Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Iron Metabolism
Caricato da
Daniel MatiusDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Iron Metabolism
Caricato da
Daniel MatiusCopyright:
Formati disponibili
Iron Metabolism
Iron is a critical element in the function of all cells, although the amount of iron required by individual tissues varies during development. At the same time, the body must protect itself from free iron, which is highly toxic in that it participates in chemical reactions that generate free radicals such as singlet O2 or OH-. Consequently, elaborate mechanisms have evolved that allow iron to be made available for critical physiologic functions while at the same time conserving this element and handling it in such a way that toxicity is avoided.
The major role of iron in mammals is to carry O2 as part of the heme protein that, in turn, is part of hemoglobin. O2 is also bound by a heme protein in muscle, myoglobin. Iron is a critical element in iron containing enzymes, including the cytochrome system in mitochondria; Without iron, cells lose their capacity for electron transport and energy metabolism; in erythroid cells hemoglobin synthesis is impaired, resulting in anemia and reduced O2 delivery to tissue.
Absorption of iron
Iron absorption takes place largely in the proximal small intestine and is a carefully regulated process. For absorption, iron must be taken up by the luminal cell. That process is facilitated by the acidic contents of the stomach, which maintains the iron in solution. At the brush border of the absorptive cell, the ferric iron is converted to the ferrous form by a ferrireductase.
Transport across the membrane is accomplished by divalent metal transporter 1 (DMT1, also known as Nramp2 or DCT1). DMT1 is a general cation transporter. Once iron is inside the gut cell, the iron may be stored as ferritin or transported through the cell to be released at the basolateral surface to plasma transferrin. It is likely that another transporter acts here in concert with hephaestin, another ferroxidase. Hephaestin is similar to ceruloplasmin, the copper-carrying protein.
Iron absorption is influenced by a number of physiologic states. Erythroid hyperplasia, for example, stimulates iron absorption, even in the face of normal or increased iron stores. Patients with anemias associated with high levels of ineffective erythropoiesis absorb excess amounts of dietary iron. Over time, this may lead to iron overload and tissue damage. In iron deficiency, iron is much more efficiently absorbed from a given diet; the contrary is true in the presence of iron overload. This is possibly mediated through signals that become fixed before the jejunal crypt cell migrates up the villus to become an absorptive cell.
The normal individual can reduce iron absorption in situations of excessive intake or medicinal iron intake; however, while the percentage of iron absorbed goes down, the absolute amount goes up. This accounts for the acute iron toxicity occasionally seen when children ingest large numbers of iron tablets. Under these circumstances, the amount of iron absorbed exceeds the transferrin binding capacity of the plasma, resulting in free iron that affects critical organs such as cardiac muscle cells.
Absorption of iron. Fe3+ is converted to Fe2+ by ferric reductase, and Fe2+ is transported into the enterocyte by the apical membrane iron transporter DMT1. Heme is transported into the enterocyte by a separate heme transporter (HT), and HO2 releases Fe2+ from the heme. Some of the intracellular Fe2+ is converted to Fe3+ and bound to ferritin. The rest binds to the basolateral Fe2+ transporter ferroportin (FP) and is transported to the interstitial fluid. The transport is aided by hephaestin (Hp). In plasma,Fe2+ is converted to Fe3+ and bound to the iron transport protein transferrin (TF).
Enterocytes in the proximal duodenum are responsible for absorption of iron. Incoming iron in the Fe3+ state is reduced to Fe2+ by a ferrireductase present on the surface of enterocytes. Vitamin C in food also favors reduction of ferric iron to ferrous iron. The transfer of iron from the apical surfaces of enterocytes into their interiors is performed by a proton-coupled divalent metal transporter (DMT1). This protein is not specific for iron, as it can transport a wide variety of divalent cations.
A peptide appears to play an important role in iron metabolism (25 amino acids, synthesized by liver cells) named hepcidin It down-regulates the intestinal absorption and placental transfer of iron and also the release of iron from macrophages, possibly by interaction with ferroportin. When plasma levels of iron are high, synthesis of hepcidin increases; the opposite occurs when plasma levels of iron are low may play an important role in hemochromatosis and also in the iron deficiency anemia seen in chronic inflammatory conditions. Another protein named hemojuvelin may act by modulating the expression of hepcidin.
