Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
NCP PROPER Pain and Decreased Cardiac Output
Caricato da
Erienne Lae Manangan - CadalsoDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
NCP PROPER Pain and Decreased Cardiac Output
Caricato da
Erienne Lae Manangan - CadalsoCopyright:
Formati disponibili
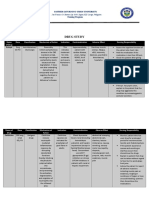
1.
ACUTE PAIN R/T TISSUE TRAUMA SECONDARY TO WOUND DEBRIDMENT SUBJECTIVE AND OBJECTIVE CUES S> Ang sakit ng tiyan ko! O> facial grimacing noted Aldrete score of 10 s/p wound exploration With dry and intact dressing Abdominal guarding noted Moaning noted Restlessness noted Vital signs of bp = 130/90mmhg; PR = 89bpm; RR = 23cpm; T = 35.8C Oriented to time, place, person and situation Medications taken were Ketorolac IV and Morphine sulphate 30ml for 10 mins EXPLANATION OF PROBLEM Last year the patient was confined due to rectal cancer and has undergone exploratory laparotomy for 2 times. Last week the patient had wound dehiscence so had undergone emergency wound exploration for debridement and suturing. After the procedure, the patient stayed in the RR and complained of pain in the abdominal area. OBJECTIVES STO: Within 8 hours of dependent and independent nursing interventions, the patient will: a. Verbalize pain is relieved with a pain scale of 0-4/10 b. Be able to sleep continuously for a minimum of 3 hours c. Demonstrate proper use of pain management techniques such as DBE and splinting LTO: After 72 hours of nursing intervention the patient will a. Verbalize pain is relived with a pain scale of 0/10 b. Demonstrate proper use of pain management techniques such as DBE and splinting c. Show no signs of infection such as abnormal drainage from wound, fever, redness NURSING INTERVENTIONS Independent 1. Monitor vital signs 2. Assess level of consciousness 3. Assess PQRST of pain RATIONALE Vital signs are usually altered in acute pain Pain can result in narrowed focus preventing the patient to assess the current situation Pain is a subjective experience and must be described by the client in order to plan effective treatment Indicate if there is an on-going infectious process Observations may or may not be congruent with verbal reports indicating need for further evaluation Noise may be a factor which can aggravated feeling of pain therefore should be minimized or eliminated DBE helps the body relax and contributes to pain relief by reducing muscle tension and anxiety To promote circulation and prevent tissue pressure To prevent fatigue EVALUATION STO: Objective partially met since the patient was able to sleep for 1 hour following pharmacologic treatment for pain Modification: Reassess PQRST of pain and Reinforce pain management techniques
4. Assess wound dressing and wound site 5. Observe for nonverbal cues of pain 6. Provide minimally stimulating environment 7. Encourage and assist client in deep breathing exercises 8. Encourage patient to turn gradually 9. Encourage adequate rest periods Dependent 1. Administer pain medications as ordered 2. Assist with laboratory or diagnostic procedures 3. Evaluate, with the patient and the health care team, the effectiveness of past pain control measures that have been used
Nursing Diagnosis: Acute pain related to tissue trauma
For faster relief of intolerable pain To identify underlying cause of pain
To make adjustments if necessary regarding the dosage and treatment of the patient
