Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Sanjivani Anesthesia Record
Caricato da
Advait KarmarkarDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Sanjivani Anesthesia Record
Caricato da
Advait KarmarkarCopyright:
Formati disponibili
ANESTHESIA RECORD
Date OR # Page of
Procedure(s) Surgeon(s)
START
STOP
Anesthesia Procedure
Room Time IN: OUT:
PRE-PROCEDURE
MONITORS AND EQUIPMENT
ANESTHETIC TECHNIQUE
AIRWAY MANAGEMENT
Magill forceps Oral ETT RAE L.T.A. Nasal ETT LMA # Stylet LMA Fastrach # DL LMA ProSeal # Tube size: FOI Awake Blade: Laser ETT LIS Attempts x EMG ETT Bougie Grade: I II III IV blind Armored ETT TTJV Atraumatic intubation/LMA DLT Secured at _________ cm Bronchial blocker system ET C02 present Breath sounds = bilateral Rigid FO laryngoscope Cuffed - min occ pressure Uncuffed ETT - leaks at Nerve blocks / Topical / ____________ cm H20 Nebulizer - See Remarks Oral airway Nasal airway Bite block Cannot Easy Head-tilt Max jaw-thrust Mask vent: Ventilate Circuit: Circle system NRB Bain Mask case Via tracheotomy / stoma Simple 02 mask Nasal cannula
Pre-02 GA Induction: Pt Identified: ID Band Questioned Guardian Steth: Esophageal Precordial Suprasternal Intravenous RSI Chart reviewed Permit signed Non-Invasive B/P V lead ECG Cricoid pressure Inhalation IM PR GA Maintenance: NPO since ____________ Full stomach Continuous ECG ST / Dysrhy. analysis Inhalation Inhalation / IV Patient reassessed prior to anesthesia & Pulse oximeter Nerve stimulator: GA / Regional combination TIVA End tidal C02 surgery; surgical site verified - Ready to proceed Ulnar Tibial Sedation & Analgesia / Monitored Anesthesia Care Peri-operative pain management discussed Regional: Oxygen monitor Facial Epidural Thoracic Lumbar Caudal with patient / guardian, plan of care completed ET agent analyzer Fluid / Blood warmer SAB Ankle Femoral Axillary Interscalene Pre-Anesthetic state: Temp:______________ Cell Saver BIS CSE Bier Continuous Spinal Cervical Plexus Awake Anxious Uncooperative Body warmer TEE ICP Other: Regional Technique: Calm Lethargic Unresponsive Airway humidifier: CPB EEG Position ___________________ Evoked potential: See remarks Prep PATIENT SAFETY Anesthesia machine # ____________ checked NG / OG tube Local Site Introducer Critical clinical alarms checked & activated Foley: OR Ward Doppler: Needle Secured with safety belt Axillary roll Arterial line LA Arm(s) secured on armboards: L R C-line/CVP Narcotic Arm(s) tucked: L R Arms < 90 PA line Additive Pressure points checked, padded, monitored IV(s) Test dose Rx Eye Care: Taped closed Ointment Attempts x Level By surgeon Saline Goggles Catheter: Test dose response: Prone - no pressure on orbits/nose/ears/genitals L.O.R. _______ cm Skin _______ cm Secured Remarks: POST ANESTHESIA CARE NOTES Location Time Awake Somnolent POST ANAESTHESIA INSTRUCTIONS: 02 Sat B/P Unarousable % Stable 1. Nil orally till Pulse Resp Temp Unstable Supplimental 2. T,P,R,BP 1/2 hourly. Pain care plan discussed with RN Oxygen Regional - dermatome level: OPA / NPA 3.Watch for effects of anaesthesia Continuous epidural analgesia LMA Recovery recorded on anes. form Intubated 4. IV fluids: Direct admit to hospital ward, Aldrete score _________ No intra-operative anesthesia adverse events noted 5. Analgesia For >24 hour admits:
