Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Acute Superficial Venous Thrombophlebitis
Caricato da
krughooburDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Acute Superficial Venous Thrombophlebitis
Caricato da
krughooburCopyright:
Formati disponibili
ACUTE SUPERFICIAL VENOUS THROMBOPHLEBITIS
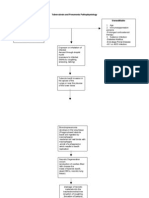
the lower extremities Thrombophlebitis - inflammation of a vein with the formation of thrombi in their lumen. Etiology and pathogenesis Thrombophlebitis is divided into traumatic and non-traumatic. Traumatic thrombophlebitis occurs in cases where the injured vessel wall itself (intravenous injection, including long-term catheterization of veins, traumatic injury, surgery). Non-traumatic thrombosis - is often a transition of inflammation to the surrounding tissue to the venous wall with the subsequent formation of thrombus. Non-traumatic thrombophlebitis may occur also in violation of local hypercoagulation and blood. Thrombophlebitis Thrombophlebitis is divided into varicose veins and thrombophlebitis nonextended veins. Thrombosed veins under the influence of conservative tive therapy, usually within 2 ... 3 months rekanaliziruyutsya, but the inflammation ends with the formation of scar tissue, so the venous wall loses its elasticity, impaired function of its valvular apparatus. In some cases, scar obliteration of the vein occurs. The clinical picture In the event of thrombosis in patients complain of throbbing pain in the course of the venous trunk, sometimes very intense, worse when walking. Fever, malaise, and weakness. On examination, most often on the lower leg on the thigh are less inflammatory infiltrates along the saphenous vein, the skin over the infiltration hyperemic and edematous. Skin hot to touch, sharply painful. A number of patients indicated lymphangitis and / or enlarged inguinal lymph nodes (regional lymphadenitis). Appears leukocytosis, increased erythrocyte sedimentation rate. In rare cases, infiltration occurs in the course of softening, skin becomes bluish-purple color is determined by the fluctuation, which indicates that abscess formation (suppurative thrombophlebitis). Thrombophlebitis of superficial veins, if you do not extend to the deep veins, almost never causes pulmonary thromboembolism. Treatment In the acute stage of thrombosis can be treated conservatively: bed rest; antibiotic therapy; direct-acting anticoagulants (heparin, fraxiparine for 6 ... 8 days); anticoagulants of indirect action (fenilin, bishydroxycoumarin, pelentan, etc.) shall be appointed for 3 ... 4 day and received within 3 ... 4 weeks; anti-inflammatory (ibuprofen, Indus-tatsin, etc.); antihistamines. Non-variceal vein thrombophlebitis treated conservatively. Thrombophlebitis of varicose veins modified after eliminating acute phenomenon undergoes surgical treatment: resection is timecharged veins together with the surrounding infiltrate. Postoperative rehabilitation is required with the zinc-gelatin dressings as in varicose veins. Thrombosis and deep vein thrombophlebitis the lower extremities Primary (spontaneous) phlebemphraxis - is an aseptic condition, or more often a complication caused by Virchow's triad: hypercoagulability, injury (violation) of the vessel wall, upset regional blood flow. Secondary phlebemphraxis (thrombophlebitis), deep vein phenomenon is relatively rare, most often associated with septic process, which are located close to the corresponding vein. A significant difference between primary and secondary phlebemphraxis is a strong fixation of the thrombus to the vessel wall with secondary phlebothrombosis, which dramatically reduces or virtually eliminates the possibility of pulmonary thromboembolism (PTE). In the primary deep vein phlebothrombosis possible pulmonary embolism is often a natural outcome. The etiology and pathogenesis. Contributing factors in the development of deep vein phlebothrombosis are: hypercoagulation; reduction of fibrinolytic activity of blood; damage to the vessel wall; slowing or impairing blood flow; allergic condition of the body; violation of the rheological properties of blood; elderly age; cancer; Pregnancy obesity; presence of varicose veins. A very big danger is postoperative phlebothrombosis in which there are a number of predisposing factors. Spontaneous postoperative phlebothrombosis and other deep veins in the majority of cases occur in the lower limbs, due to specific morphological and functional features of legs veins located in the soleus and gastrocnemius muscles - suralnye vein.
Clinic phlebothrombosis deep vein A. A sense of fullness in the back of the gol-no. Two. Swelling of the distal limb - the rear area of the foot and ankle. Three. Spontaneous pain in the heels (symptom Ryabov GA) 4. Skin color is not changed or more bluish in the foot and n / s leg. Five. Palpation in the swelling is painless, there is pain in the calf muscles 6. Movement in the ankle joint is limited because of pain 7. Dorsal flexion sharply painful (symptom Homansa). Diagnosis A. Doppler Two. Rheography Three. Manometry 4. Phlebography (in the planning of surgery on the veins).
