Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Esophageal Cancer
Caricato da
Sarah GatuzDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Esophageal Cancer
Caricato da
Sarah GatuzCopyright:
Formati disponibili
Introduction The incidence of esophageal cancer is on the rise with over 12,000 Americans developing this disease each
year (Figure 2). Variations in the incidence of esophageal cancer are seen with age, sex, and race. Advances in medical and surgical therapy have led to improvement in the survival rates but continued improvement in survival is dependent on a better understanding of the relationship between environmental factors and the disease itself. The incidence of esophageal cancer fluctuates dramatically throughout various regions of the world and has the largest variability of any known malignacy. High rates are found in people living in northeast China to north central Asia, Afghanistan and northern Iran. Other high-risk groups include the white population in parts of South Africa and areas of Finland, Iceland, and France. In the United States, trends demonstrate that black men have a fourfold greater incidence than white men for squamous cell esophageal cancer with significant variation in locale, nutritional status, socioeconomic status, and alcohol and cigarette use. Figure 1. Location of the esophagus in the body. General Info What is Esophageal Cancer? Esophageal cancer may be classified according to the site of origin. The malignancy may originate in the squamous cells, or in the columnar cells that line the esophageal lumen. Squamous cell carcinoma may occur throughout the length of the esophagus, whereas adenocarcinoma generally occurs just above the esophagogastric junction (Figure 3).
Figure 3. Histology; A, adenocarcinoma; B, squamous cell carcinoma
Symptoms Early stage esophageal cancer may be totally asymptomatic or may present with mild nonspecific symptoms such as heartburn, atypical chest pain, or dyspepsia. Alternatively, patients may present with symptoms such as occult blood in the stool or iron deficiency anemia. Patients may report mild or intermittent dysphagia, odynophagia, or a foreign body sensation. These symptoms generally warrant diagnostic evaluation, including an esophagogastroduodenoscopy (EGD) (upper endoscopy), including diagnostic mucosal biopsy. Some early cancers are diagnosed during routine upper endoscopic surveillance forBarretts esophagus. The symptoms of esophageal cancer generally progress rapidly. Symptoms of advanced esophagealcarcinoma become apparent with tumor growth. An initial inability to swallow solids is followed by difficulty in swallowing ground food and finally liquids. Progressive dysphagia is the most common complaint in most patients (90%) with greater than 50% luminal occlusion or where luminal diameter is less than 13 mm. Weight loss and anorexia are often present in patients with more advanced disease (due to inadequate intake of food secondary to dysphagia, or to a nonspecific effect of the cancer), predisposing the patient to nutritional deficits. Odynophagiaoccurs in about
one half of the patients. Esophageal obstruction may cause aspiration of food and pneumonia. Tumor extension to the pericardium or mediastinum may cause retrosternal or back pain, as well as abscess formation. Hoarseness is usually associated with recurrent laryngeal nerve paralysis. Hiccups may occur due to mediastinal and/or diaphragmatic involvement of the tumor. Anemia and/or gastrointestinal bleeding and weakness may be present if the tumor is ulcerated andfriable. Incessant cough and pneumonia should alert the clinician to the possibility of a tracheo- or bronchio-esophageal fistularesulting from tumor invasion of the nearby airways. Esophageal cancer is a disease in which malignant (cancer) cells form in the tissues of the esophagus. The esophagus is the hollow, muscular tube that moves food and liquid from the throat to the stomach. The wall of the esophagus is made up of several layers of tissue, including mucous membrane, muscle, and connective tissue. Esophageal cancer starts at the inside lining of the esophagus and spreads outward through the other layers as it grows. Enlarge
The stomach and esophagus are part of the upper digestive system.
The two most common forms of esophageal cancer are named for the type of cells that become malignant (cancerous): Squamous cell carcinoma: Cancer that forms in squamous cells, the thin, flat cells lining the esophagus. This cancer is most often found in the upper and middle part of the esophagus, but can occur anywhere along the esophagus. This is also called epidermoid carcinoma. Adenocarcinoma: Cancer that begins in glandular (secretory) cells. Glandular cells in the lining of the esophagus produce and release fluids such asmucus. Adenocarcinomas usually form in the lower part of the esophagus, near the stomach. Smoking, heavy alcohol use, and Barrett esophagus can increase the risk of developing esophageal cancer. Risk factors include the following:
Tobacco use. Heavy alcohol use. Barrett esophagus: A condition in which the cells lining the lower part of the esophagus have changed or been replaced with abnormal cells that could lead to cancer of the esophagus. Gastric reflux (the backing up of stomach contents into the lower section of the esophagus) may irritate the esophagus and, over time, cause Barrett esophagus. Older age. Being male. Being African-American. The most common signs of esophageal cancer are painful or difficult swallowing and weight loss. These and other symptoms may be caused by esophageal cancer or by other conditions. A doctor should be consulted if any of the following problems occur:
Painful or difficult swallowing. Weight loss. Pain behind the breastbone. Hoarseness and cough. Indigestion and heartburn. Tests that examine the esophagus are used to detect (find) and diagnose esophageal cancer. The following tests and procedures may be used:
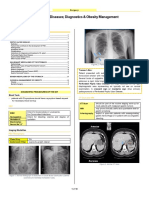
Chest x-ray: An x-ray of the organs and bones inside the chest. An x-ray is a type of energy beam that can go through the body and onto film, making a picture of areas inside the body. Barium swallow: A series of x-rays of the esophagus and stomach. The patient drinks a liquid that contains barium (a silver-white metallic compound). The liquid coats the esophagus and stomach, and x-rays are taken. This procedure is also called an upper GI series. Enlarge
Barium swallow. The patient swallows barium liquid and it flows through the esophagus and into
the stomach. X-rays are taken to look for abnormal areas. Esophagoscopy: A procedure to look inside the esophagus to check for abnormal areas. An esophagoscope is inserted through the mouth or nose and down the throat into the esophagus. An esophagoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove tissue samples, which are checked under a microscope for signs of cancer. Enlarge
Esophagoscopy. A thin, lighted tube is inserted through the mouth and into the esophagus to look for abnormal areas. Biopsy: The removal of cells or tissues so they can be viewed under a microscope by a pathologist to check for signs of cancer. The biopsy is usually done during an esophagoscopy. Sometimes a biopsy shows changes in the esophagus that are not cancer but may lead to cancer. Certain factors affect prognosis (chance of recovery) and treatment options. The prognosis (chance of recovery) and treatment options depend on the following: The stage of the cancer (whether it affects part of the esophagus, involves the whole esophagus, or has spread to other places in the body). The size of the tumor. The patients general health. After esophageal cancer has been diagnosed, tests are done to find out if cancer cells have spread within the esophagus or to other parts of the body. The process used to find out if cancer cells have spread within the esophagus or to other parts of the body is called staging. The information gathered from the staging process determines the stage of the disease. It is important to know the stage in order to plan treatment. The following tests and procedures may be used in the staging process: Bronchoscopy: A procedure to look inside the trachea and large airways in the lung for abnormal areas. A bronchoscope is inserted through the nose or mouth into the trachea and lungs. A bronchoscope is a thin, tube-like
