Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Hmole Final
Caricato da
Joyce Anne Simangan NaragDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Hmole Final
Caricato da
Joyce Anne Simangan NaragCopyright:
Formati disponibili
GESTATIONAL THROPOBLASTIC DISEASE HYDATIDIFORM MOLE
I.
INTRODUCTION:
A hydatidiform mole is a rare mass or growth that forms inside the uterus at the beginning of a pregnancy. It is a type of gestational trophoblastic disease (GTD). A hydatidiform mole is growth of an abnormal fertilized egg or an overgrowth of tissue from the placenta. It is a neoplastic proliferation of the trophoblast in which the terminal villi are transformed into vesicles filled with clear viscid material Two types of molar growth can be identified by chromosomal analysis: COMPLETE MOLE: All trophoblastic villi swell and become cystic. If an embryo forms, it dies early at only 1 to 2 mm in size, with no fetal blood present in the villi. On chromosomal analysis, although the karyotype is a normal 46XX or 46XY, this chromosome component was contributed only by a father or an empty ovum was fertilized and the chromosome material was duplicated (Fig. 1).
Sperm 23
Ovum + + Duplication = 46
Fig. 1.Complete mole. PARTIAL MOLE: With a partial mole, some of the villi form normally. The syncytiotrophoblastic layer of the villi, however, is swollen and misshapen. A macerated embryo of approximately 9 weeks; gestation may be present in the villi. A partial mole has 69 chromosomes (a triploid formation in which there is three chromosomes instead of two for every pair, one set supplied by an ovum that apparently was fertilized by two sperm or an ovum fertilized by one sperm in which meiosis or reduction division did not occur). This could also occur if one set of 23 chromosomes was supplied by one sperm and an ovum did not undergo reduction division supplied 46 (see Fig. 2). In contrast to complete moles, partial moles rarely lead to choriocarcinoma.
Sperm 46
Ovum 23 69
+ 23 or 23 23
69
Fig. 2. Partial mole.
FEATURES Embryonic/fetal tissue
COMPLETE
PARTIAL Present (with fetus or at least an amniotic sac) Focal Focal Paternal and maternal 69XXY or 69XYY Rare
Absent (whole conceptus is transformed into a mass of vesicles) Swelling of villi Diffuse Trophoblastic hyperplasia Diffuse Karyotype Paternal 46XX (97%) or 46XY (47%) Malignant changes 5-10% Table 1. Various features of a complete and a partial mole. II. A. B. C.
PREVELANCE AND POPULATION AT RISK.
North America and Europe: 1:1000 to 1:1500 pregnancies Asia and Latin America: 1:400 to 1:200 pregnancies Philippines: 1:250 III. RISK FACTORS
A. Diet: Low CHON, Folic Acid and low Vitamin A (carotene) intake. B. Age: Women younger than 25 years and older than 35 years. GTD is higher toward the beginning and toward the end of child bearing period. It is ten times more in women who are 45 years old and beyond.
C. Race: Asian heritage. Molar pregnancy has no racial or ethnic predilection, although Asian countries show a rate 15 times higher than the US rate.
D. History: Prior Molar Pregnancy; The risk of recurrence is 1-2%. After 2 or more molar pregnancies, the risk of recurrence has been reported as 1 in 6.5 to 1 in 17.5. E. High Parity
IV. PATHOPHYSIOLOGY
PRECIPITATING FACTORS -DIET: Low CHON, Folic Acid and low
Vitamin A (carotene) intake.
