Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
2001 Lameness
Caricato da
Zozo MostafaDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
2001 Lameness
Caricato da
Zozo MostafaCopyright:
Formati disponibili
THE
VETERINARY
CLINICS OF
NORTH
AMERICA
lCOMPRAI
SMALL ANIMAL PRACTICE
Lameness
WALTER C. RENBERG, DVM, MS, AND
JAMES K. ROUSH, DVM, MS
SERVoI,OS DE E DE tXiEtlSA8
V.T.A.D.
2 r; f65YO
N . ... ..2 ........................... .... - ..
Clus . ....................................
VOLUME 31 NUMBER 1
W.B. SAUNDERS COMPANY
A Harcourt Health Sciences Company
PHILADELPHIA LONDON TORONTO MONTREAL
JANUARY 2001
W.B. SAUNDERS COMPANY
A Harcourt Health Sciences Company
The Curtis Center' Independence Square West Philadelphia, Pennsylvania 19106
http: //www.wbsaunders.com
THE VETERINARY CLINICS OF NORTH AMERICA:
SMALL ANIMAL PRACTICE
January 2001
Editor: John Vassallo
Volume 31, Number 1
ISSN 0195-5616
Copyright 2001 by W.B. Saunders Company. All rights reserved. No part of this
publication may be reproduced or transmitted in any form or by any means, electronic or
mechanical, including photocopy, recording, or any information retrieval system, without
written permission from the Publisher.
The appearance of the code at the top of the first page of an article in this periodical
indicates the consent of the W.B. Saunders Company that copies of the article may be
made for personal or internal use, or for the personal or internal use of specific clients, for
those registered with the Copyright Clearance Center, Inc. (222 Rosewood Drive, Danvers, MA
01923: (978) 750-8400; www.copyright. com). This consent is given on the condition that the
copier pay the stated per-copy fee for that article through the Copyright Clearance Center,
Inc. for copying beyond that permitted by Sections 107 or 108 of the US Copyright Law.
This consent does not extend to other kinds of copying, such as copying for general
distribution, for advertising or promotional purposes, for creating new collective works,
or for resale. Absence of the code indicates that the material may not be processed through
the Copyright Clearance Center, Inc.
The ideas and opinions expressed in The VeterinanJ Clinics of North America: Small Animal
Practice do not necessarily reflect those of the Publisher. The Publisher does not assume
any responsibility for any injury andlor damage to persons or property arising out of or
related to any use of the material contained in this periodical. The reader is advised to
check the appropriate medical literature and the product information currently provided
by the manufacturer of each drug to be administered to verify the dosage, the method
and duration of administration, or contraindications. It is the responsibility of the treating
physician or other health care professional, relying on independent experience and knowl-
edge of the patient, to determine drug dosages and the best treatment for the patient.
Mention of any product in this issue should not be construed as endorsement by the
contributors, editors, or the Publisher of the product or manufacturers' claims.
The Veterinary Clinics of North America: Small Animal Practice (ISSN 0195-5616) is published
bimonthly by W.B. Saunders Company. Corporate and editorial offices: The Curtis Center,
Independence Square West, Philadelphia, PA 19106-3399. Accounting and circulation of-
fices: 6277 Sea Harbor Drive, Orlando, FL 32887-4800. Periodicals postage paid at Orlando,
FL 32862, and additional mailing offices. Subscription prices are $145.00 per year (U.S.
individuals), $195.00 per year (U.S. institutions), $177.00 per year (Canadian individuals),
$249.00 per year (Canadian institutions), $199.00 per year (foreign individuals), and $249.00
per year (foreign institutions). F o ~ e i g n air speed delivery is included in all Clinics subscrip-
tion prices. All prices are subject. to change without notice. POSTMASTER: Send address
changes to The Veterinary Clinics of North America: Small Animal Practice, W.B. Saunders
Company, Periodicals Fulfillment, Orlando, FL 32887-4800. Customer Service: 1-800-654-
2452 (US). From outside of the US; call 1-407-345-4000.
The Veterinary Clinics of North America: Small Animal Practice is also published in Italian by
Antonio Delfino Editore, Via Udine 32/40,00161 Rome, Italy; and in Japanese by Gaku-
sosha Company Ltd., 2-16-28 Nishikata, Bunkyo-ku, Tokyo 113, Japan.
The Veterinary Clinics of North America: Small Animal Practice is covered in Current Conceptsl
Agriculture, Science Citation Index, ASCA, Index Medicus, BiologtJ and Environmental Sciences,
Excerpta Medica, and BIOSIS.
Printed in Jhe United States of America . .
LAMENESS
GUEST EDITORS
WALTER C. RENBERG, DVM, MS, Diplomate, American College of Veterinary
Surgeons; Assistant Professor, Small Animal Surgery, Department of Clinical
Sciences, Kansas State University, College of Veterinary Medicine, Manhattan,
Kansas
JAMES K. ROUSH, DVM, MS, Diplomate, American College of Veterinary Surgeons;
Associate Professor and Section Head, Small Animal Surgery, Department of Clinical
Sciences, Kansas State University, College of Veterinary Medicine, Manhattan,
Kansas
CONTRIBUTORS
LEIGH A. CLAYTON, DVM, Department of Animal Health, Smithsonian National
Zoological Park, Washington, DC
JAMES L. COOK, DVM, PhD, Diplomate, American College of Veterinary Surgeons;
Assistant Professor, Small Animal Orthopaedics, Assistant Professor, Orthopaedic
Surgery, and Director, Comparative OrthopaediC Laboratory, University of Missouri-
Columbia, Columbia, Missouri
JAMES J. HOSKINSON, DVM, Diplomate, Al!lerican College of Veterinary Radiology;
Associate Professor, Kansas State University, College of Veterinary Medicine,
Manhattan, Kansas
SPENCER A. JOHNSTON, VMD, Diplomate, American College of Veterinary Surgeons;
Associate Professor, Department of Small Animal Clinical Sciences, Virginia-
Maryland Regional College of Veterinary Medicine, Virginia Tech, Blacksburg,
Virginia
CYNTHIA ANNE LEONARD, DVM, Department of Small Animal Surgery, Veterinary
Teaching Hospital, Ontario Veterinary College, University of Guelph, Guelph,
Ontario
JOHN J. McDONNELL, DVM, MS, Diplomate, American College of Veterinary Internal
Medicine (Neurology); Assistant Professor, Department of Clinical Sciences, School
of Veterinary Medicine, Tufts University, North Grafton, Massachusetts
RON M. McLAUGHLIN, DVM, DVSc, Diplomate, American College of Veterinary
Surgeons; Associate Professor and Chief of Surgery, The Animal Health Center,
College of Veterinary Medicine, Mississippi State University, Mississippi State,
Mississippi
iii
SIMON R. PLATT, BVM&S, Diplomate, American College of Veterinary Internal
Medicine (Neurology); Assistant Professor, The Animal Health Trust, Centre for
Small Animal Studies, Lanwades Park, Kentford, Newmarket, Suffolk, England
MARY ANN RADLINSKY, DVM, MS, Diplomate, American College of Veterinary
ASSIstant Professor, Small Animal Surgery, Department of Clinical
SCIences, Kansas State University, Veterinary Medical Teaching Hospital, Manhattan,
Kansas
WALTER C. RENBERG, DVM, MS, Diplomate, American College of Veterinary
Surgeons; ASSIstant Professor, Small Animal Surgery, Department of Clinical
Sciences, Kansas State University, College of Veterinary Medicine, Manhattan,
Kansas .
JAMES K ROUSH, DVM, MS, Diplomate, American College of Veterinary Surgeons;
Professor and Section Head, Small Animal Surgery, Department of Clinical
SCIences, Kansas State UniverSity, Cqllege of Veterinary Medicine, Manhattan,
Kansas ..
KURT S. SCHULZ, DVM, MS, Diplomate, American College of Veterinary Surgeons;
ASSIstant. and Chief of Small Animal Surgery, Department of Surgical and
RadlOlogIcal SCIences, School of Veterinary Medicine, University of California Davis
California ' ,
MICHAEL TILLSON, DVM, Diplomate, American College of Veterinary Surgeons;
ASSIstant Professor, Small Animal Surgery, Auburn University College of Veterinary
Medicine, Auburn, Alabama
RUSSELL 1. TUCKER, DVM: Diplomate, American College of Veterinary Radiology;
ASSIstant Professor, Washington State University, College of Veterinary Medicine,
Pullman, Washington
iv
CONTRIBUTORS
LAMENESS
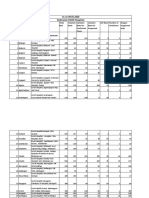
CONTENTS
Preface
Walter C. Renberg and James K. Roush
Evaluation of the Lame Patient
Walter C. Renberg
Competence in evaluating lameness is vital for the veterinary
practitioner. This skill is becoming even more important with the
increasing popularity of large-breed dogs and the corresponding
increase in the number of developmental orthopedic problems
seen on a day-to-day basis. A proper physical examination of the
lame patient is essential to the management of the case. This
article reviews the initial evaluation of the lame veterinary patient
without dwelling on the specific differential diagnoses and corres-
ponding treatments.
Neurologic Conditions Causing Lameness in
Companion Animals
John J. McDonnell, Simon R. Platt, and Leigh A. Clayton
Neurologic disease can cause lameness mimicking orthopedic
disease in companion animals. This article presents a logical step-
wise approach to help differentiate between orthopedic and
neurologic causes of lameness. The neurologic examination, diag-
nostic techniques, and treatment options for these challenging
cases are discussed. Specific diseases examined include myopa-
thies, neuropathies, intervertebral disk disease, lumbosacral dis-
ease, peripheral nerve sheath tumors, spinal cord tumors, and
traumatic neuropathies.
VETERINARY CLINICS OF NORTH AMERICA:
SMALL ANIMAL PRACTICE
VOLUME 31 NUMBER 1 JANUARY 2001
xi
1
17
v
Overview of Pain in the Lame Patient
Spencer A. Johnston
The experience of pain is often associated with the stimulation
of peripheral nociceptors. These neuroreceptors are activated by
stimuli sufficient to potentially or actually cause tissue damage.
This article reviews the types of neuroreceptors present in periar-
ticular tissues, the changes that occur in the periarticular tissues
associated with joint injury, and how those changes can influence
nociceptor activity and subsequently pain. Peripheral nociceptor
activity, as well as the influence of nociceptive input on the spinal
transmission of neural impulses, is discussed.
Forelimb Lameness in the Young Patient
James L. Cook
This article discusses causes of forelimb lameness in dogs
younger than 1 year of age. The major categories covered include
congenital, developmental, traumatic, infectious, nutritional, met-
abolic, and neoplastic disorders. Diagnosis, treatment options,
and prognosis are covered for each disorder.
Forelimb Lameness in the Adult Patient
Kurt S. Schulz
Lameness of the forelimb may be one of the more frustrating
problems in small animal orthopedics. It is likely that numerous
causes of forelimb lameness are not yet defined or well under-
stood. The common and some less common causes of forelimb
lameness are discussed as well as their means of diagnosis. The
application of new diagnostic tools including arthroscopy and
ultrasound are also discussed.
Hind Limb Lameness in the Young Patient
Ron M. McLaughlin
This article reviews the common causes of hind limb lameness in
young dogs. Legg-Calve-Perthes, hip dysplasia, cruciate ligament
injury, patella luxation, osteochondrosis, hypertrophic osteodys-
trophy, panosteitis, and common growth plate fractures are de-
scribed. Emphasis is placed on the clinical signs, diagnosis, and
treatment options available for each disease.
Hind Limb Lameness in the Mature Dog
James K. Roush
This article describes the differential diagnosis of hind limb lame-
ness in adult dogs with common clinical presentations and diag-
nostic methods outlined.
39
55
85
101
125
vi CONTENTS
Feline Lameness
Cynthia Anne Leonard and Michael Tillson
Feline lameness is an increasingly recognized clinical problem.
Today's veterinary practitioner with his/her
ability to diagnose the various for lam:-
ness in the cat and be able to dISCUSS the slgmflcance of therr
findings with the client. Disease of the
system can be grouped into broad categones,. mcludmg: trauma,
arthritis, infectious causes, developmental dIsorders, neoplasIa,
and muscular problems. Specific diseases from each these
categories will be discussed, particularly those that dIffer m therr
presentation or clinical behavior from that same dIsease m the
canine patient.
Diagnostic Imaging of Lameness in Small Animals
James J. Hoskinson and Russell L. Tucker
The demand for advanced diagnostic imaging procedures such
as nuclear scintigraphy, ultrasonography, computed
and magnetic resonance imaging has over
the past 10 .years. seeking to
tic capabIlIties and clIents wIllmg to pursue best medicme
driven this demand, resulting in installation of advanced Imagmg
facilities at most academic and private referral practices. Knowl-
edge of potential benefits of various will.
veterinarian to optimize his or her use of dIagnostic Imagmg m
his or her own practice or in a referral practice.
Ancillary Diagnostic Techniques for the Lame Patient
Mary Ann Radlinsky
The cause of lameness is usually identified through evaluation
of signalment, history, and physical examination. Radiographic
evaluation provides a definitive diagnosis in. many cases; h<;,w-
ever, laboratory evaluation may prove useful m the charactenza-
tion of certain conditions or in the prognostication of the condI-
tion. In some instances where the definitive diagnosis remains
elusive, arthroscopic examination is a minimally invasive diag-
nostic tool that may be more affordable and available than com-
puted tomography. This article reviews evaluation of
the lame patient and arthrOSCOpIC evaluation of Jomt abnormalI-
ties.
Kinetic and Kinematic Gait Analysis in Dogs
Ron M. McLaughlin
This article reviews computerized force plate analysis and kine-
matic gait analysis techniques currently in The neces-
sary equipment is describecl and the baslC pnncipies of data
CONTENTS
143
165
181
193
vii
collection are reviewed. These techniques are frequently used in
experimental studies evaluating gait and their use as clinical and
diagnostic tools is increasing.
Index
203
Subscription Information
Inside back cover
viii
CONTENTS
FORTHCOMING ISSUES
March 2001
CLINICAL THERJOGENOLOGY
Autumn Davidson, DVM, Guest Editor
May 2001
VACCINES AND VACCINATIONS
Richard B. Ford, DVM, MS, Guest Editor
July 2001
ENDOSCOPY
Lynda Melendez, DVM, MS, Guest Editor
RECENT ISSUES
November 2000
RESPIRATORY MEDICINE AND SURGERY
Philip Padrid, RN, DVM, Guest Editor
September 2000
INFECTIOUS DISEASE AND THE EYE
Jean Stiles, DVM, MS, Guest Editor
July 2000
MANAGEMENT OF PAIN
Karol A. Mathews, DVM, DVSc, Guest Editor
VISIT OUR WEB SITE
For more information about Clinics:
http://www.wbsaunders.com/periodicals/clinicsfindex.htm
PREFACE
WALTER C. RENBERG,
DVM,MS
JAMES K. ROUSH,
DVM,MS
Guest Editors
This issue of The Veterinary Clinics of North America: Small Animal Practice is
dedicated to lameness in the small animal patient. The diagnosis of orthopedic
problems is straightforward, but when the problem is not obvious, the
cases can be among the most challenging and frustrating clinical problems. The
clinician therefore needs to rely on a systematic examination, an awareness of
the differentials, and a solid grasp of the available diagnostic tests as well as
their indications. It is our hope that this issue will provide that information
thereby enabling the clinician to deal more effectively with cases of lameness.
The first article details a thorough physical evaluation of the musculoskele-
tal system, the foundation of managing a lame patient. Subsequent articles
explore specific aspects of lameness (e.g., pathophysiology, presentation in cats),
and review the differentials for lameness in the forelimbs and hindlimbs of
immature and adult animals. Finally, we review various diagnostic procedures
to familiarize veterinarians with their use and appropriateness.
We sincerely appreciate the efforts of this issue's contributing authors. Their
contribution in sharing their expertise and experience was invaluable. We also
express our appreciation to W.B. Saunders Company for inviting us to present
this information to our colleagues and friends in the veterinary profession.
Department of Clinical Sciences
. Kansas State University
College of Veterinary Medicine
1800 Denison Road
Manhattan, KS 66506-5606
WALTER C. RENBERG, DVM, MS
JAMES K. ROUSH, DVM, MS
Guest Editors
LAMENESS 0195 -5616/01 $15.00 + .00
EVALUATION OF THE
LAME PATIENT
Walter C. Renberg, DVM, MS
Competence in evaluating lameness is vital for the veterinary prac-
titioner. This skill is becoming even more important with the increasing
popularity of large-breed dogs and the corresponding increase in the
number of developmental orthopedic problems seen on a day-to-day
basis. A proper physical examination of the lame patient is essential to
the management of the case. This article reviews the initial evaluation of
the lame veterinary patient without dwelling on the specific differential
diagnoses and corresponding treatments. The' reader is referred to other
articles in this issue for more specific information on the various causes.
Lameness can be best defined as an alteration in the normal gait of
the animal. As such, it may arise from painful conditions such as trauma
or osteoarthritis, or it may stem from mechanical dysfunction as in
quadriceps contracture or patella luxation. The source of the problem
may be any of the tissues involved in normal weight bearing or locomo-
tion, including muscles or tendons, bones or ligaments, joints, central or
peripheral nerve tissue, or even other parts of the body as in the case of
the animal with abdominal pain, orthopnea (leading to altered stance),
or vestibular disease. It should be obvious that the clinician must formu-
late and revise a list of differential diagnoses at each stage of the
evaluation. Such lists are more fully detailed in subsequent articles in
this issue.
Orthopedic examination or lameness examination is a dangerous term,
because such an evaluation should not exist in isolation. Rather, the
evaluation of a given lameness should be conducted by evaluating the
entire animal and considering information about all body systems. The
From the Department of Clinical Sciences, Kansas State Unjversity College of Veterinary
Medicine, Manhattan, Kansas
VETERINARY CLINICS OF NORTH AMERICA: SMALL ANIMAL PRACTICE
VOLUME 31 NUMBER 1 JANUARY 2001 1
2 RENBERG
source of the lameness may be directly related to a condition at a
different site (e.g., a septic joint caused by hematogenous spread from
an abscess), or it may be that in light of systemic illness, the lameness is
only of secondary importance. The clinician must balance the desire and
ability to expediently identify the problem against the tendency to fall
into. tunnel vision. This approach is one that focuses exclusively on an
ObVIOUS or presumed problem, thereby running the risk of overlooking
other findings .
Aside from a commitment to be thorough, the veterinarian needs
an understandin? of normal anatomy and function to successfully con-
du<:t an. evaluatIon of the.lam.e patient. It is difficult or impOSSible
to IdentIfy the abnormal SituatIon without understanding the normal
situation. This applies not only to the anatomy but also to the manner
in which animals normally move, sit, rise, and stand as well as to the
normal range of motion for a given joint. Additionally, clinicians must
have an understanding of the differences in the various breeds they may
encounter. For example, there is a measurable difference in the normal
joint angle of the hock of a German Shepherd Dog as compared with an
Akita. A veterinarian not familiar with breed norms may jump to errone-
ous conclusions. Furthermore, a familiarity with breed-specific problems
helps to prioritize the differential list. For example, a Yorkshire Terrier
with hip pain is more likely to have Perthes' disease, whereas a Golden
Retriever with similar signs likely has hip dysplasia. As the clinician
begins to develop an individual approach to evaluating lameness, it is
important to maintain an organized and systematic method that can be
repeated with minimal variation. This allows an almost subconscious
routine and lessens the likelihood of overlooking a particular aspect of
the examination. Examining a lame animal becomes quicker and easier
with experience. Given an understanding of the process, however, there
is no reason that an inexperienced veterinarian should feel ill prepared
to evaluate most such cases.
Conceptually, the evaluation of the lame patient can be divided into
two components. The first component is localizing the problem. This
involves determining which limb or area of the body is involved and
then what portion of that limb or area is affected. In most cases, the
affected region is a specific joint or other portion of the leg, but as has
been mentioned, the problem may be caused by a lesion elsewhere (e.g.,
root signature from a herniated disk). The second component to the
evaluation is diagnosing the specific cause of the problem. The two
components may overlap or may involve entirely separate exercises. For
example, a lu;np may J:>e noted in the left rear limb, and then pain may
be detected ill the Stifle. At the same time in the examination the
examiner may discover that laxity exists in the joint in the of
cranial In instance, the localization of the problem
and the dIagnOSIS (l.e., cramal cruciate ligament rupture) occurs almost
simultaneously. Alternatively, after finding pain in the stifle, the exam-
iner may have later obtained radiographs of the stifle and noted a lesion
consistent with osteochondritis dissecans. Despite the temporal blurring
EVALUATION OF THE LAME PATIENT 3
of these two components, it is useful to. think of the various actions
taken during the examination in light of either localization or diagnosis.
This helps to focus the examiner's thoughts. It should be made clear to
the client that common diseases are ruled in or out with the more
common and less invasive diagnostic procedures. Negative results re-
quire that the client agrees to more time-consuming, expensive, or inva-
sive procedures as the clinician attempts to diagnose less common prob-
lems.
HISTORY AND SIGNALMENT
The first step in evaluating the lame patient is to obtain adequate
background information, including signalment and history. Again, as-
pects of localization (e.g., a history of left forelimb lameness) and diagno-
sis (noting breed predispositions or previous surgery) occur at the same
time. Most examiners also take the opportunity to observe the animal
while they are conversing with the owner.
Obtaining -sufficient background information facilitates the hands-
on portion of the examination. The first item of information to gather is
usually the client's chief complaint. This is the abnormality the client
has noticed that prompted the visit to the veterinarian. Although in
most cases that serves as the starting point for the investigation, clini-
cians should verify that the client is communicating correctly. Such
simple observations as which leg an animal limps on may be incorrect
if the client thinks of the leg while the animal is facing him or her versus
a consideration from the animal's viewpoint. Additionally, phrases such
as "he can't walk" may mean nonambulatory paraplegia to a veterinar-
ian when the client merely means that the animal is reluctant to move
around. Many lay terms such as stiff, limping, or slow seem to have no
consistent meaning at all. Be wary when clients arrive with a specific
diagnosis (e.g., "shoulder pain"), because they may be basing their
observation on incorrect assumptions. It is true, however, that some
clients are well informed and very observant, and their insight can prove
invaluable. In today's society, clients have access to a great deal of
information, which may be only partially correct; often, the clinician
. must spend extra time putting such information into context or ex-
plaining.
Signalment is the next item of information that helps to refine
the differential list. As previously stated, specific breeds have various
predispositions that can help to focus the investigation. The vast number
of breeds and associated problems is beyond the scope of this article,
but the clinician is advised to remain informed concerning these tenden-
cies. In addition to breed, age and sex are important items of informa-
tion. In particular, age may suggest a developmental problem or, alter-
nately, steer a clinician into a more careful search for arthritis or
neoplasia.
After learning the chief complaint and signalment, the investigator
4 RENBERG
needs to obtain a detailed history of the specific problem. Particular
items of information that are of interest include the following:
Duration of problem
Manner of onset
Diet
Association with trauma
Intermittent or constant
Associated events or activities
Progression
Presence in other legs
Previous treatments or medications
Efficacy of treatments
Systemic signs
Typical and projected use of the pet
Although not every item has a bearing on every case, most help to
refine the clinician's suspicions and the differential list. Of particular
importance is the manner in which the lameness began and how it has
progressed. Sudden-onset lameness is suggestive of trauma even if no
such event is known. A chronic course of lameness may have an impact
not only on the diagnosis by alerting the clinician to consider the
likelihood of arthritis or other diseases but also on the selection of
treatments and the prognosis. Similarly, if significant arthritis is found,
but the history consists of only a brief duration of signs, the examiner
should carefully search for other problems before deciding that the
arthritis is the cause.
GENERAL OBSERVATIONS
During and after the time the clinician is obtaining a history, he or
she should observe the animal. This is the best opportunity to note how
the animal rests and moves while relaxed. It should be noted that some
animals are not relaxed at all during the visit to the veterinarian and
thus may display different clinical signs than could be observed in the
er:vironment. Particular attention should be paid to how the
anlillal SItS or stands. For example, animals with stifle pain may be
reluctant to fully flex the joint and thus may sit with the affected limb
out to the side. Similarly, most animals stand with their sound legs
further w:der the body to bear more weight on them while placing a
sore leg :n a more abducted position to spare it. Other noteworthy
postures mclude those of animals that lower their heads and arch their
backs in an to weight to the forelimbs. Additionally,
With elbow dIsease abduct their elbows, and dogs with
mfraspmatous contracture have a characteristic manner of holdino- the
affected forelimb. Other aspects of the stance that should be at
this time include the presence of a palmigrade or plantigrade stance.
These abnormalities may only be detected when the animal is bearing
EVALUATION OF THE LAME PATIENT 5
weight or when it is walking or trotting. They should be investigated
more fully when the focused examination of the limbs is performed.
Next, it is helpful to observe the animal walking or trotting slowly.
Again, the main purpose is to localize the lesion to a particular lim.b ?r
to determine if the lameness is more likely orthopedic or neurologIC m
origin. Animals that are experiencing pain in a limb may attempt. to
transfer weight off the affected limb and may attempt to :VIth
the affected limb in contact with the ground for shortest pOSSIble time.
In the case of a forelimb lameness, animals typically raise their head
while the affected limb is in contact with the ground and lower their
head when the sound limb is in contact with the ground. This gait gives
them the classic "head-bob" appearance as they walk or trot and serves
to help in transfering weight off the painful limb. In the case of hu:d
limb lamenesses, the animals may incline their pelvis or adopt certam
head movements, but these mannerisms are sometimes difficult to de-
tect. It is often easier to note that they bring the sound limb down onto
the ground more forcefully than the sore limb. Additionally,. they may
"short-step" with the affected limb while keeping the sound 11mb on. the
ground for a longer time during each gait cycle. All these affectations
are easiest to see in a large dog. Even at a slow pace, toy breeds and
smaller dogs move their legs so rapidly that noting which limb is
exhibiting the lameness takes patience and practice.
Cats also present a challenge. These patients in particular seem to
attempt to mask any lameness during the visit to the veterinarian. Often,
they are reluctant to move around the examination room,
instead to rapidly hide under a chair or in corner. 0r:e that
may aid in evaluating a cat with lameness IS to place It m a portion of
the room farthest from the hiding place to give the examiner a chance
to watch it move as it seeks the shelter. Additionally, every attempt
should be made to minimize stress and distractions (e.g., large numbers
of people, barking dogs) . . .
Many clinicians find that taking dogs outSIde to evaluate theIr
movements is helpful. Regardless of the environment, good footing
should be provided, and distractions should be .An animal
that is constantly pulling on the leash may mask even sIgmficant lame-
ness. The patient should be viewed from the front, back, and side. Note
any scuffing of the nails or stumbling during turning that may suggest
neurologic involvement.
After observing the animal at rest and moving, the clinician should
be able to tell which limb(s) seems to be most affected. In some cases,
the observation may have pointed away from any specific limb and
more toward systemic or central neurologic problems. The next phase
of the evaluation is to gently palpate the animal while it is standing in
a relaxed manner. At this point in the examination, the clinician should
be focusing on asymmetry. Differences in muscling are most likely
caused by disuse or neurologic atrophy but also could be conSIstent
with muscle tears or previous surgery. By palpating gently up and down
the left and right limbs simultaneously, the clinician can note atrophy or
6 RENBERG
swelling (e.g., neoplasia, inflammation) and joint effusion most readily.
Comparing the contralateral limb helps to determine the significance of
a finding unless the lesion is bilateral. While the animal is standing
quietly, the clinician should also check for the presence of proprioceptive
deficits as a minimal test to eliminate neurologic disease.
FOCUSED INSPECTION
After performing the general observation of the animal, the clinician
must begin a more focused inspection that localizes the lesion more
specifically. In almost every case, this inspection is best performed in
dogs with the animal placed in a lateral recumbent position. A system-
atic evaluation of each aspect of each limb is begun. The clinician should
generally start with the unaffected limbs and conclude with the limb
most likely to be painful. This allows the animal to remain calm and
comfortable for the longest possible time. Additionally, starting at the
toes and gradually working proximally up the limb minimizes the
chance of confusing the source of pain. For example, a clinician who
extends the hips looking for hip pain is also extending the stifles in the
process. If one has not first eliminated the stifles as a source of discom-
fort, any pain elicited on hip extension could be just as reasonably
attributed to either joint.
In general, the paws of the forelimbs and hind limbs are examined
in a similar manner. Initially, the pads and interdigital spaces should be
inspected for evidence of wounds, swelling, or pain. Any evidence of
inflammation may indicate a previous wound or a foreign body. Each
digit should be examined for evidence of fractures or luxations. The
joints of the phalanges are best evaluated for instability while in exten-
sion, as they may be falsely perceived to be lax if examined in flexion.
Most injuries of the distal foot are easily noted because of the presence
of pain and palpable abnormalities. The remainder of the foot is exam-
ined next. Special attention should be directed to palpating the sesa-
moids located on the plantar and palmar aspects of the metatarso- and
metacarpophalangeal joints. Again, injuries in the region of the metatar-
sal or metacarpal bones are typically obvious on examination.
The hock is best palpated for pain, effusion, swelling, and instability.
Pain in the hock is most easily elicited by placing the joint in extension.
A normal animal should not resent 180
0
of extension. When palpating a
joint, the clinician should gently cycle the joint through a range of
motion to note any crepitus, and then place the joint at the limit of its
range of motion (Table 1). At that point, additional gentle pressure
should not meet with discomfort. Effusion in the stifle can most reliably
be felt on either side of the calcaneus just caudal to the malleolus. Any
"puffiness" or soft distention is likely caused by effusion within the
tibiotarsal joint, although soft tissue swelling associated with inflamma-
tion or neoplasia should be considered. With the joint in moderate
extension, the examiner should exert medial, lateral, cranial, and caudal
EVALUATION OF THE LAME PATIENT
Table 1. NORMAL RANGES OF MOTION FOR CANINE JOINTS
Joint
Shoulder (relative to the spine of the scapula)
Elbow (relative to the axis of the humerus)
Carpus (relative to the antebrachium)
Hip (relative to the axis of the pelvis)
Stifle (relative to the femur)
Tarsus (relative to the tibia with the stifle at 90)
Range of Motion'
Flexion to 20- 30
Extension to 155-165
Flexion to 15-20
0
Extension to 160-165
Flexion to 20-25
Extension to 200-210
Flexion to 10_20
Extension to 170-180
Flexion to 15-25
Extension to 155-165
Flexion to 15-25
Extension to 180-200
7
'The clinician is advi sed to depend on experience and comparison with the contralateral joint
rather than adhering rigidly to the data presented here. This information should serve as a useful guide.
Data from Newton C: Examination of the orthopaedic patient. In Newton C, Nunamaker 0 (eds):
Textbook of Small Animal Orthopaedics. Philadelphia, JB Lippincott, 1985, pp 1101-1106.
pressure on the foot in an attempt to demonstrate laxity. Animals that
have previously been noted to have a plantigrade stance should be
examined for the presence of tarsalluxations or calcanean tendon tears.
With the stifle held in extension, an attempt to flex the hock should be
made. A normal hock does not flex with the stifle extended, and any
abnormality suggests a disruption at some point of the muscle-tendon
unit. If the hock flexes, it is important to note if the toes also flex, which
may indicate that the digital flexors are intact. If the lesion in an animal
with a plantigrade stance does not seem to involve the calcanean tendon,
attempts should be made to manipulate the intertarsal and tarsometatar-
sal joints to investigate any luxation or subluxation there.
After palpating the region of the hock, the clinician should evaluate
the crus. The tibia can be palpated easily on the medial side, and deep
pressure should be exerted on the bone to detect pain as might be
expected with neoplasia or panosteitis. When palpating any bone for
evidence of pain, care must be taken to ensure that the pressure is placed
against the bone and not on overlying structures such as muscles or
nerves. The fibula can also be palpated, although isolated injuries to the
fibula are less common.
To test for the presence of pain in the stifle, the clinician should
place the joint into firm extension. Again, evidence of medial or lateral
instability should be noted . Effusion in the stifle is best detected with
the joint in moderate flexion. The thumb and forefinger should be placed
on either side of the straight patellar tendon. In a normal patient, the
tendon should be easily palpated, and the fingers should extend around
one half to two thirds of the circumference of the tendon. Effusion is felt
as a softness or puffiness on either side of the tendon, preventing crisp
borders from being felt. The examiner should also carefully check for
the presence of a firm swelling on the medial aspect of the stifle. This is
8 RENBERG
composed of fibrous tissue, is known as the medial buttress, and is typical
of chronic injuries to the cranial cruciate ligament.
To test for cranial drawer motion, proper hand position is vital (Fig.
1). The thumb of the more proximal hand should be placed firmly caudal
to the lateral fabella, and the forefinger of the same hand should be
positioned on the patella. The thumb of the more distal hand is placed
caudal to the fibular head, and the forefinger of the same hand is placed
on the tibial crest. It is important that the bony landmarks be felt,
because otherwise the examiner may merely slide the patient's skin and
falsely believe that drawer motion is present. With the fingers placed in
the appropriate position, the hand on the femur is held still while the
hand on the tibia is used in an attempt to slide the tibia forward without
rotating it. The plane of forwarq pressure should be parallel to the
perceived plateau of the tibia. The joint should be examined in flexion
and extension, as laxity may not be present in both instances. By posi-
tioning the fingers correctly, and directing the cranial pressure parallel
to the tibial plateau, even clinicians with small hands should be able to
appreciate cranial drawer motion. It should be noted that if no drawer
motion is detected but a high index of suspicion still exists for a torn
Figure 1. Proper hand positi on to obtain cranial drawer motion in diagnosing cranial
cruciate ligament rupture. The test should be performed in flexion (A) and extension
(8). The arrow indicates the direction in which the lower hand should move to obtain
cranial drawer.
EVALUATION OF THE LAME PATIENT 9
cruciate ligament, the animal should be sedated and re-examined. This
is vitally important, as some animals are able to guard their stifle to the
extent that they can mask any drawer motion present.
The stifle should also be examined for the presence of cranial tibial
thrust, which can also result from deficiencies of the cranial cruciate
ligament. To evaluate a patient for cranial tibial thrust, the stifle is placed
and held in extension . With a finger resting lightly on the tibial crest,
the hock is flexed (Fig. 2). Any cranial movement of the tibial crest is
cranial tibial thrust. Additionally, the examiner should be alert for the
presence of caudal drawer motion, which is detected in the same manner
that one tests for cranial drawer motion but with pressure directed
caudally. Cranial and caudal drawer motion can sometimes be confused,
but the stifle should generally come to an abrupt stop in the direction
in which the ligament is intact and should reach a less distinct end point
in the direction in which the ligament is torn.
After evaluating for drawer motion, the clinician should attempt to
luxate the patella. This should be attempted by exerting pressure against
the side of the patella and attempting to dislodge it from its groove in
the femoral condyle. This maneuver must be attempted in flexion and
in extension as well as in medial and lateral directions. At times, it may
be easier to evaluate the patient for luxating patellas while the animal is
standing.
After evaluating the stifle, the upper limb is evaluated for pain or
swelling. Although the femur is less superficial than the tibia, deep bone
pain can still be assessed by palpating on the lateral aspects distally and
proximally.
Pain is most consistently noted in the coxofemoral joints when the
Figure 2. Proper hand and patient position to evaluate tibial thrust in diagnosing cranial
cruciate ligament rupture.
10 RENBERG
hips are extended. As previously noted, this motion also causes exten-
sion of the stifles, thus, discomfort in those joints must be eliminated
before examining the hips. Animals with lower spine pain may also
resent extension of their hips; thus, this possibility must be carefully
investigated. A normal animal does not resent having its hips extended
to almost 180.
Evidence of coxofemoral subluxation can be noted through a variety
of tests, but the most reliable is the Ortolani sign. To perform this test,
the stifle should be grasped with one hand while the opposite hand
steadies the spine dorsally (Fig. 3). Firm pressure is exerted dorsally
from the stifle in a direction parallel to the femur while the hip is
maintained at 90 of flexion. The dorsal pressure is maintained as the
leg is carefully abducted. The angle of the hip should not change. The
dorsal pressure on the femur causes the femoral head to subluxate onto
the dorsal acetabular rim in a lax joint. As the leg is abducted, the head
of the femur snaps back into the acetabulum with a palpable and often
visible motion. This motion is a positive Ortolani sign and indicates joint
laxity. Some dogs resent this test, and a positive result can only be
detected after sedating the animal. The Ortolani sign is not a test of hip
dysplasia per se but of subluxation, and even then it is only positive if
the dorsal acetabular rim has not undergone excessive remodeling.
There are a variety of methods to determine if the hip has luxated.
Most luxations are craniodorsal in nature and can be readily detected,
although final confirmation requires radiographs. The "thumb test" in-
volves placing the thumb in the patient's ischiatic notch just caudal to
the greater trochanter (Fig. 4). The limb is then externally rotated, which
results in the examiner's thumb being squeezed or displaced by the
greater trochanter if the joint is in place. In a dog with a craniodorsal
luxation, the external rotation causes the femoral head to rotate cranially,
Figure 3. Proper hand pOSition to obtain Ortolani sign in evaluation of hip laxity.
,
.,
EVALUATION OF THE LAME PATIENT 11
Figure 4. Proper hand pOSition to test for hi p luxation using the thumb test. Note that the
limb is palpated in neutral orientation (A) and then externally rotated (8, arrow). The
examiner's thurnb in 8 has been pinched by the greater trochanter, indicating a normal jOint.
and the greater trochanter does not move. The examiner's thumb is thus
not squeezed or displaced. Alternately, the examiner can note the rela-
tion between the ischiatic tuberosity, the greater trochanter, and the crest
of the ilium. These three landmarks should form an obvious triangle,
with the greater trochanter forming a downward (Fig. 5) . In the
case of a craniodorsalluxation, the three landmarks form more of a line.
Ventral luxations are less obviously palpated, but the relation between
the same three landmarks is different than that seen on the contralateral
side, and the greater trochanter is more medially located.
Although direct palpation of the bones of the pelvis is difficult, it is
possible to obtain some information that may increase the suspicion of
pelvic lesions (e.g., fractures). In all but the most overweight dogs, the
crests of each ilium can be grasped, and pressure can be exerted caudally
12 RENBERG
Figure 5. Landmark identification to test for hip luxation using the triangle test. C = iliac
crest; G = greater trochanter; T = ischiatic tuberosity.
and ventrally. Any crepitus or motion suggests a sacroiliac luxation or a
fracture in the region. Medial pressure can be exerted on the ischiatic
tuberosities to make similar determinations. Finally, a rectal examination
should be performed to aid in palpating any fractures as well as in
determining the degree of pelvic compromise and palpating the prostate
in male dogs. This examination should be done gently and cautiously,
because it may be painful in a patient that has experienced trauma and
because sharp bony fragments may be present in the pelvic canal.
Examination of the forelimbs is accomplished in a manner similar
to that used for the hind limbs. Again, it is important to begin palpation
at the paw and progress proximally up the limb. The investigation of
the digits and metacarpal region is identical to that of the rear paw.
When the carpus is examined, the investigator should palpate the cranial
aspect of the joint with the joint in mild flexion. The carpal joints should
be palpable on the cranial surface with no puffiness, except in obese
animals. Any softness over the cranial surface is likely caused by joint
effusion. The carpus can best be evaluated for pain by placing it in
flexion. A normal joint can be flexed to the extent that the digital pads
touch the antebrachium without pain. One caveat is that many dogs
develop some decreased range of motion in the carpus as they age
without showing any apparent clinical problems. The clinician should
carefully search for other causes before attributing an older animal's
lameness to a decrease in carpal range of motion. Although luxations
are rare, the carpus should be evaluated for medial and lateral laxity.
EVALUATION OF THE LAME PATIENT 13
Normal animals should have minimal extension of the carpus past 180.
H the animal was noted to have a palmigrade stance, attempts should
be made to verify the abnormality by forcibly extending the joint.
The antebrachium should be palpated for swelling, asymmetry, or
edema. Deep bone pain can easily be assessed in the ulna and radius
for much of the length of either bone. When the elbow is palpated, it
should be assessed for medial and lateral laxity as well as for range of
motion and effusion. Effusion in the elbow is best palpated medial and
lateral to the olecranon. The relation between the landmarks of the
elbow in a normal dog should be noted, because luxations are often
diagnosed by palpating an excessively prominent medial epicondyle
and not being able to palpate a distinct lateral epicondyle (assuming a
lateral luxation). The normal elbow should be able to be flexed to the
point that the muscles of the antebrachium meet the muscles of the
upper limb and should be able to be extended to almost 180. Pain is
best noted by applying firm pressure in extension. Some investigators
apply pressure over the region of the medial coronoid process of the
ulna in an attempt to localize discomfort to that structure.
Evaluation' of the upper limbs is accomplished by searching for
asymmetry, swelling, or pain on palpation. Deep bone pain of the
humerus can only be evaluated at the proximal and distal ends of the
bone because of overlying structures in the diaphyseal area. At the
shoulder, the clinician should carefully place the joint through a range
of motion. Normal dogs should tolerate having the joint flexed and
extended to parallel to the spine. Pain can be elicited in either flexion or
extension. Often, mild internal rotation with flexion elicits a painful
response in dogs with pathology of the shoulder. It should be noted that
it is difficult to separate pain in the elbow from pain in the shoulder, as
pressure is often exerted on one joint when examining the other. The
clinician should be especially diligent in trying to differentiate pain in
one joint from the other joint, but isolating the source of discomfort may
not be possible on physical examination alone. When an investigator is
suspicious of bicipital tenosynovitis, the shoulder should be flexed while
the elbow is extended so as to stretch the entire myotendinous unit,
which runs from the scapula to the radius and ulna. Often, application
of digital pressure over the biceps tendon of origin while the biceps is
stretched may be necessary to elicit this discomfort. Finally, it is im-
portant to note the relation between the acromion and greater tubercle
so as to evaluate the joint for luxation. Luxations of the shoulder should
be medial or lateral and may reduce and reluxate easily. For this reason,
the clinician should palpate the joint lightly while placing it through a
range of motion.
Finally, the scapula should be examined. Firm palpation of the spine
and dorsal edge of the scapula is possible and may help to diagnose
pain in the region. Any muscle atrophy of the infraspinatus or supraspi-
natus muscle should be palpable. Firm palpation of the axillary region
assists in diagnosing tumors of the nerve roots.
14 RENBERG
ADDITIONAL EVALUATIONS
As a last component of the examination of the lame animal, the
clinician should search for evidence of spinal pain. This should be
performed in every animal even if no evidence of neurologic injury is
noted, because root signature may be the only presenting clinical sign
of a neurologic lesion. Firm dorsal pressure can be exerted over the
spine without causing discomfort in the normal dog. Because spinal
hyperpathia can be severe in affected dogs, the author has found it
helpful to begin with gentle palpation and work up to firm pressure,
stopping when discomfort is noted. Additionally, the range of motion of
the neck in all directions should be assessed. Most dogs can touch their
nose to their ribs, although this may not be possible in dogs with short
necks. Caution should be exercised if any suspicion of spinal fracture or
other instabilities (e.g., atlantoaxial instability, cervical vertebral instabil-
ity) is present.
PITFALLS AND COMPLICATIONS
Most examinations of lame animals are straightforward and enable
the clinician either to diagnose the problem or to suggest further tests
to provide a definitive diagnosis. Occasionally, various difficulties that
complicate the diagnosis arise. Often, these situations necessitate serial
examinations. Every veterinarian should keep in mind that there are
some patients whose problem cannot be diagnosed regardless of the
skills of the clinician or the technical capabilities of the hospital. By
being thorough and systematic, the number of these open diagnoses is
reduced.
One reason to be systematic in one's approach to the lame patient
is to avoid missing a second problem. Patients with more than one
orthopedic condition are actually relatively common, a fact that should
not be surprising, because the signalment is similar for many problems.
In most cases, fortunately, one of the lesions is causing the bulk of the
clinical signs and can be treated to provide relief to the animal. Factors
that may help the clinician sort out which of many problems seems to
be the most important include such considerations as the degree to
which a lesion is chronic or acute. One must be cautious in attributing
an acute unilateral lameness to chronic hip dysplasia instead of a possi-
ble cruciate ligament injury. At times, the degree of pain may help the
clinician to decide which lesion is the most significant. This is a subjec-
tive assessment and should only be based on serial examinations.
Another problem that may arise is the need to examine a patient
that is already sedated. This may occur if a lesion is incidentally noted
on radiographic examination for another problem or if an animal has
been sedated for the car ride to the clinic. Depending on the degree of
sedation, animals may still respond to discomfort; thus, the examination
should still be conducted. Some examinations (e.g., assessment of cranial
EVALUATION OF THE LAME PATIENT 15
drawer or Ortolani sign) are easier under. sedation; thus, the clinician
should take advantage of the situation. In most cases where there is
uncertainty as to the significance of the lesion, the examination can be
repeated once the sedation has worn off.
The opposite end of the spectrum occurs when an animal is stressed
or to such an extent that a thorough examination is not
possIble: In these cases, a decision must be made whether to proceed or
not. :\t an of discomfort may still be possible, although
specIfIc manIpulatIOns (e.g., cranial drawer motion) are not. In other
cases, no examination is possible or prudent, and the patient must be
As n?ted pre:riously, although some assessment of pain is often
possIble deSpIte sedatIOn, subtle lesions may be missed. In cases where
the examination must be conducted on a sedated animal, the owners
be informed of the suboptimal conditions and the possible sig-
mflcance as well as potential complications or risks.
.. There. are. times. when the veterinarian may be the source of the
dIfficulty In dIagnOSIng the problem. Most clinicians presented with a
?-year-?ld Rottweiler with acute hind limb lameness are tempted to
ImmedIately test for cranial drawer motion. Because the problem could
be any n.umber ?f the a.s!ute clinician still conducts a thorough
systematic eXamInatIOn. The abIlIty to narrow the differential list based
.history signalment is a valuable skill. Such "appropriate" tunnel
VISIon may Increase efficiency but should not cause rare lesions to be
overlooked.
the common and most frustrating lame patients are
those. wIth IntermIttent lameness. This situation is frequently found in
wc;>rking hunting dogs, which only display their lameness when
achv.ely When the dog is examined in the veterinary
no dIscomfort IS found. Such patients usually have a mild or early
.the problem mayor may not show up on radiographs even
If the to look. One solution is to exercise the dog
the clIme. ThIS bnng on the lameness and also gives the veterinar-
Ian the opportunIty to ?bserve the animal in motion. Unfortunately,
there may not be the hme or space available to properly stress the
ammal to the extent that the problem becomes visible. In those instances
it is best to have the owner return the animal for examination as
the develop during work or to proceed to a more sensitive
such .as nuclear scintigraphy. Alternatively, the owner
can unhl. the leSIOn and thus becomes easier to diagnose.
ObVIOusly, thIS latter solutIOn, although economical, is not ideal. As
in other articles in this issue, there are a battery of ancillary
dIagnostic procedures that may be useful in difficult cases.
Finally, the clinician should always remember that common diseases
is to say that before diagnosing an uncommon
condItion (a zebra), the more common diseases ("horses") should be
ruled out. Such an approach usually saves time and expense in per-
forming the diagnostic workup.
16 RENBERG
References
1. Arnoczky S, Tarvin G: Physical examination of the musculoskeletal system. Vet Clin
North Am Small Anim Pract 11:575-593, 1981 .
2. Barr A, Houlton J: Clinical investigation of the lame dog. J Small Anim Pract 29:695-
703, 1988 f S 11 An' 1
3. Lewis D, Parker R, Bloomberg M: Self-Assessment Color Review 0 ma una
Orthopedics. Ames, Iowa State University Press, 1998 . .
4. Muir P: Physical examination of lame dogs. Compend Contin Educ Pract Vet 19.1149-
1160, 1997 .
5. Newton C: Examination of the orthopaedic patient. Section One: Evaluation of the
nonemergency patient. In Newton C, Nunamaker D (eds): Textbook of Small Ammal
Orthopaedics. Philadelphia, JB Lippincott, 1985, pp 1577-1586 '. .
6. Schrader S, Prieur W, Bruse S: DIagnOSIS: Histoncal, and ancillary examma-
tions In Olmstead M (ed): Small Animal Orthopedics. St Loms, Mosby, 1995
7. Sumner-Smith G: Gait analysis and orthopedic examination In Slatter D (ed): Textbook
of Small Animal Surgery. Philadelphia, WB Saunders, 1993
Address reprint requests to
Walter C. Renberg, DVM, MS
Deparhnent of Clinical Sciences
Kansas State University
College of Veterinary Medicine
1800 Denison Road
Manhattan, KS 66506-5606
e-mail: renberg@vet.ksu.edu
LAMENESS 0195-5616/01 $15.00 + .00
NEUROLOGIC CONDITIONS
CAUSING LAMENESS IN
COMPANION ANIMALS
John J. McDormell, DVM, MS, Simon R. Platt, BVM&S,
and Leigh A. Clayton, DVM
The most common cause of non-weight-bearing lameness is ortho-
pediC disease, but neurologic causes should always be a diagnostic
consideration. Distll1.guishing between orthopedic and neurologic causes
of lameness can be difficult but is critical in formulating a diagnostic
and therapeutic plan. The diagnostic plan for neurologic disease often
varies significantly from the workup for an orthopedic disease. The two
most common categories of neurologic diseases that are confused with
orthopedic disease are myopathies and spinal nerve pathologies.
The diagnostic evaluation of an animal with the complaint of non-
weight-bearing lameness should ll1.clude a complete and chronologie
history to identify onset, progression, and other related symptoms. A
physical examination emphasizing the orthopedic and neurologic com-
ponents is also required to differentiate between these two causes of
disease. The neurologic examination is a system by which the clinician
can evaluate the functional integrity of the nervous system. The compo-
nents of the neurologic examination can be divided into observation,
palpation, postural reactions, spinal reflexes, cranial nerves, and sensa-
From the Deparhnent of Clinical Sciences, School of Veterinary Medicine,. Tufts University,
North Grafton, Massachusetts GJM); The Animal Health Trust, Centre for Small
Animal Studies, Lanwades Park, Kentford, Newmarket, Suffolk, England (SRP); and
the Deparhnent of Animal Health, Smithsonian National Zoological Park, Washington,
DC (LAC)
VETERINARY CLINICS OF NORTH AMEF1CA: SMALL ANIMAL PRACTfCE
VOLUME 31 - NUMBER 1 JANUARY 2001 17
18 McDONNELL et al
tion as shown in the box on this page. An understanding of the perform-
ance and interpretation of the neurologic examination helps the clinician
to differentiate between neurologic and orthopedic causes of lameness.
Abnormalities that are or can be neurologic in origin include the
following:
Seizures, convulsions, or fits
Altered states of consciousness (stupor, coma, rage, somnolence)
Paresis or paralysis with proprioceptive deficits .
Vestibular ataxia: head tilt, nystagmus, asymmetric ataxia, roll-
ing, falling
Cerebellar ataxia: wide-based stance, intention tremors, dysmetria
Hyperesthesia, anesthesia (localized or generalized)
Blindness
Hearing deficit
Incontinence
Vomiting or regurgitation
Observation
Mental status
Posture
Movement
Neurologic Examination
Triceps
Biceps
Gait, locomotion
Palpation
Muscle atrophy
Hypertrophy
Pain
Postural reactions
Proprioceptive positioning
Wheelbarrowing
Wheelbarrowing with neck
extended
Hopping
Extensor postural thrust
Hemistanding and hemiwalking
Placing (tactile)
Placing (visual)
Spinal reflexes
Quadriceps reflex
Cranial tibial reflex
Extensor carpi radialis
Flexor (thoracic limb)
Flexor (pelvic limb reflex)
Perineal reflex
Cranial nerves
Olfactory
Optic
Oculomotor
Trochlear
Trigeminal
Abducent
Facial
Vestibulocochlear
Glossopharyngeal
Vagus
Accessory
Hypoglossal
Sensation
Dermatomal mapping
Superficial pain
Deep pain
If these irregularities are noted to have commenced simultaneous to
the presenting complaint, the clinician should be aware that other proc-
NEUROLOGIC CONDITIONS CAUSING LAMENESS IN COMPANION ANIMALS 19
esses besides those purely orthopedic in nature may be the cause of the
animal's presentation. Mental status abnormalities such as personality
changes, seizures, rage, and decreasing levels of consciousness can be
caused by primary brain abnormalities. It should be remembered that
individuals and breeds have their own level of attentiveness and that
environmental factors can influence an animal's temperament. Gait ab-
normalities should be carefully investigated in a large open area that
provides good traction. The clinician should have a thorough knowledge
of the normal gait differences between different breeds of dogs and
cats. A wide-based stance, ataxia with no loss of strength, dysmetria
(particularly hypermetria), and intention tremors are hallmarks of cere-
bellar disease. Nystagmus, strabismus, asymmetric ataxia, falling, roll-
ing, and head tilt are signs that the vestibular system is involved. Cranial
nerve dysfunctions are indications that there may be neurologic rather
than orthopedic disease present in the patient.
Postural reactions should be tested in all animals presented for
non - weight-bearing lameness. Animals with only orthopedic disease
should not have deficits in proprioceptive placing, hopping, hemistand-
ing, or placing Feactions. Support may be necessary if significant pain is
a component of the presenting complaint. As an example, a dog with a
femoral fracture may attempt to replace its paw to the normal position
after the paw is knuckled over if the animal is given enough support.
Postural reactions that rely on muscle strength such as wheelbarrowing,
extensor postural thrust reaction, and hemiwalking can be performed,
but results should not be overinterpreted if significant pain caused by
orthopedic disease is present.
Lower motor neuron (LMN) disease is often confused with orthope-
dic diseases such as arthritis or other joint abnormalities. If the clinician
performs a thorough neurologic examination, these perplexing signs can
be easily recognized as neurologic. LMN signs include placcid paresis
and paralysis, hypotonia and atonia, hyporeflexia and areflexia, and
pronounced rapid muscle atrophy. These signs develop almost immedi-
ately after disturbance of the spinal nerves affected. Muscle atrophy is
detectable within 1 week of serious nerve injury and is severe. Weakness
or paresis can be recognized by gait evaluation, and subtle disturbances
can be documented by testing postural reactions. Hypotonia and atonia
are recognized by palpation of the muscles innervated by the spinal
nerves affected. Reflexes are evaluated by myotatic reflexes such as the
quadriceps reflex (knee jerk) and cranial tibial reflex in the pelvic limb
and the extensor carpi radialis reflex in. the thoracic limb. Flexor reflexes
of the pelvic and thoracic limbs are easy to perform and can demonstrate
weakness earlier than other signs of LMN disease.
The sensory component of the neurologic examination is typically
carried out last in the examination to avoid losing the patient's coopera-
tion. Pain or hyperesthesia may have been detected during palpation, or
during the cranial nerve or spinal reflexes portion of the examination.
During the sensory examination, areas of increased sensitivity (hyperes-
20 McDONNELL et al
thesia), decreased sensation (hypesthesia), or absent sensation (anesthe-
sia) are investigated and mapped out.
A careful sensory evaluation for paraspinal hyperpathia can discern
areas of hyperesthesia. Beginning with L7 and progressing cranially, the
transverse processes are squeezed, or alternatively, the spinous processes
are pressed firmly. The stimulus increases from light touch to deep
palpation. A behavioral reaction to what should be an innocuous stimu-
lus can be interpreted as pain. Proper palpation should cause no reaction
in normal areas. Placing one hand on the abdomen as the vertebral
column is palpated allows detection of abdominal muscle splinting when
pain is experienced. Flexing and extending the neck as well as palpation
is used to examine the cervical area. Cervical palpation is performed by
firmly pressing on the transverse processes from C1 through C7. During
palpation, areas of hyperesthesia are noted and compared with the
presenting nerve-root signs. Significant correlation found between the
sensory examination and the nerve-root distribution of the limb-carrying
lameness would indicate neurologic rather than orthopedic disease. Ad-
ministration of anti-inflammatory or analgesic medications and overex-
citement of the animal during the examination may influence the results
of the sensory examination.
Hypesthesia and anesthesia are hallmarks of neurologic disease.
Testing should be done with the animal in a relaxed setting. A fold of
skin is grasped gently, and a small hemostat pinches the skin fold; the
stimulus intensity increases only until a behavioral response (vocalizing,
escape behavior, or turning of the head) is noted. This procedure is
repeated in a systematic way bilaterally from either a distal to proximal
or caudal to cranial direction. There are individual and breed variations
in the animals tested. Remember that withdrawal of the limb is a reflex
and does not indicate intact sensory function.
Conditions that rule out lameness caused by neurologic diseases
should include muscle diseases (myopathies), neuropathies, interverte-
bral disk disease (IVDD), lumbosacral (LS) disease, nerve root tumors,
spinal cord tumors, and traumatic neuropathies such as brachial plexus
avulsion. Common clinical presentations as well as useful ancillary
diagnostics are discussed for these conditions. For a complete discussion,
including treatment of these diseases, a review of the literature is encour-
aged? 11.14.24. 25. 31. 37. 38. 43. 50. 60. 63
MYOPATHIES
Acquired, familial, and congenital disorders of skeletal and smooth
muscle are called myopathies. In most cases, they are characterized by
pain, generalized weakness, exercise intolerance, fatigue, and a stiff and
stilted gait.
37
6o
The gait disturbance can present as shifting leg lameness.
Muscle pain can be elicited with palpation of individual muscles or
groups of muscles. Clinical signs that can help to distinguish between
myopathies and orthopedic disease include a gait disturbance that is
NEUROLOGIC CONDITIONS CAUSING LAMENESS IN COMPANION ANIMALS
21
often worsened by exercise, bilaterally symmetric distribution of affected
muscles, localized or generalized muscle atrophy, and limited joint
movement.
37
60
Common myopathies include muscular dystrophy, poly-
myositis, endocrine myopathies, infectious myopathies, and myasthenia
gravis.
Ancillary tests helpful in diagnosing myopathies should be selected
based on the results of the complete physical examination. Serum levels
of muscle enzyme concentrations such as creatine kinase, lactate dehy-
drogenase, and aspartate aminotransferase may be elevated in muscular
dystrophy and myositis.
56
6o
Urinalysis may show the presence of myo-
globin with inflammatory myopathies, which is often incorrectly re-
ported as blood on urine dipsticks. There is a high likelihood that blood
reported on urinalysis is actually myoglobin if no red blood cells are
reported on the microscopic evaluation. Serum chemistry analysis may
show elevations in alkaline phosphate, triglyceride, and cholesterol lev-
els in cases of endocrine myopathies.
34
Infectious myopathies may show
elevation in total serum protein in association with increased f3- and "{-
globulin fractions.
56
60 Definitive diagnosis of myasthenia gravis is made
by detection of serum acetylcholine receptor antibodies or immune com-
plexes at the neuromuscular junction. 51 In patients with signs of vom-
iting, regurgitation, dysphagia, or excessive salivation, thoracic radio-
graphs are indicated to investigate megaesophagus.
51
Electrodiagnostic tests do not diagnose specific myopathies but can
confirm myopathies suspected from the neurologic examination. Electro-
myography (EMG), nerve conduction, f-wave analysis, and repetitive
nerve stimulation are electrodiagnostic tests that aid in localizing the
abnormality to muscle or nerve. Specific distribution of nerve or muscle
abnormalities can be mapped out with these testsY 53 This aids in
guiding additional tests such as nerve and muscle biopsies. Animals are
typically anesthetized for electrodiagnostic testing to eliminate volitional
activity and movement artifacts. Widespread use of electro diagnosis is
limited by equipment costs and availability of trained personneL
EMG is useful for evaluating spontaneous electric activity within
muscles caused by myopathies and neuropathies. These diseases .have
similar clinical signs and include diseases of the ventral horn nerve
cell, nerve root, peripheral nerve, neuromuscular junction, and muscle.
Electrically evoked potentials such as motor nerve conduction, sensory
nerv.e f-wave analysis, and repetitive nerve stimulation help
to dIfferentiate between neuropathies and myopathies. A complete re-
view regarding the performance and interpretation of these tests can be
found in the literature.
42
53
Electrodiagnostic signs of myopathies are
abnormal electromyograms with normal nerve function as revealed by
nerve conduction studies and f-wave analYSis. Animals with myasthenia
gravis and some myopathies often have decreased amplitude and pro-
longed latency after repetitive nerve stimulation. 53 This decremental
response can be corrected with the administration of the short-acting
anticholinesterase edrophonium chloride (Tensilon) at a dose of 0.1 to
0.2 mg/kg. Electrodiagnostic testing for myasthenia gravis does not
22 McDONNELL et al
replace the definitive laboratory testing of this disease, because other
diseases such as polymyositis can show a similar response.
51
Nerve and Muscle Biopsies
Nerve and muscle biopsies are required to confirm clinical and
electro diagnostic evidence of neuromuscular disease and may discern
causative diagnosis. Methods and criteria for obtaining these biopsies
are available for various nerves and muscles.
2
, 5 Although affected nerve
and muscle should be selected based on the results of the clinical
and electro diagnostic examinations, end-stage tissue should be avoided.
Instead, tissue that is only moderately affected may provide a more
accurate diagnosis. There are specialized laboratories that provide mor-
phologic, morphometric, histochemical, ultrastructural, and biochemical
evaluation of muscle and nerve samples.*t It is strongly recommended
that the clinician consult with these laboratories so as to select and
correctly process the samples,
The two most common nerves that are biopsied are the common
peroneal nerve as it passes over the lateral head of the gastrocnemius
muscle near the stifle joint and the ulnar nerve as it courses parallel to
the medial head of the triceps and superficial digital flexor muscles near
the elbow.
