Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Phlebitic Risks and Prevention
Caricato da
Afri SunadiDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Phlebitic Risks and Prevention
Caricato da
Afri SunadiCopyright:
Formati disponibili
research perspective
PerIPHeraL InTraVenOUs CaTHeTer:
nOra D. yan, bsn, Msn(c), rn, PCCn
Phlebitic risks and Prevention
uring one of my MSN classes, an assignment I particularly enjoyed completing was an evidenced-based nursing project. By evidenced-based nursing, Im referring to The conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients or groups.(which) requires integration of individual clinical expertise and patient preferences with the best available external clinical evidence from systematic research, and consideration of available resources1. I decided to focus my research on the incidence of phlebitis as it relates to peripheral intravenous catheters or PICs. I chose this particular topic because of my own experience with patients who had complications with their peripheral IV sites. Placement of a PIC can be one of the most invasive and painful procedures patients encounter during their hospitalization. Studies have revealed that 20-80 percent of patients receiving IV infusions develop phlebitis, and more than 40% of these patients develop post-infusion phlebitis more than 24 hours after the PIC has been removed2. It is thus very important that nurses become familiar with the complications that can occur with PICs in order to prevent numerous IV sticks, keep the patient safe, and increase the nurse workload. In this article, I summarize what is found in the literature regarding the risk factors that can lead to phlebitis as it relates to PICs and the preventative measures that can help reduce the incidence of phlebitis.
Phlebitis is an inflammation of the vein with signs and symptoms that include pain, erythema, edema, streak formation and/or palpable cord. In my research, which covered the last ten years, I found conflicting results from various studies researching the contributing factors for phlebitis. Therefore, I took the consensus of the results from these studies and list the common risk factors for phlebitis below1-10:
PIC: lack of skill in peripheral IV starts, location of IV
sites, loose dressings, two or more PICs (especially if on the same extremity), unit or location where IV was inserted (e.g. ER, OR, Med-Surg; emergent situations have a higher frequency) Indwell tIme: if phlebitis occurs, highest frequency is usually after 72 hours3 from insertion PatIent CondItIon: age (>60), females, diagnosis (e.g. diabetics, infection, circulatory problems) VesICant IV medICatIons: pH, osmolarity, fast rate (varies depending on solution), frequency Problems in placing PICs can cause thrombophlebitis to occur. If the vein is punctured completely through both walls, it is important to apply pressure so that blood does not leak in the surrounding tissues. Loose dressings can cause phlebitis by allowing movement of the PIC, which causes trauma to the vein. Studies have found the highest risks of phlebitis occur on the hands and antecubital fossa4.
TAblE 1. vESicANT MEDicATiONS7,8
ANTibiOTicS doxycyline nafcillin piperacillin vancomycin ANTiNEOplASTic (chEMO) dectinomycin daunorubicin doxorubicin epirubicin idarubicin mechlorethamine mitomycin C paclitaxel vinblastine vincristine vinorelbine ElEcTROlyTES calcium chloride calcium gluconate potassium chloride sodium bicarbonate cARDiAc/ vASO-AcTivE amiodarone dobutamine dopamine epinephrine metaraminol norepinephrine MiScEllANEOUS radiocontrast media doxapram lorazepam phenytoin dextrose >10% promethazine
p. 16
STANFORD NURSE
Sp R iN G 2 0 1 0
nIne stePs to PreVentIng PhlebItIs
based on the research, the following steps are recommended to prevent phlebitis:
educate/review IV
start techniques and risks for phlebitis with new and experienced nurses
decrease the rate of
and/or dilute vesicant medications during administration
be aware that an IV placed
during an emergent situation may need to be replaced earlier than 96 hours
educate patients on
the risks for phlebitis and encourage them to report any pain, discomfort, leaking, edema, or pinkish tinge at the IV site immediately
change PIC sites every
96 hours as needed (with physician order, may be extended for 1-2 days) advise physicians to place a central access if vesicant infusions are necessary and continuous
use the chlorhexidine gluconate solution
prior to each IV start and allow it to dry for at least 30 seconds (This should be standard practice. It also helps to prevent infections and decrease the incidence of phlebitis due to possible antibiotics administration if an infection occurs).
closely monitor/ assess IV sites especially
before an infusion is started
flush IV lines before and after starting an IV infusion
It is the nurses responsibility to insert and assess peripheral intravenous catheters to prevent phlebitis and other IV complications from occurring. Understanding the risk factors, being aware of potential problems, and following recommended guidelines will foster both patient well-being and nurse work satisfaction.
