Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Logy Notes
Caricato da
Rose LiDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Logy Notes
Caricato da
Rose LiCopyright:
Formati disponibili
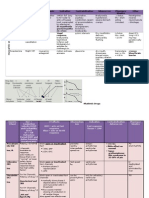
Disease Seronegati ve (no autoantibo dies) Spondyloar thropathies (Anko Spond, Reactive, IBS, Psoriatic) Ankylosing Spondylitis More
common in YOUNG Men
Genetics/Environmental Mechanisms Completely DIFFERENT set of genes that other inflammatory diseases NOT PRECEDED BY AN INFECTION PERSAY Maybe respond to commensal bacteria? HLA B-27 (MHC Class I, but acts like class II? homodimerize)- subtypes 97% of patients with AS low PPV HLA B-27 patients have poor ability to handle GI bacteria Evidence for GI association Gram (-) enteropathogenic bacteria Microscopic bowel inflammation present in most B27+ patients w/spondylitis, even those w/o GI symptoms High IgA levels ( mucosal) Alternative explanations? HLA-B27 form homodimers Cause stress response Activate CD4 T-cells (act like MHCII)
Presentation Chronic Inflammatory disorder of axial skeleton lower back pain> 3months calcification of the vertebrae joints Multisystem: spine, peripheral joints, & periarticular structures Axial arthritis- Sacroiliitis & inflammation involving lumbosacral spine Enthesitis- inflammation of sites of ligament & capsular attachment to bone Extraarticular manifestions inc. Uveitis, Aortitis, Psoriasis-like skin & nail changes Inflammation of intervertebral ligaments, leading to bone formation w/in disc space & loss of flexibility Iritis & Iridocyclitis (irregular pupil periphery from affected ciliary muscles)
Clinical/ Diagnosis Pathognomic: inflammation of sacroiliac joint Dx by SI X-Raytrabeculae span jointno space Pain relieved by activity, not helped by rest Lumbar flexibility Schobers test NO arch in back chest expansion Spinal X-Ray shows new bone, Squaring of Vertebrae
Pathogenesis No autoantibodies 1. Molecular Mimicry- Autoimmunity 2o Response to infection with sequence similarity b/t Bacterial Ag/B27 Complex & HLA B27/Self peptide complex 2. Arithritogenic Peptide- immune response to peptide that can only be presented by B27 molecule; may activate pool of autoreactive T Cells, be a bacterial Cross Reactive peptide, or a self-peptide 3. Altered host-microbe interactionsB27 impairs ability to clear bacteria -ex. Chlamydia induced RxA -patients w/RxA have prolonged Ab response to GI pathogens failure to clear Salmonella
Seronegati ve Spondyloar thropathies Reactive Arthritis
Maybe immune complex deposition? (Non-Gonoccal) Urethritis or cervicitis-Chlamydia HLA-B27+ patients w/IBD Psoriatic Arthritis Bacterial Ag associated w/GI inflammation found in joint, disease preceded by GI bacterial infection PPL who get RA have persistent
Asymmetric Polyarthritis joint Inflammation Enthesitis Infectious Diarrheas triggered by GI pathogens Presents acutely Resolves ~80% Skin & nail manifections -2-4 weeks post-infection
Inflammatory Eye Dz Balanitis Oral Ulcerations Keratoderma
No autoantibodies Mouse models: express 100 copies of HLA-B27 in mice Inflammatory disease in GI Spinal arthritis Skin and nail changes Male disease sterility If never exposed to GI flora (germ free), never develop disease Inject bacteria DEVELOP disease
Disease
