Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
DPD-3 21jan Brain Resusitation
Caricato da
wawanpecelTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
DPD-3 21jan Brain Resusitation
Caricato da
wawanpecelCopyright:
Formati disponibili
Patofisiologi
Cardiopulmonary Cerebral Resuscitation Basics For Life Support
Rita A. Sutjahjo
Lab/SMF Anestesiologi FK. Unair / RSUD Dr. Soetomo Surabaya
Hypoventilation / apnea Low blood flow / cardiac arrest
neuron
ISCHEMIA
Reperfusion CPCR Reoxygenation Good Result
INJURY
Instructional Objective
To understand the pathophysiologic mechanism of post resuscitation syndroma
To define the ultimate potentials & limitations
of resuscitation
Dying Cells Metabolic changes as result of Depletion of oxygen Depletion of energy substrate Accumulation of metabolic end products
Point of Threatening Viability MAP < 60 - severe hypotension PaO2 < 50 - severe hypoxaemia
Determinan kerusakan sel karena anoksia Sel otak Sel miokard 50 % Myosit rusak
Waktu 5 menit 15 menit
Fungsi pompa jantung dapat kembali
Sekelompok sel neurom area tertentu di otak rusak
Gangguan human mentation
S S
Energy deficit
Glutamate excitotoxicity Intracellular accumulation of Ca2+, Acidosis
Oxidative stress Activated NO synthesis Cytokine imbalance Local inflammation, microcirculation derangement
Apoptosis, Trophic dysfunction
Ischemia Minutes
Hours Days
12
24
Time after ischemia onset
Temporal development of processes inducing focal ischemic brain damage
Post-Resuscitation Syndrome
Safar P, 1981
Safar P, 1993
Reperfusion - Reoxygenation Stage I II : No reflow : Transient hyperemia (Acidosis Vasodilation)
5 - 10
III
: Hypoperfusion
30 - 60 48 - 72 hrs
IV
: Evolution
Hypothetical events in the brain following total circulatory arrest
Safar P, 1981
Bio Chemical Changes In Re - Perfusion Injury
Tissue edema vasospasm Red cell sludging Intracellular edema (Impaired ionic pump) Release of excitatory AA Free radicals - lipid preoxidation Cell membrane damage Intracellular Ca overload S
Cascade of early biochemical events occurring during an ischaemic episode
Baillieres Clinical Anaesthesiology-Vo.10.No.3 September 1996
Decreased CBF
Tissue ATP falls
Failure of energy-dependent processes
Glutamate release
Neuronal depolarization
Sodium influx Potassium efflux Calcium influx
Stimulates NMDA receptors
Opens VSCCs
Cell swelling
Calcium entry
Activating of phospholipases, calpains, gene expression etc
Pathway for events linking cerebral ischemia-reperfusion to cellular injury
Role of Glutamate in Excitotoxic Neuroral Injury
VOCC G L U T A M A T E Depolarization
AMPA
Na+ Ca2+
Ca2+/CAM kinase PKC
Free radical production Lipid peroxidation DNA damage Energy depletion
(a)
NMDA
Na+ Ca2+ PLC
cAMP cGMP
NO synthase PLA2
Ca2+ stores
Cell death
m G GLU
Calpains
O2 supply < O2 demand synthesis ATP ATP stores sodium pumps Na+ influx K+ efflux Membrane depolarization Opening of coltage-sensitive Ca2+ channels Release of glutamate
Cell Injury occurred during ischemia reperfusion
Glutamate A mediator of neuronal damage during ischemia
Opening of NMDA receptorcontrolled Ca2+ channels Massive influx of Ca2+ Activation of proteases
Activation of phospholipases Hydrolysis of membrane phosphollipids FFA
Amitochondrial accumulation Uncoupling of oxidative phosphorylation Free radicals Vascular damage
arachidonic acid
prostaglandins
Irreversible cell membrane damage
Lipid peroxidation
Components Contribute To Ultimate Cell Damage
Ischemic component Severity Duration
Re - Perfusion component
Biochemical changes
Cell death
Cell Injury
Reversible injury
Reperfusion component
No injury No injury Treatment window Beyond treatment
TIME
Out come after CPCR Pre insult derangement Duration & type of primary insult Post oxygention syndroma
Clinical Conditions That Are Accompanied By Oxidant Stress*
Target Organs Lung Clinical Conditions Acute respiratory distress syndrome Asthma Reperfusion pulmonary edema Acid aspiration Pulmonary oxygen toxicity Comments The lung is vulnerable to oxidant injury from the airways (e.g. high inspired O2) and from the microcirculation (e.g.WBC sequestration). Protection from O2 is aided by high levels of glutahione and vitamin C in the epithelial lining of the lower airways. Oxidants most likely play a role in the stunned myocardium associated with reperfusion injury
Heart
Acute myocardial infarction Reperfusion injury due to : Angioplasty Cardioplegia Coronary occlusion Thrombolysis Stroke Traumatic brain injury Postresuscitation injury Spinal cord injury
Nervous system
Lipid peroxidation is a prominent form of oxidant injury in the brain and spinal cord. Steroids that inhibit lipid peroxidation are being evaluated for nervous systems injury
..clinical conditions that are accompanied by oxidant stress
Target Organs Gastroinstestinal tract Kidney Clinical Conditions Drug-indused mucosal injury Intestinal ischemia Peptic ulcer disease Acute renal failure due to Aminoglycosides Ischemia Myoglobinuria Cardiopulmonary bypass Multiple organ dysfunction syndrome Multisystem trauma Postresuscitation injury Septic shock Thermal injury Comments The gut is susceptible to reperfusion injury, possibly due to the abundance of xanthine dehydrogenase (a source of O2 during ischemia) in the bowel wall Hydrogen peroxide and iron may have important roles in oxidant injury involving the kidneys. Inflamation is a common source of oxidant production in these conditions Nitric oxide may promote hypotension in septic shock. Agents that inhibit nitric oxide production are being evaluated in septic shock (Ann Phamacother 1995;29;36-46).
