Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Examination of The Patient - I, P. 158-167
Caricato da
lycan007Descrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Examination of The Patient - I, P. 158-167
Caricato da
lycan007Copyright:
Formati disponibili
CHAPTER
11
not always clear. However, this information may provide information regarding the physical and mental maturation and general health of a patient. The questions must be asked skillfully and gently so as not to cause guilt feelings in the mother or to imply that a mistake was made in the delivery room. An attempt should be made to establish the age at which the position of the patients eyes was rst noted to be abnormal. It is especially valuable to know the opinion of the parents as to which eye deviates and whether it is always the same eye that is turned. When this question is asked, it is not unusual for the mother of a child with an obvious esotropia of the left eye to state that the right eye deviates. The right eye? one asks. Look at the child. Sure, the right eye, says the mother and points her nger toward the childs left eye. It is also important to learn whether the deviation was constant or intermittent at rst and whether it becomes worse when the child is tired or ill, more obvious in distance xation or in near vision, and worse or better when the patient is visually attentive or daydreaming. The existence of a cyclic pattern of strabismus (see Chapter 21) should always be remembered when taking the history.
Examination of the PatientI
PRELIMINARIES
History
A carefully obtained history, beginning with the family history, is essential in treating a patient with neuromuscular anomalies of the eyes. One should ask not only about grandparents, parents, and siblings but also about more distant relatives (uncles, aunts, cousins). The questions should not be restricted to actual turning of the eyes. An effort should also be made to nd out whether a large number of relatives wear strong glasses. We have found the question of whether a relative has or had a lazy eye of little help since that term means different things to different people and thus the answers may be misleading. While the ophthalmologist may use this term to explain amblyopia to the patient or the parents, the layperson will use it for any number of ocular anomalies, which may include amblyopia but also any form of latent or manifest strabismus, refractive errors, or other types of visual decits. Next, the personal history of the patient should be obtained, beginning with the mothers pregnancy and the events at birth. Factors such as prematurity and birth weight, unusual length of labor, abnormal position, and use of instruments should be documented. The extent to which these factors contribute to the etiology of strabismus is
158
Examination of the PatientI
159
Certain manifestations are often volunteered by the parents. For instance, they may report that their child closes one eye in bright light, which is a phenomenon often but not exclusively associated with an intermittent deviation (see Chapter 17). The parents should be asked whether convulsions, disease, or trauma preceded onset of the deviation. Then ask about development of the child (motor, speech), health, motor behavior patterns, handedness, general behavior anomalies such as enuresis, and last but very important, about any treatment for the strabismus (glasses, patching, exercises, operations) that the patient may have had. In adults and in all patients in whom onset of the deviation is acute, one should determine whether diplopia is present if the patient does not voluntarily report this symptom. If so, ascertain whether diplopia is present at all times when both eyes are open or whether it occurs more often or is more marked in distance vision or in near vision. The term double vision does not necessarily have the same meaning for every patient as it does for the ophthalmologist (p. 153). Careful questioning may reveal that the patient is bothered by blurring of vision or a partial overlay of contours rather than by actual image separation. Demonstration of true diplopia by holding a prism before one eye of the patient may save time otherwise wasted by looking for a nonexistent motility problem. In patients with no obvious ocular deviation, complaints about double vision should immediately alert the physician to the possibility of monocular diplopia. Retesting with a cover held rst before one eye and then before the other eye will quickly establish whether diplopia is monocular or binocular. All histories must be evaluated critically; at times they are of doubtful value. Occasionally, baby pictures of the patient are useful in substantiating the parents claim about the time of onset of the deviation. The accuracy of observation of some people is low and their memory short. Parents often do not care to admit that their child may have a defect, especially if the defect is familial on the side of the reporting parent. They may overstress the seriousness of an accident or illness and look for a cause of a condition that actually preexisted. Nevertheless, when talking with a seemingly reliable mother, the ophthalmologist will do well not to take her report too lightly. More often than not she is right. For example, if a mother is quite sure that her childs eyes are misaligned only occasionally, for instance, after
school or when daydreaming, and if the ophthalmologist is unable to nd a deviation during the rst examination, it is unwise to dismiss the patient with the advice that nothing is wrong. Quite likely the ophthalmologist will nd a deviation at one of the next examinations. Taking the history need not consume a long time, but however long it takes, it is time usefully spent. From the history the more experienced ophthalmologist often can arrive at a presumptive diagnosis, which is particularly helpful in very young, uncooperative patients on whom it may not be possible to perform a detailed examination at the rst visit. Busy ophthalmologists may have a lay assistant or orthoptist take the history. However, ideally, this task should not be delegated to another, for this rst encounter with a patient and his or her family provides a unique opportunity to follow and evaluate certain leads and to establish communication and a basis for trust between the physician and the patient or parents. Moreover, during this initial discussion the patient may be casually observed for evidence of the type of strabismus (unilateral or alternating), the preferred eye, an anomalous head posture, and so on. This is often helpful in young children who may become intimidated and uncooperative once the actual examination starts.