5
General anesthesia is required to perform a fasicular nerve
biopsy. No more than 30% of the total diameter of the parent nerve
should be sampled so as to preserve the anatomic and electrophysiologic
integrity of the nerve. Preparation of the surgical site should be the same
as that for any sterile procedure. After the skin incision, the nerve is
isolated from the fat and connective tissue. A 5-0 or 6-0 monofilament
suture with a swedged-on taper point needle is used to isolate 30% of
the diameter of the nerve. The intended biopsy sample is then sharply
excised with ophthalmic surgical scissors. Using gentle traction on the
suture, the ophthalmic scissors or scalpel is used to divide one third of
the nerve fascicles from the parent nerve. A total length of 2 to 4 cm
is required to provide samples necessary for histologic, morphologic,
ultrastructural, and teased fiber studies. Fascial and subcutaneous tissues
are closed routinely with absorbable suture. The skin closure is per-
formed using nonabsorbable suture. The nerve sample is gently
stretched using pins or suture material on a piece of wooden tongue
depressor and placed in fixative. A solution of 2.5% glutaraldehyde
fixative is preferable to 10% formalin for some of the nerve studies
performed,
s
'Comparative Neuromuscular Laboratory, Basic Science Building, Room 1107, Univer-
sity of California, San Diego, La Jolla, CA 92093-D612; telephone: (858) 534-1537; http: / /
medicine. ucsd.edu/ vet neuromuscular /
tDr Kyle C. B r a ~ d , c/o Peripheral 'Nerve Laboratory, 1476 Lakeview Ridge, Dade-
ville, AL 36853; telephone: (256) 825-2624; fax: (603) 676-2383; http:/ / www.lakemartin,
net / - khbraund/ ner vepath.html
NEUROLOGIC CONDITIONS CAUSING LAMENESS IN COMPANION ANIMALS 23
Muscle biopsy is best performed under general anesthesia. Prepara-
tion of the surgical site should be the same as that for any sterile
procedure. After making the skin incision, fat and connective tissue
should be dissected and retracted so that the direction of the muscle
fibers can be visualized. Stay sutures of 2-0 or 3-0 monofilament are
placed at each end of the muscle to be biopsied 1 to 2 cm apart and at
right angles to the muscle fibers. The sutures should loosely encompass
a cylinder of muscle approximately 0.5 cm in diameter without com-
pressing the muscle. A scalpel or iris scissors are used to make parallel
incisions along the length of the biopsy specimen, While gentle traction
is placed on the stay sutures, the blade or scissors are used to undermine
the specimen between the incisions. After the length of the biopsy
specimen has been completely undermined, the ends of the specimen
are cut with a scalpel or scissors. After specimen removal, hemorrhage
is controlled with direct pressure; in the case of arterial bleeding, ligation
may be required to achieve hemostasis. After biopsy removal, the speci-
men is placed in a gauze sponge moistened with physiologic saline
solution and kept at refrigeration temperatures unless a particular labo-
ratory has different requirements.
2
, 60
DISEASES OF NERVE ROOTS AND PERIPHERAL
NERVES
Any disease process that causes impingement, entrapment, com-
pression, or destruction of the nerve root or peripheral nerve may cause
lameness and pain suggestive of musculoskeletal disease (Fig. 1), This
non-weight-bearing lameness is also referred to as nerve-root signature, a
term that describes disturbances of sensation in the distribution of a
nerve's sensory distribution.
33
Pathology at the peripheral nerve or nerve
root may occur at any level of the spinal column, but non-weight-
bearing lameness is present only when it occurs at the cervical or
lumbar intumescences, Knowing the common clinical presentations and
following a logical plan in evaluating non-weight-bearing lameness can
help the clinician to differentiate between these two causes of lameness.
Diseases of nerve roots and peripheral nerves that cause non-
weight-bearing lameness include IVDD, neoplasia of the nerve roots,
'spinal cord tumors, and traumatic neuropathies. LMN disease can cause
signs of a focal neuropathic syndrome of the muscles innervated, LMN
disease is characterized by flaccid paresis or paralysis, reduced or absent
reflexes, reduced or absent muscle tone, and neurogenic atrophy. The
presence of these signs should alert the clinician to the possibility that
there is neurologic disease involving the LMN unit.
Intervertebral Disk Disease
IVDD is one of the most common canine neurologic diseases pre-
sented to companion animal veterinarians.
n
, 12, 15, 24, 25, 48, 49 This disease
24 McDONNELL et al
Figure 1. A transverse view representing compression of the ventral branch of the spinal
nerve (arrows). Pathology may occur at any level of the spinal nerve and may cause
lameness and pain suggestive of musculoskeletal disease.
can occur anywhere in the vertebral column caudal to Cl to C2. Cervical
IVDD can be seen between C2 and C3 and C7 and T1 intervertebral disk
(IVD) spaces. Thoracolumbar IVDD is seen typically between IVD spaces
T9 and 10 and L5. Lumbosacral disease affects the vertebral canal from
L5 to S3 and is discussed in a separate section. When an IVD impinges
directly on the spinal cord within the vertebral column, the resulting
deficits range from mild back pain to paralysis. Nerve-root pain may be
the primary sign when disk material impinges on the nerve root either
within the vertebral column, at the intervertebral foramen, or along the
course of the spinal nerve after it exits from the vertebral column.
3
These
lateralized disks can cause non-weight-bearing lameness if the affected
nerve root is within the cervical or lumbar intumescences.
Diagnosing a lateralized IVD requires signalment evaluation, a com-
plete physical examination, and appropriate an.cillary diagnostic tests.
In general, the chondrodystrophic or chondrodystrophic-like breeds such
as the Dachshund, Cocker Spaniel, Basset Hound, Beagle, Pekingese,
and Poodle are prone to develop the kind of disk degeneration that can
result in the acute severe onset of clinical neurologic signsy,24 Cats are
rarely affected by IVDD, and there have been no reports of lateralized
disks causing nerve-root signs. Physical examination, including evalua-
tion of the musculoskeletal and neurologic systems, often reveals focal
pain in a dermatomal distribution rather than pain confined to an
anatomic region such as a joint or specific bone. The orthopedic examina-
NEUROLOGIC CONDITIONS CAUSING LAMENESS IN COMPANION ANIMALS 25
tion and ancillary tests for orthopedic diseases are covered more thor-
oughly in another article in this issue. Neurologic evaluation may reveal
LMN disease affecting the involved nerve roots. It may be difficult to
distinguish between neurogenic and disuse muscular atrophy. Conscious
proprioceptive or other postural reaction deficits may be present in the
involved limb. If the nerve roots of C8 through T2 are involved, there
may be ipsilateral Horner's syndrome and loss of the cutaneous trunci
(panniculus) reflex. The Horner's syndrome can be explained by the
interruption of the sympathetic supply to the pupil, which exits with
spinal nerves Tl through T3. An ipsilateral cutaneous trunci reflex deficit
is caused by disruption of the lateral thoracic nerve, a motor nerve that
has a cell body origin at the level of the C8 and Tl spinal cord segments.
A careful sensory evaluation for paraspinal hyperesthesia could
discern an area of hypersensitivity associated with the nerve-root
involvement. Paraspinal palpation is done from a caudal to cranial
direction with the stimulus increasing from light touch to deep palpa-
tion. A behavioral reaction to what should be an innocuous stimulus
can be interpreted as pain. Placing one hand on the abdomen as the
vertebral column is palpated allows detection of abdominal muscle
splinting when pain is experienced. Cervical palpation is performed by
firmly pressing on the transverse processes from Cl to C7. The cervical
area can also be examined by flexing and extending the animal's neck.
During palpation, areas of hyperesthesia are noted and compared with
the presenting nerve-root signs. If Significant correlation is found be-
tween the sensory examination and the nerve-root distribution of the
limb-carrying lameness, further diagnostic testing is warranted. Previous
administration of anti-inflammatory or analgesic medications and over-
excitement of the animal during the examination may influence the
results of the sensory examination.
Diagnostic testing for suspected nerve-root impingement from a
lateralized disk includes electro diagnostic testing and advanced neuro-
imaging. If the extruded disk material is calcified, radiopaque material
may be seen within or adjacent to the intervertebral formina with routine
survey radiographs. Orthognic views (perpendicular to each other) are
needed to accurately localize an extruded IVD. Oblique views accentuat-
ing the intervertebral space are helpful in demonstrating which side of
. the spinal cord the disk is affecting. Myelography and epidurography
may show evidence of IVDD such as a protruding disk. These studies
can be normal, however, because a lateralized disk is outside the verte-
bral canal and cannot be seen readily with these imaging techniques.
s
Electrodiagnostic testing that may be helpful in investigating lateral-
ized disks includes EMG, nerve conduction, and f-wave analysis. Herni-
ated lateralized disks that cause compression can cause EMG changes
characterized by denervation potentials in a typical peripheral nerve
distribution pattern.
42
, 53, 54 For example, compression at the L4 nerve root
would result in denervation potentials in the quadriceps, iliopsoas, and
sartorius muscles. Although specific diseases cannot be diagnosed with
eJectrodiagnostic testing, specific nerve distribution can be mapped out
26 McDONNELL et al
with these tests, which aid in selecting advanced neuroimaging and
treatment planning. It commonly takes 5 to 7 days ?-e,nervation
potentials to develop after nerve pathology occurs
53
; thus, It IS Important
to know when the signs first developed. Performance of an EMG evalua-
tion before this 5-day window may result in false-negative results. Nerve
conduction should be normal, because only the peripheral portions of
the nerves are examined. F-wave analysis may be a useful electrodiag-
nostic technique to investigate the peripheral nerve proximal to the point
of stimulation and ventral roots.
Advanced imaging techniques reported to be useful in diagnosing
lateralized IVD include computed tomography (CT), magnetic resonance
(MR) imaging, linear tomography, diskography, and ultrasonograPI:y
(US). Equipment costs and training typically lm:ut the avail-
ability of these techniques to referral and other larger practIces. CT and
MR imaging are advantageous in diagnosing
of the transverse nature of the images and the abIhty to VIew the Image
of interest in multiple planes (Fig. 2).27,45,59,62 The normal anatomy and
pathologic conditions of the canine spine have been 19, 35
Mineralized disk material would appear hyperdense on CT Imagmg and
T2-weighted MR imaging. Tl-weighted MR imaging of mineralized disk
material would be iso- or hypointense.
19
, 35, 59 There is an advantage to
using CT after myelography to precisely localize the lesion when it
occurs in the cervical and thoracolumbar spine. 1, 19
Figure 2. A soft-tissue window, transverse CT image at the level of the L7-S1 intervertebral
disk space in a 4-year-old male neutered Rottweiler presenting with a 3-year history of left
pelvic limb lameness unresponsive to nonsteroidal anti-inflammatory drugs .. A soft-tissue
mass (arrowhead) is present within the left intervertebral foramen, compressing the nerve
root. Surgical decompression showed a herniated lumbosacral disk. Myelogram and epldur-
ogram showed no abnormalities. After surgical decompression and disk removal , all clinical
signs resolved. (Courtesy of Leigh Glerum, DVM, University of Georgia, Athens, GA)
NEUROLOGIC CONDITIONS CAUSING LAMENESS IN COMPANION ANIMALS 27
Linear tomography and diskography. offer little advantage over CT
and MR imaging, but the equipment may be more available because it
is less expensive. Linear tomography uses radiographic equipment that
coordinates the X-ray tube and film movement around a central pivot
point. Objects within a specific imaging plane are in sharp focus, whereas
superimposed structures above and below the imaging plane are
blurred.
33
Diskography involves the injection of contrast material under
fluoroscopic guidance through a spinal needle into the nucleus pulposus
of the IVDY, 54 This technique may be quite sensitive, especially when it
is interpreted with the results of radiographs, epidurograms, and EMG.54
In veterinary and human medicine, US has been used to identify
herniated disk material outside the vertebral column preoperatively as
well as to identify disk material intraoperativelyl6, 21, 46 Ultrasound im-
ages of peripheral nerves have been described in the dog.
22
Herniated
disk material is hyperechoic, allowing good contrast betvveen the disk
and the surrounding tissue at the intervertebral foramen or along the
spinal nerve. Ultrasound examination of the structures within the verte-
bral canal is restricted by the bony encasement surrounding the spinal
cord, although. intraoperative US after ventral slot or dorsal laminectomy
is extremely helpful in identifying disk material as well as in assessing
completeness of disk removal,16, 21, 46
The definitive diagnOSiS of a lateralized IVD requires surgical explo-
ration and sometimes histopathology of the disk, although most experi-
enced veterinary surgeons readily recognize nucleus pulposus. Surgical
exploration is guided by the results of the neurologic, radiologic, and
electro diagnostic tests performed. Access to various sites of the spinal
cord, intervertebral foramen, and paravertebral area has been described.
5
.
36, 61 Alternatively, prolonged conservative management with anti-
inflanunatory drugs may reduce the nerve-root signs in some patients.
The benefits of surgical exploration should be weighed against the
likelihood of treatment efficacy of the most likely diagnosis.
Degenerative Lumbosacral Stenosis
Degenerative LS stenosis, also known as LS instability, LS disease,
. and cauda equina syndrome, is a disease of older large-breed dogs, with
a predilection for male dogs.
J4
,31 The median age of affected animals has
been reported to be 7 years, with the most cases reported in German
Shepherd DogS. 13. 14,31 This is a rare condition in cats. The most common
disk space affected in dogs is L7 to S1, although any disk space from L5
to S3 may be affected. In most dogs, the spinal cord ends in the sixth
lumbar vertebrae. Nerve roots arise at the termination of the spinal cord
and run in the vertebral canal to exit at the intervertebral foramina.
When there is compression directly on these nerve roots, nerve-root pain
and dysfunction are the common results. The cause of degenerative LS
stenosis is multifactorial, but it is usually caused by disk extrusion and
stenosis, which often occur together.
28 McDONNELL et al
There is usually a presenting history of vague pain in most o.f
dogs, with common complaints of difficulty rising,
stairs, a reluctance to jump, and lamenessY14 Umlateral and mtermIttent
shifting limb lameness signs are common. A hist<:>ry of arthri!is or hip
dysplasia may exist, and some dogs improve WIth .anti-
inflammatory drugs or analgesics. Inability to raise the tall urmary
or fecal incontinence are usually later developments. On phYSIcal examI-
nation, there is focal pain over the LS junction. Digital pressure over the
LS junction or extension of the LS junction ?y lifting the pelvis while
pressing on the lumbar vertebrae are specIfic methods to assess LS
pain. Care must be taken to hip from
extension, as many of these dogs have hlp dysplasIa. Excellent palpation
of the hips with assessment of pain is required of the clinician to identify
hip dysplasia with and without LS disease. Li!?ht sedat.ion may. be
needed in performing hip palpation. If the dog obJects. to hlp
and the range of motion is poor, the dog may have hip d;:splasla
or without LS degeneration. If the dog objects to extreme hlp extenslOn,
but the range of motion is normal, LS disease should be suspected.
Paresis of the tail, limb, or sphincters is stronger evidence of LS degener-
ative disease, although these signs are less common now because of the
increased knowledge of the client and veterinarian.
Neuroimaging and electro diagnostics are the most helpful ancillary
diagnostic tools for LS degenerative disease. Survey radiographs <:>f
some benefit. Spondylosis is present in almost all such cases, but It IS
also common in clinically normal dogs of this size and age. Many of
these dogs have degenerative or developmental abnormalities seen on
plain radiographs.
32
, 40 Narrowing of the vertebral canal can be accentu-
ated by extension of the LS junction. Myelography can be to
demonstrate compression at the LS junction, although false-r,osltlve an.d
false-negative results are possible, the. spac: IS
absent in most large-breed dogs at the LS Junction. Epldurography IS a
relatively easy procedure useful in demonstrating LS is
performed by injecting iohexa!- <:>r a. lOdme solutlOn
in the epidural space. The mJection IS typIcally made caudal to S3
through Cdl and should not be made at the site of the suspected lesion.
Flexed and extended views of the LS joint during epidurography may
demonstrate a dynamic message. The interpretation and performance of
epidurograms require some experience. Diskography is another re.la-
tively easy procedure to perform and may d.lsk
protrusionY 54 Epidurograms and diskograms are snnplified by usmg
fluoroscopy. Myelography should precede .epidurograJ?hy and. diskogra-
phy, as the presence of epidural contrast mterferes WIth the mterpreta-
tion of the myelogram.
Images obtained with CT or MR ar: superior. to those
obtained using conventional radiography in dlagnosmg laterahzed dIsks
in the LS area, as disks are commonly located in the lateral recesses of
the sacrum, causing compression of the nerve root.
l
, 27, 28, 45. 59 The normal
anatomy of the LS area has been described.
1
.
26
Mineralized disk material
NEUROLOGIC CONDITIONS CAUSING LAMENESS IN COMPANION ANIMALS 29
would appear hyperdense on CT imaging and T2-weighted MR imaging
(see Fig. 2). Tl-weighted MR imaging of mineralized disk material
would be iso- or hypointense.
1
.
26
Bloom artifact may be a problem in
CT-myelography examination of the LS spine.
27
.
45
Intravenous contrast
administration has been shown to be helpful in diagnosing LS
stenosis.
28
, 45
Electrodiagnostic testing is useful to confirm suspected cases of LS
degenerative disease. Motor nerve conduction and f-wave analysis may
be normal in patients with LS pain as the only sign. The presence of
EMG changes such as fibrillation potentials and positive sharp waves in
affected muscles of the pelvic limbs, paravertebral area, tail, and peri-
neum confirms the location of the lesion. 53, 54 Mapping the distribution
of the abnormality is useful in estimating the extent and severity of
the lesion. 54
Prolonged medical management with strict cage rest and anti-
inflammatory drugs may benefit first-episode patients with minimal
signs. Animals with recurrent signs, severe unrelenting pain, or LMN
signs are good candidates for early surgical intervention.
13
, 14 The defini-
tive diagnosis' of LS degenerative disease requires surgical exploration
usually via a LS laminectomy and diskectomy with or without foramin-
ectomy depending on neurologic, radiographic, electrodiagnostic, and
surgical findings. The surgical approaches to the LS area have been
described.
61
Dogs with chronic compressive lesions have an excellent
prognosis if treated surgically unless there are severe LMN deficits.
Spinal Cord Neoplasia
The spinal cord may be affected by metastatic or primary tumors
arising from the surrounding supporting structures such as the verte-
brae, fibrous tissue, cartilage, or blood vessels associated with the verte-
brae.
38
Primary neural tumors also affecting the spinal cord include
astrocytoma, glioma, ependymoma, neuroepithelioma, menigioma, me-
ningeal sarcoma, malignant peripheral nerve sheath tumor (MPNST),
lymphosarcoma, and reticulum cell sarcoma.
38
Epidural lymphosarcoma
is the most commonly reported spinal tumor in cats.
31
, 43, 57 MPNST is
discussed in the next section of this article. Clinical signs typically
reflect the location of the tumor and usually result in slowly progressive
neurologic deficits. Spinal cord tumors that impinge on spinal nerve
roots or the cervical and lumbar intumescences may re:;;ult in nerve-root
signs and lameness.
lo
. 35, 38 Spinal cord tumors and lesions distant from
the origin of the spinal nerve roots have been reported to cause nerve-
root signs in human patients.
23
, 47 Newton and Rea
41
propose that these
signs are caused by tumor-induced distortion and demyelination of
cervical dorsal sensory axons. This phenomenon has not been reported
in animals.
Diagnosing a spinal cord tumor causing lameness or nerve-root
signature requires signalment evaluation, a complete physical examina-
30 McDONNELL et al
tion, and choosing appropriate ancillary diagnostic tests. Tumors more
commonly occur in large-breed dogs older than 5 years of age.
33
,38 Feline
spinal lymphosarcoma is more common in young animals.
31
, 43, 57 Nerve-
root signs may be obvious on physical examination, and neurologic
evaluation may show LMN signs. Muscle atrophy may be present in a
spinal nerve distribution, although distinguishing between neurogenic
and disuse atrophy may be difficult. Postural reactions may be delayed
in the limbs that are caudal to or at the site of the tumor. If the nerve
roots of the cervicothoracic spinal cord are involved, Horner's syndrome
and abnormalities in the cutaneous trunci reflex may be present as
described in the section on IVDD. Paraspinal hyperesthesia may be
found with careful palpation. Extradural and intradural-extramedullary
tumors commonly have hypersensitivity associated with a process in-
volving the nerve roots, the vertebrae, the IVD, or the meninges. Intra-
medullary tumors are rarely associated with signs of pain in people and
animals.
Ancillary diagnostic tests may include radiology and myelography,
electrodiagnostic testing, and advanced neuroimaging (MR imaging or
CT). Spinal column radiographs may detect neoplasia involving the
vertebral bone or cartilaginous support structures that compress the
spinal cord or nerve roots exiting the intervertebral foramen. Myelogra-
phy cannot definitively diagnose spinal cord tumors but should allow
identification of the site of the tumor and its relation to the spinal cord
and meninges (Fig. 3).38 Tumor classification as extradural, intramedul-
lary, or intradural-extramedullary may be difficult, because tumors may
occupy more than one of these compartments.
35
Nevertheless, classifica-
tion aids in the development of a differential diagnosis and prOVides
important information for prognosis and treatment planning.
Figure 3. Lateral (AJ and ventrodorsal (B) myelogram of the cervical spine in a 9-year,0Id
male neutered Labrador Retriever presenting with an 8-week history of right thoracic limb
lameness and infraspinatus and supraspinatus muscle atrophy. An intradural-extramedullary
filling defect (arrowheads) is seen at the level of C6-C7. Surgical exploration revealed a
meningioma compressing the right C7 nerve root.
NEUROLOGIC CONDITIONS CAUSING LAMENESS IN COMPANION ANIMALS 31
Electrodiagnostic testing can diagnose neither specific diseases nor
tumor types but aids in identifying whether abnormalities such as atro-
phy, pain, and other equivocal signs of lameness are caused by neuro-
logic or orthopedic disease. EMG, nerve conduction studies, and f-wave
analysis can define and localize peripheral or nerve-root disease, which
aids in the selection of advanced imaging and treatment planning. Elec-
trodiagnostic tests have been previously discussed in this article,
Advanced neuroimaging such as CT and MR imaging can aid
in the diagnosis of spinal cord tumors and is considered superior to
myelography in detecting the exact location of spinal cord tumors.
Iodinated compounds are used to enhance spinal tumors when exam-
ined by CT, whereas gadolinium-DTPA (Magnavist; Beilex Laboratories,
Wayne, NJ) is used when spinal tumors are examined by MR imaging.
Reports describe the different CT and MR imaging characteristics of
various tumors of the spine and spinal cord.
1
, 18, 29, 35 Intraoperative US
after dorsal laminectomy has been described in dogs with spinal cord
tumors, which helped to delineate the relation to the spinal cord and
the extent of the tumor.16 Tumor location and appearance are critical in
developing a 'more accurate diagnosis, better surgical planning, and
prognosis.
The definitive diagnosis of spinal cord neoplasia requires surgical
biopsy and histopathology of the lesion. Biopsy is guided by the results
of the neurologic, radiologic, and electro diagnostic tests performed. Ac-
cess to various sites of the spinal cord has been described.
6
, 36, 61 The
benefits of surgical biopsy should be weighed against the likelihood of
treatment efficacy of the most likely diagnosis.
Malignant Peripheral Nerve Sheath Tumors
MPNSTs, also called neurofibromas, schwannomas, and neurofibro-
sarcomas, arise from the myelin-producing cells (Schwann cells) or con-
nective tissue surrounding nerves.
4
, 7, 58 These are slow-growing tumors
that extend by local invasion along any of the peripheral nerves and
their branches. They rarely invade surrounding tissue, and metastasis is
also rare. Although any peripheral nerve can be affected, more than 80%
. of the reported cases involve the brachial plexus or its nerve roots,58
Other sites affected include the pelvic plexus, thoracolumbar nerves,
and cranial nerves. MPNSTs affect mature dogs with no sex or breed
predilection and only rarely affect cats,58,64
The tumors that affect the brachial or pelvic plexus result in slow
but progressive unilateral lameness and muscle atrophy of the thoracic
or pelvic limb, respectively. The initial presenting complaint is typically a
chronic and progressive non-weight-bearing lameness that is minimally
responsive to anti-inflammatory medications. Signs of LMN disease
affecting the involved limb include hypotonia, flaccid paresis, hypore-
flexia, and muscle atrophy. The muscle atrophy, hyporeflexia, and hypo-
tonia usually have a distinct spinal or peripheral nerve distribution.
Early in the course of the disease, it may be difficult to distinguish
32 McDONNELL et al
between neurogenic and disuse muscular atrophy. Conscious proprio-
ceptive deficits may be present in the involved limb at an early stage in
the disease. With involvement of the brachial plexus, MPNSTs may have
axillary pain and a palpable mass. Ipsilateral Homer's syndrome and
abnormalities in the cutaneous trunci reflex may be present as described
in the section on IVDD. MPNSTs can extend proximally along the nerve
and compress the spinal cord, causing deficits in the opposite limb. If
an MPNST of the brachial plexus invades the spinal cord, upper motor
neuron signs may be present in the pelvic limbs.
Diagnosis of MPNSTs requires a high degree of suspicion based on
the animal's signalment and choosing the appropriate ancillary diagnos-
tic testes) based on the results of a complete physical examination.
Helpful diagnostic aids include plain film radiographs, myelography,
electrodiagnosis, and advanced neuroimaging such as MR imaging, CT,
or US. Radiographs of the involved limb and associated vertebral spine
could rule out an MPNST by detecting osseous neoplasia or other
obvious musculoskeletal abnormalities. Myelography can outline spinal
tumors, including MPNSTs that have invaded the vertebral canal (Fig.
4). MPNSTs are typically classified as extradural or intradural-extramed-
ullary tumors. Electrodiagnostic techniques useful in diagnosing periph-
eral nerve disorders include EMG and nerve conduction studies.
JO
53
The electrodiagnostic abnormalities are denervation potentials, nerve
conduction slowing or block, and f-wave slowing or block. Although
electrodiagnostic testing cannot definitively diagnose MPNSTs, the ab-
normalities have a typical spinal or peripheral nerve distribution, which
can aid in the selection of advanced neuroimaging and treatment plan-
ning. If the contralateral limb has denervation potentials, there is a high
possibility that the MPNST has involved the spinal cord.
CT and MR imaging diagnosis of canine MPNSTs have been de-
scribed and are advantageous, because the transverse nature of the
images allows visualization of nerve roots, spinal nerves, and proximal
portions of the peripheral nerve.
39
, 44 If the images are centered on the
vertebral column, the contralateral clinically normal nerve root and
spinal nerves are available for comparison. MPNSTs may occur any-
where along the course of the spinal or peripheral nerve, however, and
may not be seen adjacent to the vertebral column. One recommendation
is to center the field of view on the affected limb, but this technique
requires a detailed knowledge of the normal anatomy.44 Contrast en-
hancement and signal characteristics have been described for human
and canine MPNST.9, 20,39, 44 CT visualization of the tumor is enhanced
with the intravenous administration of iodine contrast.
62
Nerve sheath
tumors in dogs and human beings have intermediate Signal on Tl-
weighted images and hyperintense signal on T2-weighted images, and
they show variable enhancement with the administration of gadolinium-
DTPA (Magnevist). 1,35, 62
US diagnosis of canine MPNSTs and human peripheral nerve sheath
tumors has been described.
4
, 44, 52 High-frequency US is highly sensitive
in the detection of nerve sheath tumors of the extremities; nerve sheath
NEUROLOGIC CONDITIONS CAUSING LAMENESS IN COMPANION ANIMALS 33
Figure 4. Lateral (A) and oblique ventrodorsal (B) myelogram of the lumbar spine of an
11-year-old female spayed Labrador Retriever that presented with a 10-month history of left
pelvic limb lameness unresponsive to nonsteroidal anti-inflammatory drugs, corticosteroids,
. acupuncture, and chiropractic manipulation. At the time of presentation, there was signifi-
cant muscle atrophy of the biceps femoris, graCiliS, and cranial tibial muscles. An intradural-
extramedullary filling defect (arrowhead) is seen at the level of L4. Electrodiagnostic testing
suggested that the mass was contiguous with the L6 nerve root. A soft-tissue window,
transverse CT image at the level of the L5-L6 intervertebral disk space (C) demonstrates
a soft-tissue mass exiting the left intervertebral foramen. Surgical decompression and
debulking revealed a malignant peripheral nerve sheath tumor of the left L6 nerve root.
tumors are recognized ;3.S a solid homogenous mass along the course of
the peripheral nerve. US has the advantage of allowing inspection of the
distal peripheral nerve and would eliminate or reduce the need for
anesthesia in veterinary patients. A high degree of clinical suspicion and
34 McDONNELLetal
a superior knowledge of the US anatomy of the region are required to
successfully diagnose these tumors.
The definitive diagnosis of MPNST requires surgical biopsy and
histopathology of the tumor. Biopsy is guided by the results of the
neurologic, radiologic, and electrodiagnostic tests performed. Access to
various sites of the spinal cord, brachial plexus, and lumbar plexus has
been described.
6
, 36, 61 The benefits of surgical biopsy should be weighed
against the likelihood of treatment efficacy of these tumors.
Traumatic Neuropathies
Traumatic injury to peripheral.nerves is a frequent cause of neuropa-
thies ill animals.
30
, 65 Common causes of nerve injury are mechanical
blows, gunshot wounds, fractures, pressure, and stretching. Iatrogenic
causes include trauma from intramedullary pins (crushing, cutting, and
spearing the nerve), casts or splints (compression), injections into or
adjacent to the nerve, and direct trauma caused by manipulation.
65
Traumatic neuropathies can often be diagnosed based purely on history
and clinical signs, although if the trauma was not witnessed, it may be
difficult to differentiate between neurologic and orthopedic disease. A
history consistent with trauma includes free-roaming animals, previous
surgery, or concomitant orthopedic injury.
Physical examination findings include abrasions, contusions, lacera-
tions, abdominal organ injury, or chest wounds associated with vehicular
trauma or gunshot wounds. Orthopedic injuries, particularly humeral
fractures, pelvic fractures, and femoral fractures, must be carefully evalu-
ated to rule out peripheral nerve injuries that may affect the outcome of
_ fracture repair. It is an unfortunate situation when a peripheral nerve
injury is overlooked until after major orthopedic repair has been per-
formed. A complete neurologic evaluation needs to be performed on
these cases to prevent similar situations. Abnormalities detected during
the neurologic examination that would indicate spinal or peripheral
nerve injuries would include LMN signs such as flaccid paresis or
paralysis, hypotonia, hyporeflexia, and rapid neurogenic muscular atro-
phy. Neurogenic atrophy should be evident within 7 to 10 days of the
injury. The other hallmark sign of spinal nerve and peripheral nerve
injuries is sensory dysfunction, which is detected by mapping areas of
decreased or absent superficial pain. This can be performed by grasping
a fold of skin and pinching with a small hemostat. The three responses
that would indicate proper functioning of the nerve are a behavioral,
response, reflex withdrawal of the limb, or twitch of the skin.
Electrodiagnostic testing is helpful in evaluating the extent and
severity of traumatic neuropathies. Approximately 5 to 7 days must pass
after the injury before denervation potentials are detected on EMG.
Nerve conduction studies can be done proximal and distal to the injured
site to assess nerve integrity. Serial examination allows for monitoring
of regeneration after nerve injuryY,53
NEUROLOGIC CONDITIONS CAUSING LAMENESS IN COMPANION ANIMALS 35
Although not described clinically, US has been used to evaluate
peripheral nerve degeneration and regeneration after experimental tran-
section?2 In this report, the proximal transected nerve was consistently
visualized, whereas the distal portion of the transected nerve was more
difficult to identify. Nerve regeneration was detected sonographically in
three of four dogs in which regeneration was confirmed by histopathol-
ogy. This study would suggest that US could be used to monitor degen-
eration and regeneration of peripheral nerves in dogs as well as to
precisely localize peripheral nerve injury. 22 The results of the neurologic
evaluation and electro diagnostic testing would assist the US examination
by localizing sections of peripheral nerve injury. A detailed knowledge
of normal anatomy is essential in performing US examination of periph-
eral nerves.
MR imaging has not been described for evaluating peripheral nerve
injuries. MR imaging might provide useful information, but its expense
may preclude its usefulness in serial examinations. Assessment of trau-
matic neuropathies using MR imaging would also require a detailed
knowledge of normal anatomy.
Exploratoty surgery has been advocated to assess peripheral nerve
injury. The advantages of surgery would be direct evaluation of damage
and direct treatment either by surgical anastomosis or freeing the nerve
from inflammatory adhesions. The obvious disadvantage to this surgery
is the requirement for precise localization of the site of injury; the results
of neurologic, electrodiagnostic, and US examinations should help to
guide the surgeon to the most likely area of injury.
SUMMARY
Animals presented with non- weight-bearing lameness are a diag-
nostic challenge for the veterinarian. It is extremely important to distin-
guish between orthopedic and neurologic causes of lameness, because
the diagnostic and therapeutic plans can be quite different. Myopathies
can be confused with orthopedic disease because of gait abnormalities
and associated muscle pain. Common myopathies seen in companion
animal medicine include polymyositis, muscular dystrophy, endocrine
. and infectious myopathies, and myasthenia gravis. Lameness caused by
disease of the nerve root or nerve is confused with orthopedic disease
because of the disturbances of a nerve's sensory distribution (nerve-root
signature) or disruption of the motor innervation. T h ~ diseases of the
nerve root or nerve discussed are lateralized intervertebral disk disease,
spinal cord neoplasia, malignant peripheral nerve sheath tumors, and
traumatic neuropathies.
The diagnosis of these diseases requires careful attention to the
signalment, a complete history, and a thorough physical examination
focusing on the neurologic and orthopedic components. Ancillary testing
should be selected based on these results and a minimum database.
Electrodiagnostic testing, radiography, and advanced imaging may help
36 McDONNELL et al
to localize the lesion more precisely and sometimes to confirm the
diagnosis. Surgical exploration and histopathology often provide the
definitive diagnosis.
These cases of non-weight-bearing lameness are a diagnostic chal-
lenge, but when successful resolution can be reached, it is gratifying to
the clinician, client, and patient.
References
1. Adams WH: The spine. Clin Tech Small Anim Pract 14:148-159, 1999
2. Amann JF: Muscle biopsy. In Bojrab MJ (ed): Current Techniques in Small Animal
Surgery, ed 3. Philadelphia, Lea & Febiger, 1990, pp 63--67
3. Bagley RS, Pluhar GE, Alexander JE: Lateral intervertebral disk extrusion causing
lameness in a dog. JAVMA 205:181-185, 1994
4. Bradley RL, Withrow SJ, Snyder SP: Nerve sheath tumors in the dog. J Am Anim
Hosp Assoc 18:915-921, 1982
5. Braund KG, Walker TL, Vandevelde M: Fascicular nerve biopsy in the dog. Am J Vet
Res 40:1025-1030, 1979
6. Braund KG, Taylor TK, Ghosh P, et al: Lateral spinal decompression in the dog. J
Small Anirn Pract 17:583-1592, 1976
7. Brehm DM, Vite CH, Steinberg HS, et al: A retrospective evaluation of 51 cases of
peripheral nerve sheath tumors in the dog. J Am Anirn Hosp Assoc 31:349-359, 1995
8. Burk RL: Problems in the radiographic interpretation of intervertebral disc disease in
the dog. Probl Vet Med 1:381-401, 1989
9. Castagno AA, Shuman WP: MR imaging in clinically suspected brachial plexus tumor.
AJR Am J Roentgenol 149:1219-1222, 1987
10. Chrisman CL: Electromyography in the localization of spinal cord and nerve root
neoplasia in dogs and cats. JAVMA 166:1074-1079, 1975
11. Coates JR: Intervertebral disk disease. Vet Clin North Am Small Anim Pract 30:77-
110,2000
12. Dallman MJ, Palettas P, Bojrab JM: Characteristics of dogs admitted for treatment of
cervical intervertebral disk disease: 105 cases (1972-1982). JAVMA 200:2009-2011, 1992
13. Danielsson F, Sjostrom L: Surgical treatment of degenerative lumbosacral stenosis in
dogs. Vet Surg 28:91-98, 1999
14. DeRisio L, Thomas WB, Sharp NJH: Degenerative lumbosacral stenosis. Vet Clin North
Am Small Anim Pract 30:111-132, 2000
15. Dhupa S, Glickman NW, Waters DJ: Functional outcome in dogs after surgical treat-
ment of caudal lumbar intervertebral disk herniation. J Am Anim Hosp Assoc 35:323-
331, 1999
16. Gallagher JG, Penninck D, Boudrieau RJ, et al: Ultrasonography of the brain and
vertebral canal in dogs and cats: 15 cases (1988-1993). JAVMA 207:1320-1324, 1995
17. Garrick JG, Sullivan CR: A technique of performing diskography in dogs. Mayo Clin
Proc 39:270--272, 1964
18. Green EM, Adams WM, Steinberg H: Malignant transformation of solitary spinal
osteochondroma in two mature dogs. Vet Radiol Ultrasound 40:634- 637, 1999
19. Hara Y, Tagawa M, Ejima H, et al: Usefulness of computed tomography after myelogra-
phy for smgery on dogs with cervical intervertebral disc protrusion. J Vet Med Sci
56:791-794,1994
20. Hems TE, Burge PD, Wilson DJ: The role of magnetic resonance imaging in the
management of peripheral nerve tumours. J Hand Surg [Brl 22:57--60, 1997
21. Hudson JA, Finn-Bodner ST, Steiss JE: Neurosonography. Vet Clin North Am Small
Anim Pract 28:943-972, 1998
22. Hudson JA, Steiss JE, Braund KG, et al: Ultrasonography of peripheral nerves during
Wallerian degeneration and regeneration following transection. Vet Radiol Ultrasound
37:302-312, 1996
NEUROLOGIC CONDITIONS CAUSING LAMENESS IN COMPANION ANIMALS 37
23. Ito T, Homrna T, Uchi yama S: Sciatica caused by cervical and thoracic spinal cord
compression. Spine 24:1265-1267, 1999
24. Jerram RM, Dewey CWo Acute thoracolumbar disk extrusion in dogs-Part 1. Compend
Contin Educ Pract Vet 21:922-930, 1999
25. Jerram RM, Dewey CWo Acute thoracolumbar disk extrusion in dogs-Part II. Compend
Contin Educ Pract Vet 21:1037-1047, 1999
26. Jones JC, Wright JC, Bartels JE: Computed tomographic morphometry of the lumbosa-
cral spine of dogs. Am J Vet Res 56:1125-1132, 1995 .
27. Jones JC, Sorjonen DC, Simpson ST, et al: Comparison between computed
and surgical findings in nine large-breed dogs with lumbosacral stenosIs. Vet RadlOl
Ultrasound 37:247-256, 1996
28. Jones JC, Shires PK, Inzana KD, et al: Evaluation of canine lumbosacral stenosis
using intravenous contrast-enhanced computed tomography. Vet RadlOl Ultrasound
40:108-114, 1999 .
29. Kippenes H, Gavin PR, Bagley RS,. et al: Magnetic resonance imaging features of
tumors of the spine and spinal cord m dogs. Vet RadlOl Ultrasound 40:627--633, 1999
30. Kornegay IN: Monoparesis (monoplegia) and cranial mononeuropathy. Penpheral/
cranial nerve and nerve root diseases. Probl Vet Med 3:356-362, 1991
31. Lane SB, Kornegay IN, Duncan JR, et al: Feline spinal lymphosarcoma: A retrospective
evaluation of 23 cats. J Vet Intern Med 8:99-104, 1994
32. Lang J, Hani H, Schawalder P: A sacral lesion resembling osteochondrosis in the
German shepherd dog. Vet Radiol Ultrasound 33:69-76, 1992
33. LeCouteur RA, Childs G: Diseases of the spinal cord. In Ettinger SJ (ed): Textbook of
Veterinary Internal Medicine, ed 3. Philadelphia, WB Samtders, 1989, pp 608--657
34. LeCouteur RA, Dow SW, Sisson AF: Metabolic and endocrme myopathIes of dogs and
cats. Semin Vet Med Surg (Small Anim). 4:146-155, 1989 ..
35. Levitski RE, Lipsitz D, Chauvet AE: Magnetic resonance imaging of the cervIcal spme
in 27 dogs. Vet Radiol Ultrasound 40:332-341, 1999 .
36. Lipsitz D, Bailey CS: Lateral approach for cervical spinal cord decompresslOn. Prog
Vet Neurol 3:39-44, 1992
37. Luttgen PJ: Miscellaneous myopathies. Semin Vet Med Surg (Small Anim) 4:168-176,
1989
38. Luttgen PJ: Neoplasms of the spine. Vet Clin North Am Small Anim Pract 22:973-
984, 1992
39. McCarthy RJ, Feeney DA, Lipowitz AJ: Preoperative diagnosis of tumors of the
brachial plexus by use of computed tomography in three dogs. JAVMA 202:291-294,
1993
40. Morgan JP, Bahr A, Franti CE, et al: Lumbosacral transitional vertebrae as a predispos-
ing cause of cauda equina syndrome in German shepherd dogs: 161 cases (1987-1990).
JAVMA 202:1877- 1882, 1993 . .
41. Newton HB, Rea GL: L'hermitte's sign as a presenting symptom of pnmary spmal
cord tumor. J Neurooncol 29:183- 188, 1996
42. Niederhauser UB, Holliday TA: Electrodiagnostic studies in diseases of muscles and
neuromuscular junctions. Sernin Vet Med Surg (Small Anim) 4:116-125, 1989
.43. Noonan M, Kline KL, Meleo K: Lymphoma of the central nervous system: A retrospec-
tive study of 18 cats. Compend Contin Educ Pract Vet 1997
44. Platt SR, Graham J, Chrisman CL, et al: Magnetic resonance rrnagmg and ultrasonogra-
phy in the diagnosis of a malignant peripheral nerve sheath tumor in a dog. Vet Radiol
Ultrasound 40:367- 371, 1999
45. Ramirez 0 III, Thrall DE: A review of imaging techniques for canine cauda equina
syndrome. Vet Radiol Ultrasound 39:283-296, 1998 .
46. Rubin JM: Ultrasonography in spinal cord surgery. In Rubm JM, Chandler WF (eds):
Ultrasound in Neurosurgery. New York, Raven, 1990, pp 68- 89 .. .
47. Sa to M, Takemitsu Y, Iwahara T, et al: Three cases of spmal cord tumor ongmatmg
from the second cervical nerve root. J Spinal Discord 11:354-358, 1998 .
48. Scavelli TD, Schoen A: Problems and complications associated with the nonsurgIcal
management of intervertebral disc disease. Prob Vet Med 1:402-414, 1989 .
49. Schulz KS, Walker M, Moon M, et al: Correlation of clinical, radiographic, and surgIcal
38 McDONNELL et al
localization of intervertebral disc extrusion in small-breed dogs: A prospective study
of 50 cases. Vet Surg 27:105-111, 1998
50. Seim HB III: Conditions of the thoracolumbar spine. Semin Vet Med Surg (Small
Anim). 11:235-253, 1996
51. Shelton GD: Acquired myasthenia gravis: What we have learned from experimental
and spontaneous animal models. Vet Immunol Imrnunopathol 69:239-249, 1999
52. Simonovsky V: Peripheral nerve schwannoma preoperatively diagnosed by sonogra-
phy: Report of three cases and discussion. Eur J Radiol 25:47-51, 1997
53. Sims MH: Electrodiagnostic techniques in the evaluation of diseases affecting skeletal
muscle. Vet Clin North Am Small Anim Pract 13:145--162, 1983
54. Sisson AF, LeCouteur RA, Ingram JT, et al: Diagnosis of cauda equina abnormalities
by using electromyography, discography, and epidurography in dogs. J Vet Intern Med
6:253-263, 1992
55. Smith MO: Idiopathic myositides in dogs. Sernin Vet Med Surg (Small Arum) 4:156-
160, 1989
56. Spodnick GJ, Berg J, Moore FM, et al: Spinal lymphoma in cats: 21 cases (1976-1989).
JAVMA 200:373-376, 1992
57. Summers BA, Cummings JF, deLahunta A: Diseases of the peripheral nervous system.
In Veterinary Neuropathology. St Louis, Mosby Yearbook, 1995, pp 402-501
58. Taga A, Taura Y, Nishimoto T, et al: The advantage of magnetic resonance imaging in
diagnosis of cauda equina syndrome in dogs. J Vet Med Sci 60:1345-1348, 1998
59. Taylor SM: Selected disorders of muscle and the neuromuscular junction. Vet Clin
North Am Small Anim Pract 30:59-75, 2000
60. Tidwell AS: Advanced imaging concepts: A pictorial glossary of CT and MRI technol-
ogy. Clin Tech Small Anim Pract, 14:65-111, 1999
61. Tomlinson J: Surgical conditions of the cervical spine. Serrtin Vet Med Surg (Small
Anim) 11:225-234, 1996
62. Tomlinson J, Schwink KL: Surgical approaches to the spine. In Slatter D (ed): Textbook
of Small Animal Surgery, ed 2. Philadelphia, WE Saunders, 1993, pp 1038-1056
63. Watrous Bf, Lipscomb TP, Heidel JR, et aI: Malignant peripheral nerve sheath tumor
in a cat. Vet Radiol Ultrasound 40:638-640, 1999
64. Welch JA: Peripheral nerve injury. Semin Vet Med Surg (Small Anim) 11:273- 284, 1996
Address reprint requests to
John J. McDonnell, DVM, MS
Department of Clinical Sciences
School of Veterinary Medicine
Tufts University
200 Westboro Road
North Grafton, MA 01536
LAMENESS 0195- 5616/01 $15.00 + .00
OVERVIEW OF PAIN IN THE
LAME PATIENT
Spencer A. Johnston, VMD
Lameness can result from a wide variety of conditions. Although
lameness can occur as the result of a purely mechanical abnormality
such as a malunion or discrepancy in limb length, lameness is most
frequently associated with a condition that causes pain either alone or in
combination with a mechanical alteration. Lameness is most commonly
associated with joint abnormalities as compared with long bone changes,
because it is the critical function of joints to allow transfer of load from
one bone to another while allowing the smooth motion and angular
change that result in successful ambulation. Any abnormality that pre-
vents this from occurring, including articular and periarticular change,
strain placed on muscles and tendons, and ligament sprains, can cause
pain and lameness.
The International Association for the Study of Pain has defined pain
as "an unpleasant sensory and emotional experience associated with
actual or potential tissue damage, or described in terms of such dam-
age.""O Pain is distinguished from nociception, which is the neurophysio-
logic response to a stimulus that actually or potentially causes tissue
damage. Although human beings can readily express the subjective
experience of pain, it is always a challenge to integrate the concepts of
nociception and pain in animals, which cannot verbalize the experience
of pain. Despite this challenge, as any clinician dealing with patients
experiencing lameness is aware, except in unusual circumstances, it is
appropriate to attribute at least part of the clinical response of animals
to actual or potential tissue damage as pain and not just as nociceptive
reflex behavior.
From the Department of Small Animal Clinical Sciences, Virginia-Maryland Regional
College of Veterinary Medicine, Virginia Tech, Blacksburg, Virginia
VETERINARY CLINICS OF NORTH AMERICA: SMALL ANIMAL PRACTICE
VOLUME 31 NUMBER 1 JANUARY 2001 39
40 JOHNSTON
It is intuitively obvious why an animal with an acute fracture of the
diaphysis of a long bone or involving the articular surface is in pain and
has an altered gait even if the neurophysiology is not known by the
casual observer. It is less obvious why an animal with more subtle
musculoskeletal change such as that occurring in osteoarthritis (OA) is
in pain and lame. This article concentrates on the mechanism by which
pain may be associated with joint abnormalities and helps to identify
the potential causes as to why the patient suffering from OA or joint
injury experiences pain. Although OA is the focus of this article, many
of the tissues and processes that result in pain with OA are similarly
affected in other acute or chronic musculoskeletal injury. Lameness is an
avoidance behavior to prevent stimulation of nociceptors present in
these tissues.
STUDY OF PAIN MECHANISMS
Pain is most easily studied in experimental models involving an
acute noxious stimulus. Studies of more chronic pain typically involve
induction of acute inflammation, with subsequent examination of the
sequelae to the inflammatory event. There are few if any good studies
of chronic pain mechanisms secondary to mechanical change or the
combination of mechanical change and mild inflammation such as oc-
curs with OA32 Because of the lack of these types of studies as well as
the clinical finding of temporal variability of changes that occur in the
articular and periarticular tissues, the individual variability with respect
to pain expression,27 and the frequent discrepancy between radiographic
evidence of OA and the clinical expression of pain, it is difficult to make
. definitive statements regarding OA pain that apply to all patients.
Despite knowledge of these limitations, it seems reasonable to glean
information from the study of acute and inflammatory pain to help us
conceptualize why OA and other joint injury cause pain, Knowledge of
the types of tissues involved, the neural linkages, the response to me-
chanical and chemical stimuli, and the plasticity of the neural system
may lead to improved understanding of OA, pain, and lameness, includ-
ing the rationale for various treatment methods and the development of
a rational expectation for treatment outcome,
OSTEOARTHRITIS
OA can be defined as a slowly progressive disorder of movable
joints characterized by deterioration of articular cartilage, osteophyte
formation and bone remodeling, changes in periarticular tissues, and a
low-grade nonpurulent inflammation of variable degreeY It is consid-
ered to be a condition that is typically initiated by mechanical alteration
of the joint but can also be caused by normal forces acting on abnormal
cartilage. It is important to recognize that stability of the joint, with
OVERVIEW OF PAIN IN THE LAME PATIENT 41
appropriate transmission, dissipation, and absorption of forces generated
during motion, occurs only when all the constituent tissues function
normally.2 Articular cartilage is most frequently the focus of study of
this condition, with changes of the periarticular structures such as sub-
chondral bone, synovium, joint capsule, ligaments, and muscle receiving
less consideration. Because of the complex nature of OA, it is relatively
easy to focus on the more readily documentable changes of articular
cartilage that occur. It is more difficult to evaluate the periarticular
tissues involved. Unfortunately, because articular cartilage is aneural, it
is the changes in these periarticular tissues that have an integral role in
the pain and dysfunction associated with this condition.
The spectrum of clinical manifestations associated with OA is less
easily defined than are the pathologic changes. Pain is the clinical symp-
tom most frequently associated with OAs This pain may be quite vari-
able, being present in some patients with relatively minor radiographic
change of the affected joint, although it is absent in other patients with
much more dramatic evidence of change.
9
When considering a large
population of patients with OA, it is most commonly recognized that
pain intensifies "and becomes more persistent as OA progresses. During
the initial stages of OA, the condition may be asymptomatic. As OA
progresses, pain may be present only during motion and weight bearing.
As the condition progresses further, there may be continuous discomfort
that is exacerbated by motion and weight bearing. Ultimately, pain
associated with OA can become pervasive and affect nearly all activities,
including sleep. Alleviation of this pain is the goal of most treatments
of OA
The source of pain associated with OA is multifactorial. Although
the discomfort caused by this condition to the patient affected with OA
is easily understood, to the student studying OA, the physiologic cause
of the acute and chronic pain associated with OA is more elusive. The
situation is complicated even further when considering that it is well
recognized in human beings that pain is influenced by nonarticular and
supraspinal factors such as psychologic state, past experience, gender,
social status, and environmental factors .
s
, 28 Similar factors have not been
documented as influencing OA pain in dogs and cats. Nevertheless,
given the degree of human and animal interaction that occurs with pet
dogs and cats, it is reasonable to believe that similar nonarticular and
supraspinal factors can contribute to an animal's ability to cope with OA
NEURORECEPTORS AND NERVE FIBERS
Joints are innervated by articular branches from main peripheral
nerves and by branches of nerves that supply nearby muscles. These
articular nerves contain myelinated and unmyelinated afferent fibers as
well as unmyelinated sympathetic efferent fibers.3s It has been estimated
that 20% of the fibers of an articular nerve are myelinated, and 80%
are unmyelinated.
38
Postganglionic sympathetic efferent fibers make up
42 JOHNSTON
approximately 40% of joint nerve fibers, or approximately 50% of the
unmyelinated fibers.
I 7
38
Neuroreceptors are specialized neural structures that are necessary
to provide input from the peripheral tissues to the central nervous
system. Many types of specialized neuroreceptors exist, and their activa-
tion provides raw information for tactile, thermal, and pain sensations.
Joints typically contain mechanoreceptors and nociceptors. Mechanore-
ceptors are sensitive to mechanical stimuli such as stretch and pressure.
Their activation is important in sensing static position and dynamic
movement of the joint. Nociceptors are activated by a noxious stimulus,
which is a stimulus sufficient to potentially cause or actually cause tissue
damage. Under normal circumstances, the activation of nociceptors often
leads to the sensation of pain.
Input from peripheral mechanoreceptors travels to the dorsal spinal
horn via myelinated afferent fibers, most of which are classified as A[3
fibers. These relatively large myelinated fibers provide for the rapid
transmission of impulses to the spinal cord, where they synapse with
second-order neurons and interneurons in the dorsal spinal horn. Im-
pulses originating from mechanoreceptors that then ascend to supraspi-
nal centers are processed to provide information regarding joint position
and status. Nociceptive impulses travel along thinly myelinated (Ao)
and unmyelinated (C) fibers. These impulses travel from the joint to the
dorsal spinal horn, where they can converge and synapse on many of
the same second-order neurons to which the mechanoreceptors project.
Once a nociceptive impulse reaches the dorsal spinal horn, it can initiate
a reflex arc, sending a signal to periarticular muscle, or it can ascend the
spinal cord to the brain. It may also be modulated by inhibitory in-
terneurons or by descending neural mechanisms such as the endogenous
opiates (enkephalins and dynorphins) and be terminated. Impulses that
originate from nociceptors that ascend to supraspinal centers are proc-
essed to form the experience known as pain.
Postganglionic sympathetic efferent nerve fibers found in the articu-
lar nerves terminate near blood vessels and within the synovial lining
and sub synovial layers,24 and are associated with control of the vascular
tone of articular vessels.
38
Activation of these sympathetic fibers is re-
sponsible for vasoconstriction. Some sympathetic fibers contain neuro-
peptide Y, a peptide that causes vasoconstriction and may also potentiate
the action of other neurotransmittersY Postganglionic sympathetic fibers
may also be stimulated to produce prostaglandins and interleukin-l,
which then may act to sensitize type IV nociceptors.
I 6
The role of the
sympathetic response in arthritis is not entirely known, although it is
speculated that it may be more important in rheumatoid arthritis than
inOAY
Once a nociceptor is stimulated, it is likely to respond to subsequent
noxious stimulation more vigorously and at a lower activation threshold.
This phenomenon is termed hyperalgesia. Hyperalgesia is commonly
associated with the presence of inflammatory mediators released from
damaged tissue. Inflammatory mediators that directly excite the nocicep-
OVERVIEW OF PAIN IN THE LAME PATIENT 43
tor are called algogenic substances. Bradykinin, a substance produced as
part of the clotting cascade, is considered to be algogenic. Other direct
stimulators of primary nociceptor afferents include histamine, serotonin,
and protons.
I 6
Other inflammatory mediators contribute to hyperalgesia
by lowering the threshold for nociceptor activation. Prostaglandin is
considered to act in this manner, although it has been suggested that
prostaglandins E2 and 12 can also act as direct sensitizers.
6
16
The area
experiencing tissue damage is considered to be the region of primary
hyperalgesia. Once an inciting event occurs, however, it is possible that
the surrounding tissues demonstrate an exaggerated response to further
stimuli. This phenomenon is termed secondary hyperalgesia. Secondary
hyperalgesia may occur as a result of collateral branches of afferent
nerves being primarily stimulated, or it may occur as a result of central
sensitization, which occurs because of the afferent fibers projected over
multiple segments of the spinal cord.
Primary afferent fibers distribute over a relatively large area of the
spinal cord. This results in poor localization of a stimulus associated
with a somatic region because of overlap of neural input, and it can
contribute to the sometimes relatively vague nature of joint pain. Within
the dorsal spinal horn, there are two types of (second-order) dorsal horn
neurons: nociceptive-specific and wide dynamic- range (WDR) neu-
ronsY Nociceptive-specific neurons respond only to noxious stimuli,
whereas WDR neurons respond to various stimuli, including noxious
stimuli. Chronic activation of primary afferent C fibers results in an
increase in the excitability of neurons in the spinal cord. This phenome-
non is known as central sensitization.
43
Central sensitization occurs as a
result of the activity of glutamate, substance P, and calcitonin gene-
related peptide (CGRP) within the dorsal horn. Release of these sub-
stances occurs as a result of stimulation from small afferent fibers. The
outcome is an alteration in the receptive field and a decrease in the
activation threshold of the dorsal horn neurons. Subsequently, there is
an increase in the magnitude and response of the postsynaptic ascending
spinal neurons to further noxious stimuli as well as an increased re-
sponse to low-threshold stimuli such as those originating from A[3
fibers. The expansion of the receptive field is consistent with secondary
hyperalgesia, where the area surrounding the region of primary tissue
injury also demonstrates increased sensitivity. In joint pain, this process
explains why tissues surrounding the injured joint are sensitive to stim-
uli. This phenomenon includes increased sensitivity of mechanoreceptors
and not just nociceptors. For example, an inflamed and painful joint
may not only demonstrate increased sensitivity to flexion and extension
but even light touch may elicit an exaggerated response, whereas it
may normally not even be recognized. The phenomenon of a normally
innocuous stimulus eliciting a painful response is termed al/odynia. Al-
though the stimulus would normally be considered innocuous, the mes-
sage that is transmitted to the supraspinal levels is consistent with
stimulation of nociceptor fields and is interpreted as being associated
with a noxious and painful event.
44 JOHNSTON
These changes in nociceptive threshold can occur with acute or
chronic injury. The process explains why joint tenderness and sensitivity
to motion or touch can occur after joint sprain or why muscle tenderness
(sensitivity to pressure or stretch) follows muscle strain. Avoiding joint
motion or decreasing the force placed on a limb helps to decrease
nociceptor activation and results in the clinical sign of lameness.
TYPES OF NEURORECEPTORS FOUND IN JOINTS
Much of the work describing the types of neuroreceptors present in
joints has been performed in cats.39 Wyke
44
described four types of
sensory receptors in joints. Type I and II receptors are mechanoreceptors
(receptor organs that respond to mechanical stimuli such as pressure or
tension). These receptors are located in the joint capsule, with type I
receptors located in the superficial layers and type II receptors located
in the deeper layers.
44
They are low-threshold receptors that are activated
by joint movement or pressure and are able to rapidly transmit this
information to the central nervous system via myelinated fibers. Both
type I and II receptors are thinly encapsulated organs. Type I receptors
are slowly adapting and thus serve static and dynamic functions . Type
II receptors are more rapidly adapting and thus have a more dynamic
function.44 The combination of input from type I and II receptors as well
as from other neuroreceptors located in the muscle and skin allows an
individual to recognize the orientation of the limb and joint in space.
3
,
32,39 The response properties of type II (mostly A(3) fibers are similar in
the normal and inflamed joint, and these fibers are not likely to have a
role in nociception.
39
Type III receptors are thinly encapsulated organs found on the
surface of ligaments.
44
Relatively large myelinated afferent fibers (Aex)
are attached to type III receptors, and these allow rapid transmission of
an impulse.
44
Type III receptors have a relatively high threshold and
thus require a substantial stimulus for activation. They are inactive at
rest and within normal and safe ranges of joint motion. They are acti-
vated when a strong mechanical stimulus approaching the level that
may cause tissue damage is present. As such, type III articular neurore-
ceptors are considered to be nociceptors.
Type IV receptors are actually free nerve endings.
44
These receptors
differ markedly from types I through III because they are not specific
receptor organs. With the exception of articular cartilage, type IV recep-
tors are found in all tissues of the joint, including subchondral bone.
Type IV receptors are nociceptors, They are high-threshold slowly adap-
tive receptors that are considered to be polymodal. Polymodal receptors
respond to mechanical stimuli as do type I through III receptors, and
they also respond to thermal and chemical stimuli and are thus inti-
mately involved in the pain associated with the inflammatory process.
Impulses from type IV receptors are transmitted toward the dorsal spinal
horn via thinly myelinated AS fibers or unmyelinated C fibers.
OVERVIEW OF PAIN IN THE LAME PATIENT 45
, Some type IV receptors are considered to be silent nociceptors.
39
These receptors are considered to be mechanoinsensitive under normal
do mechanosensitivity under inflammatory
condItI(:ms .. substances such as prostaglandin 2, bradykinin,
serotonm, hlstamme, nerve gro,,:,th factor can sensitize these recep-
tors. Under normal Clrcumstances, sIlent nociceptors do not contribute
any sensory information, after injury, they contribute to the barrage
of sensory Impulses reachmg the dorsal spinal horn and contributing to
central sensitization.
MECHANICAL STIMULATION OF ARTICULAR
NOCICEPTORS
Type IV nociceptors are typically stimulated by tension and pres-
sure. can result in nociceptor stimulation, this may help
to explam why motIon may exacerbate discomfort associated with the
osteoarthritic joint. Movement of a joint results in tension on one side of
the joint and co.mpression on the other. Intra-articular pressures
mcreased m?tlOn, and this in intra-articular pressure
IS correlated WIth pam? Increased synovIal fluid volume also creates
pressure and is frequently recognized in osteo-
such as in the patient with chronic OA secondary to
cruclate lIgament rupture. Increased fluid volume may also occur in the
early stage of OA: it has been documented with hip dysplasia
1s
,19 and
may also occur WIth any acute joint injury that results in inflammation
or hemorrhage. Another situation where there is a relative increase in
intra-articular pressure occurS when there is a decrease in atmospheric
pressure such as that occurring with the low-pressure systems typically
associated with bad weather.44
. st.imulation of type I and II neuroreceptors may also
mfluence nOClceptIon but in a manner opposite to direct stimulation of
type IV nociceptors, This occurs through the gate theory originally
by Melzack and Wall.