Heme LOR CSF
Pares
+ + + -
A S
No adverse anesthesia related complications noted, satisfactory progress and recovery See progress notes for anesthesia related concerns
Des N20 Oxygen AGENTS
Iso Air
Sev
TIME: Hal (ET%) (L/min) (L/min) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( )
TOTALS
FLUIDS Urine EBL Gastric ECG % Oxygen Inspired (Fi02) 02 Saturation (Sa02) End Tidal C02 Temp: C F
OUTPUT
(ml) (ml) (ml) SYMBOLS
MONITORS
B/P CUFF PRESSURE
ARTERIAL LINE
PERI-OP MEDS
TIME
X
200 180 160
150 150 180 180
MEAN ARTERIAL PRESSURE
PULSE
VENTILATION
140 120 100 80
Pre-procedure Vital Signs
100 120 120
O / SV
SPONTANEOUS
/ AV
100 100 100
ASSISTED
80
80
/ CV
CONTROLLED TOURNIQUET
Pulse
Resp
60
50 50
40
LOCATION:
BP
Temp Sa02 Tidal Volume (ml) Respiratory Rate Peak Pressure PEEP CPAP
20
mmHg:
UP:
VENT
(cm H20) (cm H20)
DOWN:
Symbols for Remarks Position
TOTAL TIME:
History from:
Patient Parent / Guardian Significant Other
Chart Poor Historian Language Barrier
PRE-ANESTHESIA EVALUATION
AGE SEX
See previous anesthesia record dated _________________ for information
HEIGHT WEIGHT
PROPOSED PROCEDURE
M
PREVIOUS ANESTHESIA / OPERATIONS NONE CURRENT MEDICATION(S) NONE
F
in / cm lb / kg
Hx Illicit drug use
Hx Herbal / OTC drug use
MP1 MP2 MP3 MP4
WNL
T-M distance = M-O distance = Neck FULL LIMITED NONE ROM
Morbid obesity Hx difficult airway Teeth poor repair Teeth Chipped / Loose:
AIRWAY
Edentulous Facial hair Short muscular neck
ALLERGIES
NONE
SYSTEM
RESPIRATORY
Chronic tonsillitis Chronic OM Recent URI TB / +PPD Pneumonia Productive cough SOB / Dyspnea OSA Orthopnea Wheezing Abnormal ECG Dysrhythmia Hypovolemia Chronic fatigue Pacemaker / AICD Murmur Valvular Dz / MVP Hx Rheumatic fever Endocarditis Aneurysm N&V Diarrhea IBS / Chrohn's Dz Pancreatitis Gallbladder Dz Diverticulum Colon polyps Muscle weakness Neuromuscular Dz Paralysis Paresthesia(s) CVA / TIA Seizures / Epilepsy Psychiatric disorder Prostate BPH / CA UTI / Incontinence Diabetes mellitus: Type I / II / Gest. Pituitary disorder Asthma / RAD Bronchiolitis COPD Emphysema Bronchitis Respiratory failure Pleural effusion Pulmonary embolism Sinusitis / Rhinitis Environ. allergies
COMMENTS
TOBACCO USE: No Yes _______ Packs / Day for ______ Years Quit
DIAGNOSTIC STUDIES
ECG:
Pre-procedure Pulmonary Physical Exam:
WNL
CARDIOVASCULAR
Hypertension Hyperlipoproteinemia CAD / Cardiomyopathy Angina Stable / Unstable Myocardial infarction CHF DOE PND Peripheral Vascular Dz Exercise Tolerance METs: > 4 <4
Pre-procedure Cardiac Physical Exam:
ETHANOL USE: No Yes Frequency ________________ Hx ETOH abuse Quit
LABORATORY STUDIES
WNL
HEPATO / GASTROINTESTINAL
Obesity Cirrhosis / Liver Dz Hepatitis / Jaundice Bowel obstruction Ulcers Hiatal hernia GERD
T&S / T&C:
WNL
NEURO / MUSCULOSKELETAL
Arthritis / DJD / DDD OA / RA / Gout Back Problems (LBP) Scoliosis / Kyphosis Headaches / Migraine ICP / Head injury LOC / Unconscious
HCG: LMP:
Location
U/A:
WNL
RENAL / ENDOCRINE
Thyroid disease Bladder Dz / tumor Renal stones Renal insufficiency Renal Failure / Dialysis Adrenocortical insuff.