Assessment of Visual Acuity in Children
Testing the vision of patients with neuromuscular anomalies of the eyes is not merely a matter of having them read a chart. It is a more complex procedure because of the youth of many of these patients and because of certain characteristics of visual acuity (see Chapter 7), especially in amblyopia (see Chapter 14).
Estimation of Visual Acuity in Infants
Although knowledge of the actual visual acuity in normal infants and its development in early childhood is important, the ophthalmologist treating an infant who manifests a heterotropia is more concerned with the acuity of one eye relative to that of the other rather than with absolute visual acuity levels in each eye. It must be known whether amblyopia is present in one eye. Such a nding is important, and luckily it can be readily
160
Introduction to Neuromuscular Anomalies of the Eyes
established in most instances by mere observation of the patient. If by history and observation one eye is always deviated and if the infant objects more strenuously to covering one eye than the other, the assumption of amblyopia must be made, provided the fundus examination was normal, and immediate treatment is mandatory. The importance of establishing xation preference in diagnosing amblyopia is discussed further in Chapter 14. The growing awareness of the sensitivity of immature visual systems to abnormal stimulation,3, 26, 42, 43, 60 the need to treat amblyopia early in life, and the prevention of visual deprivation amblyopia by overtreatment have stimulated development of quantitative methods to estimate visual acuity in infants. Three such methods (optokinetic nystagmus, preferential looking, and evoked cortical potentials) are now available. While few pediatric ophthalmologists use these methods routinely in an ofce environment, these techniques have added to our knowledge of the development of visual acuity in infants. For a summary of the developmental aspects of visual acuity testing in infants and a comparison of the different methods available, the reader is referred to recent reviews.6, 12, 13, 20, 21, 47, 57
OPTOKINETIC NYSTAGMUS. Optokinetic nys-
still elicits an eye movement (minimum separable, p. 114) is a measure of visual acuity. The only cooperation required is that the subject be awake and hold both eyes open. Gorman and coworkers22 were the rst to use this method of acuity testing in newborns. Other investigators rened the method11 and extended its use to older infants.17, 19, 31 These data varied considerably, undoubtedly because of methodological differences in stimulus parameters and response determination; however, one can reasonably conclude from these studies that optokinetic nystagmus acuity is at least 6/120 in the newborn and improves fairly rapidly during the rst few months of life. Dobson and Teller13 offered valuable suggestions about how to standardize the testing procedure and response evaluation of this method. Since it has been reported that optokinetic responses can be elicited in the presence of cortical blindness,59 this test must be interpreted cautiously since subcortical mechanisms may be involved. Moreover, a negative response may be due to lack of attention to the optokinetic stimulus and to a delayed maturation of the motor pathways involved with the response.9, 16
PREFERENTIAL LOOKING. This technique is
tagmus has been used for a long time to determine visual acuity objectively. Nystagmus is elicited by passing a succession of black and white stripes through the patients eld of vision. The visual angle subtended by the smallest stripe width that
based on the fact that an infants attention is more attracted by patterned stimuli than by a homogeneous surface. 4, 18 Consequently, if offered the choice between a patterned stimulus (e.g., black and white stripes) and a homogeneous background, an infant will prefer to look at the pat-
FIGURE 111. Testing of an infants acuity with forced-choice preferential looking. The observer is hidden behind the screen and monitors through a peephole the direction of eye or head movements in response to the appearance of the striped stimulus. (From Teller DY, Movshon JA: Visual development. Vision Res 26:1483, 1986.)
Examination of the PatientI
161
terned stimulus as long as the pattern is above the visual acuity threshold. This technique, originally described by Fantz,18 was further developed by Dobson and Teller and their coworkers14, 55 to exclude observer bias. During the test, an observer is hidden behind a screen on which a visually homogeneous surface on one side of the screen is alternated randomly with black and white stripes on the other side. The baby faces the screen, and the observer records the direction of head or eye movements in response to the appearance of the striped stimulus (Fig. 111). Gwiazda and coworkers23 further modied the preferential looking method and Jacobson and coworkers28 reported its effectiveness in monitoring the visual acuity of the occluded eye in infants undergoing treatment for amblyopia. Most studies have shown that this method of acuity testing is especially suitable for infants up to 4 months of age. Older infants are too easily distracted. Visual acuities determined with this method range from approximately 6/240 in the newborn to 6/60 at 3 months and 6/6 at 36 months of age37 (Fig. 112). It is generally assumed that foveal immaturity contributes to the lower neonatal visual acuity, although it may not be its exclusive cause.25 To adapt the time-consuming, forced-choice preferen-
tial looking procedure to a clinical setting, McDonald and coworkers39 introduced acuity cards (Teller Acuity Cards, Vistech, Inc., Dayton, OH) containing grating patterns of various spatial frequencies. An observer watches an infants eye and head movements in response to repeated presentations of these cards at a 38 cm xation distance. This method has undergone extensive clinical testing (for a review of the literature, see Dobson12) and has been accepted by some pediatric ophthalmologists as an ofce procedure for estimating visual acuity in infants. It must be realized, however, that grating acuity testing cannot automatically be equated with acuity testing based on recognition tasks, such as naming pictures or Snellen letters. In normal children, grating acuity is better than recognition acuity,38, 58 and this difference is exaggerated in children with amblyopia.15, 30, 36, 44, 48 Thus children with strabismic amblyopia and other forms of visual impairment may have their visual acuity underestimated, which limits the value of the Teller Acuity Card Test in clinical practice.8, 32, 46 As a visual screening method the Teller cards yield a high rate of false-positive results.53 The improved performance on spatial discrimination vs. recognition tasks suggests that different
FIGURE 112. Compilation of behavioral data from different studies showing the development of binocular grating acuity in humans over the rst 5 postnatal years. (From Teller DY, Movshon JA: Visual development. Vision Res 26:1483, 1986.)
