Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Emergency Drugs: Vasoppressors - Recommended by AHA
Caricato da
Jaffy EspirituDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Emergency Drugs: Vasoppressors - Recommended by AHA
Caricato da
Jaffy EspirituCopyright:
Formati disponibili
Emergency Drug Therapy Objectives: At the end of the lesson the student nurses will have increased their
knowledge of emergency drugs and their use and will be able will be able to
Identify emergency cardiovascular drugs and their use based on evaluated evidence from the 2005
International Consensus Conference of Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations.
Indicate appropriate drug interventions in cardiopulmonary arrest situations based on current
guidelines.
Relate expected patient outcomes to individual emergency drugs.
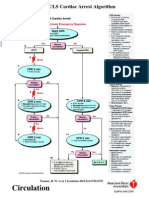
During a code: drug therapy is not your first priority. Your first priority is Airway, Breathing, Circulation, Defibrillation, and determining a Differential Diagnosis. ABCD, reminds us what to do in an emergency situation. It is essential that first responders to a code perform high-quality CPR. Good quality CPR skills are essential to all ACLS interventions. Drugs, when required, play an important role in management of an arrest situation. Drug administration should not interrupt CPR. Instead, drugs should be delivered during CPR if at all possible. Drug therapy should be implemented after the ABCD survey, and after accurately assessing the cardiac rhythm. In the event emergency cardiac drug therapy is necessary, nurses will probably encounter one or more of the drugs discussed below during a code.
Emergency Drugs
vasoconstrictors - first drug given in a pulseless rhythm. Pulseless arrests : ventricular fibrillation ventricular tachycardia pulseless electrical activity (PEA) asystole. TYPES OF VASOCONSTRICTORS Vasoppressors recommended by AHA epinephrine ---o a catecholamine that increases blood flow to the heart and brain increases heart rate and blood pressure makes the heart more responsive to defibrillation. o usual dose of epinephrine is 1 mg IV push (IVP) ---with repeated doses every three to five minutes according to patient response. Each IV dose is followed by 20 mL normal saline (NS) flush. Epinephrine is supplied on crash carts in prefilled 10 mL syringes (10 mL = 1 mg, if a 1:10,000 dilution is used).
AHA guidelines recommend a continuous infusion of epinephrine (2 mcg/min to 10 mcg/min) in symptomatic bradycardia or hypotension after atropine has been given, and while awaiting transcutaneous pacing, or if the use of a transcutaneous pacemaker has failed. vasopressin
Vasopressin--- is an alternate vasopressor has a longer half-life than epinephrine. It is a powerful vasoconstrictor, producing the same effect as epinephrine, and can be used as an alternative to epinephrine for any pulseless cardiac arrest, Vasopressin is a hormone that promotes reabsorption of water in the kidneys and causes peripheral vasoconstriction. If a pulseless rhythm persists after delivery of 1 or 2 shocks plus high-quality CPR, one dose of vasopressin may be given before or after epinephrine. When a shock is not advised, vasopressin may also be given to replace the first or second dose of epinephrine. The dose of vasopressin is 40 units and is administered IVP. Vasopressin is usually supplied in crash carts as a 20 unit vial. You will need 2 vials to equal 40 units. Because vasopressin is a potent peripheral vasoconstrictor and may provoke or worsen cardiac ischemia, it is not recommended for use in responsive patients who have coronary artery disease. Atropine is a drug that has a direct vagolytic effect, increases the heart rate due to a parasympathetic action accelerating the rate of the sinus node discharge and improving AV conduction. used to treat patients with symptomatic sinus bradycardia and symptomatic AV heart blocks. not recommended