2. DECREASED CARDIAC OUTPUT R/T PLAQUE OCCLUSION SUBJECTIVE AND OBJECTIVE CUES O> Decreased Erythrocyte .33 (.37-.47); Decreased Hemoglobin 110 (120-170) as of 1/10/12 Electrolytes within normal range Oriented to time, place, person and situation With pale and cool skin With coughing episodes With vital signs of bp = 130/90mmhg; PR = 89bpm; RR = 23cpm; T = 35.8C With irregular pulse rhythm With cordarone drip x 24 hours Hooked to a cardiac monitor showing atrial fibrillation s/p wound debridement Restlessness noted With IFC and suprapubic catheter With 02sat of 70-80% at room air 90-100% with o2 therapy Nursing diagnosis: Decreased Cardiac Output R/T Plaque Occlusion EXPLANATION OF PROBLEM Due to the formation of fatty deposits in the walls of the blood vessels, the blood vessels narrowed decreasing blood flow. This decrease in blood flow creates high pressure causing the hypertension of the patient. Accompanied by decreased cardiac volume there is also decreased perfusion to myocardial muscles impairing the pumping ability of the heart hence produces signs and symptoms of dysrhythmia OBJECTIVES STO: Within 8 hours of nursing intervention the patient will display: a. BP= 120/80 mmhg b. PR = 60- 100 bpm regular rhythm c. Urinary output >30cc per hour d. RR=16-20 cpm regular e. Normal sinus rhythm f. O2sat of 90-100% LTO: After 72 hours of nursing intervention the patient will demonstrate: a. Increase in activity tolerance b. Stable vital signs as mentioned above c. No episodes of dysrhythmias d. Participate in activities that reduce workload of heart NURSING INTERVENTIONS Independent 1. Monitor vital signs 2. Review laboratory results and ECG results 3. Assess level of consciousness 4. Auscultate lung and heart sounds 5. Observe for chest pain or discomfort RATIONALE Indicate effectiveness of treatment and other underlying symptoms To note for any changes and make appropriate adjustments to treatment To note for possible oxygen insuffiency The new onset of a gallop rhythm, tachycardia, and fine crackles in lung bases can indicate onset of heart failure. Chest pain/discomfort is generally indicative of an inadequate blood supply to the heart, which can compromise cardiac output Monitor cardiac status and be prepared for other complications Decreased cardiac output results in decreased perfusion of the kidneys, with a resulting decrease in urine output. Elevating the head of the bed may decrease the work of breathing, and also decrease venous return and preload. Straining when defecating that results in the Valsalva maneuver can lead to dysrhythmia, decreased cardiac function, and sometimes death. Rest periods decrease oxygen consumption. EVALUATION STO: Objective partially met since patient was not able to ahieve a normal sinus rhythm within the shift and RR is 23cpm; PR is of irregular rhythm Modification: Continue interventions and monitoring
6. Maintain on cardiac monitoring 7. Monitor intake and output 8. Place client in semiFowler's position or position of comfort 9. Instruct patient not to do valsalva maneuver
10. Provide a restful environment by minimizing controllable stressors and unnecessary disturbances. 11. Weigh client at same time daily.
An accurate daily weight is a good indicator of fluid balance.
Dependent 1. Titrate inotropic and vasoactive medications within defined parameters to maintain contractility, preload, and afterload per physician's order. 2. Administer oxygen as needed per physician's order. 3. Gradually increase activity Serve small sodium1. restricted, lowcholesterol meals. 2. Administer blood or fluid replacement as ordered To ensure maintenance of a delicate balance of medications that stimulate the heart to increase contractility, maintaining adequate perfusion of the body.
Increase circulating oxygen in the body
Activity of the cardiac client should be closely monitored and should be gradual as not to overwork the heart Sodium-restricted diets help decrease fluid volume excess. Low-cholesterol diets help decrease atherosclerosis. Replace lost fluids and maintain cardiac output to normal
