Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Cushing's Syndrome
Caricato da
summerduskCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Cushing's Syndrome
Caricato da
summerduskCopyright:
Formati disponibili
Disorder
Cushings Syndrome/ Hypercortisolism
Risk factors
Prevalence & Demographics
Spontaneous Secondary- following therapeutic admin of synthetic steroids/ACTH caused by prolonged exposure to elevated levels of either endogenous or exogenous glucocorticoids. degree of cortisol overproduction is very variable. Spontaneous-rare : ~<5/million/year Exogenous steoids is the #1 cause 2-5% prevalence for obese patients with type 2 diabetes, especially those with poor glucose control and hypertension For Cushings syndrome due to an adrenal/pituitary tumour- Female:Male=5:1 Peak incidence of cushings syndrome caused by an adrenal or pituitary adenoma- between 25-40 years Ectopic ACTH production due to lung cancer- later in life
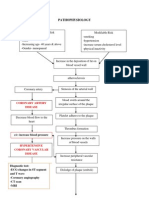
Causes & Pathogenesis
Exogenous use of glucocorticoids- Corticosteroid medications such as prednisolone, Eg. For asthma, SLE, Rheumatoid arthritis Tumours of the adrenal gland Cushings disease Tumour elsewhere in the body which causes an increased cortisol Tumours which cause increased ACTH (eg pancreas, lung, thyroid) Can be divided into two groups: ACTH-Dependent disease Non-ACTH dependent disease - Excessive ACTH from the pituitary (Cushings disease) - Adrenal adenomas (65% of cases) - Adrenal carcinomas - Ectopic ACTH-producing tumours - Excess glucocorticoid administration - ACTH administration Others: Alcohol-induced pseudo-Cushings syndrome
Presentation
Pigmentation occurs only with ACTH-dependent causes. A Cushingoid appearance can be caused by excess alcohol consumption (pseudo-Cushing's syndrome) - the pathophysiology is poorly understood. Impaired glucose tolerance or frank diabetes is common, especially in the ectopic ACTH syndrome. Hypokalaemia due to the mineralocorticoid activity of cortisol is common with ectopic ACTH secretion.
QuickTime and a decompressor are needed to see this picture.
QuickTime and a decompressor are needed to see this picture.
Differential diagnosis
-Pseudo-Cushing's syndrome: all or some of the clinical features of Cushing's syndrome, combined with biochemical evidence of hypercortisolism (but not caused by pituitary-adrenal axis problems). Causes include: Chronic severe anxiety and/or depression Prolonged excess alcohol consumption can cause a cushingoid appearance Obesity Poorly controlled diabetes HIV infection
Investigation
Full blood count: raised white cell count. Electrolytes and acid-base balance: hypokalemia (common with ectopic ACTH secretion as a result of
mineralocorticoid activity),metabolic alkalosis.
QuickTime and a decompressor are needed to see this picture.
Q u ic k T im e a n d a d e c o m p re s s o r a re n e e d e d to s e e t h is p ic t u re .