for second-degree AV heart block Mobitz Type II or third-degree AV block with wide QRS complexes. Immediate pacing is recommended for these patients. Atropine is the drug of choice (after epinephrine or vasopressin) for asystole and PEA. It is only given to patients in PEA who have an absolute bradycardia (heart rates less than 60), after epinephrine or vasopressin has failed. For asystole or PEA, atropine is given as a bolus injection into a large peripheral vein. Dose of atropine is 1 mg IVP every three to five minutes up to a maximum of 3 doses or 3 mg. In symptomatic bradycardia, the dose is 0.5 mg to 1 mg IVP, repeated every three to five minutes as needed to a total dose of 3 mg or 0.04 mg/kg. Each dose should be followed by 20 mL NS IV flush. Atropine is most commonly supplied in prefilled syringes with 1 mg in 10 mL. When administering atropine, remember the following points. First, your patients pupils will become dilated; therefore, pupil checks have no clinical significance. Second, atropine will increase the oxygen requirement of the heart, and may actually worsen ischemia or increase an area of infarct in an acute MI. Be sure to watch carefully for acute ECG changes of ischemia or injury. Atropine causes tachycardia, which also increases oxygen requirements of the heart and may lead to further ischemia or injury. Therefore, atropine should be used with caution in patients who have CHF, angina, or other cardiac issues where tachycardia could be harmful. Third, atropine is contraindicated in patients who have received heart transplants because the
transplanted heart lacks vagal innervation making atropine ineffective. Finally, watch for side effects of arrhythmias: delirium, flushed skin, ataxia, blurred vision, and coma. Amiodarone - used in the treatment of life-threatening arrhythmias. The AHA recommends amiodarone - first-line antiarrythmic for patients who experience cardiac arrest. Amiodarone is a potent vasodilator, prolongs the action potential duration and the refractory period in the cardiac cycle, thereby decreasing the AV node conduction and heart rate, and slowing SA nodal conduction. indicated for shock-refractory ventricular fibrillation and pulseless ventricular tachycardia used to treat wide-complex tachycardias and is used as an adjunct in electrical cardioversion of paroxysmal supraventricular tachycardia (PSVT). successfully used for rate control in atrial fibrillation or atrial flutter and can be used in the management of stable tachycardia. The recommended dose of amiodarone for ventricular fibrillation and pulseless ventricular tachycardia is 300 mg IVP. Amiodarone is supplied in glass vials, therefore a filter needle is used to draw it up. If there is no response to amiodarone in three to five minutes, consider a second dose of 150 mg IVP. Maximum cumulative dose of amiodarone is 2.2 g IV in 24 hours. The usual dose of amiodarone for stable wide-complex tachycardia is 150 mg IV over ten minutes. Additional infusions of 150 mg may be given every ten minutes as needed up to the maximum of 2.2 g in 24 hours. Follow a successful bolus of amiodarone with a maintenance infusion of 540 mg at a rate of 1 mg/min for 6 hours and then 0.5 mg/min for 18 hours. An in-line filter should be used during administration of amiodarone. Be aware that amiodarone may produce vasodilatation and hypotension, and may prolong the QT interval. Do not routinely administer amiodarone with procainamide or other drugs that prolong the QT interval, as doing so may lead to lethal arrhythmias. Use Amiodarone with caution in patients with renal failure. Amiodarones half-life is up to 40 days. Lidocaine is no longer given for ventricular fibrillation or pulseless ventricular tachycardia until after defibrillation, epinephrine, or vasopressin, and if amiodarone is not available. Lidocaine suppresses automaticity and excitability of the HIS-Purkinje system during diastole. Through critical appraisal