Multiple organs
* Includes only conditions that are prevalent in ICU patients
Improved outcome depend on,
1. By stander CPR response time <
2. Early advanced cardiac life support restoration of spontaneous circulation 3. Intensive care Preventing secondary neurologic insult
Extra cranial homeostasis
Myocardial Blood Flow
100
75 % 50 25 0 0/58 <15 15-20 CPP, mm Hg Coronary perfusion pressure (CPP) during closed-chest resuscitation in out-of-hospital victims of cardiac arrest. Paradis NA, 1990 >20 Out-of-Hospital Cardiac Arrest 100 Pts 10/23
14/19
Mean PETCO2 during closed-chest resuscitation in 35 human victims of cardiac arrest. Sanders AB, 1989
Data base > 800 victim (Cardiac arrest in BRCT I & II, Peter Safar)
1. Long duration of arrest & resuscitation effort outcome
poor neurologic
2. After restoration of heart beat, high arterial reprefussion pressure good cerebral recovery 3. Cardiac arrest without CPR > 5 irreversible brain damage 4. Advanced aged mortality worse neurologic outcome S
5. Steroid improved neurologic outcome after cardiac arrest
Cardio Pulmonary Cerebral Resuscitation When not to start Terminal stage of incurable disease When in doubt CPR A s/d F Prolonged life support ? When to stop Based on cardiac death (Heart cannot be restarted despite max effort at leas 30 minute) Brain death certified After 24 hr. extracerebral organ stabilization
Drugs block reperfusion injury Calcium entry blockers
Excitatory amino acid neurotransmitter antagonists
Free radical scavengers
Antagonists to the arachidonic acid cascade
Steroid (inhibit lipid peroxidation of cell membranes) ?
Clinical criteria for brain death certification
Exclusion of reversible CNS depression
Absence of hypothermia Absence of drugs (e.g. ethanol, barbiburates) Absence of metabolic perturbations that could potentiate CNS depression (e.g. abnormalities in electrolytes, osmolarity, serum ammonia, creatinine, hypercarbia, hypoxemia)
Absent cortical function
Unresponsiveness to painfull stimuli No spontaneous muscular movements (in the absence of muscle relaxants) no posturing, shivering, or sezure activity (in the absence of musle relaxants)
Absent brainstem function
Pupils nonreactive and fixed to light No corneal reflexes No gag or cough reflexes No oculocephalic reflexes No oculovestibular reflexes
Organ blood flow measurements utilizing radioactive mecrospheres in a rodent model of cardiac arrest. Precordial compression was initiated 4 minutes after induction of ventricular fibrillation. Spontaneous circulation was successfully restored by external transthoracic countershock in 5 of 10 animals after 9 minutes of ventricular fibrillation.
Blood flow generated as a function of depth of compression during closed-chest resuscitation in 8 dogs. Cardiac output (CO) is represented as a fraction of the cardiac output generated at a compression depth of 5 cm.
