Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
11 Core Competencies
Caricato da
jubalmenesesDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
11 Core Competencies
Caricato da
jubalmenesesCopyright:
Formati disponibili
11 CORE COMPETENCIES
KEY AREAS OF RESPONSIBILITY:
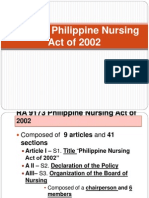
CORE COMPETENCY STANDARDS FOR NURSING PRACTICE IN THE PHILIPPINES (Click here to show the content of each core competency standards) Safe & quality nursing practice Management of resources & environment Health education Legal responsibility Ethico moral responsibility Personal & professional development Quality improvement Research Record management Communication Collaboration & teamwork LEGAL BASES Article 3 Sec.9 (c) of R.A. 9173/ Philippine Nursing Act 2002 Board shall monitor & enforce quality standards of nursing practice necessary to ensure the maintenance of efficient, ethical and technical, moral and professional standards in the practice of nursing taking into account the health needs of the nation. SIGNIFICANCE OF CORE COMPETENCY STANDARDS Unifying framework for nursing practice, education, regulation Guide in nursing curriculum development Framework in developing test syllabus for nursing profession entrants Tool for nurses performance evaluation Basis for advanced nursing practice, specialization Framework for developing nursing training curriculum Public protection from incompetent practitioners Yardstick for unethical, unprofessional nursing practice Phases of developing competency standards 1st Phase Competency identification through DACUM 2nd Phase Verification of identified competencies
3rd Phase Pilot testing ( senior student in 8 nursing colleges) 4th Phase Benchmarking with exiting standards from 3 countries + ICN
SAFE AND QUALITY NURSING CARE
I. SAFE AND QUALITY NURSING CARE CORE COMPETENCY 1: Demonstrate knowledge based on health/illness status of individual/ groups Indicators : Identifies health needs of patients/groups Explains patient/group status CORE COMPETENCY 2: Provides sound decision making in care of individual/groups considering their beliefs, values Indicators : Problem identification Data gathering related to problem Data analysis Selection appropriate action Monitor progress of action taken CORE COMPETENCY 3: Promotes patient safety and comfort Indicators : Performs age-specific safety measures and comfort measure in all aspects of patient care CORE COMPETENCY 4: Priority setting in nursing care based on patients needs Indicators : Identifies priority needs of patients Analysis of patients needs Determine appropriate nursing care to be provided CORE COMPETENCY 5: Ensures continuity of care
Indicators : Refers identified problems to appropriate individuals/ agencies Establish means of providing continuous patient care CORE COMPETENCY 6: Administers medications and other health therapeutics Indicators : Conforms to the 10 golden rules in medication administration and health therapeutics CORE COMPETENCY 7: Utilizes nursing process as framework for nursing. Performs comprehensive, systematic nursing assessment Indicators : Obtains consent Complete appropriate assessment forms Performs effective assessment techniques Obtains comprehensive client information Maintains privacy and confidentiality Identifies health needs CORE COMPETENCY 8: Formulates care plan in collaboration with patients, other health team members Indicators : Includes patients, family in care planning States expected outcomes in nursing interventions Develops comprehensive patient care plan Accomplishes patient centered discharge plan CORE COMPETENCY 9: Implements NCP to achieve identified outcomes Indicators : Explain interventions to patient, family before carrying them out Implement safe, comfortable nursing interventions Acts according to clients health conditions, needs Performs nursing interventions effectively and in timely manner CORE COMPETENCY 10: Implements NCP progress toward expected outcomes Indicators : Monitors effectiveness of nursing interventions Revises care plan PRN
CORE COMPETENCY 11: Responds to urgency of patients condition Indicators : Identifies sudden changes in patients health conditions Implements immediate, appropriate interventions
MANAGEMENT OF RESOURCES AND ENVIRONMENT
II. MANAGEMENT OF RESOURCES AND ENVIRONMENT CORE COMPETENCY 1: Organizes workload to facilitate patient care Indicators: Identifies task or activities that need to be accomplished Plans the performance of task or activities based on priority Finishes work assignment on time CORE COMPETENCY 2: Utilizes resources to support patient care Indicators: Determines the resources needed to deliver patient care Control the use of equipment CORE COMPETENCY 3: Ensures the functioning of resources Indicators: Check proper functioning of the equipment Refers Malfunctioning equipment to appropriate unit CORE COMPETENCY 4: Check the Proper functioning of the Equipment Indicators: Determines the task and procedures that can be safely assigned to the other members of the team Verifies the competence of the staff prior to delegating tasks CORE COMPETENCY 5: Maintains safe Environment