instrument with a light and a lens for viewing. It may also have a tool to remove tissue samples, which are checked under a microscope for signs of cancer. Chest x-ray: An x-ray of the organs and bones inside the chest. An x-ray is a type of energy beam that can go through the body and onto film, making a picture of areas inside the body. Laryngoscopy: A procedure in which the doctor checks the larynx (voice box) with a mirror or with alaryngoscope. A laryngoscope is a thin, tube-like instrument with a light and a lens for viewing. CT scan (CAT scan): A procedure that makes a series of detailed pictures of areas inside the body, taken from different angles. The pictures are made by a computer linked to an x-ray machine. A dye may beinjected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography. Endoscopic ultrasound (EUS): A procedure in which an endoscope is inserted into the body, usually through the mouth or rectum. An endoscope is a thin, tube-like instrument with a light and a lens for viewing. A probe at the end of the endoscope is used to bounce high-energy sound waves (ultrasound) off internal tissues or organs and make echoes. The echoes form a picture of body tissues called a sonogram. This procedure is also called endosonography. Thoracoscopy: A surgical procedure to look at the organs inside the chest to check for abnormal areas. Anincision (cut) is made between two ribs and a thoracoscope is inserted into the chest. A thoracoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove tissue or lymph node samples, which are checked under a microscope for signs of cancer. In some cases, this procedure may be used to remove part of the esophagus or lung. Laparoscopy: A surgical procedure to look at the organs inside the abdomen to check for signs of disease. Small incisions (cuts) are made in the wall of the abdomen and a laparoscope (a thin, lighted tube) is inserted into one of the incisions. Other instruments may be inserted through the same or other incisions to perform procedures such as removing organs or taking tissue samples to be checked under a microscope for signs of disease. PET scan (positron emission tomography scan): A procedure to find malignant tumor cells in the body. A small amount of radionuclide glucose (sugar) is injected into a vein. The PET scanner rotates around the body and makes a picture of where glucose is being used in the body. Malignant tumor cells show up brighter in the picture because they are more active and take up more glucose than normal cells do. The use of PET for staging esophageal cancer is being studied in clinical trials. There are three ways that cancer spreads in the body. The three ways that cancer spreads in the body are: Through tissue. Cancer invades the surrounding normal tissue. Through the lymph system. Cancer invades the lymph system and travels through the lymph vessels to other places in the body. Through the blood. Cancer invades the veins and capillaries and travels through the blood to other places in the body. When cancer cells break away from the primary (original) tumor and travel through the lymph or blood to other places in the body, another (secondary) tumor may form. This process is called metastasis. The secondary (metastatic) tumor is the same type of cancer as the primary tumor. For example, if breast cancer spreads to the bones, the cancer cells in the bones are actually breast cancer cells. The disease is metastatic breast cancer, not bone cancer. The following stages are used for squamous cell carcinoma of the esophagus: Stage 0 (High-grade Dysplasia)
In stage 0, abnormal cells are found in the inner (mucosal) layer of the esophageal wall. These abnormal cells may become cancer and spread into nearby normal tissue. Stage 0 is also called high-grade dysplasia. Stage I squamous cell carcinoma of the esophagus Stage I is divided into Stage IA and Stage IB, depending on where the cancer is found. o o Stage IA: Cancer has formed in the inner (mucosal) layer of the esophageal wall. The tumor cells look a lot like normal cells under a microscope. Stage IB: Cancer has formed: in the inner (mucosal) layer of the esophageal wall. The tumor cells do not look at all like normal cells under a microscope; or in the inner (mucosal) layer and spread into the middle (muscle) layer or the outer (connective tissue) layer of the esophageal wall. The tumor cells look a lot like normal cells under a microscope. The tumor is in the lower esophagus or it is not known where the tumor is. Stage II squamous cell carcinoma of the esophagus Stage II is divided into Stage IIA and Stage IIB, depending on where the cancer has spread. o o Stage IIA: Cancer has spread: into the middle (muscle) layer or the outer (connective tissue) layer of the esophageal wall. The tumorcells look a lot like normal cells under a microscope. The tumor is in either the upper or middleesophagus; or into the middle (muscle) layer or the outer (connective tissue) layer of the esophageal wall. The tumor cells do not look at all like normal cells under a microscope. The tumor is in the lower esophagus or it is not known where the tumor is. Stage IIB: Cancer: has spread into the middle (muscle) layer or the outer (connective tissue) layer of the esophagealwall. The tumor cells do not look at all like normal cells under a microscope. The tumor is in either the upper or middle esophagus; or is in the inner (mucosal) layer and may have spread into the middle (muscle) layer of the esophageal wall. Cancer is found in 1 or 2 lymph nodes near the tumor. Stage III squamous cell carcinoma of the esophagus Stage III is divided into Stage IIIA, Stage IIIB, and Stage IIIC, depending on where the cancer has spread. o o o Stage IIIA: Cancer: is in the inner (mucosal) layer and may have spread into the middle (muscle) layer of the esophagealwall. Cancer is found in 3 to 6 lymph nodes near the tumor; or has spread into the outer (connective tissue) layer of the esophageal wall. Cancer is found in 1 or 2 lymph nodes near the tumor; or has spread into the diaphragm, sac around the heart, or tissue that covers the lungs and lines the inner wall of the chest cavity. The cancer can be removed by surgery. Stage IIIB: Cancer has spread into the outer (connective tissue) layer of the esophageal wall. Cancer is found in 3 to 6 lymph nodes near the tumor. Stage IIIC: Cancer has spread:
o o o
into the diaphragm, sac around the heart, or tissue that covers the lungs and lines the inner wall of the chest cavity; the cancer can be removed by surgery. Cancer is found in 1 to 6 lymph nodes near the tumor; or into other nearby organs such as the aorta, trachea, or spine, and the cancer cannot be removed by surgery; or to 7 or more lymph nodes near the tumor. Stage IV squamous cell carcinoma of the esophagus In Stage IV, cancer has spread to other parts of the body. The following stages are used for adenocarcinoma of the esophagus: Stage 0 (High-grade Dysplasia) In stage 0, abnormal cells are found in the inner (mucosal) layer of the esophageal wall. These abnormal cells may become cancer and spread into nearby normal tissue. Stage 0 is also called high-grade dysplasia. Stage I adenocarcinoma of the esophagus Stage I is divided into Stage IA and Stage IB, depending on where the cancer is found.
