Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Fluids & Electrolytes: Scott G. Sagraves, MD, FACS
Caricato da
Asad Khan KhalilTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Fluids & Electrolytes: Scott G. Sagraves, MD, FACS
Caricato da
Asad Khan KhalilCopyright:
Formati disponibili
Fluids &
Electrolytes
Scott G. Sagraves, MD, FACS
Assistant Professor
Trauma & Surgical Critical Care
The recognition and
management of fluid,
electrolyte, and related
acid-base problems are
common challenges on the
surgical service.
Lawrence, Essentials of General Surgery
Goals
Review concept of total body fluids
Review types of crystalloids
Review electrolytes disturbances & their
treatment strategies.
Body Fluids
Intercellular
Intravascular
Interstitial
40%
16%
4%
Body Water = 60% of a patients body weight
Why do you give
D
5
NS + 20 mEq/L KCl
at 125 cc/hr to a
patient?
Fluid Requirements
typically 35 mL/kg/day
insensible loss = 700 mL/day or 0.2
cc/kg/day for every 1 C > 37
1-10 kg = 100 mL/kg/day {4mL/kg/hr}
11-20 kg = 50 mL/kg/day {2mL/kg/hr}
> 21 kg = 20 mL/kg/day {1mL/kg/hr}
Trick for hourly maintenance = 40 + weight (kg)
Serum Values of
Electrolytes
Cations Concentration, mEq/L
Sodium 135 - 145
Potassium 3.5 - 4.5
Calcium 4.0 - 5.5
Magnesium 1.5 - 2.5
Anions
Chloride 95 - 105
CO2 24 - 30
Phosphate 2.5 - 4.5
Daily Requirements for
Electrolytes
Sodium: 1-2 mEq/kg/d
Potassium: 0.5-1 mEq/kg/d
Calcium: 800 - 1200 mg/d
Magnesium: 300 - 400 mg/d
Phosphorus: 800 - 1200 mg/d
IV Solutions
Solution Na
+
Cl
-
K
+
Ca
+2
HCO3
-
Glu
Plasma 141 103 4-5 5 26 0
NS 154 154 0 0 0 0
D5W 0 0 0 0 0 50 G
LR 130 109 4 3 28 0
Serum Osmolality = [2 x Na] + [BUN/2.8] + [glucose/18]
Replacement Strategies
Sweat: D
5
NS + 5 mEq KCl/L
Gastric: D
5
NS + 20 mEq KCl/L
Biliary/pancreatic: LR
Small Bowel: LR
Colon: LR
3
rd
space losses: LR
Resuscitation
Crystalloids
Replace blood loss at a 3:1 ratio
Initial bolus 1-2 liters, usually normal
saline
If they have transient response, give
additional fluids. Once 3-4 liters of
crystalloid has been given consider
blood.
INDICATORS OF SUCCESSFUL
RESUSCITATION
PULSE 100 - 120 bpm
URINARY OUTPUT
CHILDREN = 1.0 ml/kg/hr
ADULT = 0.5 ml/kg/hr
Clearance of lactate
Resolution of base deficit
BLOOD PRESSURE POOR
INDICATOR
Fluid Status
[Na]
ECV
low normal
high
160
140
120
140
GI loss
SIADH
Hypothyroid
Cortisol
CHF
Cirrhosis
NaHCO
3
3% NaCl
Seawater
DI
Insensible
GI Loss
Renal loss
Osmotic
Renal Regulatory
Mechanisms
Aldosterone
distal tubules
sodium exchanged for K
+
and H
+
released by volume reduction
Antidiuretic Hormone (ADH)
increased tubular water reabsorption
posterior pituitary release
Acid/base
7.4
BE = 0
HCO3 = 24
Respiratory
Acidosis
Metabolic
Acidosis
Metabolic
Alkalosis
Respiratory
Alkalosis
ABG Rules
Rule 1: An increase or decrease in
PaCO
2
of 10 mm Hg, respectively, is
associated with a reciprocal decrease or
increase of 0.08 pH units.
Rule 2: An increase or decrease in
[HCO3
-
] or 10 mEq/L respectively is
associated with a directly related
increase or decrease of 0.15 pH units.