and expert discussion, lidocaine has now been classified as an indeterminate ACLS recommendation. It does no harm and has no benefit. The dose of lidocaine for ventricular fibrillation is 1 mg/kg to 1.5 mg/kg IVP, and may be repeated every three to five minutes to a maximum of 3 mg/kg. The dose for ventricular tachycardia is 1 mg/kg to 1.5 mg/kg IVP with doses of 0.5 mg/kg to 0.75 mg/kg repeated every five to ten minutes up to a maximum dose of 3 mg/kg. Following a successful lidocaine bolus, run a continuous IV infusion (2 Gm in 500 mL D5W) at 2 mg/min to 4 mg/min. Prophylactic lidocaine is not recommended. Administer lidocaine with caution in patients with conduction disturbances, avoiding it completely for patients in third-degree heart block who have ventricular escape beats. Large doses of lidocaine may depress the sinus node and produce heart block. Lidocaine may be used for bradycardia in patients with ventricular escape beats if an external pacemaker in standby mode is on the patient, in case they
become asystolic or develop symptomatic bradycardia. Also, you might want to reduce the dosage for those who have impaired hepatic function, pulmonary edema, or shock, and for patients over the age of 70. Be alert for signs and symptoms of toxicity, which may include drowsiness, disorientation, tinnitus, paresthesias, and seizures. If toxicity is suspected, stop the drip, hang a NS IV, and promptly notify the physician. Adenosine is an antiarrythmic drug that works by slow initiation of SA node impulses and blocking AV conduction reentry. This drug is especially effective on re-entry tachycardia such as PSVT. Adenosine is the drug of choice for most narrow-complex tachycardias. It will not convert atrial fibrillation or atrial flutter, but may be used as a diagnostic aid in determining the underlying rhythm because it produces a transient AV block that assists in clarifying the underlying rhythm. Adenosine is preferred over verapamil because of its transient effects, and because it does not produce hypotension. Adenosine is not used for wide-complex tachycardias of uncertain origin. ACLS guidelines recommend cardioversion for unstable wide-complex tachycardia of unknown type. Patients receiving adenosine should always be on a cardiac monitor. The usual dose of adenosine is 6 mg given rapidly, (over 1-3 seconds) IVP in a large vein such as the antecubetal, to enhance delivery to the heart. This is followed by 20 mL NS IV flush with elevation of the arm with the IV access. The second dose is 12 mg given one to two minutes later if there is no response to the first dose. The 12 mg dose may be repeated one more time after one to two minutes, if needed. The maximum dose is 30 mg. An important fact to keep in mind regarding adenosine is that it has an extremely short half-life (<10 seconds) and must be administered rapidly (one to three seconds) through the IV port that is closest to the systemic circulation. The onset of action of adenosine is usually 10-15 seconds. A stopcock setup with a NS filled syringe attached to one port and adenosine attached to another port assists in rapid administration necessary to get into the blood system quickly. Because adenosine slows AV conduction, it is contraindicated in patients with second- or third-degree AV blocks who do not have artificial pacemakers. In addition, adenosine is contraindicated in patients taking theophylline derivatives, carbamazepine (Tegretol), or dipyridamole (Persantine), and pentaxphylline (Trentol), because they may interfere with the drugs action. When administering adenosine, you must observe the cardiac monitor closely for brief periods of asystole, sinus bradycardia, or ventricular ectopy. Your patient may also experience flushing, bronchospasms, and dyspnea. These symptoms are usually short-lived and generally disappear within a minute. Emergency equipment should be immediately available in case resuscitation becomes necessary.