Potrebbero piacerti anche
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Dapsa EngDocumento1 paginaDapsa EngwawanpecelNessuna valutazione finora
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5795)
- Number 1 MARCH 2006Documento178 pagineNumber 1 MARCH 2006wawanpecelNessuna valutazione finora
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Number 1 MARCH 2006Documento178 pagineNumber 1 MARCH 2006wawanpecelNessuna valutazione finora
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Models of Viral Hepatitis PDFDocumento173 pagineModels of Viral Hepatitis PDFwawanpecelNessuna valutazione finora
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Preamble: Podcast Interview: - Also Available On ItunesDocumento18 paginePreamble: Podcast Interview: - Also Available On ItuneswawanpecelNessuna valutazione finora
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- DemamDocumento50 pagineDemamwawanpecelNessuna valutazione finora
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Nigella Sativa: (Black Cumin) Seed Extract Alleviates Symptoms of Allergic Diarrhea in Mice, Involving Opioid ReceptorsDocumento11 pagineNigella Sativa: (Black Cumin) Seed Extract Alleviates Symptoms of Allergic Diarrhea in Mice, Involving Opioid ReceptorswawanpecelNessuna valutazione finora
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Sexual SelfDocumento19 pagineSexual SelfErica SisgonNessuna valutazione finora
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- ParaphrasingDocumento12 pagineParaphrasingXia U Rong100% (1)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Introduction To Clinical ParasitologyDocumento6 pagineIntroduction To Clinical ParasitologyJennifer HerediaNessuna valutazione finora
- Supervisi Berjenjang Di Era Pandemi Covid-19 Dalam Manajemen KeperawatanDocumento10 pagineSupervisi Berjenjang Di Era Pandemi Covid-19 Dalam Manajemen Keperawatanfebrian rahmatNessuna valutazione finora
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- Physical DiagnosisDocumento97 paginePhysical Diagnosisaxmedfare138Nessuna valutazione finora
- Hidden Pain: Ehlers-Danlos SyndromeDocumento28 pagineHidden Pain: Ehlers-Danlos SyndromeVictoria67% (3)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Milia AriaDocumento8 pagineMilia AriaAtsabitFarisNessuna valutazione finora
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- tmpB0AD TMPDocumento10 paginetmpB0AD TMPFrontiersNessuna valutazione finora
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- Assessment of The Ears Rev 4-2013Documento8 pagineAssessment of The Ears Rev 4-2013alphabennydelta4468Nessuna valutazione finora
- Biology 9 Science Al-Raza Institute Paper I Group-I Time Allowed: 20 Min Objective Marks: 12Documento3 pagineBiology 9 Science Al-Raza Institute Paper I Group-I Time Allowed: 20 Min Objective Marks: 12Anonymous WDvB6A0Nessuna valutazione finora
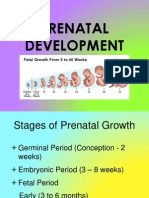
- Prenatal DevelopmentDocumento23 paginePrenatal DevelopmentCelestina TanNessuna valutazione finora
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Color Therapy GeneralDocumento39 pagineColor Therapy GeneralNowo BudirahardjoNessuna valutazione finora
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Diminished Capacity Issue 5Documento29 pagineDiminished Capacity Issue 5Sheena LeanoNessuna valutazione finora
- Cara Baca Foto ThoraxDocumento23 pagineCara Baca Foto ThoraxNofilia Citra CandraNessuna valutazione finora
- 2 Ligan First MassengerDocumento32 pagine2 Ligan First MassengerikhararaNessuna valutazione finora
- Final Exam Anatomy and PhysiologyDocumento5 pagineFinal Exam Anatomy and PhysiologyAlibasher MacalnasNessuna valutazione finora
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Acute Coronary Syndrome: An Essential & Practical ApproachDocumento35 pagineAcute Coronary Syndrome: An Essential & Practical ApproachGinawidiyastutiNessuna valutazione finora
- Host Parasite InteractionDocumento20 pagineHost Parasite InteractionRhomizal MazaliNessuna valutazione finora
- Roland Barthes - Steak and ChipsDocumento3 pagineRoland Barthes - Steak and ChipsmishaiolandaNessuna valutazione finora
- Trilemma Adventures BestiaryDocumento17 pagineTrilemma Adventures BestiaryZamak50% (2)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- The Tonsils (Waldeyer's Ring) - Lingual - Pharyngeal - Palatine - Tubal - TeachMeAnatomyDocumento4 pagineThe Tonsils (Waldeyer's Ring) - Lingual - Pharyngeal - Palatine - Tubal - TeachMeAnatomywachito ricoNessuna valutazione finora
- Lacunar Infarct - Radiology Reference Article - RadiopaediaDocumento8 pagineLacunar Infarct - Radiology Reference Article - RadiopaediaRismanto TorsioNessuna valutazione finora
- Artículo de Royal Canin - The Barf Trend Advantages, Drawbacks and RisksDocumento8 pagineArtículo de Royal Canin - The Barf Trend Advantages, Drawbacks and RisksAlejandra CárdenasNessuna valutazione finora
- Uwise HYDocumento3 pagineUwise HYJack GuccioneNessuna valutazione finora
- Dairy FarmingDocumento1 paginaDairy FarmingyogasanaNessuna valutazione finora
- Retention and RelapseDocumento32 pagineRetention and RelapseRana SayedNessuna valutazione finora
- RabbitDocumento3 pagineRabbit002211exeNessuna valutazione finora
- Streets Family FarmDocumento3 pagineStreets Family Farmapi-299299446Nessuna valutazione finora
- Women Health Presentation (Ovarian Cyst)Documento17 pagineWomen Health Presentation (Ovarian Cyst)Lim Su-WeiNessuna valutazione finora
- Power Taiji Vol 1Documento99 paginePower Taiji Vol 1English Teaching100% (3)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)