomere:
(a) new ATP must bind to the myosin head to
break the cross-bridge
(b) Ca++ must be removed from the sarcoplasm
and transported back into the SR
(active transport of Ca++ by the Ca++
ATPase in the SR)
NOTE: ATP is required for both contraction and relaxation
of skeletal muscle.
If there is no new ATP, the muscle cross-bridges are frozen
in an attached position = rigor. This is why muscles are
frozen in a contracted state at death rigor mortis
If a new ATP is present, but Ca++ is not removed or Ca++
is again released by another action potential, the
contraction events start over again.
ATP + removal of Ca++ relaxation
ATP + presence of Ca++ myosin-actin binding+contraction
No ATP rigor - tight myosin-actin binding no relaxation
A single contraction of a single muscle fiber (one muscle
cell) = a twitch - measured as force or tension of the
muscle. See the graphs action potentials and a twitch in
Figure: Note the time delay (latent period) between an
action potential and a twitch
Note in this Figure how phosphocreatine is formed in
muscles at rest and how phosphocreatine + ADP can be
used to generate ATP in working muscle; i.e.
phosphocreatine is an important source of ATP in
muscles. The reaction catalyzed by creatine kinase is
reversible;i.e., the ezyme
catalyzes the formation of
phosphocreatine (top
reaction in the figure) as
well as its breakdown
(bottom reaction). The
action of the creatine
kinase in
phosphorylating creatine is
how the enzyme got its
name.
Skeletal Muscle Classification by speed of contraction and resistance
to fatigue (endurance)
Fatigue resistance (endurance) is determined primarily by the type of
muscle metabolism oxidative or glycolytic
Fatigue Resistant Muscles Easily fatigued Muscles
Aerobic (Oxidative) Anaerobic (Glycolytic)
- ATP produced quickly
but little of it
Krebs cycle Glycolysis
Many mitochondria Lactic acid by-product
Many capillaries fatigue
High level myoglobin Depletion of
(O2 binding protein) glycogen fatigue
Even oxidative fibers fatigue after prolonged exertion due
to depletion of muscle glycogen
Improved oxidative metabolism is key to increased
endurance
Speed of contraction is increased by
-the fast isoform of myosin ATPase activity
and
-high levels of Ca++ ATPase (duration of the twitch
decreases if Ca++ is pumped faster into the SR)
-Faster relaxation between twitches
Generally ATPase is key to increased speed.
Color of the muscle depends on the amount of
myoglobin, which gives the muscle a red color.
Absence of myoglobin makes the muscle appear
white.
Physics of Muscle Contraction
Relationship of muscle fiber length and force of
contraction (length- tension relationship)
Relationship of frequency of stimulation of a muscle
fiber and force of contraction.
Relationship between size of the stimulus and
number of motor units activated
Relationship of muscle fiber length and force of
contraction (tension)
Relationship of frequency of stimulation of a muscle
fiber and force of contraction.
High frequency
action potentials
temporal
summation of contractions
Fused contractions with
maximal force (tetanus)
Note fatigue -
Muscle cramps result from tetanus. Cause = high
frequency neural stimulation
Abnormally low levels of plasma Ca++ may cause
Hypocalcemic tetany. This is because normal levels of
plasma calcium are needed to prevent excessive
excitability of neurons. If calcium levels are too low,
neurons generate action potentials very rapidly, which
can cause tetanus of the muscles. Low levels of
plasma calcium do not directly affect contraction of
skeletal muscles because these fibers obtain calcium
from the sarcoplasmic reticulum, not from the
plasma. The effect of the low calcium levels on the
nerves indirectly increases the frequency of skeletal
muscle contractions, which in turn leads to fusion of
contractions into a fused forceful contraction.
Motor Unit One motor neuron + all muscle fibers
innervated.
One neuron innervating many muscle fibers permits
only gross control by the neuron (example moving an
arm). One neuron innervating only a few fibers permits
fine control as in the fine control of hand movements.
All fibers in one motor unit are of the same fiber type,
so there are slow twitch motor units and fast twitch
motor units, dependent on the metabolic characteristics
of the fiber
Endurance training can affect the metabolic
characteristics of the muscle fibers - convert to a
more oxidative fatigue-resistant type
All fibers in one motor unit are of the same fiber type,
But one muscle is often composed of more than one
type of fiber (one muscle is composed of multiple
motor units)
nerve to a
muscle
consists of
a bundle of
neuronal
axons from
several
motor
neurons.
Relationship between size of the stimulus and number
of motor units activated
Stronger stimuli activate more motor units. This is
called recruitment. This is a type of spatial summation.
Weak stimuli recruit only the low threshold motor units,
whereas strong stimuli recruit low and high threshold motor
units.
Asynchronous recruitment is the activation of different
motor units at different times, which helps to avoid fatigue
of all fibers at the same time.
