Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Arthroscopically Guided Osteotomy
Caricato da
Comunicación PiñalCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Arthroscopically Guided Osteotomy
Caricato da
Comunicación PiñalCopyright:
Formati disponibili
SCIENTIFIC ARTICLE
Arthroscopically Guided Osteotomy for Management of Intra-Articular Distal Radius Malunions
Francisco del Pial, MD, PhD, Leopoldo Cagigal, MD, Francisco J. Garca-Bernal, MD, PhD, Alexis Studer, MD, Javier Regalado, MD, Carlos Thams, MD
Purpose A malunion with a step-off of 1 mm or more after an intra-articular distal radius fracture may cause pain and arthritic changes at midterm follow-up. We present our technique for treating intra-articular distal radius malunions by carrying out an osteotomy from inside the joint outward under arthroscopic guidance using the dry arthroscopy technique, with emphasis on the clinical and radiologic outcomes. Methods We performed surgery on 11 patients for intra-articular malunion of the distal radius 1 to 5 months after the injury. Preoperative step-offs ranged from 2 to 5 mm (average, 2.5 mm) on plain radiographs. Original fracture patterns involved 1 radial styloid fracture, 1 radiocarpal fracture dislocation, and 9 comminuted intra-articular fractures. In 5 cases an anterior-ulnar or radial styloid fragment was repositioned. In the rest, more than 1 fragment (up to 3) was osteotomized. In 1 patient the articular osteotomy was combined with an ulnar shortening osteotomy. Results Follow-up ranged from 12 to 48 months. Step-offs were reduced in most cases to 0 mm; however, localized gaps ( 2 mm) and cartilage defects were commonly seen intraoperatively because the fragments did not accurately t. According to the Gartland and Werley score, there were 4 excellent and 7 good results (mean score of 2.8). The Modied Green and OBrien system achieved a mean score of 83, with 3 excellent, 5 good, and 3 fair results. One patient showed radiolunate narrowing on follow-up radiographs. Conclusions Arthroscopically assisted osteotomy permits direct visualization of the osteotomy site with good midterm clinical and radiologic outcomes. The technique can be used in irregularly dened fragments. (J Hand Surg 2010;35A:392397. 2010 Published by Elsevier Inc. on behalf of the American Society for Surgery of the Hand.) Type of study/level of evidence Therapeutic IV. Key words Wrist arthroscopy, radius malunion, distal radius osteotomy, dry arthroscopy.
degenerative arthritis may be expected when anatomical reduction is not achieved after distal radius fractures.13 Several authors have pointed out that the goal is anatomical reduction, or at worst a step-off of less than 1 mm.46
NFAVORABLE RESULTS AND From the Instituto de Ciruga Plstica y de la Mano, Private Practice and Hospital Mutua Montaesa, Santander, Spain. Received for publication July 24, 2009; accepted in revised form December 1, 2009. No benets in any form have been received or will be received related directly or indirectly to the subject of this article. Corresponding author: Francisco del Pial, MD, PhD, Caldern de la Barca 16-entlo, E-39002 Santander, Spain; e-mail: drpinal@drpinal.com. 0363-5023/10/35A03-0005$36.00/0 doi:10.1016/j.jhsa.2009.12.001
Management of the young and/or active patient with a step-off after a malunited distal radius fracture includes intra-articular osteotomy, which is nonetheless hampered by limited vision. For volar shearing type malunions, the joint is approached volarly, the external callus is removed, and the osteotomy is directed toward the joint, with the intent that the osteotome follows the original fracture line.79 For other types of intra-articular malunion, the approach is through a dorsal capsular window.812 Fernndez10 considered this technique appropriate only for single line fractures, whereas others8,12 used it for the more complex 4-part fracture congurations. We investigated the possibility of direct arthroscopic manipulation of the displaced fragments by working
392 Published by Elsevier, Inc. on behalf of the ASSH.
INSIDE-OUT OSTEOTOMY FOR RADIUS MALUNIONS
393
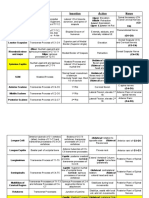
TABLE 1.