Acute phlebothrombosis This disease is caused by the development of primary thrombus in the lumen of one or another is not affected inflammation vein due to disturbances in coagulation and anticoagulation systems blood with a local slowing of venous flow. Subsequently, a thromboDhu join secondary inflammatory changes of the venous wall. When phlebothrombosis large veins (these include deep vein) is always there is a risk of pulmonary embolism and thrombophlebitis in this complication occurs much less frequently due to the strong fixation of the thrombus to the vevenous wall. Symptoms. Thrombophlebitis in contrast to phlebothrombosis from the beginning proceeds with oolee severe clinical picture of acute inflammation. Acute thrombosis is characterized by a combination of symptoms of illness regionarnogo venous blood with signs of acute inflammation fever, rapid deterioration of the patient's general condition, second, weak, weakness, leukocytosis with a shift of leukocyte left, a sharp pain along the thrombosed vein area, Regitionary lymphadenitis. Sometimes in the course of the affected veins are formed purulent ki, requiring autopsy. The clinical picture phlebothrombosis depends on the localization of a blood clot, and the degree of blockage of the lumen of their veins. Phlebemphraxis-characterized the edema and cyanosis of limbs with less of pain, almost total reaction of the organism, if it exists, it appears the subfebrile body temperature, slight malaise and weakness. Flebotromboz can proceed completely asymptomatic, especially in the floating (Floating) thrombus. These forms of thrombosis are dangerous, because these clots can easily rejected, and sometimes the first clinical sign of disease are no disturbances of blood circulation in the limb renoznogo and symptoms of emboLeah pulmonary artery. Phlebemphraxis calf deep vein often develops in patients are on bedrest (which is why all patients who findXia in bed, need to appoint a special preventive esk events). The first signs of deep vein phlebothrombosis golare often no feeling of heaviness in the legs and slight swelling (The latter may be absent). At the rear of the passive flexion of the foot there is pain on the back of the leg extending to the popliteal pitky, and in the popliteal fossa, as well as pressure on the sole. A large diagnostic value of a test, consisting in the lower leg compression
cuff of the device for measuring blood pressure in the deep flebotromooze at a pressure of 80-100 mm Hg. of Art. there is a sharp pain in the the affected leg, while the increase in pressure up to 150-170 mm Hg. of Art. in a healthy calf does not cause discomfort. Ilio-femoral phlebemphraxis (ileofemoralny). At full-Zach the lumen of the vein flogging ileofemoralny phlebemphraxis begins acutely with sharp What the pain in all limbs, accompanied by fever and chills with a decrease in skin temperature of the affected leg. Limb becomes pale and cyanotic. There is swelling throughout the leg, the decay rostranyayuschayasya on the abdomen and lumbar region. Ripple peripheral due to reflex spasm of the arteries is greatly weakened or even completely ceases to be determined, which often creates certain difficulties in the differential the differential diagnosis of arterial thrombosis ileofemoralnogo emboliher. Sometimes the only clinical manifestation of thrombotic ileofemoralnogo for it may be a pain when walking. Emergency care and hospitalization. All patients are subject to immediate statecapitalization in the surgical hospital. When phlebothrombosis chances on the effectiveness of fibrinolytic therapy restrictions HN. Treatment in hospital should be complex: the general anti-inflammatory Indeed, and anticoagulant therapy, topical treatment - complete rest toinfinity, physiotherapy, x-ray. Surgical treatment is applicable etsya when complications arise (ascending septic thrombosis, beneTurn embolism, the formation of ulcers, etc.). The operation is vein ligation and dissection of purulent foci. In some cases, thrombosing the bathroom is completely excised vein Phlebemphraxis deep veins - a potentially life-threatening disease. Thrombosis of the main veins of the pelvis and hips can be a primary location in the deep veins of the legs, or ilio-femoral veins. In the first 3-4 days of a blood clot poorly fixed to the vessel wall, possible separation of the thrombus and thromboembolism branches of the pulmonary artery (pulmonary embolism). After 5-6 days, joins an inflammation of the intima, contributing to fixing the clot, deep vein thrombophlebitis. In the U.S. each year the disease affects about 250,000 people. Etiology. Launchers consider the following factors: - Trauma