WNL
OTHER
Immunosuppressed Sickle Cell Dz / Trait Recent steroids Cushingoid Sepsis / Infection Transfusion Hx Weight loss / gain Hearing loss Peripheral edema Multiple gest VBAC IUGR
Anemia Bleeding disorder Cancer Chemotherapy Radiation Tx Nonambulatory Eye Dz / Glaucoma HIV / AIDS G6PD Deficiency
FAMILIAL ANES PROBLEMS:
No
Yes
Description _________________________
WNL
TIUP Pre-eclampsia HELLP
PREGNANCY
SGA LGA PROM
AROM
Mg DRIP:
__________gm/hr SROM PITOCIN DRIP G: P: INDUCTION
WEEKS GEST: EDC: 1
PHYSICAL STATUS
POST ANESTHESIA CARE NOTES Awake Time Somnolent 02 Sat B/P Unarousable % Stable Pulse Resp Temp Unstable Supplimental Pain care plan discussed with RN Oxygen Regional - dermatome level: OPA / NPA Continuous epidural analgesia LMA Recovery recorded on anes. form Intubated Direct admit to hospital ward, Aldrete score _________ No intra-operative anesthesia adverse events noted For >24 hour admits: No adverse anesthesia related complications noted, satisfactory progress and recovery See progress notes for anesthesia related concerns DATE PROVIDER
E
CONTROLLED MEDICATIONS
TIME
HISTORY PRESENT ILLNESS / SURGICAL DIAGNOSIS
MEDICATION
USED
DESTROYED
RETURNED
PLANNED ANESTHESIA GA Local / MAC Epidural Caudal Cont Spinal CSE
Special Monitors / Airway / Concerns:
PROVIDER WITNESS
Deep Sedation SAB Regional: PRE-ANESTHESIA DIRECTIONS / MEDICATIONS
EVALUATOR / DATE:
NPO per ASA EVALUATOR / DATE: Guidelines
See previous anesthesia record dated _________________ for information
lb / kg
NONE
DIAGNOSTIC STUDIES
LABORATORY STUDIES
POST ANESTHESIA CARE NOTES Somnolent Unarousable
Supplimental OPA / NPA Intubated Direct admit to hospital ward, Aldrete score _________ No intra-operative anesthesia adverse events noted
See progress notes for anesthesia related concerns
CONTROLLED MEDICATIONS
RETURNED
Potrebbero piacerti anche
- General Biology 1 NOTES PDFDocumento18 pagineGeneral Biology 1 NOTES PDFRose Mendizabal82% (17)
- Toltec Body Healing EbookDocumento204 pagineToltec Body Healing EbookDanielle Grace100% (3)
- List of Anesthesia Library BooksDocumento3 pagineList of Anesthesia Library BooksSivaramakrishnan Dhamotharan100% (2)
- PacuDocumento24 paginePacuLamtioma GultomNessuna valutazione finora
- Respiratory Assessment GuidelinesDocumento1 paginaRespiratory Assessment GuidelinesAmeliaM100% (2)
- Gunshot WoundDocumento57 pagineGunshot Woundnecrophilia090407Nessuna valutazione finora
- Sodium Chloride Injection and Intravenous Infusion-PiDocumento4 pagineSodium Chloride Injection and Intravenous Infusion-PiNg Chee LunNessuna valutazione finora
- Learning and Memory 3rd Edition Gluck Test BankDocumento26 pagineLearning and Memory 3rd Edition Gluck Test Banklaurenhaynesnjqcdgotay100% (15)
- Bio Lab ReportDocumento7 pagineBio Lab Reportjoylee05Nessuna valutazione finora
- Anaesthesia RecordDocumento1 paginaAnaesthesia RecordАндрій ДанильцівNessuna valutazione finora
- Form 7389 Medical Record AnesthesiaDocumento3 pagineForm 7389 Medical Record Anesthesiasabbo morsNessuna valutazione finora
- 5-Hole 1/4 1 3/8 C-To-C: Anesthesia RecordDocumento10 pagine5-Hole 1/4 1 3/8 C-To-C: Anesthesia RecordMohammed100% (2)