21
When all neuroreceptors experience a
stImul';ls .that exceeds the activation threshold, an impulse is generated,
and thIS travels via the afferent nerve fiber to the dorsal spinal
horn, where It synapses on a second-order neuron or an interneuron. At
this site, the impulse may ascend the spinal cord, initiate a reflex arc, or
be otherwise modified. The gate theory suggests that impulses generated
by (mainly types I and II) have the ability to stimulate
an inhIbItory mterneuron or directly block activation of second-order
neurons. by impulses generated by nociceptive afferents, thereby pre-
Impulses by nociceptor activation from ascending the
spmal cord. If nOCIceptor Impulses do not reach supraspinal sites, they
cannot ?e interpreted as contributing to the pain response.
. ThIS be used as a therapeutic modality. For the
patIent wIth.Jomt mJ:-rry, stImulation of peripheral mechanoreceptors can
be accomplIshed WIth transcutaneous nerve stimulators, massage of
46 JOHNSTON
tissues, or compression of overlying tissues with a bandage. In human
beings, it has been speculated that rhythmic stimulation of mechanore-
ceptors such as that occurring when the patient uses a rocking chair
provides relief from joint pain associated with OA.44 It is possible that
this mechanism also provides symptomatic relief in dogs and cats that
rest in a hammock type bed, where gentle movement along with redistri-
bution of force over a larger area instead of on focal pressure points
may be beneficial.
INFLAMMATION AND SENSITIZATION
Normal joints are painful only when an extreme force is applied
such as that occurring when the safe range of motion of the joint is
exceeded or when the tissues comprising the joint experience excessive
pressure. Once disease or injury is present, however, pain may be experi-
enced without motion or with normal motion. This occurs primarily
through chemical mediation, which is typically associated with the pro-
duction of inflammatory mediators. This occurs through sensitization of
joint afferents.
Although OA is considered to be a noninflammatory condition
characterized by variable degrees of mild inflammation, it is recognized
that the level of inflammatory mediators such as bradykinin, serotonin,
histamine, lactic acid, prostaglandin E
2
, and substance P is increased at
times, particularly during acute exacerbations. In addition, cytokines
such as interleukin-l, interleukin-6, and tumor necrosis factor-a are
increased in synovial fluid in the osteoarthritic joint and are believed to
influence the release of prostaglandins as well as tissue metalloprotein-
ases. Although they are most frequently associated with rheumatoid
arthritis, leukotrienes may also contribute to the inflammatory environ-
ment of the osteoarthritic joint because they are products of the lipoxy-
genase pathway of arachidonic acid metabolism. Nerve growth factor,
which is increased with inflammation, may also have a role in hyperalge-
sia by directly sensitizing nociceptors, increasing levels of substance P
and CGRP in peripheral tissues and centrally, and contributing to the
release of algogenic substances such as histamine.
1
All these inflamma-
tory mediators are believed to decrease the nociceptive threshold for
receptors within the joint.
When tissue injury occurs, whether as a result of OA or acute joint
injury, inflammation induces change not only in the periphery as just
described, but there are also changes in the dorsal spinal horn to enhance
these peripheral changes. Small afferents (C fibers) project to WDR
neurons in the dorsal spinal horn. These WDR neurons project supraspi-
nally to the brain stem and thalamus. Persistent activation of WDR
neurons by small afferents results in progressive enhancement of the
WDR response to subsequent input as well as an increase in the dimen-
sion of the peripheral receptive field to which the spinal neuron re-
sponds.
45
The basic response to small afferent activation is the spinal
OVERVIEW OF PAIN IN THE LAME PATIENT
47
of neurotransmitters such as the excitatory amino acids, which
mclude glutamate, and the neurokinins, which include substance P and
CGRP, from the presynaptic terminals.
4
Substance P activates second-
order neurons by acting on the neurokinin-l postsynaptic receptor. Glu-
tamate activity occurs through the N-methyl-D-aspartate (NMDA) and
non-NMDA postsynaptic receptors. It has been demonstrated that the
spinal ,?f substance P or of NMDA or non-NMDA recep-
tor a.gomsts e,:"okes and that administration of similar antagonists
portIOns of the pain response. In addition, prostaglan-
and mtnc OXIde are released from the spinal cord after a peripheral
stImulus, and these can further potentiate the release of substance P and
45 it is activity at the NMDA receptor that seems to
be Important m the development of spinal wind-up, the phenomenon
whereby the response to primary afferent stimulation increases dramati-
cally in amplitude and duration without an increase in peripheral input,
as well as rn the maintenance of cmonic pain as compared with acute
Gi:ren the activity of r:eurotransmitters such as glutamate, recogni-
tIon that rnflammatory medIators such as prostaglandins and nitric oxide
have a role in the spinal cord, and recognition that inhibition of these
substances results in alteration of nociceptive impulse transmission and
subsequent pain perception, it is interesting to speculate that this area
may become the focus of future treatment modalities for chronic pain
conditions, including OA.
Once a stimulus is received in the dorsal spinal horn, a reflex arc
to the joint may be initiated as well as an ascending impulse to the
brarn. The reflex arc may result in stimulation of the muscles sur-
rounding the joint or in the antidromic release of neuropeptides (sub-
stance P and CGRP) into the joint itself or near blood vessels in the
synovium and joint capsule. This phenomenon is termed neurogenic
These neuropeptides are found in the small unmyelinated
fIb.ers. Substance P is recognized as having many functions, including
bemg able to cause and perpetuate inflammation through stimulation of
prostaglandin and cytokine release, chemotaxis, and decreasing nocicep-
tor thereby perpetuating the cycle of inflammation and pain
WIth OA.15, 16 Substance P is considered to have an important
role m inflammatory arthropathies such as rheumatoid arthritis, but its
role in the development of OA is less well defined.
of is .typically directed toward the inflammatory
process .wIth Jornt mJury or toward providing pure analgeSia.
NonsterOIdal antI-rnflammatory drugs interfere with the .production of
an necessary for the production of prostaglan-
'penpherally and rn the dorsal spinal horn. Although nonsteroidal
have traditionally been thought to work in the
penphe.ry at SIte of mflammation, they may have central activity by
mterferrng WIth cyclooxygenase activity in the dorsal spinal horn or at
higher supraspinal centers.42
48 JOHNSTON
ANATOMY AND CHANGE WITH OSTEOARTHRITIS
The joint is primarily composed of the ends of the adjacent bones,
which are covered with hyaline cartilage. Subchondral bone (including
the subchondral bone plate and trabecular bone) supports the articular
surface. Synovium and fibrous joint capsule surround the joint. The joint
is held together by the synovium, joint capsule, ligaments, and travers-
ing muscle, and it is further stabilized by the congruity of the joint
associated with conformation of the bone ends.
Hyaline cartilage is a smooth wear-resistant tissue that serves to
dissipate the force of weight bearing from focal regions to the broader
articular surface. This is accomplished through the elasticity and com-
pressibility of cartilage that results from the combination of collagen,
proteoglycan, and water, which are its main constituents. Hyaline carti-
lage is maintained by a delicate homeostasis of chondrocyte anabolism
and catabolism. In OA, this homeostasis is disrupted, with the eventual
result being the loss of this smooth and resilient surface and the inability
to dissipate force from focal regions. This results in further cartilage loss
and pressure over focal areas of subchondral bone.
The subchondral bone region consists of a thin plate of bone that is
in direct contact with hyaline cartilage and the cancellous bone that
supports this bony plate. This region deforms with load application and
serves an important role in force distribution in normal joints. Thick-
ening of the subchondral bone plate and cancellous trabeculae occurs
during OA The combination of change in articular cartilage and sub-
chondral bone leads to a decrease in the ability to dissipate the forces
being transmitted across the joint. Subchondral bone contains unmyelin-
ated nerve fibers, which are usually associated with vessels, and these
fibers increase in number when OA is present.
36
Increased pressure on
subchondral bone caused by the loss of articular surface integrity results
in stimulation of these nociceptors and is thought to contribute to the
vague but consistent pain frequently associated with OAIn the human
hip, it has been recognized that there can be an increase in intra osseous
pressure of subchondral bone associated with venous stasis secondary
to soft tissue compression and femoral head deformity associated with
degenerative changeP This increase in intraosseous pressure may be
associated with chronic pain,14 particularly nocturnal pain.
33
The periosteum is richly innervated with nociceptors. Disruption of
the periosteum such as that occurring with long bone fracture leads to
stimulation of the nociceptors and is a source of pain. With fractures,
pain may also result from stimulation of unmyelinated C fibers found
in the cortical bone.
9
When OA is present, osteophytes may form at
the junction of the joint capsule, periosteum, and perichondrium. It is
suspected that elevation of the periosteum by osteophytes is associated
with stimulation of nociceptors in this tissue.
33
Movement of periarticular
tissues such as the joint capsule against the elevated periosteum may
result in stimulation of these nociceptors. As OA progresses, boundary
lubrication between the soft tissues and bone may decrease, increasing
OVERVIEW OF PAIN IN THE LAME PATIENT 49
friction between the soft tissues and periosteum and allowing additional
stimulation of the nociceptors present in these tissues.
The synovium is composed of two layers: the synovial lining layer
and the subsynoviallayer. The type A and B synoviocytes present in the
synovial lining layer serve to produce synovial fluid and provide a
cellular mechanism to remove debris from the joint. The subsynovial
layer consists of relatively loose connective tissue. Blood vessels, lym-
phatics, and free nerve endings are found in this layer. The subsynovial
layer serves to allow motion between the synovial lining layer and the
fibrous joint capsule.
Under homeostatic conditions, there is a normal ingress and egress
of fluid across the synovial lining layer. In OA, there is an increase in
the thickness of the synovial lining layer and an initial increase in the
production of synovial fluid. Synoviocytes become an important source
of inflammatory mediators, including cytokines and prostaglandins.
There is increased vascularity and cellular infiltration along with fibro-
plasia of the subsynovial layer. When OA becomes severe, the quality
and amount of synovial fluid present decrease, and the subsynovial
layer loses its nmmal function.
The joint capsule that surrounds the synovium is more fibrous in
composition and provides more of a structural and supportive function
than does the synovium. The fibrous joint capsule has a rich supply of
neuroreceptors. As a result of fibroplasia and irlcreased vascularity, the
joint capsule becomes thickened during OA, limiting its ability to distend
and stretch with motion. Subluxation of a joint, which is associated with
poor joint congruity, causes tension in or pressure on the joint capsule.
Once fibrotic changes occur in the joint capsule, less stretch in the joint
capsule caused by angular change or traction on the joint is necessary
to result in nociceptor stimulation. Joint dislocation similarly causes
stimulation of nociceptors in the joint capsule and ligaments.
Menisci are considered to be extensions of the joint capsule that
have been modified to form fibrocartilage.
34
When present, they function
to stabilize the joint and help to distribute load across the joint. Menisci
are known to contain C fibers in their outer one third.
26
Excessive
pressure on these tissues or disruption of the tissue by tearing and
subsequent increased stimulation of these nociceptors can contribute to
pain associated with acute injury or OA
Other sources of pain associated with OA are the ligaments and
muscles that surround the joint. Neuroreceptors are present in the liga-
ments that are either adjacent to or within the joint. These ligaments
may experience excessive strain with OA conditions because of the
abnormal biomechanics that exist.
23
Although neuroreceptors present in
ligament s may serve mainly to determine the spatial orientation of the
joint, strain on these tissues may contribute to the pain state23
Muscle function is important in supporting the joint. Input from
mechanoreceptors results in reflex facilitation or inhibition of flexor and
extensor muscles to allow smooth motion of the joint.
44
Mechanorecep-
tors and nociceptors have an important role in providing for reflex
50 JOHNSTON
contraction of muscles to help protect joints. For example, stimulation
of mechanoreceptors of the feline cranial cruciate ligament results in
increased tension of the extensor and flexor muscles of the stifle.
37
This
results in a reflex stiffening of the joint to applied loads, an action that
would likely serve to protect the joint surfaces from damage caused by
instability associated with loss of the stabilizing properties of the cranial
cruciate ligament,37
Muscle weakness is known to coexist with OA either as a contribut-
ing cause or as a result of disuse.
31
. 40 Muscle weakness is associated with
pain and disability.41 Pain in muscle tissue may result from increased
stress caused by abnormal biomechanics associated with OA-affected
joints or from muscle spasm. Muscle spasm may occur as a result off
the constant stimulation of musclE: tissue, resulting in a reflex arc associ-
ated with stimulation of neuroreceptors within the damaged joint.
46
Muscle spasm and muscle fatigue may greatly contribute to OA pain.
Muscle soreness frequently follows active use of the arthritic joint. This
is likely a result of the combination of muscle weakness creating a
condition whereby the muscle is poorly prepared to deal with even
normal weight-bearing forces and excessive strain produced by the
abnormal biomechanics and load application across the osteoarthritic
joint.
23
Release of inflammatory mediators resulting from this mild
trauma is likely to create sensitization of muscle nociceptors to further
mechanical stimulation.
22
Nociceptors are found in muscle, fascia, and tendons.
35
These noci-
ceptors can be stimulated by mechanical or chemical stimuli. Sensitiza-
tion of muscle nociceptors by inflammatory mediators such as bradyki-
nin and prostaglandin E2 after trauma or excessive exercise often results
in local tenderness, characterized by sensitivity to further mechanical
stimulation.
22
25 Afferent nerve fibers from muscle distribute over a
relatively large region of the dorsal spinal horn, resulting in poor local-
ization of muscle pain and contributing to its often vague nature,zO.22
JOINT INNERVATION AND OSTEOARTHRITIS
Experimentally, loss of joint innervation along with biomechanical
injury results in rapid progression of degenerative changes, whereas loss
of innervation alone does not result in substantial change.
29
.
3o
This is
thought to result from loss of the ability of muscle activity to protect the
abnormal joint from abnormal loads. It has been speculated that a
decrease in neural function may contribute to the loss of the normal
protective mechanism necessary to coordinate receptive impulses from
the joint with muscular activity necessary to protect the joint.
37
Although
this loss of function occurs with nerve damage, it has also been demon-
strated to occur with aging in mice and with chronic anterior cruciate
ligament injury in human beingsY Although a causal relation is not
clear, speculation can be made that the development of OA may be
influenced by the loss of joint receptor .input.
37
OVERVIEW OF PAIN IN THE LAME PATIENT 51
SUMMARY
Pain is often the limiting factor associated with joint disease. Pain
results from the stimulation of nociceptors by excessive mechanical
stimulation, chemical stimulation associated with the inflammatory proc-
ess, or a combination of both. Even though OA is considered to be a
noninflammatory disease, the mild degree of inflammation frequently
associated with this condition can result in peripheral sensitization.
This results in increased spontaneous activity and decreased activation
threshold of nociceptive fibers. Activity of the primary joint afferents
also leads to changes within the dorsal spinal horn, resulting in central
sensitization and changes in the neural structures of the dorsal horn
that facilitate and amplify the nociceptive response. Changes in the
periarticular tissues correspond to the neurobiologic changes, resulting
in increased stimulation of nociceptors caused by mechanical and chemi-
cal alterations resulting from tissue damage. Similar pathophysiologic
events occur regardless of whether the initiating event is an acute joint
injury or a chronic condition such as OA.
The combination of these events results in the complex dynamic of
joint pain. Because of this complex interaction of the musculoskeletal
and nervous systems, it is difficult to imagine a single treatment that is
effective for the alleviation of pain, because that agent would require
inhibition of a number of stimulatory pathways. Instead, restoration of
mechanical integrity, relief of peripheral inflammation, and blockage of
central neurotransmission are all likely to have a role in the relief of
joint pain and resolution of lameness.
References
1. Anand P: Nerve growth factor regulates nociception in human health and disease. Br
J Anaesth 75:201- 208, 1995
2. Billingham MEJ: Tissue interfaces in the synovial joint: Changes during the develop-
ment of arthritic tissue. In Archer CW, Caterson B, Benjamin M, et al (eds): Biology of
the Synovial Joint. Amsterdam, Harwood Academic Publishers, 1999, pp 347-360
3. Caron JP: Neurogenic factors in joint pain and disease pathogenesis. In Molwraith
CW, Trotter GW (eds): Joint Disease in the Horse. Philadelphia, WB Saunders, 1996,
pp 40- 70
4. Dickenson AH: Spinal cord pharmacology of pain. Br J Anaesth 75:193- 200, 1995
5. Dolan S, Field LC, Nolan AM: The role of nitric oxide and prostaglandin signaling
pathways in spinal nociceptive processing in chronic inflammation. Pain 86:311-320,
2000
6. Dray A: Inflammatory mediators of pain. Br J Anaesth 75:125-131, 1995
7. Goddard NJ, Gosling PTe Intra-articular fluid pressure and pain in osteoarthritis of the
hip. J Bone Joint Surg Br 70:52-55, 1988
8. Hadler NM: Why does the patient with osteoarthritis hurt? 111 Brandt KD, Doherty
M, Lohmander LS (eds): Osteoarthritis. New York, Oxford University Press, 1998,
pp 255- 261
9. Hannan MT, Felson DT, Pincus T: Analysis of the discordance between radiographic
changes and knee pain in osteoarthritis of the knee. J Rheumatol 27:1513-1517, 2000
10. Hoffert MJ: The neurophysiology of pain. Neurol Clin 7:183- 203, 1989
52 JOHNSTON
11. Johnston SA: Osteoarthritis: Joint anatomy, physiology, and pathobiology. Vet Clin
North Am Small Anim Pract 27:699-723, 1997
12. Kiaer T, Gronlund J, Sorenson KH: Intraosseous pressure and partial pressures of
oxygen and carbon dioxide in osteoarthritis. Semin Arthritis Rheum 18:57-60, 1989
13. Kidd BL, Cruwys S, Mapp PI, et al: Role of the sympathetic nervous system in chronic
joint pain and inflammation. Ann Rheum Dis 51:1188--1191, 1992
14. Kofoed H: Positive correlation between osteoarthritic pain and bone marrow pressure.
J Rheumatol 13:801-803, 1986
15. Konttinen Y, Gronblad M, Hukkanen M, et al: Pain fibers in osteoarthritis: A review.
Sernin Arthritis Rheum 18:35-40, 1989
16. Konttinen YT, Kemppinen P, Segerberg M, et al: Peripheral and spinal neural mecha-
nisms in arthritis, with particular reference to treatment of inflammation and pain.
Arthritis Rheum 37:965-982, 1994
17. Langford LA, Schmidt RF: Afferent and efferent axons in the medial and posterior
articular nerves of the cat. Anat Rec 206:71-78, 1983
18. Lust G, Summers BA: Early, asymptomatic stage of degenerative joint disease in canine
hip joints. Am J Vet Res 42:1849-1855, 1981
19. Lust G, Beilman WY, Rendano VT: A relationship between degree of laxity and
synovial fluid volume in coxofemoral joints of dogs predisposed for hip dysplasia.
Am J Vet Res 41:55-60, 1980
20. Marchettini P: Muscle pain: Animal and human experimental and clinical studies.
Muscle Nerve 16:1033-1039, 1993
21. Melzack R, Wall PD: Pain mechanisms: A new theory. Science 150:971-979, 1965
22. Mense S: Considerations concerning the neurobiological basis of muscle pain. Can J
Physiol Pharmacol 69:610-616, 1991
23. Merritt J: Soft tissue mechanisms of pain in osteoarthritis. Semin Arthritis Rheum
18:51-56, 1989
24. Messner K: The innervation of synovial joints. In Archer CW, Caterson B, Benjamin
M, et al (eds): Biology of the Synovial Joint. Amsterdam, Harwood Academic Publish-
ers, 1999, pp 347-360
25. Miles MP, Clarkson PM: Exercise-induced muscle pain, soreness, and cramps. J Sports
Med Phys Fitness 34:203-216, 1994
26. Mine T, Kimura M, Sakka A, Kawai S: Innervation of nociceptors in the menisci of the
knee joint: An immunohistochemical study. Arch Orthop Trauma Surg 120:201-204,
2000
27. Mogi! JS: The genetic mediation of individual differences in sensitivity to pain and its
inhibition. Proc Natl Acad Sci USA 96:7744-7751, 1999
28. Morin C, Lund JP, Villarroel T, et al: Differences between the sexes in post-surgical
pain. Pain 85:79-85, 2000
29. O'Connor BL, Palmoski MJ, Brandt KD: Neurogenic acceleration of degenerative joint
lesions. J Bone Joint Surg Am 67:562- 572, 1985
30. O'Connor BL, Visco DM, Brandt KD, et al: Neurogenic acceleration of osteoarthritis. J
Bone Joint Surg Am 74:367-376, 1992
31. O' Reilly S, Jones A, Doherty M: Muscle weakness in osteoarthritis. Curr Opin Rheuma-
tol 9:259-262, 1997
32. Perrot G, Guilbaud G: Pathophysiology of joint pain. Rev Rhum Engl Ed 63:485-492,
1996
33. Pinals RS: Mechanisms of joint destruction, pain and disability in osteoarthritis. Drugs
52(suppl 3):14-20, 1996
34. Ralphs JR, Benjamin M: The joint capsule: Structure, composition, ageing and disease.
J Anat 184:503-509, 1994
35. Randich A: Neural substrates of pain and analgesia. Arthritis Care and Research
6:171-177, 1993
36. Reimann I, Christensen SB: A histological demonstration of nerves in subchondral
bone. Acta Orthop Scand 48:345-352, 1977
37. Salo P: The role of joint innervation in the pathogenesis of arthritis. Can J Surg
42:91-100, 1999
38. Schaible HG, Grubb BD: Afferent and spinal mecharrisms of joint pain. Pain 55:5-54,
1993
OVERVIEW OF PAIN IN THE LAME PATIENT 53
39. Schmidt RF: The articular polymodal receptor in health and disease. Prog Brain Res
113:53-81, 1996
40. Slemenda C, Brandt KD, Heilman DK, et al: Quadriceps weakness and osteoarthritis
of the knee. Ann Intern Med 127:97- 104, 1997
41. van Baar ME, Dekker L Lemmens JAM, et al: Pain and disability in patients with
osteoarthritis of hip or knee: The relationship with articular, kinesiological, and psycho-
logical characteristics. J Rheumatol 25:125-133, 1998
42. Vasko MR: Prostaglandin-induced neuropeptide release from spinal cord. Prog Brain
Res 104:367-380, 1995
43. Woolf CJ: Somatic pain-pathogenesis and prevention. Br J Anaesth 75:169-176, 1995
44. Wyke B: The neurology of joints: A review of general principles. Clin Rheum Dis
7:223-239, 1981
45. Yaksh TL, Hua XY, Kalcheva I, et al: The spinal biology in humans and animals of
pain states generated by persistent small afferent input. Proc Natl Acad Sci USA
96:7680-7686, 1999
46. Zimmermann M: Pain mechanisms and mediators in osteoarthritis. Semin Arthritis
Rheum 18: 22-29, 1989
Address reprint requests to
Spencer A. Johnston, VMD
Department of Small Animal Clinical Sciences
Virginia-Maryland Regional College of Veterinary Medicine
Virginia Tech
Blacksburg, VA 24061-0442
e-mail: spencerj@vt.edu
LAMENESS 0195-5616/01 $15.00 + .00
FORELIMB LAMENESS IN THE
YOUNG PATIENT
James L. Cook, DVM, PhD
Forelimb lameness is a common problem in dogs less than 1 year
of age. The differential diagnoses for forelimb lameness in the young
patient are numerous and varied. Accurate and comprehensive diagnos-
tic and t r e a t m ~ n t plans must be carried out to optimize the prognosis
for these patients. Knowledge of the possible causes of the lameness as
well as appropriate treatment options should be mastered by the veteri-
nary practitioner.
Differential diagnoses for forelimb lameness in the young patient
can be divided into seven categories (Table 1). Congenital abnormalities
are those that are truly present at birth and thus most often occur in the
youngest of these patients. These problems mayor may not be the result
of genetic abnormalities. Developmental abnormalities occur during the
growth phases of a patient's life and may also have a genetic basis.
Traumatic injuries are common in young dogs. Idiopathic abnormalities
are a frequent cause of forelimb lameness. Infectious, nutritional, meta-
bolic, and neoplastic causes of lameness occur much less frequently in
young patients.
As discussed in previous articles in this issue, signalment and his-
tory can be important determinants in distinguishing between differen-
tial diagnoses for a given patient. It is vital that attention be given to
these areas and that interview of the client be conducted in such a way
.as to consistently obtain necessary information. The general physical
examination is also crucial in these patients. Nonorthopedic abnormali-
ties may occur concurrently and may have a significant impact on
diagnosis, treatment, and prognosis. The orthopedic examination in
From the Comparative Orthopaedic Laboratory, University of Missouri- Columbia, Colum-
bia, Missouri
VETERINARY CLINICS OF NORTH AMERICA: SMALL ANIMAL PRACTICE
VOLUME 31 NUMBER 1 JANUARY 2001 55
CJl
0'1
CJl
"
Table 1. DIFFERENTIAL DIAGNOSES FOR FORELIMB LAMENESS IN YOUNG DOGS
Category Disorder. Frequency Age'
Congenital
Shoulder luxation Rare First weeks to
months
Elbow luxation Rare First weeks to
months
Radial agenesis Very rare First weeks
Ectrodactyly Very rare First weeks
Mucopolysaccharidoses Very rare First weeks to
months
Osteogenesis Very rare First weeks to
imperfecta months
Oevelopmen tal
Osteochondrosis- Common 4-10 months
shoulder
Osteochondrosis-elbow Common 5-8 months
Ununited anconeal Common 5-12 months
process
Fragmented medial Common 4-9 months
coronoid process
Asynchronous growth Common? First months to
2 years
Ununited picondyles Rare 4-6 months
Retained cartilaginous Rare 4-8 months
cores
Carpal laxity syndrome Rare 2-5 months
Traumatic
Fractures Common Any
Luxations Uncommon Any
Sprains/strains Rare? Any
Muscle damage Rare? Any
Idiopathic
Pan osteitis Common Any
Hypertrophic Uncommon 2-8 months
osteodystrophy
Infectious
Septic arthritis/ Rare Any
osteomyelitis
Rickettsial arthritides Rare Any
Nutritional!
metabolic
Secondary Very rare Any
hyperparathyroidism
Vitamin 0 deficiency Very rare Any
Neoplastic
Osteosarcoma Very rare Any
'Most common age for clinical manifestation of di sorder.
t Gender that the disorder has a reported predilection for or higher frequency in.
:j:Breed(s) that the disorder is most commonly seen in.
Most frequently unilateral or bilateral involvement.
IIDiagnostics helpful for determining the diagnosis.
Gendert Breeds:t
n CH, PM, TP
M AK, BO, BH,
BT, CH, ~ C ,
GSO,MP,
MX, PG, PK,
SS, VT
n n
n n
n MP,MX, PH
n n
M Large and giant
breeds
M Large and giant
breeds (BMO,
GR, LR)
M Large and giant
breeds (esp
GSO)
M Large and giant
breeds
n n
n Large breeds
(esp LR)
n Large and giant
breeds
n OP, GO, GSO
n n
n n
n n
n ri
M BH,GSO
M? Large and giant
breeds
n n
n n
n n
n n
n n
UNI/BI Diagnosticsii Prognosis
BI P,R Guarded-good
BI P, R Poor-fair
UNI E, R Poor-fair
.uNI E,R Poor-fair
BI R, BW,S Grave
BI E, R, BW, S Grave
BI E, R, S Fair-excellent
BI E, R,S Poor-fair
UNI E,R Fair-excellent
BI E, R, S Poor-good
UNI/BI E,R Poor-excellent
BI E,R Fair-excellent
BI E, R Guarded-excellent
-:.
BI E Good-excellert t
UNI E,P,R Guarded-excellent
UNI E,P, R Guarded-excellent
UNl E, P, R, S Fair-excellent
UNI E, P, S Fair-excellent
UNIIBl E,P,R Good-excellen t
BI E,R Guarded-excellent
UNI/Bl E, BW, SF, C Grave .. :fair
BI E, BW, SF Guarded-excellent
BI E,R, BW Guarded-fair
BI E,R, BW Guarded-fair
UNI E,R,H Grave
M ~ male; n ~ none; AK ~ Akita; BD ~ Bulldog; BH ~ Basset Hound; BMD ~ Bernese Mountain Dog; BT ~ Boston Terrier; CH ~ Chlhuahua; DC ~ Dachshund;
DP ~ Doberman Pinscher; GO = Great Dane; GR = Golden Retriever; GSD = German Shepherd Dog; LR = Labrador Retriever; MP = Miniature Pinscher; MX = Mixed
Breed; PG = Pug; PH = Plott Hound; PK = Pekingese; PM = Pomeranian; SS = Shetland Sheepdog; TP = Toy Poodle; YT = Yorkshire Terrier; UN] = unilateral; Bl =
bilateral; BW = blood work (complete blood cell count, serum chemistries, titer); C = microbial culture; E = complete physical examination; H = hlstopathology; P =
palpation; R = radiographic examination; S = special procedures (advanced imaging, biochemical tests); SF = synovial fl uid analysis.
58 COOK
these patients must encompass all the facets discussed in the article on
evaluation of the lame patient. It is important to thoroughly evaluate
these young patients, as multiple disorders can occur in the patient.
This may be significant with respect to treatment and prognOS1S.
The diagnostic modalities used to differentiate the causes of fore-
limb lameness in the young patient are discussed for each disorder.
CONGENITAL CAUSES
Congenital causes of forelimb lameness that occur with at least
some ' frequency in young dogs include luxations of the shoulder and
elbow, agenesis or dysgenesis of portions of the limb, and .a number
of biochemical disorders resulting in deformity or dysfunchon. These
disorders may be genetic, traumatic, or the result of prenatal insult of
various causes.
Congenital luxation of the shoulder is an cause of lame-
ness in young dogs.
34
, 118 It occurs most frequently m small breeds of
dogs such as Toy Poodles, Chihuahuas, and Congenital
shoulder luxation is thought to result from an mhented weakness of the
supporting structures of the glenohumeral joint, a malformation of the
glenoid and humeral head, or both.3o, 52, 118 The luxation is frequently
bilateral. The humeral head luxates medially in nearly all cases,
Many affected dogs have only mild intermittent lameness with
occasional episodes of dysfunction. These dogs compensate for the ab-
normality by maintaining shoulder function through periarticular tissue
support for weight bearn:g. , , .
Diagnosis of congemtal shoulder luxahon 1S made based on S1g-
nalment, history, palpation of medial displacement of
cle with instability, and radiographic evidence of med1al luxatlOn w1th
abnormal glenohumeral conformation. .
Treatment should be based on clinical function. Surgery 1S not
recommended for dogs with pain-free weight-bearing function. These
dogs often continue to compensate well for the remainder of their.
They should be monitored for the effec,ts of secondary and
the possibility of traumatic exacerbahon of the ":'It,h appro-
priate treatment in the event that these occur. Dogs WIth clmlCal S1gnS
of pain and dysfunction are candidates for Reduc-
tion and stabilization of congemtal medIal shoulder luxatlOns have been
accomplished successfully. 52 Because the inherent laxity. and malfor-
mation of the joint, glenohumeral eXClSlOn, arthrodes1s, or, m rare cases,
amputation may be necessary for definitive treatment,34, 87, 112, 117, The
prognosis for nonathletic function is considered good m these pahents.
Affected dogs should not be bred... .
Congenital luxation of the elbow 1S also to a
tary disease affecting primarily small breeds of do!?s mcludmg
ese, Boston Terriers, Miniature Poodles, Pugs, Chihuahuas, MIniature
Pinschers, Dachshunds, and Yorkshire TerriersY, 18, 112 It has also been
f
FORELIMB LAMENESS IN THE YOUNG PATIENT 59
reported in larger breeds, including Bulldogs, Basset Hounds, Akitas,
Shetland Sheepdogs, mixed breeds, and German Shepherd Dogs.12, 18,35,71
Male dogs seem to be overrepresented?l The luxation is usually bilateral.
The cause is thought to involve agenesis or hypoplasia of the medial
collateral ligament, abnormal development of the humeral trochlea and
anconeal process, or both.
12
, 18 This disorder has been reported to occur
concurrently with ectrodactyly?3 Affected dogs should not be bred.
Dogs with congenital elbow luxation may be presented for evalua-
tion as early as 3 to 6 weeks of age with varying degrees of pain,
lameness, and dysfunction. These dogs may shown no gross lameness,
with owners complaining only of a firm swelling associated with the
elbow. Other puppies may be completely non-weight bearing on the
affected limb(s). The forelimbs typically demonstrate varus of the ante-
brachium, giving the dogs a "bow-legged" appearance.
1B
,71
DiagnOSiS of congenital elbow luxation is readily made based on
signalment, history, palpation of the abnormal articulation, and radio-
graphic findings. Congenital elbow luxation is categorized into three
types radiographically.6o Type I congenital elbow luxation is described
as a humeroradialluxation. The proximal radius is displaced caudolater-
ally and does not articulate with the humeral capitulum. Type II congeni-
tal elbow luxation is a humeroulnar luxation. The proximal radius has a
normal anatomic relationship to the humerus, but the ulna is displaced
in a laterally rotated manner. Type III congenital elbow luxations are
both humeroradial and humeroulnar, with the radius and ulna displaced
laterally to the humeral condyle and rotated approximately 90 to the
sagittal plane of the humerus.
Treatment of congenital elbow luxation depends on the age of the
animal, the severity of the luxation and clinical signs, the degree of
secondary changes present, and the intended use of the dog. The basic
tenet of treatment is early (3-4 months of age) aggressive therapy to
potentiate successful reduction and minimize the secondary growth
abnormalities and osteoarthritis that often occur.35, 71, 72, 122 Conservative
management of congenital elbow luxations is not effective. Humerora-
dial luxations have been reported to require a proximal radial wedge
osteotomy with internal fixation to achieve success.
18
Surgical stabiliza-
tion to address the medial collateral ligament abnormalities is often
-necessary as welp5 Secondary changes still progress, however, and the
prognosis is guarded. Humeroulnar luxations may be reduced using
closed or open techniques. Reduction is then maintained by transarticu-
lar pinning or trans articular external skeletal fixation.
71
,72, 122 Similarly,
secondary changes are common, and the prognosis is guarded. 'When
humeroradial and humeroulnar luxations are present (type III luxations),
combined techniques can be attempted, but the long-term prognosis is
poor at best.
Limb agenesis or dysgenesis is an infrequent cause of lameness in
puppies. Radial agenesis is a rare congenital defect in dogs and is
classified as an intercalary incomplete longitudinal paraxial hemimelia.
ll2
The cause is unknown. Ulnar agenesis has also been reported.
54
The
60 COOK
condition is most often unilateral. Radial agenesis is apparent soon
after birth, as it results in severe deformity and dysfunction. Physical
examination of the affected puppy reveals marked rotational and angu-
lar deformity of the forelimb with limited range of motion of the elbow
and carpus. The affected limb is usually nonfunctional as a result of
shortening, carpal varus, and hyperflexion. Some dogs traumatize the
skin of the lateral carpus and manus by trying to bear weight on
the limb.
Radiography of limbs with radial agenesis reveals complete or par-
tial absence of the radius with compensatory ulnar hypertrophy (Fig.
1).54 Rotational and angular deformities are noted as well as resultant
elbow and carpal subluxations.
Treatment options for radial a,genesis include amputation, arthrode-
ses, or corticocancellous (rib) bone-grafting techniques.
83
, 93, 112 The sal-
vage techniques are not often successful in restoring limb function;
therefore, amputation is considered the treatment of choice for unilateral
lesions. Euthanasia may be appropriate in bilaterally affected dogs;
however, some dogs compensate by ambulating entirely on the hind
limbs. Affected dogs should not be bred.
3
Ectrodactyly is a rare congenital failure of fusion of the embryonic
precursors of the bones of the forelimb.
21
, 73, 112 It is classified as a terminal
longitudinal partial adactylia.
ll2
The cause is unknown in dogs. Ectrodac-
tyly is noticed soon after birth. The condition is usually unilateral. The
deformity manifests as separation of the medial and lateral portions of
the affected limb, with the separation occurring between any of the
Figure 1. Radiographic views of the forelimbs of a 6-week-old male Jack Russell Terrier
with congenital radial aplasia depicting the normal (A) and affected (8) limbs.
FORELIMB LAMENESS IN THE YOUNG PATIENT 61
metacarpal bones and extending proximally to various levels of the
antebrachium. Soft tissue separation often accompanies the bone defect.
Affected dogs are presented because of the cosmetic defect and
various degrees of lameness or dysfunction. Definitive diagnosis can be
made on physical examination. Radiographic examination is important
to determine the degree of involvement and the validity of various
treatment options. Radiography may reveal aplasia or hypoplasia of
metacarpal and carpal bones, radioulnar hypoplasia, and associated
subluxations or luxations of the carpal or cubital jointS.
21
, 73
Treatment options vary with the type and severity of the defect.
Primary reconstruction of the bone and skin defects can be successfully
accomplished in cases with intact bone and joint structure. Reconstruc-
tion of the defects with carpal arthrodesis is also feasible if elbow joint
function is intact.
59
, 73 Secondary osteoarthritis and dysfunction may
occur with these options; thus, amputation is often the treatment of
choice in unilaterally affected dogs. Euthanasia may be necessary in
bilaterally affected dogs that cannot compensate or be surgically re-
paired. Affected animals should not be bred.
Skeletal dysplasia associated with retinal dysplasia of Labrador
Retrievers has been reported as a cause of forelimb lameness in yOWLg
dogs.
22
, 26 This syndrome is an inherited disease, resulting in abnormal
retinal differentiation and various manifestations of abnormal skeletal
development,22 Skeletal abnormalities involving the forelimb include
retarded and asynchronous growth of the radius and ulna, ununited and
hypoplastic anconeal and coronoid processes, and delayed epiphyseal
development.
22
,26 There is no definitive treatment for the ophthalmologic
or skeletal abnormalities. Affected dogs should not be bred.
Achondroplasia and hypochondroplasia are two other forms of skel-
etal dysgenesis that may result in forelimb lameness. These syndromes
are considered normal phenotypes for chondrodystrophoid breeds of
dogs, however. Secondary manifestations of these developmental traits
are usually necessary to result in lameness.
Many congenital, genetically based, biochemical alterations exist in
human beings that result in skeletal abnormalities. Relatively few of
these have been reported as causes of lameness in dogs. It is likely that
many other yet to be identified biochemically related abnormalities exist
. in dogs. It is also likely that some of these congenital abnormalities may
playa role in the developmental orthopedic diseases that are currently
of unknown cause.
Mucopolysaccharidosis has been identified in dogs and can result
in orthopedic disorders causing lameness.
50
,99 The mucopolysacchar-
idoses are a group of heritable autosomal recessive lysosomal storage
diseases.
39
, 50, 99 The disorder is a deficiency in the lysosomal enzymes
required for degradation of glycosaminoglycans. As a result, the gly-
cosaminoglycans are stored in the lysosome, causing progressive tis-
sue alterations and dysfunction. Resulting orthopedic abnormalities in-
clude dysostOSiS multiplex, articular dysplasias, osteoarthritis, and
dwarfism.
5o
,99 Diagnosis is based on clinical signs, identification of nu-
62 COOK
merous distinctive metachromatic granules within neutrophils and
monocytes on Wright's stained blood smears, excess undegraded gly-
cosaminoglycans in the urine, and radiographic findings of low bone
density with thin cortices and epiphyseal irregularities.
39
, so, 99 Definitive
diagnosis is based on measurement of lysosomal enzyme activity in
serum, leukocyte pellets, or frozen liver. 50, 99 Although bone marrow
transplant to young animals from a normal sibling donor has allowed
preservation of a near-normal life, a practical and effective treatment
method is not available at this time.
39
Affected animals should not
be bred.
. Collagen disorders are relatively common causes of skeletal abnor-
malities in people. More than 250 different mutations in the genes
that control the collagens involveci in skeletal development have been
recognized in human beings.
62
Osteogenesis imperfecta is one of these
disorders that has been reported in dogsY It is a heritable disease caused
by a mutation in a collagen type I geneY Clinically, it manifests as
lameness and dysfunction resulting from multiple fractures as a result
of brittleness of the bones. Radiographs of affected dogs demonstrate
multiple appendicular fractures in various stages of healing. Diagnosis
is made by ruling out metabolic bone diseases such as secondary hyper-
parathyroidism and by demonstrating collagen type I abnormalities in a
cell culture of dermal fibroblastsY No effective treatment is available at
this time in dogs, and affected dogs should not be bred.
DEVELOPMENTAL CAUSES
Developmental causes of forelimb lameness in the young dog are
commonly encountered in veterinary medicine, Early diagnosis and
treatment are vital for preserving function in these patients, Thorough
knowledge and understanding of these disorders are thus of the utmost
importance for the veterinary practitioner, Many of the developmental
and idiopathic causes of forelimb lameness can occur concurrently in
young dogs. It is thus imperative to be thorough and comprehensive in
the assessment of these patients,
Osteochondrosis (OC) lesions causing lameness in the forelimb pri-
marily involve the humeral head and the medial aspect of the humeral
condyle, 7, 29, 37, 38, 42, 43, 45, 57, 69, 80 The ununited anconeal process (UAP),
fragmented medial coronoid process (FMCP), and retained cartilaginous
cores have also been classified as OC lesions, In the strictest definition
of Oc, a disturbance of endochondral ossification, all these disorders
should be classified in this category. The etiopathogenesis of these disor-
ders is poorly understood, h o w e v e l ~ and likely involves a multifactorial
process, For the purposes of this discussion, OC refers to the articular
cartilage disturbances on the humeral head and condyle.
OC of the articular cartilage is a widely studied yet poorly under-
FORELIMB LAMENESS IN THE YOUNG PATIENT 63
stood disorder. * The cause is considered by most clinicians and research-
ers to be multifactorial, with genetic, nutritional, traumatic, and vascular
factors all having potential roles. These multiple alterations and insults
during skeletal development result in a progressive disturbance in the
endochondral ossification process, causing focal epiphyseal cartilage ne-
crosis, cartilage retention, failure of matrix calcification, vascular penetra-
tion, and ossification. This abnormal area of cartilage is structurally and
biomechanically inferior to surrounding cartilage and bone and is subject
to detachment and resorption with normal phYSiologic loading.
13
, 42, 57, 81
These abnormalities result in articular incongruity, synovitis, joint effu-
sion, pain, and lameness.
OC of the humeral head is a common cause of forelimb lameness
in young dogs. It most frequently occurs in the caudocentral region of
the humeral head. OC of the humeral head is most common in large
and giant breeds of dogs. Some large and giant breeds seem to be at
low risk for shoulder OC, however, and it has been reported in small
and medium breeds of dogs,57,96 Male dogs are reported to be affected
more often than female dogsP' 58, 84, 89, 96, 103 The onset of lameness from
shoulder OC typically occurs when the dog is between 4 and 8 months
of age, Affected dogs are often presented for a unilateral lameness of
variable severity. The disease may be either unilateral or bilateral, with
the reported incidence of bilateral shoulder OC ranging from 20% to
85% of cases.
29
, 42, 58, 84, 89, 96 Up to 80% of dogs with bilateral shoulder OC
are presented with only unilateral lameness. 58, 89, 96, 103 It is thus important
to carefully investigate the status of the contralateral shoulder in all
cases to prevent misdiagnosis and potentiation of pathologic changes in
the joint, ,
Physical examination of patients with shoulder OC typically reveals
a weight-bearing lameness in one or both forelimbs that is exacerbated
by exercise, Pain on flexion and extension of the shoulder is common,
Atrophy of the supraspinatus, infraspinatus, and deltoideus muscles
may also be apparent, Direct pressure over the tendon of origin of the
biceps brachii muscle or manual stretching of the muscle itself may elicit
signs of pain, Observation of the dog's gait often reveals a pronounced
"head bob" during weight bearing on the clinically affected limb. A
shortened stride in one or both of the forelimbs may also be noted. Some
'affected dogs are reluctant to stand or ambulate, It is vital to completely
examine the elbows of these patients as well, because many of these
disorders can occur concurrently.
Definitive diagnosis of shoulder OC is typically made from radio-
graphic examination, 57, 61 Sedation with analgeSia should be used for
positioning of these patients for radiography. The mediolateral radio-
graphic view is the most useful for making a diagnosis of shoulder
OC
57
, 61 Two orthogonal views should always be obtained, however,
When obtaining the mediolateral view, craniodistal traction is placed on
'References 7, 13, 15, 16, 29, 33, 37, 38, 41, 42, 43-46, 48, 49, 57, 58, 61, 69, 80, 81, 84,
89, 90, 94, 96, 103, 111, 114- 116.
64 COOK
the limb of interest while the contralateral limb is retracted caudally to
avoid problems of superimposition and summation. In addition, varymg
degrees of internal rotation of the forelimb may be necessary to elucidate
some OC lesions on the mediolateral view. Radiographic examination of
both shoulders is recommended in all cases. Radiographic findings may
include a radiolucent defect in the subchondral bone of the caudal
humeral head, intra-articular mineralized cartilage, and secondary osteo-
arthritic changes. Advanced imaging techniques such as contrast
arthrography, computed tomography, magnetic resonance imaging, or
,exploratory arthroscopy may be required for definitive diagnosis of
shoulder OC.
61
, 84, 114, 115 The author prefers exploratory arthroscopy of
the shoulder for definitive diagnosis that cannot be made on routine
radiographic examination.
Treatment options for shoulder OC include nonsurgical and surgical
modalities. Nonsurgical treatment consists of exercise restriction and
pain management for 4 to 6 weeks in an attempt to allow repair of the
cartilage abnormality and subsequent resolution of clinical signs.13,42, 57, 96
Resolution of lameness with conservative treatment is unpredictable and
may take approximately 7 months.13, 42 Nonsurgical treatment consisting
of vigorous exercise to produce detachment of the abnormal cartilage
with subsequent fibrocartilage repair has also been recommended, but
because of the potential for exacerbation of secondary pathologic
changes within the joint and persistent pain and lameness in these
patients, this protocol is not recommended.
57
Surgical treatment consists of removal of detached or abnormal
cartilage, debridement of the lesion, and curettage of the lesion to the
level of bleeding subchondral bone via open arthrotomy or arthroscopic
visualization.
38
, 58, 84, 89, 111, 114, 115 Debridement and curettage of OC lesions
allow for repair of the defect with functional fibrocartilage and a return
to pain-free function in most cases. Complete resolution of lameness has
been reported in 75% of cases treated surgically, with more than 90% of
these animals returning to an acceptable level of function.
96
Resolution
of clinical signs typically occurs within 4 to 8 weeks in dogs treated
with surgery. Recommendations for surgical therapy have been based
on the age of the animal, severity of the clinical signs, size of the OC
lesion, presence and location of detached cartilage flaps within the
joint, and secondary changes present.1
3
, 29, 42, 57, 58, 84, 89, 96, 103 The author
recommends surgical treatment of shoulder OC in all cases with clinical
signs attributable to the shoulder joint or where a demonstrable detached
flap of cartilage is present. In all patients fitting these criteria, we cur-
rently perform exploratory arthroscopy followed by removal of detached
cartilage flaps, debridement, curettage, and thorough joint lavage. This
treatment allows for assessment of the entire glenohumeral joint, bilater-
ally if necessary, as well as accurate and precise treatment of OC lesions
with minimal morbidity.
Minimizing the manifestation of OC in predisposed dogs is a crucial
component of a comprehensive health program in which the veterinarian
can playa vital role. Breeding of affected animals should be avoided.
FORELIMB LAMENESS IN THE YOUNG PATIENT 65
Nutritional management aimed at preventing rapid weight gain and
skeletal growth and maintaining dogs at an ideal lean weight is im-
portant in the prevention of all developmental ortI-lOpedic disorders in
dogs.
94
Avoiding overnutrition and oversupplementation of vitamins
and minerals should be strongly encouraged during initial conversations
with owners.
Incomplete ossification of the caudal aspect of the glenoid has been
reported as a cause of forelimb lameness in young dogs?8 This syndrome
has been proposed to be the result of Oc. It is still poorly understood
and characterized, however, and often occurs concurrently with other
causes of lameness.
78
The veterinary practitioner should rule out all other
potential causes of lameness in patients with incomplete ossification of
the caudal aspect of the glenoid and undertake surgical treatment of this
disorder with caution.
OC of the humeral condyle is considered to be attributable to the
same multifactorial etiopathogenesis as described for OC of the humeral
head. This disorder has been included in a group of developmental
abnormalities affecting the elbow joint of dogs and is discussed in the
subsequent section on elbow dysplasia.
33
Elbow dysplasia is a general term that has been used to describe a
group of developmental abnormalities affecting the elbow joint of
dogs.
33
, 37, 41, 86, 108, 124 UAP, OC of the medial portion of the humeral
condyle, FMCP, asynchronous growth of the radius and ulna, and un-
united epicondyles have all been included in this terminology. All these
disorders are similar in signalment and history, clinical signs, and diag-
nostic techniques employed and can occur concurrently. Each can have
vastly different treatment modalities and prognosis from the others,
however, and must be differentiated.
OC of tl'le elbow involves the medial portion of the humeral con-
dyle. Elbow OC occurs most commonly in large and giant breeds of
dogs, with Bernese Mountain Dogs, Golden Retrievers, Labrador Re-
trievers, and Rottweilers being overrepresented. 80, 86 The onset of clinical
signs is typically when the dog is between 5 and 8 months of age. Male
dogs are more commonly affected.
31
, 80, 90 The disease has been reported
to be bilateral in 20% to 50% of cases.
31
, so, 90
Physical examination of patients with elbow OC typically reveals a
weight-bearing lameness of variable severity in one or both forelimbs,
with pain on flexion and extension of the elbow. The lameness is often
exacerbated by exercise or minor trauma. Joint capsule distention re-
sulting from joint effusion can often be palpated in the standing dog
between the lateral humeral epicondyle and the olecranon. Periarticular
fibrosis is often present in older dogs. Muscle atrophy mayor may not
be present. Observation of the dog's gait often reveals a pronounced
"head bob" during weight-bearing on the clinically affected limb. A
shortened stride in one or both of the forelimbs may also be noted. Some
dogs hold the limbs with the elbows abducted, causing the owners to
complain of a bow-legged appearance. Some affected dogs are reluctant
66 COOK
to stand or ambulate. It is vital to completely examine the shoulders of
these patients to rule out concurrent abnormalities.
Definitive diagnosis of elbow OC can often be made from radio-
graphic examination. Sedation with analgesia should be used for posi-
tioning of these patients for radiography. Radiographic views that
should be obtained for diagnosis of dogs with elbow dysplasia include
a craniocaudal view, an extended mediolateral view, and a maximally
flexed mediolateral view.
33
, 41, 44, 61, 80 Various oblique views have also been
reported to be helpful for highlighting the craniomedial compartment of
the elbow joint for diagnosis of OC and FMCp'41, 61, 80, 123 The radiographic
' findings associated with elbow OC have been described.
33
, 41, 61, 80, 123
Radiographic findings may include a radiolucent defect in the subchon-
dral bone of the medial aspect of .the humeral condyle, with associated
sclerosis, roughening of the medial epicondyle, and varying degrees
of radiographic osteoarthritis. The secondary changes associated with
osteoarthritis, including periosteal proliferation on the dorsal anconeal
ridge, proximal radius, and medial aspects of the humerus and ulna
along with sclerosis of the trochlear notch, are the most consistent
findings noted. These secondary changes are common to all causes of
elbow dysplasia and only signify the elbow as the potential source of
the clinical signs without delineating a specific diagnosis. If definitive
diagnosis carmot be made on radiographic findings alone, more ad-
vanced imaging techniques, including contrast arthrography, linear to-
mography, computed tomography, magnetic resonance imaging, or
exploratory arthroscopy, may be required.
61
, 105 The author prefers explor-
atory arthroscopy for definitive diagnosis of causes of elbow dysplasia
that carmot be made on routine radiographic examination.
Treatment of elbow OC consists of removal of detached or abnormal
cartilage, debridement of the lesion, and curettage of the lesion to the
level of bleeding subchondral bone through open arthrotomy or arthro-
scopic visualization.
7
, 15, 31, 41, 45, 90 Treatment is best performed before the
development of secondary osteoarthritic changes.
86
It is important to
treat these dogs as soon after diagnosis as possible, as the prognosis
worsens as the age of the animal increases.
86
It is important to communi-
cate to owners that the osteoarthritis is going to progress and that weight
management and nonsurgical therapy are going to be necessary as the
animal ages. Grondalen
45
reported better outcomes in patients with
elbow osteochondrosis than with FMCP. 01sson
80
reported contradictory
findings. Long-term studies investigating effects on function and studies
comparing the results of arthroscopic versus open procedures have not
been reported.
Prevention of elbow OC is similar to that for all developmental
disorders of the forelimb. Appropriate nutrition and breeding programs
are vital to minimizing the occurrence of these disorders.
33
,94 Breeding
of affected dogs should be discouraged.
FMCP of the ulna also occurs most commonly in large and giant
breeds of dogs, with Bernese Mountain Dogs, Rottweilers, Retrievers,
Newfoundlands, German Shepherd Dogs, and Chow Chows most com-
monly affected.
16
, 31. 37. 49. 66 FMCP more commonly affects male dogs and
r
FORELIMB LAMENESS IN THE YOUNG PATIENT 67
is typically bilateraL 16,66 The onset of clinical signs is reported to occur
most often between 4 and 7 months of age, but dogs often are not
presented to the veterinarian until they are 7 to 9 months of age or later.
The etiopathogenesis of FMCP is extremely controversial and poorly
understood.
46
, 49, 79-81. 120, 121 It is likely that the disease is multifactorial
in nature, with various causes contributing to a common phenotypic
manifestation. Genetics almost certainly plays a role in most cases, and
affected dogs should not be bred. Nutrition and growth rate have the
potential to at least exacerbate this developmental disorder and should
be addressed in puppies of large and giant breeds.
94
The possibility of
FMCP lesions being the result of OC has been proposed.
46
, 49, 80, 81 Others
suggest that FMCP is caused by asynchronous growth of the radius and
ulna or humerus and ulna.
46
,49, 79, 120, 121 Abnormalities in extracellular
matrix components are also under investigation as potential factors in
the development of this disorder (DT Crouch, DVM, et aI, unpublished
data, 2000).
Physical examination of patients with FMCP is similar to that de-
scribed for elbow Oc. A weight-bearing lameness of variable severity in
one or both forelimbs sometimes exacerbated by exercise or minor
trauma is often present. Flexion and extension of the elbow elicits signs
of pain. Joint capsule distention, periarticular fibrosis, and muscle atro-
phy may be present. A "head bob," shortened stride, and bow-legged
stance may also be noted. A complete orthopedic examination to rule
out other forelimb abnormalities is imperative.
Determination of a definitive diagnosis of FMCP is sometimes possi-
ble from radiographic examination.
9
. 10, 19, 46. 61. 80, 92, 123 Sedation with anal-
gesia should be used for positioning of these patients for radiography,
Radiographic views that should be obtained include a craniocaudal
view, an extended mediolateral view, and a maximally flexed mediolat-
eral view. Various oblique views have also been reported to be helpfuL
1
<\.
61,123 The fragmented portion of the ulna may be radiographically evident
in some cases, Alternatively, radiographic findings may consist only of
loss of normal radiographiC detail in the anatomic location of the medial
coronoid process and secondary changes of elbow osteoarthritis.
9
, 10. 19. <\6.
80. 92 The secondary changes associated with osteoarthritis, including
periosteal proliferation on the dorsal anconeal ridge, proximal radius,
.and medial aspects of the humerus and ulna along with sclerosis of the
trochlear notch, are the most consistent radiographic findings for FMCp' 9,
10. 19, 66, 80. 92. 123 These secondary changes are common to all causes of
elbow dysplasia, however. If definitive diagnOSiS cannot be made on
radiographic findings alone, more advanced imaging techniques, includ-
ing contrast arthrography, linear tomography, computed tomography,
magnetic resonance imaging, or exploratory arthroscopy, may be re-
quired for definitive diagnosis.
16
, 19.36.61, 105. 106 A study comparing the
effectiveness of radiography, xeroradiography, linear tomography,
arthrography, and computed tomography reported computed tomogra-
phy as having the highest accuracy and sensitivity for diagnosis of
FMCp'19 The author prefers exploratory arthroscopy for definitive diag-
68 COOK
nosis of causes of elbow dysplasia that cannot be made on routine
radiographic examination (Fig. 2).
Treatment of FMCP is as controversial (if not more) as its etiopatho-
genesis. Nonsurgical and surgical therapies have been recommended.*
It should be noted that no study has shown definitive long-term benefits
of surgical therapy, nor has any study reported the long-term results
comparing various surgical teclmiques, including open and arthroscopic
approaches. In addition, the author believes strongly that nonsurgical
aspects of therapy are a vital part of a comprehensive treatment plan for
every case of FMCP and should be discussed thoroughly with the owner
after diagnosis.
Nonsurgical therapy involves weight management, activity control,
and medical therapy. Keeping the dog at an ideal lean weight is vital for
successful management. Activities should be geared toward minimizing
concussive activities and maximizing activities that the dog can perform
without marked pain or lameness. Medical therapy should be used to
augment control of the clinical signs associated with FMCP.
Surgical therapy is aimed at removing abnormal cartilage and bone
or correction of articular incongruity causing osteochondral damage in
an attempt to relieve pain and allow fibrocartilage repair with resultant
abatement of clinical signs?' 15, 16, 31, 45, 53, 66, 76, 90, 92, 110, 123 Surgical treatment
options include open arthrotomy or arthroscopy followed by removal of
abnormal cartilage and bone with debridement and curettage of the
lesion, The author prefers arthroscopic treatment because of a perceived
advantage in accuracy and completeness of joint assessment and de-
bridement, decreased morbidity with faster recovery times, and de-
creased length of hospital stays with higher owner satisfaction, These
proposed advantages have not been proven in cases of canine FMCP,
*References 4, 7, 11, 15, 16, 31, 41, 43, 45, 49, 53, 65, 66,70, 76, 90, 92, 1l0, 120, 121, 123.
Figure 2. Arthroscopic views of the elbow of a dog with concurrent osteochondrosis (0) of
the medial humeral condyle and fragmented medial coronoid process (F) of the ulna
(U) demonstrating the appearance before (A) and after (B) fragment removal and initial
debridement and curettage. The head of the radius (R) is noted in the far field of view.
FORELIMB LAMENESS IN THE YOUNG PATIENT 69
however, and surgeon preference remains the primary criterion in de-
termining surgical treatment option. At our institution, we recommend
surgery for FMCP in dogs that are under 12 months of age with clinical
or radiographic signs attributable to elbow dysplasia. We also perform
surgery in dogs up to 24 months of age with large radiographically
visible FMCP and clinical signs attributable to elbow pathologic changes.
Dogs with severe radiographic osteoarthritis already present are not
considered appropriate surgical candidates by the author.
No surgical therapy of FMCP is curative in that the secondary
osteoarthritis still progresses. A comprehensive treatment plan should
thus be adopted by the owners. The prognosis for FMCP varies widely
with the age of the dog, severity of clinical signs, severity of osteoarthri-
tis, intended function of the dog, and treatment method. Prevention is
aimed at appropriate nutritional management of growing puppies and
breeding programs based on radiographic phenotype.
33
,94
DAP is reported in large and giant breeds of dogs, with the highest
incidence reported in the German Shepherd Dog.23, 101, 102, 108, 120 Male dogs
are affected more commonly than female dogs,lOl, 102, 108 The disorder is
reported to be. bilateral in 20% to 35% of affected dogs. 100, 101 Definitive
diagnosis of DAP should not be made before the dog is 20 weeks of
age, as bony union between the anconeal ossification center and ulna
normally occurs when dogs are between 16 and 20 weeks of age.
37
, 100, 101
Most dogs are presented for lameness because of DAP when they are
between 5 and 12 months of age.
The etiopathogenesis of DAP remains unknown and controversial.
Like other components of elbow dysplasia, genetics, nutrition, growth
rate, and trauma have been implicated.
37
, 101, 102, 108, 121 Most investigators
agree on a genetic component to the disorder and recommend that
affected dogs not be bred.
37
, 101, 102, 108, 121 Some argue that DAP follows a
disease course similar to that of Oc, although others are adamant that
cases of DAP are related to asynchronous growthY, 100-102. 108, 121 As is
the case with other causes of elbow dysplasia, multifactorial causes
are likely.
Diagnosis is based on radiographs obtained after the dog is 20
weeks of age.
101
, 102, 108 Sedation with analgesia should be used for radio-
graphic examination. A maximally flexed mediolateral radiographic
. view is imperative for delineating the DAP from the ossification center
of the medial epicondyle. Both elbows should be radiographed in all
cases. The secondary changes of osteoarthritis in the elbow may be
evident and can be important in determining prognosis:
Surgical treatment is recommended in cases of DAp'sl, 88, 100-102 Sur-
gery is only part of a comprehensive treatment plan, including weight
management, activity control, and appropriate medical therapy, how-
ever. Surgical teclul.iques described have been aimed at either removal
of the DAP or attempts at uniting the DAP with the ulna. 51, 88, 100-102
Surgical removal by caudolateral arthrotomy typically provides accept-
able long-term function and joint stability, with minimal complications
for nonathletic dogs.
JOO
, 101 At our instition, we have also performed
removal of the DAP arthroscopically. Surgical attachment procedures
70 COOK
have included lag screw fixation of the UAP or dynamic ulnar osteotomy
to allow for attachment over time.
51
. 88. 102 Good long-term results have
been reported using both techniques. Currently, the author advocates
dynamic ulnar osteotomy in dogs with clinical signs attributable to UAP
as a first line of therapy. Removal of the UAP is performed by arthrot-
omy or arthroscopy if attachment of the UAP has not occurred 12 to 18
weeks after ulnar osteotomy with persistent clinical signs. The prognosis
for dogs with UAP is generally good provided that treatment is initiated
before severe osteoarthritis is present.