162
Introduction to Neuromuscular Anomalies of the Eyes
neural processing mechanisms in the brain are addressed by either test. For this reason caution is advised in listing Snellen acuity equivalents when displaying grating acuity data, a practice that has become widespread in psychophysical literature (see Fig. 112). Such comparisons, though of some value for quick orientation, must be considered approximations rather than true equivalence. Examiner bias, accuracy of measurement, and failure to detect myopia are listed as additional limitations of this method.12 Held and coworkers5, 24 applied the principle of preferential looking to assessing stereoacuity in infants and concluded that the mean age at which stereopsis could rst be demonstrated was 16 weeks. By the mean age of 21 weeks, stereoacuity was 1 minute of arc or better. Thus, in comparison with visual acuity, development of stereopsis is quite rapid.
VISUALLY EVOKED POTENTIALS. A variety of
stimuli and recording methods using cortical potentials have been used to assess visual acuity in infants. Marg and coworkers,35 using square wave gratings alternated with a homogeneous eld to produce transient visually evoked potentials (VEPs), demonstrated visual acuity of 6/120 at 1 month of age, which rapidly reached standard adult acuity by 6 months of age. Sokol51 recorded steady-state VEPs produced by alternating checkerboards and reported visual acuity values to be slightly below those obtained by Marg. VEP Vernier acuity remains strikingly immature throughout the rst year of life, similar to behavioral Vernier acuity.49 However, most VEP studies suggest that the infant visual system matures to allow detection of 6/6 targets by at least 1 year of age or possibly earlier. The discrepancy between estimated acuity values established by the optokinetic nystagmus and preferential looking techniques and those obtained using VEPs by 6 months of age (Table 111) must be noted. However, Sokol and Moskovitz52 showed that when VEP latency rather than ampli-
tude is used to estimate acuity, there is a signicant correlation between electrophysiologic and behavioral data, and Katsumi and coworkers29 reported a good correlation with preferential looking when spatial frequency sweep pattern visual evoked responses were used. Minor differences between the results of different testing methods notwithstanding, psychophysical and electrophysiologic research during recent years has established that visual acuity in infants develops much more rapidly than once thought, that an infants visual capacities are surprisingly rather well established shortly after birth, and that adult levels are reached at approximately 2 to 3 years of age. While the information provided by these tests cannot be accurate, it has been extremely useful for collecting information on the maturation of visual functions.9, 16, 56 Clinically, the tests may establish whether the responses from the two eyes differ. They are also useful for the follow-up of patients with bilateral reduction of visual acuity to chart progression of the condition.
Measurement of Visual Acuity in Preschool-Age Children
Reliable visual acuity measurements cannot be obtained until children are old enough to cooperate with tests that are based on recognition, such as illiterate Es in a linear arrangement. This usually occurs between the ages of 212 and 3 years. The child is given a cutout of an E and asked to match this E with isolated Es of varying sizes. The rst attempt is not always successful. One may then instruct the mother to teach the child the E game at home. The mother may be provided with two Es cut out of cardboard, one for the child to hold and another for the mother to show to the child. When the child is ready for it, a visual acuity chart consisting of Es oriented in various directions may be used. The advantage of
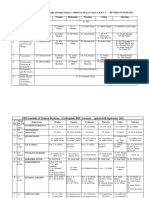
TABLE 111.
Estimated Visual Acuity at Different Ages
1 mo 6/120 6/120 6/120 2 mo 6/60 6/60 6/60 6 mo 6/30 6/30 6/6 6/12 Age at Which 6/6 Achieved 2030 mo 2436 mo 6 12 mo
Method Optokinetic nystagmus Preferential looking Visually evoked potentials
Modied from Dobson V, Teller D: Visual acuity in human infants. A review and comparison of behavioral and electro-physiological studies. Vision Res 18:1469, 1978.