or excessive physical stress; - A bacterial infection; - Prolonged bed rest in surgical, therapeutic, neurological diseases; - Post-natal period; - Use of oral contraceptives; - Cancer (especially lung, stomach, under-gastric cancer); - DIC. The localization process. Clinically distinguish deep vein thrombosis leg and iliac-femoral (iliofemoralny) phlebemphraxis. Emboli in the pulmonary artery originate from these vessels in approximately 80-90% of cases of pulmonary embolism. More than a rare localization. - Subclavian Vienna. - Vienna's upper extremities and neck (especially when catheterization). - The right atrium. - Renal vein (especially with renal disease). The clinical picture. Deep phlebemphraxis accompanied by persistent swelling of the legs or the whole foot, feeling of heaviness in the legs. The skin is glossy, clear picture appears saphenous veins (symptom Pratt). Characterized as a symptom of Payr (spread the pain on the inner surface of the foot, calf or thigh), Homansa symptom (pain in the leg with back flexion of the foot). Also, there is pain in the leg cuff compression device
for measuring blood pressure at a value of 80-100 mmHg (Symptom Lovenberga), while the compression of the healthy leg up to 150-180 mm Hg. of Art. does not cause discomfort.When the pelvic vein thrombosis observed light peritoneal symptoms, and sometimes dynamic ileus. Deep venous thrombosis is the classic clinical manifestations in only 50% of cases. In 50% of cases, confirmed by venography, deep vein thrombosis is not accompanied by visible changes. The first manifestation of the disease, many patients may be thromboembolism in the pulmonary artery vessels. The diagnosis of deep vein thrombosis confirmed by the following studies. - Phlebography (distal ascending) and the most accurate method of diagnosis of deep vein thrombosis. Radiopaque substance is injected into one of the saphenous veins of the foot below the turnstile, slightly compressing the ankle to direct the movement of contrast medium into the deep vein system. If the research does not wash out the vein with heparin in 3% of cases there is inflammation or thrombosis. - Doppler ultrasound confirmed deep vein thrombosis above the knee, up to 80-90%. - Impedance plethysmography. After loosening the cuff, compressing the shin with a force sufficient for the temporary occlusion of the venous blood supply to determine the change in volume of the tibia. The sample allows you to diagnose deep venous thrombosis above the knee, up to 90%. - Scan using labeled fibrinogen. To determine the incorporation of radioactive fibrinogen in the blood clot perform batch scanning of both lower extremities. The method is most effective for the diagnosis of leg vein thrombosis. Treatment. All patients with phlebemphraxis be treated in a surgical hospital. Prescribed strict bed rest for 7-10 days with a lofty position of the patient limb. Heparin is administered / v for 7-10 days. With the development of complications (eg pulmonary embolism), or the risk of recurrent embolism term anticoagulant therapy increased. Duration receiving anticoagulants of indirect action depends on the severity of the disease. Thrombolytic therapy (streptokinase or edyukinaza) is effective at the earliest, is rarely recognizable, stages of venous thrombosis. At later stages of thrombolysis may cause fragmentation of the thrombus and the occurrence of pulmonary embolism. In the diagnosis of thrombosis of the floating station is shown in the inferior vena cava cava filter below the renal veins or the holding of various surgical interventions, preventing the migration of a thrombus in the pulmonary artery system, followed by thrombolysis and anticoagulation therapy. Thrombolytic therapy without interruption cava filter thrombosis with ileomoralnom contraindicated because it promotes the migration of blood clots in the pulmonary artery to the development of TELA. Prevention. The simplest preventive measures include early motion after surgery, the use of elastic stockings (foot compressing the superficial veins and increases blood flow in the deep veins), as well as the exclusion of risk factors. Periodic leg compression with a pneumatic cuff increases the rate of blood flow in the lower extremities and helps prevent blood stasis. Venokonstriktory (eg, dihydroergotamine, detraleks) also increase the rate of blood flow in the deep veins. Heparin, administered at prophylactic doses before and after surgery can effectively prevent deep vein thrombosis. His repeated subcutaneous administration repeatedly every 4-6 hours
Potrebbero piacerti anche
- Cardiogenic ShockDocumento19 pagineCardiogenic ShockkrughooburNessuna valutazione finora