Indicators: Observe proper disposal of waste Adheres to policies, procedures and protocols on prevention and control of infection Defines steps to follow incase of fire , earthquake and other emergency situation
HEALTH EDUCATION
III. HEALTH EDUCATION CORE COMPETENCY 1: Assesses the learning needs of the patient and the family Indicators: Obtains learning information through interview, observation and validation Defines relevant information Completes assessment records appropriately Identify priority needs CORE COMPETENCY 2: Develops Health Education plan based on assessed and anticipated needs. Indicators: Considers nature of the learner in relation to social, cultural, political, economic, educational, and religious factor CORE COMPETENCY 3: Develops learning material for health education Indicators: Involves the patient, family and significant others and other resources Formulates a comprehensive health educational plan with the following components , objectives, content and time allotment Teaching-learning resources and evaluation parameters Provides for feedback to finalize plan CORE COMPETENCY 4: Implements the health Education Plan Indicators: Provides for conducive learning situation in terms of timer and place Considers client and family preparedness Utilize appropriate strategies Provides reassuring presence through active listening, touch and facial expression and gestures Monitors client and familys responses to health education
CORE COMPETENCY 5: Evaluates the outcome of health Education Indicators: Utilizes evaluation parameters Documents outcome of care Revises health education plan when necessary
LEGAL RESPONSIBILITY
V. LEGAL RESPONSIBILITY CORE COMPETENCY 1: Adheres to practices in accordance with the nursing law and other relevant legislation including contract and informed consent. Indicators: Fulfill legal requirements in Nursing Practice Holds current professional license Acts in accordance with the terms of contract of employment and other rules and regulation Complies with the required CPE Confirms information given by the doctor for informed consent Secures waiver of responsibility for refusal to undergo treatment or procedures Check the completeness of informed consent and other legal forms CORE COMPETENCY 2: Adheres to organizational policies and procedures, local and national Indicators: Articulates the vision and mission of the institution where one belongs Acts in accordance with the established norms and conduct of the institution/ organization CORE COMPETENCY 3: Document care rendered to patients. Indicators: Utilizes appropriate patient care records and reports Accomplish accurate documentation in all matters concerning patient care in accordance with the standard of nursing practice
ETHICO-MORAL RESPONSIBILITY
IV. ETHICO-MORAL RESPONSIBILITY CORE COMPETENCY 1: Respects the rights of individual/ groups Indicator: Renders nursing care consistent with the patients bill of rights (ie. confidentiality of information, privacy, etc.) CORE COMPETENCY 2 Accepts responsibility & accountability for own decisions and actions Indicators: Meets nursing accountability requirements as embodied in the job description Justifies basis for nursing actions and judgment Protects a positive image of the profession CORE COMPETENCY 3 Adheres to the national and international code of ethics for nurses Indicators: Adheres to the Code of Ethics for Nurses and abides by its provisions Reports unethical and immoral incidents to proper authoritie
PERSONAL & PROFESSIONAL DEVELOPMENT
VI. PERSONAL & PROFESSIONAL DEVELOPMENT CORE COMPETENCY 1 Identifies own learning needs Indicators: Verbalizes strengths, weaknesses, limitations. Determines personal and professional goals and aspirations. CORE COMPETENCY 2 Pursues continuing education Indicators: Participates in formal and non-formal education. Applies learned information for the improvement of care. CORE COMPETENCY 3
Gets involved in professional organizations and civic activities Indicators: Participates actively in professional, social, civic and religious activities Maintain membership to professional organizations Support activities related to nursing and health issues CORE COMPETENCY 4 Projects a professional image of nurse Indicators: Demonstrate good manners and right conduct at all times. Dresses appropriately. Demonstrates congruence of words and actions. Behaves appropriately at all times. CORE COMPETENCY 5 Possesses positive attitude towards change and criticism Indicators: Listens to suggestions and recommendations. Tries new strategies or approaches. Adapts to changes willingly. CORE COMPETENCY 6 Performs function according to professional standards Indicators: Assesses own performance against standards of practice. Sets attainable objectives to enhance nursing knowledge and skills. Explains current nursing practices, when situations call for it.