Isometric and Isotonic Contractions:
(1) isotonic contraction shortens the muscle and
moves a load, even if the load is only the weight of the
muscle moved
(2) an isometric contraction develops tension but
does not shorten, and any load on the muscle does
not move. Examples of isometric contractions include
pushing against an immovable wall, trying to lift a load that
is too heavy to move, or simply tensing (contracting)
muscles without moving them.
The word isometric means same length, which
accurately describes what happens in an isometric
contraction the muscle develops force (tension) but does
not shorten. The word isotonic means same tension,
which is misleading, because the muscle develops
enough tension to move a load, but the term isotonic
refers to the fact that the load (the force against which the
muscle contracts) remains constant as the load is moved.
Muscles and Bones as
Levers
Effects of exercise on
skeletal muscle:
hypertrophy,
increased
vascularization of
muscles blood flow
Oxygen
Disuse Atrophy of
muscle
Gap junctions in smooth and cardiac muscles permit
many fibers to function as one unit referred to as a
syncytium. Specialized gap junctions connecting the
ends of cardiac muscles are intercalated discs.
Unique properties of smooth muscle: little or no
sarcoplasmic reticulum in smooth muscle; therefore, calcium
enters the muscle from plasma. Note that calcium channels
in the cell membrane can be opened by chemical modulators
or stretch of the muscle, in addition to action potentials
(voltage changes) Nerves not necessary.
The Ca++ binding protein in smooth muscle is calmodulin
rather than troponin C.
Ca++ bound calmodulin activates myosin light chain
kinase, which activates myosin ATPase, which permits
cross-bridge formation and contraction. Both a myosin
phosphatase and removal of Ca++ are important in the
relaxation of SMOOTH muscle.
Contraction of cardiac muscle is similar to that of
skeletal muscle, except that calcium enters the
muscle from both the sarcoplasmic reticulum and
plasma; therefore, blood calcium levels have direct
effects on the contraction of both cardiac and
smooth muscle.
Calcium channels that allow blood calcium to enter
smooth muscle and heart muscle can be inhibited by
calcium channel blockers that do not affect the
calcium channels on the skeletal muscle SR. These
calcium channel blockers can be used to decrease
smooth muscle contraction and the force of heart
contraction without affecting skeletal muscle function .
Explain why are these drugs useful in treating
blood pressure?
Potrebbero piacerti anche
- A Color Handbook of Small Animal Emergency and Critical Care MedicineDocumento296 pagineA Color Handbook of Small Animal Emergency and Critical Care MedicineNatalie PedrajaNessuna valutazione finora
- Hockenbury Discovering Psychology Chapter 1bDocumento4 pagineHockenbury Discovering Psychology Chapter 1bNatalie PedrajaNessuna valutazione finora
- Hanover High Swim Team Makes A SplashDocumento1 paginaHanover High Swim Team Makes A SplashNatalie PedrajaNessuna valutazione finora
- Burnout and Health PromotionDocumento2 pagineBurnout and Health PromotionNatalie PedrajaNessuna valutazione finora
- Chapter 1 Introduction To ReproductionDocumento11 pagineChapter 1 Introduction To ReproductionNatalie PedrajaNessuna valutazione finora
- Vol-66 VIII Continental ShelfDocumento9 pagineVol-66 VIII Continental ShelfNatalie PedrajaNessuna valutazione finora
- Case Report, Bindi Sue L.Documento3 pagineCase Report, Bindi Sue L.Natalie PedrajaNessuna valutazione finora
- Case Report, Charlie W.Documento2 pagineCase Report, Charlie W.Natalie PedrajaNessuna valutazione finora
- Hockenbury Discovering Psychology Chapter 1Documento3 pagineHockenbury Discovering Psychology Chapter 1Natalie Pedraja0% (2)
- Chap 13 Neuromuscular IntegrationDocumento17 pagineChap 13 Neuromuscular IntegrationNatalie PedrajaNessuna valutazione finora
- Chap10 Sensory Intro & Special SensoryDocumento50 pagineChap10 Sensory Intro & Special SensoryNatalie PedrajaNessuna valutazione finora
- Marine Megafauna NotesDocumento13 pagineMarine Megafauna NotesNatalie PedrajaNessuna valutazione finora
- 7 AnuraDocumento59 pagine7 AnuraNatalie PedrajaNessuna valutazione finora
- 311intro & Cell SignalingDocumento40 pagine311intro & Cell SignalingNatalie PedrajaNessuna valutazione finora