Potrebbero piacerti anche
- Emergency Drug Therapy 1ceuDocumento7 pagineEmergency Drug Therapy 1ceuRN333Nessuna valutazione finora
- ACLS DrugDocumento7 pagineACLS DrugPhongsatorn Thunin100% (1)
- Acls DrugsDocumento10 pagineAcls DrugsChintami Octavia100% (1)
- Management of Symptomatic Bradycardia and TachycardiaDocumento55 pagineManagement of Symptomatic Bradycardia and TachycardiaDewintha Airene NoviantiNessuna valutazione finora
- Advanced Cardiac Life Support Information From American Heart Association, Advanced Cardiac Life Support, 2006Documento25 pagineAdvanced Cardiac Life Support Information From American Heart Association, Advanced Cardiac Life Support, 2006karento1Nessuna valutazione finora
- Drugs Given During Cardiac Arres For CPRDocumento5 pagineDrugs Given During Cardiac Arres For CPREevyaj MimiNessuna valutazione finora
- Drug Study CARDIODocumento17 pagineDrug Study CARDIODiannetotz Morales100% (1)
- Drugs in CPR - M.H.farjooDocumento37 pagineDrugs in CPR - M.H.farjooAnonymous 34umhBmBENessuna valutazione finora
- Acls Drug OverviewDocumento2 pagineAcls Drug OverviewShannon Davis100% (1)
- Acls Drug OverviewDocumento2 pagineAcls Drug OverviewBruce Abramowitz100% (1)
- NCM 118B Emergency MedicationsDocumento110 pagineNCM 118B Emergency MedicationsJan Crizza Dale R. FrancoNessuna valutazione finora
- ACLS DrugsDocumento16 pagineACLS Drugstostc100% (2)
- ACLS Class Packet PDFDocumento9 pagineACLS Class Packet PDFImam GultomNessuna valutazione finora
- Advanced Cardiovascular Life Support in Adults (ACLS) : SubtitleDocumento30 pagineAdvanced Cardiovascular Life Support in Adults (ACLS) : SubtitleMohamad El SharNessuna valutazione finora
- ACLS PharmacologyDocumento5 pagineACLS PharmacologyKim Still ChunnNessuna valutazione finora
- SVTDocumento8 pagineSVTJulieNessuna valutazione finora
- Chest Pain, Bradycardia, & Cardiac Dysrhythmias.: Oxygen As An Emergency DrugDocumento11 pagineChest Pain, Bradycardia, & Cardiac Dysrhythmias.: Oxygen As An Emergency DrugMin Hong LuoNessuna valutazione finora
- Cardiorespiratory ArrestDocumento51 pagineCardiorespiratory ArrestIrham KhairiNessuna valutazione finora
- Ecart For PrintingDocumento10 pagineEcart For PrintingbluennaNessuna valutazione finora
- Unit 5 Cardiac Emergencies: StructureDocumento27 pagineUnit 5 Cardiac Emergencies: StructurebtaleraNessuna valutazione finora
- Handbook of AnesthesiologyDocumento176 pagineHandbook of AnesthesiologyarmelzahfauziNessuna valutazione finora
- 099 B SaroshDocumento14 pagine099 B SaroshUmair AnsariNessuna valutazione finora
- 15 - CCLS - PharmacologyDocumento32 pagine15 - CCLS - PharmacologyVENKATESH RAMSALINessuna valutazione finora
- Acls STUDY GUIDE 2017Documento19 pagineAcls STUDY GUIDE 2017jamesomooreNessuna valutazione finora
- ACLS PharmacologyDocumento6 pagineACLS PharmacologyEunice Angela Fulgueras80% (5)
- FarmakologiDocumento69 pagineFarmakologikekeyirawanNessuna valutazione finora
- 15 - CCLS - PharmacologyDocumento32 pagine15 - CCLS - PharmacologyVENKATESH RAMSALINessuna valutazione finora
- 10 Emergency DrugsDocumento4 pagine10 Emergency DrugsmusicwizardNessuna valutazione finora
- Current Clinical Strategies: Handbook of AnesthesiologyDocumento180 pagineCurrent Clinical Strategies: Handbook of AnesthesiologydramaganaNessuna valutazione finora
- Nhip Tim NhanhDocumento3 pagineNhip Tim NhanhHiếu KiềuNessuna valutazione finora
- Protocol of Management of Acute Heart FailureDocumento5 pagineProtocol of Management of Acute Heart FailureMc inloveNessuna valutazione finora