Examination of the PatientI
163
presenting the Es in a linear arrangement on a test chart over isolated optotypes held before the child when screening for amblyopia is discussed in Chapter 14. Many children have no difculty in showing whether the E points up or down but become confused when the E points to the right or left. This has nothing to do with vision as such, but with difculties in orientation. If a child repeatedly has a perfect score with the Es pointing up or down, we tend to give less weight to the errors in pointing right or left. To a preschool child the E is meaningless, even if it is spoken of by the examiner as an animal with three legs. Sjogren has replaced the E with the isolated gure of a hand, and in some children this works better than Es. When the child is able to verbalize but not old enough to indicate directions reliably, visual acuity charts showing pictures rather than symbols, such as the illiterate E, may be used. Many such charts have been devised and one should be chosen that presents pictures of objects with which the child is likely to be familiar. We have found the Allen Preschool Vision Test, which presents pictures of objects familiar to most children in the Western Hemisphere in an isolated form, especially useful for this purpose (Fig. 113).
tems (charts, projection devices) used routinely in the examination of patients. Latent nystagmus that becomes manifest when one eye is covered (see Chapter 23) may cause reduced vision of the exposed eye. In such cases it becomes necessary to resort to blurring of one eye with plus lenses of sufcient power to reduce the vision but not strong enough to provoke a nystagmus. In school-age children and adults, vision should be tested also at near. This can be done with Snellen charts, reduced photographically for near vision distance, or by reading charts.
Refraction
An essential and hardly preliminary part of the examination is determination of the refractive error of a patient with neuromuscular anomalies of the eyes. One must always strive to obtain as complete and accurate an estimate of the refractive error as possible. Cycloplegic refraction should be carried out in every patient with strabismus, but procedures adopted by different ophthalmologists may vary. The statement has been made repeatedly that 1% cyclopentolate is less effective as a cycloplegic agent than 1% atropine sulfate in hypermetropic, esotropic, and normal children.27, 45, 54 Others believe that cyclopentolate applied in the examiners ofce one to three times at 5-minute intervals is sufcient to produce good cycloplegia.
Measurement of Visual Acuity in School-Age Children and Adults
When testing children of school age and adults, the ophthalmologist may employ any of the sys-
FIGURE 113. The Allen Preschool Vision Test. (Courtesy of Ophthalmix, La Grange, IL.)
164
Introduction to Neuromuscular Anomalies of the Eyes
In most patients we induce cycloplegia in the ofce. We use two instillations of 1% cyclopentolate for white patients and one drop of 5% homatropine hydrobromide for non-whites. Since 1% cyclopentolate may cause a transient increase in blood pressure in infants, we use a 0.5% solution for this age group and add a drop of 2.5% phenylephrine hydrochloride (Neo-Synephrine Hydrochloride) if mydriasis is unsatisfactory. We have found two simple tricks to be amazingly helpful in overcoming the unpleasantness associated with application of eye drops in children. The rst is to maintain the plastic bottle containing the medication at body temperature by carrying it in a shirt or coat pocket. The stinging sensation of the cycloplegic agent is less severe than when the drops are instilled at room temperature. Second, one drop applied to the back of the patients or mothers hand to show that the medicine does not burn will help to alleviate the childs apprehension. In non-white children under 3 years of age and in those in whom accommodation remains active despite repeated instillation of cyclopentolate and homatropine, we prescribe 1% atropine sulfate solution, one drop to be instilled in each eye morning and night for 3 days. On the fourth day, the day of the examination, one drop is to be given in each eye 1 hour before the appointment time. This dosage may be excessive in view of a recent study according to which the additional cycloplegic effect of 3-day atropinization vs. two single instillations followed by refraction 90 minutes later was only 0.5D.2 A printed instruction sheet is handed to the parents, which, in addition to the dosage, describes the signs of atropine toxicity and the warning to discontinue the drug if the child seems sensitive to it. By having the mother apply the drops at home, the physician is relieved of one aspect of the examination that is unpleasant to many children, who may become apprehensive or uncooperative on future ofce visits. To properly instill atropine solution at home the child should be recumbent. The drops are placed on the conjunctiva of the lower lid, which must be somewhat pulled away from the eye and held away from it for a few seconds to avoid the uid being squeezed out by the lids. The canaliculi should be compressed for 30 seconds to reduce absorption of the atropine through the nasal mucosa. The dropper must not be brought into contact with the conjunctiva, but also must not be