o o
Stage IA: Cancer has formed in the inner (mucosal) layer of the esophageal wall. The tumor cells look a lot like normal cells under a microscope. Stage IB: Cancer has formed: in the inner (mucosal) layer of the esophageal wall. The tumor cells do not look at all like normal cells under a microscope and they grow quickly; or in the inner (mucosal) layer and spread into the middle (muscle) layer of the esophageal wall. The tumor cells look a lot like normal cells under a microscope. Stage II adenocarcinoma of the esophagus
Stage II is divided into Stage IIA and Stage IIB, depending on where the cancer has spread. o o Stage IIA: Cancer has spread into the middle (muscle) layer of the esophageal wall. The tumor cells do not look at all like normal cells under a microscope and they grow quickly. Stage IIB: Cancer: has spread into the outer (connective tissue) layer of the esophageal wall; or is in the inner (mucosal) layer and may have spread into the middle (muscle) layer of the esophageal wall. Cancer is found in 1 or 2 lymph nodes near the tumor. Stage III adenocarcinoma of the esophagus Stage III is divided into Stage IIIA, Stage IIIB, and Stage IIIC, depending on where the cancer has spread. Stage IIIA: Cancer:
o o o o o o
is in the inner (mucosal) layer and may have spread into the middle (muscle) layer of the esophagealwall. Cancer is found in 3 to 6 lymph nodes near the tumor; or has spread into the outer (connective tissue) layer of the esophageal wall. Cancer is found in 1 or 2 lymph nodes near the tumor; or has spread into the diaphragm, sac around the heart, or tissue that covers the lungs, and lines the inner wall of the chest cavity. The cancer can be removed by surgery. Stage IIIB: Cancer has spread into the outer (connective tissue) layer of the esophageal wall. Cancer is found in 3 to 6 lymph nodes near the tumor. Stage IIIC: Cancer has spread: into the diaphragm, sac around the heart, or tissue that covers the lungs and lines the inner wall of the chest cavity; the cancer can be removed by surgery. Cancer is found in 1 to 6 lymph nodes near the tumor; or into other nearby organs such as the aorta, trachea, or spine, and the cancer cannot be removed by surgery; or to 7 or more lymph nodes near the tumor. Stage IV adenocarcinoma of the esophagus Recurrent Esophageal Cancer Recurrent esophageal cancer is cancer that has recurred (come back) after it has been treated. The cancer may come back in the esophagus or in other parts of the body
esophageal cancer is malignancy of the esophagus.The subtypes are adenocarcinoma and squamous cell carcinoma. Squamous cell carcinoma arises from the cells that line the upper part of the esophagus. Adenocarcinoma arises from glandular cells that are present at the junction of the esophagus and stomach.Esophageal tumors usually lead to dysphagia , odynophagia (painful swallowing) and other symptoms, and are diagnosed with biopsy. Small and localized tumors are treated surgically with curative intent. Larger tumors tend not to be operable and hence are treated with palliative care; their growth can still be delayed with chemotherapy, radiotherapy or a combination of the two.
Squamous cell carcinomas, which are similar to head and neck cancer in their appearance and association with tobacco and alcohol consumption, and adenocarcinomas, which are often associated with a history of gastroesophageal reflux disease(GORD) and Barrett's esophagus. A general rule of thumb is that a cancer in the upper two-thirds is a squamous cell carcinoma and one in the lower one-third is a adenocarcinoma. Dysphagia (difficulty swallowing) and odynophagia (painful swallowing) are the most common symptoms of esophageal cancer. Dysphagia is the first symptom in most patients. Odynophagia may also be present.Substantial weight loss is characteristic as a result of reduced appetite and poor nutrition and the active cancer.Most of the people diagnosed with esophageal cancer have late-stage disease. This is because people usually don't have significant symptoms until half of the inside of the esophagus, called the lumen, is obstructed.If the disease has spread elsewhere, this may lead to symptoms related to this: liver metastasis could cause jaundice and ascites, lung metastasis could cause shortness of breath, pleural effusions,etc.