Case 1 2 3 4 5 6 7 8 9 10 11
Demographics
Age 46 32 42 45 45 25 49 32 27 61 53 Gender M W M M M M M M M M W Dominance D ND ND D ND D D D ND D D Fracture AO C.3.1 C.3.1 C.3.1 B.1.1 C.3.1 C.3.1 C.3.1 C.3.1 B.2.3 C.3.1 C.3.1 Delay (wk) 5 12 4 5 11 7 4 12 21 12 13 Previous Treatment Cast K-wire Cast Cast K-wire Volar plate External xator Cast K-wire K-wire K-wire external xator external xator
D, Dominant side; ND, Non-dominant side.
inside the joint.13 We found that the dry procedure without uid distension of the joint is preferable.14 In our previous report we showed that the technique was feasible; in this report, we present results of this surgery. The purpose of this retrospective study was to assess the clinical and radiographic outcomes in the management of intra-articular distal radius malunions with an arthroscopically assisted osteotomy. MATERIALS AND METHODS From 2004 to June 2008, we operated on 11 consecutive patients with intra-articular distal radius impacted fractures or malunions with an articular step-off of 2 mm or more measured on plain x-rays using an arthroscopically assisted osteotomy technique.13 Patients were observeded for at least 12 months after the surgery (mean, 32 mo; range, 12 48 mo) (Table 1). There were 9 men and 2 women with a mean age of 42 years (range, 25 61 y). All except 1 (case 8) occurred under workers compensation coverage. Four patients were involved in heavy work; all the rest were performing less demanding manual activities. The dominant hand was affected 7 times. One had a radial styloid fracture, 1 a volar radiocarpal fracturedislocation, and the rest different types of comminuted intra-articular fractures (C31 of the AO classication).15 Two of the authors measured step-offs and gaps in millimeters with a metric ruler on preoperative plain radiographs. The most displaced fragment was used as a reference when several fragments were involved. Preoperative step-offs ranged from 2 to 5 mm (average, 2.5 mm). Gaps varied from 0 to 3 mm (average, 0.73 mm).
Time from the original injury to surgery was 9.6 weeks on average (range, 4 21 wk). All patients had been managed initially elsewhere. Original treatment consisted of closed reduction and cast immobilization in 4 patients, K-wires and cast in 3 patients, closed reduction and external xator in 1 patient; K-wire and external xator in 2 patients, and a volar locking plate in 1 patient. Immobilization time ranged from 4 to 6 weeks, except in the patient with the plate (number 6), who started therapy immediately after the surgery. The technique of osteotomy has been described previously (Fig. 1).13,14 An arthroscopic arthrolysis is rst carried out to create working space, as the joint is scarred and unyielding. To cut the bone, we used a shoulder periosteal elevator (of 15 and 30 angles; Arthrex AR-1342-30 and AR-1342-15; Arthrex, Naples, FL) and also straight and curved osteotomes (Arthrex AR-1770 and AR-1771). Instruments with different angles were required. To avoid damaging the cartilage or cutting the extensor tendons, the osteotome should have a double 90 twist on its way to the joint cavity. First, it was introduced horizontally in the direction of the skin incision, then it was twisted 90 in the subcutaneous tissue to avoid the extensor tendons, and nally it was rotated again inside the joint itself. Stabilization of the fragments was carried out with volar locking plates when several fragments were mobilized; screws or buttressing plates were used when only one fragment needed to be addressed. Evaluation The patients were seen at varying intervals until discharge by the treating surgeon. For the purpose of this study, they
JHS Vol A, March
394
INSIDE-OUT OSTEOTOMY FOR RADIUS MALUNIONS
FIGURE 1: Correction of a straight line malunion in the scaphoid fossa with a simple straight osteotomy. A The probe (2 mm wide) is sitting on top of the depressed fragment to gauge the deformity. B The osteotome introduced from the 3-4 portal is cutting the malunited scaphoid fossa fragment. C Notice correction of the step-off at the end of the surgery.
TABLE 2.