Genetics/Environmental Mechanisms antibodies (fail to clear salmonella) HLA-B27 cell lines take longer to clear infection
Presentation
Clinical/ Diagnosis
Pathogenesis
Infectious Arthritis usually monoarticul ar disease Need some inflammatory trigger
Infection caused by 1. Hematological spread post S. aureas, Strep or H. Influenzae infections 2. Direct inoculation: bites, punches, or injury esp in Diabetics (peripheral neuropathy) foreign body puncture, osteomyelitis PREDISPOSITIONS: 1. prior jt damage 2. RA/osteoarthritis 3. DIABETES 4. organ failure 5. immunosuprresion steroids 6. HIV 7. Trauma DRB1*0401 allele- OspA (Lyme Ag) may induce auto-immunity via Molecular Mimicry to LFA-1
Historically grouped by 1. Non-gonoccocal: warm swollen joint (BIG) 2. Gonnococcal: 1. Like non-gonoccocal or 2. Disseminated gonnoreal infection (DGI): fever, chills, malaise, rash, tenosynovitis Damage by: 1. Direct effects (bacterial proteases) 2. Host-inflammatory: (Exotoxins LPS or immune-host reaction) IL1, IL6, IL8, cytokines, MMPs, ROS, PMNs, Macro, TNFa 3. Mechanical: Purulant exudate, causes ischemia prevent bloodflow (irreversible damage in 48 hrs!) Irreversible Subchondral Bone Loss can occur in 3-5 days Musculoskeletal involvement One or two swollen joints Oligoarthritis sometimes becoming chronic
JOINT ASPIRATE Cloudy, purulant, viscosity PMN > 95% WBCs > 50,000 >75% gram + 50% S. aureas Viruluance factors : (ie. For S. aureas) MSCRAMMs (microbial surface antigens ) Regulated by AGR gene and at low cell number, they facilitate attachment, but at high cell number, they upregulate tissue destroying enzymes
Epitope Spreading- Immune response initially directed at one element of multicomponent complex can spread to other elements of complex via X-priming by APCs Cartilage breakdown Molecular Mimicry- Ag stimulates Immune response that X-reacts w/autologous elements: e.g. (Streptococcus triggering Rheumatic Fever, anti-resi LYME) Cryptic Epitopes- Previously unseen epitopes exposed during Inflammatory response Antigen Persistence- Various elements of Ag or Ag itself persists & spreads, driving ongoing immune response: e.g. Chlamydia Immune Complexes- Ag-Ab complexes that form in serum & are deposited in tissues; often associated w/ subsequent immune response Immune complex formation; spirochetes invade synovium Driven by type II (inflammatory responeses, not direct damage)
Infectious Arthritis Lyme Dz Show up in winter time
Two types I. Early disseminated (1-3 mnths) II . late, (>3yrs): seronegative, non-septic: 2/3 of untreated patients
Joint aspirate: can be <50,000 WBCs Borrelia DO NOT produce its proteases Joint damage NOT as
Disease (august infection)
Genetics/Environmental Mechanisms MHC-II HLA-DRB1 0401 presents Epitope of OspA (on borrelia) activates T-cells that also recognize LFA1a (integrin on inflamed tissues) but LFA-1 is weak and doesnt bind similarly Arthralgias and arthritis- common in females from work w/young kids
Presentation
Clinical/ Diagnosis pronounced
Pathogenesis Can be Antibiotic Resistant Molecular mimicry .
Initial Arthalgias are common, w/intermittent Treat with Antibiotics for several months, infection stays Persistent knee effusion Resistant: immunosuppresants Rubella: Post-immunization Parvo: 1. happen if infected 1st time as adult 2. Presents like RA
Are they still seronegative???