Once inside an enterocyte, iron can either be stored as ferritin or transferred across the basolateral membrane into the plasma, where it is carried by transferrin. Passage across the basolateral membrane appears to be carried out by another protein, ferroportin. This protein may interact with the copper-containing protein hephaestin, a protein similar to ceruloplasmin. Hephaestin is thought to have a ferroxidase activity, which is important in the release of iron from cells. Thus, Fe2+ is converted back to Fe3+, the form in which it is transported in the plasma by transferrin.
The Iron Cycle In Humans
Iron absorbed from the diet or released from stores circulates in the plasma bound to transferrin, the iron transport protein. Transferrin is a bilobed glycoprotein with two iron binding sites. Transferrin that carries iron exists in two forms monoferric (one iron atom) or diferric (two iron atoms). The turnover (half-clearance time) of transferrin-bound iron is very rapidtypically 60 to 90 min. Because the overwhelming majority of iron transported by transferrin is delivered to the erythroid marrow, the clearance time of transferrin-bound iron from the circulation is affected most by the plasma iron level and the activity of the erythroid marrow. When erythropoiesis is markedly stimulated, the pool of erythroid cells requiring iron increases and the clearance time of iron from the circulation decreases
The half-clearance time of iron in the presence of iron deficiency is as short as 10 to 15 min; this value reflects the limits of iron delivery as a function of the cardiac output going to the bone marrow. With suppression of the erythroid marrow, the plasma iron level typically is increased and the half-clearance time is prolonged to as much as several hours. Normally, the iron bound to transferrin turns over 10 to 20 times per day. Assuming a normal plasma iron level of 80 to 100 g/dL, the amount of iron passing through the transferrin pool is 20 to 24 mg/d.
The iron-transferrin complex circulates in the plasma until the ironcarrying transferrin interacts with specific transferrin receptors on the surface of marrow erythroid cells. Diferric transferrin has the highest affinity for transferrin receptors; apotransferrin (transferrin not carrying iron) has very little affinity. While transferrin receptors are found on cells in many tissues within the bodyand all cells at some time during development will display transferrin receptorsthe cell having the greatest number of receptors (300,000 to 400,000/cell) is the developing erythroblast.
Once the iron-bearing transferrin interacts with its receptor, the iron-transferrin-receptor complex is internalized via clathrin-coated pits and transported to an acidic endosome, where the iron is released at the low pH. The iron is then made available for heme synthesis while the transferrin-receptor complex is recycled to the surface of the cell, where the bulk of the transferrin is released back into the circulation and the transferrin receptor reanchors into the cell membrane. At this point a certain amount of the transferrin receptor protein may be released into circulation.
Within the erythroid cell, iron that is in excess of the amount needed for hemoglobin synthesis binds to a storage protein, apoferritin, forming ferritin. This mechanism of iron exchange also takes place in other cells of the body expressing transferrin receptors, especially liver parenchymal cells where the iron can be incorporated into hemecontaining enzymes or stored. The iron incorporated into hemoglobin subsequently enters the circulation as new red cells are released from the bone marrow. The iron is then part of the red cell mass and will not become available for reutilization until the red cell dies.
In a normal individual, the average red cell life span is 120 days. Thus, 0.8 to 1.0% of red cells turn over each day. At the end of its life span, the red cell is recognized as senescent by the cells of the reticuloendothelial (RE) system, and the cell undergoes phagocytosis. Once within the RE cell, the hemoglobin from the ingested red cell is broken down, the globin and other proteins are returned to the amino acid pool, and the iron is shuttled back to the surface of the RE cell, where it is presented to circulating transferrin. The harvesting of iron from senescent red cells is both efficient and rapid, with newly recycled iron appearing in the circulation within 10 min of ingestion of the red cell. It is the efficient and highly conserved recycling of iron from senescent red cells that supports steady state (and even mildly accelerated) erythropoiesis.
Since each milliliter of red cells contains 1 mg of elemental iron, the amount of iron needed to replace those red cells lost through senescence amounts to 16 to 20 mg/d (assuming an adult with a red cell mass of 2 L). Any additional iron required for daily red cell production comes from the diet. Normally, an adult male will need to absorb at least 1 mg of elemental iron daily to meet needs, while females in the childbearing years will need to absorb an average of 1.4 mg/d. However, to achieve a maximum proliferative erythroid marrow response to anemia, additional iron must be available.