Esophageal Cancer Anatomy To better understand esophageal cancer, it helps to understand the anatomy of the esophagus. The esophagus is a muscular tube that propels food from the mouth, to the stomach. It begins in the pharynx, just below the base of the tongue, and passes through the chest, next to the spine. It then passes through the diaphragm before emptying into the stomach. The bottom of the esophagus opens during swallowing, and then closes after the food has entered the stomach. This prevents food from leaking back into the esophagus. Anatomy examples: Junction of esophagus and stomach Entire intestinal tract
HOME CARE 1. ANOREXIA
Esophageal Cancer Anorexia Many patients with esophageal cancer will suffer from anorexia. Anorexia means loss of appetite. Anorexia is a problem with many forms ofcancer, because cancer can affect the body's hormones, digestive system and brain. It is also a common side effect of chemotherapy and radiation therapy. Good nutrition is an important part of successful cancer treatment. Adequate nutrition can boost the immune system and help increase the effectiveness ofcancer therapy. Home care for anorexia includes: o o o o o o Avoid stomach irritants such as aspirin or ibuprofen. Avoid excessive caffeine and other stimulants. Check with your doctor about drinking alcohol. Do not force yourself to eat at standard times. Eat when you are hungry instead. Concentrate on eating a healthy diet. Avoid junk foods. Select healthy, high-calorie foods that you enjoy. Eat more frequent, smaller meals. Get some exercise every day. Keep a daily log of your weight. Don't smoke. Nicotine can suppress the appetite. Ask your doctor or nutritionist about dietary supplements. Ask your doctor if any medications you may be taking can cause anorexia. Take any prescribed medications as directed. Anti-nausea medications: Compazine Reglan Zofran Appetite stimulants: Dronabinol (Marinol) Progesterones (Megestrol) Dexamethasone
2.
Liquid diet
There are two main types of liquid diets: clear liquids and full liquids. Persons who have esophageal cancer may have difficulty swallowing and may require aliquid diet for a period of time. Nutritional supplements are usually
necessary in this situation. These diets may be recommended for: o o o o o Swallowing difficulty: Esophageal cancer Achalasia Esophageal stricture Repeated vomiting Inflammatory gastrointestinal disease: Acute pancreatitis Exacerbations of inflammatory bowel disease
Clear Liquid Diet Clear liquids are liquids you can see through. Clear liquids can also contain some nutrition, but are usually not adequate to support the body's energy needs for more than a few days. Clear liquids are easily absorbed by the intestines. Liquids remove the stress on the intestines. Clear liquids include: Bouillon soup Coffee Broth Fruit juices without pulp Gelatin Popsicles (no pulp) Soft drinks Sports drinks (e.g. Gatorade) Tea Water
Full Liquid Diet This type of diet lies between a solid diet and clear liquids. It is often used by someone who is tolerating clear liquids, but cannot tolerate solid food. A full liquid diet can safely sustain the body for long periods of time. Full liquids include: Cream of wheat Fruit juices Honey Jelly Milk, milkshakes and ice cream Nutrition supplement drinks, such as Ensure or Boost Pureed meats
Pureed vegetables Soups without solids Syrups Vegetable juices Yogurt and pudding 3. Pain control
Medications commonly used to control pain and inflammation in adults with esophageal cancer include: o o o o o o o Acetaminophen Aspirin Aspirin decreases pain, fever and inflammation. It is a nonsteroidal anti-inflammatory medication (NSAID). Adult dosing is two regular strength (325 mg) every 4 hours with food. There are numerous products that contain aspirin. Follow the package instructions and NSAID precautions (below). Acetaminophen decreases fever and pain, but does not help inflammation. Adult dosing is 2 regular strength (325 mg) every 4 hours or 2 extra-strength (500 mg) every 6 hours. Maximum dose is 4,000 mg per day. Avoid this drug if you have alcoholism, liver disease or an allergy to the drug. See the package instructions. Common brand names include Tylenol, Panadol, and many others. Acetaminophen Controls pain, but has no anti-inflammatory properties Nonsteroidal anti-inflammatory drugs: Aspirin Ibuprofen Naproxen Ketoprofen Narcotic pain medications: Require a doctor's prescription Generally reserved for moderate to severe pain or severe pain
Ibuprofen Ibuprofen decreases pain, fever and inflammation. It is a nonsteroidal anti-inflammatory medication (NSAID). Adult dosing is 200-400 mg every 4-6 hours. Do not exceed 1,200 mg per day without a doctor's recommendation. Brand names include Advil, Motrin and Nuprin.
Follow the package instructions and NSAID precautions (below).
Naproxen Naproxen decreases pain, fever and inflammation. It is a nonsteroidal anti-inflammatory medication (NSAID). Adult dosing is 200 or 220 mg twice a day with food. Do not exceed 500 mg per day. Its brand name is Aleve. Follow the package instructions and NSAID precautions (below).
Ketoprofen Ketoprofen decreases pain, fever and inflammation. It is a nonsteroidal anti-inflammatory medication (NSAID). Adult dosing is 12.5 mg every 4-6 hours with food. Do not exceed 75 mg per day. Its brand name is Orudis KT. Follow the package instructions and NSAID precautions (below).
NSAID Precautions o o o o o o o o Avoid using alcohol when taking any of these medications. Do not mix prescription and non-prescription NSAIDS unless directed to do so by your doctor. NSAIDS can interact with other blood thinners, such as Coumadin, and cause bleeding complications. Ask your doctor before using an NSAID if you are pregnant or breastfeeding. Ask your doctor before using an NSAID if you have a history of: Allergy to aspirin Asthma Peptic ulcer disease Stomach ulcers Esophageal ulcers Bleeding problems Liver disease Kidney disease
4.