Infectious Arthritis Rubella Parvovirus B19 (most common) Infectious Arthritis Neisseria gonorrhea Infectious Arthritis HBV
Seronegative Arthritis- PIPs & MCPs
Ag persistence access to joint by Gb4 (glycophopholipid R) Parvovirus DNA in synovium in bone marrow and joints of ppl with Parvovirus arthritis Nml ppl have it too
Young women, around menses, sexually active
Developing countries, rare today in western nations increased tissue deposition
Disseminated Gonnoreal Infection: Type II: Fever, shaking, chills, joints hurt but not big swollen joints, Pustules are classic Intense pain but no exudates Type I: Like others Arthritis/Arthralgia HBsAg Abs- formation of immune complexes deposit in synovium Hepatitis Sx appear after Ag is cleared
begins w/Serum sickness-like prodrome Complexes consumption Disease dont start until IgGs start forming
immune-complex mediated
Disease Vasculitis DEFINE BY VESSLE SIZE
Genetics/Environmental Mechanisms 1o Inflammation of Blood Vessels- pathology directed against vessels
Presentation Biopsy will show: 1. Immune complex deposition 2. Leokocyte infiltration 3. Vascular damage
Clinical/ Diagnosis Classify by vessel size 1.Large aorta 2. Medium Arterial 3. Small Microvasculitis a. ANCAs b. immune complex deposition Multi-organ involvement spares LUNG and glomerulus of kidneys
Pathogenesis
Vasculitis PAN Polyarteritis Nordosum
Rare Used to think it was associated with Hep B, not anymore Linked to shear stress during inflammatory processes
Nodular swelling Rheumatic symptoms Medium and small vasculars Affects kidney, liver, heart Ischemic symptoms: digital ischemia gangrene Thickening of vessel walls Abdominal pain; intestinal angina Kidneys respond to ischemia by upregulating RENIN Na retention Renal-vascular hypertension
To demonstrate damage Lumenal narrowing/ vessel thickening Fibrin rich from dead/damaged inflammatory cells damage Trichrome stain: Destruction of internal and external elastic lamina destruction of lamina
FIBRINOID NECROSIS
Widening, aneurysms, and dilatation of vessels beads on a string angiogram: to identify narrowing biopsy: transmural inflammation; luminal occlusion Always involves LUNG and glomerulus of kidneys Progressive swelling ANCA ANKLES peri-nuclear: pANCA) confirm with ELISA against myeloperoxidase (cytoplasmic; cANCA)- most specific, least common proteinase 3
Vasculitis ANCA--AntiNeutrophil Cytoplasmic AntibodyANCAassociated Vasculitis Wagners Granumaloti s -Primed PMNs express PR3 on surface- Abs bind precipitated by certain bacterial infections
Endothelial cells damage Neutrophila activation -Palpable Purpura- Erythematous, Puritic, Non-blanching rash; Necrosis/Blistering indicates edema & tissue damage ANCAS MEDIATE DISEASE BY ACTIVATING PMNS
Vasculitis Leukocytocl astic wbc
Cytokines which activate PMNs (IL-1,8, TNF) also stimulate endothelial cells to express selectins
Palpable purpura, Fever, Urticaria, Arthralgia, Immune complex mediated Rash in lower body PMN
Complement levels, ESR Abs & complement revealed by Immunofluorescence Vessels will light up
IC deposits attract PMNs vessel permeability -PMNs release lysosomal enzymesdamage endothelium Extravasation of RBCs, Edema, WBC infiltration of tissue ANCA ACTIVATE PMNs adherence to vascular endothelium, degranulation, lysosomal enzymes damages vessels, allowing extravasation of RBCs activates platelets, endothelial cell proliferation resulting in vessel occlusion Most common b/c precipitated by Lupus, cancer (HC leukemia), drugs (sulfa), infections (hep C) Right after an infection is cured