Acidosis
pH < 7.2
decreased responsiveness to catecholamines
cardiac dysfunction
arrhythmias
increased potassium serum levels
Case Studies
Found Down
45 yo WM, found down, presumed to be
assaulted, well known to ED for EtOH
CT head - hygromas, small ICH
labs:
Na = 118
K = 2.4
Cl = 74
What do you think? What do you do?
Severe Hyponatremia
Correct sodium to above 120 mEq/dl
NaCl + 40 mEq/L KCl
3% Saline
furosemide diuresis (euvolemic)
serial electrolytes
be prepared to handle seizures
Replace potassium
Cl should correct itself
Hyponatremia
1% of hospitalized are hyponatremic
Neurologic conditions:
Seizures, coma, encephalopathy
Results from rapid + [Na]
Peripheral symptoms:
Cramping, twitches, fasciculations
Results from ion conduction aberrations
Hints
Na
+
deficit (mEq) =
(140 Na
serum
) x 0.6 x Kg
Glucose increase 100 mg/dL or a BUN
increase of 30 mg/dL o decrease of 1.5
2 mEq/L Sodium
Central Pontine
Myelinosis
Results from overcorrection of
sodium
Correction of > 25 mEq per 24-48 hrs
Concurrent hypoxia
Presence of liver disease
Acute correction limit 25 mEq /day
Chronic correction limit 10 mEq/day
Treatment Strategies
Hypovolemic Hyponatremia
expand intravascular volume
0.9% NS or 3% Hypertonic Saline
Hypervolemic Hyponatremia
water restriction
treat medical condition
hemodialysis
Euvolemic Hyponatremia
SIADH
restrict fluid: 7-10 ml/kg/d
demeclocycline antagonizes vasopressin
HDU Code
A Code Blue is called in the HDU.
65 yo male with ESRD has arrested
awaiting his dialysis treatment. CPR and
BVM resuscitation are in progress and an
IV has been established.
What do you think? What do you do?
Pre-Arrest Rhythm Strip
Arrest Strip
Diagnosis?
HYPERKALEMIA
-Treatment
CaCl
2
10% - 1 ampule
Sodium Bicarbonate - 1 ampule
D
50
& Insulin 10 U
|
2
- agonist nebulizer- cellular K |
Kayexalate
Causes of
Hyperkalemia
Renal dysfunction
Acidemia
Hypoaldosteronism
Drugs
Excessive intake
WBC > 100,000
Platelets > 600,000
Cell Death
Rhabdomyolysis
Tumor lysis
Burns
Hemolysis
Potassium Metabolism
Normal daily intake 100 mEq
Renal filters & reabsorbs prox. Tubule
Potassium o 1/[aldosterone]
Acidosis | [potassium] with H
+
out
Alkalosis + [potassium] with H
+
in
Post op patient
42 year old female admitted to the ICU
post op after undergoing a
thyroidectomy for thyroid cancer.
She is complaining of peri-oral
numbness and tingling. Her DTRs are
hyperactive and her ECG has a
prolonged QT interval.
What do you think? What do you do?
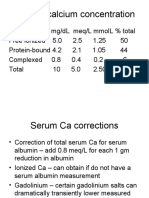
HYPOCALCEMIA
Chvosteks sign - facial muscle spasm
Trousseaus sign - carpal spasm
Treatment
monitor ECG
IV calcium
follow up labs
oral calcium supplements
normal is 1 gram/day
Blunt Trauma
23 year old male, s/p MVC with blunt
abdominal and orthopedic trauma
HD#3 develops fever, N/V, abdominal
pain, refractory hypotension, with
oliguria.
Na
+
130, K
-
5.5, Glu 65, pH 7.29
What do you think? What do you do?
ACUTE ADRENAL
INSUFFICIENCY
Treatment
fluid and vasopressor support
treat precipitating conditions
draw baseline cortisol level
administer dexamethasone
ACTH stimulation test
hydrocortisone 100 mg IV q 8
Hydrocortisone Stimulation
Test
Baseline cortisol
> 20 - no further therapy
15 - 20 - test
< 15 empiric therapy
Administer Cortrosyn 250 g IV
Obtain levels 30 & 60 minutes post
injection
You are called to the
Bedside
What Do You Think? What Do You Do?