QUALITY IMPROVEMENT
XI. QUALITY IMPROVEMENT CORE COMPETENCY 1: Gathers data for quality improvement Indicators: Demonstrates knowledge of method appropriate for the clinical problems identified Detects variation in the vital signs of the patient from day to day Reports necessary elements at the bedside to improve patient stay at hospital Solicits feedback from patient and significant others regarding care rendered CORE COMPETENCY 2:
Participates in nursing audits and rounds Indicators: Contributes relevant information about patient condition as well as unit condition and patient current reactions Shares with the team current information regarding particular patients condition Encourages the patient to speak about what is relevant to his condition Documents and records all nursing care and actions Performs daily check of patient records/condition Completes patients records Actively contributes relevant information of patients during rounds thru readings and sharing with others CORE COMPETENCY 3: Identifies and reports variances Indicators: Documents observed variance regarding patient care and submits to appropriate group within 24 hours Identifies actual and potential variance to patient care Reports actual and potential variance to patient care Submits report to appropriate groups within 24 hours CORE COMPETENCY 4: Recommends solutions to identified problems Indicators: Gives appropriate suggestions on corrective and preventive measures Communicates and discusses with appropriate groups Gives and objective and accurate reporton what was observed rather than an interpretation of the event.
RESEARCH
VII. RESEARCH CORE COMPETENCY 1: Gathers data using different methodologies Indicators: Identifies researchable problems regarding patient care and community health Identifies appropriate methods of research for a particular patient/community problem Combines quantitative and qualitative nursing design thru simple explanation on the phenomena observed Analyzes data gathered
CORE COMPETENCY 2: Recommends actions for implementation Indicator: Based on the analysis of data gathered, recommends practical solutions appropriate for the problem CORE COMPETENCY 3: Disseminates results of research findings Indicators: Communicates results of findings to colleagues/patients/family and to others Endeavors to publish research Submits research findings to own agencies and others as appropriate CORE COMPETENCY 4: Applies research findings in nursing practice Indicators: Utilizes and findings in research in the provision of nursing care to individuals/groups/communities Makes use of evidence-based nursing to ameliorate nursing practice
RECORDS MANAGEMENT
VIII. RECORDS MANAGEMENT CORE COMPETENCY 1: Maintains accurate and updated documentation of patient care Indicator: Completes updated documentation of patient care CORE COMPETENCY 2: Records outcome of patient care Indicator: Utilizes a record system CORE COMPETENCY 3: Observes legal imperatives in recording keeping Indicators: Observes confidentially and privacy of patients records
Maintains an organized system of filing and keeping patients records in a designated area Refrains from releasing records and other information without proper authority
COMMUNICATION
IX. COMMUNICATION CORE COMPETENCY 1: Establishes rapport with patients, significant others and members of the health team. Indicators: Creates trust and confidence Listens attentively to clients queries and requests Spends time with the client to facilitate conversation that allows client to express concern. CORE COMPETENCY 2: Identifies verbal and non-verbal cues Indicator: Interprets and validates clients body language and facial expression CORE COMPETENCY 3: Utilizes formal and informal channels Indicator: Makes use of available visual aids CORE COMPETENCY 4: Responds to needs of individuals, family, group and community Indicator: Provides re- assurance through therapeutic, touch, warmth and comforting words of encouragement Readily smiles CORE COMPETENCY 5: Uses appropriate information technology to facilitate communication Indicator: Utilizes telephone, mobile phone, email and internet, and informatics Identifies a significant other so that follow up care can be obtained Provides holding or emergency numbers of services