PREDISPOSING FACTORS
- Women younger than 25 years and older than45 years. - Asian heritage - Prior Molar Pregnancy
Partial mole or Complete mole
Chronic villi degenerates and become filled with fluid No vasculature in chorionic villi
Early death & absorption of embryo
Absence of FHT
Trophoblastic proliferation
Uterus expands faster than normal
Abdominal pain
High secretion of hCG High progesterone
low estrogen
High chorionic thyrotropin
Amenorrhea
Marked nausea & vomiting
Decreased contraction
Hyperthyroidism
Separation of vesicles from uterine wall Multiple theca lutein cysts in the ovaries
Vaginal bleeding & discharge of vesicles Ovarian pain Pallor Preeclampsia
Enlarged thyroid gland; tachycardia
V. PATHOLOGICAL CONSEQUENCES More than 80% of hydatidiform moles are benign (noncancerous). The outcome after treatment is usually excellent. Close follow-up is essential. After treatment, you should use very effective contraception for at least 6 to 12 months to avoid pregnancy. In some cases, hydatidiform moles may develop into invasive moles. These moles may grow so far into the uterine wall and cause bleeding or other complications. In a few cases, a hydatidiform mole may develop into a choriocarcinoma, a fast-growing cancerous form of gestational trophoblastic disease. Possible Complications Lung problems may occur after a D and C if the woman's uterus is bigger than 16 weeks gestational Other complications related to the surgery to remove a molar pregnancy include: Preeclampsia Thyroid problems VI. DIFFERENTIAL DIAGNOSIS A. Lab Studies
Quantitative beta-HCG: HCG levels greater than 100,000 mIU/mL indicate exuberant trophoblastic growth and raise suspicion that a molar pregnancy should be excluded. A molar pregnancy may have a normal HCG level. Uterine Pregnancy Test. Positive in high dilution. 1/200 is highly suggestive. 1/500 is surely diagnostic.In normal pregnancy, it is positive in dilution up to 1/100. Complete blood cell count with platelets: Anemia is a common medical complication, as is the development of a coagulopathy. Blood urea nitrogen (BUN) and creatinine studies. Positive if levels are increased. Thyroxin: Although women with molar pregnancies are usually clinically euthyroid, plasma thyroxin is usually elevated above the reference range for pregnancy. Hyperthyroidism may be the presenting symptom. B. Imaging Studies:
Ultrasonography It is the criterion standard for identifying both complete and partial molar pregnancies. The classic image, using older ultrasonographic technology, is of a snowstorm pattern indicating hydropic chorionic villi. High-resolution ultrasonography shows a complex intrauterine mass containing many small cysts (usually bilateral ovarian cysts). Chest Radiograph Once a molar pregnancy is diagnosed, a baseline chest radiograph should be taken. The lungs are a primary site of metastasis for malignant trophoblastic tumors. X-RAY of abdomen. The procedure reveals no fetal skeleton.
C.
Histological Findings:
Complete mole: Fetal tissue is absent, and severe srophoblastic proliferation, hydropic villi, and chromosomes 46,XX or 46,XY are present. Additionally, complete moles show overexpression of several growth factors, including c-myc, epidermal growth factor, and c-erb B-2, compared to normal placenta. Partial mole: Fetal tissue is often present as well as amnion and fetal red blood cells. Hydropic villi and trophoblastic proliferation are also observed.
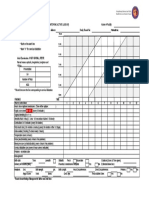
VII. MANIFESTATION AND SURVEILLANCE
A. Symptoms: 1. Amenorrhea 2. Exaggerated symptoms of pregnancy especially vomiting 3. Symptoms of preeclampsia that may be present as headache and edema. 4. Vaginal bleeding as the main complaint; due to the separation of vesicles from the uterine wall and there may be blood-stained, watery discharge (the watery part is from the ruptured vesicles) Prune juice-like discharge may occur brownish because it is retained for sometime inside the uterine cavity. Blood may be concealed in the uterus, thereby causing enlargement. 5. Abdominal pain: may be dull-aching due to rapid distension of uterine by mole or by concealed haemorrhage; colicky due to start of expulsion 6. Ovarian pain due to stretching of ovarian capsule or complication in the cystic ovary as torsion B. Signs: 1. Preeclampsia develops in 20 30 % cases, usually before 20 weeks AOG 2. Pallor indicating anemia may be present 3. Hyperthyroidism develops in 3-10% of cases manifested by enlarged thyroid gland and tachycardia (due to chorionic thyrotropin secreted by the trophoblast and hCG also has a thyroid-stimulating effect)
VIII. CLINICAL MANAGEMENT
A. Medical/Surgical Management: Medical Care:
Stabilize the patient. Transfuse for anemia. Correct any coagulopathy. Treat hypertension. Administration of Methotrexate. Some physicians give women who have had GTD a prophylactic course of this drug the drug of choice for choriocarcinoma. Because the drug interferes with WBC formation (Leukopenia), prophylactic use must be weighted carefully. If malignancy should occur, it can be treated effectively in most instances with Methotrexate at that time. (Methotrexate has the ability to dissolve fast-growing tissues). Administration of Dactinomycin. It is added to the regimen of Methotrexate if metastasis occurs. It is an antibiotic used as an antineoplastic agent prescribed in the treatment of a variety of malignant neoplastic diseases.