55 yo male, s/p fall with isolated,
repaired fractured femur.
Pts LOC decreased and patient began
to seize.
EKG showed
Hypomagnesemia
Mg plays role in energy metabolism,
protein synthesis, cell division, &
calcium regulation in muscle.
Definition < 1.6 mg/dL
Causes: poor diet, diuretics, gut losses,
& massive diarrhea, resuscitation.
Mg Rx
Replacement Magnesium Sulfate
1 gram = 8 mEq
Infuse at rate of 2 gram/hour
Emergency: 2 grams over 5
minutes
Closed Head Injury
32 year old female, MVC, GCS -7,
intubated, with CT scan showing SAH,
cerebral edema. ICP monitor shows a
pressure of 27. CPP 55.
Over the next several days, Na
+
> 150.
What do you think? What do you do?
DIABETES INSIPIDUS
Signs
[Na
+
] > 150
Urine specific gravity 1.007
polyuria, clear urine
dDAVP 1g sq raises urine osmolality in 2 hours
Treatment
free water deficit = (0.6) x (Kg) x ([Na
serum
/140] -1)
dDAVP 2g sq every 12 hours
for every L water deficit [Na
+
] will rise 3 mEq
above 140
The transfer
50 year old obese female, transferred for
critical care management after a bowel
resection. Presents with obtundation,
hypotension, tachypnea, and emesis.
C/O abdominal pain and has fruity breath
amylase, lipase are elevated, Na
+
127
What do you think? What do you do?
Work up?
ABG
Electrolyte panel
urine analysis
CBC
Serum Ketones
Hyperglycemia
Characteristic DKA NKHC
Glucose 400-800 > 1000
Acidosis Severe min.
Ketones High low
Dehydration Mod. High
Na 1.6 for every 100 glucose above 200
Treatment
Adequate fluid replacement
narrowing of anion gap
crystalloids: LR, NS, NS
Insulin
bolus 0.1 - 0.5 units/kg
infusion 0.1 units/kg/hour
goal reduce plasma glucose 75-100 mg/dL/hr
Electrolytes
K replacement 10-20 mEq/hour after UOP OK
Mg, PO
4
replacement
The drunk
37 year old male, h/o EtOH abuse fell from a
deer hunting tree stand. C5 fracture without
cord involvement.
HD #2 develops delirium tremors moved from
SIU to ICU. Librium started.
HD#4, dobhoff placed and tube feeds started.
That night, the patients respiratory status
worsens and he is intubated.
What do you think? What do you do?
HYPOPHOSPHATEMIA
Refeeding Syndrome
malnutrition
alcoholism
Hypophosphatemia
limits oxygen unloading
immunocompromise
muscle weakness failure to wean
Treatment
IV supplementation in emergent cases
sodium or potassium phosphorous
PO supplementation routinely
Keep (phosphorous x calcium) ratio <
60
Magnesium should be replenished
simultaneously
The burn patient
25 year male, caught fire after his
lawnmower exploded as he was filling it
with gasoline while smoking a cigarette.
The patient sustained second and third
degree burns estimated at 40 % total
body surface area.
Parkland Formula
4 cc x WEIGHT (kg) x (% TBSA)
Parkland Example
25 year old male
weight = 220 pounds
40% TBSA 2 - 3 burns
How much fluid do you need to give?
During the first 8 hours?
During the next 16 hours?
Parkland Example
4 cc x weight x %TBSA
4 x 100 x 40 = 16,000 cc/24 hours
first 8 hours = 16,000/2 =8,000/8 = 1,000cc/hr
next 16 hours = 8,000/16 = 500cc/hr
Diarrhea Dysrhythmia
68 yo female on digoxin for chronic
CHF, presents to the SIU for colitis as
evidenced by copious diarrhea.
The patient is weak and lethargic and
ectopic beats are noted on her ECG.
What do you think? What do you do?