Disease fragmentati on immune complex mediated
Genetics/Environmental Mechanisms Not by ALL immune complexes; depends on size of complexes: occurs where there is an excess of antigens
Presentation infiltrates, dead and dying near vessels (C3a, C5a, chemoattractant) Necrosis- tissue damage w/fibrin deposits
Clinical/ Diagnosis
Pathogenesis
ASSOCIATED WITH LUPUS Immune complex mediated
Disease Osteoarthrit is
Genetics/Environmental Mechanisms Trauma by 16x NOT estrogen AGE some known genetic factors Muscle & support tissue weakness, Subchondral Bone, Inflammation, Mechanical Alignment, Crystal deposits & Inflammation Treatment Hyaluronic Acid jt. lubricant; Jt. Replacement, Weight Loss to reduce symptoms NSAIDs Muscle Strengthening Future: MMP Inhibitors, Cytokine Inhibitors Reduce risk ? CAM- Glucosamine, Bisphosphonates may be helpful (OTC supplement)
Presentation Contrast to RA: Synovitis is localized, not-uniform present; develops over time Biochem/Biomechan mechanism, NOT auto-immune Cartilage breakdown directly results in Inflammation, not vice versa No osteopenia Sclerosis denser regions Irregular, Fissured surface Crepitus Osteophytes- bony outgrowths in an attempt to heal Narrowing of space b/t bone visible on X-Ray Edema, Microcracks, loss of GAGs (retain Water) lose cushioning Fissuring & Pitting Loss of Type II Collagen (specific to Cartilage), replaced by other, less effective (ie. Type I) Erosion of Bone where synovium touches the bone Morning Stiffness >1hr Spine unaffected- unlike Spondylarthropathies Periarticular Osteopenia Vasculitis, Serositis, Sjogrens Syndrome (affected Lacrimal & Salivary Glands dry eyes and mouth) Pannus- hypertrophic, hyperplastic synovium, inflammatory cells, granulation & fibrous tissue- erodes cartilage & bone Macrophages hepcidin anemia Treatment: Steroids, NSAIDS, Methotrexate
Clinical/ Diagnosis ACUTE BIG TOE CHRONIC Morning Stiffness <30 min Pain on Use/sitting for long time Synovial WBC count <500 fluid often straw/gold in color Instability, Limited ROM, Calor DIPs & PIPs hypertrophy KNEES and HIPS Malalignment of joints Joint space narrowing cartilage lost PRIMARY PATHOLOGY = cartilage X-ray need weight bearing Bone eburnation and sclerosis Symmetric ANEMIA OF CHRONIC DISEASE ESR Synovial damage FIRST Polyarthritis- >3 Joints, Hand Joints: 1st MCP Joint (unlike OA), MCPs, PIPs, Ulnar Deviation Serum Rheumatoid Factor Rheumatoid Nodules granuloma Fibrinoid necrosis Synovial biopsy, smears PRIMARY PATHOLOGY = synovium
Pathogenesis Pressure in joint (mechanical, obesity, trauma) Chondrocytes activate Make cytokines MMP, aggrecanases, ADAM proteases, Microfractures, fissures PDGF Cartilage breakdown where synovium penetrates it Chrondrocytes apoptosis More cytokines
Rheumatoid Arthritis
1% of population autoimmune shared epitope HLA-DRB1-0401 prominent in young women ANTI-CCP antibodies Smoking Related to DRB1 Rhematoid Factor 80% of patients POLYCLONAL ANTIBODY Immune complexes Not impor initially, but impor for perpetuation of disease
Synovial membrane thickening, Perivascular infiltrates of CD4+, Plasma Cells, Ms Chronic reaction PMNs in synovial fluid, rarely in tissue , IL-1 activate production of RANK-L by T cells, stromal cells, & synovial fibroblasts Osteoclast differentiation bone destruction cytokines induce MMPs which degrade cartilage-2o to bone destruction Rheumatoid Factor- Polyclonal Ab (often IgM) to Fc receptor
TNF
ANTI-CTLA abatacept!