Treatment & Management
tissue fragility, poor wound healing, hypertension, and diabetes mellitus, increase the risks of surgery. Drug therapy remains very important for normalising cortisol levels while awaiting the impact of more definitive treatment. Cortisol hypersecretion must be controlled prior to surgery or radiotherapy if at all possible. Drugs Metyrapone, ketoconazole, and mitotane can all be used to lower cortisol by directly inhibiting synthesis and secretion in the adrenal gland. Metyrapone and ketoconazole are enzyme inhibitors and have rapid onset of action, but control of hypercortisolism is often lost with corticotropin oversecretion in Cushing's disease. These drugs are not usually effective as long-term treatment and are used mainly for preparation for surgery or as adjunctive treatment
The treatment of choice in most patients is surgical, but the metabolic consequences, including increased
after surgery or pituitary radiotherapy. Mitotane acts as an adrenolytic drug with delayed onset but long-lasting action, but control of corticotropin oversecretion in Cushing's disease is maintained. Medical treatment can also be used in patients who are unwilling or unfit for surgery. Treatment can be used long term for patients with ectopic corticotropin secretion, but adrenalectomy may be preferred. Etomidate can be used for acute control of severe hypercortisolaemia. Surgical treatment Treatment of choice for: Pituitary tumours: trans-sphenoidal microsurgery. Radiation therapy may be used as an adjunct for patients who are not cured. Bilateral adrenalectomy may be necessary to control toxic cortisol levels. Adrenocortical tumours: require surgical removal. Laparoscopic surgery is now the treatment of choice for unilateral adrenal adenomas. Removal of neoplastic tissue is indicated for ectopic ACTH production. Metastatic spread makes a surgical cure unlikely or impossible. Bilateral adrenalectomy is indicated if necessary to control toxic cortisol levels. Pituitary radiotherapy Persisting hypercortisolaemia after trans-sphenoidal surgery can be treated with pituitary radiotherapy. Conventional fractionated radiotherapy is very effective but is associated with longterm hypopituitarism and can be very delayed in effectiveness. Prognosis
Incompletely controlled Cushing's syndrome - five-fold excess mortality Most common causes of Cushing's-associated mortality- hypertension, myocardial infarction, infection and
heart failure. The prognosis is guardedly favorable with surgery. The rare adrenocortical carcinomas have a 5-year survival rate of 30% or less. Complications Metabolic syndrome Hypertension Impaired glucose tolerance and diabetes Obesity Hyperlipidaemia: raised LDL cholesterol and triglycerides Coagulopathy: thrombophilia Osteoporosis Perforated viscera Impaired immunity, including opportunistic fungal infections Nelson's syndrome: may follow bilateral adrenalectomy for Cushing's disease
A primary pituitary tumour may cause pan-hypopituitarism and visual loss
Social
http://www.netterimages.com/image/19567.htm http://www.sciencedirect.com/science/article/pii/S0140673606686996 http://www.patient.co.uk/doctor/Cushing's-Syndrome.htm
Potrebbero piacerti anche
- Cefixime: Suprax Class and CategoryDocumento3 pagineCefixime: Suprax Class and CategoryArianne Joy SalvadorNessuna valutazione finora
- PathophysiologyDocumento1 paginaPathophysiologyHazel PalomaresNessuna valutazione finora
- GitDocumento302 pagineGitjgcriste100% (7)
- TriageDocumento8 pagineTriageSarah GuintoNessuna valutazione finora
- Nursing Management Pancreatic CancerDocumento2 pagineNursing Management Pancreatic CancerKit NameKo100% (2)