COLLABORATION and TEAMWORK
X. COLLABORATION and TEAMWORK CORE COMPETENCY 1: Establishes collaborative relationship with colleagues and other members of the health team Indicators: Contributes to decision making regarding patients needs and concerns Participates actively in patients care management including audit Recommends appropriate intervention to improve patient care Respects the role of the other members of the health team Maintains good interpersonal relationships with patients, colleagues and other members of the health team CORE COMPETENCY 2: Collaborates plan of care with other members of the health team Indicator: Refers patients to allied health team partners Acts liaison / advocate of the patients Prepares accurate documentation of efficient communication of services Posted by Chief Nurse
Importance of the Interprofessional Approach to Improving Quality and Safety
Continuous quality improvement is based on the concept that improvement comes from building knowledge and applying it appropriately. Continuous quality improvement is the process of providing care that is more economical and/or care that yields improved outcomes, using systematic methods and interprofessional teamwork. There is considerable evidence that interprofessional teamwork and enhanced communication reduce errors (Mann, Marcus, & Sachs, 2006; Morey et al., 2002), improve patient outcomes (Lau, Banaszak-Holl, & Nigam, 2007; Pronovost, Berenholtz, & Dorman, 2003), improve process outcomes (Pisano, Bohmer, & Edmondson, 2001), improve patient satisfaction (Lefebvre, Pelchat, & Levert, 2007), and increase staff satisfaction (DiMeglio, Lucas, & Padula, 2005). The Institute of Medicine (2003) described the ability to function effectively in interdisciplinary teams as one of five basic competencies needed by health professionals to bridge the quality gap in the U.S. health care system. In health care, however, interprofessional teams frequently have little or no training in team process, and teams are not routinely trained to collaboratively give and improve care (Barnsteiner, Disch, Hall, Mayer, & Moore, 2007). Interprofessional teams are composed of individuals from diverse professional disciplines, each having its unique tradition, culture, and language that describe its healing relationship to the patient or client differently. Achieving improved health outcomes usually lies outside the scope or control of any one member of the health care team (Headrick, Wilcock, & Batalden, 1998). However, because each member of the team contributes to the patient's care from his or her area of expertise, a therapeutic synergy is possible when working in collaboration with other health
professionals. Traditionally, students are enculturated into their discipline's worldview and trained to assume specific roles and perform autonomously (Drinka, 1996; Toner, Miller, & Gurland, 1994). For interprofessional teams to function effectively, each member must understand not only the roles and language of other team members, but how to function collaboratively to integrate their expertise for quality care (Wadsworth & Fallcreek, 1997). The importance of interprofessional teamwork and communication has recently been addressed by the Agency for Healthcare Research and Quality (AHRQ) and the Department of Defense in their development of a recommended standard training program (Team STEPPS) for interprofessional health care teams (King et al., 2006). TeamSTEPPS stands for Team Strategies and Tools to Enhance Performance and Patient Safety. The TeamSTEPPS program's educational materials, which focus on specific skills supporting team performance principles, including training requirements, behavioral methods, human factors, and cultural change designed to improve quality and patient safety, are provided free from AHRQ (King