Radiology
Volar Angulation () Before 4 0 2 8 dorsal 12 4 25 dorsal 10 12 10 After 1.5 0 0 0 2 dorsal 11 4 5 7 3 2 dorsal Radial Length (mm) Before 12 12 10 16 11 12 10 5 7 16 12 After 14 10 12 14 14 11 10 12 10 12 10 Ulnar Variance (mm) Before 1 5 3 1 2 2 0 2 2 5 5 After 1 3 0 1 1 0 0 2 2 0 2 Contralateral 1 3 0 0 0 1 1 0 2 1 3 Articular Steps (mm) Before 2 3 2 2 2 2 2 3 2 5 3 After 0 0 0 0 0 0 0 0 0 0 0 Articular Gaps (mm) Before 1 0 2 0 0 3 1 0 1 0 0 After 0 0 1 0 0 1 1 0 0 1 0
Radial Inclination () Case 1 2 3 4 5 6 7 8 9 10 11 Before 18 25 12 27 20 23 18 9 20 36 24 After 21.5 20 23 25 12 22 22 20 18 20 14
Mobilized Fragments 2 1 3 1 3 2 3 3 1 1 1
were called back and examined by 1 of the authors. Motion and grip strength were recorded, posteroanterior and lateral radiographs were taken, and a nal rating was assigned according to the system of Gartland and Werley16 and the Mayo modication of the system of Green and OBrien.17 A Disabilities of the Arm, Shoulder, and Hand questionnaire was administered. Two of the authors measured the nal alignment on posteroanterior and lateral radiographs, characterized by radial tilt, volar inclination, ulnar variance, and the maximum articular step-off or gap. Radiographic signs of arthrosis were rated according to the system of Knirk and Jupiter.1 In this classication, 0 is given when no sign of arthrosis exists; 1 when there is some joint space narrowing; 2 when there is marked narrowing or osteophyte formation; and 3 when there is bone-on-bone contact. We performed statistical evaluation with SPSS Statistics 17.0 software (SPSS, Cary, NC). We used paired t-test to compare preoperative and postoperative radiographic measurements. The condence interval of the difference was set at 95%.
RESULTS Patients were observed for a minimum of 12 months (range, 12 48 mo). An average of 1.9 fragments (range, 13 fragments) needed to be mobilized (Table 2). All the osteotomies were healed without radiographic evidence of osteonecrosis. Cases 4 and 9 only had a fragment that involved the scaphoid and the lunate fossa, respectively, which needed to be mobilized. In 3 patients (cases 2, 10, and 11) who had sustained a C31 fracture, only 1 fragment was mobilized. The radial shortening in these cases was treated by a concomitant open ulna shortening in 1 case (number 11), or accepted in the other 2 as the residual shortening was less than 2 mm (Fig. 2). In the rest, the joint was distorted after C31 fractures and several fragments were cut and repositioned. The arthroscopy did not reveal any major intracarpal or radioulnar ligamentous derangement. Synovitis and partial tears were debrided at the time of the arthrolysis.
JHS Vol A, March
INSIDE-OUT OSTEOTOMY FOR RADIUS MALUNIONS
395
FIGURE 2: AC This C31 fracture resulted in a relatively well-aligned, albeit incongruent, radius at the lunate and sigmoid fossae (patient 2). Despite the confusing markings in B concerning the ulnar variance depicted by her original surgeon, the axial shortening was approximately 3 mm compared with the healthy side. D Only the anterior-ulnar fragment was osteotomized.
Step-offs were completely corrected in all patients, and gaps were not evident on follow-up radiograms. However, from the intraoperative arthroscopic ndings, most patients had gaps and/or chondral defects, rarely more than 2 mm, in isolated spots. The average radial inclination changed from 21 preoperatively to 20 postoperatively, and the volar angulation from an average of 1 to 3. Ulnar variance improved on average 2 mm from the preoperative status, whereas there was a difference of 0.7 mm in relation to the normal side (Table 2). Apart from the correction of the step-offs, there were no signicant differences between preoperative and postoperative radiological parameters except for ulnar variance (p .008). The nal range of motion averaged 59 (range, 45 to 74) of wrist extension; 54 (range, 40 to 68) of wrist exion; 18 (range, 8 to 28) of radial deviation; 38 (range, 25 to 50 of ulnar deviation); 80 (range 50 to 90) of pronation; and 82 (range, 45 to 90) of supination. Grip strength was on average 85% of the contralateral side (range, 78% to 100%) (Table 3). The average score according to the system of Gartland and Werley was 2.8 points (range, 0 5 points). According to the modication of the system of Green and OBrien, the average score was 83 points (range, 75100 points). Finally, the average score on the Dis-
abilities of the Arm, Shoulder, and Hand questionnaire was 7.6 (range, 0 34). According to the classication of Knirk and Jupiter,1 5 patients showed no changes, 5 had slight changes, and 1 (patient 6) had grade 2 changes (mean 0.6) (Table 3). All returned to their previous employment and occupations at an average of 13 weeks (range, 6 20 wk). DISCUSSION Arthroscopic intra-articular osteotomy is more complicated than the repair of a simple distal radius fracture. In addition to technical challenges, the joint is scarred, requiring a preliminary arthrolysis. The assistance of another experienced surgeon is invaluable, as the surgery should be kept ideally under a tourniquet time of less than 2 hours. In early malunions the procedure is carried out as presented in the surgical technique: rst placement of a plate and then the arthroscopy.13 For late presenting malunions (more than 3 months old) or in cases in which a high suspicion of carpal ligament injury exists, the approach is reversed. In these cases, we recommend an initial exploratory arthroscopy to assess the quality of the articular cartilage and the integrity of the liga-
JHS Vol A, March
396
INSIDE-OUT OSTEOTOMY FOR RADIUS MALUNIONS
TABLE 3.