- Hypertension NclexDocumento5 pagineHypertension Nclexハニファ バランギNessuna valutazione finora
- Universidad de Zamboanga Tiguma, Pagadian City Competency Appraisal II Pre Final ExamDocumento5 pagineUniversidad de Zamboanga Tiguma, Pagadian City Competency Appraisal II Pre Final ExamKirsten SabanalNessuna valutazione finora
- HCVD Cad Cva InfarctionDocumento2 pagineHCVD Cad Cva InfarctionPamela DomingoNessuna valutazione finora
- Endocrine System Prepared By: Prof. Mike Chavez RN, USRNDocumento7 pagineEndocrine System Prepared By: Prof. Mike Chavez RN, USRNMeiJoyFlamianoIINessuna valutazione finora
- Hypertension NCLEX Quiz Questions: A. I Will Make Sure I Consume Foods High in PotassiumDocumento5 pagineHypertension NCLEX Quiz Questions: A. I Will Make Sure I Consume Foods High in PotassiumMelodia Turqueza GandezaNessuna valutazione finora
- Myocardial Infarction (Diseases For Oral Revalida)Documento12 pagineMyocardial Infarction (Diseases For Oral Revalida)Suzette PipoNessuna valutazione finora
- Hepatocellula R CarcinomaDocumento45 pagineHepatocellula R Carcinomamhean azneitaNessuna valutazione finora
- Chest Pain Care PlanDocumento2 pagineChest Pain Care Planapi-545292605Nessuna valutazione finora
- Path o PhysiologyDocumento9 paginePath o PhysiologyKyle Ü D. CunanersNessuna valutazione finora
- Film Analysis: in Health Care Ethics (NR-NUR127)Documento5 pagineFilm Analysis: in Health Care Ethics (NR-NUR127)John MagtibayNessuna valutazione finora
- Introduction - MIDocumento10 pagineIntroduction - MIkhimiiiNessuna valutazione finora
- Pathophysiology of Acute CholecystitisDocumento2 paginePathophysiology of Acute CholecystitisKush KhannaNessuna valutazione finora
- Co DiovanDocumento2 pagineCo DiovanianecunarNessuna valutazione finora
- CetirizineDocumento2 pagineCetirizinelintangNessuna valutazione finora
- Pulmonary EmbolismDocumento16 paginePulmonary EmbolismniyigokNessuna valutazione finora
- Benign Prostatic HyperplasiaDocumento4 pagineBenign Prostatic Hyperplasiaエド パジャロンNessuna valutazione finora
- AtireviewDocumento163 pagineAtireviewGlory Mimi0% (1)
- Pleural Fluid Analysis: How The Test Is PerformedDocumento4 paginePleural Fluid Analysis: How The Test Is PerformedKevin LlorenteNessuna valutazione finora
- PHEOCHROMOCYTOMADocumento25 paginePHEOCHROMOCYTOMAKristian Dave Diva100% (1)
- To Be PrintedDocumento13 pagineTo Be PrintedJosette Mae AtanacioNessuna valutazione finora
- NCP PainDocumento2 pagineNCP PainApril_Ivy_Raga_3835Nessuna valutazione finora
- HEMARATE FA Hemarate FA Consists of Folic AcidDocumento2 pagineHEMARATE FA Hemarate FA Consists of Folic AcidMarhina Asarabi MukimNessuna valutazione finora
- CoparDocumento4 pagineCopar.fayefen100% (4)
- Kabiven: (Amino Acids, Electrolytes, Dextrose and Lipid Injectable Emulsion), For Intravenous UseDocumento24 pagineKabiven: (Amino Acids, Electrolytes, Dextrose and Lipid Injectable Emulsion), For Intravenous UseDivine Mercy De JulianNessuna valutazione finora
- Rafols, Janna Mae L. 3F-2C OR QuestionsDocumento8 pagineRafols, Janna Mae L. 3F-2C OR QuestionsJan Crizza Dale R. FrancoNessuna valutazione finora
- The Correlation Between Disease Stage and Pulmonary Edema Assessed With Chest Xray in Chronic Kidney Disease PatientsDocumento6 pagineThe Correlation Between Disease Stage and Pulmonary Edema Assessed With Chest Xray in Chronic Kidney Disease PatientsAnnisa RabbaniNessuna valutazione finora
- SiadhDocumento10 pagineSiadhehjing75% (4)
- Evaluation Exam MidtermDocumento29 pagineEvaluation Exam MidtermPaolo DioquinoNessuna valutazione finora