Potrebbero piacerti anche
- Meditech Quick Reference (With CPOE)Documento16 pagineMeditech Quick Reference (With CPOE)Felice 皓思 NgNessuna valutazione finora
- Cardiac Assessment ScenariosDocumento11 pagineCardiac Assessment ScenariosShaneNessuna valutazione finora
- Concept Map - Abby !Documento2 pagineConcept Map - Abby !Abegail Abaygar100% (3)
- Case Study PsychiatricDocumento29 pagineCase Study PsychiatricSimran Josan100% (3)
- NCP: DysrhythmiasDocumento12 pagineNCP: DysrhythmiasJavie100% (3)
- Pathophysiology of HCVD DM2 CVD Left Basal GangliaDocumento1 paginaPathophysiology of HCVD DM2 CVD Left Basal GangliaJake Caballo100% (1)
- NCP Pain HypertensionDocumento3 pagineNCP Pain HypertensionEzron Kendrick Duran50% (2)
- Decreased Cardiac OutputDocumento4 pagineDecreased Cardiac OutputChristine MatasNessuna valutazione finora
- NCP Ineffective TissueDocumento2 pagineNCP Ineffective TissueFhel AragonNessuna valutazione finora
- Nursing Care Plan: Pulmonary EbolismDocumento5 pagineNursing Care Plan: Pulmonary EbolismneuronurseNessuna valutazione finora
- SOMBILLO Scenario 1 ANGINADocumento2 pagineSOMBILLO Scenario 1 ANGINAKarla SombilloNessuna valutazione finora
- Assessment Needs Nursing Diagnos IS Goal/Obj Ective Intervention Rationale EvaluationDocumento10 pagineAssessment Needs Nursing Diagnos IS Goal/Obj Ective Intervention Rationale EvaluationApol Pen67% (3)
- Decreased Cardiac OutputDocumento9 pagineDecreased Cardiac OutputChinita Sangbaan75% (4)
- NCP For CoughDocumento6 pagineNCP For Coughmelerine16100% (5)
- West Visayas State University Ineffective Health MaintenanceDocumento1 paginaWest Visayas State University Ineffective Health Maintenancepircano100% (2)
- NCP For CTTDocumento1 paginaNCP For CTTJen Rhae LimNessuna valutazione finora
- Care Plan ExampleDocumento2 pagineCare Plan Exampleincess27100% (1)
- NCP Ineffective Airway Clearance Related To Presence of Secretion in Trachea-Bronchial Tree Secondary To History of CAPDocumento2 pagineNCP Ineffective Airway Clearance Related To Presence of Secretion in Trachea-Bronchial Tree Secondary To History of CAPpa3kmedina100% (1)
- Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective Short Term Short TermDocumento2 pagineAssessment Diagnosis Planning Intervention Rationale Evaluation Subjective Short Term Short TermFrancis Xavier S. MendezNessuna valutazione finora
- NCP - Acute PainDocumento1 paginaNCP - Acute PainjsthrNessuna valutazione finora
- Decreased Cardiac OutputDocumento4 pagineDecreased Cardiac OutputRenie SerranoNessuna valutazione finora
- Nursing Care PlanDocumento11 pagineNursing Care Planaycee0316100% (1)
- 66 Drug AnaDocumento3 pagine66 Drug AnaAlexa RoqueNessuna valutazione finora
- Nursing Care Plan 1 DiagDocumento4 pagineNursing Care Plan 1 Diagguysornngam100% (1)
- NCP - Hyperthermia - FEUNRMFDocumento5 pagineNCP - Hyperthermia - FEUNRMFJk SalvadorNessuna valutazione finora
- Nursing Care Plan: Date/ Time Assessment Nursing Diagnosis Planning Intervention Evaluatio NDocumento2 pagineNursing Care Plan: Date/ Time Assessment Nursing Diagnosis Planning Intervention Evaluatio NnananaNessuna valutazione finora
- NCP For SVTDocumento6 pagineNCP For SVTRen VillenaNessuna valutazione finora
- NCP Acute PainDocumento3 pagineNCP Acute PainNathalie kate petallarNessuna valutazione finora
- Drug Study: San Francisco St. Butuan City 8600, Region XIII Caraga, PhilippinesDocumento2 pagineDrug Study: San Francisco St. Butuan City 8600, Region XIII Caraga, PhilippinesNikki Caryl ZafraNessuna valutazione finora