Hypokalemia
Deficits
Serum K =
3-4 is a 100-200 mEq deficit
2-3 is a 200-400 mEq deficit
Treatment
replacement 10 mEq/hr via peripheral IV
10 mEq o 0.1 mEq/L increase in serum K
Remember to check the Mg level too
Paradoxical Aciduria
A rule: | 0.1 pH o + 0.4 - 0.5 mEq [K
+
]
pathophysiology
loss of K, severe alkalosis, |[Na
+
] load
hydrogen exchanged for K
independent of alkalosis remaining
requires emergent replacement
Cancer
72 yo female with stage 4, metastatic
breast cancer.
Patient is confused, cachetic, and
nauseated
Na
+
= 147, Ca
+2
= 14mg/dl
What do you think? What do you do?
HYPERCALCEMIA
Cancers associated
with hypercalcemia
bone
breast
kidney
colon
thyroid
multiple melanoma
Treatment
hydration
diuretics-lasix
mithramycin
corticosteroids
calcitonin-
osteoclast
resorption
phosphate
Labor and Delivery
32 year old P
3
G
3
being treated by OB
for eclampsia. You are called for a
somnolent patient in second-degree
heart block and paralysis.
What do you think? What do you do?
Hypermagnesemia
Signs
Prolonged PR interval
Hypotension, hyporeflexia, paralysis
Treatment
Calcium gluconate
Normal saline
Loop diuretics
dialysis
Questions?
Potrebbero piacerti anche
- Sagraves MSfluids Lytes 2004Documento59 pagineSagraves MSfluids Lytes 2004Burhan Ul HaqNessuna valutazione finora
- Fluids & ElectsDocumento61 pagineFluids & ElectsYousif Ahmed DANessuna valutazione finora
- IvfDocumento17 pagineIvfBima BaikuniNessuna valutazione finora
- Acute Diabetic Ketoacidosis (DKA)Documento21 pagineAcute Diabetic Ketoacidosis (DKA)Madhu Sudhan Pandeya0% (1)
- Fluid & ElectrolytesDocumento8 pagineFluid & ElectrolytesOjambo FlaviaNessuna valutazione finora
- Diabetic EmergenciesDocumento65 pagineDiabetic EmergenciesManmeet SNessuna valutazione finora
- Fluid and ElectrolyteDocumento71 pagineFluid and ElectrolytePratishtha SinghNessuna valutazione finora
- ElectrolytesDocumento65 pagineElectrolytesIgnatius Ivan PutrantyoNessuna valutazione finora
- Fluids and Electrolytes For Pediatrics: Natharina YolandaDocumento45 pagineFluids and Electrolytes For Pediatrics: Natharina YolandaTe HineahuoneNessuna valutazione finora
- Principle of Fluid & Electrolyte Management in ADocumento47 paginePrinciple of Fluid & Electrolyte Management in AAbdulazeez Abdulmalik100% (1)
- Pass Critical Care Endocrine Frcem ResourcesDocumento41 paginePass Critical Care Endocrine Frcem ResourcesYoussef SaadNessuna valutazione finora
- Keseimbangan Elektrolit Dan Asam Basa: Dr. Satriawan Abadi, SP - Pd-KicDocumento79 pagineKeseimbangan Elektrolit Dan Asam Basa: Dr. Satriawan Abadi, SP - Pd-KicInterna FKUNHASNessuna valutazione finora
- Fluid and Electrolytes: Robert Mcintyre, Jr. Associate Professor of Surgery University of Colorado Health Sciences CenterDocumento54 pagineFluid and Electrolytes: Robert Mcintyre, Jr. Associate Professor of Surgery University of Colorado Health Sciences CenterWilliam Yap WLNessuna valutazione finora
- The Pathophysiology & Practical Management of Diabetic KetoacidosisDocumento45 pagineThe Pathophysiology & Practical Management of Diabetic KetoacidosisPreetibah PatelNessuna valutazione finora
- Common Electrolyte Disturbances and Management Edited 2023Documento46 pagineCommon Electrolyte Disturbances and Management Edited 2023abdurabengNessuna valutazione finora