- ICU One Pager NIPPVDocumento1 paginaICU One Pager NIPPVNicholas HelmstetterNessuna valutazione finora
- Agenda Bls-AclsDocumento2 pagineAgenda Bls-AclsespegehNessuna valutazione finora
- NeralDocumento9 pagineNeralmmNessuna valutazione finora
- AnesthesiaDocumento2 pagineAnesthesiaYuna WidjajaNessuna valutazione finora
- DPN Icu PDFDocumento1 paginaDPN Icu PDFharoonNessuna valutazione finora
- JD Respiratory TherapistDocumento3 pagineJD Respiratory TherapistLawrence MacaraegNessuna valutazione finora
- VentilatorWebinar1-Prof YasserDocumento28 pagineVentilatorWebinar1-Prof YasserShuaa AlabdulsalamNessuna valutazione finora
- Suez Canal University/ Faculty of Nursing (Medical Surgical Nursing/ Clinical Assessment Sheet 2 Year 2020/2021)Documento18 pagineSuez Canal University/ Faculty of Nursing (Medical Surgical Nursing/ Clinical Assessment Sheet 2 Year 2020/2021)طالب جامعة100% (1)
- Pediatric Assessment: General ImpressionDocumento2 paginePediatric Assessment: General ImpressionAghnia Nafila100% (1)
- Pediatric AnesthesiaDocumento6 paginePediatric AnesthesiaKeyien RadonesNessuna valutazione finora
- Introduction To Pediatric VentilationDocumento41 pagineIntroduction To Pediatric Ventilationedderj2585Nessuna valutazione finora
- Basic Mechanical Ventilation 2014Documento62 pagineBasic Mechanical Ventilation 2014dragon66Nessuna valutazione finora
- HANDOUTS-Non Invasive VentilationDocumento15 pagineHANDOUTS-Non Invasive VentilationKristine MangasepNessuna valutazione finora
- How To Treat: Septic ShockDocumento6 pagineHow To Treat: Septic ShockmeeandsoeNessuna valutazione finora
- Respiratory Therapist, NICU/ICUDocumento5 pagineRespiratory Therapist, NICU/ICUapi-77517256Nessuna valutazione finora
- Bsn-Rs-Careplan 2Documento9 pagineBsn-Rs-Careplan 2api-520841770Nessuna valutazione finora
- ACLS Class Packet PDFDocumento9 pagineACLS Class Packet PDFImam GultomNessuna valutazione finora
- An Easy Guide To Head To Toe Assessment Vrtis 12 2008 WebsiteDocumento6 pagineAn Easy Guide To Head To Toe Assessment Vrtis 12 2008 WebsiteGary Cochran100% (1)
- A B C D e AssessmentDocumento6 pagineA B C D e AssessmentANGELICA JANE FLORENDONessuna valutazione finora
- Medical Emergencies OMFSDocumento72 pagineMedical Emergencies OMFSkatnev100% (1)
- Location at Time of Fall (Ward, Clinic, Service, Etc.) : - Inpatient Outpatient Date of Fall: Time of Fall (Military)Documento5 pagineLocation at Time of Fall (Ward, Clinic, Service, Etc.) : - Inpatient Outpatient Date of Fall: Time of Fall (Military)Eduard RiparipNessuna valutazione finora
- Preparation-Surgical Area: Have To Operate Without ConsentDocumento5 paginePreparation-Surgical Area: Have To Operate Without ConsentJane Bautista100% (1)
- PRE ANAESTHETIC ASSESSMENT New 1Documento41 paginePRE ANAESTHETIC ASSESSMENT New 1lokeswara reddyNessuna valutazione finora
- 2020 Acls Megacode Testing Scenarios - 2Documento13 pagine2020 Acls Megacode Testing Scenarios - 2Dr. Saqib RazaNessuna valutazione finora
- Critical Care Skills Checklist: Personal InformationDocumento5 pagineCritical Care Skills Checklist: Personal InformationRin noharaNessuna valutazione finora