Life-span shortened Atherosclerosis, MI
TNF receptors antagonist Check PPD Prone to infection RANK inhibition
region of IgGformation of Immune complexes may trigger complement cascade vasculitis, serositis
Gout hyperuricem ia Monosodium -Urate Crystal deposition in joint. Pseudogout = Rhomboid, blue
90% M 40s ETHANOL -Treatments NSAIDs, Dietary purine reduction, Allopurinol 2o causes- Excessive Intake, Increased Nucleic Acid Turnover (Leukemias, Anemias), Accelerated ATP degradation- Ill individuals Overproduction and Undersecretion Alcohol consumption, G6Pase Deficiency PRPP (De novo) amidophosphorybotransferase (RateLim De novo) Xanthine Oxidase uric acid HGPRT (SALVAGE) URATE-1 (pyrazinamide, nicotinate, BAD) (probenecid GOOD)
CHRONIC GOUT GRANULOMA Tophaceous nodules Acute Uric Acid Nephropathyprecipitation of crystals in collecting ducts and ureters Acute Renal Failure, Uric Acid Kidney Stones Acute Gouty Arthritis- MSU crystals trigger inflammatory mediatorsC5a, Contact Factor Clotting pathway 1. Inflammasome monocytes 2. IL1b IL1R 3.NF-kB signaling 4.Cytokine production 5.PMN infiltration
Hyperuricemia inadequate for diagnosis Pathognomic Needle Shaped crystals negatively biferingic inside PMNs under polarized light need biopsy When light is parallel, the crystal is YELLOW consider Septic Arthritis in Dx 1st MTP Joint, Knee, Ankle Histology: clear areas where crystals were and absorbed Histiocytes are walling off to form foreign body granulomas
PMN influx MSU induced synovitis Monocytes phagocytosis rupture of Phagolysosomal membrane release of inflammatory mediatorsIL 1,6,8 TNF 10% cause = Overproduction PRPP overactive Purine synthesis Amidophosphoribosyltransferase Rate-limiting step:Purine HGPRT- Catalyzes salvage rxnDeficiency ( Purine) Xanthine Oxidase overactive Purine Inhibit w/ Allopurinol! 90% cause = reduced Excretion 95% through Glomerulus is reabsorbed into Proximal tubule- Lactate, Ketoacids, PZA, Probenecid Probenecid treats hyperuricemia -40% Post-secretory Reabsorption; 10% Excreted
RA Tx & Principles of Therapy Goals: systemic relief of Dz activity improved Quality of Life minimal Toxicity Categories o NSAIDS
o o o o
Glucocoricoids Disease Modifying Anti-Rheumatic Drugs Methotrexate- 1st-line DMARD Biologics Monoclonal antibodies -ximab chimeric (Rituximab, infliximab) 75% humanized -zumab - <5% human (Natalizumab) -umab FULLY human (adalimumab) Receptor fusion proteins -cept (etanercept, abatacept) Metalloproteinases
Strategy Start with AGGRESSIVE tx Methotrexate Block Intracellular machinery DMARD But not as targeted, off-target effects 1.Methotrexate a. Most commonly used 2nd line (2nd only to NSAIDS for pain) b. Block dihydrofolate reductase c. adenosine d. cytokines e. antiangiogenic f. Rheumatoid factor 2.Leflunomide a. Pyrimidine antagonist b. For people who have neg rxt to methotrexate c. T Cells d. Toxicity include diarrhea, alopecia etc Biologics DIRECT, but can cause infections o o o o 1. Block activation Abetacept CTLA-4 + Fc of IgG block CD80/86 binding to CD28 by binding to B-cell CD80 Block T-cell dependent humoral response (co-stimulation) 3. Anti-B cell antigens to kill B cells a. Rituximab b. Chimeric IgG1 to B-cell antigen CD20 c. Fab binds to CD20 (expressed on naive B cells) d. Fc recruits complement and lyse B cells e. Inhibits B cell activation and proliferation f. Plasma cells still there 4. Cell signaling a. Targets IL1, TNFa b. Also IL1, IL6