Asynchronous growth of the radius and ulna likely occurs at a
microscopic level in all dogs. Compensation quickly occurs by a variety
of mechanisms, providing a macroscopic synchrony that ensures appro-
priate joint congruity, bone lengtJ;:t, alignment, and function.20. 24. 64. 79
Skeletal growth is typically completed in most breeds by 12 months of
age.
24
. 104 Problems related to asynchronous growth are thus generally
noted within the first 12 to 18 months. As discussed previously, asyn-
chronous growth has been hypothesized to be primarily responsible for
UAP and FMCP. Asynchronous growth is a definitive cause of angular
limb deformity and joint incongruity.20. 32. 40.64.77.79.91 Causes of asynchro-
nous growth include trauma, hypertrophic osteodystrophy, septic phy-
sitis, genetic disorders, and idiopathic causes.
40
. 64. 77.79. 91 Trauma in the
form of concussive injury is the most common cause of asynchronous
growth.
24
The pathologic changes are typically in the form of a Salter-
Harris type V fracture to the growth plate, which causes biomechanical
or ischemic damage to the germinal chondrocytes of the physis.
24
This
injury may not be clinically or radiographically apparent until the se-
quelae of the pathologic changes are manifested. It is thus imperative to
counsel owners of growing dogs about the possibility of physeal trauma
after any concussive injury. Owners should carefully monitor these dogs
for evidence of clinical dysfunction or angular limb deformity, and
radiographs of both forelimbs should be obtained in any dog that is
demonstrating problems after concussive injury.
The two major effects of asynchronous growth resulting in clinical
dysfunction are joint incongruity and abnormal bone modeling.
24
Joint
incongruity is a major problem associated with asynchronous growth
and requires immediate attention. The subluxation and abnormal bio-
mechanics that occur in the elbow and carpus result in pain, lameness,
and osteoarthritis.20. 24. 32. 40. 64. 79.91 Restoring the congruity and alignment
of the joints is critical for providing a good long-term outcome in
affected dogs. Abnormal bone modeling mayor may not manifest in
clinical problems. Radioulnar bowing and rotation can occur without
significant malalignment or incongruity of the elbow and carpus as
evidenced by many of the chondrodystrophic breeds. Bowing or rotation
resulting in joint alterations should be addressed as soon as possible
to avoid clinical dysfunction and circumvent or diminish secondary
osteoarthritis.20. 24. 32. 40. 79. 91
Asynchronous radioulnar growth can occur with injury or insult to
any of the physes of the radius or ulna. Clinical abnormalities caused
FORELIMB LAMENESS IN THE YOUNG PATIENT 71
by proximal ulnar physeal pathologic changes are rare, as this physis
contributes little, if any, to the ulnar length distal to the elbow joint.
24
25.
79.104 The clinical and radiographic findings as well as treatment options
and prognoses for each of the common syndromes associated with
asynchronous growth of the radius and ulna as a result of trauma to the
proximal radial physis, distal radial physis, and distal ulnar physis have
been well described.
20
. 24. 32. 40. 64. 79. 91
Ununited epicondyles have been reported and included in the el-
bow dysplasia syndrome by some authors. 6. 81. 86 The etiopathogenesis is
unknown, however, and may be an exclusively traumatic event.
63
Lack
of union or avulsion of the medial and lateral epicondyles has been
reported, with the medial epicondyle being affected far more com-
monly.6. 63. 81. 86. 124 Typically, this disorder is seen in 4- to 6-month-old
large-breed dogs. Affected dogs may be asymptomatic or have a mild
intermittent weight-bearing lameness with pain and swelling over the
area of the lesion. The disorder is often bilateral. Concurrent elbow OC
or FMCP may be present.
86
Maximally flexed lateral and craniocaudal
radiographic views are the most diagnostic. Radiographic examination
reveals evidence of nonunion or avulsion of a portion of the epicondyle
that is of bone density and located medial (or lateral) to the joint space
or caudal to the remaining epicondyle.
86
Surgery is recommended in
dogs with lameness that can be attributed to ununited epicondyle.
Removal of all bony fragments by sharp dissection is recommended and
is typically successful in patients with no other elbow pathologic changes
present.
86
Retained cartilaginous cores are seen in the distal ulna of large and
giant breeds of dogs as a result of delayed endochondral ossification of
an area of the distal ulnar metaphysis. 56. 95 The abnormal endochondral
ossification results in retention of hypertrophied chondrocytes and their
extracellular matrix rather than in production of bony trabeculae. The
cause of this syndrome is unknown but has been speculated to involve
the same multifactorial processes as are associated with OC.
56
.
95
The
abnormal ossification process can result in slowed distal ulnar growth
with resultant joint and bone abnormalities associated with asynchro-
nous radioulnar growth.
95
Affected dogs are typically presented between 4 and 8 months of
age for a bilateral weight-bearing lameness with associated distal ulnar
pain and swelling. Angular and rotational deformities associated with
retarded distal ulnar physeal growth may be present. Diagnosis is made
based on clinical signs and radiographic findings of a radiolucent defect
extending from the distal ulnar physis and tapering proximally. 56. 95
Radiographic examination should be performed to incorporate the elbow
and carpal joints in the mediolateral and craniocaudal views so as
to determine joint alignment and congruity. Many dogs with retained
cartilaginous cores are minimally affected and require only careful moni-
toring to assess for incongruity, malalignment, and angulation. Clinically
affected dogs with manifestations of retarded distal ulnar physeal
growth that are still skeletally immature may benefit from a partial distal
72 COOK
ulnar ostectomy. Clinically affected skeletally mature dogs may require
radial and ulnar osteotomies with subsequent correction of malalign-
ment, angulation, and incongruity. The prognosis varies with the age of
the dog, severity of the pathologic changes, secondary changes present,
treatment employed, and intended function of the dog.
Carpal laxity syndrome has been reported in young Doberman
Pinschers, German Shepherd Dogs, and Great Danes.
2
,98 The disorder
typically occurs bilaterally in 8- to 16-week-old puppies and results in a
palmigrade stance, increased laxity of the carpal joints, and
during weight bearing. The cause is unknown, but genetIc and nutn-
tional causes have been proposed.
2
, 98 No evidence of a traumatic cause
has been reported. The treatment for this syndrome is to provide con-
trolled exercise on level surfaces "l(Vith good footing. Protection of the
palmar surfaces of the carpus may be necessary to prevent soft tissue
trauma, but supporting bandages or splints are contraindicated. Most
dogs respond well to therapy in 2 to 6 weeks, with no apparent long-
term abnormalities,
TRAUMATIC CAUSES
Trauma to the young dog can often result in lameness and dysfunc-
tion requiring treatment. Fractures, luxations, tendon and ligament
sprains and strains, and muscle damage occur frequently in the young
canine patient. Early and accurate diagnosis and treatment are VItal for
long-term success.
Fractures of all types can occur in the forelimb of young dogs.
Scapular, humeral, radial, ulnar, carpal, metacarpal, and phalangeal frac-
tures are all well described in the literature.
28
, 82, 85, 113 b:litial management
of these fractures is critical to success, especially in cases of open frac-
tures, Complete patient assessment and stabilization, wound manage-
ment, appropriate fracture stabilization or management, and analgesic
therapy are important in all cases. It is important to note that most dogs
with forelimb fractures have concurrent trauma that may be as or more
Significant than the fractured bone.
28
, 107, 109
Salter-Harris fractures are unique to young patients and are ad-
dressed here to highlight the salient points of diagnosis, management,
and prognosis. Salter-Harris fractures are those that involve an open
physis and thus occur in skeletally immature Sa.lter an?
have classified physeal fractures based on theIr anatomIC confIguratIOn.
The classification scheme initially outlined was also designed to incorpo-
rate prognostic information for each fracture type, but this has not been
verified in dogs. Figure 3 provides a description of each fracture type
along with the most common location(s) of each type in the forelimb
of dogs.
Fractures in immature dogs often involve the physis because of the
biomechanical inferiority of the cartilaginous growth plate in comparison
to adjacent bone and ligaments. 55, 97 Physeal fractures have tremendous
FORELIMB LAMENESS IN THE YOUNG PATIENT 73
Salter-Harris
Common location(s)
Classification Anatomical Description Illustration in forelimb
Type I Fracture through the physis
Q2;
Proximal humerus
only with separation between Distal radius
the epiphysis and metaphysis
rIl
(
Type II Fracture through the physis
!l
Proximal humerus
with extension into a portion of Distal humerus
the metaphysis Distal radius
cf11
Type II I Fracture through the physis Distal humerus
with extension into a portion of
the epiphysis (articular)
OlP
Type IV Fracture through a portion of
!J6
Distal humerus
the metaphYSiS, across the
physis, and through a portion
of the epiphysis (articular)
Type V Parti al or complete crushing or Distal ulna
compression injury of the Distal radius
physis
. Figure 3. Description of physeal fractures causing forelimb lameness in young dogs.
potential for achieving bony union; however, the rapid healing that
occurs mayor may not allow for continued function of the physis in
skeletal growth. The primary determinant in preserving function is the
viability of germinal cells in the proliferative zone of the growth plate.
97
These cells can be injured during the initial trauma, during subsequent
trauma before definitive surgical stabilization, during surgical manipula-
tion and stabilization, or in the postoperative period. Because the latter
three can be at least partially controlled by the veterinarian, it is vital to
be attentive to these issues so as to maximize the prognosis in these
74 COOK
patients. Immediate evaluation of these patients with complete and
accurate assessment is imperative. Young dogs subjected to trauma
should have radiographic examination of the affected limb performed
in all cases. Comparison with similar radiographic views of the contralat-
eral limb is often helpful for determining subtle physeal abnormalities.
Salter-Harris type V fractures are rarely diagnosed by clinical and radio-
graphic examination, but if suspected, they should be monitored closely
with re-examination of the dog in 2 to 3 weeks to assess for signs of
asynchronous growth. For physeal fractures involving the elbow or
carpus, the affected limb should be immediately stabilized with a large
soft-padded bandage extending as proximal on the brachium as possible.
For those involving the proximal humerus, a spica splint can be placed.
Adequate stabilization of these fractures with a spica splint is difficult
to achieve, however, and strict cage rest with analgesics is the standard
of care at our hospital.
Dogs with physeal fractures should receive surgical reduction and
stabilization of the fracture as soon as possible. Most surgeons recom-
mend surgical repair of physeal fractures within the first 72 hours to
allow for success in reduction of the fracture with minimal morbidity.B,
10, 2B, 55, 67. 68 Open or closed reduction techniques can be used effectively. 10,
27, 67, 68 Internal fixation with small and smooth intramedullary pins or
Kirschner wires placed perpendicular or at an angle to the physis is
recommended for stabilization (Fig. 4). Physeal fractures involving the
articular surface require anatomic reduction, with rigid compressing
stabilization across the epiphyseal fracture line for the best long-term
outcome. Postoperative management should include analgesics, carefully
restricted exercise, physical rehabilitation addressed at preserving joint
and muscle function, a recheck examination at 2 to 4 weeks to assess
healing and function, and further recheck examinations as indicated
until the dog achieves skeletal maturity to monitor joint congruity and
function as well as limb alignment and length.
Luxations and subluxations can occur in the forelimb of young
dogs. All the diarthrodial joints of the forelimb can be affected. These
injuries occur in the same manner as in older dogs, and diagnosis,
treatment options, and prognoses are similar. The reader is referred to
the article on forelimb lameness in the adult patient for complete discus-
sion of these injuries. It is important to remember that physeal injury is
likely in young patients sustaining trauma that results in luxation or
subluxation. Owners of these dogs should be counseled concerning the
likelihood of these injuries and their possible sequelae.
Similarly, tendon and ligament sprains and strains certainly can and
do occur in young dogs. It is imperative to rule out all other causes
of lameness in these patients to prevent misdiagnosis and subsequent
irreversible pathologic changes caused by more common causes of lame-
ness in the young dog.
Diagnosis of muscle damage follows the same protocol as for luxa-
tions, subluxations, sprains, and strains. These injuries do occur, but
complete assessment, including radiographic examination, must rule out
FORELIMB LAMENESS IN THE YOUNG PATIENT 75
A
Figure 4. Intraoperative fluoroscopic views of the forelimb of a dog with a Salter Harris
type I fracture (arrows) of the distal radius before (A) and after (B) closed reduction with
internal fixation.
all other causes before definitive diagnosis of isolated muscle injury can
be made.
IDIOPATHIC CAUSES
Two common diagnoses for forelimb lameness in the young canine
patient are panosteitis and hypertrophic osteodystrophy. Both of these
disorders have unknown etiopathogeneses at this time.
. Panosteitis is a common condition causing lameness in young dogs.
The disorder can affect any and all of the long bones. It has been
reported in a variety of breeds, with the German Shepherd Dog and
Basset Hound being the most common.
5
14, 74 Male dogs are affected
more often than female dogs. As stated, it has no known cause but has
been hypothesized to be the result of viral or bacterial infection, stress,
metabolic disease, vascular abnormalities, allergy, immune-mediated dis-
orders, parasitism, and genetic causes.
s
, 14, 74 The disease is a primary
degeneration of fatty bone marrow with secondary endosteal and perios-
teal proliferation.11
6
These events are typically cyclic in nature, with new
bone resorption and bone marrow restoration within 60 to 90 days
after onset.
1l6
76 COOK
Physical examination reveals an acute, often severe, lameness of one
or more limbs in an otherwise healthy dog. The lameness often shifts
from limb to limb. Typically, dogs are presented during their first 2 years
of life, but dogs as old as 5 years of age can be affected.
14
Palpation of
the long bones of the affected limb(s) often elicits signs of pain. It is
important to carefully examine the joints of dogs with panosteitis, as
this disorder can be seen concurrently with many of the developmental
diseases of young dogs.
Radiographic examination usually provides a definitive diagnosis.
Sedation with analgesia should be used for radiographic examination of
affected dogs. Three stages of the disease have been delineated based
on radiographic findings.
14
The early stage is characterized by loss of
normal trabecular patterns and medullary-cortical contrast at the proxi-
mal and distal ends of the affected diaphysis. A few intramedullary
granular densities may also be seen. Radiographs taken during the
middle stage of the disease typically reveal patchy, mottled, sclerotic
densities of various size and extent, which are predominantly seen in
the area of nutrient foramens. An increase in density and roughening of
the periosteum may also be noted. The late stage is characterized by
recovery, with a decrease in the number of granular densities, return to
a normal medullary appearance, and cortical and trabecular remodeling.
Other clinical or laboratory abnormalities, including pyrexia, an-
orexia, muscle atrophy, and eosinophilia, have also been reported in
dogs with panosteitis but are not consistent or unique diagnostic find-
ings.5, 14, 74
Panosteitis is a self-limiting disease with most affected dogs demon-
strating complete resolution by 18 to 20 months of age.
5
, 14, 74,116 Treatment
is aimed at supportive care for patients with pyrexia or anorexia and
analgesic therapy for clinical signs of pain. Client education is important
to inform owners of the likelihood of recurrence before the dog reaches
2 years of age. The prognosis is excellent in most cases, as secondary
manifestations of the disease are rare.
5
, 14,74,116
Hypertrophic osteodystrophy (HOD) is an uncommon idiopathic
disease affecting young large and giant breeds of dogs.
1
, 43, 75, 119 Male
dogs may be more commonly affected than female dogs, but some
investigators report no gender predilection.
1
, 47, 75, 119 The clinical manifes-
tations of HOD are typically noted in dogs between 2 and 8 months of
age. Causes of HOD that have been proposed include viral and bacterial
infection, hypovitaminosis C, oversupplementation of vitamins and min-
erals, vascular abnormalities, and genetic causes.
1
, 47, 75, lJ9 HOD results
from an idiopathic abnormality in endochondral ossification, causing
subsequent inflammation, hemorrhage, necrosis, and microfracture of
metaphyseal bone subjacent to the affected physis. A secondary prolifer-
ative periosteal response may ensue.
Physical examination of affected puppies typically reveals an acute
lameness of variable severity ranging from mild to non-weight-bearing.
The metaphyseal areas of affected long bones, most often the distal
radius and ulna, are swollen and painful. The lesions are usually bilateral
FORELIMB LAMENESS IN THE YOUNG PATIENT 77
and symmetric. It is important to note that many of these patients can
be systemically affected with marked pyrexia, anorexia, depression, and
weight loss. Addressing the overall status of the patient must be the
first concern.
Definitive diagnosis is based on radiographic findings of an irregu-
lar radiolucent line (" double physeal line"), soft tissue swelling, and
periosteal proliferation in the metaphyseal region of affected bones.1' 47,
75, 119 As stated previously, other juvenile orthopedic disorders can be
seen concurrently and should be investigated in dogs with HOD.
H<?D i ~ another self-limiting disease, with most dogs experiencing
resolutlOn ill days to months. Treatment is similar to that described
for panosteitis: fluid, electrolyte, and nutritional imbalance correction;
analgesic therapy; and supportive care. The prognosis is excellent in
patients with uncomplicated HOD. In more severe cases, the prognosis
is guarded because of complications associated with the systemic illness,
secondary bacterial infections, and effects on physeal growth and normal
skeletal development.
INFECTIOUS CAUSES
Infectious agents are not common causes of forelimb lameness in
young dogs. Septic arthritis and osteomyelitis can occur as the result of
septicemia in neonatal puppies, but they are extremely uncommon. The
overall health status of the patient is the primary concern in these
cases and should be immediately addressed. Forelimb lameness may be
present but is of secondary importance. The prognosis in these puppies
is guarded at best.
Septic arthritis and osteomyelitis can also occur as the result of
penetrating wounds or trauma, including surgical wounds. Rickettsial
arthritides causing forelimb lameness can occur in young dogs; however,
these problems are more commonly seen in older patients. These disor-
ders are discussed in the article on forelimb lameness in the adult pa-
hent.
NUTRITIONAL AND METABOLIC CAUSES
The importance and effects of nutrition on developmental skeletal
disease of dogs have already been discussed. Although many other
skeletal abnormalities can occur secondary to nutritional and metabolic
abnormalities in the dog, they are extremely rare. Appropriate nutrition
by feeding of commercially available high-quality pet foods has nearly
eradicated these problems in young dogs. Hyperparathyroidism second-
ary to nutritionally induced hypocalcemia, hyperphosphatemia, or inad-
equate amounts of vitamin D can result in osteopenia, skeletal deformi-
ties, and pathologic fractures. This disorder most often occurs as the
result of feeding young puppies a diet composed primarily of meat.
78 COOK
NEOPLASIA
Neoplasia causing lameness occurs rarely in canine patients under
1 year of age. Osteosarcoma has been reported in dogs as young 6
months of age, however and should be kept in mind when evaluatmg
these patients. Forelimb neoplasia is discussed in detail in the article on
forelimb lameness in the adult patient.
SUMMARY
Forelimb lameness is a common problem in young dogs and can be
caused by a wide variety of problems. Accurate
diagnosis and treatment must be provided for DIfferenhal
diagnoses for forelimb lameness in the young fall mto the catego-
ries of congenital abnormalities; dIsorders; and
infectious, nutritional, metabolic, and neoplastic causes. The etiopatho-
geneses of many of these disorders are still treatment
options and prognoses U:ntil definihve causes are
determined, it is the responsIbility of vetermanans to address the factors
that contribute to the development and progression of these disorders.
These areas primarily involve weight and nutritional management as
well as breeding programs.
References
1. Alexander JW: Hypertrophic osteodystrophy. Canine Pract 5:48, 1978
2. Alexander JW, Earley TD: A carpal laxity syndrome in young dogs. J Vet Orthop
3:22,1984
3. Alonso RA, Hernandez A, Diaz P, et al: An autosomal recessive form of hemimelia
in dogs. Vet Rec 110:128, 1982 . .
4. Anderson SM, Lippincott CL, Schulman AJ: Longttudmal myotomy of the flexor
carpii radialis: A new approach to the medial aspect of the elbow Jomt. J Am Anim
Hosp Assoc 25:499, 1989 . .
5. Barrett RB, Schall WD, Lewis RE: Clinical and radiographic features of canme eosmo-
philic panosteitis. J Am Anim Hosp Assoc 4:94, 1968 .
6. Bennett D, May C: Joint diseases of dogs and cats. In Ettinger SJ, Feldman EC (eds):
Textbook of Veterinary Internal Medicine, ed 4. Philadelphia, WB Saunders, 1995,
pp 2032-2077 .
7. Bennett D, Duff RI, Kene RO, et al: Osteochondritis dissecans and fragmentation of
the coronoid process in the elbow joint of the dog. Vet Rec 109:329, 1981
8. Berg RJ, Egger EL, Konde V, et al: Evaluation of prognostic factors for growth
following distal femoral physeal injuries in 17 dogs. Vet Surg 13:172, 1984.
9. Berry CR: Evaluation of the canine elbow for fragtnented medial coronOld process.
Vet Radiol Ultrasound 33:273, 1992
10. Berzon JL: The classification and management of epiphyseal plate fractures. J Am
Anim Hosp Assoc 16:651, 1980
11. Berzon JL, Quick CB: Fragtnented coronoid process: Anatomical, clinical, and radio-
graphic considerations with case analysis. J Am Anim Hosp Assoc 16:241, 1980
12. Bingel SA, Riser WHo Congenital elbow luxation in the dog. J Small Anim Pract
18:445, 1977
FORELIMB LAMENESS IN THE YOUNG PATIENT 79
13. Birkeland R: Osteochondritis dissecans in the humeral head of the dog. Nord Vet
Med 19:291, 1967
14. Bohning R, Suter P, Hohn RB, et al: Clinical and radiographic survey of canine
panosteitis. JAVMA 156:870, 1970
15. Bouck GR, Miller CW, Taves CL: A comparison of surgical and medical treatment of
fragmented coronoid process and osteochondritis dissecans of the canine elbow. Vet
Comp Orthop Traumatal 8:177, 1995
16. Boulay JP: Fragmented medial coronoid process of the ulna of the dog. Vet Clin
North Am Small Anim Pract 28:51, 1998
17. Campbell BG, Wootton JA, Krook L, et al: Clinical signs and diagnosis of osteogenesis
imperfecta in three dogs. JAVMA 211 :183, 1997
18. Campbell JR: Congenital luxation of the elbow in the dog. Vet Annu 19:229, 1979
19. Carpenter LG, Schwarz PD, Lowry TE, et al: Comparison of radiologic imaging
techniques for diagnosis of fragmented medial coronoid process of the cubital joint
in dogs. JAVMA 203:78, 1993 .
20. Carrig CB, Morgan TP, Pool RR: Effects of asynchronous growth of the radius and
ulna of the canine elbow joint following experimental retardation of longitudinal
growth of the ulna. J Am Anim Hosp Assoc 11:560, 1975
21. Carrig CB, Wortman JA, Morris EL, et al: Ectrodactyly (split-hand deformity) in the
dog. Vet Radiol 22:123, 1981
22. Carrig CB, MacMillan A, Brundage S, et al: Retinal dysplasia associated with skeletal
abnormalities in Labrador retrievers. JAVMA 170:49, 1977
23. Cawley AJ, Ar.chibald J: Ununited anconeal process of the dog. JAVMA 134:454, 1959
24. Chambers IN: Developmental and congenital problems of the antebrachium and
adjacent joints. In Bojrab MJ (ed): Disease Mechanisms in Small Animal Surgery, ed
2. Philadelphia, Lea & Febiger, 1993, pp 834--840
25. Chapman WL: Appearance of ossification centers and epiphyseal closures as deter-
mined by radiographic techniques. JAVMA 147:138, 1965
26. Cook JL, Jordan RC: What is your diagnosis? (Skeletal and retinal dysplasia in a
Labrador Retriever). JAVMA 210:329, 1997
27. Cook JL, Tomlinson JL, Reed AL: Fluoroscopically guided closed reduction and
internal fixation of fractures of the lateral portion of the humeral condyle: Prospective
clinical study of the technique and results in ten dogs. Vet Surg 28:315, 1999
28. Cook JL, Cook CR, Tomlinson JL, et al: Scapular fractures in dogs: Epidemiology,
classification, and concurrent injuries in 105 cases (1988-1994) . J Am Anim Hosp
Assoc 33:528, 1997
29. Craig PH, Riser WHo Osteochondritis dissecans in the proximal humerus of the dog.
J Am Vet Radiol Soc 6:40, 1965
30. DeAngelis MP, Schwartz A: Surgical correction of cranial dislocation of the scapulo-
humeral joint in a dog. JAVMA 156:435, 1970
31. Denny HR, Gibbs C: The surgical treatment of osteochondritis dissecans and ununited
coronoid process in the canine elbow joint. J Small Arum Pract 21:323, 1980
32. Egger EL, Stoll SG: Ulnar styloid transposition as an experimental treatment for
premature closure of the distal ulnar physis. J Am Anim Hosp Assoc 14:690, 1978
33. Elbow Regishy Columbia, MO, Orthopedic Foundation for Animals, 1996
34. Engen MH: Surgical treatment of shoulder luxations. In Bojrab MJ (ed) : Current
Techniques in Small Animal Surgery, ed 4. Baltimore, Williams & Wilkins, 1998,
pp 1075-1079
35. Flo GL, DeCamp CEo Surgical correction of congenital radialluxati<;>ns. In Proceedings
of the 17th Annual Conference of the Veterinary Orthopedic Society, Jackson Hole,
Wyoming, 1990
36. Fox SM, Roberts R: Linear tomography in diagnosing fragmented coronoid processes
in carline elbows. Compend Contin Educ Pract Vet 9:60,1987
37. Fox SM, Bloomberg MS, Bright RM: Developmental anomalies of the canine elbow. J
Am Anim Hosp Assoc 19:605, 1983
38. Gahring DR: A modified caudal approach to the canine shoulder joint. J Am Anim
Hosp Assoc 21 :613, 1985
39. Gasper PW, Thrall MA, Wegner DW, et al: Correction of feline arylsulphatase B
80 COOK
deficiency (mucopolysaccharidosis VI) by bone marrow transplantation. Nature
12:467, 1984
40. Gilson SD, Piermattei SL, Schwarz PD: Treatment of humeroulnar subluxation with
a dynamic proximal ulnar osteotomy. A review of 13 cases. Vet Surg 18:114, 1989
41. Goring RL, Bloomberg MS: Selected developmental abnormalitIes of the carune elbow:
Radiographic evaluation and surgical management. Compend Contin Educ Pract Vet
5:178, 1983
42. Griffiths R: Osteochondritis dissecans of the canine shoulder. JAVMA 53:1733, 1968
43. Grondalen J: Arthrosis with special reference to the elbow joint of young rapidly
growing dogs. I. Nord Vet Med 31:62, 1979 . . .
44. Grondalen J: Arthrosis with special reference to the elbow Jomt of young rapIdly
growing dogs. II. Occurrence, clinical and radiographic findings. Nord Vet Med
31:69, 1979
45. Grondalen J: Arthrosis with special reference to the elbow joint of young rapidly
growing dogs. m. Ununited medial coronoid process of the u l n ~ and osteochondritis
dissecans of the humeral condyle. Surgical procedure for correctIon and postoperatIve
investigation. Nord Vet Med 34:520, 1979 . . .
46. Grondalen J: Arthrosis with special reference to the elbow Jomt of young rap,dly
growing dogs. VI. Interrelation between clinical, radiographical, and pathoanatomical
findings . Nord Vet Med 34:65, 1982
47. Grondalen J: Metaphyseal osteopathy (hypertrophic osteodystrophy) in growing dogs.
A clinical study. J Small Anim Pract 17:721, 1976
48. Grondalen J, Rorvik AM: Arthrosis with special reference to the elbow joint of young
rapidly growing dogs. IV. Ununited anconeal process. A follow up investigation of
operated dogs. Nord Vet Med 35:212, 1980
49. Grondalen J, Grondalen T: Arthrosis with special reference to the elbow joint of
young rapidly growing dogs. V. A pathoanatomical investigation. Nord Vet Med
33:1, 1981
50. Haskins ME, Otis EJ, Hayden JE, et al: Hepatic storage of glycosaminoglycans in feline
and canine models of mucopolysaccharidoses I, VI, and VII. Vet Pathol 29:112, 1992
51. Herron MR: Ununited anconeal process in the dog. Vet Clin North Am Small Anim
Pract 1:417, 1971
52. Hohn RB, Rosen H, Bohning RH, et ale Surgical stabilization of recurrent shoulder
luxation. Vet Clin North Am Small Arlim Pract 1:537, 1971
53. Huibregste BA, Johnson AL, Muhlbauer MC, et al: The effect of treatment of frag-
mented coronoid process on the development of osteoarthritis of the elbow. J Am
Arlim Hosp Assoc 30:190, 1994
54. Jezyk PF: Constitutional disorders of the skeleton in dogs and cats. In Newton CD,
Nunamaker DM (eds): Textbook of Small Animal Orthopaedics. Philadelphia, JB
Lippincott, 1985 .
55. Jolmson JM, Johnson AL, Eurell JC: Histologic appearance of naturally occurrmg
canine physeal fractures. Vet Surg 23:81, 1994
56. Johnson KA: Retardation of endochondral ossification at the distal ulnar growth plate
in dogs. Aust Vet 57:474, 1981
57. Johnston SA: Osteochondritis dissecans of the humeral head. Vet Clin North Am
Small Anim Pract 28:33, 1998
58. Jones DGC, Vaughan LC: The surgical treatment of osteochondritis dissecans of the
humeral head of dogs. J Small Anim Pract 11:803, 1970
59. Keller WG, Chambers IN: Antebrachial metacarpal arthrodesis for fusion of deranged
carpal joints in two dogs. JAVMA 195:1382, 1989
60. Kene ROC, Lee R, Bennett D: The radiographic features of congenital elbow luxation/
subluxation in the dog. J Small Anim Pract 23:621, 1982
61. Kippenes H, Johnston G: Diagnostic imaging of osteochondrosis. Vet Clin North Am
Small Anim Pract 28:137, 1998
62. Kuivaniemi H, Tromp G, Prockop DJ: Mutations in fibrillar collagens (types I, II, III,
XI), fibril associated collagen (type IX), and network-forming coUagen (type X) cause
a spectrum of diseases of bone, cartilage, and blood vessels. Hum Mutat 9:300, 1997
FORELIMB LAMENESS IN THE YOUNG PATIENT 81
63 .. Lakatos L: Fractures of humeral epicondyles in young dogs (German). Schweiz Arch
Tierheilkd 115:412, 1973
64. Lau RB: Inherited premature closure of the distal ulnar physes. J Am Anim Hosp
Assoc 13:609, 1977
65. Lenehan TM, Nunamaker DM: Lateral approach to the canine elbow by proximal
ulnar diaphyseal osteotomy. JAVMA 180:523, 1982
66. Lewis DD, Parker RB, Hager DA: Fragmented medial coronoid process of the canine
elbow. Compend Contin Educ Pract Vet 11:703, 1989
67. Llewellyn HR: Growth plate injuries-Diagnosis, prognosis, and treatment. J Am
Anim Hosp Assoc 12:77, 1976
68. Manfra SM, Schrader SC: Physeal injuries in the dog: A review of 35 cases. JAVMA
182:708, 1983
69. Mason TA, LaVelle RB, Skipper SC, et al: Osteochondrosis of the elbow joint in young
dogs. J Small Anim Pract 21:641, 1980 .
70. McCurnin DM, Slusher R, Grier RL: A medial approach to the canine elbow joint. J
Am Anim Hosp Assoc 12:475, 1976
71. Milton JL, Montgomery RD: Congenital elbow dislocations. Vet Clin North Am Small
Anim Pract 17:873, 1987
72. Milton JL, Home RD, Bartels JE, et ale Congenital elbow luxation in the dog. JAVMA
175:572, 1979
73. Montgomery M, Tomlinson JL: Two cases of ectrodactyly and congenital elbow
luxation in the dog. J Am Anim Hosp Assoc 21:781, 1985
74. Muir P, Dubielzig RR, Johnson KA: Pan osteitis. Compend Contin Educ Pract Vet
18:29, 1996
75. Munjar TA, Austin CC, Breur GJ: Comparison of risk factors for hypertrophic osteo-
dystrophy, craniomandibular osteopathy, and canine distemper virus infection. Vet
Comp Orthop Traumatol11:37, 1998
76. Ness MG: Treatment of fragmented coronoid process in young dogs by proximal
ulnar osteotomy. J Small Anim Pract 39:15, 1998
77. Newton CD: Surgical management of distal ulnar physeal growth disturbances in
dogs. JAVMA 164:479, 1974
78. Oliveri M, Piras A, Vezzoni A, et al: Incomplete ossification of the caudal aspect of
the glenoid in dogs: Arthroscopic diagnosis and treatment. In Proceedings of the 27th
Annual Conference of the Veterinary Orthopedic Society, Val d'Isere, France, 2000,
p 20
79. Olson NL, Carrig CB, Brinker WOo Asynchronous growth of the canine radius and
ulna: Effects of retardation of longitudinal growth of the radius. Am J Vet Res
40:351, 1979
80. Olsson SEc The early diagnosis of fragmented medial coronoid process and osteochon-
dritis dissecans of the canine elbow joint. J Am Anim Hosp Assoc 19:616, 1983
81. Olsson SEc Osteochondrosis-a growing problem to dog breeders. In Gaines Dog
Research Progress. White Plains, NY, Gaines Dog Research Center, 1976, p 1
82. Ormrod AN: Limb fractures in the dog and cat. IV. Fractures of the forelimb. J Small
Anim Pract 7:155, 1966
.83. Pederson NC: Surgical correction of a congenital defect of the radius and ulna of a
dog. JAVMA 153:1328, 1968
84. Person MW: Arthroscopic treatment of osteochondritis dissecans of the canine shoul-
der. Vet Surg 18:175, 1989
85. Phillips IR: A survey of bone fractures in the dog and cat. J Small Anim Pract
20:661, 1979
86. Piermattei DL, Flo GL: The elbow joint. In Brinker WO, Piermattei DL, Flo GL (eds):
Brinker, Piermattei, and Flo's Handbook of Small Animal Orthopedics and Fracture
Repair. Philadelphia, WB Saunders, 1997, pp 288-320
87. Piennattei DL, Blass DH: Resection of the glenoid rim and humeral head. 111 Bojrab
MJ (ed): Current Teclmiques in Small Animal Surgery, ed 3. Philadelphia, Lea &
Febiger, 1990, pp 748- 749
88. Pritchard DL: Anconeal process pseudarthrosis treated with lag screw fixation. Canine
Pract 3:18-23, 1976
82 COOK
89. Probst C, Flo GL: Comparison of two caudolateral approaches to the scapulohumeral
joint for treatment of osteochondritis dissecans in dogs. JAVMA 191:1101, 1987
90. Probst CW, Flo GL, McLoughlin MA, et al: A simple medial approach to the canine
elbow for treatment of fragmented coronoid process and osteochondritis dissecans. J
Am Anim Hosp Assoc 25:331, 1989
91. Ramandan RO, Vaughan LC: Premature closure of the distal ulnar growth plate in
dogs: A review of 58 cases. J Small Anim Pract 19:647, 1978
92. Read RA, Armstrong SJ, O'Keefe JD, et al: Fragmentation of the medial coronoid
process of the ulna in dogs: A study of 109 cases. J Small Anim Pract 31:330, 1990
93. Richardson DC: Radial agenesis. J Vet Orthop 1:39, 1979
94. Richardson DC, Zentek J: Nutrition and osteochondrosis. Vet Clin North Am Small
Anim Pract 28:115, 1998
95. Riser WH, Shirer JF: Normal and abnormal growth of the distal forelimb in large and
giant dogs. J Am Vet Radiol Soc 8:23, 1967
96. Rudd RG, Whitehair JG, Margolis JH: Results of management of osteochondritis
dissecans of the humeral head in dogs: ,44 cases (1982-1987). J Am Anim Hosp Assoc
26:173, 1990
97. Salter RB, Harris WR: Injuries involving the epiphyseal plate. J Bone Surg Am
45:587, 1963
98. Shires PK, Hulse DA, Kearney MT: Carpal hyperextension in two-month-old pups.
JAVMA 186:49, 1985
99. Shull RM, HelmanRG, Spellacy E, et al: Morphologic and biochemical studies of
canine mucopolysaccharidosis 1. Am J Pathol 114:487, 1984
100. Sinibaldi KR, Arnoczky SP: Surgical removal of the ununited anconeal process in the
dog. J Am Anim Hosp Assoc 11:192, 1975
101. Sjostrom L: Ununited anconeal process in the dog. Vet Clin North Am Small Anim
Pract 28:75, 1998
102. Sjostrom L, Kasstrom H, Kalberg M: Ununited anconeal process in the dog. Pathogen-
esis and treatment by osteotomy of the ulna. Vet Comp Orthop Traumatol 8:170, 1995
103. Smith CW, Stowater JL: Osteochondritis dissecans of the canine shoulder joint: A
review of 35 cases. JAm Anim Hosp Assoc 11:658, 1975
104. Smith RN: Epiphyseal fusion in the greyhound. Vet Rec 72:75, 1960
105. Snaps FR, Saunders JH, Park RD, et al: Comparison of spin echo, gradient echo, and
fat saturation magnetic resonance imaging sequences for imaging the canine elbow.
Vet Radiol Ultrasound 39:518, 1998
106. Snaps FR, Park RD, Saunders JH, et al: Magnetic resonance arthrography of the
cubital joint in dogs affected with fragmented medial coronoid process. Am J Vet Res
60:190, 1999
107. Spackman CJ, Caywood DD, Feeney DA, et al: Thoracic wall and pulmonary trauma
in dogs sustaining fractures as a result of motor vehicle accidents. JAVMA 185:975,
1984
108. StevenS DR, Sande RD: An elbow dysplasia syndrome in the dog. JAVMA 165:1065,
1974
109. Tamas PM, Paddleford RR, Krahwinkel DJ: Thoracic trauma in dogs and cats pre-
sented for limb fractures. J Am Anim Hosp Assoc 21:161, 1985
110. Tobias TA, Miyabayashi T, Olmstead ML, et al: Surgical removal of fragmented
medial coronoid process in the dog: Comparative effects of surgical approach and
age at time of surgery. J Am Anim Hosp Assoc 30:360, 1994
111. Tomlinson I, Constantinescu G, McClure R, et al: Caudal approach to the shoulder
joint in the dog. Vet Surg 15:294, 1986
112. Turek SL: Orthopaedics, ed 4. Philadelphia, JB Lippincott, 1984
113. Turner TM: Fractures of the front limb. In Olmstead ML (ed): Small Animal Orthope-
dics, St. Louis, Mosby, 1995, pp 195-217
114. van Bree H: Comparison of the diagnostic accuracy of positive-contrast shoulder
arthrography and arthrotomy in evaluation of osteochondrosis lesions in the scapulo-
humeral joint in dogs. JAVMA 203:84, 1993
115. van Bree H, Van Ryssen B, Desmidt M: Osteochondrosis lesions of the canine shoul-
FORELIMB LAMENESS IN THE YOUNG PATIENT 83
der: Correlation of positive contrast arthrography and arthroscopy. Vet Radiol Ultra-
sound 33:342, 1992
116. Van Sickle DC, Hohn RB: Selected Orthopedic Problems in the Growing Dog. Ameri-
can Animal Hospital Association, 1975
117. Vasseur PB: Arthrodesis for congenital medial luxation of the shoulder. JAVMA
197:50, 1990
118. Vaughn JL, Jones DGC: Congenital dislocation of the shoulder joint in the dog. J
Small Anim Pract 10:1, 1969
119. Watson ADI, Blair RC, Farrow BRH, et al: Hypertrophic osteodystrophy in the dog.
Aust Vet J 49:433, 1973
120. Wind AP: Elbow incongruity and developmental elbow diseases in the dog: Part 1. J
Am Anim Hosp Assoc 22:711, 1986
12l. Wind AP: Elbow incongruity and developmental elbow diseases in the dog: Part II. J
Am Anim Hosp Assoc 22:725,1986
122. Withrow SJ: Management of a congenital elbow luxation by temporary transarticular
pinning. Vet Med Small Anim Clin 72:1597, 1977
123. Wosar MA, Lewis DD, Neuwirth L, et al: Radiographic evaluation of elbow joints
before and after surgery in dogs with possible fragmented medial coronoid process.
JAVMA 214:52, 1999
124. Zontine WI, Weitkamp RA, Lippincott CL: Redefined type of elbow dysplasia involv-
ing calcified flexor tendons attached to the medial humeral epicondyle in three dogs.
JAVMA 194:1082, 1989
Address reprint requests to
James L. Cook, DVM, PhD
Comparative Orthopaedic Laboratory
University of Missouri
379 East Campus Drive
Columbia, MO 65211
e-mail: CookJL@missouri.edu
LAMENESS 0195-5616/01 $15.00 + .00
FORELIMB LAMENESS IN THE
ADULT PATIENT
Kurt S. Schulz, DVM, MS
Forelimb lameness in the adult patient can be one of the more
frustrating problems in small animal orthopedics. This is partially a
result of the difficulty of diagnosis of some known disease, including
nerve sheath tumors and biceps tendon disease, and partially a result of
the likelihood that relatively common causes of forelimb lameness re-
main undescribed. The inability to reach a final diagnosis in cases
of forelimb lameness is more common than in hind limb lameness.
Subsequently, it is important in working up these cases that the veteri-
narian approach them in a practical and rational manner and that the
client understands the basis for this approach.
Two sound principles should be applied in working up any lame-
ness. The first principle is ruling out common diagnoses first and then
looking for the unusual diagnosis. Common diagnoses may include
fracture, osteoarthritis of any joint, and neoplasia. More unusual diagno-
ses include nerve sheath tumors, tendon tears and avulsions, and sublux-
ations. The author routinely explains to clients at the beginning of what
looks like a challenging case that we first need to rule out the most
common diagnoses ("horses") and then start to look for the "zebras." I
further state that if we reach the zebra stage, it requires more work on
my part as well as patience and greater financial commitment on their
part. As long as they understand this process, I find that most clients
are cooperative.
A second principle for approaching a lameness is to apply mini-
mally invasive diagnostic techniques first and then consider more inva-
sive diagnostics. This coincides well with the first principle, because
From the Department of Surgical and Radiological Sciences, School of Veterinary Medi.cine,
University of California, Davis, California
VETERINARY CLINICS OF NORTH AMERICA: SMALL ANIMAL PRACTICE
VOLUME 31 NUMBER 1 JANUARY 2001
86 SCHULZ
most common diseases are diagnosed with minimally invasive tech-
niques. Techniques of diagnosis of orthopedics are discussed in other
articles in this issue, but those to consider for use in the adult patient
with forelimb lameness include:
Minimally invasive techniques
Physical examination
Orthopedic examination
Neurologic examination
Arthrocentesis
Radiography
Ultrasonography
Nuclear scintigraphy (minimally invasive, although not readily
available)
Electrodiagnostics (minimally invasive, although not readily avail-
able)
More invasive techniques
Arthroscopy
Computed tomography (CT)
Magnetic resonance (MR) imaging
Myelography
Exploratory surgery
The most important of these tools is without question the orthopedic
examination. In most case, an orthopedic examination can demonstrate
the limb affected based on gait evaluation and palpation for muscle
atrophy and the site of the problem based on localization of pain and
palpation of an abnormality. The author strongly recommends that a
complete (including the hind limbs) orthopedic examination be per-
formed in every lameness case before any other diagnostics. There is a
tie for the second most valuable diagnostic tool between radiography
and arthrocentesis. Radiography is certainly performed more commonly,
but with practice, arthrocentesis can be performed simply and routinely.
The power of arthrocentesis is to determine, with little question, if a
joint is abnormal or normal and with less subjectivity than a radiograph.
Arthrocentesis should certainly be performed in all cases of forelimb
lameness when the diagnosis is not readily apparent.
By following these principles most cases of forelimb lameness can
be successfully diagnosed. Some cases may require advanced skills such
as ultrasonography or arthroscopy, whereas others may require ad-
vanced equipment such as that used for CT or nuclear scintigraphy. In
the more difficult cases, a practical approach and an educated and
understanding client help to reach the final diagnosis.
DISEASES OF THE SCAPULAR REGION
Diseases of the scapular region include:
'/ Scapula fracture
FORELIMB LAMENESS IN THE ADULT PATIENT 87
Scapula neoplasia
Nerve sheath tumor
Partial brachial plexus avulsion
Diseases of the scapula are relatively uncommon but include trauma
and neoplasia. Most fractures of the scapula in adult dogs occur at the
neck or body of the bone, whereas in younger dogs with open growth
plates, fractures of the superglenoid tubercle or acromion process are
more Fra.ctures in adult dogs should be readily diagnosed by
palpahon and radIOgraphy. Neoplasia of the scapula is less common
than that of other parts of the appendicular skeleton, but osteosarcoma
and other have been described.
8
Bone tumors that are suspected
based on plam may be confirmed in some cases by ultra-
aspIratlOn. The ultrasonography is used to localize a lytic
ill the. bone and to guide a fine needle (20-22 gauge) into the
leslOn. The shdes can be read immediately and may eliminate the need
for surgical biopsy in some cases.
Other pathologic findings in the region of the scapula that may
cause forehmb Jameness include cervical spinal cord or nerve root dis-
ease,.o.r nerve tumor. can be one of the most frustrating
to dIagnose. Palpation ill the area of the brachial plexus may
reve.al a mass or pain; however, deep palpation in this
regIOn may be paillful even in normal patients. Nerve sheath tumors are
frequently too small to be. definit.ively identified with MR imaging,
the use of may be helpful. Partial traumatic
brachial plexus avulsIOns are similarly difficult to diagnose unless a
ne.urologic and history of trauma strongly support
tJ-:e dIa1Sl1:0sls. These sltuahons tend to fall into the zebra category, and
pahence and perseverance are necessary to reach the final diagno-
SIS .. Generally, most adult canine orthopedic problems of the scapular
regIOn are caused by trauma or neoplasia, and most are readily diag-
nosed.
. suspecting a nerve sheath tumor or brachial plexus disease,
begin by ruling out common orthopedic differential
dlagnoses. JOillt taps and full-limb radiographs should be obtained, and
a bone scan may be performed as well. If the results of these tests are
negative, the. workup, including MR imaging, myelography,
and IS then required. MR imaging may demonstrate
a mass ill the reglOn of the brachial plexus or spinal cord. Myelography
demonstrate a mass or swelling in the region of the brachial
illtumescence. Electrodiagnostics, including motor nerve conduction ve-
locity and electromyography, may show altered nerve function.
DISEASES OF THE SHOULDER REGION
Diseases of the shoulder region include:
Osteoarthritis
88 SCHULZ
Shoulder luxation
Shoulder subluxation
Infraspinatus contracture
Biceps tenosynovitis or tear
Other shoulder trauma
Septic arthritis
Immune-mediated arthritis
Calcification of the supraspinatus
Clinically significant osteoarthritis of the shoulder is relatively un-
common in comparison to osteoarthritis of other joints. This may be a
result of the fact that this large, relatively flat, congruent joint tolerates
osteoarthritic changes better than smaller and less congruent joints in
the dog. Osteoarthritis may be secondary to osteochondrosis dissecans
(OCD), previous trauma (including fracture or luxation), immune-medi-
ated joint disease, or diseases of the biceps tendon. The diagnosis of
shoulder arthritis can be made from lateral radiographs of the joint and
from a joint tap. A definitive diagnosis can be made with arthroscopy,
which also provides an opportunity to look for predisposing factors,
including previous OCD, migrated OCD flaps, and trauma to the gleno-
humeral ligaments. A diagnosis of shoulder arthritis based on radiogra-
phy or arthrocentesis should be followed by further diagnostics for the
underlying cause, since shoulder arthritis alone is rarely a cause of
forelimb lameness.
Shoulder luxations in adult dogs may be either traumatic or congen-
ital. Most congenitalluxations occur in small-breed dogs and are diag-
nosed while the animal is still young. Further discussion of congenital
shoulder luxations may be found in other articles in this issue. Traumatic
luxations of the shoulder are relatively uncommon, because trauma more
commonly results in fractures of the scapula or humerus. The diagnosis
is most often made by palpation. The patient should be heavily sedated
or anesthetized before manipulation. Radiographs (mediolateral and
ventrodorsal) may then be obtained, or the diagnosis may be made by
palpating severe instability or luxation of the joint. Most traumatic
luxations can be reduced at the time of diagnosis and then stabilized
with either a velpeau bandage for medialluxations or a spica splint for
lateral luxations. In rare cases, internal stabilization is necessary. The
overall prognosis for these unusual injuries is favorable.
Subluxation or instability of the shoulder has been recently suggested
as a cause of forelimb lameness.] Subluxation or instability may be
diagnosed by palpating in a motion similar to that of performing drawer
motion on a knee.] This instability may be associated with damage to
the tendons or muscles surrounding the joint or damage to the glenohu-
meralligaments or joint capsule. Further clinical research is required to
determine if this a real entity of forelimb lameness; however, experience
with human shoulder injuries and concern for missed diagnoses of
shoulder joint problems in the dog make this a realistic possibility.
Extensive use of arthroscopy in evaluation of the shoulder joint should
FORELIMB LAMENESS IN THE ADULT PATIENT 89
dramatically improve our understanding of these injuries over the com-
ing years.
Infraspinatus contracture is reported most commonly in hunting
dogs and is of an unknown pathogenesis, although most evidence sug-
gests that it is a primary muscle disorder resulting from trauma (Fig.
1).2 Fortunately, the disease is relatively easily diagnosed, and the treat-
ment is highly successful. Dogs with infraspinatus contracture carry the
limb with dramatic external rotation. The limb is commonly circum-
ducted as the animal attempts to walk, and atrophy of the muscle is
noted on palpation. The disease is readily treated by tenotomy of the
insertion of the muscle and results in almost immediate improvement.
Diseases of the biceps tendon are now being recognized as a com-
mon cause of forelimb lameness. Numerous diseases and names are
associated, including biceps tenosynovitis, bicipital bursitis, and tearing
or rupture of the biceps tendon. These diseases may be associated with
a single episode of trauma but more commonly are diagnosed in work-
Figure 1. Golden Retriever with external rotation of the forelimb associated with contracture
of the infraspinatus muscle.
90 SCHULZ
ing or performance dogs and may be caused by chronic low-grade
trauma? The lameness may be mild or non-weight-bearing. Physical
examination reveals muscle atrophy on the side affected and pain on
simultaneous flexion of the shoulder and extension of the elbow. Pain
may be accentuated by palpation of the biceps tendon while the limb is
in this position. In severe cases, radiographs demonstrate calcification in
the bicipital groove of the humerus and osteoarthritis of the shoulder
joint. Arthrocentesis of the joint or bursa should be compatible. with
osteoarthritis. Ultrasonography has recently proven to be valuable ill the
diagnosis of diseases of the biceps tendon.
4
Ultrasonography may show
changes in the fluid volume of the bursa, disruption of fibers of the
tendon, or complete rupture of the tendon. Previously, contrast arthrog-
raphy was used to diagnose this disease, but it is no longer necessary if
ultrasonography is available. In cases where the tendon trauma is close
to the superglenoid tubercle, the diagnosis can also be made by arthros-
copy. Arthroscopy is strongly recommended as part of the workup and
treatment in these cases because it may reveal concurrent injuries to
other structures surrounding the joint, which may alter the treatment or
prognosis. Medical management of these cases includes steroid injection
into the bursa and strict exercise limitation for 2 to 3 months. Surgical
options include open or arthroscopic tenotomy or open tenodesis of the
origin of the biceps tendon to the proximal humerus.
Other forms of trauma that have been recognized around the shoul-
der joint include damage to the glenohumeral ligaments or other tendons
around the joint (Fig. 2) . These less common injuries require either
Figure 2. Arthroscopic view of a partially torn medial glenohumeral ligament.
l
r
I
I
FORELIMB LAMENESS IN THE ADULT PATIENT 91
ultrasonography or arthroscopy to diagnose. Currently, not enough in-
formation is available regarding these problems to discuss their defini-
tive diagnOSiS or prognosis; however, aggressive diagnostics with ultra-
sonography or arthroscopy may provide a diagnosis in many cases of
uncertain shoulder injuries.
Septic and immune-mediated arthritis of the shoulder is uncommon.
Septic arthritis may be a result of either trauma or previous surgery.
Septic and immune-mediated arthritides are readily diagnosed by
arthrocentesis.
Calcification of the supraspinatus tendon is infrequently recognized
on lateral shoulder radiographs and mayor may not be a significant
clinical finding.
3
Little is known about the causes or significance of this
problem, although it has been recognized to cause lameness in some
cases. This finding may also be noted when other diseases of the biceps
tendon have been diagnosed. The disease is suspected based on pain in
the shoulder region and palpation of the tendon, and it is confirmed by
lateral radiography of the shoulder. Other disease processes in the limb
and particularly in the shoulder region should be ruled out before
treatment for this problem is implemented.
DISEASES OF THE HUMERAL REGION
Diseases of the humeral region include:
Fracture
Neoplasia
Other diseases
In the adult dog, diseases of the humeral region are generally
limited to neoplasia and fracture. Osteosarcoma is the most common
neoplasia of the humerus and is most frequently identified in the proxi-
mal aspect of the bone. Physical examination findings include pain on
deep palpation and generalized muscle atrophy of the limb. Radiogra-
phy reveals an osteolytic or osteoproductive lesion. Again, ultrasonogra-
phy may be useful in identifying lytic areas of the lesion, which enables
fine-needle aspiration and diagnosis based on cytology alone. Although
the definitive diagnosis may not be determined by fine-needle aspiration,
the aspirate may provide enough information to decide between surgical
biopsy and amputation.
DISEASES OF THE ELBOW JOiNT REGION
Diseases of the elbow joint region include:
Humeral condylar fracture
Osteoarthritis
Elbow joint luxation
92 SCHULZ
Neoplasia
Infectious and immune-mediated arthritis
Fracture of the lateral portion of the humeral condyle is the most
common fracture involving the elbow (Fig. 3). This fracture has been
identified most commonly in the Cocker Spaniel in the United States
but has also been reported commonly in other breeds in other countries.
s
Fracture of the lateral portion of the humeral condyle is seen after minor
trauma or normal activity such as jumping off a bed or out of a car.
Certain animals are thought to be predisposed to this disease because of
incomplete fusion of the medial and lateral growth centers of the hu-
meral condyles. These dogs are left with a fibrous nonunion between
the condyles that can fracture with only minimal force. In addition, the
radius articulates primarily with the lateral portion of the humeral
condyle, which is offset from the longitudinal axis of the humerus,
making it particularly susceptible to shearing forces. The diagnosis is
obvious on examination and radiographic findings; however, it is
Figure 3. Radiograph of a lateral humeral condylar fracture.
FORELIMB LAMENESS IN THE ADULT PATIENT 93
strongly recommended that radiographs of the ?pposite elbow: be ob-
tained at the time of diagnosis to evaluate for mcomplete fuslOn that
might lead to fracture in the future. In these cases, it has been recom-
mended that a transcondylar screw be placed across the condyle to
lessen the chance of fracture.
Osteoarthritis of the elbow joint is a common and often debilitating
disease in adult dogs. This may be the result of any of the juvenile
diseases of the elbow, including a fragmented coronoid process, an
ununited anconeal process, or osteochondrosis. It may also be an end
result of previous trauma or previous immune-mediated or septic arthri-
tis. An additional cause of significant elbow joint arthritis is elbow joint
incongruity associated with premature closure of a growth plate. ~ s
discussed in other articles in this issue, the most common form is
premature closure of the distal ulnar growth plate, which leads to elbow
joint incongruity and secondary osteoarthritis. The diagnosis of arthritis
is made based on the orthopedic examination, radiographic evaluation,
and arthrocentesis. Palpation of the limb reveals relative muscle atrophy
and potentially fibrous or bony thickening of the elbow joint. In severe
cases, the range. of motion of the elbow joint in flexion is limited to 90
between the humerus and antebrachium. Crepitus may also be felt
on joint manipulation. Radiographs may demonstrate mild osteophyte
production or complete destruction of the bony anatomy. They n::ay also
demonstrate the underlying cause such as a fragmented coronOld proc-
ess, an ununited anconceal process,or joint incongruity. Arthrocentesis
should demonstrate a low to moderate cell count (3000-8000 cells/ul)
composed primarily of mature mononuclear cells. Joint fluid is obtained
from the elbow joint by inserting a needle in a craniomedial and distal
direction starting midway between the lateral epicondyle and ulna.
Arthroscopy may also be of value in early cases of elbow arthritis to
determine the location and severity of the lesions and to evaluate the
potential efficacy of surgical therapy. .
Luxation of the elbow joint may be either traumatic or congenital
(Fig. 4). The congenital form of the disease is discussed elsewhere in this
issue. Traumatic elbow luxation is a cornmon injury, with most luxation
resulting in lateral displacement of the antebrachium relative to the
humerus. The diagnosis is based on orthopedic examination and radiog-
raphy. On presentation, the animal is non-weight-bearing with a severely
swollen elbow joint region. The limb is held in slight flexion and is quite
painful. The patient should be heavily sedated or anesthetized as soon
as possible, and radiographs should be obtained to confirm the diagnosis
and evaluate for additional trauma such as a fracture. Once the diagnosis
is confirmed, the elbow joint should be reduced immediately and placed
in a cast, with the elbow joint extended for 10 to 14 days. In most cases,
this results in an excellent outcome, because surgery is rarely indicated.
Neoplasia of the elbow joint is rarely diagnosed. Differential diagno-
ses include synovial cell sarcoma, chondrosarcoma, and fibrosarcoma. A
high degree of suspicion is often based on radiographs of the joint, which
demonstrate a soft tissue mass effect and some degree of osteolysis. The
94 SCHULZ
Figure 4. Weimaraner with swelling of the elbow region caused by luxation of the joint.
diagnosis may be supported by ultrasound-guided aspiration or surgical
or arthroscopic biopsy.
Infectious and immune-mediated arthritis occurs more commonly
in the elbow joint than in the shoulder joint but less commonly than in
many other joints in the body. Bacterial infectious arthritis of the elbow
is probably most commonly a result of trauma or surgery. The diagnosis
is most often made based on arthrocentesis and joint culture. Cytology
of the joint fluid usually demonstrates moderate to high numbers of
cells (30,000-100,000 cells/ul), of which a large percentage are degenerate
neutrophils. The fluid should be submitted for culture; however, there is
a high degree of false-negative results with routine culturing techniques.
When submitting cultures, it is important to consult with your laboratory
regarding specific techniques for improving joint culturing. One recom-
mended technique is to dilute joint fluid at a 1:9 ratio in blood culture
medium and submit this to the laboratory as well. This has been shown
to improve chances of a positive culture as compared with routine
culture of fluid or synovium.
6
FORELIMB LAMENESS IN THE ADULT PATIENT 95
Rickettsial diseases may also be a cause of septic arthritis in the
elbow or other joints. If rickettsial infection is suspected based on joint
fluid evaluation, titers for common infectious agents should be per-
formed. The patient may be started on doxycycline while waiting for
test results, and a response to therapy may further support a diagnosis
of rickettsial infection. Immune-mediated joint diseases also cause a
significant elevation in joint fluid cell counts and a dramatic increase in
the percentage of neutrophils, although the neutrophils are most often
not degenerate to the degree observed with bacterial arthritis. The value
of immune panels and assays remains in question in these cases because
of the high degree of false-negative and false-positive results associated
with these tests (antinuclear antibodies, rheumatoid factor). When im-
mune-mediated joint disease is suspected, we continue to recommend
titers for rickettsial diseases and initial treatment with doxycycline to
evaluate for a positive reponse before initiating immunosuppressive
therapy.
DI SEASES OF- THE RADIOULNAR REGION
Diseases of the radioulnar region include:
Fracture
Neoplasia
Bone cysts
Fractures of the radius and ulna tend to occur most commonly in
the middle and distal diaphysis. Caution should be taken in treatment
of these lesions in small-breed dogs, where improper repair is associated
with a high degree of nonunion, and in older dogs, where the fracture
may be pathologic secondary to osteosarcoma.
Osteosarcoma occurs most commonly in the distal radius of the
dog. Physical examination may demonstrate muscle atrophy and pain
on deep palpation of the region. Radiographs should be obtained and
demonstrate an osteoproductive or osteolytic lesion in most cases. In
other cases, nuclear scintigraphy or bone scanning may be necessary to
define the location of early lesions. Radiographs supporting a diagnosis
of neoplasia in this region are often adequate to support amputation as
long as thoracic radiographs do not reveal metastatic disease. Again,
however, a diagnosis may be made cytologically with the aid of ultraso-
nography and fine-needle aspiration. .
Bone cysts are uncommonly diagnosed lesions that may occur any-
where in the skeleton but have been most often described in the radius.
The cause of simple fluid-filled bone cysts is unknown but may be
related to altered vascular flow. Aneurysmal bone cysts are composed
of compartmentalized vascular sinusoids. Although generally benign,
bone cysts can cause lameness and may be confused on radiographs
and histopathology with osteosarcoma. Radiographs may demonstrate
an osteolytic expansile lesion in the diaphysis surrounded by a sclerotic
96 SCHULZ
region of bone. Definitive diagnosis requires bone biopsy, at which time
treatment, including debridement and filling with cancellous bone graft,
may be recommended.
DISEASES OF THE CARPAL REGION
Diseases of the carpal region include:
Osteoarthritis
Fracture
Hyperextension
Immune-mediated joint disease
Collateral ligament injury
Osteoarthritis is a common finding of the carpal joint but is not
always clinically significant. In many older or more active dogs, the
range of motion of the carpal joint is reduced in flexion in association
with fibrosis of the periarticular soft tissues and osteoarthritis. In a
normal dog, the carpus should be able to flex such that the digital pads
can contact the caudal surface of the antebrachium. Fibrosis around the
joint often limits the range of motion in flexion; however, in most cases,
this is not associated with lameness. Clinically significant osteoarthritis
of the carpus may be a result of previous immune-mediated joint disease,
septic arthritis, previous trauma, or angular limb deformity. The diagno-
sis is confirmed by radiography, which shows progressive osteophytosis,
and by arthrocentesis. Joint taps are performed on the carpus by flexing
the joint and inserting a small-gauge (22-gauge) needle into the joint
from the dorsal surface. As is the case with all joint taps, the patient
should be sedated, and the site should be clipped and scrubbed. Sedation
is important to minimize pain to the patient and trauma to the articular
surface, which occur if the animal moves during the joint tap.