- Final Major Clinical Case Study Online VersionDocumento14 pagineFinal Major Clinical Case Study Online Versionapi-282107708Nessuna valutazione finora
- Adult HealthDocumento28 pagineAdult HealthL1NEDS DNessuna valutazione finora
- Topic 1: Introduction To Geria Nursing: Activity 1.1: Grandparents' LoveDocumento11 pagineTopic 1: Introduction To Geria Nursing: Activity 1.1: Grandparents' LoveMarissa AsimNessuna valutazione finora
- Pharmacologic Management: BleomycinDocumento1 paginaPharmacologic Management: BleomycinKim ApuradoNessuna valutazione finora
- Grand Coaching: Medical Surgical NursingDocumento22 pagineGrand Coaching: Medical Surgical NursingEsarpy (Nana)Nessuna valutazione finora
- Liver CancerDocumento1 paginaLiver CancerTarantado67% (3)
- Acute Kidney InjuryDocumento43 pagineAcute Kidney InjuryIwan ToniroNessuna valutazione finora
- COVID-19: Brian, Fernando, Jason, FelitaDocumento8 pagineCOVID-19: Brian, Fernando, Jason, FelitaCharson ChenNessuna valutazione finora
- Oral Revalida MuscuDocumento3 pagineOral Revalida MuscuDoyTanNessuna valutazione finora
- Sas 35Documento2 pagineSas 35Sistine Rose LabajoNessuna valutazione finora
- Cap Grand Case PreDocumento46 pagineCap Grand Case PreMatty FelNessuna valutazione finora
- Cutask 5Documento2 pagineCutask 5Nicole RagustaNessuna valutazione finora
- JDM Care PlanDocumento5 pagineJDM Care PlangopscharanNessuna valutazione finora
- Drug StudyDocumento8 pagineDrug StudyRizzi DeveraNessuna valutazione finora
- Drug Study FinalDocumento6 pagineDrug Study FinalJade HemmingsNessuna valutazione finora
- Meniere's Disease - Case StudyDocumento3 pagineMeniere's Disease - Case StudyZORANASNNessuna valutazione finora
- Are You Kidding MeDocumento10 pagineAre You Kidding MeChelsea RoseNessuna valutazione finora
- From Chronic To Critical: A Latino Family Confronts End-of-Life DecisionsDocumento2 pagineFrom Chronic To Critical: A Latino Family Confronts End-of-Life DecisionsRoyKimNessuna valutazione finora
- Pathophysiology Cushing S SyndromeDocumento4 paginePathophysiology Cushing S SyndromeMaria Luisa VillalunaNessuna valutazione finora
- Group 2 DkaDocumento73 pagineGroup 2 DkaAkio Ozaraga100% (1)
- Addison'sDocumento4 pagineAddison'sKoRnflakesNessuna valutazione finora
- Case Analysis On Respiratory DisordersDocumento5 pagineCase Analysis On Respiratory DisordersAaron ConstantinoNessuna valutazione finora
- A Simple Guide to Parathyroid Adenoma, Diagnosis, Treatment and Related ConditionsDa EverandA Simple Guide to Parathyroid Adenoma, Diagnosis, Treatment and Related ConditionsNessuna valutazione finora
- Community Acquired Pneumonia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDa EverandCommunity Acquired Pneumonia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNessuna valutazione finora
- Competency #14 Ay 2022-2023 Social StudiesDocumento22 pagineCompetency #14 Ay 2022-2023 Social StudiesCharis RebanalNessuna valutazione finora
- Curriculum Vitae ofDocumento4 pagineCurriculum Vitae ofAndrew OlsonNessuna valutazione finora
- Tabulation Sheet (LABO)Documento9 pagineTabulation Sheet (LABO)KetIanCotalesNessuna valutazione finora
- LoperAmid 1Documento5 pagineLoperAmid 1Hemma KusumaningrumNessuna valutazione finora
- Navigation - Star FinderDocumento31 pagineNavigation - Star FinderPrasadtNessuna valutazione finora
- Low Voltage Alternator - 4 Pole: 25 To 60 kVA - 50 HZ / 31.5 To 75 kVA - 60 HZ Electrical and Mechanical DataDocumento12 pagineLow Voltage Alternator - 4 Pole: 25 To 60 kVA - 50 HZ / 31.5 To 75 kVA - 60 HZ Electrical and Mechanical DataDjamel BeddarNessuna valutazione finora