et al., 2006). When health care professionals understand each other's roles and are able to communicate and work together effectively, patients are more likely to receive safe, quality care. Team members learn through the process of continual movement between practice and reflection on practice. This promotes higher performance in the short-term, while building a learning culture for the long-term. Well-functioning interprofessional teams not only recognize and build on the contributions of others, but they also focus on improving their process and their product through conscious and continuous cycles of learning together.
Potrebbero piacerti anche
- 11 Key Areas of Responsibilities of NursingDocumento2 pagine11 Key Areas of Responsibilities of NursingDaniel Bernabe90% (10)
- 11 Core Competencies in NursingDocumento4 pagine11 Core Competencies in NursingJOvie Rectin67% (3)
- 11 Core Competencies in NursingDocumento9 pagine11 Core Competencies in NursingSweetcharmed Go100% (1)
- PRC-BoN Core Competency Standards - Nle Test Framework.06.07.sDocumento43 paginePRC-BoN Core Competency Standards - Nle Test Framework.06.07.sjosephine100% (7)
- 11 Core CompetenciesDocumento20 pagine11 Core CompetenciesPingkian MildredNessuna valutazione finora
- Ched Memorandum Order FinalDocumento95 pagineChed Memorandum Order Finalrvmpresas100% (3)
- Principal Authors of The Philippine Nursing Act of 2002 - R.A. 9173Documento7 paginePrincipal Authors of The Philippine Nursing Act of 2002 - R.A. 9173Katrina Lagman CanlasNessuna valutazione finora
- Intensive Nursing Practicum: Bachelor of Science in NursingDocumento11 pagineIntensive Nursing Practicum: Bachelor of Science in NursingMichelle Gliselle Guinto Mallare100% (1)
- Professional Adjustment For NursingDocumento13 pagineProfessional Adjustment For Nursingprokuno86% (35)
- 11 Key Areas of ResponsibilitiesDocumento2 pagine11 Key Areas of ResponsibilitiesJoesineNessuna valutazione finora
- PRC-BON National Core Competency Standards For Filipino Nurses (Rev. May 2009)Documento9 paginePRC-BON National Core Competency Standards For Filipino Nurses (Rev. May 2009)PhilippineNursingDirectory.com93% (15)
- The Philippine Nursing Act of 2002Documento7 pagineThe Philippine Nursing Act of 2002sabduraupNessuna valutazione finora
- 8 Roles and Responsibilities of Beginning Nurse PractitionerDocumento21 pagine8 Roles and Responsibilities of Beginning Nurse Practitionernelo041350% (4)
- Competency Standards of Nursing Practice in The PhilippinesDocumento5 pagineCompetency Standards of Nursing Practice in The Philippinespamcarl100% (2)
- About OrnapDocumento4 pagineAbout Ornaplezsor100% (1)
- Rle NCM 107 - Maternal & Child Nursing 1 (Well Clients)Documento4 pagineRle NCM 107 - Maternal & Child Nursing 1 (Well Clients)ChelleyOllitro100% (4)
- CHED Memorandum Order No. 14 Series of 2009Documento129 pagineCHED Memorandum Order No. 14 Series of 2009PhilippineNursingDirectory.com81% (27)
- Competency Appraisal TopicsDocumento1 paginaCompetency Appraisal Topicsmevellemic100% (2)
- Competency Appraisal 1 and 2 (Complete)Documento4 pagineCompetency Appraisal 1 and 2 (Complete)Mary Grace Mas86% (7)
- Nursing Core Competency Standards 2012Documento35 pagineNursing Core Competency Standards 2012Roeder Cuerda100% (1)
- NCM 119 CompilationDocumento57 pagineNCM 119 Compilationticker100% (1)
- Ob Bag ContentsDocumento1 paginaOb Bag ContentsMike RemorcaNessuna valutazione finora
- Clinical Teaching Plan - NCM 117 (Student's Copy)Documento32 pagineClinical Teaching Plan - NCM 117 (Student's Copy)Jay Villasoto100% (4)
- Sterilization and MutilationDocumento17 pagineSterilization and Mutilationacha90% (10)
- Intensive Nursing Practicum: Bachelor of Science in NursingDocumento9 pagineIntensive Nursing Practicum: Bachelor of Science in NursingMichelle Gliselle Guinto MallareNessuna valutazione finora
- Cellular AberrationDocumento71 pagineCellular AberrationKris TejereroNessuna valutazione finora
- Narrative ReportDocumento2 pagineNarrative ReportRrichard Prieto Mmallari100% (4)