Fractures of the carpal bones are uncommon except in racing dogs.
Other trauma includes carpal hyperextension injuries (Fig. 5). These
occur most commonly when all. animal accidentally falls from a high
surface and lands on its front feet. In most cases, the patient is unable
to stand on one or both forelimbs. When it does attempt to stand, the
carpal pad contacts the ground, and all. obvious hyperextension defor-
mity is noted. The dog should be sedated or anesthetized as soon
as possible for palpation, radiography, and temporary or permanent
stabilization. Palpation of the joint demonstrates extension of the carpus
beyond the normal 10 to 15. If the other carpus is normal, it may be
used for comparison in the orthopedic and radiographic examinations.
Radiographs should include dorsoventral and mediolateral views as
well as stressed extension views with comparison to the normal limb. In
most cases, the damage is primarily to the carpal fibrocartilage, but the
radiographs should be scrutinized for other injuries such as fractures.
After a thorough evaluation, the affected limb should be placed in a
metasplint or fiberglass splint to support it and help to relieve the pain.
FORELIMB LAMENESS IN THE ADULT PATIENT 97
Figure 5. Mixed-breed dog with traumatic carpal hyperextension injury
Although splinting and bandaging have been described as a means of
therapy for these cases, most dogs eventually require arthrodesis; how-
ever, the outcome with arthrodesis of the carpus is generally excellent.
Like the tarsus, the carpus is one of the most common sites for
immune-mediated joint disease. As previously described, the diagnosis
is made based on radiographic findings of erosive or nonerosive arthritis
and joint taps demonstrating significantly increased cell counts and
percentages of nondegenerate neutrophils. Again, bacterial and rickett-
sial causes of arthritis must be ruled out by joint culture or titers before
initiation of immunosuppressive therapy. Septic arthritis may occur in
the carpus secondary to penetrating foreign bodies or dog bite wounds.
-Although most joint infections are caused by Staphylococcus species,
proper culturing of the joint is imperative to ensure selection of the
correct antibiotic.
Other injuries to the carpal joint include avulsion or tearing of the
collateral ligaments. Although not as common as damage to the collat-
eral ligaments of the tarsus, it should be included as a differential
diagnosis for dogs with traumatic injuries. This injury occurs most
commonly in hunting and active dogs and often results in a 11.011.- or
minimally weight-bearing lameness. The diagnosis is made by palpation
and radiography. With the animal heavily sedated or anesthetized, the
jOill.t is palpated in the mediolateral plane, trying to break the joint open
in each direction. Comparison with the normal limb helps in ascertaining
98 SCHULZ
if the range of motion is normal. Stress radiographs can be performed,
again, trying to break the joint open either medially or laterally and
using the opposite limb as a means of comparison. At the conclusion of
the studies, the limb should be temporarily stabilized with a fiberglass
splint or metasplint if definitive therapy is not going to be performed at
that time.
DISEASES OF THE FOOT
Diseases of the foot include:
Osteoarthritis
Fractures
Fragmented sesamoid
Osteoarthritis may occur in any of the joints of the foot and is most
often a result of previous trauma. The diagnosis is initially based on
careful palpation of the joints of the foot. This reveals firm thickening of
the joint or joints and an accompanying decreased range of motion. The
diagnosis is confirmed by radiography. Arthrocentesis of these joints is
usually impractical because of their small size and the difficulty in
obtaining fluid. Fractures may also occur in any of the bones of the foot
but happen most frequently in the metacarpals. Again, the diagnosis
is based on palpation of crepitus and instability and confirmation by
radiography.
Fragmented sesamoid disease remains a difficult problem in dogs.
The breeds most commonly involved include Rottweilers, Labrador Re-
trievers, and Greyhounds. The bones involved are usually the second or
seventh sesamoids. The disease may be suspected based on pain on
manipulation of the foot. Specific maneuvers to screen for the disease
include hyperextension and hyperflexion of the metacarpal-phalangeal
joints and direct pressure over the area of the sesamoids. It should be
noted, however, that many dogs are sensitive to palpation of the feet,
particularly the front feet, making it difficult to differentiate between a
true pain response and just annoyance.
A definitive diagnosis of fragmentation of the sesamoids is made
by radiography. Most cases are evident on a dorsoventral view. In some
cases, the sesamoid in question may be isolated on a lateral view by
pulling the remaining digits dorsally or ventrally out of the way. The
presence of fragmentation of the sesamoid on a radiograph does not
indicate that it is a clinical problem. Clinically sound dogs may have
radiographic diagnoses of fragmented sesamoids. Furthermore, because
an acceptably successful therapy has not yet been determined for this
problem, other sources of lameness should be investigated before initiat-
ing potentially harmful therapy for this poorly understood disease.
l
i
I
!
I
FORELIMB LAMENESS IN THE ADULT PATIENT 99
CONCLUSIONS
Lameness of the forelimb may be one of the more frustrating prob-
lems in small animal orthopedics. It is likely that numerous causes of
forelimb lameness are not yet defined or well understood. In an ap-
proach to these cases, one should always begin with a thorough orthope-
dic examination and then proceed to minimally invasive diagnostics,
including radiography, ultrasonography, and arthrocentesis. Additional
steps may include bone scanning, arthroscopy, and CT or MR imaging.
The simplest causes should be ruled out first; then, with the understand-
ing of the owner, more obscure diagnoses can be pursued. Keep it
simple, but watch out for zebras.
References
1. Bardet JF: Diagnosis of shoulder instability in dogs and cats. Vet Comp Orthop Trau-
matol 34:42- 54, 1998
2. Bennett RA: Contracture of the infraspinatus muscle in dogs: A review of 12 cases. J
Am Arum Hosp"Assoc 22:481--487, 1986
3. Flo GL, Middleton 0: Mineralization of the supraspinatus tendon in dogs. JAVMA
197:95- 97, 1990
4. Long CD, Nyland TG: Ultrasonographic evaluation of the canine shoulder. Vet Radiol
Ultrasound 40:372-379, 1999
5. Marcellin-Little DJ, DeYoung DJ, Ferris KK, et al: Incomplete ossification of the humeral
condyle in spaniels. Vet Surg 23:475--487, 1994
6. Montgomery RD, Long IR, Jr, Milton JL, et al: Comparison of aerobic culturette, synovial
membrane biopsy, and blood culture medium in detection of canine bacterial arthritis.
Vet Surg 18:300- 303, 1989
7. Stobie D, Wallace LJ, Lipowitz AJ, et al: Chronic bicipital tenosynovitis in dogs: 29 cases
(1985- 1992). JAVMA 207:201-207, 1995
8. Trout NJ, Pavletic M, Kraus KH: Partial scapulectomy for management of sarcomas in
three dogs and two cats. JAVMA 207:585- 587, 1995
Address reprint requests to
Kurt S. Schulz, DVM, MS
Department of Surgical and Radiological Sciences
School of Veterinary Medicine
University of California, Davis
2112 Tupper Hall
Davis, CA 95616
LAMENESS 0195-5616/01 $15.00 + .00
HIND LIMB LAMENESS IN THE
YOUNG PATIENT
Ron M. McLaughlin, DVM, DVSc
Hind limb lameness is common in young dogs and may result
from congenital abnormalities, developmental orthopedic diseases, and
trauma. Some causes of lameness more frequently affect fast-growing
large breeds of dogs, although other diseases more commonly affect
smaller breeds. In most cases, the lameness can be successfully treated
if it is diagnosed early and appropriate treatment is initiated. Reaching
an accurate diagnosis of a hind limb lameness requires consideration
of the patient's signalment, a good physical examination, a complete
understanding of the patient's history, and a knowledge of common
diseases affecting certain breeds and sizes of dogs.
ABNORMALITIES OF THE COXOFEMORAL JOINT
Legg-Calve-Perthes Disease
Legg-Calve-Perthes (LCP) disease is an aseptic necrosis of the femo-
ral head.
31
It affects primarily small and miniature breeds of dogs at
approximately 4 to 11 months of age. The disease is bilateral in approxi-
mately 15% of cases, and male and female dogs are equally affected.
The exact cause of LCP is unknown, although several possible causes
.have been investigated. An autosomal recessive gene has been reported
to be the cause in some dogs.
31
In children, LCP has been associated
with trauma to the hip joint.
From The Animal Health Center, College of Veterinary Medicine, Mississippi State Univer-
sity, Mississippi State, Mississippi
VETERINARY CLINICS OF NORTH AMERICA: SMALL ANIMAL PRACTICE
VOLUME 31 NUMBER 1 JANUARY 2001 101
102 McLAUGHLIN
Clinical Signs
Clinical signs of LCP include hip pain, crepitus, lameness, and
muscle atrophy. The lameness is often acute and may occur after a
"minor trauma" such as jumping or falling. In some cases, the owners
may report an intermittent lameness. Once the disease has progressed,
the patient is often non- weight bearing and may be reluctant to walk,
particularly in cases of bilateral disease.
Diagnosis
The diagnosis of LCP can generally be confirmed by radiography.
Radiographic signs include flattening and irregularity of the femoral
head, an irregular radiographic density of the femoral head ("moth-
eaten"), shortening and widening of the femoral neck, and possibly
femoral neck fractures (Fig. 1).
Figure 1. Ventrodorsal hip-extended radiographic view of a young, small -breed . dog with
Legg-Calve-Perthes disease. Note the lysis and irregularity of the left femoral head (arrow).
HIND LIMB LAMENESS IN THE YOUNG PATIENT 103
Treatment
The most common treatment for LCP in dogs is femoral head and
neck excision (FHNE) arthroplasty, although other treatments have been
attempted with limited success. The prognosis for function after excision
arthroplasty is good in these smaller dogs.
Hip Dysplasia
Hip dysplasia is a common skeletal developmental defect in dogs
produced by a genetic predisposition to subluxation of the immature
hip joint.
33
, 35, 44 It more commonly affects large-breed dogs but is also
seen in many small-breed dogs and cats. Joint laxity is the initiating
cause of dysplasia and leads to subluxation and poor congruence be-
tween the femoral head and acetabulum. This creates abnormal forces
across the joint that interfere with normal development and overload
areas of articular cartilage. Over time, degeneration of the joint occurs.
Numerous factprs influence the development and progression of hip
dysplasia, including genetics, rapid weight gain in growing animals, a
high nutrition level, and pelvic muscle mass.
33
, 35, 44
Clinical Signs
Hip dysplasia usually affects both hips, although one hip may seem
to be more severely affected than the other. In many cases, dogs are
presented for a lameness in only one hind limb. Clinical signs of hip
dysplasia can be variable and may include decreased activity, difficulty
in rising, reluctance to run or climb stairs, intermittent hind limb lame-
ness, "bunny hopping," swaying gait, narrow stance, hip pain, atrophy
of the thigh muscles, hypertrophy of shoulder muscles, crepitus, and
reduced hip joint motion. Joint laxity (detected clinically by a positive
Ortolani sign) is characteristic of early hip dysplasia; however, joint
laxity may no longer be present in chronic cases because of periarticular
fibrosis. In many cases, early signs are overlooked by owners, and the
dogs may not be presented for veterinary care until late in the disease.
Diagnosis
A tentative diagnosis of hip dysplasia can often be made based on
palpation, history, and clinical signs; however, a defmitive diagnosis
requires radiographic confirmation of hip joint laxity (subluxation) or
secondary morphometric and degenerative changes within the joint (Fig.
2).13 Early in the disease, the shapes of the acetabulum and femoral head
are normal, and the primary radiographic finding is joint incongruity.
Identification of this joint laxity is essential to the early diagnosis of hip
dysplasia.
Joint subluxation may be observed subjectively on a ventrodorsal
104 McLAUGHLIN
Figure 2. Ventrodorsal hip-extended radiographic view of a young, large-breed dog with
hip dysplasia. Subluxation of the coxofemoral joint is evident bilaterally.
hip-extended radiographic view of the pelvis.
9
, 10 The degree of subluxa-
tion can be quantified by measuring the Norberg angle (angle formed
by a line drawn from the center of the femoral head to the cranial
acetabular rim and a line drawn between the centers of the two femoral
heads) or by calculating the percentage of coverage of the femoral head
by the acetabulum. Unfortunately, the magnitude of joint subluxation
observed on ventrodorsal hip-extended radiographs is positionally de-
pendent and can vary significantly in sequential radiographs obtained
in the same dog. Additionally, the twisting of the joint capsule that
occurs when the dog is placed in this position can mask the presence of
joint laxity.25
A better method of measuring joint laxity uses distraction radiogra-
phy. Two techniques have been described to obtain distraction radio-
graphs in the dog. In the first technique, used with the PennHip system
(Symbiotics Corporation, PennHip Analysis Center, Malvern, PA), the
dog is positioned in dorsal recumbency with the femurs in a neutral
position.
5
0,51 Distraction is created by placing a wedge between the dog's
HIND LIMB LAMENESS IN THE YOUNG PATIENT 105
thighs and applying a medially directed force to the stifles, The distance
the femoral head moves out of the acetabulum is measured to obtain a
"distraction index," which is a measure of the passive laxity present in
the joint. Measurement of the distraction index has been shown to be a
reliable predictor of the eventual development of osteoarthritis in lax
hip joints. In the second technique, the dorsolateral subluxation test, the
dog is positioned in sternal recumbency with the knees flexed and
adducted so that the femurs are perpendicular to the table surface. IS, 16
With the hind limbs in this kneeling position, weight bearing is simu-
lated and the femoral head subluxates dorsolaterally when laxity is
present. The dorsolateral subluxation technique seems to provide a way
to measure the chondro-osseus hip joint conformation, which differs
from the measurement of passive joint laxity provided by the distraction
index.1s, 16
In more chronic cases of hip dysplasia, radiographic changes indica-
tive of joint degeneration and remodeling can be seen.
13
As abnormal
forces continue to act on the lax hip joint, the acetabulum becomes
shallow, and the femoral head begins to flatten. Osteophytes form at the
joint margins and are apparent radiographically as new bone production,
The acetabular margin becomes irregular, and the femoral neck becomes
thicker as the osteophytes are formed. Sclerosis of the subchondral bone
develops and is often most apparent on the craniodorsal acetabular rim.
Fibrosis and increased density of the periarticular soft tissues are also
apparent radiographically. Because of periarticular fibrosis, joint laxity
may no longer be a major component of the disease in chronic hip
dysplasia.
Treatment
Medical and surgical treatments have been used for hip dysplasia
in young dogs. Medical treatment typically includes weight control or
weight loss, physical therapy and exercise control, nonsteroidal anti-
inflammatory drugs, and disease-modifying osteoarthritis agents.
7
, 8, 12, 18,
28,29,32, 34,38,40,58 Medical therapy is quite successful in many cases.
Surgical techniques used to treat hip dysplaSia depend on the size
and age of the dog the amount of osteoarthritis present, cost, and
clinician preference. In young dogs with hip joint laxity and no osteoar-
thritis, a triple pelvic osteotomy (TPO) is often recommended.
26
, 36, 37, 48
TPO is a corrective surgical procedure that reorients the acetabulum to
establish congruity between the femoral head and acetabulum. It in-
creases acetabular coverage of the femoral head to eliminate subluxation
and improve joint stability. To be successful, the procedure must be
performed early in the disease process before osteoarthritic changes
develop and while the remodeling capability exists to allow develop-
ment of a more congruent joint.
36
, 37 Ideally, TPO should be performed in
dogs less than 10 months of age. TPO is contraindicated once significant
osteoarthritis is present, Whether TPO is indicated in asymptomatic
dogs with radiographic evidence of hip laxity remains controversial;
106 McLAUGHLIN
however, many clinicians believe the potential success of conservative
medical therapy precludes the use of TPO unless significant clinical
signs are present.
In dysplastic dogs with osteoarthritis that are unresponsive to medi-
cal therapy, total hip arthroplasty is recommendedY The procedure to
implant the prosthetic hip components requires specialized equipment
and training but yields excellent results in most cases. Generally, total
hip arthroplasty is performed after the dog reaches skeletal maturity. If
possible, the dysplastic dogs are managed medically until they are at
least 10 to 12 months of age before performing total hip arthroplasty.
Alternatively, a FHNE arthroplasty can be performed.
5
, 20 The goal is to
eliminate hip pain by removing the femoral head and neck and initiating
the development of a fibrous pseup-oarthrosis that permits ambulation.
The procedure can be performed in dogs of all sizes; however, results are
usually better in smaller and lighter dogs 20 kg). FHNE arthroplasty is
the current surgery of choice for smaller dogs with hip dysplasia that is
unresponsive to medical treatment. FHNE arthroplasty can also be used
with success in large dogs. In the author's experience, prevention of
arthritic changes with TPO or replacement of an arthritic hip with a
total hip prosthesis gives the best chance for return of normal function
in larger dogs.
ABNORMALITIES OF THE STIFLE JOINT
Cranial Cruciate Ligament Injury
The cranial cruciate ligament (CrCL) is critical for the congruent
anatomy and function of the canine stifle. The CrCL prevents stifle
hyperextension, internal rotation of the tibia, and cranial translation of
the tibia relative to the femoral condyles (drawer motion). The CrCL
consists of two parts. The "anterior medial band" is taut throughout
extension and flexion of the stifle joint. The "posterior lateral band" is
lax in stifle flexion.
Injury and rupture of the CrCL is the major cause of degenerative
joint disease in the stifle and one of the most common injuries in the
dog. The exact cause of cruciate ligament injury is not always apparent,
and numerous factors may playa role. In some cases, the application of
a supraphysiologic load to the ligament can cause rupture such as occurs
with sudden hyperextension of the stifle or with severe internal rotation
of the tibia when the stifle flexed. In many mature dogs, the primary
cause of CrCL rupture is degeneration of the ligament, which occurs
with age and a sedentary life style. Rupture of the CrCL is also com-
monly seen in young active dogs that have sustained no known trauma
to the stifle.
14
In this younger group of dogs, the ligament seems to
rupture gradually, perhaps as a result of conformational abnormalities,
joint inflammation, primary degenerative changes, or other factors.
1
In a
recent study, Newfoundland and Rottweiler dogs less than 2 years of
HIND LIMB LAMENESS IN THE YOUNG PATIENT 107
age were found to have a higher risk of CrCL rupture compared with a
control population of dogs of the same age category. Other overrepre-
sented breeds in this same study were the Akita, Labrador Retriever,
Mastiff, Staffordshire Terrier, English Bulldog, Boxer, St Bernard, Chesa-
peake Bay Retriever, Giant Schnauzer, and Bouvier des Flanders.14
Clinical Signs
Injury to the CrCL often occurs in younger active dogs. Clinical
signs include a sudden onset of non-weight-bearing lameness, stifle
pain, and palpable joint effusion. The lameness may improve with rest
but redevelops several weeks to months later. The lameness may also be
progressive and persistent, and it is often worse after exercise. Most of
these dogs have a palpable positive cranial drawer sign and stifle effu-
sion, crepitus, and radiographic signs consistent with osteoarthritis may
already be present in the stifle at the time of diagnosis. In more chronic
cases, muscle atrophy and a firm swelling on the medial aspect of the
stifle joint may be present. This medial swelling, often called a medial
buttress, is caused by periarticular fibrosis in the region of the medial
collateral ligament. A cranial drawer sign may or may not be present
depending on the degree of periarticular fibrosis . Radiographs of the
stifle often reveal a decreased fat pad density in the cranial compartment
of the stifle, increases in soft tissue density surrounding the joint (espe-
cially medially), and periarticular osteophyte formation.
In some dogs, a chronic, insidious, intermittent, weight-bearing
lameness occurs with pain in the stifle joint. The lameness varies signifi-
cantly in severity and occurs in young and old dogs. A cranial drawer
motion can be difficult to palpate, although joint effusion is often pres-
ent. This history is consistent with partial tears of the CrCL. Many of
these dogs eventually develop significant osteoarthritis, and the lame-
ness becomes more persistent and severe. The partial tear may progress
to a complete rupture of the CrCL with time.
Diagnosis
Diagnosis of a CrCL injury is based on history and palpation of
joint laxity (cranial drawer motion). In chronic cases, when drawer
motion may be masked by periarticular fibrosis, cruciate ligament injury
should be strongly suspected in dogs with stifle pain, joint effusion,
lameness, and a medial buttress. In large or muscular dogs, it is im-
portant to examine for stifle laxity with the dog placed under sedation.
Also, the clinician must always palpate the stifle joint in flexion and
extension to identify partial tears. Dogs with a partial tear of the CrCL
often have cranial drawer motion in flexion only. The tibial compression
test (flexion of the hock with the stifle in extension) may also be used to
assess .cruciate ligament stability. The tibial crest is displaced cranially
when the cruciate ligament is ruptured. In some cases, a "click" or
"popping" sensation may be noted during manipulation of the stifle
108 McLAUGHLIN
joint and can be indicative of a n:eniscal Radios;raphs C?f stifle
may reveal joint effusion, and m chromc cases, radIOgraphic SIgnS of
osteoarthritis may be seen. In extremely young dogs, avulSIOn
from the ligament's femoral origin or tibial insertion may be apprecIated.
Treatment
Rest and analgesic medications are an acceptable treatment for
cruciate ligament injuries in cats and some small dogs.
57
fibrosis eventually minimizes joint instability and reduces pam; however,
cartilage damage and degenerative joint disease proogress and can.
persistent joint pain and lameness. In study, 86 Yo of dogs welghmg
less than 15 kg were considered to be clmlcally normal after conservahve
therapy.57 .
Conservative therapy is not m dogs large: than 15
kg, because joint instability persists contmues to cause dIscomfort
in these animals. In these cases, surgery IS recommended to evaluate the
menisci, assess other joint structures, and stabilize the joint. Many
surgical techniques have been described, and most reqUIre arthrot-
omy to lavage the joint, debride ren:nants of .the ruptured and
address meniscal injuries. The surgIcal technique chosen to stablhze the
stifle depends on the size of the dOl? and the surgeon's preference. In
some cases, techniques may be combmed. ...
Many extracapsular techniques described to
the lateral joint tissues to prevent cramal mohon and mmmuze
internal rotation of the tibia.
17
These techniques are used on small and
large dogs with reported clinical rates of 60?0 to
extracapsular techniques use a combmahon of capsular (Le.,
sutures placed in the lateral fibrous joint capsule) and retmacular
imbrication (i.e., sutures placed from the fabella to the tiblal crest). Many
variations in technique exist using different nun:l:ers . of sutures and
various suture placements. Fibular head transpo.slilon another com-
mon technique that stabilizes the stifle by the mserhon the
lateral collateralligament.
49
Intracapsular techruqu.es are also descnbed
and are used primarily on larger dogs. These techniques use
or synthetic grafts to replace the ruptured CrCL. The fascIa lata and
portions of the straight patellar ligament are most commonly used as
grafts in dogs.
47
. .
Newer techniques being used to treat CrCL ruptures m dogs mclude
tibial plateau leveling osteotomy and graft replacement.
The tibial plateau leveling osteotomy teclIDlque preve.n:s cramal trar:-sla-
tion of the tibia during weight bearing by osteotoIDlzmg the proxImal
tibia and rotating the tibial plateau . . Arthroscopic s;raft placement IS
silnilar to the technique often used m human patIents and uses an
arthroscope to place an intra-articular graft. Synthehc and cadaver
bone-ligament-bone grafts have been used. These techniques are
rently being evaluated; however, they have been used successfully m a
large number of patients.
HIND LIMB LAMENESS IN THE YOUNG PATIENT
109
Patellar Luxation
Medial patellar luxation is a common abnormality in toy, miniature,
and some large-breed dogs. Lateral luxation may also occur and is more
often seen in large-breed dogs.
24
Patellar luxation is usually congenital,
and although the cause has not been definitively proven, it may be
caused by abnormal hip conformation leading to displacement of the
quadriceps mechanism. Patellar luxations may also occur as a result of
traumatic injury to the medial or lateral fascia surrounding the stifle
joint after surgical repair of other stifle injuries or femoral fracture repair.
Displacement of the patella from the trochlear groove can cause pain
and may predispose the dog to rupture of the CrCL.
Clinical Signs
Initial clinical signs of patellar luxation include intermittent lame-
ness and pain. In many cases, the owners describe episodes where the
dogs carry the "limb and "skip" or "hop" for several steps. These epi-
sodes often become more frequent as the dog ages, and some owners
describe feeling a "pop" when they pick the dog up or manipulate the
hind legs. Eventually, as a result of the patellar luxation, rotational and
angular deformities begin to develop in the distal femur and proximal
tibia. Also, without the normal forces applied by the patella, the trochlear
groove becomes more shallow. In chronic cases, the trochlear ridge may
become small and irregularly shaped. It is also common for dogs with
chronic patellar luxation to be presented for a more severe acute lame-
ness caused by cruciate ligament injury. In cases of traumatic patellar
luxation, the pain and lameness are usually acute and persistent.
A grading system is used to describe the severity of the patellar
luxation. In grade I, the patella can be manually luxated using digital
pressure but reduces spontaneously when pressure is released. The dog
is rarely lame but may occasionally skip when th.e patella briefly luxates.
In grade II, the patella can be luxated manually by digital pressure or
with rotation of the tibia. The patella can then be reduced manually and
remains in place until the limb is manipulated. The dog may skip
occasionally or be persistently lame. Dogs with grade II patellar luxation
are slightly "bow-legged," and some rotation of the tibia is often present.
In grade III, the patella is luxated at the time of the examination. It can
be manipulated back into the trochlear groove but immediately relux-
ates. The degree of lameness is variable with grade III luxations but is
usually persistent. The dogs are often bow-legged, and tibial rotational,
angular, and torsional deformities are more apparent. In grade IV; the
patella is permanently luxated and cannot be reduced. The patient is
lame (may be non-weight bearing) and often stands in a crouched
stance. Angular and torsional deformities may be marked in a grade IV
luxation, and the trochlea may be absent or convex.
110 McLAUGHLIN
Diagnosis
The diagnosis of patellar luxation is made by palpation of the joint
and evaluation of patellar stability. The displaced patella may also be
observed on craniocaudal radiographs of the stifle.
Treatment
Conservative treatment consisting of restricted activity and analge-
sic medications is often prescribed for dogs with grade I luxation, partic-
ularly if the frequency of luxation is low. treatment is
recommended for dogs with more severe luxation to prevent pamful
episodes associated with luxation to help prevent t?rsional
angular changes in the femur andhbia. Surgery can realIgn the shfle
extensor apparatus and normalize the forces acting on the
and articular surfaces. Soft tissue procedures alone may be suffICIent m
mild cases; however, a combination of soft tissue and bone reconstructive
procedures is more commonly used. Several surgical techniques are used
together depending on the severity of the luxation.
Perhaps the most valuable surgical procedure performed t<;> correct
patellar luxation is a tibial crest transposition. This procedure
moving the insertion of the straight patellar tendon so as to dIrect the
pull of the quadriceps through the center of the trochlear groove. Be-
cause the patella is encased in the quadriceps at the origin of the straight
patellar tendon, realigning the quadriceps mechanism allows the patella
to remain in the trochlear groove during joint movement. To correct a
medial patellar luxation, the tibial crest is moved to a more lateral
position and reattached using wires. Anot.her
nique used to treat patellar luxation IS trochlear ThIS te.chnique
deepens the trochlear groove to improve patellar stabIlIty. A tnangular
wedge recession or rectangular recession technique is reported to deepen
the trochlear groove while preserving articular cartilage. Many other
"trochleoplasty" techniques are described; however, most do not p.re-
serve the articular cartilage. In addition to these bony reconstructIve
procedures, soft tissue imbrication techniques are often used to enhance
stability. These may include tightening the fascia surrounding the patella
with Lembert sutures or placing sutures from the fabella to the patella.
In cases of severe patellar luxation, release of contracted tissues on the
side of the luxation ("medial release") and corrective osteotomies of the
femur or tibia may be required to reduce and stabilize the patella.
DEVELOPMENTAL ORTHOPEDIC DISEASES IN DOGS
Osteochondrosis
Osteochondrosis (OC) is a generalized disturbances of endochondral
ossification.
31
Portions of the growing cartilage fail to mature into bone,
HIND LIMB LAMENESS IN THE YOUNG PATIENT 111
resulting in a thickened area of cartilage that is susceptible to injury and
necrosis. Eventually, a dissecting flap of cartilage may develop in the
articular surface (osteochondritis dissecans). Genetics, rapid growth,
overnutrition, and trauma have been implicated as causes of Oc. Al-
though it is uncommon in cats, OC is common in dogs and primarily
affects young (4-10 months of age), fast-growing, large breeds. Male
dogs are affected two to three times more often than female dogs. The
shoulder joint is the most frequently affected joint in dogs; however, OC
may also occur in the femoral condyles and in the trochlear ridges of
the tarsus (Fig. 3).31,41,60
Clinical Signs
Clinical signs of OC include lameness, joint pain, joint effusion, and
reluctance to exercise. Pain and lameness may be mild to severe and
can be intermittent. Development and progression of degenerative joint
disease can aggravate clinical signs, particularly in chronic cases.
Diagnosis
The diagnosis of OC is usually made based on clinical findings and
radiographs of the affected joint. Radiographic signs include flattening
Figure 3. Craniocaudal (A) and lateral (B) radiographic views of the stifle joint of a Great
Dane with osteochondrosis. A radiolucent defect is visible on the femoral condyle (arrows) .
112 McLAUGHLIN
of the femoral condyle or talar ridge, a defect in the subchondral bone,
joint mice, and early degenerative joint disease.
6o
Bilateral OC lesions
are observed radiographically in some cases.
Treatment
Treatment of OC can be conservative or surgical; however, results
of nonsurgical management of OC are generally unrewarding.
52
Surgery
is preferred in the early stage of the. t? speed recovery
minimize the development of degenerative Jomt dlsease.
2
Once the leslOn
is exposed, the necrotic cartilage flap is excised, and. a curette is used to
debride the defect down to subchondral bone. Exposmg the subchondral
bone allows ingrowth of mesenchymal cells and reparative fibrous or
fibrocartilaginous tissue. Arthroscopic exploration: flap removal, a.nd
curettage of the lesion may also be performed and IS a good alternative
to arthrotomy. Unfortunately, the prognosis after treatment of stifle or
tarsal OC is guarded, because intermittent joint pain and progression of
osteoarthritis occur in many cases.
52
Hypertrophic Osteodystrophy
Hypertrophic osteodystrophy (HOD) first in. the
1930s; however, the cause of the disease remams unknown. VltaIDln C
deficiency has been implicated; however, a cause-and-effect relati0!lship
has never been proven.
31
Lesions similar to HOD have been expenmen-
tally produced in dogs by feeding a free-choice diet high in protein,
calories, and calcium. Clinically, dogs with HOD frequently have a recent
history of mild gastrointestinal disease, suggesting an inflammatory or
immune-mediated cause. Bacterial infection (Escherichia coli) and canine
distemper virus have also been implicated as possible causes of HOD,
although this remains unproven,,
6
HOD typically affects young (2- 8
months old) rapidly growing dogs of large and giant Great
Danes, Chesapeake Bay Retrievers, and Irish Setters are specIfically at
risk for developing HOD, and male dogs are 2.3 times more commonly
affected than female dogs. Patients with HOD typically have open
physes radiographically.
Clinical Signs
Clinical signs of HOD include mild to severe lameness and reluc-
tance to move. Warm painful swelling is evident at the metaphyseal
regions of the long bones on physical examination. Systemic signs can
include severe anorexia, weight loss, fever, and depression.
31
Diagnosis
The diagnosis of HOD is based on clinical signs and radiographic
findings. Radiographic lesions are observed most commonly in the distal
HIND LIMB LAMENESS IN THE YOUNG PATIENT 113
radius, ulna, and tibia but are often evident in the femur as well.
The characteristic radiographic finding is a radiolucent region in the
metaphysis parallel to the physis ("double physeal line"). An irregular
widening of the physis and subperiosteal and extraperiosteal bone for-
mation may also be seen.
Treatment
Treatment for HOD consists of supportive care to prevent decubital
ulcers and maintain hydration. Nonsteroidal anti-inflammatory agents
are used to control pain. Correcting obvious dietary imbalances and
decreasing caloric intake may be beneficial in these large-
breed dogs. It is important to note that supplementation with vitamins
C and D has not been beneficial and may actually increase the risk of
dystrophic calcification. The prognosis with HOD is generally good,
because the disease is usually self-limiting. Permanent bone changes and
growth plate deformities are possible but rarely occur.
Panosteitis
The cause of panosteitis is unknown. Histologically, the disease
results in degeneration of medullary adipocytes followed by connective
tissue proliferation and intramembranous ossification.
42
Panosteitis is
one of the most common causes of lameness in young large-breed
dogs. Clinical signs typically manifest between 5 and 12 months of age,
although the disease has been reported in dogs up to 5 years of age.
Male dogs are more commonly affected than female dogs. It is frequently
diagnosed in German Shepherd Dogs (suggesting a genetic influence),
but almost all breeds can be affected.
Clinical Signs
Clinical signs of panosteitis include acute lameness, with or without
a history of trauma. A "shifting leg" lameness and lethargy are often
described by the owner. On physical examination, pain is elicited on
firm palpation of the diaphysis of the affected long boneY
Diagnosis
The diagnosis of panosteitis is based on physical examination find-
ings and radiographs. The characteristic radiographic findings include
an increased density and blurring of the trabecular pattern in the medul-
lary cavity of the long bones (Fig. 4). This is often described as patchy
and mottled radio densities in the medullary cavity, which typically
are located near the nutrient foramen. In some cases, the radiographic
appearance of panosteitis does not correlate with clinical signs. Panos-
teitis is often over-diagnosed in young dogs when another cause of
114 McLAUGHLIN
Figure 4. Lateral radiographic view of the femur of a large-breed dog with panosteitis.
Increased density is visible within the medullary cavity of the femur (arrow).
lameness cannot be confirmed. It is important to remember that panos-
teitis often occurs concurrently with other causes of lameness in young
dogs, including hip dysplasia.
Treatment
Panosteitis is a self-limiting disease, and no specific therapy exists.
Restricted activity and analgesic medications are usually prescribed. The
prognosis is excellent, although the lameness may shift to other limbs,
and some dogs may be intermittently lame for 6 to 18 months.
HIND LIMB FRACTURES UNIQUE TO IMMATURE
ANIMALS
Fractures of the Proximal Femoral Physis
Fracture of the proximal femoral physis is common in immature
dogs and is often termed capital physeal fracture or slipped capital epiphy-
HIND LIMB LAMENESS IN THE YOUNG PATIENT 115
s i s : ~ 6 These are typically Salter-Harris type I or II fractures.
45
The proxi-
mal femoral growth plate normally begins to close at approximately 6
to 11 months of age in dogs. The average age of dogs with fractures of
the physis is 5.6 months.
56
Clinical Signs
Most dogs present with a history of trauma and clinical signs of
hip pain and lameness. Crepitus may be palpable on manipulation of
the joint.
Diagnosis
Diagnosis of a slipped capital physis is based on radiographic
evaluation of the affected hip joint (Fig. 5) . Lateral, ventrodorsal hip-
extended, and ventrodorsal frog-legged radiographic views should be
obtained. Significant displacement of the epiphysis is evident in many
cases and is easily identified radiographically. In some cases, however,
only minor displacement is seen radiographically, and careful evaluation
of the films is required to reach a diagnosis. In cases that initially go
undiagnosed, later radiographic evaluation may reveal narrowing of the
femoral neck, early degenerative joint disease, and malformation of the
femoral head.
Treatment
External coaptation is ineffective at stabilizing capital fractures, and
internal fracture fixation is recommended.
56
In smaller dogs or dogs with
Figure 5. Craniocaudal radiographic view of the coxofemoral jOints of an immature dog
with a fracture of the right proximal femoral growth plate (Salter-Harris type I fracture) .
Displacement of femoral epiphysis is visible.
116 McLAUGHLIN
radiographic evidence of severe trauma to the epiphysis, a femoral head
and neck ostectomy may be performed. In larger dogs, however, internal
fixation of the fracture is recommended to accurately reduce the fracture,
provide rigid fixation, and allow return to j.o.int Several
surgical techniques have descnbed to. stabIlIze capItal fractures,
including placement of multIple smooth prns or screws through the
femoral neck into the epiphysis and retrograde placement of pins or
screws from the articular surface.
3
, 4, 11, 21, 27, 30, 39, 54, 55, 59 Implants placed
from the articular surface are countersunk below the cartilage to prevent
further cartilage damage.
3o
Controversy exists as to which methods are
best, and each technique has advantages and disadvantages. Smooth
pins may provide while allowing contin.ued ?f the
physis. Some surgeons belIeve that physeal growth IS already lImIted as
a result of the trauma and prefer to achieve rigid fixation through the
use of screws. 30, 56 Retrograde implant placement causes greater damage
to the articular cartilage but may allow more anatomic reduction. Unfor-
tunately, no matter which stabilization technique is used, complications
are common after repair of proximal femoral physeal fractures. These
complications include poor reduction, implant failure, femoral neck nar-
rowing or lysiS, premature closure of the physis resulting in subluxation
of the femoral head, avascular necrosis of the femoral head, iatrogenic
fracture of the femoral neck, degenerative joint disease, articular carti-
lage damage from implants, and coxofemoral luxation.
21
, 39, 56 Dogs
younger than 4 to 6 months of a.ge .the the fracture occurs ha.ve
a higher incidence of degenerative Jornt dIsease than older dogs WIth
capital fractures.
56
When complications occur, femoral head and neck
ostectomy may be necessary to establish pain-free hip function. If the
dog is skeletally mature, total hip arthroplasty may be performed.
Fracture of the Distal Femoral Physis
Fractures of the distal femoral growth plate are common in imma-
ture dogs and are typically Salter-Harris type I or II fractures.
Clinical Signs
Dogs with fractures of the distal femoral physis typically are pre-
sented with a history of trauma and clinical signs of swelling, crepitus,
and pain in the distal femur. Most are initially non-weight bearing
although some dogs bear some weight on the limb, particularly if the
injury is several days old.
Diagnosis
The diagnosis of distal femoral physeal fractures can be made from
radiographs of the femur. The epiphysis is generally displaced cauda:lly
and proximally by the caudal thigh muscles. A craniocaudal radio-
HIND LIMB LAMENESS IN THE YOUNG PATIENT
117
graphic view is helpful to confirm the type of growth plate fracture
present and to rule out articular fractures.
Treatment
. External is usually ineffective, because the epiphysis is
dIsplaced by ItS muscular attachments. Inten1al fixation allows better
anatomic reduction and implant placement to provide stability to the
23, Several methods of stabilizing the fractures have been
rncludrng.a single intramedullary pin, cross pins, smooth pins
placed. rn Rush and parallel smooth pins.
19
, 23, 53 In most cases,
these lffiplants are .rnserted . within the stifle joint and placed
.the non-:weight-bearmg Jomt surface. The prognosis after inter-
nal of dIstal plate fracture is good, although
such as malalIgnment, Implant failure, nonunion, quadri-
ceps be-down, and patellar luxation have been reported. 23
Avulsion Fractllres of the Tibial Tuberosity
The growth plate for the tibial tuberosity normally closes at 6 to 11
of age in dogs. Separation of the growth plate may occur in
Immature when they. are under 10 months of age, as a
result of sbfle hyperflexlOn. The avulSIOn may occur bilaterally.
Clinical Signs
sii?ns of a tibial crest avulsion vary with the chronicity of
the ImtIally, the dogs are often non-weight bearing. Pain and
swellrng are eVIdent the proxir,nal tibia. Shortly after injury, how-
ever, dogs bear weIght on the 11mb but may assume a characteristic
if the injury is bilateral. Dogs with avul-
SIon of the tibIal tuberoSIty tend to walk with a shuffling hind limb gait
and seem reluctant to flex the stifle joints.
Diagnosis
diagnosis of an avulsion fracture of the tibial tuberosity is based
on (FIg. 6). The growth plate may seem wider than ex-
or m severe cases, the tuberosity may be significantly
dIsplaced proXImally by the pull of the quadriceps muscles. The patella
may also be located more proximally in the trochlear O'roove. It is
important to both stifle joints to identify injuries or
to allow companson WIth the contralateral normal tibia.
Treatment
coaptation confinement may be successful in treating
avulSIOn fractures of the bbial tuberoSIty when displacement is minimal
118 McLAUGHLIN
Figure 6. Lateral radiographic view of the stifle of a young dog with an avulsion fracture of
tibial tuberosity. The tuberosity is displaced proximally.
3 mm) and in chronic cases when some healing is evident radiographi-
cally. Internal fixation is recommended in other cases. The stifle is ex-
tended, and traction is applied to the patellar ligament to fatigue the
quadriceps muscles and reduce the displaced fragment. Care is taken to
avoid traumatizing the zone of dividing cartilage cells. A tension band
wire is the preferred method of fixation. Two Kirschner wires or a
cancellous bone screw and a Kirschner wire may be used if the fragment
is of sufficient size. A ligament-bone suture technique is useful for
reattaching smaller fragments.
Postoperative complications after repair of tibial tuberosity fractures
are related to implant failure or subsequent growth abnormalities in
the tibia.
22
Pin bending and migration, wire breakage, avulsion of the
tuberosity from the implants, and patellar luxation have been reported.
Flattening and distal translocation of the tibial tuberosity may occur
after fixation but is reported to cause minimal loss of function. In
immature animals, the fixation device should be removed as soon as
healing is complete to avoid premature closure of the growth center and
HIND LIMB LAMENESS IN THE YOUNG PATIENT 119
malformation of the proximal tibia. The prognosis for limb function after
repair is good to excellent if the condition is treated early and anatomic
reduction and rigid fixation are achieved.
Avulsion Fracture of the Calcaneus
The common calcanean tendon (Achilles tendon) inserts on the
calcaneus and is composed of the gastrocnemius tendon, the superficial
digital flexor (SDF) tendon, and the common tendon of the biceps
femoris, semitendinosus, and gracilis muscles. Avulsion fractures of the
apophysis of the calcaneus occur infrequently in immature dogs.
Clinical Signs
Avulsion fractures of the calcaneal apophysis result in acute pain,
swelling of the proximal calcaneal region, and non-weight-bearing lame-
ness. The resultant dysfunction of the Achilles mechanism allows the
hock joint to be flexed while the stifle is in full extension.
Diagnosis
Radiographic findings after avulsion fracture of the calcaneus in-
clude widening of the growth plate or complete proximal displacement
of the apophysis (Fig. 7). Marked soft tissue swelling is generally appar-
ent surrounding the proximal calcaneous and distal Achilles tendon.
Treatment
Surgical stabilization of the fracture is required to regain function,
particularly if displacement is severe. A lateral paramedian approach is
used, and the SDF tendon is reflected to expose the fracture site. A
tension band fixation or lag screw fixation is used most commonly. The
limb is bandaged after surgery, and activity is restricted for 6 weeks to
allow healing.
Tendon Injuries: Superficial Digital Flexor Tendon
Luxation
The SDF tendon originates on the lateral fabella of the stifle joint,
courses distally along with the gastrocnemius muscle, and crosses over
the proximal end of the calcarleus before inserting on the digits. It forms
a fibrocartilaginous cap over the tip of the calcaneus, and a synovial
bursa is present between the tip of the calcaneus and the SDF tendon.
The SDF tendon is stabilized as it courses over the calcaneus by a medial
and a lateral retinaculum. Rupture of the medial or lateral retinaculum,
likely a result of trauma, allows the tendon to luxate. The medial retinac-
120 McLAUGHLIN
Figure 7. Lateral radiographic view of the tarsal joint of a young dog with an avulsion
fracture of the calcaneous. Proximal displacement of the apophysis is evident.
ulum is the smaller and weaker of the two; thus, lateral luxation is
significantly more common in dogs. Luxation of the SDF tendon is most
commonly reported in Shelties and Collies.
Clinical Signs
Clinical signs of SDF tendon luxation may include a mild intermit-
tent lameness and swelling near the tip of the calcaneus. Owners occa-
sionally report hearing a popping sound associated with the dog's
lameness.
Diagnosis
Luxation of the tendon may be palpated over the calcaneus and is
generally induced by internal and external rotation of the tarsus with
the joint in extension. Radiographic evaluation of dogs with SDF tendon
luxation may reveal soft tissue swelling and abnormal morphology of
the proximal calcaneus. The calcaneus is often slender, and the calcaneal
groove seems shallow. The tip of the calcaneus is often slanted distolater-
ally, which may predispose to luxation.
HIND LIMB LAMENESS IN THE YOUNG PATIENT 121
Treatment
Stabilization of the tendon using external coaptation is often unre-
warding. Surgical stabilization is indicated and consists of replacing the
tendon in the calcaneal groove and imbricating the torn retinaculum.
Nonabsorbable suture material has been recommended, and a splint or
padded bandage is applied for 4 weeks after surgery. The prognosis
after surgical repair of an SDF tendon luxation is good, although luxation
of the contralateral SDF tendon may occur.
SUMMARY
Hind limb lameness is seen frequently in young dogs and may
result from congenital abnormalities, traumatic injuries, or develop-
mental diseases. An understanding of the patient's history, a good physi-
cal and radiographic evaluation, and sound knowledge of the common
diseases affecting immature dogs permit early diagnosis and successful
treatment in most cases.
References
1. Aiken SW, Kass PH, Toombs JP: Intercondylar notch width in dogs with and without
cranial cruciate ligament injuries. Vet Comp Orthop Traumatol 8:128-132, 1995
2. Beale BS, Goring RL, Herrington J, et ale A prospective evaluation of four surgical
approaches to the talus of the dog used in the treatment of osteochondritis dissecans.
J Am Anim Hosp Assoc 27:221-229, 1991
3. Belkoff SM, Millis DL, Probst CWo Biomechanical comparison of three internal fixations
for treatment of slipped capital femoral epiphysis in immature dogs. Am J Vet Res
53:2136-2140, 1992
4. Belkoff SM, Millis DL, Probst CWo Biomechanical comparison of I-screw and 2-
divergent pin internal fixations for treatment of slipped capital femoral epiphysis,
using specimens obtained from immature dogs. Am J Vet Res 54:1770- 1773, 1993
5. Berzon JL, Howard PE, Covell Sf, et ale A retrospective study of the efficacy of femoral
head and neck excisions in 94 dogs and cats. Vet Surg 9:88-92, 1980
6. Bruer GJ, Spaulding KA, Braden TD. Osteochondritis dissecans of the medial trochlear
ridge of the talus in the dog. Vet Comp Orthop Traumatol 4:168- 176, 1989
7. Budsberg SC, Johnston SA, Schwarz PD, et ale Efficacy of etodolac for the treatment
of osteoarthritis of the hip joints in dogs. JAVMA 214:206-210, 1999
8. Canapp SO, McLaughlin RM, Hoskinson n, et al: Scintigraphic evaluation of glucos-
amiTle hydrochloride and chondroitin sulfate as treatments for acute synovitis in dogs.
Am J Vet Res 60:1550- 1556, 1999
9. Corley EA: Role of the Orthopedic Foundation for Animals in the control of carline
hip dysplasia. Vet Clin North Am Small Anim Pract 22:579-593, 1992
10. Corley EA, Hogan PM: Trends in hip dysplasia control: Analysis of radiographs
submitted to the Orthopedic Foundation for Animals, 1974-1984. JAVMA 187:805-
809,1985
11. DeCamp CE, Probst CW, Thomas MW: Internal fixation of femoral capital physeal
injuries in dogs: 40 cases (1979-1987). JAVMA 194:1750-1754, 1989
12. De Haan n, Goring R, Beale BS: Evaluation of polysulfated glycosaminoglycan for the
treatment of hip dysplasia in dogs. Vet Surg 23:177-181,1994
122 McLAUGHLIN
13. Douglas SW, Williamson HD: Veterinary Radiological Interpretation. Philadelphia,
Lea & 1970
14. Duval JM, Budsberg SC, Flo GL, et al: Breed, sex, and body weight as risk factors for
rupture of the cranial cruciate ligament in youn? dogs. JAVMA 215:811-814, 1999
15. Farese JP, Lust G, Williams AI, et al: Companson of of dorsolateral
subluxation of the femoral head and maximal passive laxity for evaluation of the
coxofemoral joint in dogs. Am J Vet Res 60:1571-1576, 1999
16. Farese JP, Todhunter RJ, Lust G, et al: Dorsolateral subluxation of hip joints in dogs
measured in a weight-bearing position with radiography and computed tomography.
Vet Surg 27:393-405, 1998 . .. . . .
17. Flo G: Modification of the lateral retinacular unbncatIon technIque for the surg:tcal
correction of anterior cruciate ligament rupture in the dog. J Am Anim Hosp Assoc
11:570-576, 1975
18. Fox SM, Johnston SA: Use of carprofen for the treatment of pain and inflammation in
dogs. JAVMA 210:1493-1498, 1997 ..... .
19. Franczuszki D, Chalman JA, Butler HC: . The use of parred pms m the fixation of dIstal
femur fractures in the dog and cat. JAm Anim Hosp Assoc 22:173-178, 1986
20. Gendreau C, Cawley AJ: Excision of the femoral head and neck: The long-term results
of 35 operations. J Am Anim Hosp Assoc 1977 .
21. Gibson KL, van Ee RT, Pechman RD: Femoral capItal physeal fractures m dogs: 34
cases (1979-1989). JAVMA 198:886-890, 1991
22. Goldsmith S, Johnson KA: Complications of canine tibial tuberosity avulsion fractures.
Vet Comp Orthop Traumatol 4:54-58, 1991
23. Hardie EM, Chambers IN: Factors influencing the outcome of distal femoral physeal
fracture fixation: A retrospective study. J Am Anim Hosp Assoc 20:927-931, 1984
24. Hayes AG, Boudrieau RJ, Hungerford LL: Frequency and distribution of medial and
lateral patellar luxation in dogs: 124 cases (1982-1992). JAVMA 205:716-720, 1994
25. Heyman SJ, Smith GK, Cofone MA: Biomechanical study of the effect of coxofemoral
positioning on passive hip joint in dogs. Am JVet Res 54:21?-215, 1993 .
26. Hosgood G, Lewis DD: RetrospectIve evaluation of fixatIon comphcations of 49 pelVIC
osteotomies in 36 dogs. J Small Anim Pract 34:123-130, 1993
27. Hulse DH, Wilson JW, Butler HC: Use of the lag screw principle for stabilization
of femoral neck and femoral capital epiphyseal fractures. J Am Anim Hosp Assoc
10:29-36, 1974 .
28. Johnston SA, Fox SM: Mechanisms of actions of anti-inflammatory medications used
for the treatment of osteoarthritis. JAVMA 210:1486-1492, 1997
29. Johnston SA, Budsberg SC: Nonsteroidal anti-inflammatory drugs and corticosteroids
for the management of canine osteoarthritis. Vet Clin North Am Small Anim Pract
27:841-862, 1997
30. Kuzma A, Sumner-Smith G, Miller C, et al: A technique of repair of femoral capital
epiphyseal fractures in the dog. J Small Anim Pract 30:444-448, 1989
31. Lewis DD, McCarthy RJ, Pechman RD: Diagnosis of common developmental orthope-
dic conditions in caninie pediatric patients. Compend Contin Educ Pract Vet 14:287-
301, 1992
32. Lippiello L, Idouraine A, McNamara PS, et al: Cartilage stimulatory and antiproteolytic
activity is present in sera of dogs treated with a chondroprotectIve agent. Carlffie Pract
24:18-19,1999
33. Lust G, Geary JC, Sheffy BE: Development of hip dysplasia in dogs. Am J Vet Res
34:87-91, 1973
34. Lust G, Williams MS, Burton-Wurster N, et al: Effects of intramuscular administration
of glycosaminoglycan polysulfates on signs of incipient hip dysplasia in growing pups.
Am J Vet Res 53:1836-1843, 1992
35. Lust G, Williams AJ, Burton-Wurster N, et al: Joint laxity and its association with hip
dysplasia in Labrador Retrievers. Am J Vet Res 54:1990-1999, 1993 .
36. McLaughlin RM, Miller CW: Evaluation of hip joint congruence and range of motion
before and after triple pelvic osteotomy. Vet Comp Orthop TraumatoI4:65-69, 1991 .
37. McLaughlin RM, Miller CW, Taves CL, et al: Force plate analYSIS of trIple pelVIC
osteotomy for the treatment of canine hip dysplasia. Vet Surg 20:291-297, 1991
HIND LIMB LAMENESS IN THE YOUNG PATIENT 123
38. 'McNamara PS, Johnston SA, Todhunter RJ: Slow-acting disease-modifying osteoarthri-
tis agents. Vet Clin North Am Small Arum Pract 27:863-881, 1997
39. Miller A, Anderson n: Complications of articular lag screw fixation of femoral capital
epiphyseal separations. J Small Anim Pract 34:9-12, 1993
40. Millis DL, Levine 0: The role of exercise and physical modalities in the treatment of
osteoarthritis. Vet Clin North Am Small Anim Pract 27:913-930, 1997
41. Montgomery RD, Hathcock JT, Milton JL, et al: Osteochondritis dissecans of the canine
tarsal joint. Compend Contin Educ Pract Vet 16:835-845, 1994
42. Muir P, Dubeilzig RR, Johnson KA: Panosteitis. Compend Cantin Educ Pract Vet
18:29-33, 1996
43. Olmstead ML, Hohn RB, Turner TM: A five-year study of 221 total hip replacements
in the dog. JAVMA 183:191-194, 1983
44. Riser WH: Canine hip dysplasia: Cause and controL JAVMA 165:360--362, 1974
45. Salter RB, Harris WR: Injuries involving the epiphyseal plate. J Bone Joint Surg Am
45:587-622, 1963
46. Schulz KS, Payne JT, Aronson E: Escherichia coli bacteremia associated with hypertro-
phic osteodystrophy in a dog. JAVMA 199:1170-1173, 1991
47. Shires PK, Hulse DA, Liu W: The under-and-over fascial replacement technique for
anterior cruciate ligament rupture in dogs: A retrospective study. J Am Anim Hosp
Assoc 20:69-77, 1984
48. Slocum B, Devine T: Pelvic osteotomy technique for axial rotation of the acetabular
segment in dogs. J Am Anim Hosp Assoc 22:331-338, 1986
49. Smith GK, Torg JS: Fibular head transposition for repair of cruciate-deficient stifle in
the dog. JAVMA 187:375-383, 1985
50. Smith GK, Biery DN, Gregor TP: New concepts of coxofemoral joint stability and the
development of a clinical stress-radiographic method for quantitating hip joint laxity
in the dog. JAVMA 196:59-70, 1990
51. Smith GK, Gregor TP, Rhodes WH, et al: Coxofemoral joint laxity from distraction
radiography and its contemporaneous and prospective correlation with laxity, subjec-
tive score, and evidence of degenerative joint disease from conventional hip-extended
radiography in dogs. Am J Vet Res 54:1021-1042, 1993
52. Smith MM, Vasseur PB, Morgan JP: Clinical evaluation of dogs after surgical and
nonsurgical management of osteochondritis dissecans of the talus. JAVMA 187:31-35,
1985 .
53. Stone EA, Betts CW, Rowland GN: Effects of Rush pins on the distal femoral growth
plate of young dogs. Am J Vet Res 42:261-265, 1981
54. Tillson DM, Roush JK, McLaughlin RM, et al: Biomechanical comparison of three
repair methods for proximal femoral physeal fractures in shear and tension. Vet Comp
Orthop Traumatol 7:136-139, 1994
55. Tillson DM, McLaughlin RM, Roush JK: Evaluation of experimental proximal femoral
physeal fractures repaired with two cortical screws placed from the articular surface.
Vet Comp Orthop Traumatol 7:140--147, 1994
56. Tillson DM, McLaughlin RM, Roush JK: Fractures of the proximal femoral physis in
dogs. Compend Contin Educ Pract Vet 18:1164-1181, 1996
57. Vasseur PB: Clinical results following nonoperative management for rupture of the
cranial cruciate ligament in dogs. Vet Surg 13:242-246, 1984
58. Vasseur PB, Johnson AL, Budsberg Sc, et al: Randomized, controlled trial of the
efficacy of carprofen, a nonsteroidal anti-inflammatory dnlg on the treatment of osteo-
arthritis in dogs. JAVMA 206:807-811, 1995 .
59. Ward WT, Stefko I, Wood KB, et al: Fixation with a single screw for slipped capital
femoral epiphysis. J Bone Joint Surg Am 74:799-809, 1992
60. Wisner ER, Berry CR, Morgan JP, et al: Osteochondrosis of the lateral trochlear ridge
of the talus in seven Rottweiler dogs. Vet Surg 19:435-439, 1990
Address reprint requests to
Ron M. McLaughlin, DVM, DVSc
The Animal Health Center
College of Veterinary Medicine
Mississippi State University
Wise Center
Mississippi State, MS 39762
LAMENESS 0195-5616 / 01 $15.00 + .00
HIND LIMB LAMENESS IN THE
MATURE DOG
James K. Roush, DVM, MS
Hind limb lamenesses in the adult dog are most likely the result of
trauma, chronic degenerative joint disease from a variety of causes, or
neoplasia, with the prevalence of a few common infectious or mycotic
diseases such a..s blastomycosis, ehrlichiosis, or borreliosis rising or de-
clining on the differential list based on the geographic location of the
animal. Beyond all other causes of hind limb lameness described in this
article, however, the most important recommendation to be garnered is
that all hind limb lameness in adult pet or working dogs should be
initially ascribed to cranial cruciate ligament rupture; hind limb lame-
nesses in large adult dogs are cranial cruciate ligament ruptures until
proven otherwise. Although cruciate gameI\t disease is the most com-
mon single cause of hind limb in the adult animal, it is the
opinion of the author that it is also the most commonly missed diagnosis
by small or mixed animal veterinary practitioners. As discussed later,
cruciate ligament disease, particularly partial cranial cruciate rupture,
can be difficult to diagnose, and lamenesses that are the reslllt of cranial
cruciate rupture can be easily but wrongly attributed to preexisting hip
dysplasia or other chronic degenerative diseases.
EXAMINATION FOR HIND LIMB LAMENESS
Signalment and history data are critically important for correct
identification of the cause of most hind limb lamenesses and should be
carefully gathered. Signalment considerations can result in early nar-
From the Section of Small Animal Surgery, Department of Clinical Sciences, College of
Veterinary Medicine, Kansas State University, Manhattan, Kansas
VETERINARY CLINICS OF NORTH AMERICA: SMALL ANIMAL PRACTICE
VOLUME 31 NUMBER I JANUARY 2001 125
126 ROUSH
rowing of differential possibilities for lameness, and complete elimina-
tion of some causes can be made on the basis of signalment alone. For
example, although hip dysplasia can, almost without exception, be ruled
out as the cause of hind limb lameness in the adult Toy Poodle, aseptic
femoral head necrosis must remain in the differential list until specifi-
cally eliminated. When gathering historical data, the onset, duration,
and progression of clinical lameness; presence or absence of possible
traumatic episodes; and familial history of the dog are primary consider-
ations. Clinical histories of traumatic wounds, acute and severe lame-
ness, or other links to traumatic origin lead to differential diagnoses
consisting largely of trauma-related diseases. Clinical histories of slow-
onset and progressive lamenesses lead the veterinarian toward diagnoses
related to osteoarthritis or neoplasia. Familial history may be useful to
help determine the likelihood of congenital disease manifestations such
as patellar luxation or hip dysplasia, which are obviously more likely to
occur in siblings or if one or both parents were affected by the disease.
Many orthopedic diseases of small animals have conformational or
hereditary origins, and the addition of several recent diseases such as
aseptic necrosis of the femoral head to the list of those with autosomal
recessive or incomplete dominant heritability keeps this list increasing.
One should begin examination of the lame dog by observing the
animal at a walk or trot. For evaluation of hind limb lameness, it is most
useful to observe the animal moving away on a straight line. The lame
limb is determined by observing which leg is held away or further
from the center of gravity (or vertical midline of the dog). Abnormal
movements useful for the evaluation of equine lameness such as "hip-
hikes" are generally not useful aids in diagnosing lameness in the dog,
because the differing hair coat length and gait of the various dog
breeds make determining such movements difficult. Because a common
lameness grading scale has not been widely accepted in small animal
breeds, lamenesses should be described as fully weight-bearing, partially
weight-bearing, or non-weight-bearing lameness. Useful additions to
visual observation of weight bearing include determination of muscle
atrophy by comparison with the opposite limb, visual observation of
discrete regions of swelling, and observation of the gait from the side
for assessment of decreased range of motion at one or more joints.
Although not absolutely characteristic for joint pain, decreased range of
motion at one or more joints may aid the veterinarian in early localiza-
tion of the painful region on the limb.
Early in the examination, neurologic causes of hind limb lameness
should be differentiated from orthopedic causes in the mature dog. The
author accomplishes this differentiation by assessing proprioception in
the hind limb and assessing the presence or absence of back pain on
palpation. If pain on spinal palpation is not elicited and hind limb
proprioception is normal, all but the most subtle lamenesses can be
eliminated as having neurologic causes. Obviously if hill.d limb proprio-
ception is delayed or absent, or if pain is elicited on spinal manipulation,
1
I
I
HIND LIMB LAMENESS IN THE MATURE DOG 127
ne'urologic causes of hind limb lameness should be moved to the top
of the differential list, and diagnosis proceeds on the basis of those
eventualities. In the adult dog, only claudication from nerve root im-
pingement secondary to lumbosacral disease is likely to cause lameness
without accompanying peripheral neurologic abnormalities.