Side effects
Tips to control nausea and vomiting in someone with esophageal cancer include: Avoid stomach irritants such as aspirin or ibuprofen. Avoid exposure to unpleasant odors. Drink cool beverages throughout the day. Try un-sweetened tea or flat sodas.
o o o o o o o
Don't force yourself to eat at standard times. Eat when you are hungry instead. Concentrate on eating a healthy diet. Avoid junk foods. Eat more frequent, smaller meals. Relax in comfortable clothes after meals, but don't lie flat. Try relaxation techniques such as meditation. Ask your doctor or nutritionist about liquid dietary supplements. Ask your doctor about acupressure or acupuncture. Ask your doctor if any medications you may be taking can cause nausea orvomiting. Take any prescribed medications as directed. Medications used for nausea and vomiting due Aprepitant (Emend) Dolasetron (Anzemet) Granisetron (Kytril) Metoclopramide (Reglan) Ondansetron (Zofran) Palonosetron (Aloxi) Prochlorperazine (Compazine, Compro)
to chemotherapy include:
Irritation of the lining of the mouth and intestinal tract is called mucositis. Home care measures for mucositis include: o o o o o o o o o o Stop smoking Avoid hot, spicy and irritating foods. Drink plenty of liquids. Maintain good oral and dental hygiene with daily brushing, flossing and regular visits to your dentist. Try a soft diet. Try Chloraseptic or Cepacol spray, gargles or lozenges. Try Orabase B or Oral Balance topical dental paste. Try rinsing your mouth or gargling several times a day with a solution of one of the following: Salt water Baking soda Diphenhydramine (Benadryl) elixir or lozenges Dilute chlorhexidine (Peridex or Periogard) solution Dilute milk of magnesia or Maalox Use any prescribed medications for mucositis as directed. These may include: Oral acyclovir (Zovirax): for herpes infections Oral fluconazole (Diflucan): for fungal infections Palifermin (Kepivance) Topical dexamethasone (Decadron) Topical lidocaine (Xylocaine)
Topical nystatin (Mycostatin): for fungal infections
5.
Taking control
The successful treatment of esophageal cancer requires your participation. Here are answers to some important questions. Do you have control over your health and wellness? Many people believe they have no control over their health and wellness. Many ignore personal health decisions or simply leave them to their doctors, relatives, or friends. In reality, you have the greatest potential to determine your relative health. How is this possible? Do people really have control of their own health? The biggest killers are heart disease and cancer. Although many of these diseasesseem to strike at random, our lifestyle choices greatly influence personal risk. How can you participate in your health care? To participate you must: Learn to take responsibility for your own health. Learn to partner with your doctor. Learn how to make active decisions about your health.
How can you learn what you need to know? o o o o o Educate yourself. Be skeptical: Learn to separate fact from fiction. Billions of dollars are spent each year marketing dietary supplements, vitamins, and new medical Be careful about where you get your health information. Some of the best sources for health information on the web are professional societies and nonAsk your doctor what he or she recommends. Examine the credentials of the authors. If you are reading about symptoms and disease, your best source is a licensed physician. Pay attention to when the content was last updated. Make sure the person is not just trying to sell you something.
treatments. Much of this is unnecessary and wasteful.
profit organizations.
Important questions you need to answer: What things in your control can increase your risk for disease? What can you do to decrease this risk?
What are vaccines and how can they help you? How do your lifestyle choices increase your risk for disease? How can you reduce stress? What minor health problems can you treat at home? When is a medical problem "serious"? When should you call the doctor?
How can you find the right doctor? Key points: o Everyone should have a primary care physician or family doctor. A primaryphysician is usually a family Establish a relationship in advance with your doctor. Make sure you are comfortable with your primary care physician. The internet contains many resources where you can do research to locate the doctor that is best for you. You may wish to schedule a brief visit with the doctor to see if he or she is right for you. Be open-minded, and allow your doctor to know you well. This will improve communication.
practitioner, internist, or pediatrician.
Important information you need to make your decision: o major hospitals. o o o o o o o Look for board certification in the specialty. Ask about membership in medical societies. Community and professional reputation are also important. Are other patients happy with the doctor? Has the doctor been disciplined by hospitals or agencies? How long has the doctor been in practice? In general, more than a few malpractice suits over a 5-10 year period should trigger caution. Does the doctor communicate well? Are your questions answered during busy times? Does the doctor welcome you to help make decisions about your care? Is the doctor available when you need care? What is the doctor's after-hours coverage? Is he or she a member of a large group? Do the doctors' cross-cover one another? Where do they admit patients? Physician credentials: Internship and residency training is usually best from respected institutions, universities, and
What is shared decision making? You and your doctor must work together to jointly decide the best course of action to manage your health. This process is called "shared decision making". Your doctor becomes a guide and teacher and helps steer you toward the best treatment. Most doctors welcome this partnership. You must learn about your illnesses for shared decisionmaking to work.
For any recommended test, medication, or surgery, remember to ask: How will this help me? How much will it cost? Is it covered by your insurance? What are the potential side effects and risks? What are my alternatives?
For tests, remember to ask: Is it done in the office or at another facility? Is it painful? How will the results of this test influence my care?
For surgery or other procedures, remember to ask: How long will it take to heal? How many cases has the doctor done? What would your doctor do if he or she were the patient? Where is it done? Who will perform it? What are the doctor's qualifications?
What should you expect? Shared decision making becomes impossible if you do not know what to expect from your doctor. The American Hospital Association has published a "Patient's Bill of Rights" that is a good guide. It states that you have the right: To be spoken to in words that you understand To be told what's wrong with you To know the benefits of any treatment and any alternatives To know what a treatment or test will cost To share in treatment decisions To read your medical record To refuse any medical procedure
What should you do before an office visit? o o o Bring all important medical information with you to the visit. Make sure you can answer questions about the following: Allergies and side effects to medicines Current medicines you are taking. This includes herbs and vitamins. Make a list if necessary. Insurance information
o o o o o o o
Marital and sexual history Past injuries and hospital stays Past medical problems Past surgeries and operations Pre-visit questionnaires Use of tobacco, alcohol and drugs Work history
What should you expect from the visit? task. Talk to your doctor and do not leave the office without asking necessary questions. Your doctor can make you more comfortable if he or she understands your concerns. What should you know about your medications? Every year many people become ill because of problems with medications. Remember to ask: o o interactions. o o Some drugs interact with certain foods, vitamins, nicotine, and alcohol. Make sure you can drive or operate machines safely while taking a medicine. Ask your doctor how much a prescription costs. Is there a less expensive option or a generic version? What side effects to expect. What drug interactions are possible. Find out if a new medicine reacts with those that you are taking now. Many over-the-counter drugs and dietary supplements can also cause serious side effects and drug You should plan to wait if you go without an appointment. Emergencies or sick patients in the hospital may Bring along a book or toys for the kids. You may also have to wait during busy times. Tell your doctor about your problem in a clear manner. Start from the beginning and go through each Before the visit, think about what makes your problem better or worse. Your doctor will probably ask you Most doctors ask many questions about unrelated symptoms. These questions help assure that there are no Be sure to answer all questions truthfully. This includes sensitive questions about smoking, drug use, If you have any difficulty communicating your concerns, bring a family member or friend to assist in this
interrupt your doctor.
symptom as it appeared. questions about this. other problems that need attention. sexual activity, and work. Your history is the most important part of deciding what is wrong with you.