c. Fleeting TNF homotrimers and engages TNF receptors A. Adalimuab, Golimumab Fully human IgG1 B. Infliximab chimeric IgG1 C. Etanercept D. Bind TNFa ligand IL6 a. Toccilizumab b. Blocks both transmemebrane and soluble IL-6 receptors 5. Intracellular Molecules of signaling a. NF-kB transcription b. JAK inhibit receptor activity/prevent STAT activation fairly safe Target inflammatory output c. Corticosteroids d. NSAIDS e. MMP inhibitors
TNF very bad osteoclast activation Endothelial cell activation Chemokine release Chondrocyte activation Angiogenesis Hepcidin
Disease and Epi Scleroderma F, 30-50 Prevalence in Choctaw NAs 100% concordance of antibodies, but only 6% concordance of disease Hair loss due to regression of vessels, no, absent PMN infiltrates because of occlusion
Genetics/Environmen tal Mechanisms HLA DQ7- antiTopoisomerase I Abs HLA DQ5 vinyl chloride Mouse model KO for fibrillin gene TSK mouse shows skin abnormalities like humans Duplication Mutation of Fibrillin gene FBN1 Fibrillin ECM Disorganized; Inappropriate signaling to fibroblasts TGF, less MMP Collagen I transcription/depo s Fetal MicrochimerismIntermingling of Maternal & Fetal DNA Allogeneic Engraftment of cells into tissuesGVHD Rapeseed Oil (aniline contamin)
Presentation Capillary dropout (nailfolds) Digital gangrene (ischemia) Chronic ulcers Systemic Scleroderma Symmetric, bilateral widespread skin fibrosis Distal & proximal extremities, trunk and face Rapid progression Early visceral organ damage Anti-topo I Anti-RNAPol -CREST- Symmetric but restricted skin fibrosis often involving only distal extremities (to MCP) delay in internal organs dmg Anti-centromere Calcinosiscalcifications in tissues Raynauds - Vascular spasms Esophageal Dismotility- fibrosis w/in esophagus Sclerodactylyhardening in fingers Telangectasias - features of other
Clinical/ Diagnosis +ANA w/Nucleolar Pattern on ANA Non-specific- 95% w/+ANA Anti-topo I Anti-RNAPol Anti-centromere -Lung Involvement- 70% of cases -Diffuse fibrotic replacement of lung tissue- associated w/Anti-Topo -Pulmonary HTNfrom fibrosis or SM hypertrophy morbidity, death in 2yrs Renal Crisis can occur early and abruptly VasospasmsIncreased Reactivity, both Cutaneous & Visceral Vasospasms Ultimately type I collagen is the most predominant molecule
Rx cytokines act on fibroblasts as transcription regulatory protein Synthesis of ECM- Type I Collagen -replaces SQ dermis & fat
Pathogenesis 1. Autoimmunity mediated by B-cells Identify autoantibodies (ANA in ~95%); nonspecific, NOT pathogenic 2. Plateles, monocytes cytokines lead to Ongoing Vasospasm Structural s Intimal and SMC Proliferation, Matrix Deposition decreased luminal size Ischemia occlusion, Reynolds 3. Endothelial Cell Injury and cytokine production Apoptosis of endothelial cells ROS stim by injury (persistent, Granzyme A (T Cell Serine Protease) Endothelin on Endothelial cells to increase PDGF, mitogen of FB Fib PDGF-R by TGF IL4 (by t-cells), IL1 (by FBs, Mono, Dendrities) : FB proliferation 4. Stimulation Endothelial cells to Endothelin secretion vasoconstriction fibroblasts Collagen synthesis, TGF- secretion and MORE endothelin 5. TGF self-perpetuate collagen, ECM transcription TFG endothelin synthesis PDGF-Rs ROS, antioxidant enzymes 6. RESULTS in fibrosis
TGF
Disease and Epi
Genetics/Environmen tal Mechanisms EBC, CMV C1q deficiency ~ 100%PPV Type II&III Immune responses Apoptosis seems normal, but there may be reduced clearance of blebs - UV exposure can exacerbate HLA-?!??! Integrins TLRs Fcgammac Estrogens?