With markedly stimulated erythropoiesis, demands for iron are increased by as much as six- to eightfold. With hemolytic anemias, the rate of red cell destruction is increased, but the iron recovered from the red cells is efficiently reutilized for hemoglobin synthesis. In contrast, with blood loss anemia the rate of red cell production is limited by the amount of iron that can be mobilized from ferritin and hemosiderin stores. Typically, the rate of mobilization under these circumstances will not support red cell production more than 2.5 to 3 times normal. If the delivery of iron to the stimulated marrow is suboptimal, the marrows proliferative response is blunted and normal hemoglobin synthesis is impaired. The result is a hypoproliferative marrow accompanied by microcytic, hypochromic anemia.
While blood loss or hemolysis places a demand for iron to be supplied to the erythroid marrow, other conditions such as inflammation interfere with iron release from stores and can result in a rapid decrease in the serum iron
Potrebbero piacerti anche
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Management of Severe Malaria: Paul N HarijantoDocumento56 pagineManagement of Severe Malaria: Paul N HarijantoDaniel MatiusNessuna valutazione finora
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Who2006 Growth StandardDocumento74 pagineWho2006 Growth StandardDaniel MatiusNessuna valutazione finora
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Abdominal PainDocumento10 pagineAbdominal PainDaniel MatiusNessuna valutazione finora
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Case Report Tiroid - WordDocumento2 pagineCase Report Tiroid - WordDaniel MatiusNessuna valutazione finora
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
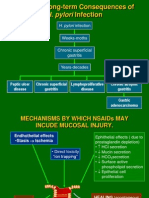
- Pathogenesis Tukak LambungDocumento30 paginePathogenesis Tukak LambungDaniel MatiusNessuna valutazione finora
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Acute PancreatitisDocumento7 pagineAcute PancreatitisDaniel MatiusNessuna valutazione finora
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Enzymes and SubstratesDocumento19 pagineEnzymes and SubstratesDaniel MatiusNessuna valutazione finora
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- BPH Score IndexDocumento1 paginaBPH Score IndexDaniel MatiusNessuna valutazione finora
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Sirosis HepatisDocumento40 pagineSirosis HepatisDaniel Matius100% (1)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Sirosis - NephroticDocumento5 pagineSirosis - NephroticDaniel MatiusNessuna valutazione finora
- Chlamydia SlidesDocumento63 pagineChlamydia SlidesEspecialistaLanderNessuna valutazione finora
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Chickenpox in ChildrenDocumento26 pagineChickenpox in ChildrenDaniel MatiusNessuna valutazione finora
- Kuliah HypertensiDocumento56 pagineKuliah HypertensiDaniel MatiusNessuna valutazione finora
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- Netter 1Documento27 pagineNetter 1Daniel MatiusNessuna valutazione finora
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- R.Schoen, R.Vender. Am J Med 1989Documento15 pagineR.Schoen, R.Vender. Am J Med 1989Daniel MatiusNessuna valutazione finora
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Netter 2Documento12 pagineNetter 2Daniel Matius100% (1)
- GUIDED READING & Video Notes - Cell Membrane & TransportDocumento4 pagineGUIDED READING & Video Notes - Cell Membrane & TransportMs. BainNessuna valutazione finora
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- PlantDerived Edible Nanoparticles and MiRNAs Emerging Frontier For Therapeutics and Targeted DrugDeliveryDocumento15 paginePlantDerived Edible Nanoparticles and MiRNAs Emerging Frontier For Therapeutics and Targeted DrugDeliveryS. MartinezNessuna valutazione finora