What is a treatment plan?
A treatment plan is what you and your doctor decide to do for an illness. A treatment plan cannot be effective without your participation. Three simple questions can help you get the most from your treatment plan: What is my main problem? What do I need to do? Why is it important for me to do these things?
Other important points: Be sure you understand your treatment plan. Stick with the treatment plan and allow time for improvement. Don't stop medicines when you feel better; check with your doctor first. Call your doctor if your condition is becoming worse. Your doctor should tell you what to expect and when to follow-up or call the office. 6.S/Sx Notify your doctor if you have esophageal cancer and any of the following: Vomiting blood Vomiting dark material that look like coffee grounds Black stool Rectal bleeding Choking during eating Worsening abdominal pain Worsening chest pain Inability to swallow Repeated vomiting
Anatomy of the Esophagus
The esophagus is a tube that makes up part of the digestive tract. It measures about 10 inches long. The esophagus connects the throat with the stomach, carrying the food and liquid you eat from your throat to the stomach. Thats why you often hear it called the food pipe. The esophagus is located behind the windpipe (trachea) and in front of the spine.
When you swallow, the esophagus tightens and relaxes, causing waves along the tube. This motion moves food down into the stomach. Glands in the esophagus create mucus to keep the lining moist and to make swallowing easier.
The wall of the esophagus has several layers. The innermost coating is called themucosa. Squamous cells are one kind of cell found in the mucosa throughout the esophagus. These cells are normally long and flat. Other cells are glandular oradenoid cells. These cells produce mucus and other fluids. They are found mostly in the stomach but may grow up into the lower part of the esophagus. The lowest end of the esophagus connects to the stomach. This is called thegastroesophageal (GE) junction. Often, this junction is where esophageal adenocarcinoma cancer starts, while squamous cell carcinoma starts anywhere in the esophagus.
Potrebbero piacerti anche
- Gastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDa EverandGastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNessuna valutazione finora
- Esophageal CancerDocumento8 pagineEsophageal CancerSakthiswaran RajaNessuna valutazione finora
- A Simple Guide to Adrenal Cancer, Diagnosis, Treatment and Related ConditionsDa EverandA Simple Guide to Adrenal Cancer, Diagnosis, Treatment and Related ConditionsNessuna valutazione finora
- Esophageal Cancer:-: Smoking Tobacco GerdDocumento4 pagineEsophageal Cancer:-: Smoking Tobacco GerdPriyanjali Saini100% (1)
- Pancreatic Cancer (Cancer of The Pancreas) : Patient Discussions: FindDocumento13 paginePancreatic Cancer (Cancer of The Pancreas) : Patient Discussions: FindMoses ZainaNessuna valutazione finora
- Treatments and Drugs: by Mayo Clinic StaffDocumento23 pagineTreatments and Drugs: by Mayo Clinic StaffJr D BayzNessuna valutazione finora
- Esophageal CancerDocumento3 pagineEsophageal CancerChanthorn SokNessuna valutazione finora
- Esophageal CancerDocumento66 pagineEsophageal Canceroezeamuzie100% (1)
- Esophageal CancerDocumento23 pagineEsophageal Cancerabhandlung100% (3)
- Colon CancerDocumento65 pagineColon CancerKristine Young100% (1)
- Hiatal Hernia AchalasiaDocumento22 pagineHiatal Hernia AchalasiaDhen MarcNessuna valutazione finora
- Adrenal DisordersDocumento48 pagineAdrenal DisordersMubeenUrRehmanNessuna valutazione finora
- Esophageal Cancer NewDocumento52 pagineEsophageal Cancer Newapi-282115150Nessuna valutazione finora
- JaundiceDocumento53 pagineJaundiceAbhishiktaAbhiNessuna valutazione finora
- What Are Liver EnzymesDocumento2 pagineWhat Are Liver EnzymesAAANessuna valutazione finora
- Peptic Ulcer Disease NCLEX ReviewDocumento16 paginePeptic Ulcer Disease NCLEX ReviewBianca Trish ManlangitNessuna valutazione finora
- Carcinoma StomachDocumento43 pagineCarcinoma StomachRukman Mecca100% (1)
- Case Presentation Lump Right HypochondriumDocumento22 pagineCase Presentation Lump Right HypochondriumNANDAN RAINessuna valutazione finora
- Heme Degradation & HyperbilirubinemiasDocumento30 pagineHeme Degradation & HyperbilirubinemiasSubhi MishraNessuna valutazione finora
- Teaching Project - Colon CancerDocumento3 pagineTeaching Project - Colon Cancerapi-384853579Nessuna valutazione finora
- Pancretic Cancer Case Study - BurkeDocumento52 paginePancretic Cancer Case Study - Burkeapi-282999254Nessuna valutazione finora
- Hepatomegaly 1Documento5 pagineHepatomegaly 1Bobby ParksNessuna valutazione finora
- An Approach To A Patient With JaundiceDocumento48 pagineAn Approach To A Patient With JaundiceSuranga Lakshitha PereraNessuna valutazione finora
- Carcinoma of The Breast - Bailey & LoveDocumento5 pagineCarcinoma of The Breast - Bailey & LoveKeyshia Yazid100% (1)
- Surgical Anatomy of The StomachDocumento75 pagineSurgical Anatomy of The StomachMohamoud MohamedNessuna valutazione finora
- Cancer of The LarynxDocumento16 pagineCancer of The Larynxhelaley_1983Nessuna valutazione finora
- Colon Cancer: Risk FactorsDocumento3 pagineColon Cancer: Risk FactorsAshley VillanuevaNessuna valutazione finora
- Physio Reviewer Renal To Acid BaseDocumento11 paginePhysio Reviewer Renal To Acid BaseNicole ChanNessuna valutazione finora