Determination of the region and likely cause of hind limb lameness
in dogs occurs most often by careful and systematic palpation of the
affected limb, with frequent comparison with the other presumably
normal limb. There is no generally accepted set pattern of hind limb
palpation, but the author prefers to begin at the toes of the affected hind
limb and move toward the body trunk. During examination of the hind
limb, each bone should receive individual palpation over the bone's
entire length while observing the animal for elicitation of pain, and each
joint should be carefully palpated for joint effusion, frictionless range of
motion, elicitation of pain on motion, and collateral stability. Often, the
only physical finding in slowly progressive mild lameness is the pres-
ence of joint effusion, which serves to localize the lameness. Careful
observation of joint effusion and areas of muscle atrophy are two widely
overlooked physical parameters that may help to localize and aid in the
diagnosis of many subtle lamenesses. Firm sequential flexion of the
more mobile joints and observation of locomotion after each joint is
flexed may help to localize pain to a specific joint. Once the limb has
been examined and the animal has been observed for signs of localized
pain, many examinations benefit from sedation of the dog, which allows
further joint manipulation without resistance. In the author's practice,
most hind limb manipulative tests and radiographs are performed with
the animal sedated with acepromazine (0.05 mg/ kg intravenously) and
oxymorphone (0.05 mg/ kg intravenously).
SPECIFIC DIAGNOSTIC TESTS
There are several described and named "special" manipulations for
hind limb lameness as a result of stifle disease. The "drawer" test is
used to determine cruciate ligament stability. For proper performance of
the drawer test, the examiner should place the thumb of one hand on
-the lateral fabella and the index finger over the patella. The thumb of
the other hand is placed on the fibular head with the index finger placed
on the tibial crest. An attempt is then made to move the tibia cranially
(positive cranial drawer) or caudally relative (positive caudal drawer)
relative to the femur. For inexperienced examiners, part"icularly in unse-
dated animals, any amount of elicited drawer movement is likely a
positive indication of cruciate rupture. Of particular usefulness for aid-
ing in the proper diagnosis of cranial cruciate ligament rupture is palpa-
tion for and the finding of a "medial buttress" (Fig. 1). This is a firm
swelling present in the region of the medial collateral stifle ligament,
which arises within hours of cranial cruciate or partial cruciate ligament
128 ROUSH
Figure 1. Caudal view of the stifles of a dog with a bilateral medial buttress.
rupture. The swelling can be more easily discovered by simultaneous
palpation of the region on both limbs while the animal is still standing.
A medial buttress finding is pathopneumonic for cranial cruciate rup-
ture; even in the absence of palpable cranial drawer, it is an indication
for stifle arthrotomy or arthroscopy and direct assessment of the cruciate
ligament continuity. A third method of diagnosis of cranial cruciate
rupture involves the "tibial thrust" manipulation. In this test, the index
finger of one hand is extended from the patella along the patella tendon
to the tibial crest. With the other hand, the hock is flexed until tension
of the common calcanean tendon is achieved. If the cranial cruciate
ligament is ruptured, the tensed gastrocnemius muscle pushes the tibia
forward in relation to the femur, which is palpable by movement of the
index finger along the patella tendon.
For patients in which history and signalment findings lean toward
the diagnosis of patella luxation, direct palpation of the patella is the
most likely aid to diagnosis.
3
For grade 1 and 2 patella luxations, medial
pressure is put on the patella during internal rotation of the tibia to
confirm medial luxation, or lateral pressure is placed on the patella
during external tibia rotation to confirm lateral luxation. In obese pa-
tients or chondrodystrophic dogs, where the patella can be difficult to
HIND LIMB LAMENESS IN THE MATURE DOG 129
palpate, one often finds that the patella tendon can be located at its
insertion on the tibial crest, and palpation of the direction of the tendon
can result in a diagnosis of patella luxation to the medial or lateral
femoral condylar surface.
There are also special manipulations that can aid in the diagnosis
of lameness caused by hip disease. The Ortolani sign is a described test
where a lax hip is first subluxated by pressure on the stifle toward the
hip and then slow abduction of the hip until relocation of the femoral
head into the acetabulum occurs.
1
As a method of diagnosis of hip
dysplasia, it is less useful in the adult animal, because the bone changes
of secondary osteoarthritis often result in diminution or elimination of
palpable hip laxity. For diagnosis of hip luxation, the "thumb" test or
"triangle" test is most often diagnostic. The thumb test is performed by
placing the thumb of one hand between the greater trochanter and
ischiatic tuberosity and rotating the femur internally and externally with
the other hand. In an intact hip, the greater trochanter displaces the
thumb from this area during rotation; the greater trochanter does not
displace the thumb if the hip is luxated. Placing a digit of one hand
simultaneously on the ischiatic tuberosity, greater trochanter, and dorsal
ilial wing performs the triangle test. If the resulting three points form a
triangle, the hip is normal, but if a straight line is formed, the hip is
likely luxated dorsally.
Ancillary diagnostic techniques useful in the diagnosis of hind limb
lamenesses include survey radiography of the affected joint or bone,
stress radiography of an affected joint, nuclear scintigraphy, computer-
ized tomography, and joint arthrocentesis and synovial fluid analysis. Of
these, nuclear scintigraphy is the most useful technique for determining
increased blood flow (inflammation) or increased bone hlrnover to help
localize and diagnose lesions in dogs where physical examination has
failed to localize the lesion. Computerized tomography is often limited
in availability to large or specialty practices and is most useful in the
diagnosis of traumatic or degenerative lesions of the tarsus. A useful
technique that is not often performed in small animal examination is the
intra-articular injection of local analgesics to aid in localization of lame-
ness or elimination of pain in a specific joint.
FRACTURES OF THE HIND LIMB
Of the diseases causing hind limb lameness in the dog, fracture of
one or more long bones is likely the easiest to diagnose and carries the
best prognosis after treatment. Hind limb fractures present as acute,
partial, or non-weight-bearing lamenesses often associated with a his-
tory of trauma, particularly vehicular trauma. Presenting signs include
pain or crepitation elicited during palpation of the affected long bone,
malangulation of the limb, and swelling of the limb. Survey orthogonal
radiographs of the suspected fracture are essential to confirm the fracture
and to establish the configuration and comminution of the fracture so
130 ROUSH
as ' to allow proper preoperative plarming. Additional diagnostic tools
are usually not necessary, although scintigraphy may aid in the diagnosis
of nondisplaced or stress-origin long bone fractures, and computed
tomography may be useful for fractures involving the tarsal bones. Most
long bone fractures in the hind limb are best repaired using established
orthopedic principles of anatomic reduction, rigid fixation, and early
return to function. Methods for selection of fracture fixation appliances
and optimum fracture management have been thoroughly described.
4
Internal fixation of long bone fractures is best accomplished by experic
enced surgeons and should not be attempted unless the veterinarian is
familiar with and has available the chosen method of repair and alterna-
tive repair methods. Open fractures should be treated as emergencies,
and proper debridement, lavage, al{d fixation should occur immediately.
Fractures involving articular surfaces should be carefully reduced to
minimize subsequent degenerative joint disease.
For the individual long bones of the hind limb, several surgical
options are generally available. Fractures the articular
of the hind limb bones or the metaphyseal regIons are usually repaIred
using lag screws, K-wires, or some combination of these. Diaphyseal
fractures of the femur are repaired with intramedullary pins, interlocking
nails, external skeletal fixation (type I or quadrilateral), bone plates, or
a combination of any of these. Caution should be used in repairing
diaphyseal femoral fractures with single intramedullary pins, because
these allow rotation at the fracture site and are the single most common
repair to result in nonunion of the femur. Diaphyseal fractures of the
tibia may be repaired with intramedullary pins, interlocking nails, exter-
nal skeletal fixation (type I, II, or III), circular ring fixation, or bone
plates. Fractures of the tarsal bones are often repaired with small lag
screws. The surgical approaches for tarsal fractures often require special-
ized knowledge and experience, and the repairs are difficult and best
left in the hands of specialists. Fractures of the metatarsals may be
repaired with intramedullary pins introduced through holes made in the
metaphyseal regions of these bones or with small bone plates. Fractures
of the phalanges may be repaired with small bone plates; however, in
the event of fractures of the second and fifth digits, these digits may be
amputated without affecting gait. Minimally displaced fractures involv-
ing the tibia, tarsal bones, or metatarsals may be casted. External coapta-
tion devices popular in earlier veterinary practice such as the Thomas
splint are detrimental to distal limb joints and should not be used under
any circumstances in modern practice.
JOINT LUXATION AND INSTABILITY
Like fractures, luxations or instabilities of the hind limb joints are
often relatively simple to diagnose, and the accepted treatments are well
described. Dogs are presented with acute, partial, or non-weight-bearing
lamenesses often associated with a history of trauma. Presenting signs
HIND LIMB LAMENESS IN THE MATURE DOG 131
include pain or crepitation elicited during palpation of the joint, malan-
gulation of the limb, and swelling of the affected joint. For the stifle and
tarsus, particular attention should be given to ascertain the mediolateral
stability and the craniocaudal stability of the joint to assess the status of
the collateral ligaments of these joints. Survey orthogonal radiographs
of the affected joint can confirm complete luxation, but additional stress
radiographs may be necessary to confirm the trauma and ligaments
injured for unstable joints. Additional diagnostic tools are usually not
necessary. Luxated hip joints that are reduced before extensive damage
occurs to the femoral articular surface carry a good prognosis.
Dogs presented with traumatic luxations of the hip joint do not bear
weight on the affected limb and hold the limb in an externally rotated
and adducted position. Survey orthogonal radiographs should be per-
formed in all cases of traumatic hip luxation, not because they are
necessary to establish the diagnosis but because of their importance to
eliminate fractures of the acetabulum or avulsion fractures of the femoral
head as complicating factors and because of the necessity to eliminate
hip dysplasia as a secondary contributor to the luxation. Closed reduc-
tion may be attempted in all cases where no complicating factors are
present and is particularly useful if the luxation is several hours or less
in duration. If the hip is not easily reluxated on manipulation after
reduction, the prognosis for healing and return to full function of the
limb is good. Most closed reductions that fail do so because of preex-
isting hip dysplasia in the joint. Classically, the limb is placed in an
Ehmer sling after closed reduction for 10 to 14 days, but in the author's
experience, similar results are likely if the animal is merely placed in
cage rest for the necessary 10 to 14 days to allow for formation of a
fibrous joint capsule. Postreduction radiographs should be taken to
confirm reduction, and repeat radiographs are taken at the end of con-
finement to assess reduction before normal activities are resumed.
Surgical or open approaches and reductions of the hip are reserved
for hips that cannot be reduced through closed manipulation, for hips
that do not stay reduced after closed reduction, or for hip luxations with
complicating factors such as avulsion fragments of the femoral head. A
craniolateral approach to the hip is performed, and the acetabulum is
cleared of hematoma, avulsion fragments, and capsular and round liga-
. ment remnants. Fractures of the acetabulum are repaired. Numerous
methods to stabilize the reduced hip joint have been described, but the
best methods currently used include toggle pin fixation or extracapsular
suture stabilization (prosthetic joint capsule). 2 Triple pelvic osteotomy
has been performed to aid in stabilization of the hip joint in dogs with
chronic luxations or in dogs with repeated luxations after reduction.
Femoral head and neck excision or total hip replacement is a viable
alternative for dogs with extensive damage to the femoral head.
Luxations of the stifle require extensive trauma to create and carry
a guarded prognosis for normal return to function because of the dam-
age that must occur to at least one collateral ligament and the cruciate
ligaments to allow complete luxation. Animals have a likely history of
132 ROUSH
vehicular trauma and do not bear weight on the limb, with the joint
grossly swollen, the limb malaligned at the stifle, and the stifle painful
to manipulation. Diagnosis is confirmed by stress radiography of the
stifle. Repair commonly involves correcting associated damage to the
cruciate ligaments and menisci, followed by repair of the collateral
ligaments by the creation of a prosthetic ligament with screws placed
above and below the joint at the origin and insertion, respectively, of the
affected collateral. Figure-eight prosthetic material is placed around the
screw heads to simulate the ligament. The suture material used should
be large, nonabsorbable, and a monofilament so as to provide sufficient
strength during healing and to minimize postoperative complications.
External skeletal fixation has been used to supplement repair, but it is
not ideal and should be removed by 6 weeks in all cases to provide for
return to joint mobility and joint cartilage homeostasis. Stifle arthrodesis
for stifle luxation should be considered a salvage procedure only. Stifle
arthrodesis is useful in chronic cases of luxation or those resulting in
degenerative joint disease, but it is not recommended, as dogs do not
ambulate normally or easily after stifle arthrodesis.
Tarsal luxations and instabilities carry a generally good prognosis,
if not for return to function, then as a last resort after arthrodesis. Dogs
with tarsalluxations are partially weight bearing or non-weight bearing
with a swollen joint. The limb may be grossly malaligned. Diagnosis is
confirmed by radiography and stress radiography of the affected joints.
Luxation of the tibiotarsal joint is caused by rupture of one or more of
the collateral ligaments, and these may be repaired by prosthetic liga-
ment techniques with care taken to restore the function of the long and
short components of the collateral ligaments.
2
These repairs generally
are supplemented by 4 to 6 weeks in a splint or cast, with exercise
restriction carried out over an additional 4 to 8 weeks. Chronic tibiotarsal
luxations resulting in degenerative joint disease in dogs respond to
pantarsal or partial tarsal arthrodesis with a good prognosis. Luxations
of the intertarsal and tarsometatarsal joints often occur in association
with compression fractures of one or more of the cuboidal bones of
the distal tarsus. Treatment by external coaptation, although commonly
attempted, results in continued instability and formation of a bony
ankylosis that remains painful to the dog. Distal tarsal or tarsometatarsal
luxations or subluxations should be repaired by distal arthrodesis by a
laterally or caudally placed bone plate or by fixation with external
skeletal fixators.
Metatarsophalangeal luxations or interphalangeal luxations occur
with minimal trauma, often from the dog being stepped on or catching
the toe during movement. Dogs with these luxations are partially weight
bearing, with minimal swelling localized in the region. Care must be
taken to individually examine each digit to determine the exact joint
affected. Diagnosis is confirmed by surveyor stress radiography. Luxa-
tions of the interphalangeal joints of any digit are treated by an open
surgical approach, reduction, and prosthetic replacement of the collateral
ligaments. Luxations involving the distal joints of the second or fifth
HIND LIMB LAMENESS IN THE MATURE DOG 133
digit with the rest of the digits intact may be most effectively treated by
amputation of the digit at the midmetatarsal level, with normal return
to function after 2 weeks in pet or working dogs.
DEGENERATIVE JOINT DISEASE
Degenerative joint disease may affect any joint of the hind limb and
occurs secondary to a variety of primary diseases, including aseptic
femoral head necrosis, hip dysplasia, cranial cruciate ligament rupture,
intra-articular fracture, patellar luxation, septic arthritis, and autoim-
mune polyarthritis. Several congenital diseases such as osteochondrosis
of the distal femur and talus present in older dogs as lameness caused
by chronic arthritis. In those dogs, treatment should be aimed at the
secondary degenerative joint disease rather than at the inciting cause.
Diagnosis of degenerative joint disease is made by finding painful,
swollen, and effused joints on physical examination and is confirmed by
radiographic findings of secondary degenerative joint disease, including
joint space collapse, osteophyte formation, and periarticular soft tissue
swelling (Fig. 2) . Scintigraphy may be useful to demonstrate and locate
synovitis in the immediate phase or subchondral bone changes in the
late phase. Arthrocentesis is useful to differentiate between the low
mononuclear cell counts of degenerative jOirlt disease, the high seg-
mented cell counts of autoimmune disease, and the high mixed popula-
tion with causative organisms present in septic arthritis. Serology testing
for specific and often regional pathogenic organisms such as Ehrlichia
canis is indicated when polyarthritis of an unknown origin is present.
Treatment of degenerative joint disease consists of a two-phase
approach of first treating the underlying disease cause and then treating
the dysfunction resulting from the chronic cartilage destruction. Septic
arthritides require culturing and lavage of the joint space, followed
by appropriate antibiotic therapy. Autoimmune polyarthritides require
specific anti-inflammatory and chemotherapeutic therapy to limit the
immune processes. Spirochetal arthritides require definitive serum titers
to determine the organism and specific treatment for the diseases.
There are two modalities currently available for medical treatment
of secondary degenerative joint disease. Analgesic therapy is useful for
dogs with mild clinical signs and when owners are compliant with the
treatment intervals necessary. The author uses buffered aspirin (10-25
mg/kg orally three times daily), carprofen (2.2 mg/kg orally twice
daily), or etodolac (10-15 mg/kg orally as needed) interchangeably
among patients depending on the owner's schedule to medicate the
animal, the duration and regularity of treatment expected, and the dog's
response to the individual agent. Ibuprofen is not a safe drug for use in
dogs, and other anti-inflammatories approved for human use are of
questionable safety and efficacy in dogs. Chondroprotective therapy,
using chondroitin sulfates, glucosamines, polysulfated glycosaminogly-
134 ROUSH
Figure 2. Craniocaudal radiograph of the left tarsus of a 2.5-year-old Golden Retriever with
slowly progressive hind limb lameness of 1 month duration. Osteoarthritis is present
secondary to a congenital OCD of the medial condyle of the talus.
cans, and other agents, is backed by multiple anecdotal reports of effi-
cacy and has been effective in some experimental and clinical trials for
the treatment of degenerative joint disease. These agents are adminis-
tered orally or by injection at varying levels depending on the source
and quality of the product and should be used at label dosages as
recommended. Analgesics and chondroprotective agents have been used
simultaneously with good results. Once clinical signs progress beyond
response to nonsteroidal analgesic therapy, surgical options should be
considered. Chronic corticosteroid administration in dogs is not recom-
mended because of the numerous and serious side effects with its use.
Many other drugs and treatment mechanisms are under investigation at
this time but cannot yet be recommended.
Successful surgical therapies for chronic degenerative jOll1t disease
vary based on the individual joint and should be considered salvage
procedures for all joints. In general, arthrodesis of the tarsus in dogs
carries a good prognosis, although arthrodesis of the stifle carries a poor
prognosis for normal function. Femoral head and neck excision is useful
in small-breed dogs for hip osteoarthritis, although total hip replace-
ment, as described below, results in better function for large-breed dogs.
HIND LIMB LAMENESS IN THE MATURE DOG 135
Hind limb amputation should not be considered unless normal function
of the opposite hind limb is guaranteed for the foreseeable future and
even then should be considered a last resort for alleviation of pain but
not for restoration of activity.
HIP DYSPLASIA
Hip dysplasia is a common cause of hind limb lameness in the
mature dog, but care must be taken not to ascribe lameness resulting
from a multitude of other mostly acute causes to chronic hip dysplaSia.
Although acute exacerbations of chronic osteoarthritis of hip dysplasia
may occur, they are infrequent and usually respond to 2 to 3 days of
enforced rest and analgesics. Of dogs referred to the author for total hip
replacement because of lameness attributed to hip dysplasia, approxi-
mately 25% have ipsilateral cranial cruciate ruptures that are responsible
for most of the acute or chronic lameness. Although hip dysplasia is a
real cause of lameness in older dogs, surgical treatment can often be
postponed for -several years with analgeSic and anti-inflammatory ther-
apy while the clinical signs slowly progress.
The history of a dysplastic dog is one of a slowly progressive
lameness that is worse after inactivity and improved after mild activity.
The lameness may be unilateral or bilateral depending on the severity
of disease in each hip. Dogs are often presented with histories of being
"slow to get up" or "reluctant to jump into a vehicle" as perceived by
the owner. During physical examination, pain may be elicited on exten-
sion of one or both hip joints. The Ortolani test is often negative in
patients with severe degenerative joint disease. The definitive diagnOSis
of hip dysplasia in the mature dog is made on the basis of survey
radiographs. Classic radiographic signs of secondary degenerative joint
disease are seen, ll1cluding osteophyte formation on the femoral neck
and acetabulum, collapse of the radiographically lucent joint space,
and luxation or subluxation of the joint. Further special radiographic
techniques such as the PennHip technique and others described else-
where in this issue are urmecessary to establish diagnosis in the mature
patient with secondary degenerative joint disease.
Treatment for hip dysplasia in the mature animal is primarily di-
vided ll1tO three options: analgesic or chondroprotective therapy, femoral
head and neck excision, or total hip replacement. Analgesic and chondro-
protective therapy should be instituted in mild cases as previously
described for secondary jOll1t disease. Femoral head arid neck excision
results in fair to good pain relief and return to function of many adult
dogs with hip dysplasia but should be limited to dogs weighing less
than 20 kg for best results. Dogs weighing over 20 kg respond better to
total hip replacement as a salvage procedure. The use of muscle flaps in
conjunction with femoral head and neck excision is not necessary and is
not beneficial in most reports. The most beneficial method to improve
136 ROUSH
the postsurgical function of a dog after femoral head and neck excision
is to begin immediate postoperative physical therapy such as joint ma-
nipulation, controlled exercise, or swimming. In the author's experience,
the better the use of the limb within the first week, the better is the
ultimate outcome for the dog.
Total hip replacement stands as the" gold standard" for alleviation
of pain caused by hip dysplasia but should be reserved for dogs that
weigh over 20 kg and are nonresponsive to medical therapy because of
the expense and the low but real incidence of severe complications.
Conversely, however, the best candidates for full recovery after total hip
replacement are dogs that have minimal muscle atrophy of the affected
lirnb(s) and good preoperative limb function. In current practice, most
hip prostheses placed in dogs are c ~ m e n t e d components, with the femo-
ral head separate from the femoral stem. The prognosis for return to
normal function after total hip replacement, including that of working
dogs, is greater than 95%, with a 1% to 2% risk of infection and a 3%
risk of postoperative hip luxation. Although earlier reports stated that
only one third of dogs required the replacement of the second hip with
bilateral hip dysplasia, careful observation of the animals and increased
client awareness of discomfort in the hip not operated on are currently
resulting in increased numbers of dogs undergoing bilateral replace-
ment. Total hip replacement requires a recovery period of 1 to 2 months,
controlled exercise, and periodic (yearly) rechecks to assess the condition
of the prostl1esis. Total hip replacement in dogs is limited primarily to
specialist practices in the United States because of the specialized equip-
ment and expertise necessary.
CRUCIATE LIGAMENT RUPTURE
As stated previously, this author believes that cruciate ligament
rupture is the most common but most underdiagnosed cause of hind
limb lameness. This underdiagnosis can be explained by the extensive
experience necessary for making a correct diagnosis of many ruptures
and by the lack of understanding of the disease process by general
practitioners and specialists alike. As understood by many practicing
veterinarians, cruciate ligament rupture is an acute injury often occurred
by trauma or overactivity. Although some cruciate injuries do indeed
occur acutely, or at least are manifested acutely, there is a growing
awareness that most cruciate ruptures occur through slow degeneration
of the cruciate ligaments as the result of an unknown cause suspected
to be autoimmune in nature. These dogs are often older, obese, large-
breed patients that have existing degenerative joint disease already pres-
ent at the time of the acute onset of lameness (Fig. 3). Biopsy of the
synovium in these dogs often is diagnosed as a plasmocytic synovitis of
unknown cause.
Just as the field of mathematics has rules, laws, and corollaries
HIND LIMB LAMENESS IN THE MATURE DOG 137
necessary to help us perform functions, similar laws can be formulated
to aid in the diagnosis of cranial cruciate ruptures. A list of these "laws"
is found in the box below. Although these laws do not substitute for
careful physical examination by an experienced veterinarian, they can
help in the diagnosis and guard against the underdiagnosis of cruciate
ligament rupture. The diagnosis of cruciate ligament rupture can be
made by the presence of a positive drawer test or tibial thrust test, both
of which were described previously in this article. This author believes
that a case can be also be made that any dog with a palpable medial
buttress or any dog with advanced degenerative stifle joint disease of
unknown origin should have the suspected stifle examined by arthrot-
omy or arthroscopy to confirm the presence of the presumptive cranial
cruciate rupture. Radiographs are neither necessary nor often useful to
aid in the diagnosis of cranial cruciate rupture, although they can docu-
ment the degree of secondary degenerative joint disease present. Second-
ary osteoarthritis is radiographically apparent within 6 weeks after cra-
nial cruciate rupture in the dog but may be present at the time of
presentation of chronic cases of partial cranial cruciate ligament rupture.
Laws for Cruciate Rupture Diagnosis
Law 1: If there is an acute-onset hi nd li mb lameness in a large-breed adult
dog, it is caused by a cruciate ligament rupture until proven otherwise.
Corollary 1 a: Immature dogs do not rupture their cranial cruciate liga-
ments unless severe trauma to the stifle has occurred.
Coroll ary 1 b: Small-breed dogs can rupture their cruciate ligaments, but
this most often occurs secondary to chronic endogenous or exogenous
corticosteroids or secondary to degenerative joint disease or second-
ary to trauma.
Law 2: If a medial buttress exists on the stifle of a dog with hind limb
lameness, there is a partial or full cranial cruciate ligament rupture pres-
ent.
Corollary 2a: There are no exceptions to Law 2.
Law 3: If moderate to severe degenerat ive joint disease exists in the stifle
of a large-breed dog, a cranial cruciate ligament rupture is present.
Corollary 3a: The only exception to Law 3 is penetrating trauma resulting
in septic arthritis or previous trauma resulting in intraarticular fracture.
Law 4: Confirmation of hip dysplasia in a dog with an acute hind li mb
lameness does not rule out cruciate ligament rupture.
Corollary 4a: Dogs presenting with acute lameness, confirmed hip dys
plasia, and a cruciate rupture are primarily lame because of the cruci-
ate instability and not the hip dysplasia.
138 ROUSH
Figure 3. Mediolateral radiograph of the left stifle of a 6-year-old Labrador Retri ever with
severe secondary osteoarthritis manifested by osteophyte formation and remodel ing of the
tibial plateau.
As previously mentioned, stifle arthroscopy is a useful technique to
confirm the diagnosis of cruciate ligament rupture. Stifle ultrasound or
magnetic resonance imaging of the stifle can demonstrate the ruptured
cranial cruciate ligament, but the use of these techniques is limited by
the availability of equipment and expertise to interpret the findings of
these modalities.
Cranial cruciate ligament rupture is a disease that requires surgical
stabilization in the dog. Analgesics, rest, or alternative therapy modal-
ities only temporarily alleviate the clinical signs, although they allow
continued and rapid progression of the secondary osteoarthritis. De-
scribed surgical treatments are numerous, but the three most commonly
used treatments at the present time are lateral (extracapsular) suture
stabilization with nylon monofilament/ the under and over fascial strip
technique,z and the tibial plateau leveling osteotomy. Controversy cur-
rently exists over which is the best technique, as all have their propo-
nents; however, a good prognosis exists with all three techniques . .
HIND LIMB LAMENESS IN THE MATURE DOG 139
PATELLAR LUXATION
Medial patella luxation is a common cause of hind limb lameness
in the small-breed dog and occurs as a rare cause of hind limb lameness
in the large-breed dog. In the large-breed dog, patella luxation can occur
either medially or laterally, and presentation and treatment are similar
to those in small-breed dogs. Patella luxation is congenital, often bilat-
eral, and likely heritable in origin in small-breed dogs. Medial patella
luxation occurs in association with a number of conformation anomalies
in the dog and is clinically graded from 1 through 4 (Table 1) depending
on severity.3 Dogs are presented with intermittent or chronic lameness
or no lameness at all. A common history of a dog with a: grade 2 medial
patellar luxation is that it walks normally, takes a few lame steps and
may exhibit pain, extends its stifle, and then walks normally again.
Owners often describe this as "skipping." Diagnosis is by physical
examination and determination of an abnormal position of the patella
either at rest (grade 3 or 4) or during motion (grade 1 or 2). Crepitation
may be detected during flexion and extension of the stifle and during
luxation and replacement of the patella. Survey orthogonal radiography
may demonstrate the patella in the luxated position but is primarily
useful to document the presence and degree of secondary degenerative
joint disease.
Treatment for medial patella luxation involves surgical correction
of the patellar luxation and sometimes the associated conformational
abnormalities. The two primary surgical therapies are trochlear wedge
recession and tibial crest transposition, both used in association with
lateral capsular imbrication. Grade 1 patella luxations do not commonly
cause clinical signs and do not require treatment. Grade 2 patella luxa-
tions are treated with either trochlear wedge recession if the trochlear
groove is not deep enough or tibial crest transposition if the conforma-
tional abnormality is the main cause. For grade 3 luxations, both surger-
ies are performed simultaneously on the affected stifle. Grade 4luxations
require both surgeries as well as midfemoral osteotomy or other correc-
tive procedures. A small number of dogs with patella luxation present
throughout their life are presented for acute lameness; in these dogs, the
Table 1. PATELLA LUXATION GRADES
Grade
1
2
3
4
Description
Patella is present in the trochlear groove and can be manually
luxated but replaces spontaneousl y
Patella moves spontaneously in and out of the trochlea during
movement of the stifle
Patella is luxated but can be manually replaced
Patella is luxated and cannot be replaced
140 ROUSH
cruciate ligament also needs examination and, if ruptured, repair along
with replacement of the patella.
NEOPLASIA
Neoplasia as a cause of hind limb lameness in dogs occurs most
often in older large-breed dogs and is of connective tissue origin. The
most common sites for bone neoplasia in the hind limb are the distal
femoral metaphysis and proximal tibial metaphysis, although any long
bone can be affected. Dogs are presented with an acute or short history
of lameness, which is sometimes progressive, and the lameness is re-
sponsive to analgesics. During physical examination, pain may be noted
on palpation of a metaphyseal region of a long bone. Confirmation is by
orthogonal survey radiographs of the affected area demonstrating the
characteristic signs of bone lysis, bone production, and the formation of
"Codman's triangle," a manifestation of reactive periosteum near the
tumor site. Old dogs with fractures in the metaphyseal region from
minimal trauma should be carefully examined for pathologic fracture
evidenced by bone lysis in the region of the fracture. Bone scintigraphy
may be useful to demonstrate bone turnover for early tumors in metaphy-
seal regions that are difficult to diagnose on survey radiographs. Ninety
percent of long bone tumors are osteosarcoma, with the remainder
evenly divided between chondrosarcoma, fibrosarcoma, and metastatic
tumors. Osteosarcomas are aggressively metastatic, and the primary
tumor is not often the cause of death of the animal. Synovial cell
sarcomas occur but are relatively rare and are characterized by lytic
destruction of both ends of the bones forming the affected joint. Synovial
cell sarcoma is less likely to metastasize than tumors of bone origin and
carries a better prognosis after amputation. Hypertrophic osteopathy
presents with a similar clinical history, although the lameness is some-
times bilateral. Radiographic lesions in hypertrophic osteopathy are
periosteal reactions on the diaphyses of long bones, primarily the distal
limb bones, and the radiographic lesions are often bilateral. Hypertro-
phic osteopathy is caused by space-occupying masses in the thorax or
abdomen, and treatment should be aimed at removing the primary
lesion, after which the pathologic changes of bone usually regress and
the lameness resolves.
Treatment for bone neoplasia is amputation above the affected bone
(hip disarticulation or mid femoral amputation) followed by three to
six courses of cisplatin chemotherapy. Limb-sparing surgery may be
performed for distal femoral or proximal tibial tumors but risks local
tumor return and carries a guarded prognosis for return to function.
References
1. Chalman l A, Butler HC: Coxofemoral joint laxity and the Ortolani sign. 1 Am Anim
Hosp Assoc 21:671, 1985
HIND LIMB LAMENESS IN THE MATURE DOG
141
2. Hulse DA, Jolmson Al: Management of joint disease. In Fossum TW (ed): Small Animal
Surgery. Philadelphia, Mosby, 1997, p 883 '
3. Roush JK: Canine patellar luxation. Vet Clin North Am Small Anim Pract 23:855, 1993
4. Roush JK, McLaughim RM: Fundamentals of fracture management Vet Med 93'1065
1998 . . ,
Address reprint requests to
James K. Roush, DVS, MS
Section of Small Animal Surgery
Department of Clinical Sciences
College of Veterinary Medicine
Kansas State University
Manhattan, KS 66506
e-mail: roushjk@vet.ksu. edu
1
LAMENESS 0195-5616/ 01 $15.00 + .00
FELINE LAMENESS
Cynthia Anne Leonard, DVM, and Michael Tillson, DVM, MS
Lameness in the feline patient has historically been an infrequently
encountered problem when compared with the incidence of this com-
plaint in the dogY With the growing number of cats living longer lives
as well as the changing attitudes of people regarding cats as pets, the
veterinarian faces increasing pressure to diagnose and treat a variety of
feline lamenesses. The goal at this time should be to develop a list of
suitable differential diagnoses tailored toward the cat. Many of the
more common causes of canine lameness are included; however, their
significance may differ greatly. There are also many causes of feline
lameness that are not common in the canine patient (Table 1).
ORTHOPEDIC EXAMINATION
The orthopedic examination is performed in a similar manner in
the cat and in the dog. Two important differences are the lack of willing-
ness of a lame cat to walk around an examination room and the potential
difficulties in the restraint of a fractious or painful cat. The initial phase
of any orthopedic examination involves observing the animal walking
on a regular surface. This can be more challenging when dealing with
cats and may involve observing the cat from behind a door, placing the
cat in a more comfortable setting, or potentially having the owners bring
a videocassette made at home. It is important to establish which leg is
affected by the lameness either by watching the animal or by listening
to the owner's description of the cat's history.
From the Department of Small Animal Surgery, Veterinary Teaching Hospital, Ontario
Veterinary College, University of Guelph, Guelph, Ontario (CAL); and Department of
Small Animal Surgery, Auburn University College of Veterinary Medicine, Auburn,
Alabama (MT)
VETERINARY CLINICS OF NORTH AMERICA: SMALL ANIMAL PRACTICE
VOLUME 31 NUMBER 1 JANUARY 2001 143
'-
tIS
"5
0
IIJ
::J
:2:
tIS
'iii
tIS
Q.
0
Q)
z
iii
"E
Q)
E
a.
0
Qj
>
Q)
c
IIJ
::J
.S!
"0
oS!
.E
(f)
(f)
UJ
Z
UJ
:2
-'
UJ
.;:
Z
..c
::i
1:
UJ
LL
LL
0
(f)
UJ
(f)
::J
()
tIS
...:
E
Q) ::J
:c
tIS
.=
144
>,
.s
'" 0..
0
>,
E
u
'.0
0
....
",'
S E Kj
E Sl
'"
.2
'" E
- E X
E CJ Q) Q)
0
0
u_ '"
.S
e
'u
....
.5
'"
'"
u
bOEbO u
0
0
' '" e
'" ro':a e
'"
....
'"
"0
0
E
....
"0
'"
'"
'"
0 u
C'
u
'" C'
H
"'-
'" '"
<il e
0
2"3
.
'"
::l
p... (f]
'" ,'00
0
"'"0
.!S! c
0..",
"'..0:
>,u
<il
"0 u
'"
>,8
'"
.u;
'" '"
'" 0..
-"Ro...]
'"
>,
e 2 u u
"0 OQ) ....... O::l
0..
tE & 0
'" '"
.u; .u;
0 0
'"
E S
::l
'" '"
....
'" '"
:
Q. Q.
0
.8
u
>,
i u
'"
'.0
:g :g
'"
.... .... <f>
'" '" '"
>, >,
'" -0 -0
'"
0.. 0.. il
'"
'" .S
'"
'"
:> .Q..
'"
'"
'"
.... .... '"
bO'"
bOa;
o > 0 .......
H
OJ
Q) Cl) b.- e
;.co;.co
?;;,
'" '"
OJ
0
b!)
'" '"
'"
.2 E
'"
u
v
'" '" '"
....
U 0
FELINE LAMENESS 145
'. The actual physical examination begins (if possible) with the cat in a
standing position. Careful palpation of the muscle mass of the shoulders,
lumbar area, and hind limbs should be done before the cat is p laced in
lateral recumbency. Muscle atrophy or discomfort should be noted.
The cat is placed in lateral recumbency, with the lame leg on the
down side. Careful manipulation of the normal joints and long bones is
done beginning at the phalanges. Each joint is run through a full range
of flexion, extension, rotation, and lateral-to-medial and cranial-to-caudal
stability as well as assessed for effusion and crepitus. Each long bone
should be palpated along its length for any discomfort. An attempt
should be made to repeat any manipulation that causes a response in
the cat. A reaction on multiple occasions is more likely to imply a
significant lesion as opposed to a fidgety animal. This comprehensive
examination is done on all limbs, with the lame leg being evaluated last.
OTHER FACTORS CONTRIBUTING TO LAMENESS
It is suspected that most of the conditions affecting the musculoskel-
etal system in cats are subclinical. It has been noted that overweight cats
are 2.8 times and obese cats are 5.4 times more likely to suffer from
lameness visible to owners.23
CAT BITES
Cat bites are a common occurrence, contributing to 4.7% of all visits
made by cats to veterinarians. To establish relevance, canine lameness is
responsible for 3.1% of all veterinary visits.
12
Obviously, not all cat bites
result in lameness, but it is the typical presentation for any bite-related
abscess that develops in the limbs.
Diagnosis of a deep abscess can be difficult if the cat is depressed,
or worse, fractious. It is important to try to perform an orthopedic
examination in the awake animal; however, a mild sedative can expedite
the process. Sedatives such as propofol, ketamine, or medetomidine
given at a low dosage can make the animal more amenable to the
examination while leaving it with enough consciousness or pain sensa-
tion to respond during manipulation. The easiest way to detect deep
limb abscesses is to perform systematic careful palpation of the leg
muscles and joints for pain or for small scabs over pun,cture wounds.
Any suspicious findings should prompt a thorough clipping of the fur
in the region to search for puncture wounds or scratch marks (Figs. 1
and 2). Abscesses are drained with a suitable ventral exit hole and then
lavaged. Debridement of necrotic tissues may be required in severe
cases. Bandaging a feline limb can be challenging. A Penrose drain
should not be placed if the exit site cannot be covered. An unbandaged
drain is an invitation to further infection. It has been our experience that
cat bite wounds on the limbs often result in diffuse cellulitis rather than
146 LEONARD & TILLSON
Figure 1. Lateral pelvis, cellulitis of soft tissue caudal to femur secondary to cat bite.
Figure 2. Ventrodorsal pelvis, cellulitis of soft tissue caudal to femur secondary to cat bite.
FELINE LAMENESS 147
a true abscess (Figs. 3 and 4). Establishing drainage can be difficult, and
these cases may respond better to appropriate antibiotic therapy and
warm compresses.
Cat bites involving a joint should be copiously lavaged either percu-
taneously or via an arthrotomy. Bacterial culture tests are performed on
the tissues after lavage to determine the appropriate antibiotic therapy.
Bacterial cultures can also be taken from skin wounds, particularly those
that are not healing as rapidly as expected.
OSTEOARTHRITIS
Feline Progressive Polyarthritis
Feline polyarthropathy is often the first differential diagnosis con-
sidered by many practitioners when presented with a lame cat. There
Figure 3. Lateral tarsus, osteomyelitis.
Figure 4. Dorsoplantar tarsus, osteomyelitis.
148 LEONARD & TILLSON
are two recognized varieties of feline progressive polyarthritis. The more
common proliferative form is characterized by an acute onset of fever
and malaise, a painful stiff gait, and joint effusion. Other associated
clinical signs include peripheral or localized lymphadenopathy and gen-
eralized muscle wasting. Within weeks of this initial phase, new perios-
teal bone formation occurs, with the eventual development of palpable
exostoses. This type of feline polyarthritis occurs in cats from 1 to 5
years of age. The second type of feline polyarthritis is severely erosive
and bears many similarities to human and canine rheumatoid arthritis.
Although this condition usually presents with a gradual onset, it causes
a progressive lameness that eventually results in the complete debilita-
tion of the cat. Characteristic radiographic signs include severe subchon-
dral bone lysis with secondary joint deformity, instability, and eventual
luxation (Fig. 5). There is no acute illness associated with this type of
feline polyarthritis, and affected cats are generally over 5 years of age
(Table 2). Both types of feline progressive polyarthritis affect the distal
Figure 5. Dorsopalmar carpus/antebrachium, feline polyarthritis in carpus.
Figure 6. Dorsoplantar carpus, degenerative joint disease-metacarpophalangeal joint.
FELINE LAMENESS 149
Table 2, CHARACTERISTI CS OF FELINE PROGRESSIVE POLYARTHRITIS
Erosive Polyarthritis
No acute illness, gradual onset
No significant joint effusion
Severe subchondral bone lysis
Joint deformity
Joint instability/luxation
Proliferative Polyarthritis
Acute illness B fever, malaise, painful, stiff gait
Joint effusion
New periosteal bone
Exostoses
joints of male cats. It is reported that 100% of these animals are infected
with syncytia-forming virus, and as many as 66% may be infected
with feline leukemia virus.
13
Diagnosis of the condition is based on the
appearance of erosive arthritis on radiographs and the documentation
of inflammatory nonseptic joint fluid. Arthrocentesis of affected joints
reveals discolored, cloudy, or flocculent fluid with decreased viscosity.
There are greater than 5000 cells per microliter, with a large proportion
of these cells being neutrophils. The protein level of the fluid is greater
than 5 g/ dL. There is no effective treatment for either form of this
diseaseY
Degenerative Joint Disease
With the growing proportion of elderly cats, degenerative joint
disease is being recognized as a clinical problem with greater frequency?
In many cats, degenerative joints are an incidental finding. Degenerative
joint disease causing clinical signs is usually found during a workup of
forelimb lameness and is more commonly diagnosed in the elbows and
shoulders.7 The radiographic signs of degenerative joint disease in the
cat are identical to those in the dog, including subchondral bone sclero-
sis, changes in bone shape, a thickened joint capsule with secondary soft
tissue swelling, and osteophytes and new bone formation (Fig. 6)? An
important anatomic variation in the cat is the presence of a sesamoid
bone in the tendon of origin of the supinator muscle. This sesamoid is
visible radiographically where it articulates with the craniolateral head
of the radius. On a lateral radiograph, this bone looks remarkably similar
to an osteophyte.
32
Arthrocentesis of these joints can be done in a
manner similar to that employed in the canine patient. Most cats with
degenerative joint disease have normal joint fluid or only a minimal
increase in the number of cells.
13
DEVELOPMENTAL DISEASES
Hip Dysplasia
Hip dysplaSia is diagnosed infrequently in the feline patient, but it
is possible that the rate of diagnosis would increase if hip radiographs
150 LEONARD & TILLSON
were made more often. This disease is present in approximately 18% of
the Maine Coon cat population based on reports from the Orthopedic
Foundation of America. Most cats are presented at less than 1 year of
age with clinical signs of reluctance to walk, hind limb and
pain or crepitus on hip The treatment of chOlce for these
animals is cage rest, after whIch hme the lameness seems to resolve.
Most cases of hip dysplasia in the cat are subclinical, and the diagnosis
is most often made as an incidental finding. Radiographic changes
associated with feline hip dysplasia include a shallow acetabula, which
can also be seen in normal cats; a flat craniolateral acetabular rim; and
coxofemoral luxation or subluxation (Figs. 7 and 8).19 There are no
established normal values for the Norberg angle in the cat, but an angle
of less than 105 is deemed abnormal in the dog, and cats described
with this condition have had Norb'erg angles between 73 and 100.19 In
most of these cats, even those diagnosed at an older age, minimal
degenerative joint disease was associated with the condition. Given
enough time, many of these cats develop pseudoarthroses, but few seem
to demonstrate any clinical signs of lameness beyond that seen at the
time of initial presentation.
19
The treatments of choice for this disease
Figure 7. Ventrodorsal pelvis, hip dysplasia.
n
\
FELINE LAMENESS 151
Figure 8. Lateral pelvis, hip dysplasia.
include cage rest for 2 to 3 weeks or femoral head and neck ostectomy.
Pectineus tenectomy has also been described as a treatment for hip
dysplasia in the cat, with an apparently high rate of success. It is
important to note that there is an increased incidence of medial patellar
luxation in cats with hip dysplasia.
19
.
Femoral Neck Metaphyseal Osteopathy
Femoral neck metaphyseal osteopathy is a syndrome that was re-
cently described in 17 cats over a 10-year period.
21
The cats were pre-
sented with a history of vague hind limb lameness with an inevitable
acute progression to severe lameness. Most of the animals were less than
2 years of age, and 15 of the 17 were castrated male cats. Physeal closure
occurs much later in neutered male cats than in intact male or female
cats, whose capital physes close between 7 and 10 months of age, and
may playa role in this condition.
21
Radiographic changes associated with
the disease included femoral neck lucency with decreased definition of
the proximal femoral metaphysis. Twelve of the reported cats had also
suffered a pathologic fracture of the femoral neck (Figs. 9 and 10).21 Three
of the cats were diagnosed with concurrent medial patellar luxation, and
4 of the cats had bilateral disease occur within 5 months of the original
diagnosis.
Histopathologic analysis of the femoral heads and necks revealed
thickening and splitting of the articular cartilage with necrotic bone,
152 LEONARD & TILLSON
Figure 9. Ventrodorsal pelvis, femoral neck fracture.
Figure 10. Ventrodorsal pelvis, femoral neck fracture 4 months after injury.
hemorrhage, and vascular congestion at the epiphyses. A significant
amount of fibrous tissue and fibrocartilage and an increased number of
osteoclasts were seen. Based on the pattern of bone loss in these cases,
it is highly suspected that the bone loss was the primary problem, with
the fractures occurring secondarily. Femoral neck fractures comprise 16%
of femur fractures in the cat, with most of these occurring when the cat
is less than 1 year of age.
2
Perhaps metaphyseal osteopathy is a more
common condition than previously believed and is responsible for a
certain proportion of these femoral neck fractures.
The cause of this disease remains unknown; however, an ischemic
incident is suspected. The blood supply to the femoral head and neck
comes from three principal sources. The first is the intraosseous supply
from the nutrient artery. The second is direct penetration of the epiphysis
and metaphysis by the medial and lateral circumflex femoral arteries as
well as by the caudal gluteal artery. These vessels form an extracapsular
ring around the femoral neck with secondary branches supplying a
second intracapsular ring. In the adult cat, there are many anastomotic
branches between these two rings, but this is prevented by the physis
in the juvenile animal. The third source of blood supply to the femoral
neck and head comes from the teres ligament, which is much more
substantial than in the dog. This three-tiered blood supply is tortuous
and prone to embolism and infection. Any damage to this blood supply
FELINE LAMENESS 153
could lead to bone loss in the femoral neck with secondary pathologic
fracture.
21
Osteochondrodysplasia
Osteochondrodysplasia is a syndrome that contributes to the pheno-
type of many common canine breeds such as the Dachshund or Basset
Hound. A new cat breed, the Munchkin, has been created by selecting
for this disorder. There do not seem to be any described problems
associated with this breed; however, any potential problems are likely
be similar to those in the dog such as limb deformities and intervertebral
disk disease. Osteochondrodysplasia has also been described in the
Scottish Fold cat. If phenotypically positive folded ear cats are mated to
other folded ear cats, the progeny have a high possibility of inheriting
this disease. The clinical signs first appear at 7 weeks of age as a wide-
based inflexible tail followed by the development of progressive hind
limb lameness. Radiographic signs at this time include wide physes
over the tarsal -and metatarsal bones, with decreased bone growth and
abnormal bone shape. Short caudal vertebrae are also visible. By 6
months of age, gross plantar exostoses around the tarsal and metatarsal
bones are palpable clinically and visible radiographically. These exosto-
ses lead to eventual ankylosis of the joints, resulting in severe hind limb
lameness.
14
Histologic findings were 'consistent with aberrant ossification
and included abnormal chondroblast proliferation, thick physes with
decreased ossification, irregular patterns of mineralization, and supernu-
merary ossification centers. The progression of the lameness and the age
at onset of the condition varied significantly between different cats.14
Mucopolysaccharidosis
This disease is caused by errors of glycosaminoglycan metabolism
and has been reported in the Siamese breed. Clinical signs include
progressive hind limb lameness, broad face, depressed nasal bridge,
small ears, corneal clouding, and potentially multiple bone dysplasias.
The more commonly n oticed orthopedic problems are hip dysplasia,
cervical vertebral widening and fusion, and pectus excavatum (Figs. 11
to 13).8
INFECTIOUS CAUSES
Calicivirus
The incidence of lameness related to calicivirus infection seems to
be greater after v accination for calicivirus than for naturally acquired
infections. In one study of 123 cats that had suffered from a vaccine
154 LEONARD & TILLSON
Figure 11. Lateral antebrachium, mucopolysaccharidosis, carpus,
Figure 12. Dorsopalmar antebrachium, mucopolysaccharidosis, carpus,
Figure 13. Lateral antebrachium, mucopolysaccharidosis, carpus,
reaction after administration of calicivirus vaccine, 8,0% with
clinical signs of lameness, although only had 'prImary related
to an upper respiratory infection,4 chmcal.signs of ar-
thropathy include shifting lameness with a noticea.bly stiff gait These
cats also resist handling and may have secondary SignS of oral
ulceration, and upper respiratory infec,tion,.3. 4 Most ?f ammals
were presented witlUn 1 week of vaccmation for cahciviruS., Most of
these cats were kittens less than 6 months of age and had received only
the first vaccination,3.4 ,
Naturally occurring calicivirus infection most commonly m
cattery kittens. The clinical signs include generalIZed u:'-us-
cle soreness, stiff gait, and a reported erythema over the tarsal Jomts.
These signs tend to last for 24 to 48 hours, and kittens generally have a
full recovery.
4
FELINE LAMENESS 155
Experimental inoculation of cats with virulent strains of calicivirus
revealed that no lesions were found in the muscles, joints, or central
nervous system. All the changes caused by the viremia, which may have
contributed to the lameness, were found in the synovium.
4
Mycoplasma
Mycoplasma gatteae is a reported cause of polyarthritis and tenosyno-
vitis in the cat.
16
Affected cats are presented with swollen limbs, painful
joints, lameness, and pyrexia. Culture results of the synovium and,
potentially, of the synovial fluid are positive for the organism. A tenta-
tive diagnosis can also be made if the organism is recognized on cyto-
logic testing.
Histoplasmosis
Histoplasma capsulatum is a soil-borne organism found throughout
the American midwestern and southeastern regions. It is most prevalent
along the drainage systems of the Ohio, Missouri, and Mississippi Rivers
and is contracted by inhalation of the fungal spore. Osseous histoplasmo-
sis has been reported in seven cats between the ages of 8 months and 8
years. Most cats were presented with signs of lameness, soft tissue
swelling over the limb, and pain on bone palpation. Lymphadenopathy
was seen in four cats, and draining tracts over the bone lesion were
noted in two cats.
31
Other systemic signs of pyrexia, anorexia, weight loss, lethargy,
or chorioretinitis were occasionally noted. No respiratory signs were
described. Diagnosis of the disease was made by identification of the
organism in lymph nodes, peripheral blood, or bone biopsy, Radial
immunodiffusion was performed in two cats and was only positive in
one of them. Radiographic changes were noted in the skull in one cat
and in the appendicular skeleton, especially adjacent to the carpal or
tarsal joints, and multiple bones were occasionally infected. Multifocal
irregular areas of osteolysis and endosteal new bone were seen around
the metaphyses. Pathologic fractures were noted in two cats.
31
NEOPLASIA
The cat is similar to the dog in that it can be plagued by a variety
of primary bone tumors as well as by metastases to the skeletal system.
The incidence of neoplasia involving the skeletal system is low, at
approximately 4.9 per 100,000 cats.s The behavior of these tumors is
generally aggressive, with 67% to 90% being malignant.
27
The site of
these tumors tends to be in the long bones and axial skeleton, and the
hind limbs are much more frequently involved than the forelimbs.
27
156 LEONARD & TILLSON
Discussed here are those tumors that behave in a manner different from
their canine counterparts (Table 3).
Mammary Adenocarcinoma
Mammary tumors have a much higher likelihood of malignant
behavior (80%) in the cat than in the dog. The most common sites
of metastasis are the lungs and regional lymph nodes.
5
, 9 Mammary
adenocarcinoma to the bone is a rare occurrence in cats and dogs, with
only four cases reported in feline patients.
29
In a second study of 300
cases of metastases from mammary adenocarcinoma in the cat, only 12
involved the bones. The difference in the metastatic behavior of this
tumor in the cat as compared with the dog is that the distal portions of
the limbs are primarily affected, particularly the talus.
29
Pulmonary Adenocarcinoma
Feline pulmonary adenocarcinoma also has a preference for metasta-
sis to the distal limb and digits. In . one study of 13 cats with skeletal
metastases, six cases involved the phalanges, and five of these were
from pulmonary adenocarcinoma.
29
Any cat with a digital mass found
to be a carcinoma on histopathologic evaluation should have thoracic
radiographs made to rule out a primary pulmonary lesion.
Synovial Tumors
Four cases of synovial tumors have been reported in the caP' 10, 17, 25
Three of these cases were benign with eventual cure by complete exci-
sion, although this was done with apparent difficulty. The distal limb
and joints were affected. The fourth case was a synovial sarcoma, which
presented with lameness, joint swelling, and decreased range of motion.
Radiographic changes were soft tissue swelling and a smooth periosteal
reaction in the region of the joint capsule attachment. This tumor was
treated with amputation, and the cat had remained tumor-free for 1 year
after surgery at the time of publication of the report.
25
Confirmation of
the tumor type was made through joint capsule biopsy.
Giant Cell Tumor
Giant cell tumors occur rarely in small animal practice, but they
seem to be more commonly diagnosed in the cat than in the dog. The
radiographic appearance is characteristic, with an expansile multilocu-
lated mass causing significant osteolysis of the long bone diaphysis. IS
Treatment of this tumor has been successful with amputation.
~
(j)
<{
-'
Cl...
o
w
z
-'
~
w
-'
w
~
(j)
w
z
::J
w
LL
,.;
(1)
:c
~
ClI
E
:..0
... C
ClI._
CO
o ...
E rl
-0
::> C
11.(1)
't:!
ClI
E
:..0
... C
E n ~
E rl
ClI 0
2 C
(1)
't:!
157
158 LEONARD & TILLSON
Osteosarcoma
Osteosarcoma occurs much less commonly in the cat than in the
dog. The clinical history and radiographic changes mimic those of the
canine patient, but the primary tumor site is more likely to be found in
the hind limbs. The behavior of feline osteosarcoma is much less aggres-
sive than in the dog, with a low metastatic rate. Treatment with surgery
can be successful, with an average 24-month length of survival after
amputation alone (Figs. 14 to 18).27
Multiple Myeloma
Myeloma is a tumor of p l a s m ~ cells originating in the bone marrow.
A plasma cell tumor arising from a tissue other than bone marrow is
termed a plasmacytoma. Only eight cats with multiple myeloma have
been reported to have osteolytic bone lesions.
6
, 24, 30 This differs from the
incidence in dogs, in which 56% of the cases are diagnosed with bony
involvement.
,s
,'8 Other clinical signs associated with the tumor include
lethargy, anorexia, weight loss, polyuria, polydipsia, neurologic changes,
and retinal hemorrhage and detachmenpo Laboratory findings include
increased globulin with a monoclonal gammopathy seen on protein
electrophoresis, anemia, and thrombocytopenia. Twelve of the 19 re-
ported cats had Bence Jones protein in the urine.
3D
To confirm a diagnosis
Figure 14. Lateral stifle, osteosarcoma, distal femur.
FELINE LAMENESS 159
Figure 15. Dorsoplantar stifle, o$teosarcoma, distal femur.
Figure 16. Lateral stifle, osteosarcoma, distal femur with pathologic fracture.
of multiple myeloma, it is recommended that the cat be positive for a
minimum of two of four criteria: greater than 20% plasma cells in the
bone marrow, paraproteinemia or monoclonal gammopathy, osteolytic
bone lesions, or Bence Jones proteins in the urine. Histopathologic con-
firmation of the tumor can also be made from a bone biopsy.3D The
average age of cats in the study was 10 years, with male cats being
overrepresented. 30 All the cats were negative for feline leukemia virus.
3D
The osteolytic bone lesions can occur throughout the skeletal system,
but the distal extremities were more commonly affected. This also differs
from the dog, in which the spine, pelvis, ribs, skull, and proximal
extremities were most frequently involved.
' 8
It is thought that the cause
of the lysis is primary tumor invasion into bone or osteoclast activating
factor produced by the plasma cells.
Multiple Cartilaginous Exostosis
Multiple cartilaginous exostosis is a rare condition most commonly
associated with bony outgrowths occurring in the immature dog. A
160 LEONARD & TILLSON
Figure 17. Lateral tarsus, osteosarcoma.
Figure 18. Dorsoplantar tarsus, osteosarcoma.
similar disease occurs in cats but affects only those with a mature
skeleton. These lesions are progressive, with firm swellings over the
scapula, vertebrae, mandible, or long bones. They lead to pain, stiffness,
and loss of function over the affected area. Cats with this disease should
be considered to be feline leukemia virus- positive until proven other-
wise, and owners should be warned about the possibility of malignant
transformation. The radiographic appearance of these lesions consists of
bony protuberances with an indistinct border with the remaining bone.
No effective treatment is available for this disease. Surgical resection of
the masses may provide temporary relief, but recurrence is likely.20.22
FIBROTIC MYOPATHY
Fibrotic myopathy is a relatively frequently observed problem in
the canine patient, and it has also been reported in the cat. The clinical
signs include insidious progressive hind limb lameness. Increased
flexion of the hip, stifle, and hock; increased early swing phase; and
FELINE LAMENESS 161
decreased abduction are the typical gait abnormalities associated with
this condition. On palpation of these animals, a taut band can be felt on
the caudomedial surface of the thigh. This lameness is nonpainful,
with normal neurologic examination and radiographic findings. Surgical
exploration of the band has revealed a firm white semitendinosus muscle
caused by fibrosis of unknown origin. Treatment of the disease is diffi-
cult, as recurrence is common after muscle lengthening procedures.
ll
One case report described treatment with a Z-plasty lengthening until
full abduction of the limb was possible during surgery. The lameness
had recurred by 2 months after surgery, but there was no decrease in
limb abductionY Although no comments were made regarding the hips
of this cat, this disease can be associated with hip dysplasia in dogs.
DECLAWING
Postoperative lameness is a well-documented complication after
onychectomy (Fig. 19). What should be noted is that 50% of cats may
have lameness -lasting anywhere from 1 to 54 days and that cats have
Figure 19. Carpus, postoperative declaw.
162 LEONARD & TILLSON
occasionally been described as suffering from long-term discomfort after
this procedure.
26
The acute lameness is more often associated (in the
teaching hospital) with the blade technique and the use of tissue adhe-
sive, whereas long-term complications are more commonly associated
with the nail clipper technique.
26
References
1. Bennett D, Gaskell RM, Mills A, et al: Detection of feline calicivirus antigens in the
joints of infected cats. Vet Rec 124:329-332, 1989
2. Daly WR: Femoral head and neck fractures in the dog and cat: A review of 115 cases.
Vet Surg 7:29-33, 1978 .
3. Davies JD, Little NRF: Synovioma in a cat. J Small Arum Pract 13:127-133, 1972
4. Dawson S, McArdle F, BelU1ett D, et al: Investigation of vaccine reactions and break-
downs after feline calicivirus vaccination. Vet Rec 132:346-350, 1993
5. Dorn CR, Taylor D, Schneider R: Survey of animal neoplasms in Alameda and Contra
Costa Counties, California. II. Cancer morbidity in dogs and cats from Alameda
County. J Nat! Cancer Inst 40:307-318, 1968.
6. Eastman CA: Plasma cell tumors in a cat. Feline Pract 1:26-31, 1996
7. Hardie EM: Management of osteoarthritis in cats. Vet Clin North Am Small Anim
Pract 27:945-953, 1997
8. Haskins ME, Jezyk PF, Desnick RJ, et al: Mucopolysaccharidosis in a Domestic Short-
Haired cat-a disease distinct from that seen in the Siamese cat. JAVMA 175:384-387,
1979
9. Hayes HM, Milne KL, Mandell CP: Epidemiological features of feline mammary
carcinomas. Vet Rec 108:476-479, 1981
10. Hulse EY: A benign giant cell synovioma in a cat. J Pathol 91:269-271, 1966
11. Lewis DD: Fibrotic myopathy of the semitendinosus muscle in a cat. JAVMA 193:240-
241, 1988
12. Lund EM, Armstrong pJ, Kirk CA, et al: Health stahts and population characteristics
of dogs and cats examined at private veterinary practices in the United States. JAVMA
214: 1336-1341, 1999
13. Magne ML: Swollen joints and lameness. In Ettinger SJ (ed): Textbook of Veterinary
Internal Medicine, ed 5. Philadelphia, WB Saunders, 2000, pp 77-80
14. Malik K, Allan GS, Howlett CR, et al: Osteochondrodysplasia in Scottish Fold cats.
Aust Vet J 77:85-92, 1999
15. Matus RE, Leifer CE, MacEwen EG, et al: Prognostic factors for multiple myeloma in
the dog. JAVMA 188:1288-1291, 1986
16. Moise NS, Crissman JW, Fairbrother JF, et al: Mycoplasma gateae arthritis and tenosyno-
vitis in cats: Case report and experimental reproduction of the disease. Am J Vet Res
44:16-21, 1983
17. Nielsen SW: Extra-skeletal giant cell tumor in a cat. Cornell Vet 42:306-311, 1952
18. Osborne CA, Perman V, Sautter JH, et al: Multiple myeloma in the dog. J Am Vet Med
Assoc 153:1300-l319, 1968
19. Patsikas MN, Papazoglou LG, Komninou A, et al: Hip dysplasia in the cat: A report
of three cases. J Small Anim Pract 39:290-294, 1998
20. Pool RR, Carrig CB: Multiple cartilaginous exostosis in a cat. Vet Pathol 9:350-359, 1972
21. Queen J, Bennett D, Carmichael S, et al: Femoral neck metaphyseal osteopathy in the
cat. Vet Rec 142:159-162, 1998
22. Riddle WEI, Leighton Rl: Osteochondromatosis in a cat. J Am Vet Med Assoc 56:1428-
1430, 1970
23. Scarlett 1M, Donoghue S: Associations between body condition and disease in cats. J
Am Vet Assoc 212:1725-1731, 1998
24. Sheafor SE, Gamblin RM, Couto CG: Hypercalcemia in two cats with multiple my-
eloma. J Am Anim Hosp Assoc 32:503- 508, 1996
FELINE LAMENESS 163
25. Silva-Krott IU, Tucker RL, Meeks JC: Synovial sarcoma in a cat. JAVMA 203:1430-
1431, 1993 .