held too high lest there be some unpleasantness from the impact of the falling drop. Although one drop is prescribed, the mother is advised that she may use a second drop if the rst one lands mostly on the cheek. In spite of careful instruction, not all mothers are successful in applying the drops, which is why some ophthalmologists prefer the use of atropine sulfate in an ointment. This somewhat messy method has the disadvantage that the dosage is difcult to control, and the child may receive an unnecessarily large amount of atropine, which, after all, is a very potent alkaloid. Even the best and most complete cycloplegic refraction does not guarantee that one can successfully perform retinoscopy on a child. Some children are too restless or obstreperous and cannot be persuaded to cooperate. An assistant may immobilize them by holding or bundling them,41 but these procedures are crude and rather frightening to the child. We have found it helpful to ask the mother to withhold the feeding bottle from an infant until we are ready to start the examination. Most infants are oblivious to their surroundings while feeding, and this provides an excellent opportunity to perform retinoscopy and ophthalmoscopy on an otherwise uncooperative patient. After all, nothing is gained by letting the mother feed her child in the waiting room, so that by the time the physician is ready the infant is sound asleep and reacts with anger and irritation to all attempts to arouse it. A fundus examination is an integral part of the refractive procedure but, unfortunately, it is not always done or is not properly done. We have seen a number of children who had suffered weeks and months of useless occlusion of the better eye because it was thought that the fellow eye was amblyopic but in whom a fundus examination showed a dense macular scar or an atrophy of the optic nerve. In some patients, an examination and refraction under general anesthesia cannot be avoided. This method permits a thorough inspection of the fundus. In many such instances the size of the deviation and the type of strabismus are such that previous examinations had already indicated the need for an operation. In that case and when the refractive error is found to be insignicant the surgeon may then proceed with the operation as planned, thus saving the child another general anesthesia. On the other hand, if the refractive error is signicant, the surgeon should postpone surgery and prescribe glasses as a rst step.
Examination of the PatientI
165
FIGURE 114. Relationship between spherical equivalent of refractive error and age (solid line in upper part of graph), based on 35,570 refractions. (Data from Slataper FJ: Age norms of refraction and vision. Arch Ophthalmol 43:466, 1950.)
Changes of Refraction with Age
Refraction of neonates and changes of refraction with age need be mentioned only briey. The opinion, widely held in the past and also recently implied by some authors, that all neonates are hypermetropic and that those few with a congenital stable myopia have an error ranging from plano to 12.0D or more is erroneous. Cook and Glasscock,10 who performed retinoscopy on 1000 neonates, found 749 to be hypermetropic and 251 to be myopic. Mohindra and Held40 followed 400 patients from birth to 5 years of age, and their results showed newborns to be relatively myopic. As they grew older, the myopic spheric equivalent refraction declined and the infants became emmetropic at about 6 months of age and hypermetropic thereafter. This process of emmetropization is said to be delayed in the nonxating eye of strabismic children.33, 34 According to Abrahamson and coworkers1 a hypermetropic refractive error tends to increase with time in esotropia and remains stationary in exotropia. Another misconception is that the hypermetropia of neonates and infants decreases from birth. Brown7 has shown that hypermetropia tends to
increase up to about 7 years of age, at which time it begins to decrease. The data of Slataper,50 based on 38,570 refractions (see Fig. 114), clearly show this trend and Ingram and Bar26 reported similar ndings in 145 children between the ages of 1 and 312 years.
REFERENCES 1. Abrahamson M, Fabian G, Sjostrand J: Refraction changes in children developing convergent or divergent strabismus. Br J Ophthalmol 76:723, 1992. 2. Auffahrt G, Hunold W: Cycloplegic refraction in children: Single-dose atropinization versus three-day atropinization. Doc Ophthalmol 80:353, 1992. 3. Baker FH, Grigg P, Noorden GK von: Effect of visual deprivation and strabismus on the response of neurons in the visual cortex of the monkey, including studies on the striate and prestriate cortex in the normal animal. Brain Res 66:185, 1974. 4. Berlyne DE: The inuence of the albedo and complexity of stimuli on visual functions in the human infant. Br J Psychol 49:315, 1958. 5. Birch E, Shimojo S, Held R: Preferential-looking assessment of fusion and stereopsis in infants aged 16 months. Invest Ophthalmol Vis Sci 26:366, 1985. 6. Boothe RG, Dobson V, Teller DY: Postnatal development of vision in human and nonhuman primates. Annu Rev Neurosci 8:495, 1985. 7. Brown EV: Net average yearly change in refraction of atropinized eyes from birth to beyond middle age. Arch Ophthalmol 19:719, 1938.