- Elaborare Modele de Rating in Conformitate Cu IFRS 9Documento8 pagineElaborare Modele de Rating in Conformitate Cu IFRS 9MstefNessuna valutazione finora
- Argumentative EssayDocumento7 pagineArgumentative EssayHoang Thi Huyen DieuNessuna valutazione finora
- Unpriced Proposed Renovation of Bugolobi Flat, Block C For Uganda Coffee Development AuthorityDocumento39 pagineUnpriced Proposed Renovation of Bugolobi Flat, Block C For Uganda Coffee Development AuthoritynicolasNessuna valutazione finora
- Prototyping: by DR Sampa Unnikrishnan Yateer Creative Solutions Reachus@Yateer - In, 8971442777Documento70 paginePrototyping: by DR Sampa Unnikrishnan Yateer Creative Solutions Reachus@Yateer - In, 8971442777ShivashankarNessuna valutazione finora
- CATL 34189-20AH Low Temperature Cell SpecificationDocumento17 pagineCATL 34189-20AH Low Temperature Cell Specificationxueziying741Nessuna valutazione finora
- Educational Strategic Plans in Nigeria: Challenges of Implementation and Ways ForwardsDocumento7 pagineEducational Strategic Plans in Nigeria: Challenges of Implementation and Ways ForwardsresearchparksNessuna valutazione finora
- Utah Vaccine AdministrationDocumento1 paginaUtah Vaccine AdministrationOffice of Utah Gov. Spencer J. CoxNessuna valutazione finora
- Admission Prspectus English 2021-2022Documento9 pagineAdmission Prspectus English 2021-2022A.B. SiNessuna valutazione finora
- Gynaecology Thesis TopicsDocumento7 pagineGynaecology Thesis TopicsDawn Cook100% (2)
- Emc VNX MatrixDocumento8 pagineEmc VNX Matrixpolivni0% (1)
- Answer Set 5 - Fall 2009Documento38 pagineAnswer Set 5 - Fall 2009zachNessuna valutazione finora
- Negotiation SimulationDocumento11 pagineNegotiation SimulationJade Arbee BarbosaNessuna valutazione finora
- Draft Plant Design PaperDocumento65 pagineDraft Plant Design Paper202040336Nessuna valutazione finora
- Position Trading Maximizing Probability of Winning TradesDocumento91 paginePosition Trading Maximizing Probability of Winning Tradescarlo bakaakoNessuna valutazione finora
- Andre Bazin, The Ontology of The Photographic Image From His Book What Is Cinema Vol. IDocumento8 pagineAndre Bazin, The Ontology of The Photographic Image From His Book What Is Cinema Vol. IAnkit LadiaNessuna valutazione finora
- Annex 1: Homeroom Guidance Monitoring Tool (School Level) Homeroom Guidance Monitoring ToolDocumento2 pagineAnnex 1: Homeroom Guidance Monitoring Tool (School Level) Homeroom Guidance Monitoring ToolMariel Gregore0% (1)
- FPI - Study Permit Application GuideDocumento9 pagineFPI - Study Permit Application GuideKian Mark DarioNessuna valutazione finora
- Simon Bolivar PresentationDocumento7 pagineSimon Bolivar Presentationapi-345742212Nessuna valutazione finora
- Binary To DecimalDocumento8 pagineBinary To DecimalEmmanuel JoshuaNessuna valutazione finora
- MBTI - 4 Temperaments: Guardians (SJ) Rationals (NT) Idealists (NF) Artisans (SP)Documento20 pagineMBTI - 4 Temperaments: Guardians (SJ) Rationals (NT) Idealists (NF) Artisans (SP)Muhammad Fauzan MauliawanNessuna valutazione finora
- Epri Guide For Transmission Line Groundingpdf PDF FreeDocumento188 pagineEpri Guide For Transmission Line Groundingpdf PDF FreeHolman Wbeimar Suarez Niño100% (1)
- Listening 3b Skills Test 1aDocumento3 pagineListening 3b Skills Test 1aPticaSelicaNessuna valutazione finora
- Nur Syamimi - Noor Nasruddin - Presentation - 1002 - 1010 - 1024Documento14 pagineNur Syamimi - Noor Nasruddin - Presentation - 1002 - 1010 - 1024abdulhasnalNessuna valutazione finora
- Risk Factors of Oral CancerDocumento12 pagineRisk Factors of Oral CancerNauman ArshadNessuna valutazione finora