26. Tobias KS: Feline onychectomy at a teaching institution: A retrospective study of 163
cases. Vet Surg 23:274-280, 1994
27. Turrel 1M, Pool RR: Primary bone tumors in the cat: A retrospective study of fifteen
cats and a literature review. Vet Radiol 23:152-166, 1982
28. Walsh BA, Rhodes WH: Giant cell tumour of bone in a cat. J Small Anirn Pract
36:325-329, 1995
29. Waters DJ, Honeckman A, Cooley DM, et al: Skeletal metastasis in feline mammary
carcinoma: Case report and literature review. J Am Anirn Hosp Assoc 34:103-108,1998
30. Weber NA, Tebeau CS: An unusual presentation of multiple myeloma in two cats. J
Am Anim Hosp Assoc 34:477-483, 1998
31. Wolf AM: Histoplasma capsulatum osteomyelitis in the cat. J Vet Intern Med 1:158-
162, 1987
32. Wood AKW, McCarthy PH, Martine CA: Anatomic and radiographic appearance of a
sesamoid bone in the tendon of origin of the supinator muscle of fue cat. Am J Vet
Res 56:736-738, 1995
Address reprint requests to
Cynthia Leonard, DVM
Veterinary Teaching Hospital
Ontario Veterinary College
UniverSity of Guelph
Guelph, Ontario
N1G 4S7 Canada
e-mail: cleonard@ovc.uoguelph.ca
LAMENESS 0195-5616/01 $15.00 + .00
DIAGNOSTIC IMAGING OF
LAMENESS IN SMALL ANIMALS
James J. Hoskinson, DVM, and Russell L. Tucker, DVM
Diagnostic imaging is a fundamental part of the evaluation of the
lame small animal patient. Diagnostic imaging is not, however, intended
to serve as a shortcut to diagnosis or to take precedence over a thorough
physical examination. Imaging alone rarely provides a specific indication
of the cause of a particular disease, although it may provide the basis
for establishing potential diagnoses from which the final diagnosis can
be determined with discrimination.
35
The indications for diagnostic imaging include to confirm or refute a
clinically suspected lesion, to suggest or document the site of a suspected
lesion, to characterize the nature and extent of a known or suspected
lesion, to follow the progression of disease or healing, to aid in establish-
ing prognosis, to plan or evaluate surgical therapies, to suggest or guide
additional diagnostic procedures, and to screen for diseases with obscure
clinical signs. 35
The selection of the appropriate diagnostic imaging study is deter-
mined by the anatomic structure to be evaluated and the type of informa-
tion sought. With the advent of newer imaging modalities, anatomic
and functional information about the musculoskeletal system can be
determined with increasing diagnostic accuracy and anatomic resolution.
Survey and contrast radiography, although replaced in some areas
by newer imaging modalities, continue to be readily available, cost-
effective, and accurate tools in the evaluation of the lame patient. It is
recommended that survey radiographs precede any special imaging
studies.
The demand for advanced diagnostic imaging procedures such as
From the College of Veterinary Medicine, Kansas State University, Manhattan, Kansas
GJH); and the College of Veterinary Medicine, Washington State University, Pullman,
Washington
VETERINARY CLINICS OF NORTH AMERICA: SMALL ANIMAL PRACTICE
VOLUME 31 NUMBER 1 JANUARY 2001 165
166 HOSKINSON & TUCKER
nuclear scintigraphy, ultrasonography, computed tomography (CT), and
magnetic resonance (MR) imaging has increased dramatically over the
last 10 years. Veterinarians seeking to improve their diagnostic capabili-
ties and clients willing to pursue ''best medicine" have driven this
demand, resulting in the installation of advanced imaging facilities at
most academic and private referral practices. Knowledge of the potential
benefits of various imaging modalities allows veterinarians to optimize
their use of diagnostic imaging in their own practice or in a referral
practice.
SURVEY RADIOGRAPHY
Survey radiography remains the primary diagnostic imaging tech-
nique for evaluation of the lame patient. After localization of the lame-
ness by means of a physical examination, survey radiographs can
quickly and accurately provide morphologic information about the area.
This morphologic characterization of bone and soft tissue abnormalities
can lead to formation of a definitive or differential diagnosis. It can also
delineate the nature and extent of involvement and characterize the
aggressiveness of the lesion. These factors guide further diagnostic tests,
therapeutic plans, and prognoses for the patient. By combining serial
radiographic studies of an area, physiologic information can be inferred
(i.e., fracture healing). The survey radiographic findings in orthopedic
disease are well described in various textbooks.
23
, 36
FLUOROSCOPY
Fluoroscopy involves the use of a continuous beam of x-rays passed
through the patient and directed toward an image-intensifying system
or digital image-recording system. These systems are linked to a video
monitor, allowing real-time evaluation of the patient.
Heat buildup limits the x-ray tube current (and the number of x-rays
that can be produced) during an exposure. Because of the continuous
x-ray production during the fluoroscopic study, the x-ray tube current
(and the number of x-rays produced per unit of time) is much lower
than that used for standard radiographic exposures. Fluoroscopy results
in a much smaller number of x-rays being used to create a Single
image (and thus less detail). Fluoroscopy, however, has the advantage
of allowing evaluation during motion or movement of the patient.
Fluoroscopy can be combined with spot filming to take advantage
of motion and detail. Spot filming involves the temporary increase in the
fluoroscopic x-ray tube current for the production of a higher resolution
radiographic image during fluoroscopy. These spot films may be stored
in a digital format or on radiographic film.
Fluoroscopy may be of value in the evaluation of a number of
musculoskeletal abnormalities.
3D
By manipulation of a limb under the
DIAGNOSTIC IMAGING OF LAMENESS 167
fluoroscope, normal and abnormal joint motion can be assessed under a
range of movements and angles. Fractures may be identified in patients
with inconclusive radiographic findings by manipulation of the limb to
cause the fracture to be seen in tangent to the beam or by removing
overlying osseous and soft tissue structures. This same principle can be
applied to identification of small cartilage lesions of osteochondrosis or
localizing osteochondral bodies in or around joints.
Fluoroscopy can also be used in combination with contrast proce-
dures for the evaluation of a lame patient. Contrast arthrography is
often guided by fluoroscopy. Evaluation of the contrast arthrogram can
be done in real time and during a range of patient motion so as to
more accurately identify small cartilage defects and characterize lesions.
Fluoroscopic guidance can also be of value in guiding biopsy of sus-
pected lesions, In the management of lame animals, fluoroscopy can
guide reduction of osseous structures and placement of orthopedic appli-
ances.
ULTRASONOGHAPHY
Ultrasonography offers a real-time noninvasive method for evalua-
tion of muscular and tendinous structures. Although its role in small
animal musculoskeletal imaging continues to evolve, its use has become
well established in the assessment of equine lameness.
12
Recent improve-
ments in image quality and resolution have resulted in expanded appli-
cation of this technique.
Sound of a specific frequency is directed into a region of the body
by an ultrasound transducer. The interaction of propagated sound waves
with tissue interfaces (differing acoustic impedances) in the body results
in reflection of some of the sound. The transducer detects these reflected
sound waves and converts them into an electric signal that is then
displayed as an ultrasound image.
This imaging modality is particularly well suited to evaluation of
soft tissue structures. Ultrasound travels well through soft tissues and
fluids, and the magnitude of signal is dependent on the number and
orientation of reflectors within the tissue. Because normal tendons and
ligaments consist of many closely aligned parallel fibers, abnormalities
are easily recognized as either high- or low-signal areas in an otherwise
uniform structure. The echogenicity of the lesion also suggests the type
of tissue involved in the lesion (i.e., hypoechogenicity within a tendon
suggests acute hemorrhage or edema and hyperechogenicity suggests
fibrous tissue) (Fig. 1).
In additional to evaluation of tendons and ligaments, ultrasonogra-
phy has a number of other clinical indications in the lame animal.
Ultrasonography can be useful in evaluating the amount and nature of
joint fluid as well as the thickness of the synovium and articular cartilage
and in localizing periarticular mineralization. Although unable to visual-
ize structures beyond the surface of bone, ultrasonography can provide
168 HOSKINSON & TUCKER
Figure 1. Longitudinal ultrasound image of the calcanean tendon of a 5-year-old Viszla
with a history of chronic intermittent lameness. Proximal is to the left, and distal to the right
of the image. There is normal fiber alignment and echogenicity proximally (arrowheads).
Distally there is decreased echogenicity and loss of normal fiber pattern (arrows). A focal
area of mineralization associated with previous injury is noted resulting in hyperechogenicity
with acoustic shadowing.
accurate evaluation of the periosteum, soft tissue tumors invading bone,
and, in some instances, fractures and sequestration. Abscesses, seromas,
hematomas, and other fluid or cystic masses within soft tissues are
easily visualized and can be aspirated with ultrasound guidance for
therapeutic or diagnostic purposes. Diffuse soft tissue changes such
as cellulitis, edema, or hemorrhage can be identified, localized, and
characterized using ultrasonography. Foreign bodies of the soft tissues
of the musculoskeletal system are easily identified (Fig. 2). Using ultra-
sound imaging and Doppler ultrasound, the integrity of the blood sup-
ply to a region can be assessed.
NUCLEAR MEDICINE
Skeletal scintigraphy is one of the most commonly performed veteri-
nary nuclear medicine proceduresY Skeletal scintigraphy (or bone scan-
ning) offers high sensitivity for detecting early disease, and the ease of
evaluation of the entire skeleton (or a region) makes it an ideal tool for
screening cases of obscure or occult lameness. Scintigraphy also offers
an easily quantified method for determining the activity of a bone lesion,
allowing assessment of the significance of radiographically identified
lesions of questionable activity and monitoring of lesions in response
to therapy.
DIAGNOSTIC IMAGING OF LAMENESS 169
Figure 2. A transverse image from the plantar surface of the metatarus of a dog with a
chronic swelling of the distal real limb. The plantar aspects of the metatarsal bones (MT2
and MT3) are identified as curved hyperechoic lines. There is increased thickness to the
soft tissues with a distinct curved hyperechoic structure corresponding to a wooden foreign
body (FB) located plantar (above) the metatarsal bones.
Skeletal scintigraphy involves the intravenous injection of a radio-
labeled phosphonate compound and subsequent imaging of the distribu-
tion of radioactivity within the patient. The most commonly used radio-
pharmaceutical is technetium-99m-labeled methylene diphosphonate
(99mTc-MDP) . The distribution of 99mTc-MDP is dependent on delivery
(blood flow) and uptake (osteoblastic activity). Imaging at different times
after injection allows evaluation of different physiologic processes. The
initial vascular phase follows the course of the radiopharmaceutic
through vessels. After distribution in the blood pool, the 99mTc-MDP
rapidly distributes into the extracellular fluid (ECF) space, resulting in a
soft tissue phase. The 99mTc-MDP is taken up by metabolically active
bone over the next 20 minutes or so. The 99mTc-MDP that is not taken up
by the skeleton is renally cleared. Bone phase images are made 2 to 3
hours after injection to allow an optimal bone-to-soft ti.ssue (target-to-
background) ratio.
Vascular phase images made immediately after injection are depen-
dent primarily on blood flow to a region. They are a sensitive method
of identifying hyperemia, ischemia, and abnormal patterns of flow. Un-
like other methods of evaluation of perfusion, the radionuclide readily
penetrates the (normal or abnormal) superficial soft tissues of the limb,
allowing evaluation of deep and superficial vascular supply. Decreased
flow may be seen after frostbite, degloving injuries, or wrapping of
170 HOSKINSON & TUCKER
objects around the limb. Increased vascular flow may be seen in acute
active lesions with hyperemia or neovascularization.
Soft tissue phase images made 2 to 10 minutes after injection repre-
sent the distribution in the ECF. ECF distribution is determined by
delivery to the region (blood flow), flux in and out of the local ECF
space, and the overall amount of ECF in a region. Decreased activity to
a region can occur with ischemia.
16
Increased activity is commonly seen
at sites of active inflammation as a result of increased blood flow and
capillary permeability. Although these changes are nonspecific, they can
be a sensitive indicator of the site of soft tissue injury such as synovitis,
tendinitis, cellulitis, or bicipital bursitis.
Bone phase images are dependent on blood flow, ECF distribution,
and bone metabolic activity. AlthQugh all normal bone is constantly
remodeling, areas of bone injury often demonstrate increased rates of
bone activity, which subsequently result in increased uptake of radio-
activity visible as "hot spots" on the scan. The degree of uptake of the
99mTc-MDP is determined by the activity at the lesion. Areas of mild
increased turnover occur with mild degenerative joint disease. More
intense uptake occurs at sites of high bone activity such as fractures,
tumors, or infection. Bone lesions typically exhibit increased activity
within 24 to 72 hours after injury, although radiographs may not demon-
strate lesions for up to 2 weeks.
Bone phase images are extremely sensitive and accurate in assessing
occult lameness caused by stress fractures or nonradiographicallY appar-
ent fractures.
26
Because bone phase imaging characterizes the metabolic
activity of bone, it can provide a more sensitive indicator of degenerative
joint disease versus radiographs, which are limited to demonstrating
anatomic changes. Scintigraphy may also identify sites of panosteitis or
bone metastasis before radiographic signs are evident.
1s
In addition to finding lesions that are not apparent, scintigraphy
can characterize the activity at known sites of disease or radiographic
abnormalities. Scintigraphy has been used to determine the level of
activity of degenerative changes at joints/
s
confirm bone involvement
at sites of adjacent soft tissue infection, and monitor healing of bone
injuriesY
Because scintigraphy involves the use of radioactive materials, cer-
tain restrictions to its use apply. Special training and licensing re-
quirements exist in most states for the use of radioactive materials.
Scintigraphy requires moderately expensive equipment ($30,000 and up).
Animals must be placed in radiation quarantine for some period,
usually 12 to 24 hours, during which time, there is a decrease in the
amount of radiation within the patient as a result of biologic and physi-
cal decay.
Scintigraphy is a sensitive but not specific method for assessing
bone lesions. Bone lesions are typically best seen when active. Lesions
may not be seen in animals that have been rested for an extended period
of time or in patients with mechanical causes for lameness.
DIAGNOSTIC IMAGING OF LAMENESS 171
COMPUTED TOMOGRAPHY
CT has become a well-established diagnostic imaging modality for
small animal musculoskeletal diseases.
s
, 10, 13, 14, 20, 2S, 29, 31 In CT, multiple
radiographic projections of a particular slice of tissue are made, and
information from all projections is combined to create a single tomo-
graphic (slice) image, Typical orthopedic CT studies include acquisition
of several thin (1-10 mm) slices through the specific region of interest.
The images can be displayed one at a time or reformatted to create
two- or three-dimensional reconstruction images. Similar to conventional
radiography, the diagnostic information from CT is represented as a
gray-scale image based on the differential x-ray attenuation of tissues,
Unlike radiography, CT information is captured by several radiation
sensors, converted into a digital file, and finally viewed as a tomographic
slice on a computer screen, Whereas conventional radiographs have five
radiographic opacities (metal, bone, soft tissues, fat, and air), CT systems
can record thousands of separate opacities ranging from air to high-
density metal. Each of the possible densities (Hounsfield units) repre-
sents the differential linear coefficients of the x-ray absorption as it
passes through the specific section of tissue, In the development of CT,
water was designated to have a Hounsfield unit value equal to 0, air
was designated to be equal to -1000 Hounsfield units, and dense
cortical bone was designated to be equal to + 3000 Hounsfield units.
The fundamental concepts of CT and MR imaging have been reviewed
recently in the veterinary literature.
7
, 37
There are several advantages of CT in veterinary orthopedics, High
contrast and resolution of osseous tissues are the hallmarks of CT im-
aging, CT allows better visualization of osseous structures than conven-
tional radiography by eliminating opacities caused by superimposed
tissues
13
; thus, a more accurate view of articular surfaces and bone
contours is obtained with CT imaging. Additionally, tomographic dis-
play of CT slices imparts a perception of depth, a third dimension
lacking in conventional radiography,28 Furthermore, the ability to manip-
ulate the digital information can be helpful in orthopedic diseases, Once
the CT scan has been completed, clinicians can review the images in a
variety of display formats to enhance soft tissue or osseous structures
individually. This is accomplished by viewing the CT images under
display parameters selected to concentrate on certain attenuation ranges
(window and level). The "window" width selects the overall range of
Hounsrield units to be displayed, The "level" sets the center of the range
of Hounsfield units to be displayed, Orthopedic images are commonly
reviewed in a "soft tissue window" (e,g" window width = 400 Houns-
field units, window level = 40 Hounsfield units) and a "bone window"
(e.g., window width = 2000 Hounsfield units, window level = 400
Hounsfield units) (Fig, 3),
Another useful feature of CT is the ability to create reconstruction
images from the original acquisition data.
28
During CT acquisition, the
tissue slices must be oriented perpendicular to the body part as it is
172 HOSKINSON & TUCKER
Figure 3. Identical transverse CT slices of the elbow joint of a dog displaced in soft tissue
(A) and bone (B) windows.
moved through the imaging gantry. The x-ray attenuation information
from these slices is stored as a three-dimensional numeric matrix in the
computer's memory. It is later possible to create "reconstruction" slices
(i.e., images in a plane other than that in which the information was
obtained) along any desired image axis within the numeric matrix.
This may be helpful when alternate imaging planes provide additional
diagnostic information or determine treatment options.
28
Surface con-
tours of bones and joints can also be created by reconstructing original
slice data into three-dimensional surface views (Fig. 4).
Conventional radiographic arthrography techniques with negative
or positive (radiopaque) contrast agents can be used in combination
Figure 4. Surface reconstruction CT images of the ventral (A) and dorsal (B) aspects of a
dog pelviS. The ori ginal data was acquired in axial slices, and reformated for three-
dimensional display.
DIAGNOSTIC IMAGING OF LAMENESS 173
with CT scanning.
32
High-resolution thin-slice arthrogram images pro-
duced by CT scanning may demonstrate lesions undetected on standard
contrast radiography. Myelography and epidurography can also be per-
formed with CT, yielding superior visualization of the contrast columns
within the spinal canal.
Skeletal CT may be helpful in clinical cases in which standard
radiography is negative or inconclusive and there is a high suspicion of
osseous pathology.19,28 CT allows detection of density differences as low
as 0.5% versus approximately 30% with conventional radiography. As
a result, CT reveals osteolysis and osteogenesis before conventional
radiography can detect such changes.
The ability to view images in several image planes may help to
better delineate fracture orientation or bone fragmentation. The use of
CT in complex fractures can aid in planning the repair process or may
reveal articular involvement unrecognized with standard radiographic
projections (Fig. 5). CT has also been helpful in the diagnosis of osteo-
chondral defects and other bone growth disorders.19, 28 The sensitivity of
CT to detect fragmented medial coronoid disease in young dogs has
been reported to be 88% compared with 50% sensitivity using conven-
tional radiography alone.lO CT has also been used to diagnose ununited
anconeal processes and incomplete ossification of humeral condyles. 20, 31
In addition to diagnostic imaging, CT has applications in orthopedic
research. For example, CT offers the ability to noninvasively quantitate
the volume and density of the osseous reaction to various implants,
compounds, or treatment protocols.
13
, 21 Mineral content of bone can be
Figure 5. Sagittal CT image of a fracture of the lateral trochlear ridge (arrow) that was not
visible on survey radiography.
174 HOSKINSON & TUCKER
approximated within user-defined regions of interest. Cross-sectional
area of long bones and volumetric analysis of bone sections can be
accurately calculated with CT.
There are certain limitations and artifacts that must be considered
with the use of CT in orthopedic diseases. Inherently, the diagnostic
strength of CT is its superior evaluation of bone; although better than
with conventional radiography, distinct contrast between different soft
tissues remains poor with CT. Metal devices create expansive CT artifacts
because of the sum effect of the high attenuation metal, which is of
particular concern to orthopedic imaging. Even small orthopedic im-
plants cast beam-hardening artifacts that partially obscure visualization
of the tissues surrounding them. Whenever the x-ray beam travels
through substantial volumes of dense bone and metal, lower energy
x-rays are absorbed by the dense material, and the mean energy of the
x-ray beam becomes increased. The tissues on the far side of the dense
object seem more radiolucent than expected because of the higher energy
beam overpenetrating the distal tissues. Such artifacts should be antici-
pated in specific anatomic regions, along certain anatomic planes, or if
metal implants or external devices are present.
Another misleading CT artifact is the "slice thickness" or "volume
averaging" artifact. The attenuation information of each tomographic
slice actually displays the average attenuation within each small volume
(voxel) of the tissue. At certain tissue interfaces, the margins or borders
are indistinct or fuzzy. These artifacts can lead to a false impression of
bony proliferation or periosteal reactions.
Several generations of CT scanners have been developed since its
original introduction in 1970. Each new generation improves the spatial
resolution and decreases the time required to perform examinations.
Modern helical CT systems are now available with spatial resolution of
less than 1 mm and require scan times of less than 1 minute for an entire
scan. A comprehensive CT examination can often be performed in less
time than that required for the multiple survey radiographic views
necessary to yield similar information. Despite the rapid scan times,
anesthesia or profound sedation is required to eliminate patient motion,
which results in image degradation.
With CT scanners becoming more common in veterinary medicine,
orthopedic applications should continue to expand. The excellent osse-
ous detail obtained with CT is unsurpassed with other imaging techno-
logies, and the ability to reconstruct images in any image plane can be
helpful in evaluating complex fractures and articular trauma.
MAGNETIC RESONANCE IMAGING
MR imaging characterizes the magnetic properties of tissues and
does not rely on the x-ray attenuation used in radiographic and CT
studies. MR imaging yields excellent tissue contrast based on emphasiz-
ing the differences in magnetic properties of each tissue. With increasing
DIAGNOSTIC IMAGING OF LAMENESS 175
accessibility and decreasing costs, MR imaging has become a valuable
modality for lameness evaluations in some small animal pa-
tients.
imaging is typically performed in several different MR imaging
se9.uences that emphasize different magnetic properties of
tIssues. T2-wei.ghted, and proton density (PD) properties
are c?mmonly The time between the radiofrequency pulses and
the tIme fr?m the radlOfrequency pulse to the emitted signal are chosen
to emphaSIze one or more of these magnetic properties and determine
the specific contrast and appearance of tissues. The timing of acquisition
sequences can be selected to highlight tissue characteristics within articu-
lar cartilage, synovial fluid,3 or cortical and subchondral bone. A con-
ventional MR imaging examination called a spin-echo sequence includes
Tl -weighted, PD, and T2-weighted images. Simplified, Tl-weighted im-
a.ges emphasize the anatomic characteristics of tissue, PD images display
contrast based on the relative free proton concentrations of each
tIssue, and T2-weighted images emphasize the fluid characteristics of
are sensitive to certain types of pathologic changes. Special-
Iz:ed Imagmg sequences such as gradient echoes or fat-suppression tech-
mques can be used to eliminate or enhance specific tissues and are
helpful when evaluating orthopedic disease.
3o
In addition to the type of
the. MR selects several imaging parameters, including
shce orIentation, the thIckness and spacing between the slices, and the
use of contrast agents.
Paramagnetic contrast agents such as gadolinium can be combined
:-vith 0R to changes in vascularity and vascular
mtegrIty withm tissues, whIch can occur with neoplastic and inflamma-
tory dIseases. Before contrast administration, images are obtained
through the area of interest. Immediately after administration of the
gadolinium, repeat T1-weighted images are acquired through the same
regIon. Increased permeability and disruption of vascular integrity cause
leakage of the contrast agent into tissues, resulting in increased T1-
weighted signal.
. field strength is measured in tesla (T). Currently, MR
systems used in clinical veterinary medicine range from low-
field magnets (20.064 T) to high-field magnets (2:1.0 T) . The higher field
are of faster scanning times and have better
slgnal-to-n?ISe Image qualIty. Unfortunately, high-field strength systems
are expenSIve to purchase and maintain, limiting them to referral centers
and vetermary colleges. permanent magnets are less expensive
to and mamtam b:rt result in longer scan times and poorer
qualIty Images. Because motion degrades the image quality, long scan
hmes are a problem for veterinary patients.
Because MR imaging requires the patient to lie motionless for sev-
e.ral minutes, anesthesia is usually required for veterinary pa-
tients. In addItion, the strong magnetic field prohibits ferromagnetic
metals .from being situated close to the magnet system. Nonferrous
magnetIc devices (most surgical implants) can be safely introduced into
176 HOSKINSON & TUCKER
the magnetic field, but even small nonferrous metallic implants may
create large imaging artifacts that interfere with visualization of adja-
cent tissue.
s
MR imaging has several advantages for imaging of orthopedic dis-
eases. One of the primary advantages of MR imaging is the ability to
acquire images in any desired anatomic plane. This ability to select the
slice orientation relative to specific structures improves the diagnostic
capabilities of this modality. Second, the high-resolution MR images
demonstrate remarkable tissue contrast in osseous and soft tissue struc-
tures.
Veterinary orthopedic applications of MR imaging have been re-
ported for evaluation of tendons, ligaments, and synovial linings such
as in examinations for bicipital tenosynovitis.
3
, 13, 37 MR imaging has been
reported as an excellent method of imaging cruciate ligament (Fig. 6)
and meniscal injuries
4
(Fig. 7) and facilitates the early detection of articu-
lar cartilage destruction.
9
,41 Other proven applications include the detec-
tion of osteochondrosis, subchondral bone necrosis, osteomyelitis, or
invasive neoplasia of osseous structures
19
(Fig. 8). MR imaging may also
be helpful in the diagnosis of elbow dysplasia.
28
, 33, 34 The potential to
detect early cartilage and subchondral changes is an obvious advantage
of MR imaging over other imaging modalities in orthopedic diseases.
38
The optimal imaging sequences for articular cartilage evaluation, how-
ever, are still under investigation.
3D
41
Development of quantitative MR
assessment techniques, including measurement of magnetic transfer,
Figure 6. Sagittal T1-weighted MR image positioned to visualize the normal cranial cruciate
ligament (arrow). Ligaments and cortical bone structures appear dark due to relatively low
content of unbound hydrogen atoms (fat and water) .
DIAGNOSTIC IMAGING OF LAMENESS 177
Figure 7. Sagittal 'f.2-weighted image of a dog with a tear in the caudal meniscus (arrow).
The area of the meniscal tear appears white (high signal) from hemorrhage and edema at
this si te.
Figure 8. Axial T2-weighted image of a dog with a fragmented medial coronoid process
(FMCP) . A low signal (black) line separat'3s the coronoid fragment from the remainder of
the ulna (U). While cortical bone appears dark, the fat in the marrow of the ulna has a high
signal (white area).
178
HOSKINSON & TUCKER
changes in signal intensity, and physical diffusion parameters, may offer
the best methods to detect early stages of cartilage abnormalities.
6
,18
Gadolinium contrast agents can also be used for MR arthrography,
although the benefits are unproved in veterinary medicine,s, 38 Use of a
500- iJ-M solution of gadolinium-DTPA was found to be unrewarding in
delineation of normal articular cartilage and cartilage lesions in dogs
with scapulohumeral oste6chondrosis,39 It has been suggested that the
appearance of articular cartilage seen with contrast administration in
cadaver joint studies differs from that of articular cartilage in live ani-
mals, The use of specific imaging sequences to emphasize the appearance
of fluid (strong T2 effect) may yield a sufficient "arthrogram-like"
effect to eliminate the need for contrast, Future modifications of contrast
may include incorporating gadolinium into encapsulated liposomes to
reduce contrast agent diffusion into articular cartilage for better demar-
cation between the joint space and hyaline cartilage,22
The advantages of MR imaging for the diagnosis of spinal and
intervertebral disk disease have been well established in human beings,
In dogs, MR imaging has proven particularly valuable in evaluation of
the lumbosacral region, where conventional radiography, myelography,
and epidurography are often inconclusive,l MR imaging has also proven
helpful for the diagnosis of perispinal and nerve sheath tumors,
Several important limitations to MR imaging must be recognized.
The requirement of general anesthesia and the time required for scan-
ning must be considered, The costs of the purchase and maintenance of
the equipment limit availability to referral centers or to teaching institu-
tions. Some veterinarians have developed agreements with human facili-
ties to use their MR imaging systems on a fee basis, MR scanning is . a
technical, involved, and interactive process; thus, skilled technical sup-
port is essential. In addition, interpretation of the images requires a
precise knowledge of anatomy and normal tissue patterns, MR imaging
examinations can include several images and multiple sequences, which
must be carefully reviewed and compared, Optimal imaging sequences
and parameters still need to be determined for most veterinary orthope-
dic applications. With continued clinical and research experience, this
modality should become an important orthopediC tool in veterinary
medicine,
CONCLUSIONS
The demand for advanced diagnostic imaging procedures such as
nuclear scintigraphy, ultrasonography, CT, and MR imaging has in-
creased dramatically over the last 10 years. Veterinarians seeking to
improve their diagnostic capabilities and clients willing to pursue "best
medicine" have driven this demand, resulting in installation of advanced
imaging facilities at most academic and private referral practices, Knowl-
edge of the potential benefits of various imaging modalities allows
DIAGNOSTIC IMAGING OF LAMENESS 179
veterinarians to optimize the use of diagnostic imaging in their own
practice or in a referral practice,
References
1. Adams WH, Daniel GB, Pardo AD, et al: Magnetic resonance imaging of the caudal
lumbar and lumbosacral spine in 13 dogs (1990- 1993) . Vet Radiol Ultrasound 36'3- 13
1995 . ,
2. Baird OK, Kincaid SA, Hathcock JT, et al: Effect of hydration on signal intensity on
gelatin phantoms usmg low-fIeld magnehc resonance imaging: Possible application in
osteoarthritis, Vet Radiol Ulh'asound 40:27- 35, 1999
3. Baird OK, Hathcock JT,. Kincaid SA, et al: Low-field magnetic resonance imaging of
early subchondral cyst-like leSIOns m mduced cranial cruciate ligament deficient dogs
Vet Radiol Ultrasound 39:167-173, 1998 .
4. OK, Hathcock JT, Rumph PF, et al: Low-field magnetic resonance imaging of the
canme stifle Jomt: Normal anatomy, Vet Radiol Ultrasound 39:87-97, 1998
5. Banfield CM, Morrison WB: Magnetic resonance arthrography of the canine stifle
1':)1nt: Technique and applicahons m eleven military dogs. Vet Radiol Ultrasound
41:200- 213, 2000
6, Bashir A Gray ML, Hartke J, et al: Nondestructive imaging of human cartilage
glycosammoglycan concentration by MRI. Magn Reson Med 41:857-865,1999
7. Berry CR: Anatomic and physiologic imaging of the canine and feline brain. In Thrall
DE (ed): Textbook of Veterinary Diagnostic Radiology, ed 3. Philadelphia, WB Saun-
ders, 1998, pp 66-79
8. Braden TO, Stikle, RL: Dejardin LM, et al: The use of computed tomography in
fragmented coronOid disease: A case report. Vet Comp Orthop Traumatol 7:40-44, 1994
9. EM, Brandt KD, Albrecht M: MRI demonstration of hypertrophic articular
carhlage repmr m osteoarthnhs. Skeletal RadioI19:335-339, 1990
10, Carpenter LG, Schwarz PO, Lowry JE, et al: Comparison of radiologic imaging tech-
mques for diagnOSIs of fragmented medial coronoid process. JAVMA 203:78- 83 1993
11 , Chambers MD: Bone imaging: The diphosphonates, In Daniel GB, Berry CR (eds):
Handbook of Vetermary Nuclear Medicine, Raleigh, North Carolina State University
1996, pp 49-59 '
12. Craychee TJ: Ultrasonographic evaluation c;f equine musculoskeletal injury. II1 Nyland
TG, Mattoon JS (eds): Vetermary Diagnostic Ultrasound. Philadelphia WB Saunders
1995, pp 265-304 ' . ,
13. Fitch RB, Hathcock JT, Montgomery RD: Radiographic and computed tomoaraphic
evaluahon of the camne mtercondylar fossa in normal stifles and after notchplasty in
stable and unstable shfles. Vet Radiol Ultrasound 37:266-274 1996
14, Fitch RB, Wilson ER., Hathcock JT, et al: Radiographic, tomographic and
magnetic. resonance Imagmg evaluation of a chronic long digital extensor tendon
avulsIOn m a dog. Vet Radiol Ultrasound 38:177-181,1997
15. Forrest LJ, Thrall DE: Bone scintigraphy for metastasis detection in canine osteosar-
coma. Vet Radiol Ultrasound 35:124-130, 1994
16. Goggin JM, Hoskinson n, Carpenter JW, et al: Scintigraphic assessment of distal
extremIty perfusion in 17 patients. Vet Radiol Ultrasound 38:211- 220, 1997
17. Hathcock JT,. Rumph PF, Kincaid SA, et al: Low-field magnetic resonance imaging of
the canme shfle Jomt: Normal anatomy. Vet Radiol Ultrasound 39:87-97, 1998
18, KaufmanJH, Regatte RR, Bolinger L: A novel approach to observing articular cartilage
m Vitro VIa magnehc resonance imaging. J Magn Reson Imaging 9:653-
19. Kippenes H, Johnston GJ: Diagnostic imaging of osteochondrosis. Vet Clin North Am
Small Anim Pract 28:137- 160, 1998
20. Marcellin-Little OJ, DeYoun OJ, Ferris KK, et al : Incomplete ossification of the humeral
condyle m spaniels. Vet Surg 23:475-487, 1994
21. Markel MD, Winkenheiser MA, Morin RL, et al: Non-invasive measurement of the
180 HOSKINSON & TUCKER
material properties of bone healing with quantitative computed tomography, magnetic
resonance imaging, single photon absorptiometry, and dual energy x-ray absorptiome-
try. Vet Surg 19:71, 1990
22. Matteucci ML, Thrall DE: The role of liposomes in drug delivery and diagnostic
imaging: A review. Vet Radiol Ultrasound 41:100-107, 2000
23. Morgan JP, Wolvekamp P: Radiology of the Traumatized Dog and Cat. Philadelphia,
JB Lippincott, 1994
24. Nordberg CC, Johnson KA: Magnetic resonance imaging of normal canine carpal
ligaments. Vet Radiol Ultrasound 40:128-136, 1999
25. Papageorges M, Gavin PR, Barbee DD, et ale Quantitative joint scintigraphy in a
lentivirus-induced arthritis in goats. Vet Radiol Ultrasound 32:82-86, 1991
26. Pleasant RS, Baker GJ, Muhlbauer Me, et ale Stress reactions and stress fractures of
the proximal palmar aspect of the third metacarpal bone in horses: 58 cases (1980-
1?90). JAVMA 201:1918-1923, 1992
27. Recht MP, Resnick D: MR imaging of articular cartilage: Current status and future
directions. AJR Am J Radiol 163:283-290, 1994
28. Reichle JK, Snaps FR: The elbow. Clin Tech Small Anim Pract 14:177- 186, 1999
29. Reichle JK, Park RD, Bahr AM: Computed tomographic findings of the cubital joint of
dogs with lameness. Vet Radiol Ultrasound 41:125-130, 2000
30. Resnick D: Fluoroscopy. In Bone and Joint Imaging, ed 2. Philadelphia, WB Saunders,
1996, pp 51-52
31. Rovesti GL, Fluckiger M, Margini A, et ale Fragmented coronoid process and incom-
plete humeral condyle in a rottweiler. Vet Surg 27:354-357, 1998
32. Sartoris DJ, Kursunoglu S, Pineda C, et ale Detection of intra-articular osteochondral
bodies in the knee using computed arthrotomography. Radiology 155:447-450, 1985
33. Snaps FR, Balligand MH, Saunders JH, et ale Comparison of radiography, magnetic
resonance imaging and surgical findings in dogs with elbow dysplasia. Am J Vet Res
58:1366-1370, 1997
34. Snaps FR, Saunders JH, Park RD, et al: Comparison of spin echo, gradient echo and
fat saturation magnetic resonance imaging sequences for imaging the canine elbow.
Vet Radiol UltrasOlmd 39:518-523, 1998
35. Suter PF: Normal radiographic anatomy and radiographic examination. In Thoracic
Radiography: Thoracic Disease of the Dog and Cat. Wettswil, Switzerland, PF Suter,
1984, p 2
36. Thrall DE: Textbook of Veterinary Diagnostic Radiology, ed 3. Philadelphia, WB Saun-
ders, 1999
37. Tidwell AS, Jones JC: Advanced imaging concepts: A pictorial glossary of CT and MRi
technology. Clin Tech Small Anim Pract 14:65-111, 1999
38. Tirman PFJ, Bost FW, Garvin GJ, et ale Posterosuperior glenoid impingement of the
shoulder: Findings at MR imaging and MR arthrography with arthroscopic correlation.
Radiology 193:431-436, 1994
39. Van Bree H, Van Ryssen B, Degryse H, et ale Magnetic resonance arthrography of
the scapulohumeral joint in dogs, using gadopentetate dimeglumine. Am J Vet Res
56:286-288, 1995
40. Van Bree H, Degryse H, Van Ryssen B, et ale Pathologic correla tions with magnetic
resonance images of osteochondrosis lesions in canine shoulders. JAVMA 202:1099-
1105,1993
41. Widmer WR, Buckwalter KA, Braunstein EM, et a1: Radiographic and magnetic reso-
nance imaging of the stifle joint in experimental osteoarthritis of dogs. Vet Radiol
Ultrasound 35:371-383, 1994
42. Wilkens BE, Millis DL, Daniel GB, et al: Metabolic and histologic effects of recombinant
canine somatotropin on bone healing in dogs. Am J Vet Res 57:1395-1401, 1996
Address reprint reques ts to
James J. Hoskinson, DVM
College of Veterinary Medicine
Kansas State University
Manhattan, KS 66506
LAMENESS
,::
0195-5616/ 01 $15.00 + .00
ANCILLARY DIAGNOSTIC
TECHNIQUES FOR THE
LAME PATIENT
Mary Ann Radlinsky, DVM, MS
. The of lameness is usually identified through evaluation of
SIgnalment, histo;ry, physical examination (including neurologic and
exammatlOns). RadiographiC evaluation provides a definitive
m many cases; .however, evaluation may prove
m the of certam conditions (i.e., inflammatory
J<;>mt dIsorders, systemIC dIsorders) or m prognostication of the condition
(l.e., serum alkalIne phosP?hatase [SAP] levels in dogs with appendicular
osteosarcoma).6, 9, 12, 14, 16, 18, _3, 29, 30,32 In some instances where the definitive
diagnosis elu.sive. (i,e., medial coronoid process),
arthrOSCOpIC exammahon IS a mmimally invasive diagnostic tool that
may be .more and available . than computed tomography.19
ThIS evaluation of the lame patient and
arthroSCOPIC evaluatlOn of Jomt abnormalities.
ROUTINE LABORATORY EVALUATION
Hematology
. Results of a complete blood cell count (CBC) are normal in most
patients that are presented for lameness (i.e., degenerative arthropathy,
developmental or congemtal abnormalities, neoplasia), Any animal that
IS for and has other systemic clinical signs such as
fever, artIcular swellmg, anorexia, malaise, or cutaneous lesions should
From the Department of Clinical Sciences, Kansas State University Veterinary Medical
Teaching Hospital, Manhattan, Kansas '
VETERINARY CLINICS OF NORTH AMERICA: SMALL ANIMAL PRACTICE
VOLUME 31 NUMBER 1 JANUARY 2001 181
182 RADLINSKY
undergo routine laboratory evaluation.
6
, 11, 14, 16, 23, 33 Likewise, any lame
animal with unexpected changes on a CBC should be evaluated for
concurrent disorders that mayor may not be associated with lameness.
Hematology is valuable in patients with undiagnosed arthropathies; in
those cases, the CBC may reflect multisystemic disorders or infectious
disease.J4 23 Occasionally, animals may have neutrophilia, monocytosis,
or lymphopenia, reflecting chronic stress associated with their disease
or with bouts of active inflammation.
23
In traumatic injuries, the CBC
reflects the severity of damage sustained; patients may develop abnor-
malities, including anemia, thrombocytopenia, and many variations in
leukocyte numbers.
Anemia is not an indicator of any specific condition resulting in
lameness. Anemia may simply reflect chronic inflammatory disease,
which may be associated with nutnerous types of bone and joint disor-
ders. Chronic renal failure can cause nonregenerative anemia and may
be a cause of lameness as a result of renal secondary hyperparathyroid-
ism or via its association with rickettsial disease or immune-mediated
conditions such as systemic lupus erythematosus (SLE).6, 11, 14, 23 Hemo-
lytic anemia occurs in 10% to 20% of patients with SLE, and animals
with drug-induced arthritis may have anemia, thrombocytopenia, and
leukopenia.
23
Dogs with ehrlichiosis or SLE may have Coomb's positive
anemia, but dogs with Rocky Mountain spotted fever (RMSF) and Lyme
borreliosis are usually Coomb's negative.
6
, 11, 12 Anemia, thrombocyto-
penia, leukopenia, and pancytopenia may occur with any rickettsial
disease.
6
,11 Granular lymphocytosis may be present with Ehrlichia canis
infection, and morulae may be noted on blood smears of dogs with E.
canis.
6
Thrombocytopenia has been reported in all phases of ehrlichiosis,
and it is the most consistent laboratory abnormality associated with
Rickettsia ric7cettsii, the agent of RMSP' 10 Dogs with RMSF tend to
hemorrhage at higher platelet counts than dogs with ehrlichiosis. Leuko-
penia followed by leukocytosis and anemia is also commonly observed
with RMSP Consistent changes in CBC have not been reported with
Lyme borreliosisY
The patient's leukogram is thus rarely indicative of a specific diag-
nosis, and its abnormalities may reflect chronic inflammation, primary
or secondary infection, systemic disorders, or bone marrow abnormali-
ties. The character of the white blood cells (WBCs) and presence or
absence of a left shift are important to the interpretation and importance
of the CBC findings. The leukogram should always be interpreted in
conjunction with the patient's signalment, history, and other physical
examination findings.
Biochemical Profile
As is the case with the CBC, a biochemical profile may be used to
investigate concurrent clinical signs and systemic or infectious disease
in cases of lameness. Degenerative joint disease and congenital or devel-
ANCILLARY DIAGNOSTIC TECHNIQUES FOR lHE LAME PATIENT 183
opmental disorders do not usually result in abnormalities in serum
biochemistry. Biochemical values in young animals with developmental
diseases may be consistent with young age (i.e., low total protein and
elevated calcium, phosphorus, and SAP). As is the case with the CBC,
traumatic injuries may cause changes in the biochemical profile that
reflect the severity of the trauma and the organs affected.
An abnormal biochemical profile may be present with a variety of
systemic illnesses associated with bone or joint pain. For example, liver
enzyme abnormalities would be expected in animals with hepatopathic
arthritis. J4, 23 Renal values, including blood urea nitrogen, creatinine,
and phosphorus, may be elevated in animals with renal secondary
hyperparathyroidism. In those cases, calcium may be within the normal
range, but phosphorus is usually elevated.
23
With nutritional secondary
hyperparathyroidism, calcium may be normal, but phosphorus and SAP
may be elevated in young growing dogs that are fed a balanced diet,
thereby complicating the diagnosis based on serum biochemistry alone.
23
Hypocalcemia and hypophosphatemia and elevated SAP are expected
in young dogs with rickets.
23
The alkaline phosphatase bone isoenzyme
can be elevatec;l. in any patient with increased bone turnover. SAP may
thus be increased in cases of bacterial or fungal osteomyelitis or bony
neoplasia. Elevation in SAP has been reported as a prognostic indicator
in dogs with appendicular osteosarcoma.
9
A number of biochemical profile changes may be present in animals
with inflammatory polyarthritis. Animals with SLE may have hepatic or
renal abnormalities on serum chemistry reflective of the multisystemic
nature of the condition.
14
Rickettsial arthritides, including RMSF and
ehrlichiosis, may result in elevations in serum protein, globulins, alanine
amino transferase, and SAp' 6, 11, 12 Albumin may be decreased because
of renal loss or compensation for hyperglobulinemia, and electrolyte
abnormalities may be present because of the systemic effect of
vasculitis.
6
,13 In canine ehrlichiosis, hyperglobulinemia is more promi-
nent than in RMSF and may be characterized by electrophoresIs as a
mono- or polyclonal disease.
6
, 11 Hypercholesterolemia and elevated se-
rum glucose have been reported with RMSF, and renal failure leading to
azotemia has been noted late in the diseaseY No consistent biochemical
changes have been reported with Lyme borreliosis, but renal azotemia
may occur late in the course of the disease as is the case with RMSF12
In septic arthritis, the primary site of infection may be the urinary
tract, resulting in azotemia as a result of pyelonephritis. Multiple organ
systems may become affected in septic patients, leading to variable
abnormalities in electrolytes and liver enzymes, as well 'as to azotemia.
Urinalysis
Proteinuria may occur with ehrlichiosis, RMSF, rheumatoid arthritis
(RA), and SLE, possibly resulting in a decline in serum albumin. n,23
Protein or creatinine may be increased depending on the cause of pro-
184 RADLINSKY
teinuria.23 Hematuria may also occur secondary to coagulation abnor-
malities (i.e., RMSF) and should be evaluated with the rest of the urine
sedimentY An active sediment would be expected if hematuria is the
result of an infectious process.
ARTHROCENTESIS
Synovial fluid analysis is a useful tool in the diagnosis of joint
disorders in the dog and cat and can be used to guide further diagnostic
tests and treatment. The first step in interpretation is the determination
of the process present, differentiating inflammatory from noninflamma-
tory disease. Within the inflammatory category, one must then determine
whether the process is septic or not. Culture and susceptibility testing
of joint fluid is recommended in any case of inflammatory arthritis. It
can also be difficult to differentiate between the causes of nonseptic
inflammatory joint disease, and further diagnostic testing is usually
warranted in those cases.
Fluid Collection
Sedation may be required for successful arthrocentesis, but rarely is
general anesthesia required; the patient should be adequately restrained
to minimize motion and trauma to the joint. Fluid may be collected from
the shoulder, elbow, carpus, hip, stifle, or hock.
13
.
18
Distal joints are often
involved with pauci- or polyarthropathies and are easy to sample. In
polyarthropathies, it is recommended that more than one joint be sam-
pled even in apparently normal joints. Proximal joints are difficult to
sample; they lack obvious bony landmarks and may require general
anesthesia and wide skin preparation for palpation and atraumatic
arthrocentesis.
The shoulder may be approached laterally or medially; the elbow is
approached caudomedially or laterally, or laterally or medially; and the
carpus is usually sampled dorsally at the radiocarpal jointY 18. 30 The
coxofemoral joint may be sampled from a lateral or ventral direction;
the stifle is approached medially or laterally; and the tarsocrural joint is
sampled from a plantar, dorsal, medial, or lateral approachY 18. 30 The
landmarks used for arthrocentesis have been described.
13
. 18. 29 The skin
around the joint should be clipped with a number 40 blade and prepared
with surgical scrub and rinse solution. 13. 18 Sterile gloves and strict aseptic
technique are recommended for fluid collection.
J3
18 A 20- to 22-gauge
needle and 3-mL syringe usually suffice; it is rare that large amounts of
joint fluid are obtained even from inflamed joints.
n
. 18. 30 Blood contami-
nation may occur before or at the end of aspiration; negative pressure
should cease when blood is identified, and the needle should be changed
if hemorrhage occurs before penetration of the joint. Cytologic examina-
tion (number, type, and integrity of the nucleated cells) is the most
important aspect of fluid analysis. Secondary to cytologic evaluation is
ANCILLARY DIAGNOSTIC TECHNIQUES FOR THE LAME PATIENT 185
culture and susceptibility information. Once slides are made for exami-
nation and a sample is procured for culture, the remaining fluid may be
placed in an ethylenediarninetetra-acetic acid (EDTA) tube.
Fluid Examination
Synovial fluid is normally clear and colorless to slightly yellow and
is highly viscous. It forms a 2.5-cm string when a drop is suspended
between the tip of the needle and a microscope slide or between two
fingers; viscosity is lost with degradation or dilution of hyaluronic
acid.
14
.
18
Significant hemarthrosis or xanthochromia is abnormal. Iatro-
genic blood contamination may be differentiated from hemarthrosis on
centrifugation; in hemarthrosis, the supernatant remains yellow to red
from chronic red blood cell contamination. 14. 30 Decreased joint fluid
viscosity is also expected with true hemarthrosis but not with a small
amount of iatrogenic blood contamination.
Nucleated cell count, cytology, and culture samples should be per-
formed first; total protein measurement and a mucin clot test should
only be done {f sufficient volume remains. WBC numbers can be esti-
mated based on a direct smear, but actual cell counts are desired.
3
. 18. 29
Normal joint fluid contains less than 1500 to 3000 WBCs per microliter,
with a predominance of mononuclear cells (90%); neutrophils represent
less than 5% to 10% of the normal cell count.14. 18. 22. 30 Noninflammatory
conditions, including degenerative joint disease, may be normal on
fluid analysis or may result in nucleated cell counts up to 10,000 per
microliter. 18. 23 Most cells should be mononuclear, although vacuolated
changes in the mononuclear cells may increase (10%).18 Neutrophils and
red blood cell numbers may also be elevated, but hemorrhage associated
with degenerative arthropathy is usually minimaP8
A significantly elevated nucleated cell count in joint fluid is indica-
tive of an inflammatory arthropathy. Nonerosive immune-mediated ar-
thritis is the predominant inflammatory joint disorder in dogs. WBCs
are elevated from 3000 to 100,000 per microliter. 14. 23 Neutrophils predom-
inate and range from 30% to 100% of the cells seen.1
4
.
23
Mononuclear
cells are often vacuolated, and lupus erythematosus (LE) cells may be
present in SLE; LE cells are phagocytic cells that have phagocytosed
nuclei from cells opsonized by antinuclear antibody (ANA)Y Erosive
arthritis, or RA, results in 6000 to 85,000 WBCs per microliter with a
majority of neutrophils (20%-95%), some of which may show degenera-
tive changes.
14
Free nuclear material and ragocytes (neutrophils con-
taining cytoplasmic inclusions of phagocytized immune complexes) may
also be identified in synovial fluid from cases of RA,14.3o Synovial fluid
from dogs with plasmacytic-lymphocytic gonitis contains 5000 to 20,000
WBCs per microliter with 10% to 40% neutrophils; lymphocytes predom-
inate in this inflammatory condition.
J4
30
Cell counts in septic arthritis range from 40,000 to 100,000 per
microliter or greaterY Degenerative neutrophils and bacteria mayor
186 RADLINSKY
may not be identified on cytology.23 111e
arthritis increase cell counts, and organisms may b.e.1dentified . . Synov1al
changes with Lyme borreliosis include neutrophil1c \> 95%)
tion (cell count range, 5,000-100,000 per microliter) w1th an elevation m
proteinY
Microbiologic Examination
Septic arthropathies tend to be whereas
inflammatory conditions are usually polyarticular but can pauCl- or
monoarticularY' 23,32 Degenerative changes of :n:-af be
absent on examination of joint fluid in septic arthr1tis, makmg d1fficult
to differentiate septic from nonseptic inflammatory arthropathies. Bacte-
rial culture and susceptibility testing is
in any case of inflammatory joint disease. Jo:nt flUld 1S all that 1S
for culture (synovial biopsies are not reqUlred); however, negative cul-
tures may result in 50% of cases handled with. culturettes.
30
, 32
The fluid sample should be diluted at a 1:9 ratio m aerob1c culture
media for transport, and samples incubated for 24 hours m the blood
culture media consistently yielded positive results in one Syno-
vial fluid samples should be transported to m bl?od
culture media and cultured immediately for rap1d te.stmg;
the sample should again be cultured after 24 hours of J? the
culture media for the best possible yield.
21
of. d1fficulty
associated with isolation, the requirement for speClal faCliltles, and the
risk of human infection, rickettsial isolation testing is rarely per-
formedY, 12
OTHER SEROLOGY
Cases of idiopathic polyarthritis are negative on
serology, ANA, LE preparation, factor (RF) testing,
microbial culture.
14
, 23 In endemic areas, confrrmatlon of RMSF reqUlres
indirect immunofluorescent antibody (!FA) titers, usually acute
valescent IgG titers (convalescent titers .are run 2-:-3 the llutlal
sample),u It is recommended that w1th any ncketts1al titer, . the two
samples be run at the same time in one laboratory,. fourf?ld
are diagnostic of active infection. are
often positive in endemic may the. d1agnos1s of
RMSF as a result of cross-reactiv1ty.6, 11 Definitive d1agnos1s can be ob-
tained with direct immunofluorescence on tissue samples or
chain reaction (PCR) amplification of rickettsial DNA, the latter of which
is currently not widely available.
6
, . .
Ehrlichiosis can likewise be d1agnosed by md1rect IFA or enzyme-
linked immunosorbent assay.6,11 Some nonpathogenic sF:ecies .can cross-
react with E. canis; however, cross-reaction with R. rzCkettSll, Brucella
ANCILLARY DIAGNOSTIC TECHNIQUES FOR THE LAME PATIENT 187
canis, Ehrlichia platys, or Ehrlichia equi is considered milikely.6, 11 A positive
E. canis titer is considered diagnostic; however, 20.3% of healthy kennel
dogs in endemic areas had increased antibody titers to E. canis.n Titers
peak at 80 days in infected untreated dogs, but the patient should
seroconvert with effective treatment.
6
Ehrlichia ewingii causes polyarthri-
tis in dogs and may result in a positive result on E. canis IFA testing.
PCR or immunoblotting can distinguish between the two infections, but
rarely is PCR justified because of the similarity of therapy for either
ehrlichial infection.
6
, ]] , 23 Lyme borreliosis may be diagnosed with titers
also, but dogs in endemic areas may have positive titers as a result of
exposure alone.
30
A positive Lyme's titer outside an endemic area is
considered diagnostic for Lyme borreliosis.
12
It is recommended that as
for RMSF, paired titers be measured simultaneously by one laboratory. 6, 12
Otl1er Borrelia species may cross-react on IFA testing, and immunoblot-
ting or enzyme-linked immunosorbent assay testing may improve the
specificity of diagnosis in the futureY Also remember that thrombocyto-
penia is not a common finding with Lyme borreliosis, which may be
useful in ruling in or out the conditiony,23
RFs are ouly present at a low level in 25% to 70% of dogs with RA
depending on the specificity and sensitivity of the test system.14, 23 The
most common RF in dogs is IgM, and tests in human beings evaluate
the presence of IgG RF.3, 14 RF also may be positive in up to 5% of normal
dogs or in dogs with other diseases such as idiopathic polyarthritis,
heartworm disease, pyometra, and SLE.14, 23, 30 ANA may be detected in
some dogs with RAY Immunofluorescence testing is considered to be a
reliable test for ANA detection.
4
, 14 Dogs with SLE are usually RF-
negative, may have LE cells on examination, and should be ANA-
positive. The ANA titer should be evaluated in light of the multisystemic
nature of the disease as well as other possible diagnoses. ANA, however,
may be positive in cases of persistent inflammatory diseaseY, 30 Normal
dogs or dogs with diseases other than SLE should not have an ANA
titer greater than 1:40.
30
ARTHROSCOPY
Arthroscopy has become more popular in veterinary medicine as a
minimally invasive diagnostic and therapeutic techni que for a variety of
joint disorders. The associated recovery time has been shown to be
shorter than with arthrotomy, and destabilization of the joint should not
occur.
s
Magnification of the joint surface, joint capsule, and intra-articu-
lar structures along with joint irrigation may make arthroscopy better
than arthrotomy as a diagnostic tool in some instances (i.e., soft tissue
structural abnonnalities.
1
, 5, 16, 27 Lesions may be diagnosed before degen-
erative changes are present on radiographs.
1s
Because the technique is
less invasive, anesthetic time should be reduced compared with
arthrotomy. 'n,27
Few disadvantages accompany arthroscopy, the most important of
188 RADLINSKY
which is technical difficulty, which must be considered in light of the
expensive equipment required for the procedure.
16
, 18, 19 The ease and
speed of the procedure are depender:t on skill of the
Other disadvantages include small vlsual fields confined wlthin a ngld
space and the fragility of equipment, both of less of
problem with time and are compllcatlOns.assoCl-
ated with arthroscopy, the nsk of whlch also declmes wlth expenence.
Instrumentation
A 2.7-rnrn 30 oblique arthroscope is most commonly used with a
xenon light source.
1
-
3
, 16, 18, 19,24,28 Hypodermic needles or a Verres needle,
sharp trochar, blunt obturator, arthroscope sleeve, egress and
irrigation solution are required for ..'-3, 16, 18, 19, 24, _8 A camera
and video screen are useful, as the entIre surglcal team can Vlew and
assist in the procedure. A of ca:mu.lae are required for
surgical therapy. Tools used for jomt mampulatlOn mclude a
probe (which can add depth perception and measurements to dlagnostIc
arthroscopy), grasping forceps, basket forceps, curettes, and. an arthr.os-
copy knife.
1
-
3
, 16, lB, 19.24,28 Power instruments are also hel:pf,ul m removmg
free fragments, foreign bodies, or osteophytes from the Jomt and mclude
shavers, bits, and burrs.' 8
Technique
The patient should be placed in the po.sition
for the joint to be evaluated, and the surroundmg halr should be clIpped
as for an arthrotomy.18 Strict asepsis should be to, and
sion to an arthrotomy should always be consldered and pOSSIble: '
Aseptic preparation of the skin and sterile 11mb
should be positioned to allow full range of motion of the Jomt.
The landmarks for portal and needle placement have been described
for the shoulder, elbow, carpus, hip, stifle, and hock.
'
-
3
, 16, 18, 19,24,28 The
shoulder is approached caudolaterally, and the elbow is approached
medially because of the ease of portal placement and visibility of medial
structures.
1
, 2, 18, 28, 35, 36 The carpus may be approached dorsally, the hip
dorsolaterally, and stifle craniolaterally or craniomedially.3, 5, 16, 18, 19, 27,
31,32 A combination of approaches may be used for complete exploratIOn
of the hock; dorsolateral or dorsomedial and plantarolateral approaches
are used.
1s
,35
Before port placement, a hypodermic or used. to
aspirate joint fluid for analysis and to distend the
solution.
1
-
3
, 16, 18, 19, 24,26 Once the joint is distended, the skm IS 1l1.ClSed over
the proposed cannula or arthroscope insertion site, and a trochar is used
to penetrate the fascia and joint.
'
-
3
, 16, 18.. 19, 24. A sharp trochar. can
penetrate the soft tissues easily but has a higher nsk of artIcular cartilage
ANCILLARY DIAGNOSTIC TECHNIQUES FOR THE LAME PATIENT 189
d<i"inage; in most cases, a blunt obturator suffices for entering the joint
with minimal trauma. The carmula remains in place, the trochar or
obturator is removed, and the arthroscope is placed into the joint
through the carmula and locked into place.
1
-
3
, 16, 18, 24, 28 Any time the
cannula is repositioned, a blunt obturator should be m place rather than
a sharp trochar or the arthroscope so as to avoid iatrogenic trauma or
instrument damage. When the arthroscope is in place, irrigation solution
is attached to the arthroscope for constant infusion and visualization.
Sterile isotonic crystalloid solutions are usually used for irrigation
of the joint during arthroscopy. The most cOrnni.only used solution is
lactated Ringer's solution, but no difference was noted between lactated
RinO'er's solution, saline, and sterile water in one study.1-3, 16, 19,24,28 A I-
to bag of irrigation solution may be cOlUl.ected to an infusion set,
extension set, and arthroscope for free flow of solution into the joint.
Other means of irrigating the joint include use of a manual infusion bag,
a three-way stopcock and a 30-mL syringe for intermittent infusion, an
infusion pump, or a syringe pump. Pressurized infusion should not
exceed 50 mm Hg at any time.
1S
Drainage of the fluid from the joint is
achieved thro1.lgh the needle used to distend the joint or, more appropri-
ately, by replacing the needle with an egress catheter to reduce the risk
of iatrogenic trauma.
1
, 2, 16,18,19 If periarticular fluid accumulation occurs,
the skin incisions may be enlarged to encourage fluid to escape.
18
After the joint has been explored, a second portal may be required
for therapeutic intervention. Instrument portal landmarks have been
described.
18
Of utmost importance is the concept of triangulation: the
instrument portal should be placed so that the angle between it and the
arthroscope is appropriate for easy orientation but not so narrow as to
cause interference between the arthroscope and surgical instruments. IS
A needle can be inserted at the proposed instrument portal to check
placement and angulation before inserting the instrument,
which is placed similar to the initial arthroscope cannula. Free bodIes or
cartilage flaps may be removed en toto with forceps or piecemeal with
power instruments. A bone curette or automated shaver can be used to
curette the subchondral bone as necessary. On completion of the proce-
dure, local anesthetic may be instilled into the joint, and the fascia,
subcutis, and skin are closed as dictated by the procedure.'8
Uses
Arthroscopy has been used in clinical and research situations, in-
cluding diagnostic evaluation of joints, removal of loose fragments or
foreign bodies, debridement with septic arthritis, osteophyte excision,
synovectOlny with RA, and arthrolysis of contractures. 1,2,5,16, ]8, 19. 24,25,27.28.
31,32 Arthroscopy has proven to be useful in research situations requiring
multiple evaluations of a joint; no adverse effects were associated with
repeated arthroscopic examinations of the stifle in dogs.