Surgical Care:
Evacuation of the uterus by dilation and curettage is always necessary. Suction curettage: a method of curettage in which a specimen of the endometrium or the products of conception are removed by aspiration. The procedure is done through general anesthesia, but not which relaxes the uterus as it may induce severe bleeding. A cannula is connected to a suction pump adjusted at negative pressure of 300-500 mmHg but depends according to the duration of the pregnancy. Prostaglandin or oxytocin induction is not recommended because of the increased risk of bleeding and malignant sequelae. Intravenous oxytocin should be started with the dilation of the cervix and continued postoperatively to reduce the likelihood of hemorrhage. Consideration of using other uterotonic formulations (eg, Methergine, Hemabate) is also warranted. Respiratory distress is often observed at the time of surgery. This may be due to trophoblastic embolization, high-output congestive heart failure caused by anemia, or iatrogenic fluid overload. Distress should be aggressively treated with assisted ventilation and monitoring, as required.
B. Nursing Management:
A gynecologic oncologist should be consulted if the patient is believed to be at risk for or has developed malignant disease. No special diet is required. Patients may resume activity as tolerated. Pelvic rest is recommended for 4-6 weeks after evacuation of the uterus, and the patient is instructed not to become pregnant for 12 months. Adequate contraception is recommended during this period. Monitor serial beta-HCG values to identify the rare patient who develops malignant disease. If a pregnancy does occur, the elevation in beta-HCG would be confused with development of malignant disease.
Further Outpatient Care:
Serial quantitative beta-HCG levels should be determined. Draw the first level 48 hours after evacuation and then every 2 weeks until the levels are within reference ranges. Levels should consistently drop and should never increase. Once levels have reached reference ranges, check them each month for a year. Any rise in levels should prompt a chest radiograph and pelvic examination to facilitate early detection of metastases. Contraception is recommended for 6 months to a year after evacuation. Patients with a prior complete or partial molar pregnancy have a 10-fold risk of a second mole in a future pregnancy. Work with the team to evaluate all future pregnancies early with ultrasonography.
Patient Education:
Because of the small but real potential for development of malignant disease and because these malignancies are absolutely curable, the importance of consistent follow-up care must be emphasized. The patient must avoid pregnancy for 1 year to avoid any confusion about the development of malignant disease. Effective contraception should be used. If a pregnancy occurs, the elevation in beta-HCG levels cannot be differentiated from the disease process. Future pregnancies should undergo early sonographic evaluation because of the increased risk of recurrence of a molar gestation.
IX. CONCEPTUAL MODELS AND FRAME WORKS (Theories Applied)
Interpersonal Model by Hildegard Peplau The main goal of this in caring for the patient is to educate to recognize and respond to need of help. Adaptation Theory by Sister Callista Roy Its goal is to help the person adapt to any changes in physiological needs, self-concept, role function and interdependent relations during health and illness Behavioral System Model by Dorothy Johnson Focuses on how the client adapts to illness; the goal of nursing is to reduse stress so that the client can move more easily through recovery.
X.
CASE SCENARIO
After my husband and I tried to get pregnant for 2 years exactly, I finally got a + test! It was so exciting. We told everyone after getting up off the ground from crying and praising God for the good news. Doctors didnt want to have me come in until 10 weeks. At 9.5 weeks, I began bleeding a very little bit with no pain. My mother came to take me to the ER but then it stopped so I didnt worry. We went out to eat and when we were leaving there, I went to the bathroom and I bled out like crazy and had INTENSE pain. Rushed to the ER and they couldnt find a fetus. It was almost like they thought I was lying about begin pregnant to begin with. I ended up being transferred to another hospital and had a D&C. We thought it was just a miscarriage until 4 weeks later when we went to an appointment and found out it was a_________. On one hand, it was horrible, because we now had to wait to try again, on top of having weekly blood work for who knows how long until the levels went down to zero. On the other hand, I sort of felt good that it was not a child that died, but rather a problem with conception that did not produce a fetus. We ended up trying 6 months later and got pregnant right away.