- Bridge of Stone and MagicDocumento208 pagineBridge of Stone and MagicTrevor Hopkins100% (6)
- Mitral StenosisDocumento10 pagineMitral StenosiskrughooburNessuna valutazione finora
- Human Immunodeficiency Virus: Presented by Rughoobur Chitra Group 2 (A) Faculty of Foreign StudentsDocumento51 pagineHuman Immunodeficiency Virus: Presented by Rughoobur Chitra Group 2 (A) Faculty of Foreign StudentskrughooburNessuna valutazione finora
- CARDIOSPASMDocumento2 pagineCARDIOSPASMkrughooburNessuna valutazione finora
- YersiniosisDocumento10 pagineYersiniosiskrughooburNessuna valutazione finora
- AmoebiasisDocumento3 pagineAmoebiasiskirtyy20Nessuna valutazione finora
- BrucellosisDocumento9 pagineBrucellosiskrughooburNessuna valutazione finora
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (120)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- ETT Seminar - Isotopes in MedicineDocumento71 pagineETT Seminar - Isotopes in MedicineisocenterNessuna valutazione finora
- Salalima v. ECC & SSS, GR No. 146360, May 20, 2004Documento5 pagineSalalima v. ECC & SSS, GR No. 146360, May 20, 2004Jonna Maye Loras CanindoNessuna valutazione finora
- Anaesthesia and Parkinsons DiseaseDocumento14 pagineAnaesthesia and Parkinsons DiseasedrjaikrishNessuna valutazione finora
- DIAGNOSTICS (Student Copy)Documento59 pagineDIAGNOSTICS (Student Copy)Abigail Mayled LausNessuna valutazione finora
- Filetype PDF SplenectomyDocumento2 pagineFiletype PDF SplenectomyDanNessuna valutazione finora
- ALZHEIMERDocumento9 pagineALZHEIMERKhem Limoso100% (2)
- Mom WP Med RPTDocumento1 paginaMom WP Med RPTravi kumar v100% (1)
- 1201 Alodine, AKA DX 503Documento7 pagine1201 Alodine, AKA DX 503Mark Evan SalutinNessuna valutazione finora
- First Virtual Autopsy in Saudi ArabiaDocumento5 pagineFirst Virtual Autopsy in Saudi ArabiaNatasyaNessuna valutazione finora
- Effectivity of Lumbrokinase in Reducing Proteinuria On Patients With Diabetic Kidney DiseaseDocumento11 pagineEffectivity of Lumbrokinase in Reducing Proteinuria On Patients With Diabetic Kidney Diseasevedora angeliaNessuna valutazione finora
- Sample Statement of Research Proposal and Personal Statement For The Gates Cambridge Scholarship Application-Student #1Documento4 pagineSample Statement of Research Proposal and Personal Statement For The Gates Cambridge Scholarship Application-Student #1Edward Kofi AzeleorNessuna valutazione finora
- Castle Connolly Graduate Board Review SeriesDocumento63 pagineCastle Connolly Graduate Board Review SeriesCCGMPNessuna valutazione finora
- Spiritual Care in Hospice and Palliative CareDocumento6 pagineSpiritual Care in Hospice and Palliative CareKrisnaNessuna valutazione finora
- Drug Profile 2015Documento75 pagineDrug Profile 2015api-324380555100% (1)
- ENT Notes CrakDocumento52 pagineENT Notes CrakGrant KimNessuna valutazione finora
- Lung Cancer - 2021Documento20 pagineLung Cancer - 2021Gilbert LazarusNessuna valutazione finora
- Textbook of Clinical Occupational and Environmental MedicineDocumento4 pagineTextbook of Clinical Occupational and Environmental MedicineAmos SiraitNessuna valutazione finora
- 114-Raro vs. ECCDocumento6 pagine114-Raro vs. ECCNimpa PichayNessuna valutazione finora
- NCM 106 Midterm 2013Documento6 pagineNCM 106 Midterm 2013Kirsten Sabanal100% (1)
- Times Leader 03-31-2013Documento67 pagineTimes Leader 03-31-2013The Times LeaderNessuna valutazione finora
- Patient Medical History FormDocumento5 paginePatient Medical History FormDavid Fernando Gutierrez HernandezNessuna valutazione finora
- Dermoid CystDocumento29 pagineDermoid CystAlik ChuaNessuna valutazione finora
- My Experience With Kali Brom in A Case of Polycystic Ovarian SyndromeDocumento6 pagineMy Experience With Kali Brom in A Case of Polycystic Ovarian SyndromeHomoeopathic Pulse100% (1)
- PathophysiologyDocumento6 paginePathophysiologyElbert Hermogino ﭢNessuna valutazione finora
- Tateishi's Cancer Healing FormulaDocumento8 pagineTateishi's Cancer Healing FormulaSyafiq Abdullah100% (1)
- Bethesda System For ThyroidDocumento61 pagineBethesda System For ThyroidAkanksha KushwahNessuna valutazione finora
- Clinical Ophthalmic Oncology Retinal Tumors 3rd EdDocumento174 pagineClinical Ophthalmic Oncology Retinal Tumors 3rd EdInstituto de la VisionNessuna valutazione finora
- Metabolisme Lipoprotein Modul 2.2Documento72 pagineMetabolisme Lipoprotein Modul 2.2Rizky AkbarNessuna valutazione finora
- English Training For Nurses and Hospital StaffDocumento73 pagineEnglish Training For Nurses and Hospital Staffviaerea100% (1)
- LECTURE 1: Organon 1. "The Sick": PrinciplesDocumento13 pagineLECTURE 1: Organon 1. "The Sick": PrinciplesOana SandraNessuna valutazione finora