- NCP For Mi PainDocumento2 pagineNCP For Mi PainKahMallariNessuna valutazione finora
- Rufino, Leslie Kriztel S. BSN 3-2 Group 1Documento6 pagineRufino, Leslie Kriztel S. BSN 3-2 Group 1Deinielle Magdangal RomeroNessuna valutazione finora
- NCP AidsDocumento16 pagineNCP AidstferdianingsihNessuna valutazione finora
- Geria NCPDocumento4 pagineGeria NCPBrylle CapiliNessuna valutazione finora
- San Francisco St. Butuan City 8600, Region XIII Caraga, PhilippinesDocumento3 pagineSan Francisco St. Butuan City 8600, Region XIII Caraga, Philippineskuro hanabusaNessuna valutazione finora
- NCP Ch31 p991-992Documento2 pagineNCP Ch31 p991-992Ala'a Abd Mansor100% (2)
- NCP - Ineffective Airway ClearanceDocumento4 pagineNCP - Ineffective Airway ClearanceKim Gabrielle Exene LeeNessuna valutazione finora
- Nursing Care Plan: Subjective DataDocumento4 pagineNursing Care Plan: Subjective DataAbdallah AlasalNessuna valutazione finora
- NCP DM and HCVDDocumento3 pagineNCP DM and HCVDMAYBELINE OBAOB100% (1)
- Aminogen Drug StudyDocumento2 pagineAminogen Drug Studymilesmin100% (1)
- NCP Micu Hascvd Cad - RioDocumento5 pagineNCP Micu Hascvd Cad - RioRio BonifacioNessuna valutazione finora
- DrugsDocumento7 pagineDrugsEloisa Abarintos RacalNessuna valutazione finora
- Nursing Care Plan: References: Nurse's Pocket Guide Pages 151-155Documento1 paginaNursing Care Plan: References: Nurse's Pocket Guide Pages 151-155Caroline ChaNessuna valutazione finora
- Hypertension Nursing Care PlanDocumento3 pagineHypertension Nursing Care PlanAsylla PajijiNessuna valutazione finora
- Tissue PerfusionDocumento2 pagineTissue PerfusionMichael John LeandichoNessuna valutazione finora
- Course Task CU 7Documento7 pagineCourse Task CU 7Kyla PamaNessuna valutazione finora
- Assessment Diagnosis Objectives of Care Intervention Rationale Evaluation Difficulty of Breathing (Rapid and Shallow)Documento1 paginaAssessment Diagnosis Objectives of Care Intervention Rationale Evaluation Difficulty of Breathing (Rapid and Shallow)Jamaica Leslie NovenoNessuna valutazione finora
- NCPDocumento2 pagineNCPJonathan LiscanoNessuna valutazione finora
- Glaucoma NCPDocumento4 pagineGlaucoma NCPChantal CaraganNessuna valutazione finora
- NCPDocumento3 pagineNCPArien CaleonNessuna valutazione finora
- NCPDocumento5 pagineNCPRose AnnNessuna valutazione finora
- 312 MR NathanielDocumento2 pagine312 MR NathanielCarl SantosNessuna valutazione finora
- Acc Phu Case NCP HyperthermiaDocumento1 paginaAcc Phu Case NCP Hyperthermiamacy_bautistaNessuna valutazione finora
- Hyperthermia Pneumonia Nursing Care PlanDocumento1 paginaHyperthermia Pneumonia Nursing Care Planjustin_saneNessuna valutazione finora
- Nueva Ecija University of Science and TechnologyDocumento7 pagineNueva Ecija University of Science and TechnologyKym RonquilloNessuna valutazione finora
- ANATOMY AND PHYSIOLOGY of RabiesDocumento5 pagineANATOMY AND PHYSIOLOGY of RabiesDavid CalaloNessuna valutazione finora
- Aspirin Drug SummDocumento2 pagineAspirin Drug SummWarren0% (1)
- NCP For CHF 3 Activity IntoleranceDocumento2 pagineNCP For CHF 3 Activity IntoleranceAngelyn ArdinesNessuna valutazione finora
- Nursing Measures To Maintain Normal Respiratory Function and OxygenationDocumento2 pagineNursing Measures To Maintain Normal Respiratory Function and Oxygenationlodeth100% (2)
- Nursing Care Plan: Assessment Diagnosis Planning Interventions Rationale EvaluationDocumento1 paginaNursing Care Plan: Assessment Diagnosis Planning Interventions Rationale EvaluationJhevilin RM100% (1)
- NCP 1Documento1 paginaNCP 1hsiriaNessuna valutazione finora
- Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Short Term Goal: IndependentDocumento4 pagineAssessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Short Term Goal: IndependentNinaNessuna valutazione finora