- Emerging OpportunitiesDocumento67 pagineEmerging OpportunitiesJasmin Jacob100% (5)
- Code of Ethics For NursesDocumento6 pagineCode of Ethics For NursesMarianne Jennifer Gan PauloNessuna valutazione finora
- Daily Management PlanDocumento5 pagineDaily Management PlanFirenze Fil100% (2)
- 118 A Chapter 2 - RESPONSES TO ALTERED VENTILATORY FUNCTION (EDITED) Handout #2Documento16 pagine118 A Chapter 2 - RESPONSES TO ALTERED VENTILATORY FUNCTION (EDITED) Handout #2Joanna Taylan100% (1)
- Clinical Focus: Terminal Competencies Concepts Learning ActivitiesDocumento12 pagineClinical Focus: Terminal Competencies Concepts Learning ActivitiesTanya LindainNessuna valutazione finora
- RA 9173 Philippine Nursing Act of 2002Documento50 pagineRA 9173 Philippine Nursing Act of 2002Jojebelle Kate Iyog-cabanlet100% (1)
- Clinical Duty ExpectationsDocumento1 paginaClinical Duty Expectationskuro hanabusaNessuna valutazione finora
- Scope of Nursing Practice Based On RA 9173Documento21 pagineScope of Nursing Practice Based On RA 9173Ruffa Mae Calimag100% (1)
- NCM 119 PrelimDocumento12 pagineNCM 119 Prelimczeremar chan100% (1)
- NCM 118 Notes PrelimDocumento35 pagineNCM 118 Notes PrelimCheri-Anne Diaz100% (4)
- The Philippine Nursing Act of 2002Documento11 pagineThe Philippine Nursing Act of 2002Esmareldah Henry SirueNessuna valutazione finora
- CHED MEMORANDUM ORDER (CMO) No. 14 Series of 2009Documento129 pagineCHED MEMORANDUM ORDER (CMO) No. 14 Series of 2009lylesantos85% (48)
- Comptency StandardsDocumento14 pagineComptency StandardsSeanmarie CabralesNessuna valutazione finora
- 11 Core Competencies: Mark Lawrence A. Lim RNDocumento48 pagine11 Core Competencies: Mark Lawrence A. Lim RNLawrence LimNessuna valutazione finora
- 11 Core CompetenciesDocumento11 pagine11 Core CompetenciesrlinaoNessuna valutazione finora
- I. Safe and Quality Nursing CareDocumento12 pagineI. Safe and Quality Nursing CareJoanne Sosa تNessuna valutazione finora
- 11 NURSING CORE COMPETENCY (Eca)Documento14 pagine11 NURSING CORE COMPETENCY (Eca)Jeshalaine AlawaddinNessuna valutazione finora
- Core Competency AreasDocumento54 pagineCore Competency AreastabayoyongNessuna valutazione finora
- 11 Core CompetenciesDocumento8 pagine11 Core CompetenciesJune TorrionNessuna valutazione finora
- Core Competencies Under The 11 Key Areas of ResponsibilitiesDocumento16 pagineCore Competencies Under The 11 Key Areas of ResponsibilitiesMiden AlbanoNessuna valutazione finora
- 11 Key Areas Ppt2Documento65 pagine11 Key Areas Ppt2Lorenzo DonqueNessuna valutazione finora
- 11 Core CompetenciesDocumento3 pagine11 Core CompetenciesYucef Bahian-AbangNessuna valutazione finora
- Finals Core Competencies Under The Eleven Key of Responsibility of NursingDocumento8 pagineFinals Core Competencies Under The Eleven Key of Responsibility of NursingAmiel Francisco ReyesNessuna valutazione finora
- Finals TFNDocumento44 pagineFinals TFNChristine BadanguioNessuna valutazione finora
- 11 Core Competencies in NursingDocumento4 pagine11 Core Competencies in NursingMikhael Jay IglesiasNessuna valutazione finora
- 11 Core Competencies in NursingDocumento5 pagine11 Core Competencies in NursingSarah Jane Orden DerradaNessuna valutazione finora
- TFN ReportDocumento28 pagineTFN ReportsigfrieddanilovNessuna valutazione finora
- Core Competency StandardsabdDocumento85 pagineCore Competency StandardsabdJoy PasongNessuna valutazione finora
- 11 Nursing Core Competencies: Prepared By: Anne Karen B. MendozaDocumento51 pagine11 Nursing Core Competencies: Prepared By: Anne Karen B. MendozaMiguel GatdulaNessuna valutazione finora
- The Core Competencies For The Entry LevelDocumento49 pagineThe Core Competencies For The Entry LevelKaren MendozaNessuna valutazione finora
- 11 Core Competencies On Standards of Nursing PracticeDocumento57 pagine11 Core Competencies On Standards of Nursing PracticeJenny Soriano0% (1)
- I. Safe and Quality Nursing CareDocumento15 pagineI. Safe and Quality Nursing CarePaul AnthonyNessuna valutazione finora