166
Introduction to Neuromuscular Anomalies of the Eyes Use of optokinetic nystagmus to estimate visual development. Arch Ophthalmol 75:631, 1966. Kushner GJ, Lucchese NJ, Morton GV: Grating acuity with Teller cards compared to Snellen acuity in literate patients. Arch Ophthalmol 113:485, 1995. Leffertstra LJ: Vergleichende Untersuchungen auf unterschiedliche Refraktionsa nderungen beider Augen bei Patienten mit Strabismus convergens. Klin Monatsbl Augenheilkd 170:74, 1977. Lepard CW: Comparative changes in the error of refraction between xing and amblyopic eyes during growth and development. Am J Ophthalmol 80:485, 1975. Marg E, Freeman DN, Peltzman P, et al: Visual acuity development in human infants: Evoked potential measurements. Invest Ophthalmol 15:150, 1976. Mayer DL: Acuity of amblyopic children for small eld gratings and recognition stimuli. Invest Ophthalmol Vis Sci 27:1148, 1986. Mayer DL, Beiser AS, Warner AF, et al: Monocular acuity norms for the Teller Acuity Cards between ages one month and four years. Invest Ophthalmol Vis Sci 36:671, 1995. Mayer L, Fulton A, Rodier D: Grating and recognition acuities of pediatric patients. Ophthalmology 91:947, 1984. McDonald M, Dobson V, Sebris S, et al: The acuity card procedure: A rapid test of infant acuity. Invest Ophthalmol Vis Sci 26:1158, 1985. Mohindra I, Held R: Refractions in humans from birth to 5 years. Doc Ophthalmol 28:19, 1981. Morgan AL, Arstikaitis M: Examination of children. In Ophthalmologic Staff of the Hospital for Sick Children, Toronto, eds: The Eye in Childhood. St Louis, Mosby Year Book, 1967, p 17. Noorden GK von: Klinische Aspekte der Deprivationsamblyopie. Klin Monatsbl Augenheilkd 173:464, 1978. Noorden GK von, Crawford ML: The sensitive period. Trans Ophthalmol Soc U K 99:442, 1980. Parks MM, Wheeler MB: Concomitant esodeviation. In Duane TD, Jaeger EA, eds: Clinical Ophthalmology. Ocular Motility and Strabismus, vol 1. Philadelphia, JB Lippincott, 1988, p. 2. Rosenbaum AL, Bateman JB, Bremer DL, et al: Cycloplegic refraction in esotropic children: Cyclopentolate versus atropine. Ophthalmology 88:1031, 1981. Rydberg A: Assessment of visul acuity in adult patients with strabismic amblyopia. Acta Ophthalmolol Scand 75:611, 1997. Dobson V: Visual acuity testing in infants: from laboratory to clinic. In: Simons K, ed: Early Visual Development, Normal and Abnormal. New York, Oxford University Press, 1993, p 318. Siretanu R, Fronius M, Katz B: A perspective on psychophysical testing in children. Eye 4:794, 1990. Skoczenski AM, Norcia A: Development of VEP vernier acuity and grating acuity in human infants. Invest Ophthalmol Vis Sci 40:2411, 1999. Slataper FJ: Age norms of refraction and vision. Arch Ophthalmol 43:466, 1950. Sokol S: Measurement of infant visual acuity from pattern reversal evoked potentials. Vision Res 18:33, 1978. Sokol S, Moskowitz A: Comparison of pattern VEPs and preferential-looking behavior in 3-month-old infants. Invest Ophthalmol Vis Sci 26:359, 1985. Spierer A, Royzman Z, Chetrit A, et al: Vision screening of preverbal children with Teller Acuity Cards. Ophthalmology 849:106, 1999. Stolovitch C, Loewenstein A, Nehmet P, et al: The use of cyclopentolate versus atropine cycloplegia in esotropic Caucasian children. Binocular Vision Q 7:93, 1992. Teller DY: The forced choice preferential looking proce-