Presentation Rheumatic Dz (SLE, Polymyositis) 4/11 to diagnose: Malar Discord Photosensitivity Arthritis Serositis Renal Oral Ulcers Hematological Neurological Immunologic Anti-nuclear antibodies
Clinical/ Diagnosis
Rx
Pathogenesis
SLE Vertical transmissionSx usually persist until maternal Abs are cleared Neonatal cardiac block
INF signature (microarray (+Direct Coombs Test)-Ab-mediated hemolytic anemia Anti-Nuclear Abs present
anti-SM (snRNPs)
anti-dsDNA anti-Lo/Ra (snRNPs) anti-centromeres cardiolipins;antipho pshlipids aPPT Vasculitis ANA nearly 100% of the time IgG- deposits in tissue and activate complement complement levels (complement consumption)
Rituximab, NSAIDs, AntiMalarials (Mech. Unknown), Steroids, Immunosuppres sives Cyclophosphami de New Targeted AntiComplement, AntiCD40/CD40L (BCell Receptor/T Cell Ligand), CTLA4 Ig, Anti-BAFF
-10:1 F:M- no difference in severity or onset; possibly related to sex hormones -T Cells- needed to stimulate B Cells for Auto-Ab production; end up w/Cell Mediated Immunity &susceptibility to infection -IL 4, 6, 10 levels; BAFF- M-derived B Cell stimulator NeonaTAL lupus ANTI-RHO/Anti-LA mediated IMMUNE COMPLEX MEDIATED
Membranous Cytopenias Anemia Hematuria Proteinuria Renal Dz (Smooth Glomerular Deposition of Abs); Thrombosis
Sjogrens Lymphocytic infiltration of exocrine glands; diminished lacrimal and salivary gland secretions TAL
Deminished lacrimal and salivary gland secretion
Diabetes
Loss of peripheral innervation
Death of all nerve branches leads to charcoal joint No joint spaces Muscles weak Premature
Osteoarthritis
Inflammation of
Loss fine-tune stability
Disease and Epi Inflammatory Myopathy
Genetics/Environmen tal Mechanisms muscles Ehlers Danlos Syndrome Collagen V defects
Presentation
Clinical/ Diagnosis osteoarthritis Spreads to adjacent joints
Rx
Pathogenesis
Potrebbero piacerti anche
- Cardio Pharm ALLDocumento17 pagineCardio Pharm ALLRose LiNessuna valutazione finora
- Cardio Pharm ALLDocumento17 pagineCardio Pharm ALLRose LiNessuna valutazione finora
- Cardio Pharm ALLDocumento17 pagineCardio Pharm ALLRose LiNessuna valutazione finora
- Biology EntymologyDocumento5 pagineBiology EntymologyRose Li100% (1)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (119)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Nursing Care of Clients Undergoing Eye SurgeryDocumento1 paginaNursing Care of Clients Undergoing Eye SurgerySewyel GarburiNessuna valutazione finora
- ADR UzbekistanDocumento80 pagineADR UzbekistanJose Juan Velazquez GarciaNessuna valutazione finora
- Biological Control 178 (2023) 105145 M. Yousefvand Et AlDocumento5 pagineBiological Control 178 (2023) 105145 M. Yousefvand Et AlGenaina CristofoliNessuna valutazione finora
- A Potential Siddha Mineral Drug Pavala ParpamDocumento8 pagineA Potential Siddha Mineral Drug Pavala Parpamjmanuel108yahoo.co.ukNessuna valutazione finora
- Air Traffic Controllers Warned on Sleeping on the JobDocumento108 pagineAir Traffic Controllers Warned on Sleeping on the Jobeduardo juniorNessuna valutazione finora
- ABO Incompatible Platelets: Risks Versus Benefit: ReviewDocumento5 pagineABO Incompatible Platelets: Risks Versus Benefit: Reviewmy accountNessuna valutazione finora
- Introduction and Basic Principles: Dr. K. S. Abbasi Department of Food Tech/Human NutritionDocumento8 pagineIntroduction and Basic Principles: Dr. K. S. Abbasi Department of Food Tech/Human Nutritionnouman ashrafNessuna valutazione finora