- Fluid and Electrolyte Therapy - SeblewongelDocumento47 pagineFluid and Electrolyte Therapy - SeblewongelSeblewongel AsemeNessuna valutazione finora
- CP2 A Mnemonic For The TreatDocumento15 pagineCP2 A Mnemonic For The Treateng78ineNessuna valutazione finora
- Fluid and Electrolyte TherapyDocumento39 pagineFluid and Electrolyte TherapyrikarzNessuna valutazione finora
- Nutrition, Fluid and Acid BaseDocumento35 pagineNutrition, Fluid and Acid BaseAmyandNessuna valutazione finora
- Final Common Medical Surgical EmergenciesDocumento99 pagineFinal Common Medical Surgical Emergenciesapi-195799092Nessuna valutazione finora
- Review: Diagnostic and Treatment of Electrolyte DisturbancesDocumento31 pagineReview: Diagnostic and Treatment of Electrolyte DisturbancesalvyandaniNessuna valutazione finora
- IV FluidsDocumento47 pagineIV FluidsMuvenn Kannan100% (1)
- Diabetic Emergencies by DR Gireesh Kumar K P, Department of Emergency Medicine, Amrita Institute of Medical Sciences, KochiDocumento23 pagineDiabetic Emergencies by DR Gireesh Kumar K P, Department of Emergency Medicine, Amrita Institute of Medical Sciences, KochiSreekrishnan Trikkur100% (2)
- Seminar RDocumento93 pagineSeminar Rmubarak abdulkadirNessuna valutazione finora
- Fluid & Electrolyte ImbalanceDocumento47 pagineFluid & Electrolyte ImbalanceBijeta ThapaNessuna valutazione finora
- TWIS, Fluid and Electrolytes-4Documento45 pagineTWIS, Fluid and Electrolytes-4Madison FNessuna valutazione finora
- Keseimbangan Elektrolit Dan Asam Basa: Dr. Satriawan Abadi, SP - Pd-KicDocumento79 pagineKeseimbangan Elektrolit Dan Asam Basa: Dr. Satriawan Abadi, SP - Pd-KicSteven KatuukNessuna valutazione finora
- Diabetic Ketoacidosis (DKA) - Presentation Slide EditedDocumento22 pagineDiabetic Ketoacidosis (DKA) - Presentation Slide EditedTerence Chin0% (1)
- Fluids and ElectrolytesDocumento31 pagineFluids and ElectrolytesUmarNessuna valutazione finora
- Electrolyte ImbalanceDocumento44 pagineElectrolyte ImbalanceDevi Christina Damanik (Papua medical School)Nessuna valutazione finora
- Fluids and Electrolytes: Rafael Alphonso Pintacasi Class 2016Documento32 pagineFluids and Electrolytes: Rafael Alphonso Pintacasi Class 2016Ponchoi PintacasiNessuna valutazione finora
- Chemistry Studies & Lyte DisturbancesDocumento14 pagineChemistry Studies & Lyte DisturbancesBaneenNessuna valutazione finora
- HypocalcemiaDocumento34 pagineHypocalcemiaClaudia IrimieNessuna valutazione finora
- Diabetes Emergencies ComplicationsDocumento30 pagineDiabetes Emergencies Complicationsosamafoud7710Nessuna valutazione finora
- Hyperkalemia: Michael Levin, D.O. Medical Resident PGY II P.C.O.MDocumento22 pagineHyperkalemia: Michael Levin, D.O. Medical Resident PGY II P.C.O.MsuviacesoNessuna valutazione finora
- Hyperkalemia SyedDocumento58 pagineHyperkalemia SyedSyed Shahrul Naz SyedNessuna valutazione finora
- Fluid and Electrolyte Imbalance 0Documento42 pagineFluid and Electrolyte Imbalance 0rismarini.asantiNessuna valutazione finora
- Fluids ElectrolytesDocumento37 pagineFluids ElectrolytesAlpascaFirdausNessuna valutazione finora
- Somchodok Chakreeyarat, MD. Endocrine Unit, Department of Medicine Bhumibol Adulyadej HospitalDocumento53 pagineSomchodok Chakreeyarat, MD. Endocrine Unit, Department of Medicine Bhumibol Adulyadej HospitalLing TaerahkunNessuna valutazione finora