Case 1 2 3 4 5 6 7 8 9 10 11
Outcomes
Flex/Exten/RD/UD/Pron/Sup () 68/68/28/40/90/90 65/60/18/40/75/90 59/52/22/42/90/90 60/74/25/60/90/90 40/65/15/30/90/45 45/55/22/30/60/90 55/55/15/45/90/80 60/60/15/40/50/85 40/60/17/36/80/75 45/45/08/35/80/80 55/55/18/25/80/85 Grip Strength (%) 100 84 78 93 85 78 88 87 82 86 79 Gartland and Werley 0 1 2 0 3 4 4 4 4 5 4 Modied Green and OBrien 100 90 80 90 80 75 75 85 80 75 80 DASH 0 0 3 1 1 10 10 5 9 34 11 Knirk and Jupiter 1 0 0 0 1 2 1 0 1 1 0
Follow-up (mo) 48 47 44 44 33 29 28 28 20 19 12
DASH, Disabilities of the Arm, Shoulder, and Hand questionnaire; Flex/Exten/RD/UD/Pron/Sup, exion/extension/radial deviation/ulnar deviation/pronation/supination.
FIGURE 3: Correction of a complex malunion. The scope is in the 6-R portal looking radially, whereas the instruments are coming from the 3-4 portal in a left wrist. The asterisks mark the same spots before and after the osteotomy in the lunate fossa. Notice that although step-offs have been leveled, gaps (highlighted by the lines) are unavoidable in old malunions (compare this with reduction obtained in a young malunion in Fig. 1). A Pre-reduction. B After reduction.
ments. If local conditions allow the osteotomy to be carried out, the hand is released from traction and the surgery proceeds as referred to above. The arthroscopic-guided osteotomy is not devised to deal with articular malunions in which major loss of cartilage on the radius surface itself or on the opposing carpals is detected during the arthroscopy. Our functional results are good compared with the prospect of malunited fractures,13,5 but far from a normal wrist. Although our outcomes are slightly better than those of Ring et al,8 who used an open osteotomy
technique, the meaning of those differences is difcult to interpret. A strong argument favoring carrying out the osteotomy as soon as possible is the fact that although stepoffs can be accurately corrected, even in old cases, residual gaps of about 1 mm (at times even more) are unavoidable in fractures seen late (Fig. 3). Limitations of our study include its retrospective nature and the short length of follow-up (mean, 32 mo). A long-term follow-up, prospective clinical study would be benecial for evaluating the outcomes of this
JHS Vol A, March
INSIDE-OUT OSTEOTOMY FOR RADIUS MALUNIONS
397
procedure. It is possible that with longer follow-up, further problems such as arthritic changes in the radiocarpal or distal radioulnar joint would appear to worsen the results. Furthermore, considerable arthroscopic expertise is required to perform the procedure because there is minimal working space and orientation is difcult. It is important to understand the intricacies of the dry technique14,18 to carry out the procedure in a safe and efcient manner. Any accomplished arthroscopist should not have any undue difculty incorporating the dry technique, but experience is required before the arthroscopist attempts to perform a complex osteotomy case. Only postoperative radiographic measurements were reported and compared in this study. Postoperative computed tomography scan or a second-look arthroscopy would have provided potentially more accurate data. REFERENCES
1. Knirk JL, Jupiter JB. Intra-articular fractures of the distal end of the radius in young adults. J Bone Joint Surg 1986;68A:647 659. 2. Bradway JK, Amadio PC, Cooney WP. Open reduction and internal xation of displaced, comminuted intra-articular fractures of the distal end of the radius. J Bone Joint Surg 1989;71A:839 847. 3. Catalano LW III, Cole RJ, Gelberman RH, Evanoff BA, Gilula LA, Borrelli J Jr. Displaced intra-articular fractures of the distal aspect of the radius: long-term results in young adults after open reduction and internal xation. J Bone Joint Surg 1997;79A:1290 1302. 4. Fernandez DL, Geissler WB. Treatment of displaced articular fractures of the radius. J Hand Surg 1991;16A:375384. 5. Trumble TE, Schmitt SR, Vedder NB. Factors affecting functional outcome of displaced intra-articular distal radius fractures. J Hand Surg 1994;19A:325340.