- Letter To VA From The Quinism FoundationDocumento2 pagineLetter To VA From The Quinism FoundationWUSA9 TVNessuna valutazione finora
- OEC ch25Documento10 pagineOEC ch25Phil McLeanNessuna valutazione finora
- Basic Haematology Exercise 1 (MKEB2403)Documento10 pagineBasic Haematology Exercise 1 (MKEB2403)kiedd_04100% (8)
- Chest Rub Ointment ExperimentDocumento2 pagineChest Rub Ointment ExperimentIsabel PeraltaNessuna valutazione finora
- Physiology Practice Questions: Parasympathetic Nervous System CharacteristicsDocumento4 paginePhysiology Practice Questions: Parasympathetic Nervous System CharacteristicsGregg ShanksNessuna valutazione finora
- AIPG Paper CorrectedDocumento42 pagineAIPG Paper CorrectedbrihaspathiacademyNessuna valutazione finora
- PMO - Pasteurized Milk OrdinanceDocumento340 paginePMO - Pasteurized Milk OrdinanceTato G.k.Nessuna valutazione finora
- Thandi Facial Electrical Case StudyDocumento4 pagineThandi Facial Electrical Case StudyLionel YdeNessuna valutazione finora
- Hand When You Need Them MostDocumento9 pagineHand When You Need Them MostJim SchotterNessuna valutazione finora
- International Journal of Gynecology and ObstetricsDocumento5 pagineInternational Journal of Gynecology and ObstetricsLilian Rahma AnandaNessuna valutazione finora
- Biochemistry Aspect in Human Reproduction: Lastri Mei WinarniDocumento19 pagineBiochemistry Aspect in Human Reproduction: Lastri Mei WinarniLastri Mei WinarniNessuna valutazione finora
- Nutritional Care in Respiratory Disease: DR Haerani Rasyid, Mkes, SPPD, K-GHDocumento94 pagineNutritional Care in Respiratory Disease: DR Haerani Rasyid, Mkes, SPPD, K-GHDesywinNessuna valutazione finora
- Nursing Care Plan #1 Assessment Explanation of The Problem Goal/Objective Intervention Rational EvaluationDocumento10 pagineNursing Care Plan #1 Assessment Explanation of The Problem Goal/Objective Intervention Rational EvaluationmalindaNessuna valutazione finora
- Causes, Signs, and Treatment of HyponatremiaDocumento65 pagineCauses, Signs, and Treatment of HyponatremiaFaryalBalochNessuna valutazione finora
- How Can Women Make The RulesDocumento0 pagineHow Can Women Make The Ruleshme_s100% (2)
- Grand Soya Oil 2Documento15 pagineGrand Soya Oil 2Yusuf HamidNessuna valutazione finora
- Erythrocyte Sedimentation Rate (ESR) - Group 5)Documento14 pagineErythrocyte Sedimentation Rate (ESR) - Group 5)U WidNessuna valutazione finora
- MacroMinerals: Calcium, Phosphorus, Potassium, Sodium, Chloride, and MagnesiumDocumento9 pagineMacroMinerals: Calcium, Phosphorus, Potassium, Sodium, Chloride, and MagnesiumDerek AtienzaNessuna valutazione finora
- The Impact of Life Cycles on Family HealthDocumento27 pagineThe Impact of Life Cycles on Family Healthmarcial_745578124Nessuna valutazione finora
- Modified Double Glove TechniqueDocumento1 paginaModified Double Glove TechniqueSohaib NawazNessuna valutazione finora
- Cardiovascular Embryology StagesDocumento109 pagineCardiovascular Embryology StagesBir Singh100% (1)
- Mustang Track Loader Mtl25 Service Manual 908313 RevcDocumento23 pagineMustang Track Loader Mtl25 Service Manual 908313 Revcnicoleorr110382okaNessuna valutazione finora
- Basics of Microvascular SurgeryDocumento33 pagineBasics of Microvascular SurgeryPratikshya KothiaNessuna valutazione finora