Potrebbero piacerti anche
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Ncam219 Lec PDFDocumento102 pagineNcam219 Lec PDFDAVE BARIBENessuna valutazione finora
- HIV Awareness and Family Planning SeminarDocumento3 pagineHIV Awareness and Family Planning SeminarRowena EboraNessuna valutazione finora
- Research ProposalDocumento32 pagineResearch Proposalku daarayNessuna valutazione finora
- What Makes People Gay?Documento9 pagineWhat Makes People Gay?Anthony McCartneyNessuna valutazione finora
- Biology Investigatory ProjectDocumento14 pagineBiology Investigatory Projectatharva surwaseNessuna valutazione finora
- OB GYN Mock Board QuestionnaireDocumento12 pagineOB GYN Mock Board QuestionnairejampogaottNessuna valutazione finora
- Leopold's ManeuverDocumento4 pagineLeopold's ManeuverDe Leon, Austine Sydney D.Nessuna valutazione finora
- Sociology of Kinship - Assignment (PROCREATION)Documento7 pagineSociology of Kinship - Assignment (PROCREATION)Mayank SinghNessuna valutazione finora
- Compartmental Model For Chlamydia, A Sexually Transmitted DiseaseDocumento22 pagineCompartmental Model For Chlamydia, A Sexually Transmitted DiseaseInstituto de Investigaciones InterdisciplinariasNessuna valutazione finora
- Antepartum Fetal Surveillance ACOG Bulletin 2014 PDFDocumento11 pagineAntepartum Fetal Surveillance ACOG Bulletin 2014 PDFDanNessuna valutazione finora
- Nursing Care of The Postpartum ClientDocumento13 pagineNursing Care of The Postpartum ClientLyca Mae AurelioNessuna valutazione finora
- MedITEX IVF v1 216 Releasenotes enDocumento12 pagineMedITEX IVF v1 216 Releasenotes enmichael_schindl6525Nessuna valutazione finora
- Legal Opinion For Tsi Ming ChoiDocumento2 pagineLegal Opinion For Tsi Ming ChoiJovan GasconNessuna valutazione finora
- 2 - PPT DR Liong Boy Kurniawan - Recent Update of Semen Analysis, LBK, KONAS 2022Documento34 pagine2 - PPT DR Liong Boy Kurniawan - Recent Update of Semen Analysis, LBK, KONAS 2022NANANessuna valutazione finora
- Hard Spelling Bee WordsDocumento8 pagineHard Spelling Bee WordsLee LedesmaNessuna valutazione finora
- PatriarchyDocumento1 paginaPatriarchyapi-374050745Nessuna valutazione finora
- Commed PPT (Deepthi)Documento22 pagineCommed PPT (Deepthi)Nivedha RajanNessuna valutazione finora
- AzezewDocumento48 pagineAzezewtemesgen AsmamawNessuna valutazione finora
- Sexual SelfDocumento23 pagineSexual SelfFerl Diane Siño100% (2)
- EC Information Board-FormDocumento1 paginaEC Information Board-FormSARAH MAE MARAVILLANessuna valutazione finora
- Partograph: (Use This Form For Monitoring Active Labour)Documento1 paginaPartograph: (Use This Form For Monitoring Active Labour)Omar Khalif Amad PendatunNessuna valutazione finora
- Impact of Female Education On Fertility Perspective BangladeshDocumento7 pagineImpact of Female Education On Fertility Perspective BangladeshBhudai123Nessuna valutazione finora
- Effectiveness of A Breastfeeding Self-Efficacy Intervention: Do Hospital Practices Make A Difference?Documento12 pagineEffectiveness of A Breastfeeding Self-Efficacy Intervention: Do Hospital Practices Make A Difference?cardenala haganinthaNessuna valutazione finora
- Ultrasound Examination in Obstetrics and GynecologyDocumento19 pagineUltrasound Examination in Obstetrics and GynecologyDian Putri NingsihNessuna valutazione finora
- ThesisDocumento5 pagineThesisJulia ConceNessuna valutazione finora
- Sigmund Freud'S Theory of Sexuality: Oral Stage (0-1 Year) : in The First Stage of Personality Development The Libido IsDocumento2 pagineSigmund Freud'S Theory of Sexuality: Oral Stage (0-1 Year) : in The First Stage of Personality Development The Libido IsLudovica Dettin100% (1)
- Thieme - Color Atlas of Pathophysiology (Silbernagl 2000)Documento2 pagineThieme - Color Atlas of Pathophysiology (Silbernagl 2000)Wirscka Gibran Muhammad LatukaisupyNessuna valutazione finora
- ARText 3 PDFDocumento32 pagineARText 3 PDFrakhi goyalNessuna valutazione finora
- Management of Abnormal Uterine Bleeding With Emphasis On Alternatives To HyterectomyDocumento16 pagineManagement of Abnormal Uterine Bleeding With Emphasis On Alternatives To HyterectomyEstefania gonzalez torresNessuna valutazione finora
- DLL Sci Q2 W2Documento12 pagineDLL Sci Q2 W2Raymund DelfinNessuna valutazione finora