6. Doi K, Hattori Y, Otsuka K, Abe Y, Yamamoto H. Intra-articular fractures of the distal aspect of the radius: arthroscopically assisted reduction compared with open reduction and internal xation. J Bone Joint Surg 1999;81A:10931110. 7. Thivaios GC, McKee MD. Sliding osteotomy for deformity correction following malunion of volarly displaced distal radial fractures. J Orthop Trauma 2003;17:326 333. 8. Ring D, Prommersberger KJ, Gonzlez del Pino J, Capomassi M, Slullitel M, Jupiter JB. Corrective osteotomy for intra-articular malunion of the distal part of the radius. J Bone Joint Surg 2005;87A:15031509. 9. Prommersberger KJ, Ring D, del Pino JG, Capomassi M, Slullitel M, Jupiter JB. Corrective osteotomy for intra-articular malunion of the distal part of the radius: surgical technique. J Bone Joint Surg 2006; 88A(Suppl 1):202211. 10. Fernandez DL. Reconstructive procedures for malunion and traumatic arthritis. Orthop Clin North Am 1993;24:341363. 11. Saffar P. Treatment of distal radial intra-articular malunions. In: Saffar PH, Cooney WP III, eds. Fractures of the distal radius. London: Martin Dunitz, 1995:249 258. 12. Gonzlez del Pino J, Nagy L, Gonzlez Hernandez E, Bartolome del Valle E. [Intraarticular osteotomies for complex malunited fractures: Indications and surgical technique.] Rev Ortop Traumatol 2000;44: 406 417. 13. del Pial F, Garca-Bernal FJ, Delgado J, Sanmartn M, Regalado J, Cerezal L. Correction of malunited intra-articular distal radius fractures with an inside-out osteotomy technique. J Hand Surg 2006; 31A:1029 1034. 14. del Pial F, Garca-Bernal FJ, Pisani D, Regalado J, Ayala H, Studer A. Dry arthroscopy of the wrist: surgical technique. J Hand Surg 2007;32A:119 123. 15. Muller ME, Nazarian S, Koch P, Schaftzken J. The comprehensive classication of fractures of long bones. New York: Springer, 1990: 54 63. 16. Gartland JJ Jr, Werley CW. Evaluation of healed Colles fractures. J Bone Joint Surg 1951;33A:895907. 17. Cooney WP, Bussey R, Dobyns JH, Linscheid RL. Difcult wrist fractures: perilunate fracture-dislocations of the wrist. Clin Orthop Relat Res 1987;214:136 147. 18. del Pial F. Dry arthroscopy of the wrist: its role in the management of articular distal radius fractures. Scand J Surg 2008;97:298 304.