- Module 9 Mechanical Ventilation PDFDocumento46 pagineModule 9 Mechanical Ventilation PDFChabboo SutabrataNessuna valutazione finora
- Downtime Daily Nursing Assessment & Care Plan: 1 of 5 Date: TimeDocumento5 pagineDowntime Daily Nursing Assessment & Care Plan: 1 of 5 Date: TimerupaliNessuna valutazione finora
- Acls Seminar MeDocumento62 pagineAcls Seminar MeAbnet Wondimu100% (1)
- Patient History TemplateDocumento2 paginePatient History TemplateDr Shazana NazrinNessuna valutazione finora
- Pulmonary Function Testing1Documento51 paginePulmonary Function Testing1kusaarNessuna valutazione finora
- Chapter 5: Analyzing A Rhythm StripDocumento7 pagineChapter 5: Analyzing A Rhythm StriptellyNessuna valutazione finora
- Anesthesia ManualDocumento21 pagineAnesthesia ManualDocFrankNessuna valutazione finora
- Cardiac DrugsDocumento3 pagineCardiac DrugsRon WoodardNessuna valutazione finora
- 1008 1400 ACLS - StudyGuide Print PDFDocumento54 pagine1008 1400 ACLS - StudyGuide Print PDFWaqar HassanNessuna valutazione finora
- 17 Admission APP MED 001Documento8 pagine17 Admission APP MED 001HAMMYER ALROKHAMINessuna valutazione finora
- Cardiology Teaching PackageDocumento9 pagineCardiology Teaching PackageRicy SaiteNessuna valutazione finora
- Airway MXDocumento47 pagineAirway MXansuh22Nessuna valutazione finora
- Anesthesia RecordDocumento1 paginaAnesthesia Recordpcellaneous pc rentalsNessuna valutazione finora
- Cardiovascular Disorders 1Documento44 pagineCardiovascular Disorders 1Nader Smadi100% (1)
- BLS Study Guide 020620013Documento38 pagineBLS Study Guide 020620013R RatheeshNessuna valutazione finora
- Intravenous Anesthetic AgentsDocumento23 pagineIntravenous Anesthetic Agentsdrhiwaomer100% (7)
- Anaphylaxis With Angioedema: Section I: Scenario DemographicsDocumento7 pagineAnaphylaxis With Angioedema: Section I: Scenario DemographicsharasthaNessuna valutazione finora
- Anaphylaxis CEACCP 2004Documento3 pagineAnaphylaxis CEACCP 2004kuruppukarlNessuna valutazione finora
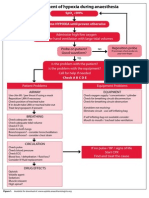
- Management of Hypoxia During AnaesthesiaDocumento5 pagineManagement of Hypoxia During AnaesthesiaNurhafizahImfista100% (1)
- 5 Shock PPT EnglishDocumento77 pagine5 Shock PPT EnglishKessi VikaneswariNessuna valutazione finora
- Antrim ED Handbook 2019Documento238 pagineAntrim ED Handbook 2019Chris Jardine LiNessuna valutazione finora
- Mechanical Ventilation Airway Pressure Release Ventilation Checklist Respiratory Therapy - 070420Documento3 pagineMechanical Ventilation Airway Pressure Release Ventilation Checklist Respiratory Therapy - 070420shubham2812Nessuna valutazione finora
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsDa EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsNessuna valutazione finora
- A Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsDa EverandA Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsNessuna valutazione finora
- Lapsus Cardio v3Documento31 pagineLapsus Cardio v3Nurfitrianti ArfahNessuna valutazione finora
- Intern Survival Guide (UIC)Documento51 pagineIntern Survival Guide (UIC)medstick100% (1)
- ShockDocumento75 pagineShockaulianmediansyahNessuna valutazione finora