- Adult and Pediatric Emergency DrugsDocumento61 pagineAdult and Pediatric Emergency DrugsYu, Denise Kyla BernadetteNessuna valutazione finora
- Adenosine 3mg-ml (Adenocor Solution For Injection I.V)Documento2 pagineAdenosine 3mg-ml (Adenocor Solution For Injection I.V)ddandan_2Nessuna valutazione finora
- Lecture - 2 Advanced Cardiac Life SupportDocumento28 pagineLecture - 2 Advanced Cardiac Life SupportJixon GeorgeNessuna valutazione finora
- Essential Facts For Med-Surg Nurses: Emergency Cardiac DrugsDocumento7 pagineEssential Facts For Med-Surg Nurses: Emergency Cardiac DrugssanthyakunjumonNessuna valutazione finora
- ACLS PrecourseAssessmentDocumento19 pagineACLS PrecourseAssessmentBrigitte Elaine81% (21)
- Life Threatening Arrhythmia and ManagementDocumento40 pagineLife Threatening Arrhythmia and ManagementRuki HartawanNessuna valutazione finora
- A Drug Study On EpinephrineDocumento7 pagineA Drug Study On EpinephrineMaesy Garcia LorenaNessuna valutazione finora
- Seminar NoteDocumento2 pagineSeminar NoteCHANDREN ARUMUGAMNessuna valutazione finora
- Hypertensive Emergencies: BY: Dr. Imtiyaz Hashim (PGR) Dr. Khalida Baloch (Ho)Documento31 pagineHypertensive Emergencies: BY: Dr. Imtiyaz Hashim (PGR) Dr. Khalida Baloch (Ho)امتیاز ہاشم بزنجوNessuna valutazione finora
- ACPDocumento3 pagineACPAbby PrimeauNessuna valutazione finora
- E Cart MedicationsDocumento12 pagineE Cart Medicationsbalong1219Nessuna valutazione finora
- Emergency Drugs For Neurosurgical DisordersDocumento12 pagineEmergency Drugs For Neurosurgical DisordersAnnie CantimbuhanNessuna valutazione finora
- Obat-Obatan Dalam Bantuan Hidup LanjutDocumento16 pagineObat-Obatan Dalam Bantuan Hidup LanjutTheresia SihotangNessuna valutazione finora
- Algoritma Bradi Dan TakikardiDocumento7 pagineAlgoritma Bradi Dan TakikardiTetha Deliana PutriNessuna valutazione finora
- Ca ChannelDocumento30 pagineCa ChannelKency DoneyNessuna valutazione finora
- Crash Cart Medication and ManagementDocumento20 pagineCrash Cart Medication and ManagementSilpa Kuruvilla100% (2)
- Guideline 11 9 Managing Acute Dysrhythmias 307Documento10 pagineGuideline 11 9 Managing Acute Dysrhythmias 307gregraynerNessuna valutazione finora
- Pacemaker Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDa EverandPacemaker Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNessuna valutazione finora
- Immediate Life Support for healthcare Practitioners: A Step-By-Step GuideDa EverandImmediate Life Support for healthcare Practitioners: A Step-By-Step GuideNessuna valutazione finora
- Atrial Fibrillation A Simple Guide to The Condition, Treatment And Related DiseasesDa EverandAtrial Fibrillation A Simple Guide to The Condition, Treatment And Related DiseasesValutazione: 4 su 5 stelle4/5 (1)
- Cardioversion, A Simple Guide To The Condition, Types, Treatment of Arrhythmias And Related ConditionsDa EverandCardioversion, A Simple Guide To The Condition, Types, Treatment of Arrhythmias And Related ConditionsNessuna valutazione finora
- The Spectrum of Amniotic Fluid Embolism: Is Intralipid the solution ?Da EverandThe Spectrum of Amniotic Fluid Embolism: Is Intralipid the solution ?Nessuna valutazione finora
- Mitral Valve Regurgitation, A Simple Guide To The Condition, Treatment And Related ConditionsDa EverandMitral Valve Regurgitation, A Simple Guide To The Condition, Treatment And Related ConditionsNessuna valutazione finora
- Classified AdsDocumento3 pagineClassified Adsapi-312735990Nessuna valutazione finora
- Case Study PneumoniaDocumento13 pagineCase Study Pneumonialavparedes93% (44)