JHS Vol A, March
Potrebbero piacerti anche
- Sagittal Rotational Malunions of The Distal Radius: The Role of Pure Derotational Osteotomy (2009)Documento6 pagineSagittal Rotational Malunions of The Distal Radius: The Role of Pure Derotational Osteotomy (2009)Comunicación PiñalNessuna valutazione finora
- Reconstruction of The Ulnar Head With A Vascularized Second Metatarsal Head: Case ReportDocumento6 pagineReconstruction of The Ulnar Head With A Vascularized Second Metatarsal Head: Case ReportComunicación PiñalNessuna valutazione finora
- Technical Tips For (Dry) Arthroscopic Reduction and Internal Fixation of Distal Radius FracturesDocumento12 pagineTechnical Tips For (Dry) Arthroscopic Reduction and Internal Fixation of Distal Radius FracturesComunicación PiñalNessuna valutazione finora
- Dry Arthroscopy and Its ApplicationsDocumento11 pagineDry Arthroscopy and Its ApplicationsComunicación PiñalNessuna valutazione finora
- Acute Hand Compartment Syndromes After Closed Crush: A ReappraisalDocumento8 pagineAcute Hand Compartment Syndromes After Closed Crush: A ReappraisalComunicación PiñalNessuna valutazione finora
- The Deep Venous System and Reverse Flow FlapsDocumento13 pagineThe Deep Venous System and Reverse Flow FlapsComunicación PiñalNessuna valutazione finora
- Piñal Opera A Rebeldes LibiosDocumento1 paginaPiñal Opera A Rebeldes LibiosComunicación PiñalNessuna valutazione finora
- Sigmoid Notch Reconstruction and Limited Carpal Arthrodesis For A Severely Comminuted Distal Radius Malunion: Case ReportDocumento5 pagineSigmoid Notch Reconstruction and Limited Carpal Arthrodesis For A Severely Comminuted Distal Radius Malunion: Case ReportComunicación PiñalNessuna valutazione finora
- An All-Inside Technique For Arthroscopic Suturing of The Volar Scapholunate LigamentDocumento3 pagineAn All-Inside Technique For Arthroscopic Suturing of The Volar Scapholunate LigamentComunicación PiñalNessuna valutazione finora
- A Technique For Arthroscopic All-Inside Suturing in The WristDocumento5 pagineA Technique For Arthroscopic All-Inside Suturing in The WristComunicación PiñalNessuna valutazione finora
- Treatment of Nonunion of The Scaphoid by A Limited Combined ApproachDocumento5 pagineTreatment of Nonunion of The Scaphoid by A Limited Combined ApproachComunicación PiñalNessuna valutazione finora
- Minimizing Impairment in Laborers With Finger Losses Distal To The Proximal Interphalangeal Joint by Second Toe TransferDocumento12 pagineMinimizing Impairment in Laborers With Finger Losses Distal To The Proximal Interphalangeal Joint by Second Toe TransferComunicación PiñalNessuna valutazione finora
- The Venous Drainage of Nerves Anatomical Study and Clinical ImplicationsDocumento10 pagineThe Venous Drainage of Nerves Anatomical Study and Clinical ImplicationsComunicación PiñalNessuna valutazione finora
- Extensor Digitorum Brevis Free Flap: Anatomic Study and Further Clinical ApplicationsDocumento10 pagineExtensor Digitorum Brevis Free Flap: Anatomic Study and Further Clinical ApplicationsComunicación PiñalNessuna valutazione finora
- A Technique To Preserve The Shape of The Calcaneus After Massive OsteomyelitisDocumento3 pagineA Technique To Preserve The Shape of The Calcaneus After Massive OsteomyelitisComunicación PiñalNessuna valutazione finora
- Is Posttraumatic First Web Contracture Avoidable? Prophylactic Guidelines and Treatment-Oriented ClassificationDocumento6 pagineIs Posttraumatic First Web Contracture Avoidable? Prophylactic Guidelines and Treatment-Oriented ClassificationComunicación PiñalNessuna valutazione finora
- Results of Osteotomy, Open Reduction, and Internal Fixation For Late-Presenting Malunited Intra-Articular Fractures of The Base of The Middle PhalanxDocumento14 pagineResults of Osteotomy, Open Reduction, and Internal Fixation For Late-Presenting Malunited Intra-Articular Fractures of The Base of The Middle PhalanxComunicación PiñalNessuna valutazione finora