31
Arthroscopy
has been recommended in cases with signs of joint disease on physical
190 RADLINSKY
examination and radiographs, including joint capsular thickening, in-
creased volume of synovial fluid, periarticular swelling, osteophyte for-
mation, bony sclerosis, narrowed joint space, cartilaginous or osseous
defects or deformities, bone chips or fragments, and joint laxity. IS Diag-
noses made by arthroscopy include osteochondritis dissecans (OCD),
meniscal injuries, fragmented medial coronoid process, degenerative
joint disease, intra-articular synovitis, bicip-
ital tendon rupture, and neoplasIa.
Is
Therapeutlc mterventIOn can be
achieved arthroscopically in cases of OCD of the shoulder, elbow, stifle,
and hock; fragmented medial coronoid process; and ruptured cranial
cruciate ligament.
2
.
s
. IS. 2S . . .
In clinical cases, arthroscopy has been successful at dlagnosmg stifle
abnormalities in dogs. The procedure resulted in a correct diagnosis
from 83% to 92% of the time in the stifle of clinical patients.
19
. 32 Surgery
could have been avoided in 39% of cases, the diagnosis being that of
degenerative joint disease alone.
32
Overinterpretation led to 17% false-
positive results in that bu: both studies found
contributed important addltlonal mformatIOn to that gamed by physlcal
examination and radiography.1
9
. 32 One experimental study found that
stifle arthroscopy and surgery were correct in 99% of cases, with one
horizontal tear in the medial meniscus seen with arthroscopy but not
with surgery and one excessively folded meniscus diagnosed with
arthroscopy but not seen with arthrotomy or at necropsy.16 One
reported arthroscopically guided stabilization of the cruciate-defiClent
stifle in dogs; however, the implant failed, and stifle instability re-
turned. 27
Arthroscopy of the shoulder and stifle for OCD has resulted in
decreased lameness after surgery but it was difficult to evaluate the
caudal portion of the femoral condyle with arthroscopy.s. 28 After arthros-
copy of the shoulder, 61% of dogs used the limb within 24 hours of
surgery, and 35% used the limb within 48 hours of
arthroscopy of stifle OCD, the dogs used the affected 11mb wIthln 24
hours, and most were using the limb at a level equal to that observed at
the preoperative evaluation within 1 to 3 days after surgery.s Only one
dog had a prolonged recovery after stifle arthroscopy, which was a result
of iatrogenic meniscal trauma.
s
In dogs and cats, arthroscopy has also been used to identify the
cause of chronic shoulder pain.
2
It was determined that the arthroscope
was valuable in identifying lesions of the humeral and glenoid margins,
capsular laxity, and medial glenohumeral ligament and bicipital tendon
trauma.
2
Arthroscopy was also used to develop a drawer test for shoul-
der instability in that study.2
Complications
The risk associated with arthroscopy decreases with experience of
the arthroscopist. Iatrogenic articular cartilage trauma can occur at the
time of trocharization; use of the blunt obturator and egress catheter
may also decrease the incidence of cartilage trauma.
1
, 3, 16, 18. 28, 32 Care
ANCILLARY DIAGNOSTIC TECHNIQUES FOR THE LAME PATIENT 191
should also be taken when manipulating power instruments within the
joint. Higher irrigation flow is required to avoid negative pressure and
air aspiration into the joint.
1s
Hemorrhage and hyperplastic synovial villi may also obscure visu-
alization during arthroscopy.I. 16. 18. 28 Knowledge of regional anatomy
and appropriate landmarks for portal placement is important in avoiding
trauma to the neurovascular structures.
1
. 18 Use of cooled irrigation solu-
tion may decrease the minimal hemorrhage normally associated with
cannula placement.
16
Periarticular accumulation of fluid can compromise
the optical window and end the procedure prematurely.ls Appropriate
infusion of fluids, widening skin incisions, and appropriate egress cathe-
terization are appropriate measures to avoid fluid accumulation. 1. 3, 16,18
Swelling after arthroscopy normally is absorbed within 24 to 48 hours
after surgery. 3. 16. 18. 2B
A final costly complication associated with arthroscopy is instru-
ment damage. With experience and careful controlled manipulation,
damage to the arthroscope and associated instruments can be avoided. lB.
2S, 32 Undue force and leverage should be avoided while working with
delicate instruments in a small confined joint space.
References
1. Bardet JF: Arthroscopy of the elbow in dogs. Part I: The normal arthroscopic anatomy
using the craniolateral portal. Vet Comp Orthop Traumatol 10:1, 1997
2. Bardet JF: Diagnosis of shoulder instability in dogs and cats: A retrospective study. J
Am Anim Hosp Assoc 34:42, 1998
3. Bell SC, Carter SD, May C, et al: IgA and IgM rheumatoid factors in canime rheumatoid
arthritis. J Small Anim Pract 34:259, 1993
4. Bennett D: Immune-based non-erosive inflammatory joint disease of the dog. 1. Canine
systemic lupus erythematosus. J Small Anim Pract 28:871, 1987
5. Bertrand SG, Lewis DD, Madison JB, et al: Arthroscopic examination and treatment of
osteochondritis dissecans of the femoral condyle of six dogs. J Am Anim Hosp Assoc
33:451, 1997
6. Breitschwerdt EB: The rickettsioses. In Ettinger SJ, Feldman EC (eds): Textbook of
Veterinary Internal Medicine, ed 5. Philadelphia, WB Saunders, 2000, p 400
7. Breitschwerdt EB, Hegarty BC, Davidson MG, et at Evalua tion of the pathogenic
potential of Rickettsia canada and Rickettsia prowazekii organisms in dogs. JAVMA
207:58, 1995
8. Cowell RL, Tyler RD, Clinkenbeard KD, et al: Ehrlichiosis and polyarthritis in three
dogs. JAVMA 192:1093, 1988
9. Ehrhart N, Dernell WS, Hoffmann WE, et al: Prognostic importance of alkaline phos-
phatase activity in serum from dogs with appendicular osteosarcoma: 75 cases (1990-
1996). JAVMA 213:1002, 1998
10. Frank JR, Breitschwerdt EB: A retrospective study of ehrlichiosis in 62 dogs from
North Carolina and Virginia. J Vet Intern Med 13:194, 1999
11. Greene CE, Breitschwerdt EB: Rocky mountain spotted fever, Q fever, and typhus. In
Greene CE (ed): Infectious Diseases of the Dog and Cat, (ed 2). Philadelphia, WB
Saunders, 1998, p 155
12. Greene CE, Appel MJG, Straubinger RK: Lyme borreliosis. In Greene CE (ed): Infectious
Diseases of the Dog and Cat, (ed 2). Philadelphia, WB Saunders, 1998, p 282
13. Hardy RM, Wallace LJ: Arthrocentesis and synovial membrane biopsy. Vet Clin North
Am Small Anim Pract 4:449, 1974
14. Hopper PE: Immune-mediated joint disease. In Slatter DS (ed): Textbook of Small
Anim.al Surgery, ed 2. Philadelphia, WB Sawlders, 1993, p 1928
192 RADLINSKY
15. Hoskins JD, Breitschwerdt EB, Gaunt SD, et al: Antibodies to Ehrlichia canis, Ehrlichia
platys, and spotted fever group rickettsiae in Louisiana dogs. J Vet Intern Med 2:55, 1988
16. Johnson KA, Watson ADJ: Skeletal diseases. In Ettinger SJ, Feldman EC (eds): Text-
book of Veterinary Internal Medicine, ed 5. Philadelphia, WB Saunders, 2000, p 1887
17. Lewis DD, Goring RL, Parker RB, et al: A comparison of diagnostic methods used in
the evaluation of early degenerative joint disease in the dog. J Am Arum Hosp Assoc
23:305, 1987
18. Lozier SM, Menard M: Arthrocentesis and synovial fluid analysis. In Bojrab MJ (ed):
Current Techniques in Small Animal Surgery, ed 4. Baltimore, Williams & Wilkins,
1998, P 1057
19. McCarthy TC: Arthroscopy. In Freeman LJ (ed): Veterinary Endosurgery. St. Louis,
Mosby, 1999, P 237
20. Miller CW, Presnell KR: Examffiation of the canine stifle: Arthroscopy versus arthrot-
omy. J Am Anim Hosp Assoc 21:623, 1985
21. Montgomery RD, Long IR, Milton JL, 'it aI: Comparison of aerobic culturette, synovial
membrane biopsy, and blood culture medium in detection of canine bacterial arthritis.
Vet Surg 18:300, 1989
22. Neer MT: Carline monocytic and granulocytic Ehrlichiosis. In Greene CE (ed): Infec-
tious Diseases of the Dog and Cat, (ed 2). Philadelphia, WB Saunders, 1998, p 139
23. Pedersen NC, Morgan JP, Vasseur PB: Joint diseases of dogs and cats. In Ettinger Sf,
Feldman EC (eds): Textbook of Veterinary Internal Medicine, ed 5. Philadelphia, WB
Saunders, 2000, p 1862
24. Perille AL, Matus RE: Carline ehrlichiosis in six dogs with persistently increased
antibody titers. J Vet Intern Med 5:195, 1991
25. Person MW: Arthroscopic treatment of osteochondritis dissecans in the canine shoul-
der. Vet Surg 18:175, 1989
26. Person MW: Arthroscopy of the canine coxofemoral joint. Compend Contin Educ Pract
Vet 11:930, 1989
27. Person MW: A procedure for arthroscopic examffiation of the canine stifle joint. J Am
Anim Hosp Assoc 21:179, 1985
28. Person MW: Prosthetic replacement of the cranial cruciate ligament under arthroscopic
guidance. Vet Surg 16:37, 1987
29. Piermattei DL, Flo GL: Orthopedic examination and diagnostic tools. In Small Animal
Orthopedics and Fracture Repair. Philadelphia, WB Saunders, p 3
30. Schrader SC: The use of the laboratory in the diagnosis of joint disorders of dogs and
cats. In Bonagura JD (ed): Kirk's Veterinary Therapy XII. Philadelphia, WB Saunders,
1995, p 1166
31. Siemering GB, Eilert RE: Arthroscopic study of cranial cruciate ligament and medial
meniscallesions in the dog. Vet Surg 13:265, 1986
32. Slnith MM: Orthopedic infections. In Slatter DS (ed): Textbook of Small Animal Sur-
gery, ed 2. Philadelphia, WB Saunders, 1993, p 1685
33. Van Gestel MA: Diagnostic accuracy of stifle arthroscopy in the dog. J Am Anim Hosp
Assoc 21:757, 1985
34. Van Ryssen B, van Bree H, Vyt P: Arthroscopy of the shoulder joint in the dog. J Am
Anim Hosp Assoc 29:101, 1993
35. Van Ryssen B, van Bree H, Vyt P: Arthroscopy of the carline hock joint. J Am Anim
Hosp Assoc 29:107, 1993
36. Van Ryssen B, van Bree H, Simoen P: Elbow arthroscopy in clinically normal dogs.
Am J Vet Res 54:191, 1993
Addres s reprint requests to
MaryAnn Radlinsky, DVM, MS
Department of Clinical Sciences
Kansas State University
Veterinary Medical Teaching Hospital
106A Mosier Hall
1800 Denison Avenue
Manhattan, KS 66506-5606
e-mail: Radlinsk@Vet.ksu.edu
LAMENESS 0195-5616/ 01 $15.00 + .00
t. ':
KINETIC AND KINEMATIC GAIT
ANALYSIS IN DOGS
Ron M. McLaughlin, DVM, DVSc
Gait analysis can accurately assess normal arid abnormal gait, iden-
tify characteristic features of specific gait abnormalities, and quantify
gait so that "numeric comparisons can be made between different
populations.
2
, 19 Kinesiology is the science of animal motion and includes
kinetics (the forces that affect motion) and kinematics (the temporal
and geometric characteristics of motion).2 Kinetic gait analysis can be
performed using a force plate to obtain a noninvasive, objective, and
quantitative assessment of the forces occurring between the foot and the
surface of the plate during the stance phase of the stride (ground-
reaction forces). 2 Data relative to the swing phase of the stride are not
measured. Successive strides during locomotion cannot be measured by
a single force plate; however, a series of plates or a force plate built into
a treadmill can be used to evaluate consecutive strides.
4
,21 Kinematic
gait analysis is performed using a series of cameras and retroreflective
targets placed on the dog's skin over specific anatomic landmarks. 1, 12 A
computer measures the flexion and extension movements of joints and
the temporal and distance variables of the dog's gait as it passes through
a three-dimensional testing area. This method provides information rela-
tive to the stance and swing phase of the dog's stride. In most cases,
kinematic analysis is combined with force-plate analysis so that dynamic
three-dimensional characteristics of limb motion can be correlated with
ground-reaction force measurementsY
From The Animal Health C e n t e l ~ College of Veterinary Medicine, Mississippi State Univer-
sity, Mississippi State, Mississippi
VETERINARY CLINICS OF NORTH AMERICA: SMALL ANIMAL PRACTICE
VOLUME 3J NUMBER J JANUARY 2001 193
194 McLAUGHLIN
FORCE-PLATE ANALYSIS
Equipment
A force plate consists of sensing elements covered by a top plate.
The force plate must be mounted firmly to a rigid level surface that does
not yield or shift when force is applied. Ideally, the platform is attached
to a heavy metal mounting plate, which is secured to a concrete founda-
tion. The plate may be recessed into a floor, or a walkway can be
constructed around the force plate level with the surface of the top plate.
The walkway must not touch the force plate or it may interfere with
data collection. It is important that the plate does not shift when force
is applied to the top plate, or erroneous results may be obtained. The
top plate is usually covered to provide a nonslip surface and to protect
it from damage; however, the covering must not absorb impacting forces
or significantly change the distance from the plate to the sensors. Force
plates are available. in numerous sizes. If the plate is small, the subject
may not contact the plate properly during each pass. If the plate is large,
the subject may strike the plate with more than one foot simultaneously
during each pass and invalidate the trial.
When a subject steps on the force plate, the magnitude of the force
is measured by deflection of the sensing elements within the plate.
2
The
displacement of the sensing elements is proportional to the force applied
to the plate and creates an electric signal, which is amplified and re-
corded by computer. Three orthogonal ground-reaction forces are meas-
ured: mediolateral (Fx), craniocaudal or braking/propulsion (Fy), and
vertical (Fz) (Fig. 1).2 Most force-plate systems can trigger data collection
to begin when a minimum force is applied to the plate or when a
Figure 1. The three orthogonal ground-reaction forces measured during force-plate analy-
sis. Solid arrow indicates forward progression. X = mediolateral force; Y = craniocaudal
force; Z = vertical force.
KINETIC AND KINEMATIC GAIT ANALYSIS IN DOGS 195
rnlhirnum voltage is generated by the sensors. The system can thus be set
to collect data beginning with the initial forelimb contact. Alternatively,
collection can be triggered by the operator. The sampling frequency
(measured in hertz as number of samples collected per second) and the
sampling time (duration in seconds) can be adjusted and determine the
amount of data collected. Collecting data at higher frequencies allows
detection of minute rapid changes in gait; however, significantly more
computer memory is required to store the data. The time of data collec-
tion depends on the velocity of the subject and should be long enough
to include the portion of the stride being evaluated. In most cases, data
are collected for the entire stance phase of the ipSilateral forelimbs and
hind limbs. Force data are collected at the designated frequency, and a
force-versus-time curve is generated by a computer. The force-versus-
time curve is a graphic representation of the ground-reaction forces
generated during the stance phase of the stride. Force is generally
reported in newtons or kilograms of force; time is reported as seconds
of stance time. Force plates can also measure vertical torque, center of
pressure, and coefficient of friction, although these parameters are not
commonly used in canine gait analysis.
A force plate may have strain gauges as the sensing elements.
2
When the top plate is loaded, deflection or bending of the metal foil
gauge produces an electric output (microstrain) The material within. the
strain gauge changes electric resistance in proportion to the deformation.
The strain gauges are connected to an electric circuit, which measures
the change in resistance and determines the force applied to the plate.
Strain gauge systems are durable and quite sensitive. Newer force plates
have eliminated the "cross-talk" b e t w ~ e n strain gauges so that the three
orthogonal forces can be accurately and independently measured. The
strain elements undergo repeated mechanical deflections with use; thus,
periodic adjustments of the bridge excitation voltage and recalibration
of the system are typically necessary. Strain gauge force plates are able
to measure forces within a specific range without recalibration; however,
applying a force that overloads the strain gauge can cause permanent
damage.
Piezoelectric force-plate systems rely on the inherent material prop-
erties of quartz crystals.
2
Quartz crystals respond to changes in shape
by generating an electric charge (piezoelectric effect) and can be oriented
to respond to external forces. Quartz crystals are placed in sensors
within the force plate. When load is applied, crystal deformation pro-
duces voltage proportional to the applied force. The electric output is
collected by electrodes attached to the surface of the crystals, amplified,
and recorded by computer for display and analysis. Data from sensing
elements in the four corners of the plate are integrated to determine the
orthogonal ground reaction forces applied to the plate even if the force
is not applied to the exact center of the plate. Piezoelectric systems are
highly sensitive over a large measuring range. The same plate has
been used to accurately measure the heartbeat of a standing subject
(ballistocardiography) and impact forces from automobile crashes. Be-
196 McLAUGHLIN
cause piezoelectric systems rely on crystal deformation to generate an
electric output, they can be extremely rigid, which allows for a higher
natural frequency, a larger measuring range, and a durable plate. Piezo-
electric force plates do not require periodic adjustments or recalibration,
do not require an external electric energy source to obtain an output
signal, and are not damaged by overloading.
Collecting Force-Plate Data
During data collection, the dog is led across the force plate by a
handler. The dog must cross the plate in a consistent manner and the
handler must not interfere in anyway while the dog is in contact with
the plate. Pulling on the leash or minor changes in the dog's body
position such as lowering or raising the head affect the ground-reaction
force measurements obtained. The plate should be inconspicuously
mounted so that the dog does not shy away or alter its gait when
approaching the plate. Each pass across the plate is evaluated by an
observer to confirm foot strikes and gait and to ensure that there is no
interference with the stride. Video recording of each pass allows re-
evaluation and documentation of valid trials. A valid trial generally
consists of distinct ipsilateral forefoot and hind foot strikes. If other feet
contact the plate, or if more than one foot contacts the plate simultane-
ously, the forces applied by the Utdividuallimbs cannot be distinguished,
and the trial is invalid. Repeated passes across the plate are usually
required to obtain a sufficient number of valid trials. For each valid trial,
orthogonal ground reaction forces in the forelimbs and hind limbs are
measured and recorded. In most situations, variation is minimized by
acquiring numerous valid trials and averaging the results to determine
a representative gait pattern.
During each trial, the dog's forward velocity is measured. This can
be achieved using a millisecond timer and two photoelectric ::;witches.
26
The timer is started when the dog passes through one photoelectric
beam and is stopped when the dog passes through the second beam.
The known distance between the photoelech'ic switches is used to calcu-
late the subject's velocity. Care must be taken to ensure that the dog
consistently triggers the timer and that a constant speed is maintained
across the plate during each trial. Acceleration or deceleration affects
force values and can be difficult to control. Use of accelerometers may
help to minimize variation during data collection.
s
Cinematography can
also be used to determine the dog's velocity.
Numerous factors can affect the generation of ground-reaction
forces during gait analysis.
2o
,30 Studies evaluating the effect of velocity
variation on ground-reaction forces and stance times in dogs at the walk
and trot found that peak vertical forces increased as velocity increased.'4,
30,31 Stance times decreased as velocity increased.
2
4-26, 29, 31 These findings
demonstrate the importance of controlling the subject's speed during
gait analysis. Only trials collected within a specific velocity range should
KINETIC AND KINEMATIC GAIT ANALYSIS IN DOGS 197
he considered valid. If velocity is not limited to a narrow range, it is
unclear if changes in ground-reaction force measurements are a result of
gait differences or velocity variation. This is important when serially
evaluating uldividual dogs (e.g., comparing pretreatment and posttreat-
ment data) and when comparing data collected from different popula-
tions of dogs. Other factors known to cause variance in force-plate data
include inherent subject variation, variation in trial repetitions for each
subject, interday variation, handler differences, force-plate sensitivity,
morphometric differences between subjects, and limb acceleration and
deceleration.
2
, 6, 20, 32 These potential causes of variance should be con-
trolled carefully during data collection. When such factors are controlled
by consistent data collection methods, the variance in force-plate data is
low, providing an accurate, and repeatable assessment of limb function
and allowing reliable comparisons between dogs and comparisons of
clinical cases with known research data.
Evaluation of Force-Plate Data
Ground-reaction force data can be presented graphically as force-
versus-time curves (Fig. 2). Mathematic transformation may be used to
analyze the curves and identify subtle gait changes indicative of subclini-
callameness.
19
26, 36 Fourier transformation decomposes the force-versus-
a 100 300 500 700 900 1100
Time (ms)
Figure 2. A force-versus-time curve from a normal dog at walk. The first peak is the
forelimb stance phase; the second peak is the hind limb stance phase.
198 McLAUGHLIN
time curves into sine and cosine components, allowing mathematic
reconstruction of the curve and making comparisons of graphic curves
convenient and reliable.
36
These methods allow evaluation of the entire
force-versus-time curve (or specified portions of the curve) but require
complex mathematic and statistical procedures.
Force plate data may also be presented numerically. Selected peaks
and slopes are chosen and analyzed for each of the orthogonal
ground reaction forces. Frequently evaluated parameters mclude peak
(maximum) force, average force, impulse (force over time), rate of load-
ing, and rate of unloading. Vertical force is the largest of
forces and is the one most commonly evaluated for galt analysis m
animals. Mediolateral and craniocaudal (braking/propulsion) forces are
smaller in magnitude and may be more significantly affected by external
factors. Force data are often normalized with respect to the dog's body
weight, because evaluation of force as of bod.y weight
eliminates variation caused by changes m the weight of subjects and
allows comparisons to be made between dogs of different weights. The
mean values of several trials are used for statistical comparisons between
docys and between evaluation times. Changes in peak force, impulse, or
slope and evaluation of the symmetry
information about limb function. Changes m the distnbutlOn of force m
the limbs caused by various types of lameness have also been evalu-
atedY' 34, 35 In most research studies, force-plate data from dogs are
pooled and compared with data from the same population at different
times (i.e., before and after treatment) .
Studies Using Force-Plate Analysis in Dogs
The force plate has been used to study normal gait and to evaluate
experimentally induced and naturally occurring lameness in dogs. Nu-
merous studies have been performed in healthy dogs to document
normal gait and to identify sources of variati.on.
6
, 9, 11, 20, 24, 25, 32, 33,
These studies have led to a better understandmg of normal canme galt
as well as to improved data collection techniques. Other studies have
evaluated the effects of lameness on force distribution to other limbs.
17
,
34,35 Additionally, force-plate gait analysis has been used to evaluate
common causes of lameness and their various treatments, including hip
dysplasia,s, 10, 14, 22, 23, 26 cruciate ligament injur.y/ ' 15, 16,
and osteoarthritis.s,37 The use of force-plate galt analysis m these studies
provided accurate and repeatable data on limb function and an objective
measurement of the efficacy of each treatment method. Currently, the
force plate is primarily a research tool used to evaluate lameness and its
treatment. As urlderstanding of force-plate technology and expenence
with clinical lameness increase, its use as a diagnostic aid in clinical
cases of lameness should increase,
KINETIC AND KINEMATIC GAIT ANALYSIS IN DOGS 199
KINEMATIC GAIT ANALYSIS
Collection of kinematic data allows accurate description of the com-
plex movements of gait but requires specialized equipment,l, 3, 12, 13, 18
Four video cameras linked to a video processor and computer are
positioned to simultaneously record the subject'S motion as it passes
through the three-dimensional testing space. Retroreflective targets are
placed on the dog's skin over specific anatomic landmarks. As the dog
is walked or trotted through the testing space, the video cameras record
the movement of the retroreflective targets. The computer then analyzes
the data from all four cameras by direct linear transformation to deter-
mine the relative positions of each target in three-dimensional spaceY
With this technology, a great deal of information can be gathered, includ-
ing subject velocity, the segmental velocities of each portion of the limb,
stride length and frequency, joint angles (flexion and extension data),
angular velocities, and temporal data. 1, 3, 12, 13, 18 This information can also
be correlated with kinetic data by integration of a force plate into the
testing space.
12
Kinematic gait analysis of dogs has been used to study the normal
gaits (walk and trot) and to evaluate dogs with hip dysplasia and
cruciate ligament rupture.
1
, 3, 12, 13,18 Although this technology is relatively
new to veterinary research, it holds great promise for future study of
lameness and treatment of joint disease in dogs.
SUMMARY
Kinetic and kinematic gait analysis provides objective, quantifiable,
and repeatable information on normal and abnormal gait in dogs, Data
collection requires specialized equipment, and techniques must be care-
fully controlled to ensure that accurate measurements are obtained.
Force-plate and kinematic analysis is currently used primarily as a
research tool to study various gait abnormalities and objectively assess
treatment efficacy. As future research identifies characteristic changes
associated with specific types of lameness, the use of gait analysis to
evaluate individual clinical patients with lameness should become more
valuable. Specialized gait analysis techniques may eventually enable
veterinarians to accurately diagnose subtle lameness, better evaluate
dogs with resolving lameness, and accurately select the appropriate time
to return an athletic dog to exercise after recovery from an injury.
References
1. Allen K, Decamp CE, Braden TD, et al: Kinematic gait analysis of the trot in healthy
mixed breed dogs. Vet Comp Orthop Traumatol 7:148- 153, 1994
2. Anderson MA, Mann FA: Force plate analysis: A noninvasive tool for gait analysis.
Compend Contin Educ Pract Vet 16:857-867, 1994
200 McLAUGHLIN
3. Bennett RL, DeCamp CE, Flo GL, et al: Kinematic gait analysis in dogs with hip
dysplasia. Am J Vet Res 57:966-971, 1996
4. Bertram JEA, Lee DV, Todhunter RI, et ale Multiple force plateform analysis of the
canine trot: A new approach to assessing basic characteristics of locomotion. Vet Comp
Orthop Traumatol 10:160-169, 1997
5. Budsberg SC, Rytz U, Johnston SA: Effects of acceleration on ground reaction forces
collected in healthy dogs at a hot. Vet Comp Orthop TraumatoI12:15-19, 1999
6. Budsberg SC, Verstraete MC, Soutas-Little RW: Force plate analysis of the walking gait
in healthy dogs. Am J Vet Res 48:915-918, 1987
7. Budsberg SC, Verstraete MC, Soutas-Little RW, et ale Force plate analyses before and
after stabilization of canine stifles for cruciate injury. Am J Vet Res 49:1522-1524, 1988
8. Budsberg SC, Johnston SA, Schwartz PD, et ale Efficacy of etodolac for the treatment
of osteoarthritis of the hip joint in dogs. JAVMA 214:206- 210, 1999
9. Budsberg Sc, Jevens DJ, Brown J, et ale Evaluation of limb symmetry indices using
ground reaction forces in healthy d o g ~ . Am J Vet Res 54:1569-1574, 1993
10. Budsberg SC, Chambers IN, Van Lu SL, et aI: Prospective evaluation of ground
reaction forces in dogs lmdergoing unilateral total hip replacement. Am J Vet Res
57:1781-1785,1996
11. Budsberg SC, Verstraete MC, Brown J, et al e Vertical loading rates in clinically normal
dogs at a trot. Am J Vet Res 56:1275-1280, 1995
12. Decamp CE, Soutas-Little RW, Hauptman I, et ale Kinematic gait analysis of the trot
in healthy Greyhounds. Am J Vet Res 54:627-634, 1993
13. Decamp CE, Riggs CM, Olivier NB, et al: Kinematic evaluation of gait in dogs with
cranial cruciate ligament rupture. Am J Vet Res 57:120-126, 1996
14. Deuland R, Bartel DL, Antonson E: Force-plate technique for canine gait analysis of
total hip and excision arthroplasty. J Am Anim Hosp Assoc 13:547-552, 1977
15. Dupuis J, Harari I, Papageorges M, et ale Evaluation of fibular head transposition for
repair of experimental cranial cruciate ligament injury in dogs. Vet Surg 23:1-12, 1994
16. Geels J, Roush JK, Hoskinson JJ, McLaughlin RM: Long-term follow-up of the under-
and over-fascia lata graft technique for stabilization of cranial cruciate ligament rup-
tures in 21 dogs. Vet Comp Orthop Traumatol, in press
17. Griffon DJ, McLaughlin RM, Roush JK: Vertical ground reaction force redistribution
during experimentally induced shoulder lameness in dogs. Vet Comp Orthop Trau-
matol 7:154-157, 1994
18. Hottinger HA, DeCamp CE, Olivier NB, et ale Noninvasive kinematic analysis of the
walk in healthy large-breed dogs. Am J Vet Res 57:381-388, 1996
19. Jacobs NA, Skoreki I, Charnley J: AnalYSis of the vertical component of force in normal
and pathological gait. J Biomech 5:11-34,1972
20. Jevens DJ, Hauptman JG, DeCamp CE, et ale Contributions to variance in force-plate
analysis of gait in dogs. Am J Vet Res 54:612-615, 1993
21. Kram R, Powell AJ: A treadmill-mounted force platform. J Appl Physiol 67:1692-
1698, 1989
22. Manley PA, Vanderby R, Dogan S, et ale Ground reaction force comparison of canine
cemented and cementless total hip replacement. Clinical Biomechanics 5:402-407,1990
23. Mann FA, Tanger CH, Wagner-Mann C, et al: A comparison of standard femoral head
and neck excision and femoral head and neck excision using a biceps femoriis muscle
sling in the dog. Vet Surg 16:223- 230, 1987
24. McLaughlin RM, Roush JK: Effects of subject stance time and velocity on ground
reaction forces in clinically normal Greyhounds at the trot. Am J Vet Res 55:1666-
1671, 1994
25. McLaughlin RM, Roush JK: Effects of increasing velocity on braking and propulsion
contact times during force plate gait analysis in Greyhounds. Am J Vet Res 56:159-
161, 1995
26. McLaughlin RM, Miller CW, Taves CL, et ale Force plate analysis of triple pelvic
osteotomy for the treatment of canine hip dysplasia. Vet Surg 20:291-297, 1991
27. Muir P, Markel MD, Bogdanske JI, et ale Dual energy X-ray absorptiometry and force-
plate analysis of gait in dogs with healed femora after leg-lengthening plate fixation.
Vet Surg 24:15-24, 1995
KINETIC AND KINEMATIC GAlT ANALYSIS IN DOGS 201
..":
28. O'Conner BL, Visco DM, Heck DA, et ale Gait alterations in dogs after transection of
the anterior cruciate ligament. Arthritis Rheum 32:1142-1147, 1989
29. Renberg WC, Johnston SA, Ye K, et ale Comparison of stance time and velocity as
control variables in force plate analysis of dogs. Am J Vet Res 60:814-819, 1999
30. Riggs CM, DeCamp CE, Soutas-Little, et ale Effects of subject velocity on force plate
measured ground reaction forces in healthy Greyhounds at the trot. Am J Vet Res
54:1523-1526, 1993
31. Roush JK, McLaughlin RM: Effects of subject stance time and velocity on ground
reaction forces in clinically normal Greyhounds at the walk. Am J Vet Res 55:1672-
1676, 1994
32. Rumph PF, Steiss JE, West MS: Interday variation in vertical grolmd reaction force in
clinically normal Greyhounds at the trot. Am J Vet Res 60:679-683, 1999
33. Rumph PF, Lander JE, Kincaid SA, et ale Ground reaction force profiles from force
plateform gait analyses of clirtically normal mesomorphic dogs at the trot. Am J Vet
Res 55:756-761, 1994
34. Rumph PF, Kincaid SA, Visco DM, et al: Redistribution of verti cal ground reaction
force in dogs with experimentally induced chronic hind limb lameness. Vet Surg
24:384-389, 1995
35. Rumph PF, Kincaid SA, Baird DK, et al: Vertical ground reaction force distribution
during experimentally induced acute synovitis in dogs. Am J Vet Res 54:365-369, 1993
36. Schneider E, Chao EY: Fourier analysis of ground reaction forces in normals and
patients with knee joint disease. J Biomech 16:591-601, 1983
37. Vasseur PB, -Johnson AL, Budsberg SC, et al e Randomized, conholled trial of the
efficacy of carprofen, a nonsteroidal anti-inflammatory drug, in the treatment of osteo-
arthritis in dogs. JAVMA 206:807-811, 1995
38. Yanoff SR, Hulse DA, Hogan HA, et al: Measurements of vertical ground reaction
force in jumping dogs. Vet Camp Orthop Traumatol 5:44-50, 1992
Address reprint requests to
Ron M. McLaughlin, DVM, DVSc
The Animal Health Center
College of Veterinary Medicine
Mississippi State University
Wise Center
Mississippi State, MS 39762
LAMENESS
INDEX
Note: Page numbers of article titles are in boldface type.
Achondroplasia, 61
Adenocarcinoma, mammary, in cats, 156
pulmonary, in cats, 156
Algogenic substances, 42-43
Anconeal process, ununited, 65-70
Animals, small, lameness in, diagnostic
imaging of. 165-180
Antebrachium, palpation of, in lameness,
13
Arthritis, of elbow, 94
Arthrocentesis, fluid collection in, 184-185
fluid examination in, 185-186
microbiologic examination in, 186
Arthroscopy, advantages of, 187
complications of, 190-191
disadvantages of, 187-188
instrumentation in, 188
technique of, 188-189
uses of, 189-190
Articular nociceptors, mechanical
stimulation of, 45-46
Biceps tendon, diseases of, 89-90
Biochemical profile, in lameness, 182-183
Bone cysts, radial. 95-96
Bone region, subchondral. 48
Bones, long, fractures of, diagnOSiS of,
129-130
surgical options in, 130
Borreliosis, Lyme, diagnosis of, 187
Calcaneus, avulsion fracture of, 119
Calicivirus, lameness associated with,
153-155
Capital epiphysis, slipped, 114-116
Capital physis, fracture of, 114-116
Carpal bones, fractures of, 96-97
Carpal joint, avulsion of, 97
immune-mediated disease of, 97
osteoarthritis of, 96
Carpal laxity syndrome, 72
Cartilaginous exostosis, multiple, in cats,
159-160
Cat bites, contributing to lameness,
145- 147
Cats, degenerative joint disease in, 148,
149
developmental diseases in, 149-153
lameness in, 143-163
Cauda equina syndrome. See Lumbosacral
stenosis, degenerative.
Companion animals, lameness in,
neurologic conditions causing, 17-38
Computed tomography, in degenerative
lumbosacral stenosis, 28-29
in evaluation of lameness, 171-174
in intervertebral disk disease, 26
in malignant nerve sheath tumors, 32
Coronoid process, medial, fragmented,
66- 69
u l n a l ~ 66-67
Coxofemoral joint(s), abnormalities of,
101-106
evaluation of, in lameness, 9-10
Cranial drawer motion, testing of, in
diagnosis of cranial cruciate ligament
rupture, 8
Cruciate ligament, cranial. injury to,
106-108
clinical signs of, 107
diagnosis of, 107- 108
treatment of, 108
rupture of, as cause of lameness, 136
diagnosis of, laws for, 136-138
preexisting joint disease in, 136, 138
surgical stabilization in, 138
Declawing, lameness following, 161-162
Degenerative joint disease, diagnosis of,
133
203
204 INDEX
Degenerative joint disease (Continued)
in cats, 148, 149
treatment of, medical, 133-134
surgical, 134--135
Developmental diseases, in cats, 149- 153
Diagnostic imaging, in lameness in small
animals, 165--180
Diagnostic techniques, ancillary, in
lameness, 181-192
Di gital flexor tendon luxation, superficial,
119-121
Diskography, in intervertebral disk
disease, 27
Disks, herniated lateralized, in
intervertebral disk disease, 25-26
Dogs, adult, forelimb l a m e ~ e s s in, 85--99
kinetic and kinemetic galt anal ysIs ill,
193-201
mature, hind limb lameness in, 125--141
young, forelimb lameness in, 55-83
hind limb lameness in, 101-123
Ectrodactyly, 60-61
Ehrlichiosis, diagnosis of, 186-187
Elbow, arthritis of, 94
dysplasia of, 65
congenital, 59
luxation of, 93, 94
congenital, 58
neoplasia of, 93-94
osteoarthritis of, 93
osteochondrosis of, 65-66
region of, diseases of, 91-95
rickettsial diseases of, 95
Electrodiagnosis, in degenerative
lumbosacral stenosis, 28, 29
in myopathies, 21-22
Electromyography, in myopathies and
neuropathies, 21
Femoral neck metaphyseal osteopathy,
151-153
Femoral physis, distal, fracture of, 116-117
proximal, fractures of, 114-116
Fibrotic myopathy, in cats, 160-161
Fluoroscopy, in evaluation of lameness,
166-167
Foot (Feet), diseases of, 98
osteoarthritis of, 98
Force plate analysis, collection of force
plate data for, 196-197
equipment for, 194--196
evaluation of force plate data for, 197-
198
studies using, in dogs, 198
Force plate systems, piezoelectric, 195-196
Forelimb(s), examination of, in lameness,
12
lameness. See Lameness, forelimb.
Fracture(s). See specific sites and types of
fractures.
Gait analysis, kinematic and kinetic, in
dogs, 193-201
Giant cell tumor, in cats, 156
Glenohumeral ligament, partiall y torn,
90-91
Hematology, in lameness, 181-182
Hemorrhage, as complication of
arthroscopy, 191
Hind limb, degenerative joint disease of,
133, 134
surgery in, 131
fractures of, unique to immature ani-
mals, 114--121
lameness of. See Lameness, hind limb.
long bones of, fractures of, 129-130
Hip, disease of, lameness due to, 129
dysplasia of, in cats, 149-151
in dogs, clinical signs of, 103
diagnosis of, 103-105
history in diagnosis of, 135
total hip replacement in, 136
treatment of, 105-106, 135-136
laxity of, evaluation of, in lameness, 10
luxation of, evaluation of, in lameness,
10-11, 12
total replacement of, in hip dysplasia,
136
Hip joint, luxation and instability of,
closed manipulation in, 131
traumatic, 131
Histoplasmosis, in cats, 155
Hock, palpation of, in lameness, 6-7
Humeral condyle, fract ure of, 92-93
Humerus, region of, diseases of, 91
Hyaline cartilage, 48
Hyperalgesia, 42
secondary, 43
Hypochondroplasia, 61
Infections, as cause of forelimb lameness,
77
Inflammation, neurogenic, joint pain in, 47
Infraspinatus muscle, contracture of, 89
Interphalangeal luxations, in minimal
trauma, 132-133
Intervertebral disk disease, diagnosis of,
24--25
, imaging techniques in, 26-27
herniated lateralized disks in, 25-26
sensory evaluation in, 25
sites of, 23-24
testing for nerve-root impingement in,
25
Joint(s), degenerative di sease of. See
Degenerative joint disease.
inflammation and sensitization of, 46-47
innervation of, osteoarthritis and, 50
luxation and instability of, hind limb
lameness in, 130-133
neuroreceptors in, 44-45
Joint capsule, 49
Kinematic gait analysis, 199
and kinetic gait analysis, in dogs, 193-
201
Lameness, 1-201
ancillary diagnostic teclmiques in, 181-
192
arthrocentesis in. See Arthrocentesis.
arthroscopy in. See Arthroscopy.
biochemical profile in, 182-183
definition of, 1
evaluation of, 1-16
components of, 2
focused inspection in, 6-13
general observations in, 4--6
history and signalment in, 3-4
pitfalls and complications in, 14--15
forelimb, in adult patient, 85-99
in yOlmg patient, 55--83
congenital causes of, 58-62
developmental causes of, 62- 72
differential diagnosis of, 55, 56-57
idiopathic causes of, 75- 77
in neoplasia, 78
infectious causes of, 77
nutritional and metabolic causes of,
77
traumatic causes of, 72- 75
hematology in, 181- 182
hind limb, diagnostic tests in, 127- 129
examination for, 125
in fractures, 129-130
in joint luxation and instability, 130-
133
in mature dog, 125- 141
in young patient, 101- 123
neoplasia as cause of, 140
in cats, 143-163
INDEX 205
causes of, 144, 145- 162
due to n eoplasia, 155-160
infectious causes of, 153-155
orthopedic examination in, 143
in companion animals, neurologic condi-
tions causing, 17-38
in diseases of nerve roots, 23- 35
in diseases of p eripheral nerves, 23-35
in myopathies, 20-23
in small animals, diagnostic imaging in,
165--180
in spinal cord nneoplasia, 29
nonweight-b earing, postural reactions
to, 19
pain in, overview of, 39-53
rheumatoid fa ctor testing in, 186, 187
routine laboratory evaluation in, 181- 184
urinalysis in, 183-184
Legg-Calve-Perthes disease, 101-103
Ligament, glenohumeral, partially torn,
90-91
Limbs, upper, evaluation of, in lameness,
13
Linear tomography, in intervertebral disk
disease, 27
Lower motor neuron disease, differential
diagnosis of, 19
Lumbosacral stenosis, degenerative, causes
of,27
computed tomography and magnetic
resonance imaging in, 28-29
lameness in, 27
neuroimaging and electrodiagnosis in,
28, 29
Lyme borreliosis, diagnosis of, 187
Magnetic resonance imaging, in
degenerati ve lumbosacral stenosis,
28-29
in evaluation of lameness, 174--178
in malignant nerve sheath tumors, 32
Mechanoreceptors, 42, 49-50
Medial butress, bilateral, in cranial cruciate
ligament rupture, 127-128
Menisci,49
Metatarsophalangealluxations, in minimal
trauma, 132
Mucopolysaccharidosis, 61-62
orthopedic problems in, 153
Multiple myeloma, in cats, 158-159
Muscle(s), infraspinatus, contracture of, 89
weakness of, with osteoarthritis, 50
Muscle biopsies, in neuromuscular disease,
23
Mycoplasma, polyarthritis and
tenosynovitis due to, 155
Myelography, in spinal cord neoplasia, 30
Myopathies, diagnosis of, tests in, 21
206 INDEX
Myopathies (Continued)
lameness in, 20-23
Neoplasia, as cause of forelimb lameness,
78
as cause of hind limb lameness, 140
of elbow, 93- 94
spinal cord, diagnosis of, 29-31
lameness in, 29
Nerve(s), peripheral, diseases of, lameness
in,23-35
Nerve biopsies, in neuromuscular disease,
22
Nerve fibers, postganglionic sympathetic
efferent, 42
primary efferent, 43
Nerve roots, diseases of, lameness in,
23-35
Neurofibromas, 31-34
Neurofibrosarcomas, 31'-34
Neuroimaging, in degenerative
lumbosacral stenosis, 28, 29
Neurologic conditions, abnormalities
caused by, 18- 20
causing lameness in companion animals,
17- 38
Neurologic examination, 18
sensory component of, 19-20
Neuropathies, traumatic, causes of, 34
electrodiagnostic testing in, 34
exploratory surgery in, 35
physical examination in, 34
Neuroreceptors, 41--42, 49 .
in joints, 44--45
Nociceptors, articular, mechanical
stimulation of, 45--46
Nuclear medicine, in evaluation of
lameness, 168-170
Nutritional deficiencies, as cause of
forelimb lameness, 77
Orthopedic diseases, developmental, in
dogs, 110-114
"Ortolani" sign, in hip disease, 129
Osteoarthritis, anatomy and change with,
48- 50
clinical manifestations of, 41
definition of, 40--41
feline, lameness in, 147- 149
joint innervation and, 50
muscle weakness in, 50
of carpal joint, 96
of elbow, 93
of feet, 98
of shoulder, 88
source of pain in, 41
Osteochondrodysplasia, in cats, 153
Osteochondrosis, 62-65, 110-112
Osteodystrophy, hypertrophic, 76, 112-113
Osteogenesis imperfecta, 62
Osteosarcoma, as cause of hind limb
lameness, 140
in cats, 158, 159, 160
radial,95
Pain, definition of, 39
in lameness, overview of, 39-53
mechanisms of, 40
Panosteitis, 75-76, 113-114
Patella, luxation of, clinical signs of, 109
diagnosis of, 110, 128-129
grades of, 139
lameness in, 9, 139
treatment of, 110, 139-140
Patient, lame. See Lameness.
Paws, examination of, in lameness, 6
Periosteum, 48--49
Peripheral nerve sheath tumors,
malignant, diagnosis of, 32-34
lameness in, 31-32
Piezoelectric force plate systems, 195-196
Polyarthritis, feline progressive, lameness
in, 147-149
Radial ageneses or dysgeneses, 59-60
Radiography, in hind limb lameness, 129
survey, in evaluation of lameness, 166
Radioulnar region, diseases of, 95-96
Radius, bone cysts of, 95- 96
fractures of, 95
osteosarcoma of, 95
Retinal dysplasia, skeletal dysplasia with,
61
Rickettsial diseases, of elbow, 95
Salter-Harris fractures, 72- 74
Scapula, examination of, in lameness, 13
region of, diseases of, 86-87
Schwannomas, 31- 34
Scintigraphy, in long bone fractures, 130
skeletal, in evaluation of lameness, 168-
171
Sesamoids, fragmentation of, 98
Shoulder, instability of, 88-89
luxation of, 88
congenital, 58
osteoarthritis of, 88
region of, diseases of, 87-91
subluxation of, 88- 89
Skeletal dysplasia, with retinal dysplasia,
61
Spinal cord neoplasia, diagnosis of, 29-31
]ameness in, 29
Stifle, abnormalities of, 106-110
in dogs, arthroscopy in, 190
luxation of, traumatic, 131-132
pain in, evaluation of, in lameness, 7-8
Synovium, 49
tumors of, in cats, 156
Tarsus, luxation and instabilities of, 132
Tendon(s), biceps, diseases of, 89- 90
injuries of, 119-121
INDEX
Tibial tuberosity, avulsi.on fj-actures of,
117-119
Trauma, as cause of forelimb lameness,
72- 75
Ulna, fractures of, 95
207
fragmented medial coronoid process of,
66-67
Ultrasound, in evaluation of lameness
167- 168 '
in malignant nerve sheath tumors, 32-34
in traumatic neuropa thies, 35
Urinalysis, in lameness, 183-184
Potrebbero piacerti anche
- Veterinary Surgical OncologyDa EverandVeterinary Surgical OncologySimon T. KudnigNessuna valutazione finora
- Practical Weight Management in Dogs and CatsDa EverandPractical Weight Management in Dogs and CatsTodd L. TowellNessuna valutazione finora
- Gaynor Handbook of Veterinary Pain Management Third Edition PDFDocumento638 pagineGaynor Handbook of Veterinary Pain Management Third Edition PDFMaca Muñoz Escobedo100% (3)
- Saunders Manual of Small Animal PracticeDocumento2.014 pagineSaunders Manual of Small Animal PracticeSara Perez Pastrana100% (11)
- Canine Infectious Diseases - Self-Assessment Color Review - (2018)Documento289 pagineCanine Infectious Diseases - Self-Assessment Color Review - (2018)aLÔ REGINA83% (6)
- The Practice of Veterinary Anesthesia - Small Animals, Birds, Fish, and ReptilesDocumento382 pagineThe Practice of Veterinary Anesthesia - Small Animals, Birds, Fish, and ReptilesMárcio MoreiraNessuna valutazione finora
- Avian Medicine and Surgery in Practice Companion and Aviary BirdsDocumento384 pagineAvian Medicine and Surgery in Practice Companion and Aviary BirdsDrogaria Econômica0% (2)
- Current Techniques in Small Animal Surgery, 5th Edition (VetBooks - Ir) PDFDocumento1.156 pagineCurrent Techniques in Small Animal Surgery, 5th Edition (VetBooks - Ir) PDFgitaNessuna valutazione finora
- Blackwell's Five-Minute Veterinary Consult: RuminantDa EverandBlackwell's Five-Minute Veterinary Consult: RuminantNessuna valutazione finora
- Duncan and Prasse's Veterinary Laboratory Medicine: Clinical PathologyDa EverandDuncan and Prasse's Veterinary Laboratory Medicine: Clinical PathologyKenneth S. LatimerNessuna valutazione finora
- Nursing the Feline PatientDa EverandNursing the Feline PatientLinda E. SchmeltzerNessuna valutazione finora
- Urological Disorders of The Dog and CatDocumento177 pagineUrological Disorders of The Dog and CatChiruc AmaliaNessuna valutazione finora
- Clinical Endocrinology of Dogs Cats PDFDocumento353 pagineClinical Endocrinology of Dogs Cats PDFsanjagruborovic100% (1)
- Anesthesia For The Pet Practitioner 2009 2 PDFDocumento154 pagineAnesthesia For The Pet Practitioner 2009 2 PDFabibullaNessuna valutazione finora
- Small Animal Spinal Disorders (Second Edition)Documento369 pagineSmall Animal Spinal Disorders (Second Edition)Aline Constantino100% (3)
- rn2 PDFDocumento237 paginern2 PDFAngel LunaNessuna valutazione finora
- Small Animal OncologyDocumento315 pagineSmall Animal OncologyMetka Trampuš100% (2)
- Pain Management in Small Animal Medicine PDFDocumento406 paginePain Management in Small Animal Medicine PDFRotar ArielaNessuna valutazione finora
- Feline Medicine - Review and TestDocumento401 pagineFeline Medicine - Review and TestBrisbany Alcibar60% (5)
- Canine Infectious Diseases, Self-Assessment Color Review (VetBooks - Ir) PDFDocumento289 pagineCanine Infectious Diseases, Self-Assessment Color Review (VetBooks - Ir) PDFPanchita Camila V. Diaz100% (1)
- Canine and Feline Geriatrics (Library Vet Practice)Documento191 pagineCanine and Feline Geriatrics (Library Vet Practice)Ariadna Benitez100% (2)
- Rabbit Medicine and SurgeryDocumento253 pagineRabbit Medicine and SurgeryKary SanchezNessuna valutazione finora
- BSAVA Manual of Canine and Feline Reproduction and Neonatology, 2nd EditionDocumento243 pagineBSAVA Manual of Canine and Feline Reproduction and Neonatology, 2nd EditionDiana Uribelarrea Sierra100% (2)
- AIDAP Prescribing GuidelinesDocumento153 pagineAIDAP Prescribing Guidelinesmarjoriet100% (2)
- (Michael Schaer D.V.M) Clinical Signs in Small AnimalDocumento506 pagine(Michael Schaer D.V.M) Clinical Signs in Small AnimalJunior SantanaNessuna valutazione finora
- Dermatology For The Small Animal PractitionerDocumento145 pagineDermatology For The Small Animal Practitionerсветлана бугаева100% (5)
- Anesthesia For The Pet Practitioner (2011 3rd Edition)Documento216 pagineAnesthesia For The Pet Practitioner (2011 3rd Edition)Amela Dolittle Halilbašić100% (5)
- Manual of Veterinary DieteticsDocumento253 pagineManual of Veterinary DieteticsNeto Mvz EJ Castazu100% (3)
- Valenciano A.c., Cowell R.L., Rizzi T.E., Tyler R.D. - Atlas of Canine and Feline Peripheral Blood Smears. Part 1Documento212 pagineValenciano A.c., Cowell R.L., Rizzi T.E., Tyler R.D. - Atlas of Canine and Feline Peripheral Blood Smears. Part 1MarciaNessuna valutazione finora
- Dictionary of Veterinary Nursing - Denis Richard Lane MSC BSC (Vet Sci) FRCVS FRAgS BSC (Hons) AAB&TDocumento5 pagineDictionary of Veterinary Nursing - Denis Richard Lane MSC BSC (Vet Sci) FRCVS FRAgS BSC (Hons) AAB&TkogekaruNessuna valutazione finora
- Smalll Animal OrthopaedicsDocumento193 pagineSmalll Animal OrthopaedicsEzequiel DiazNessuna valutazione finora
- Self-Assessment Colour Review of Small Animal Soft Tissue SurgeryDocumento194 pagineSelf-Assessment Colour Review of Small Animal Soft Tissue Surgerymiliindianu100% (3)
- BSAVA Manual of Veterinary Nursing 1999Documento303 pagineBSAVA Manual of Veterinary Nursing 1999Takács Györgyi100% (1)
- Practical Veterinary Nursing: BSAVA Manual ofDocumento418 paginePractical Veterinary Nursing: BSAVA Manual ofSarynha CostaNessuna valutazione finora
- Clinical Atlas of Canine and Feline Dermatology (VetBooks - Ir)Documento514 pagineClinical Atlas of Canine and Feline Dermatology (VetBooks - Ir)Evelyn Louise C. M. B100% (1)
- Hand Book of Veterinary Internal MedicineDocumento88 pagineHand Book of Veterinary Internal MedicineDanielle Fisher91% (11)
- Atlas of Radiology of The Traumatized Dog and Cat, The Case-Based Approach (Vetbooks - Ir) PDFDocumento566 pagineAtlas of Radiology of The Traumatized Dog and Cat, The Case-Based Approach (Vetbooks - Ir) PDFIonuț CiucăNessuna valutazione finora
- Small Animal DermatologyDocumento278 pagineSmall Animal DermatologyManuel Rodriguez100% (1)
- Skin Diseases Dogs and CatsDocumento10 pagineSkin Diseases Dogs and CatsMaria DumitruNessuna valutazione finora
- Small Animal Emergency and Critical Care Medicine - Kirby, Rebecca, Rudloff, Elke, Linklater, Drew PDFDocumento249 pagineSmall Animal Emergency and Critical Care Medicine - Kirby, Rebecca, Rudloff, Elke, Linklater, Drew PDFSanjeev Choudhary100% (2)
- Veterinary EctoparasitesDocumento274 pagineVeterinary Ectoparasitesmihaiciocea100% (3)
- BSAVA Manual of Canine and Feline Haematology and Transfusion, 2nd EditionDocumento354 pagineBSAVA Manual of Canine and Feline Haematology and Transfusion, 2nd Editionpanchulaz100% (4)
- Common Small Animal Diagnosis An Algorithmic Approach PDFDocumento2 pagineCommon Small Animal Diagnosis An Algorithmic Approach PDFAshley0% (4)
- A Color Handbook of Skin Diseases of The Dog and Cat, 2nd EditionDocumento337 pagineA Color Handbook of Skin Diseases of The Dog and Cat, 2nd EditionHo Duc Tham100% (2)
- Small Animal Dental Ora and Max DisDocumento273 pagineSmall Animal Dental Ora and Max DisAngeles Verdugo80% (5)
- Small Animal Clinical OncologyDocumento32 pagineSmall Animal Clinical OncologySándor Holdas100% (1)
- Veterinary Nursing Skills MatrixDocumento4 pagineVeterinary Nursing Skills MatrixGary75% (4)
- Lorenz Small Animal Medical Diagnosis PDFDocumento581 pagineLorenz Small Animal Medical Diagnosis PDFLucia Corlat100% (1)
- Anesthesia For The Pet Practitioner, Revised 3rd Edition (VetBooks - Ir)Documento217 pagineAnesthesia For The Pet Practitioner, Revised 3rd Edition (VetBooks - Ir)Noviana DewiNessuna valutazione finora
- Hill's Atlas of Veterinary AnatomyDocumento102 pagineHill's Atlas of Veterinary Anatomyrudolfrennarossa92% (13)
- Unusual Pet Care Vol1-4Documento628 pagineUnusual Pet Care Vol1-4afeefah walkerNessuna valutazione finora
- High-Quality, High-Volume Spay and Neuter and Other Shelter Surgeries PDFDocumento674 pagineHigh-Quality, High-Volume Spay and Neuter and Other Shelter Surgeries PDFaLÔ REGINANessuna valutazione finora
- Blackwell's Five-Minute Veterinary Consult: Canine and FelineDocumento4 pagineBlackwell's Five-Minute Veterinary Consult: Canine and FelinerocawitaNessuna valutazione finora
- Atlas of Orthopedic Surgical Procedures of The Dog and CatDocumento244 pagineAtlas of Orthopedic Surgical Procedures of The Dog and Catcamilov100100% (1)
- Diseases in DogsDocumento54 pagineDiseases in DogsMelanie100% (4)
- Veterinary Forensics: Animal Cruelty InvestigationsDa EverandVeterinary Forensics: Animal Cruelty InvestigationsMelinda MerckNessuna valutazione finora
- Radiography of the Dog and Cat: Guide to Making and Interpreting RadiographsDa EverandRadiography of the Dog and Cat: Guide to Making and Interpreting RadiographsNessuna valutazione finora
- Animal NutritionDocumento714 pagineAnimal NutritionZozo Mostafa92% (12)
- Drugs of Pet AnimalsDocumento13 pagineDrugs of Pet AnimalsZozo MostafaNessuna valutazione finora
- Diseases Poultry Diagnosis SymptomsDocumento15 pagineDiseases Poultry Diagnosis SymptomsTufail Banday100% (1)
- Vcona Sap May 2001Documento168 pagineVcona Sap May 2001Zozo MostafaNessuna valutazione finora
- Diseases Poultry Diagnosis SymptomsDocumento15 pagineDiseases Poultry Diagnosis SymptomsTufail Banday100% (1)
- Guide To Veterinary Practice PlaningDocumento17 pagineGuide To Veterinary Practice PlaningCimpo1Nessuna valutazione finora
- الفيزياء المسليهDocumento265 pagineالفيزياء المسليهmohamed abd el gawad100% (1)
- Vcona Sap May 2001Documento168 pagineVcona Sap May 2001Zozo MostafaNessuna valutazione finora
- A Color Atlas of Poultry Diseases by J.L VegadDocumento131 pagineA Color Atlas of Poultry Diseases by J.L VegadAbubakar Tahir Ramay95% (63)
- MarchDocumento122 pagineMarchZozo Mostafa100% (3)
- MarchDocumento122 pagineMarchZozo Mostafa100% (3)
- A2 - Practice 29Documento2 pagineA2 - Practice 29123VinhcuuNessuna valutazione finora
- Obg FormatDocumento17 pagineObg Formatarchana vermaNessuna valutazione finora
- Gen Bio 2 Q4 Module 4Documento25 pagineGen Bio 2 Q4 Module 4Shoto TodorokiNessuna valutazione finora
- Microbiology NotesDocumento83 pagineMicrobiology NotesPauline Añes100% (1)
- Wa0003Documento4 pagineWa0003YegaNessuna valutazione finora
- Fundamentals of NursingDocumento50 pagineFundamentals of NursingGuruKPO67% (3)
- RM NCC RN 8.0 CHP 21Documento21 pagineRM NCC RN 8.0 CHP 21LonaBrochenNessuna valutazione finora
- Bath Uni Coursework Cover SheetDocumento8 pagineBath Uni Coursework Cover Sheetvtdvkkjbf100% (2)
- Your Body Believes Every Word Y - Barbara Hoberman LevineDocumento380 pagineYour Body Believes Every Word Y - Barbara Hoberman LevineRoryBradshawNessuna valutazione finora
- 2-NPSG Chapter OBS Jan2023Documento8 pagine2-NPSG Chapter OBS Jan2023Blanca LanderosNessuna valutazione finora
- Extensive Reading - AVK44CDocumento42 pagineExtensive Reading - AVK44CNinh Nhat Thao Vy K189Nessuna valutazione finora
- Lab 1C PAR-Q and Health History QuestionnaireDocumento4 pagineLab 1C PAR-Q and Health History Questionnaireskyward23Nessuna valutazione finora
- Pneumonia Severity IndexDocumento1 paginaPneumonia Severity Indexmob3Nessuna valutazione finora
- A Simple Approach To Shared Decision Making in Cancer ScreeningDocumento6 pagineA Simple Approach To Shared Decision Making in Cancer ScreeningariskaNessuna valutazione finora
- 9721 Smoking Cessaton Newsletter 1981Documento8 pagine9721 Smoking Cessaton Newsletter 1981Julia PurperaNessuna valutazione finora
- Papaya Farming Land Preparation and Planting: Establishment of WindbreaksDocumento9 paginePapaya Farming Land Preparation and Planting: Establishment of WindbreaksmarcamilleNessuna valutazione finora
- The Role of Neuroglia in AutismDocumento30 pagineThe Role of Neuroglia in AutismWesley M.SantosNessuna valutazione finora
- Syrgery Mock 10Documento8 pagineSyrgery Mock 10Sergiu CiobanuNessuna valutazione finora
- WRH Emergency Codes: in Case of Emergency - .Documento10 pagineWRH Emergency Codes: in Case of Emergency - .Silvanus Chakra PuspitaNessuna valutazione finora
- Classification of Trauma in ChildrenDocumento9 pagineClassification of Trauma in ChildrenRita ValenteNessuna valutazione finora
- Doxycycline (As Hyclate) : Package Leaflet: Information For The User Doxycycline Pinewood 100 MG CapsulesDocumento2 pagineDoxycycline (As Hyclate) : Package Leaflet: Information For The User Doxycycline Pinewood 100 MG CapsulesZulva Chairunnisa BudimanNessuna valutazione finora
- Language and ArtsDocumento17 pagineLanguage and ArtsOpium PoppyNessuna valutazione finora
- Prognostic Factors and Management of Patients With Choanal AtresiaDocumento7 paginePrognostic Factors and Management of Patients With Choanal Atresiafarah maulida martaNessuna valutazione finora
- PDFDocumento732 paginePDFMahmud Eljaarani90% (10)
- Hiddensee - Michelle HartDocumento13 pagineHiddensee - Michelle HartviniciuscarpeNessuna valutazione finora
- Class 12th Chemistry Project On Investigatory Test On GuavaDocumento20 pagineClass 12th Chemistry Project On Investigatory Test On GuavaAyush Kumar100% (1)
- List COVID Facilities State OdishaDocumento3 pagineList COVID Facilities State OdishadrjyotivetNessuna valutazione finora
- Jpts 28 3227 PDFDocumento5 pagineJpts 28 3227 PDFphildawsonphotoNessuna valutazione finora
- PathogenesisDocumento14 paginePathogenesisIdreesNessuna valutazione finora
- BIO 1 Course Syllabus UPDDocumento3 pagineBIO 1 Course Syllabus UPDDanielle Marie100% (1)