- SMALL INTESTINE QuickDocumento8 pagineSMALL INTESTINE QuickErald PaderangaNessuna valutazione finora
- Colorectal CancerDocumento29 pagineColorectal CancerLeeyanBhadzzVagayNessuna valutazione finora
- Case Study #5Documento2 pagineCase Study #5Jenny Jenders100% (1)
- Acute AbdomenDocumento8 pagineAcute Abdomenarum1992Nessuna valutazione finora
- PancreatitisDocumento12 paginePancreatitismardsz100% (5)
- Diagnostic Exam: Colonoscopy: A Thin, Flexible Tube With: PreventionDocumento1 paginaDiagnostic Exam: Colonoscopy: A Thin, Flexible Tube With: PreventionCarmina AguilarNessuna valutazione finora
- PANCREATITISDocumento38 paginePANCREATITISVEDHIKAVIJAYANNessuna valutazione finora
- 1.40 (Surgery) GIT Surgical Diseases - Diagnostics - Obesity ManagementDocumento10 pagine1.40 (Surgery) GIT Surgical Diseases - Diagnostics - Obesity ManagementLeo Mari Go LimNessuna valutazione finora
- Upper GITDocumento13 pagineUpper GITKiara Govender100% (1)
- Gastric Carcinoma: H. Pylori InfectionDocumento7 pagineGastric Carcinoma: H. Pylori InfectionMuvenn KannanNessuna valutazione finora
- Esophageal CancerDocumento42 pagineEsophageal Cancerapi-1964133750% (2)
- 1 - Fluid and Electrolytes (Schwartz Based)Documento52 pagine1 - Fluid and Electrolytes (Schwartz Based)Alexandra RebosuraNessuna valutazione finora
- Colorectal CancerDocumento7 pagineColorectal Cancerjames garciaNessuna valutazione finora
- Perforated Peptic UlcerDocumento68 paginePerforated Peptic UlcerSaibo BoldsaikhanNessuna valutazione finora
- Renal Cell CarcinomaDocumento15 pagineRenal Cell Carcinomadger11Nessuna valutazione finora
- Cancer Pain ManagementDocumento38 pagineCancer Pain ManagementZakkyMaulanaRahmat100% (1)
- Insisi Bedah 22 PDFDocumento36 pagineInsisi Bedah 22 PDFMiftah AjiNessuna valutazione finora
- Barium Studies: Presented byDocumento18 pagineBarium Studies: Presented byHannah samuelNessuna valutazione finora
- CHOLEDOCHOLITHIASISDocumento8 pagineCHOLEDOCHOLITHIASISkuncupcupu1368Nessuna valutazione finora
- Gastrointestinal System DisordersDocumento112 pagineGastrointestinal System DisordersTaate MohammedNessuna valutazione finora
- Jaundice: Seminar Under The Guidance Of-Dr. Shiva NarangDocumento47 pagineJaundice: Seminar Under The Guidance Of-Dr. Shiva NarangMiguel MansillaNessuna valutazione finora
- Acute Abdomen The "Black Hole" of MedicineDocumento99 pagineAcute Abdomen The "Black Hole" of MedicinedebarajuNessuna valutazione finora
- LI - Physical Examination - AbdomenDocumento6 pagineLI - Physical Examination - AbdomenTravis DonohoNessuna valutazione finora
- Appendicitis and PeritonitisDocumento22 pagineAppendicitis and PeritonitisElizar JarNessuna valutazione finora
- Cogan Syndrome Surger 4, AnkitDocumento18 pagineCogan Syndrome Surger 4, AnkitAnkit Tonger AnkyNessuna valutazione finora
- Obstructive Jaundice and Perioperative ManagementsDocumento8 pagineObstructive Jaundice and Perioperative ManagementsTri UtomoNessuna valutazione finora
- VolvulusDocumento38 pagineVolvulusHector RaulNessuna valutazione finora
- Case of Obstructive JaundiceDocumento38 pagineCase of Obstructive JaundiceadiNessuna valutazione finora
- Colon CancerDocumento17 pagineColon CancerYaska MusaNessuna valutazione finora
- Head and Neck Cancer GuidelinesDocumento96 pagineHead and Neck Cancer GuidelinesTri KurniawanNessuna valutazione finora
- Ovarian Cancer: Presented By-Vaishnavi Saxena B.SC Nursing 3 YearDocumento17 pagineOvarian Cancer: Presented By-Vaishnavi Saxena B.SC Nursing 3 YearVaishnavi Saxena100% (2)
- English Sistem EndocrineDocumento9 pagineEnglish Sistem EndocrineNurlaili YaniNessuna valutazione finora
- ProkaryoticDocumento8 pagineProkaryoticFraulin Leslie Sablas IrisariNessuna valutazione finora
- Prepared By: Dr. Ma. Angelita S. Rabanal, RN, MSNDocumento9 paginePrepared By: Dr. Ma. Angelita S. Rabanal, RN, MSNAngie SaquingNessuna valutazione finora
- Edema Paru Pit FM SMGDocumento36 pagineEdema Paru Pit FM SMGAnonymous ZrLxxRUr9zNessuna valutazione finora
- Diabetes & Metabolic Syndrome: Clinical Research & Reviews: Ganiyu Oboh, Ayokunle O. AdemosunDocumento5 pagineDiabetes & Metabolic Syndrome: Clinical Research & Reviews: Ganiyu Oboh, Ayokunle O. AdemosunDian Ayu ChotimahNessuna valutazione finora
- Sudden Law 'O of The Lariat - 1931 - PDFDocumento98 pagineSudden Law 'O of The Lariat - 1931 - PDFSreenath CharyNessuna valutazione finora
- Bone HealingDocumento2 pagineBone HealingGerardLum100% (2)
- Postnatal Growth and Development: Yenny Yustisia Dept. of Oral Biology Dentistry UNEJDocumento38 paginePostnatal Growth and Development: Yenny Yustisia Dept. of Oral Biology Dentistry UNEJMelisa Novitasari100% (1)
- The Final Edited ThesisDocumento25 pagineThe Final Edited ThesisBe ChahNessuna valutazione finora
- Consensus Report: Periodontic-Endodontic Lesions: Group MembersDocumento2 pagineConsensus Report: Periodontic-Endodontic Lesions: Group MembersAlex Grande CancapaNessuna valutazione finora
- 11 Must To Raise PigsDocumento21 pagine11 Must To Raise PigsNshim TheogeneNessuna valutazione finora
- Surgical IncisionDocumento35 pagineSurgical IncisionJoshua SmithNessuna valutazione finora
- Insects Identification Key PDFDocumento8 pagineInsects Identification Key PDFWilson Gomarga0% (1)
- Guía de Práctica N° 13:: Apellidos Y Nombre:Yanela Kimberly Vitor RamosDocumento5 pagineGuía de Práctica N° 13:: Apellidos Y Nombre:Yanela Kimberly Vitor RamosYanela Kimberly VitorNessuna valutazione finora