- Diabetic KetoacidosisDocumento22 pagineDiabetic KetoacidosismartinNessuna valutazione finora
- Fluids&Lytes PediatricDocumento33 pagineFluids&Lytes Pediatricnugraha_esaNessuna valutazione finora
- Fluid - Electrolyte Imbalance 2012-InedDocumento45 pagineFluid - Electrolyte Imbalance 2012-InedmiamuhpianNessuna valutazione finora
- UNIT 3.1 - AHN - Fluid & Electrolyte ImbalanceDocumento31 pagineUNIT 3.1 - AHN - Fluid & Electrolyte Imbalanceannududi378556Nessuna valutazione finora
- DR Omar Kamal Ansari Dept of AnaesthesiologyDocumento46 pagineDR Omar Kamal Ansari Dept of Anaesthesiologyvvb_frndNessuna valutazione finora
- S.gaus-Management of Life-Threatening (Kuliah Sistem)Documento54 pagineS.gaus-Management of Life-Threatening (Kuliah Sistem)Rusmin UsmanNessuna valutazione finora
- Too Many Normal Saline? Fluids in Various ConditionDocumento26 pagineToo Many Normal Saline? Fluids in Various ConditionHandrian RahmanNessuna valutazione finora
- Pleno Minggu 2 Blok 3.4Documento84 paginePleno Minggu 2 Blok 3.4Devi Yunita PurbaNessuna valutazione finora
- Case Study: Diabetic KetoacidosisDocumento66 pagineCase Study: Diabetic Ketoacidosisllaychin100% (2)
- Fluid & Electrolyte Balance: PresentedDocumento30 pagineFluid & Electrolyte Balance: PresentedFathimathNessuna valutazione finora
- Pediatric Fluid and Electrolyte TherapyDocumento27 paginePediatric Fluid and Electrolyte TherapyNanda Cendikia100% (1)
- DKA Concepts and ManagementDocumento22 pagineDKA Concepts and ManagementMohammad AliNessuna valutazione finora
- Fluids (4th)Documento17 pagineFluids (4th)180045Nessuna valutazione finora
- Review of LaboratoryDocumento48 pagineReview of LaboratoryIkhar RidhoNessuna valutazione finora
- Hippo EM Board Review - Electrolyte Emergencies Written SummaryDocumento5 pagineHippo EM Board Review - Electrolyte Emergencies Written SummaryMichael IvanNessuna valutazione finora
- Fluid & Elec DidacticsDocumento64 pagineFluid & Elec DidacticsTonie AbabonNessuna valutazione finora
- EMERGENCIES IN DM (KAD Dan HHS)Documento26 pagineEMERGENCIES IN DM (KAD Dan HHS)ozNessuna valutazione finora
- Fluids&LytesDocumento33 pagineFluids&LytesMateen ShukriNessuna valutazione finora
- Fluids and Electrolyte DisordersDocumento74 pagineFluids and Electrolyte DisordersPrincewill SeiyefaNessuna valutazione finora
- Diagnostic Value of WBC and CRP in Peds Appendicitis PDFDocumento6 pagineDiagnostic Value of WBC and CRP in Peds Appendicitis PDFAsad Khan KhalilNessuna valutazione finora
- Neurology TipsDocumento455 pagineNeurology TipsAsad Khan KhalilNessuna valutazione finora
- The Cardiac Cycle NotesDocumento5 pagineThe Cardiac Cycle NotesAsad Khan Khalil100% (1)
- Objectives: CH 20: Integrative Physiology II Fluid & Electrolyte BalanceDocumento23 pagineObjectives: CH 20: Integrative Physiology II Fluid & Electrolyte BalanceAsad Khan KhalilNessuna valutazione finora
- Inflammatory Bowel Disease WardDocumento103 pagineInflammatory Bowel Disease WardAsad Khan KhalilNessuna valutazione finora
- CCFDocumento18 pagineCCFAsad Khan KhalilNessuna valutazione finora
- Santhigiri Siddha Therapeutic GuideDocumento36 pagineSanthigiri Siddha Therapeutic Guidedrkiranrk83% (6)
- Test Bank For Clinical Manifestations and Assessment of Respiratory Disease 8th Edition by Des JardinsDocumento14 pagineTest Bank For Clinical Manifestations and Assessment of Respiratory Disease 8th Edition by Des JardinsJohn Molon100% (44)