8. Campos EC: Amblyopia revisited: Evidence for the heterogeneity of the syndrome. Int Ophthalmol 13:327, 1989. 9. Campos EC, Chiesi C: Critical analysis of visual function evaluating techniques in newborn babies. Int Ophthalmol 8:25, 1985. 10. Cook RC, Glasscock RE: Refractive and ocular ndings in the newborn. Am J Ophthalmol 34:1407, 1951. 11. Dayton GO Jr, Jones MH, Ain P, et al: Developmental study of coordinated eye movements in man. I. Visual acuity in the newborn human: A study based on induced optokinetic nystagmus recorded by electro-oculography. Arch Ophthalmol 71:865, 1964. 12. Dobson V: Visual acuity testing in human infants: From laboratory to clinic. In Simons K, ed: Early Visual Development, Normal and Abnormal. New York, Oxford University Press, 1993, p 318. 13. Dobson V, Teller D: Visual acuity in human infants: A review and comparison of behavioral and electro-physiological studies. Vision Res 18:1469, 1978. 14. Dobson V, Teller D, Lee CP, et al: A behavioral method for efcient screening of visual acuity in young infants. I. Preliminary laboratory development. Invest Ophthalmol Vis Sci 17:1142, 1978. 15. Ellis GS, Hartmann EE, Love A, et al: Teller Acuity Cards versus clinical judgment in the diagnosis of amblyopia with strabismus. Ophthalmology 96:788, 1988. 16. Enoch JM, Campos EC: Helping the aphakic neonate to see. Int Ophthalmol 8:237, 1985. 17. Enoch JM, Rabinowicz IM: Early surgery and visual correction of an infant born with unilateral eye lens opacity. Doc Ophthalmol 41:371, 1976. 18. Fantz R: Pattern vision in young infants. Psychol Rec 8:43, 1958. 19. Fantz RL, Ordy JM, Udelf M: Maturation of pattern vision in infants during the rst six months. J Comp Physiol Psychol 55:907, 1962. 20. Friendly DS, Jaafar MS, Morillo DL: A comparative study of grating and recognition visual acuity testing in children with anisometropic amblyopia without strabismus. Am J Ophthalmol 110:293, 1990. 21. Fulton AB, Hansen RM, Mayer DL, et al: Clinical examination of infant visual status. In Simons K, ed: Early Visual Development, Normal and Abnormal. New York, Oxford University Press, 1993, p 309. 22. Gorman JJ, Cogar DG, Gellis SS: An apparatus for grading the visual acuity of infants on the basis of optokinetic nystagmus. Pediatrics 19:1088, 1957. 23. Gwiazda J, Brill S, Held R: New methods for testing infant vision. Sightsaving Rev 49:61, 1979. 24. Held R, Birch E, Gwiazda J: Stereoacuity in human infants. Proc Natl Acad Sci U S A 77:5572, 1980. 25. Hendrickson AE: Primate foveal development: A microcosmos of current questions in neurobiology. Invest Ophthalmol Vis Sci 35:3129, 1994. 26. Hubel DH, Wiesel TN: Binocular interaction in striate cortex of kittens reared with articial squint. J Neurophysiol 28:1041, 1965. 27. Ingram RM, Barr A: Refraction of 1-year-old children after cycloplegia with 1% cyclopentolate: Comparison with ndings after atropinization. Br J Ophthalmol 63:348, 1979. 28. Jacobson SG, Mohindra I, Held R: Visual acuity of infants with ocular diseases. Am J Ophthalmol 93:198, 1982. 29. Katsumi O, Denno S, Arai M, et al: Comparison of preferential looking acuity and pattern reversal evoked response acuity in pediatric patients. Graefes Arch Clin Exp Ophthalmol 235:684, 1997. 30. Katz B, Sireteanu R: The Teller Acuity Card Test: A useful method for the clinical routine? Clin Vis Sci 5:307, 1990. 31. Kiff AD, Lepard C: Visual responses in premature infants.
32. 33.
34. 35. 36. 37. 38. 39. 40. 41.
42. 43. 44.
45. 46. 47.
48. 49. 50. 51. 52. 53. 54. 55.
Examination of the PatientI dure. A psychophysical technique for use with human infants. Infant Behav Dev 2:135, 1979. 56. Teller DY: First glances: The vision of infants (Friedenwald Lecture). Invest Ophthalmol Vis Sci 38:2183, 1997. 57. Teller DY, Movshon JA: Visual development. Vision Res 26:1483, 1986. 58. Tomlinson E, Martinez D: The measurement of visual
167
acuity: Comparison of Teller Acuity Cards with Snellen and MBL results. Am Orthopics J 38:130, 1988. 59. Van Hof-van Duin J, Mohn G: Optokinetic and spontaneous nystagmus in children with neurological disorders. Behav Brain Res 10:163, 1983. 60. Wiesel TH, Hubel DH: Effects of visual deprivation on morphology and physiology of cells in the cats lateral geniculate body. J Neurophysiol 26:978, 1963.