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (119)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Physiology I MCQ PDFDocumento0 paginePhysiology I MCQ PDFRaj Cella100% (2)
- Teach Me AnatomyDocumento17 pagineTeach Me AnatomyMar Kristian Vero Lumen100% (1)
- Physiology. Hrd.Documento549 paginePhysiology. Hrd.Sʌɩĸʌt PʌʋɭNessuna valutazione finora
- The guard cells in plant A between 0600 and noon are flaccid with small stomatal aperture.(a) (ii) Explain why the guard cells in plant A are flaccid with small stomatal aperture between 0600 and noonDocumento12 pagineThe guard cells in plant A between 0600 and noon are flaccid with small stomatal aperture.(a) (ii) Explain why the guard cells in plant A are flaccid with small stomatal aperture between 0600 and noonChee Beng YeapNessuna valutazione finora
- Popping Sarcomere Hypothesis Explains Stretch Induced Muscle DamageDocumento5 paginePopping Sarcomere Hypothesis Explains Stretch Induced Muscle Damagemk78_inNessuna valutazione finora
- Principles of Anatomy and Physiology 15th Edition Tortora Test BankDocumento52 paginePrinciples of Anatomy and Physiology 15th Edition Tortora Test Bankgabrielvanztqro100% (27)
- Quarter 2 - Module 6 - Earth and Life ScienceDocumento8 pagineQuarter 2 - Module 6 - Earth and Life ScienceKristine AlcordoNessuna valutazione finora
- BIOL1040 Lecture NotesDocumento50 pagineBIOL1040 Lecture NotesJonathanZhaoNessuna valutazione finora
- The Mechanisms of Muscle Hypertrophy SchoenfeldDocumento26 pagineThe Mechanisms of Muscle Hypertrophy SchoenfeldFloren Martil Guijarro100% (1)
- Musculoskeletal SystemDocumento92 pagineMusculoskeletal SystemBrenda LynNessuna valutazione finora
- Ultimate Guide To The CSCS ExamDocumento104 pagineUltimate Guide To The CSCS Examrobertobarron88% (16)
- Bio 122 FR 10 - Smooth MuscleDocumento5 pagineBio 122 FR 10 - Smooth MuscleLance CarandangNessuna valutazione finora
- CPT7 Study GuideDocumento68 pagineCPT7 Study GuideAxel Mori100% (2)
- FF Raumenys PDFDocumento34 pagineFF Raumenys PDFLaura PaškevičiūtėNessuna valutazione finora
- Everything You Need to Know About the Muscular SystemDocumento46 pagineEverything You Need to Know About the Muscular SystemSide PoorNessuna valutazione finora
- Muscle - Coloring and QuestionsDocumento3 pagineMuscle - Coloring and QuestionsNadia ShafiqNessuna valutazione finora
- SDL MuscularDocumento6 pagineSDL MuscularMonique Eloise GualizaNessuna valutazione finora
- l3 Muscle Physiology I 201920 2Documento6 paginel3 Muscle Physiology I 201920 2ARYSSA BINTI AZRINessuna valutazione finora
- Bio201 Exam 2 Master With AnswersDocumento12 pagineBio201 Exam 2 Master With AnswersRicha Rala100% (1)
- Guide Questions Answers: Muscles Contract, They Contribute To Gross and FineDocumento7 pagineGuide Questions Answers: Muscles Contract, They Contribute To Gross and FinePrancheska Abigayle Peneyra SantiagoNessuna valutazione finora
- Muscle Twitch and Tetanus: Contraction PhaseDocumento2 pagineMuscle Twitch and Tetanus: Contraction Phasevkpremiyahoo.comNessuna valutazione finora
- Muscular System: Structure and Function: 1. Types of MusclesDocumento3 pagineMuscular System: Structure and Function: 1. Types of MusclesIceLandNessuna valutazione finora
- Chapter 4. Muscular - System JeDocumento55 pagineChapter 4. Muscular - System JeIvonike Lim100% (2)
- Muscles in MotionDocumento6 pagineMuscles in MotionLynnNessuna valutazione finora
- CH 10 Muscular TissueDocumento4 pagineCH 10 Muscular TissuemunozdexpNessuna valutazione finora
- HIPERTROFIA SARCOPLASMATICA É Um Unicornio No Treinamento ResistidoDocumento33 pagineHIPERTROFIA SARCOPLASMATICA É Um Unicornio No Treinamento ResistidoLuiz Vinicius CostaNessuna valutazione finora
- Neuromuscular JunctionDocumento16 pagineNeuromuscular JunctionSamadshahirNessuna valutazione finora
- Physiology of Theraupetic Exercise: By: Nini Natalia, DRDocumento53 paginePhysiology of Theraupetic Exercise: By: Nini Natalia, DRSaktriawan ArifNessuna valutazione finora
- Cellular Movement and Muscles: Powerpoint Lecture Slides Prepared by Stephen Gehnrich, Salisbury UniversityDocumento89 pagineCellular Movement and Muscles: Powerpoint Lecture Slides Prepared by Stephen Gehnrich, Salisbury UniversityJennie LaoNessuna valutazione finora
- Locomotion and MovementsDocumento58 pagineLocomotion and Movementspurandar puneetNessuna valutazione finora