- 11 Key Areas of Responsibility / Core Competency / IndicatorsDocumento17 pagine11 Key Areas of Responsibility / Core Competency / IndicatorsHilario. Hayascent.Reign.M.Nessuna valutazione finora
- TLE-AFA6 Mod13 Monitoring Fish Raising Project v2Documento19 pagineTLE-AFA6 Mod13 Monitoring Fish Raising Project v2Jun Aaron Sarmiento100% (1)
- A Literature Analysis of Research On Artificial Intelligence in MISDocumento10 pagineA Literature Analysis of Research On Artificial Intelligence in MISjonathasluis_17Nessuna valutazione finora
- Rosejean Pitogo Classroom ManagementDocumento24 pagineRosejean Pitogo Classroom ManagementRhodz Rhodulf Capangpangan100% (1)
- The ELC An Early Childhood Learning Community at Work 1596036495Documento169 pagineThe ELC An Early Childhood Learning Community at Work 1596036495amasrurNessuna valutazione finora
- Sources of Nursing KnowledgeDocumento13 pagineSources of Nursing KnowledgeVette Angelikka Dela CruzNessuna valutazione finora
- BSBMGT407 Student Assessment Booklet CB V2.0 (Restricted)Documento34 pagineBSBMGT407 Student Assessment Booklet CB V2.0 (Restricted)Jenny YipNessuna valutazione finora
- AhmadBukhoriShaharuddinMSKA2020 PDFDocumento27 pagineAhmadBukhoriShaharuddinMSKA2020 PDFAshma AdilahNessuna valutazione finora
- Daniel Kofi Ofosu - AsiamahDocumento117 pagineDaniel Kofi Ofosu - AsiamahshumaiylNessuna valutazione finora
- Pro S09 MinalDocumento51 paginePro S09 Minalbhaktee100% (1)
- Human Behavior (Module 1)Documento23 pagineHuman Behavior (Module 1)Katherine Ederosas100% (4)
- Diagnostic Evidence Cooperatives: Bridging The Valley of Death in Diagnostics DevelopmentDocumento3 pagineDiagnostic Evidence Cooperatives: Bridging The Valley of Death in Diagnostics DevelopmentNadia AyuningtiasNessuna valutazione finora
- Distribution Channel Example in IndiaDocumento18 pagineDistribution Channel Example in IndiaNirbhay Pandey100% (3)
- Hidden Energy of Sacred GeometryDocumento10 pagineHidden Energy of Sacred GeometryJesse Lee AlexanderNessuna valutazione finora
- A Study On Organisation Culture at Bellad and CompanyDocumento21 pagineA Study On Organisation Culture at Bellad and CompanyPrateek GaddiNessuna valutazione finora
- How We RaiseDocumento19 pagineHow We RaiseErickson ManaladNessuna valutazione finora
- Research ProblemDocumento33 pagineResearch Problemkiranpatil1014532Nessuna valutazione finora
- Beautrais SuicideDocumento94 pagineBeautrais SuicideМатиас Себальос ГусманNessuna valutazione finora
- Course Outline of Marketing Research (For MBA)Documento5 pagineCourse Outline of Marketing Research (For MBA)Azmol bdNessuna valutazione finora
- Domestoil Research ProposalDocumento0 pagineDomestoil Research ProposalNitin KumarNessuna valutazione finora
- Moving Organizational Theory in Health Care.11Documento12 pagineMoving Organizational Theory in Health Care.11Madhan KraceeNessuna valutazione finora
- Best Practices in Todays EconomyDocumento59 pagineBest Practices in Todays EconomytudorkidNessuna valutazione finora
- Dervin & Gross 2016 ICC in Education PDFDocumento270 pagineDervin & Gross 2016 ICC in Education PDFGiovanna Suárez GonzálezNessuna valutazione finora
- Shahroz Research ProposalDocumento4 pagineShahroz Research ProposalSalim KhanNessuna valutazione finora
- Lean Six SigmaDocumento15 pagineLean Six SigmaJoão Victor RoconNessuna valutazione finora
- Multi Genre Research Paper RubricDocumento7 pagineMulti Genre Research Paper Rubricttdqgsbnd100% (1)
- SPSD AssignmentDocumento21 pagineSPSD AssignmentHafidz Al-RizzoNessuna valutazione finora
- Postgraduate Course: M.SC PsychologyDocumento138 paginePostgraduate Course: M.SC PsychologyPrasanth SamyNessuna valutazione finora
- 7-Analytical Services Manager (CSE)Documento3 pagine7-Analytical Services Manager (CSE)KrishnaNessuna valutazione finora
- L. Skov, M. Riegels Melchior, 'Research Approaches To The Study of Dress and Fashion'Documento18 pagineL. Skov, M. Riegels Melchior, 'Research Approaches To The Study of Dress and Fashion'Santiago de Arma100% (2)
- ENGL 112 Syllabus (Fall 2021)Documento7 pagineENGL 112 Syllabus (Fall 2021)Adan SaeedNessuna valutazione finora