- The Indications For Toe Transfer After "Minor" Finger InjuriesDocumento10 pagineThe Indications For Toe Transfer After "Minor" Finger InjuriesComunicación PiñalNessuna valutazione finora
- Overcoming Soft-Tissue Deficiency in Toe-to-Hand Transfer Using A Dorsalis Pedis Fasciosubcutaneous Toe Free Flap: Surgical TechniqueDocumento9 pagineOvercoming Soft-Tissue Deficiency in Toe-to-Hand Transfer Using A Dorsalis Pedis Fasciosubcutaneous Toe Free Flap: Surgical TechniqueComunicación PiñalNessuna valutazione finora
- Massive Hand Crush: The Role of A Free Muscle Flap To Obliterate The Death Space and To Clear Deep InfectionDocumento5 pagineMassive Hand Crush: The Role of A Free Muscle Flap To Obliterate The Death Space and To Clear Deep InfectionComunicación PiñalNessuna valutazione finora
- Vascularized Bone Blocks From The Toe Phalanx To Solve Complex Intercalated Defects in The FingersDocumento8 pagineVascularized Bone Blocks From The Toe Phalanx To Solve Complex Intercalated Defects in The FingersComunicación PiñalNessuna valutazione finora
- Reconstruction of The Distal Radius Facet by A Free Vascularized Osteochondral Autograft: Anatomic Study and Report of A PatientDocumento14 pagineReconstruction of The Distal Radius Facet by A Free Vascularized Osteochondral Autograft: Anatomic Study and Report of A PatientComunicación PiñalNessuna valutazione finora
- Dry Arthroscopy of The Wrist: Surgical TechniqueDocumento5 pagineDry Arthroscopy of The Wrist: Surgical TechniqueComunicación PiñalNessuna valutazione finora
- Correction of Malunited Intra-Articular Distal Radius Fractures With An Inside-Out Osteotomy TechniqueDocumento6 pagineCorrection of Malunited Intra-Articular Distal Radius Fractures With An Inside-Out Osteotomy TechniqueComunicación PiñalNessuna valutazione finora
- Super-Thinned Iliac Flap For Major Defects On The Elbow and Wrist Flexion CreasesDocumento6 pagineSuper-Thinned Iliac Flap For Major Defects On The Elbow and Wrist Flexion CreasesComunicación PiñalNessuna valutazione finora
- Evolving Concepts in The Management of The Bone Gap in The Upper Limb. Long and Small DefectsDocumento17 pagineEvolving Concepts in The Management of The Bone Gap in The Upper Limb. Long and Small DefectsComunicación PiñalNessuna valutazione finora
- The Tibial Second Toe Vascularized Neurocutaneous Free Flap For Major Digital Nerve DefectsDocumento9 pagineThe Tibial Second Toe Vascularized Neurocutaneous Free Flap For Major Digital Nerve DefectsComunicación PiñalNessuna valutazione finora
- Improving Foot Appearance After Trimmed Toe or Hallux HarvestingDocumento5 pagineImproving Foot Appearance After Trimmed Toe or Hallux HarvestingComunicación PiñalNessuna valutazione finora
- Dry Arthroscopy of The Wrist: Its Role in The Management of Articular Distal Radius FractureDocumento7 pagineDry Arthroscopy of The Wrist: Its Role in The Management of Articular Distal Radius FractureComunicación PiñalNessuna valutazione finora
- Ischemic Toe Encountered During Harvesting: Report of 6 CasesDocumento6 pagineIschemic Toe Encountered During Harvesting: Report of 6 CasesComunicación PiñalNessuna valutazione finora
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5783)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (72)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (119)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Chiropractic Adjusting TechniqueDocumento111 pagineChiropractic Adjusting TechniqueDavid CristanchoNessuna valutazione finora
- PostureDocumento85 paginePostureDr.Debanjan Mondal (pt)100% (1)
- Kapha Yoga PosesDocumento33 pagineKapha Yoga PosesMarifé Cepeda CastroNessuna valutazione finora
- 3.arthrology 2010 NewDocumento25 pagine3.arthrology 2010 Newbenq373Nessuna valutazione finora
- Upper Limb RadiographyDocumento122 pagineUpper Limb RadiographyBright KapambalalaNessuna valutazione finora
- Groin StrainDocumento3 pagineGroin StrainTinaNessuna valutazione finora