If more than one PIC is necessary, it is best to place one on each arm since having two or more on the same extremity can increase the incidence of phlebitis4. Also, PICs placed during emergent situations have higher risks for phlebitis because having an IV inserted usually takes precedence over careful infection prevention.5 Patient conditions can also be contributing factors for phlebitis. Patients with a high risk of developing phlebitis include4,5: > 60 years of age Females Diabetics IV drug abusers Immunocompromised Septic Receiving chemotherapy Peripheral vascular disease Blood abnormalities Other circulatory problems Raynauds phenomenon (arterial spasm may occur compromising peripheral circulation and reducing venous blood flow) Vesicants or IV infusions that are irritating to veins have also shown to be a big factor for phlebitis. The pH of blood is between 7.35-7.40, while the osmolarity is between 280-290mOsm/kg.4,5 The pH and osmolarity are similar to isotonic fluids which do not cause phlebitis. Infused solutions should have a pH between 5-9 and osmolarity of 281-290 mOsm/L.4-6 Anything outside of these ranges can irritate and damage the venous endothelial wall, possibly leading to rupture. Vasoactive medications (e.g. dobutamine, dopamine, epinephrine) reduce blood flow from severe constriction of smooth muscles around capillaries and can result in
S pR i N G 2 0 1 0
ischemic necrosis. 4-6 Other vesicants include antibiotics and chemotherapy IV infusions.4-6 If these drugs must be administered, its best to use a central line. According to Infusion Nurses Society Standards of Practice, a central line should be used when the IV solutions final concentration contains >5% protein, >10% dextrose, or has a final total osmolarity of >500mEq/liter. 7 Table 1 (at left) shows a list of some common vesicants.4-7 An interesting new theory is that a high hematocrit decreases the dilution of vesicants, thereby predisposing patients to phlebitis.10 However, further study needs to be done in this area. SN
REFERENCES 1 DiCenso A, Guyatt G, Ciliska D. Evidence-based nursing: a guide to clinical practice. St. Louis: Mosby; 2005. 2 White, Sherrill. Peripheral intravenous therapy-related phlebitis rates in an adult population. Journal of Intravenous Nursing. 24(1). Jan/Feb 2001. 3 Frune, F., Schrappe, M., Wenchel, H.M. Phelbitis rate and time kinetics of short peripheral intravenous catheters. Infection. 32;2004(1) 4 Uslusoy, E., Mete, S. Predisposing factors to phlebitis in patients with peripheral intravenous catheters: a descriptive study. Journal of Academy of Nurse Practitioners. 2008 (20) 172-180. 5 Zarate, L., Mandieco, B., Wilshaw, R., Raver, P. Peripheral intravenous catheters started in prehospital and emergency department settings. Journal of Trauma Nursing. 2008;15;2. 6 Infiltration and Extravasation, update on prevention and management. The art and science of Infusion Nursing. July-August 2009, 32:4. 7 Intravenous Nurses Society. Infusion nursing standards of practice. Journal of Intravenous Nursing. 2001; 23:6S. 8 Hadaway, Lynn, I.V. Infiltrationnot just a peripheral problem. Nursing Management. November 2000. 9 Lee, W., Chen, H, Tsai, T. Risk factors for peripheral intravenous catheter infection in hopsitalized patients: a prospective study of 3165 patients. American Journal of Infection Control. Oct 2009. 10 Monreal, M., Quilex, F., Rey-Joly, C., Rodriguez, S., Sopena, N., Neira, C. and Roca, J. Chest 1999;115;1576-1580.
STANFORD NURSE
p. 17
Copyright of Stanford Nurse is the property of Stanford Hospital & Clinics and its content may not be copied or emailed to multiple sites or posted to a listserv without the copyright holder's express written permission. However, users may print, download, or email articles for individual use.