Potrebbero piacerti anche
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Conflict ManagementDocumento4 pagineConflict ManagementSrimant DashNessuna valutazione finora
- Full BookDocumento152 pagineFull BookJezza WilsonNessuna valutazione finora
- UPSC Combined Mecical Services Examination 2012Documento7 pagineUPSC Combined Mecical Services Examination 2012TrcStaffNessuna valutazione finora
- Case 1 Hemiplegia With AphasiaDocumento8 pagineCase 1 Hemiplegia With Aphasialycan007Nessuna valutazione finora
- Femto Laser in OphthalmologyDocumento11 pagineFemto Laser in Ophthalmologylycan007Nessuna valutazione finora
- AIIMS May 2010Documento37 pagineAIIMS May 2010naveenmunNessuna valutazione finora
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- OVERVIEW Rapid Sequence Intubation (RSI) Is An Airway Management Technique That ProducesDocumento7 pagineOVERVIEW Rapid Sequence Intubation (RSI) Is An Airway Management Technique That ProducesOkami PNessuna valutazione finora
- Sanofi Aventis Vaccines Supply Chain ProcessDocumento21 pagineSanofi Aventis Vaccines Supply Chain ProcessarnaqviNessuna valutazione finora
- Schizencephaly A Review of 734 Cases PDFDocumento20 pagineSchizencephaly A Review of 734 Cases PDFDeglenNessuna valutazione finora
- AnophthalmiaDocumento6 pagineAnophthalmialeny zabidiNessuna valutazione finora
- Hospital MarketingDocumento39 pagineHospital Marketingdivyaky100% (1)
- Topics On Prosthetics & Orthotics - PDF CreDocumento4 pagineTopics On Prosthetics & Orthotics - PDF CreSuprit MahakudNessuna valutazione finora
- UHC Vision Plan SummaryDocumento2 pagineUHC Vision Plan SummaryJanet Zimmerman McNicholNessuna valutazione finora
- Low Cobalt Diet For Dyshidrotic Eczema PatientsDocumento5 pagineLow Cobalt Diet For Dyshidrotic Eczema PatientsMaulidianaIndahNessuna valutazione finora
- StuffDocumento4.804 pagineStuffSonder LegariNessuna valutazione finora
- Inhaled Anesthesia For BirdsDocumento18 pagineInhaled Anesthesia For BirdsBianca PaludetoNessuna valutazione finora
- Intro To Orthopedic Emergencies - RCSI Orthopaedic Emergencies - MK1Documento65 pagineIntro To Orthopedic Emergencies - RCSI Orthopaedic Emergencies - MK1kylieverNessuna valutazione finora
- TeratomaDocumento17 pagineTeratomaAndri Feisal NasutionNessuna valutazione finora
- NFDN 2005 Report On Progress PortfolioDocumento2 pagineNFDN 2005 Report On Progress Portfolioapi-329794748Nessuna valutazione finora
- Revised Schedule of BHU SSH OPD (Soft Copy) 2021Documento7 pagineRevised Schedule of BHU SSH OPD (Soft Copy) 2021rajubhagatssmNessuna valutazione finora
- Patient Queue Management SolutionDocumento34 paginePatient Queue Management Solutionmunish rattiNessuna valutazione finora
- GBD Lancet Paper 2 Dec 2012Documento27 pagineGBD Lancet Paper 2 Dec 2012lawrencehaddadNessuna valutazione finora
- DR - Prabhakar Patwardhan Samiti RugnalayaDocumento18 pagineDR - Prabhakar Patwardhan Samiti RugnalayaGajendra NikaleNessuna valutazione finora
- Rogers Textbook of Pediatric Intensive Care Fifth EditionDocumento61 pagineRogers Textbook of Pediatric Intensive Care Fifth Editiondanny.johnson566100% (40)
- Knowledge, Attitudes and Practices of The Medical Personnel Regarding Atopic Dermatitis in Yaoundé, CameroonDocumento7 pagineKnowledge, Attitudes and Practices of The Medical Personnel Regarding Atopic Dermatitis in Yaoundé, CameroonNadira Juanti PratiwiNessuna valutazione finora
- Nickel Titanium Rotary Instruments Making The Right Choice Jan 2012Documento6 pagineNickel Titanium Rotary Instruments Making The Right Choice Jan 2012Muchlis fauziNessuna valutazione finora
- MEMORANDUM OF AGREEMENT (Dentist)Documento2 pagineMEMORANDUM OF AGREEMENT (Dentist)thirdyjaoNessuna valutazione finora
- Introduction To Healthcare Quality Management-Examples From Hospitals in TaiwanDocumento4 pagineIntroduction To Healthcare Quality Management-Examples From Hospitals in TaiwanNai-Wen KuoNessuna valutazione finora
- Accident Investigation ProtocolsDocumento14 pagineAccident Investigation ProtocolsgilbertwildNessuna valutazione finora
- PRC Forms Bicol University COllege of Nursing, Legazpi CityDocumento5 paginePRC Forms Bicol University COllege of Nursing, Legazpi CityekagaliasNessuna valutazione finora
- Madhya Pradesh Ayurvigyan Parishad Adhiniyam 1987Documento12 pagineMadhya Pradesh Ayurvigyan Parishad Adhiniyam 1987Latest Laws TeamNessuna valutazione finora
- A ENT Fellowship For An Internation Resident - (Archive) - Student Doctor Network ForumsDocumento5 pagineA ENT Fellowship For An Internation Resident - (Archive) - Student Doctor Network ForumsAbhishek Kumar RamadhinNessuna valutazione finora
- Charateristics of NewbornDocumento3 pagineCharateristics of NewbornRagupathyRamanjuluNessuna valutazione finora
- Renal Calyceal MicrolithiasisDocumento3 pagineRenal Calyceal MicrolithiasisVic L. AmecaNessuna valutazione finora
- Cerebral PalsyDocumento31 pagineCerebral PalsyYunita Amilia0% (1)
- Gastrointestinal Bleeding in Infants and Children AAPDocumento16 pagineGastrointestinal Bleeding in Infants and Children AAPDina MarselinaNessuna valutazione finora