- Pilates Exercises For Pregnant Women PDFDocumento5 paginePilates Exercises For Pregnant Women PDFDevina EkaraniNessuna valutazione finora
- Hatha Yoga: List of IllustrationsDocumento239 pagineHatha Yoga: List of IllustrationsEric Chambers100% (1)
- BASIC PRINCIPLES OF HAND SURGERYDocumento22 pagineBASIC PRINCIPLES OF HAND SURGERYFlorin PanduruNessuna valutazione finora
- Golf Single Plane SolutionDocumento23 pagineGolf Single Plane SolutionTommy Lee83% (6)
- 3days Ksa Crossfit: On-Ramp/Foundations Day One: 3 Fundamental Movements (Squats)Documento3 pagine3days Ksa Crossfit: On-Ramp/Foundations Day One: 3 Fundamental Movements (Squats)Игорь ОнищенкоNessuna valutazione finora
- Hamstring Exercise ProgressionDocumento15 pagineHamstring Exercise ProgressionFrancisco De VelascoNessuna valutazione finora
- Keiser University PHT 1227C Therapeutic Exercise I UE Strengthening Lab HandoutDocumento2 pagineKeiser University PHT 1227C Therapeutic Exercise I UE Strengthening Lab Handoutrmsplr1Nessuna valutazione finora
- Weight Training in Youth-Growth, Maturation, and Safety - An Evidence-Based ReviewDocumento10 pagineWeight Training in Youth-Growth, Maturation, and Safety - An Evidence-Based Reviewsadiq mohammedNessuna valutazione finora
- Biomechanics of the Lower ExtremitiesDocumento17 pagineBiomechanics of the Lower ExtremitiesMilind GuptaNessuna valutazione finora
- Muscle Origins, Insertions, Actions, and InterventionsDocumento15 pagineMuscle Origins, Insertions, Actions, and InterventionsJoseph Kachelman100% (3)
- Delp DissertationDocumento135 pagineDelp DissertationLuis GuerraNessuna valutazione finora
- Human Factors Engineering Work Station Design LectureDocumento48 pagineHuman Factors Engineering Work Station Design LecturenishthaNessuna valutazione finora
- Elbow Wrist StretchesDocumento3 pagineElbow Wrist StretchesPratik KadamNessuna valutazione finora
- Peat Set 1 Practice Exam HIGHLIGHTEDDocumento3 paginePeat Set 1 Practice Exam HIGHLIGHTEDMonica LapusNessuna valutazione finora
- Joan Edelstein - Alex Moroz - Lower-Limb Prosthetics and Orthotics - Clinical Concepts-SLACK, Incorporated (2010)Documento215 pagineJoan Edelstein - Alex Moroz - Lower-Limb Prosthetics and Orthotics - Clinical Concepts-SLACK, Incorporated (2010)Andrei ȚîrleaNessuna valutazione finora
- Test Bank For Medical Terminology A Word Building Approach 7th Edition RiceDocumento24 pagineTest Bank For Medical Terminology A Word Building Approach 7th Edition RiceMaryJohnsonafrz100% (36)
- Catalyst At-Home Training Plan Reference Document 1.1 PDFDocumento18 pagineCatalyst At-Home Training Plan Reference Document 1.1 PDFmarcos jimenezNessuna valutazione finora
- Prosthetics and Orthotics Manufacturing Guidelines: Lower Limb Prosthetics: Trans-Tibial ProsthesisDocumento52 pagineProsthetics and Orthotics Manufacturing Guidelines: Lower Limb Prosthetics: Trans-Tibial ProsthesisInternational Committee of the Red Cross100% (1)
- Developmental Milestones (Molnar)Documento4 pagineDevelopmental Milestones (Molnar)Kali Aceña100% (2)
- Late Swing or Early Stance? A Narrative Review of Hamstring Injury Mechanisms During High Speed RunningDocumento9 pagineLate Swing or Early Stance? A Narrative Review of Hamstring Injury Mechanisms During High Speed Runninggaston9reyNessuna valutazione finora
- Traditional Medicine & Clinical NaturopathyDocumento2 pagineTraditional Medicine & Clinical Naturopathyicha putri winataNessuna valutazione finora
- Ejercicios para El Suelo Pelvico Nivel Facil Moderado Dificil yDocumento46 pagineEjercicios para El Suelo Pelvico Nivel Facil Moderado Dificil yDilan LinaresNessuna valutazione finora
- McGill Et Al. 2009, Exercises For Spine Stabilization Motion Motor PatternsDocumento9 pagineMcGill Et Al. 2009, Exercises For Spine Stabilization Motion Motor Patternsok okNessuna valutazione finora
- CSKL 1b - Mechanism of LabourDocumento19 pagineCSKL 1b - Mechanism of LabourAthirahRara100% (1)