- MycosisDocumento5 pagineMycosisMaiWahidGaberNessuna valutazione finora
- Lesson Plan On Electroconvulsive TherapyDocumento13 pagineLesson Plan On Electroconvulsive Therapysimranjeet kaurNessuna valutazione finora
- Fgi Guidelines 2014 Hop TocDocumento10 pagineFgi Guidelines 2014 Hop TocZaw Moe KhineNessuna valutazione finora
- Glucose-Loesung 5 08-07 03Documento2 pagineGlucose-Loesung 5 08-07 03Andreea CaticiNessuna valutazione finora
- Erbe Apc 300 User ManualDocumento108 pagineErbe Apc 300 User ManualDavid HernandezNessuna valutazione finora
- Therapeutic Modalities: Prepared By: John Patrick B. de JesusDocumento22 pagineTherapeutic Modalities: Prepared By: John Patrick B. de JesusChiee A. CentinoNessuna valutazione finora
- WaterDocumento26 pagineWaterKisna Bhurtel100% (1)
- Lindo Wing Brochure Web VersionDocumento16 pagineLindo Wing Brochure Web VersionNetwerk24Nessuna valutazione finora
- Upper Respiratory Tract InfectionDocumento45 pagineUpper Respiratory Tract InfectionNatasha Abdulla100% (2)
- Syllabus ElectrotherapyDocumento4 pagineSyllabus ElectrotherapySYED ALI HUSSAINNessuna valutazione finora
- NCP and Drug StudyDocumento11 pagineNCP and Drug StudyTonio PagaoNessuna valutazione finora
- KuesionerDocumento2 pagineKuesionerMuklis Al FadlikaNessuna valutazione finora
- 2212-02e TPB PAC Liquid 10Documento1 pagina2212-02e TPB PAC Liquid 10Saefuddin SaefuddinNessuna valutazione finora
- Modul UrologyDocumento49 pagineModul UrologysonyNessuna valutazione finora
- Chronic Renal FailureDocumento18 pagineChronic Renal FailureJoan Carla BocoNessuna valutazione finora
- PT ProgProgressionPattern 20150825Documento2 paginePT ProgProgressionPattern 20150825yotta024Nessuna valutazione finora
- Chapter 14Documento15 pagineChapter 14missy23papNessuna valutazione finora
- Extraordinary Published by Authority No. 1235, Cuttack Saturday, June 29, 2013/ ASADHA 8, 1935 Law DepartmentDocumento9 pagineExtraordinary Published by Authority No. 1235, Cuttack Saturday, June 29, 2013/ ASADHA 8, 1935 Law DepartmentVikash GoelNessuna valutazione finora
- Tammy, 2011. Drug Interaction PDFDocumento14 pagineTammy, 2011. Drug Interaction PDFdyahNessuna valutazione finora
- RMDocumento10 pagineRMdanielNessuna valutazione finora
- Thyriodectomy BrochureDocumento2 pagineThyriodectomy BrochureHeedahNessuna valutazione finora
- Visual Schedules For Kids With AutismDocumento9 pagineVisual Schedules For Kids With AutismAutism Parenting75% (8)
- Unraveling The Mechanisms of Manual Therapy: Modeling An ApproachDocumento12 pagineUnraveling The Mechanisms of Manual Therapy: Modeling An ApproachCollin AndrusNessuna valutazione finora
- Wastewater Disposal.Documento266 pagineWastewater Disposal.FarazNessuna valutazione finora
- K SADS FragebogenDocumento241 pagineK SADS Fragebogenark1974Nessuna valutazione finora
- School-Based Play Therapy: Second EditionDocumento12 pagineSchool-Based Play Therapy: Second EditionWuDennisNessuna valutazione finora
- Montana Do Not Resuscitate FormDocumento2 pagineMontana Do Not Resuscitate FormitargetingNessuna valutazione finora
- ASD Interventions Theories, Age Range and SettingsDocumento4 pagineASD Interventions Theories, Age Range and SettingstracycwNessuna valutazione finora