- Pathophysiology of Acute GastroenteritisDocumento5 paginePathophysiology of Acute Gastroenteritisheron_bayanin_15Nessuna valutazione finora
- As en 556.1-2002 Sterilization of Medical Devices - Requirements For Medical Devices To Be Designated STERILEDocumento8 pagineAs en 556.1-2002 Sterilization of Medical Devices - Requirements For Medical Devices To Be Designated STERILESAI Global - APACNessuna valutazione finora
- Burton's Microbiology For The Health Sciences: Chapter 18. Viral InfectionsDocumento20 pagineBurton's Microbiology For The Health Sciences: Chapter 18. Viral Infectionsmirai desu100% (2)
- Clinical Approach To Optic Neuropathies: DiagnosisDocumento14 pagineClinical Approach To Optic Neuropathies: Diagnosiskmathewjames100% (1)
- Cirrhosis and Its Complications Evidence Based TreatmentDocumento20 pagineCirrhosis and Its Complications Evidence Based TreatmentSucii Sekar NingrumNessuna valutazione finora
- Case HistoryDocumento3 pagineCase Historypriyanka sNessuna valutazione finora
- Thesis Topics in Pediatrics in RguhsDocumento8 pagineThesis Topics in Pediatrics in Rguhssarahgriffinbatonrouge100% (2)
- De Thi ThuDocumento6 pagineDe Thi ThuQuynh TrangNessuna valutazione finora
- 24 Oet Full TestsDocumento212 pagine24 Oet Full TestsJoe Single86% (7)
- Chapter 12 - Hypertension - Pass The Salt, Please Level IIDocumento7 pagineChapter 12 - Hypertension - Pass The Salt, Please Level IIRichix K Yabe0% (1)
- Republic Act No. 11223 or The Universal Health Care ActDocumento2 pagineRepublic Act No. 11223 or The Universal Health Care ActChristine Joy MolinaNessuna valutazione finora
- FASENRA - PFS To Pen Communication Downloadable PDFDocumento2 pagineFASENRA - PFS To Pen Communication Downloadable PDFBrîndușa PetruțescuNessuna valutazione finora
- Attention-Deficit/Hyperactivity Disorder (ADHD)Documento4 pagineAttention-Deficit/Hyperactivity Disorder (ADHD)Sharyn Joy AgtasNessuna valutazione finora
- Gulf Care Members GuideDocumento31 pagineGulf Care Members Guidesuheil samaraNessuna valutazione finora
- WTD-0910-006 - MTI Booklet FINAL (Web-Email v2)Documento20 pagineWTD-0910-006 - MTI Booklet FINAL (Web-Email v2)Sumit BatraNessuna valutazione finora
- Company Profile-Yichang HumanwellDocumento42 pagineCompany Profile-Yichang HumanwellKino GaoNessuna valutazione finora
- Graded Midterm - Benedictine University EpidemiologyDocumento6 pagineGraded Midterm - Benedictine University EpidemiologyJoshMatthewsNessuna valutazione finora
- OBM752 HM Unit-IV NotesDocumento34 pagineOBM752 HM Unit-IV NotesRajanNessuna valutazione finora
- Gaucher DiseaseDocumento27 pagineGaucher DiseaseWahida PutriNessuna valutazione finora
- Caz Clinic PDFDocumento160 pagineCaz Clinic PDFDr.Md.AslamNessuna valutazione finora
- Family PlanningDocumento16 pagineFamily PlanningAnas Abdul SalamNessuna valutazione finora
- Paget's Disease: EtiologyDocumento8 paginePaget's Disease: EtiologyMURALINessuna valutazione finora
- ConjuntivitisDocumento21 pagineConjuntivitisjoal510Nessuna valutazione finora
- The Clear Skin Diet by Nina Nelson PDFDocumento370 pagineThe Clear Skin Diet by Nina Nelson PDFmia agustina60% (10)
- Resume PortfolioDocumento1 paginaResume Portfolioapi-491272428Nessuna valutazione finora
- FilariasisDocumento9 pagineFilariasisRizzy UgayNessuna valutazione finora
- Coxsackievirus: Presented By: LKCDocumento18 pagineCoxsackievirus: Presented By: LKCLeang KarichakNessuna valutazione finora
- STG Final Dec 2020Documento1.215 pagineSTG Final Dec 2020Bereket GGNessuna valutazione finora