- Basic Techniques in Pet Avian Clinical PathologyDocumento23 pagineBasic Techniques in Pet Avian Clinical PathologyJessica RuizNessuna valutazione finora
- Gen Bio 2NDDocumento5 pagineGen Bio 2NDZyren Joy SamillanoNessuna valutazione finora
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Lehninger Principles of Biochemistry 4/e Errata: Corrections Made in Second PrintingDocumento4 pagineLehninger Principles of Biochemistry 4/e Errata: Corrections Made in Second PrintingYara Luiza CoelhoNessuna valutazione finora
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Sonu 26S00230050665Documento1 paginaSonu 26S00230050665Rakesh KoliNessuna valutazione finora
- Sowdambikaa Group of Schools: Bio - Botany I. Choose The Best Answer: (5x1 5)Documento2 pagineSowdambikaa Group of Schools: Bio - Botany I. Choose The Best Answer: (5x1 5)fireNessuna valutazione finora
- Protein Science - 2021 - Rai - Liquid Liquid Phase Separation of Tau From Molecular Biophysics To Physiology and DiseaseDocumento21 pagineProtein Science - 2021 - Rai - Liquid Liquid Phase Separation of Tau From Molecular Biophysics To Physiology and DiseaseKeshav JhalaniNessuna valutazione finora
- Expression of Cloned Proteins in Animal Cells PDFDocumento2 pagineExpression of Cloned Proteins in Animal Cells PDFFeliciaNessuna valutazione finora
- 9700 m18 QP 22 PDFDocumento16 pagine9700 m18 QP 22 PDFIG UnionNessuna valutazione finora
- Mitosis WorksheetDocumento4 pagineMitosis WorksheetAmna Jamshed67% (3)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Lab Report 3 Cellular RespirationDocumento3 pagineLab Report 3 Cellular Respirationapi-490246824Nessuna valutazione finora
- NSTSE Sample Paper Class 9Documento4 pagineNSTSE Sample Paper Class 9Jleodennis RajNessuna valutazione finora
- USA Biology Olympiad 2003 Open Exam Answer KeyDocumento11 pagineUSA Biology Olympiad 2003 Open Exam Answer KeyLauren HuangNessuna valutazione finora
- Onion Cell Plasmolysis Lab Version 1Documento4 pagineOnion Cell Plasmolysis Lab Version 1luckyduck28690% (1)
- Photosynthesis: Rafia Urooj Saman 2020-Ag-937Documento18 paginePhotosynthesis: Rafia Urooj Saman 2020-Ag-937Rafya ShabbirNessuna valutazione finora
- Soalan Objektif Mac2014Documento2 pagineSoalan Objektif Mac2014Siti NajwaNessuna valutazione finora
- Agascalm Brossúra01Documento21 pagineAgascalm Brossúra01vukicsvikiNessuna valutazione finora
- Tugas ApolipoproteinDocumento8 pagineTugas ApolipoproteinSeptiany Christin PalilinganNessuna valutazione finora
- 10 1038@nrdp20156Documento17 pagine10 1038@nrdp20156Desi DwiNessuna valutazione finora
- Abstract BookDocumento241 pagineAbstract BookMuhammad AsaduzzamanNessuna valutazione finora
- Bio Eoc Review Session 1 Questions 11-12Documento6 pagineBio Eoc Review Session 1 Questions 11-12api-269873615Nessuna valutazione finora
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- 1 Resveratrol Internat Immunopharm2019Documento13 pagine1 Resveratrol Internat Immunopharm2019Mtro. Javier Alfredo Carballo PereaNessuna valutazione finora
- TranscriptionDocumento72 pagineTranscriptionMurthy MandalikaNessuna valutazione finora
- NucleusDocumento58 pagineNucleusImperiall100% (1)
- Pyroptosis: Gasdermin-Mediated Programmed Necrotic Cell DeathDocumento10 paginePyroptosis: Gasdermin-Mediated Programmed Necrotic Cell DeathSangat BaikNessuna valutazione finora
- IB HL BIO FULL NOTES (Onarıldı)Documento874 pagineIB HL BIO FULL NOTES (Onarıldı)Sıla DenizNessuna valutazione finora
- Plants and Society 7th Edition Levetin Test BankDocumento35 paginePlants and Society 7th Edition Levetin Test Bankconjectxanthinev76r100% (23)
- Prelims Micropara LecDocumento14 paginePrelims Micropara LecBSN1F- JACILDO, KUH KYLA C.Nessuna valutazione finora
- PHrodo Red Cell Labeling Kit For IncucyteDocumento7 paginePHrodo Red Cell Labeling Kit For Incucyte李琇琴Nessuna valutazione finora