- Client Information Sheet (CIS)Documento10 pagineClient Information Sheet (CIS)Christine RombawaNessuna valutazione finora
- NCPDocumento22 pagineNCPMaricris S. Sampang100% (1)
- And Release of Pancreatic Enzyme: Which It Is A Process Whereby Pancreatic Enzymes Destroy Its Own Tissue Leading ToDocumento15 pagineAnd Release of Pancreatic Enzyme: Which It Is A Process Whereby Pancreatic Enzymes Destroy Its Own Tissue Leading ToAriane-Gay Cristobal DuranNessuna valutazione finora
- ASSESSMENT S: "Nanghihina Ako, Hindi Ko Magawa Yung Mga GustoDocumento1 paginaASSESSMENT S: "Nanghihina Ako, Hindi Ko Magawa Yung Mga GustoCherie MayNessuna valutazione finora
- Operating Caregiving Equipment, Tools and ParaphernaliaDocumento57 pagineOperating Caregiving Equipment, Tools and ParaphernaliaAngie FillerNessuna valutazione finora
- Fourth Semester FinalDocumento14 pagineFourth Semester Finalmara5140Nessuna valutazione finora
- A Validation Study of Maternal Early Warning Systems: A Retrospective Cohort StudyDocumento9 pagineA Validation Study of Maternal Early Warning Systems: A Retrospective Cohort StudyLivianadrNessuna valutazione finora
- CTP DR 2Documento38 pagineCTP DR 2Dharyl JoshuaNessuna valutazione finora
- 50items Funda Part 1Documento52 pagine50items Funda Part 1clobregas100% (3)
- Vital SIgns - First Responder - August 2013 - v2.3Documento18 pagineVital SIgns - First Responder - August 2013 - v2.3Rayan JaafeerNessuna valutazione finora
- CASE REPORT Hipokalemia HipokalsemiaDocumento24 pagineCASE REPORT Hipokalemia HipokalsemiaRaraNessuna valutazione finora
- FundaDocumento81 pagineFundaKaye CorNessuna valutazione finora
- RPN Priority and Delegation TestDocumento5 pagineRPN Priority and Delegation Testdaljit chahalNessuna valutazione finora
- SOP StandardsDocumento18 pagineSOP StandardsTrue GeminiNessuna valutazione finora
- Physical AssessmentDocumento3 paginePhysical AssessmentKristine Anne SorianoNessuna valutazione finora
- Lesson 1 Use Tools Equipment Paraphernalia in CaregivingDocumento47 pagineLesson 1 Use Tools Equipment Paraphernalia in CaregivingÊirene Ballon100% (1)
- Mastitis Group 5Documento14 pagineMastitis Group 5Michael Barfi OwusuNessuna valutazione finora
- Department of Education: Republic of The PhilippinesDocumento2 pagineDepartment of Education: Republic of The PhilippinesDM Riel100% (1)
- Unit 1 Taking Vital SignsDocumento4 pagineUnit 1 Taking Vital SignsPhopo SandyNessuna valutazione finora
- Covid 19 Batch 5 TMSDocumento860 pagineCovid 19 Batch 5 TMSMohamad Mosallam AyoubNessuna valutazione finora
- Vital Signs PDFDocumento2 pagineVital Signs PDFsaguliteNessuna valutazione finora
- Nursing Care Plan (NCP)Documento3 pagineNursing Care Plan (NCP)Sha PinedaNessuna valutazione finora
- Implementation and Intervension (English)Documento9 pagineImplementation and Intervension (English)Devi SitudewiNessuna valutazione finora
- Vital Signs NotesDocumento3 pagineVital Signs NotesJoelyn Noble CabalatunganNessuna valutazione finora
- Casmed 740 - Service ManualDocumento148 pagineCasmed 740 - Service ManualuunrealNessuna valutazione finora
- QP HSS-Q2701 Dialysis-TechnicianDocumento100 pagineQP HSS-Q2701 Dialysis-TechnicianSantanu MunshiNessuna valutazione finora
- Impaired Physical MobilityDocumento2 pagineImpaired Physical MobilityNicole Genevie MallariNessuna valutazione finora
- Syl Lab Us Basic BSC NursingDocumento110 pagineSyl Lab Us Basic BSC NursingFabin JoseNessuna valutazione finora
- Reading Exercise For Ayuni's ClassDocumento8 pagineReading Exercise For Ayuni's ClassLismy NurhamzahNessuna valutazione finora