- In Search of The Later HahhemannDocumento9 pagineIn Search of The Later HahhemannJuan Jose JuarezNessuna valutazione finora
- Case Study Thiamine Deficiency in CatDocumento2 pagineCase Study Thiamine Deficiency in Catjerome olitinNessuna valutazione finora
- Assessment of Growth and DevelopmentDocumento29 pagineAssessment of Growth and DevelopmentKrupa JyothirmaiNessuna valutazione finora
- DR Deagle's H1N1 ReportDocumento61 pagineDR Deagle's H1N1 Reportkingofswords100% (1)
- B 4108 Borang COVID-19 Screening-Maria-18.09 PDFDocumento4 pagineB 4108 Borang COVID-19 Screening-Maria-18.09 PDFDonald RaymondNessuna valutazione finora
- Journal 1 - Plasenta PreviaDocumento5 pagineJournal 1 - Plasenta Previarizky ferdina kevinNessuna valutazione finora
- NCP-Ineffective Airway ClearanceDocumento13 pagineNCP-Ineffective Airway ClearancePaulo Manlangit86% (22)
- Reading Questions - Circulatory SystemsDocumento3 pagineReading Questions - Circulatory SystemsJanith VimukthiNessuna valutazione finora
- Higher Cortical Functions and Basis of LanguageDocumento78 pagineHigher Cortical Functions and Basis of Languagelovelots1234Nessuna valutazione finora
- Current Methods For The Diagnosis and Management of Twin - BallDocumento10 pagineCurrent Methods For The Diagnosis and Management of Twin - BallFrederick Ruz GonzalezNessuna valutazione finora
- TTS RespiDocumento1 paginaTTS RespiDinda BenitaNessuna valutazione finora
- The Endocrine System and Feedback MechanismsDocumento8 pagineThe Endocrine System and Feedback MechanismsJame SmithNessuna valutazione finora
- Superficial MycosisDocumento61 pagineSuperficial MycosisBrightKinglySweetDomsonNessuna valutazione finora
- Integrementary System 2Documento16 pagineIntegrementary System 2meyerscNessuna valutazione finora
- AL BSL OrdinancesDocumento152 pagineAL BSL OrdinancesMelanie HughesNessuna valutazione finora
- Latihan Sains UPSRDocumento6 pagineLatihan Sains UPSRAlia AminNessuna valutazione finora
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Da EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Valutazione: 3 su 5 stelle3/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityDa EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityValutazione: 4 su 5 stelle4/5 (30)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDa EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNessuna valutazione finora
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionDa EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionValutazione: 4 su 5 stelle4/5 (404)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisDa EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisValutazione: 4.5 su 5 stelle4.5/5 (42)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDDa EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDValutazione: 5 su 5 stelle5/5 (3)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDa EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeValutazione: 2 su 5 stelle2/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDa EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedValutazione: 5 su 5 stelle5/5 (81)
- The Marshmallow Test: Mastering Self-ControlDa EverandThe Marshmallow Test: Mastering Self-ControlValutazione: 4.5 su 5 stelle4.5/5 (60)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsDa EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsValutazione: 5 su 5 stelle5/5 (1)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDa EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsValutazione: 4 su 5 stelle4/5 (4)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaDa EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Obesity Code: Unlocking the Secrets of Weight LossDa EverandThe Obesity Code: Unlocking the Secrets of Weight LossValutazione: 4 su 5 stelle4/5 (6)
- Why We Die: The New Science of Aging and the Quest for ImmortalityDa EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityValutazione: 4 su 5 stelle4/5 (5)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsDa EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsValutazione: 4.5 su 5 stelle4.5/5 (170)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeDa EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeValutazione: 4.5 su 5 stelle4.5/5 (253)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisDa EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisValutazione: 3.5 su 5 stelle3.5/5 (2)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Da EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Valutazione: 4.5 su 5 stelle4.5/5 (110)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryDa EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryValutazione: 4 su 5 stelle4/5 (45)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessDa EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessValutazione: 4.5 su 5 stelle4.5/5 (328)
- Empath: The Survival Guide For Highly Sensitive People: Protect Yourself From Narcissists & Toxic Relationships. Discover How to Stop Absorbing Other People's PainDa EverandEmpath: The Survival Guide For Highly Sensitive People: Protect Yourself From Narcissists & Toxic Relationships. Discover How to Stop Absorbing Other People's PainValutazione: 4 su 5 stelle4/5 (95)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesDa EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesValutazione: 4.5 su 5 stelle4.5/5 (1412)