- Lecture Notes On Biophysics and Bioimaging 2009Documento128 pagineLecture Notes On Biophysics and Bioimaging 2009Anonymous 9rJe2lOskx100% (2)
- Semi-Detailed Lesson Plan in SCIENCE Grade 9Documento4 pagineSemi-Detailed Lesson Plan in SCIENCE Grade 9Sheryll Cayme SalindoNessuna valutazione finora
- Pathoma, Sketchy Pharm & Micro, B&B Video TimesDocumento52 paginePathoma, Sketchy Pharm & Micro, B&B Video TimesAlina PolancoNessuna valutazione finora
- Nitrogen CycleDocumento10 pagineNitrogen CyclebellaNessuna valutazione finora
- What Is Peritoneal DialysisDocumento34 pagineWhat Is Peritoneal DialysisKen MagallanesNessuna valutazione finora
- 07 Bibliography FormatDocumento14 pagine07 Bibliography FormatArjun KafleNessuna valutazione finora
- Cell 1981 Cech PDFDocumento10 pagineCell 1981 Cech PDFSpellkingNessuna valutazione finora
- AED (Automated External Defibrilation)Documento17 pagineAED (Automated External Defibrilation)Ari AsriniNessuna valutazione finora
- Weeks 3 - 8Documento32 pagineWeeks 3 - 8Stefan HutsonNessuna valutazione finora
- Chapter 20 - Embryology of The Genitourinary Tract - Campbell - Walsh-Wein UROLOGY 12thDocumento40 pagineChapter 20 - Embryology of The Genitourinary Tract - Campbell - Walsh-Wein UROLOGY 12thkrisnaNessuna valutazione finora
- Format Ketikan LabDocumento9 pagineFormat Ketikan Labapril babyNessuna valutazione finora
- Parenting Children With Reactive Attachment DisorderDocumento13 pagineParenting Children With Reactive Attachment Disorderboglous100% (1)
- Xi - Bio Zoo Question PaperDocumento9 pagineXi - Bio Zoo Question PaperVeeramaniNessuna valutazione finora
- ReceptoretDocumento37 pagineReceptoretBlodin ZylfiuNessuna valutazione finora
- Problem Set 2 EndocrinologyDocumento12 pagineProblem Set 2 EndocrinologyJessica EtieneNessuna valutazione finora
- Neonatal JaundiceDocumento56 pagineNeonatal Jaundicesuardiman acoNessuna valutazione finora
- Melatonin Disturbances in Anorexia Nervosa and Bulimia NervosaDocumento9 pagineMelatonin Disturbances in Anorexia Nervosa and Bulimia NervosaImelia AnggraeniNessuna valutazione finora
- Fluids and Transport: Fundamentals of Anatomy & PhysiologyDocumento161 pagineFluids and Transport: Fundamentals of Anatomy & Physiologyann aquinoNessuna valutazione finora
- Bloody Tears Following Lefort 1Documento3 pagineBloody Tears Following Lefort 1paulwhite1234Nessuna valutazione finora
- Chapter 18 - Apoptosis - 112612Documento28 pagineChapter 18 - Apoptosis - 112612Anonymous nkR1PhIHNessuna valutazione finora
- Li 1 Anatomy, Histology, PhysiologyDocumento17 pagineLi 1 Anatomy, Histology, PhysiologysandyaadindaNessuna valutazione finora
- Type of Cell FunctionDocumento3 pagineType of Cell FunctionDerek Pagsolingan0% (1)
- Emma Jordan - Research Final DraftDocumento7 pagineEmma Jordan - Research Final Draftapi-436829682Nessuna valutazione finora
- Australian Prescriber (1988) Bioavailability and First Past ClearanceDocumento3 pagineAustralian Prescriber (1988) Bioavailability and First Past Clearance1234chocoNessuna valutazione finora
- ADR Common Drug - Induced Organ DisordersDocumento45 pagineADR Common Drug - Induced Organ Disorders0009439Nessuna valutazione finora