Potrebbero piacerti anche
- Als Study GuideDocumento9 pagineAls Study GuideAfri SunadiNessuna valutazione finora
- Efek Clin KateterDocumento10 pagineEfek Clin KateterAfri SunadiNessuna valutazione finora
- Ilizarov Team Pin Site Care GuideDocumento2 pagineIlizarov Team Pin Site Care GuideAfri SunadiNessuna valutazione finora
- Ilizarov Team Pin Site Care GuideDocumento2 pagineIlizarov Team Pin Site Care GuideAfri SunadiNessuna valutazione finora
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (119)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- SQL 1: Basic Statements: Yufei TaoDocumento24 pagineSQL 1: Basic Statements: Yufei TaoHui Ka HoNessuna valutazione finora
- Tupperware India's Perception StudyDocumento10 pagineTupperware India's Perception StudyAnmol RahangdaleNessuna valutazione finora
- Operation Guide For The Mercedes-Benz GLA/CLADocumento5 pagineOperation Guide For The Mercedes-Benz GLA/CLASantosh TalankarNessuna valutazione finora
- Mesopotamia CivilizationDocumento56 pagineMesopotamia CivilizationYashika TharwaniNessuna valutazione finora
- Done by Akansha Bharti Harshitha K.N. Ishika Sunil Rajput Rashmi NaikDocumento12 pagineDone by Akansha Bharti Harshitha K.N. Ishika Sunil Rajput Rashmi NaikRamya BalanNessuna valutazione finora
- Rakpoxy 150 HB PrimerDocumento1 paginaRakpoxy 150 HB Primernate anantathatNessuna valutazione finora
- Chapter 1 - IntroductionDocumento42 pagineChapter 1 - IntroductionShola ayipNessuna valutazione finora
- Jesus - The Creator Unleashes Our Creative PotentialDocumento1 paginaJesus - The Creator Unleashes Our Creative PotentialKear Kyii WongNessuna valutazione finora
- City of Brescia - Map - WWW - Bresciatourism.itDocumento1 paginaCity of Brescia - Map - WWW - Bresciatourism.itBrescia TourismNessuna valutazione finora
- Donny UfoaksesDocumento27 pagineDonny UfoaksesKang Bowo D'wizardNessuna valutazione finora
- Notes On The Life and Works of Jose Rizal - IncompleteDocumento15 pagineNotes On The Life and Works of Jose Rizal - Incompleteblock_me_please50% (2)
- Critique On A Film Director's Approach To Managing CreativityDocumento2 pagineCritique On A Film Director's Approach To Managing CreativityDax GaffudNessuna valutazione finora
- STERNOL Specification ToolDocumento15 pagineSTERNOL Specification ToolMahdyZargarNessuna valutazione finora
- EPF Passbook Details for Member ID RJRAJ19545850000014181Documento3 pagineEPF Passbook Details for Member ID RJRAJ19545850000014181Parveen SainiNessuna valutazione finora
- Lab ReportDocumento5 pagineLab ReportHugsNessuna valutazione finora
- Complete Hemi Sync Gateway Experience ManualDocumento43 pagineComplete Hemi Sync Gateway Experience Manualapi-385433292% (92)
- Accidental PoisoningDocumento3 pagineAccidental PoisoningBRUELIN MELSHIA MNessuna valutazione finora
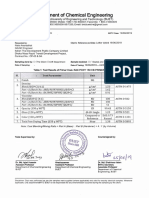
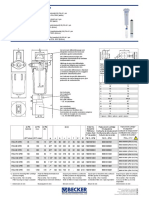
- Medical filter performance specificationsDocumento1 paginaMedical filter performance specificationsPT.Intidaya Dinamika SejatiNessuna valutazione finora
- VARCDocumento52 pagineVARCCharlie GoyalNessuna valutazione finora
- Conserve O Gram: Understanding Histograms For Digital PhotographyDocumento4 pagineConserve O Gram: Understanding Histograms For Digital PhotographyErden SizgekNessuna valutazione finora
- C11 RacloprideDocumento5 pagineC11 RacloprideAvina 123Nessuna valutazione finora
- Plant Air Centrifugal Compressors: Turbo-Air Series Featuring Oil-Free AirDocumento20 paginePlant Air Centrifugal Compressors: Turbo-Air Series Featuring Oil-Free AirSharad KokateNessuna valutazione finora
- ArtigoPublicado ABR 14360Documento14 pagineArtigoPublicado ABR 14360Sultonmurod ZokhidovNessuna valutazione finora
- EMMS SpecificationsDocumento18 pagineEMMS SpecificationsAnonymous dJtVwACc100% (2)
- MVJUSTINIANI - BAFACR16 - INTERIM ASSESSMENT 1 - 3T - AY2022 23 With Answer KeysDocumento4 pagineMVJUSTINIANI - BAFACR16 - INTERIM ASSESSMENT 1 - 3T - AY2022 23 With Answer KeysDe Gala ShailynNessuna valutazione finora
- CHB 2Documento15 pagineCHB 2Dr. Guruprasad Yashwant GadgilNessuna valutazione finora
- The Impact of Information Technology and Innovation To Improve Business Performance Through Marketing Capabilities in Online Businesses by Young GenerationsDocumento10 pagineThe Impact of Information Technology and Innovation To Improve Business Performance Through Marketing Capabilities in Online Businesses by Young GenerationsLanta KhairunisaNessuna valutazione finora
- Marksmanship: Subject: III. Definition of TermsDocumento16 pagineMarksmanship: Subject: III. Definition of TermsAmber EbayaNessuna valutazione finora
- Overview for Report Designers in 40 CharactersDocumento21 pagineOverview for Report Designers in 40 CharacterskashishNessuna valutazione finora
- Drypro832 PreInstallGude 0921YH220B 070627 FixDocumento23 pagineDrypro832 PreInstallGude 0921YH220B 070627 FixRicardoNessuna valutazione finora