Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Telaah Jurnal Fractur
Caricato da
Alif Yanur AbidinCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Telaah Jurnal Fractur
Caricato da
Alif Yanur AbidinCopyright:
Formati disponibili
CLINICAL PRACTICE COLUMN Extremity Fractures in Children: When Is It an Emergency?
Rachel DiFazio, MS, RNC Carole C. Atkinson, MS, RNC
Not all pediatric fractures require emergent orthopedic attention. The information needed to assess and provide the appropriate interventions to children and their families following an extremity fracture is discussed in this article. A case study is used to describe a fracture that requires emergent intervention. The role of the pediatric orthopaedic nurse practitioner in the emergency department, inpatient, and outpatient setting is also illustrated. n 2005 Elsevier Inc. All rights reserved.
HEN A CHILD breaks a bone (sustains a fracture), the family, the school nurse, the coach, even nonpediatric emergency departments, often consider this a medical emergency situation. Many pediatric extremity injuries are actually a low-priority situation. Overcrowded emergency departments and long waiting times necessitate alternative approaches for managing children with extremity fractures. This article describes pediatric skeletal extremity injuries, lists fractures and associated complications that require immediate evaluation, identifies teaching needs of families, and describes a unique program developed by a busy pediatric ambulatory orthopedic service at a Level I pediatric trauma center.
INCIDENCE OF FRACTURES IN CHILDREN Fractures in children are a common reason for emergency department visits and hospitalizations.
From the Department of Orthopaedic Surgery, Childrens Hospital Boston, Boston, MA, and Department of Nursing and Patient Services, Childrens Hospital Boston, Boston, MA. Address correspondence and reprint requests to Rachel DiFazio, MS, RNC, 119 Water Street, Unit 68, Beverly, MA 01915. E-mail: rachel.difazio@childrens.harvard.edu 0882-5963/$ - see front matter n 2005 Elsevier Inc. All rights reserved. doi:10.1016/j.pedn.2005.03.016
However, the majority of fractures can be safely managed on an outpatient basis. It is estimated that boys have a 42% chance of sustaining at least one fracture between the ages of 0 and 16 years and girls have a 27% chance. The chance of a fracture severe enough to require hospitalization during the first 16 years of life is 6.8%. In girls, fracture incidence peaks at age 12 years and in boys peaks at age 15 years (Beaty & Kasser, 2001). Fractures in the upper extremity are more common than fractures in the lower extremity, although admission with surgical treatment is more common for injuries to the lower extremities than the upper extremity (Kay & Matthys, 2001). The radius is the most commonly fractured upper extremity bone followed by the bones in the hand (metacarpals, carpals, and phalanges). In the lower extremities, the tibia is fractured more often than other bones (Worlokc & Stower, 1988). Fractures occur because of three main causes: accidental trauma, nonaccidental trauma (child abuse), and pathological conditions. Accidental trauma composes the largest group.
UNIQUENESS OF FRACTURES IN CHILDREN Because fractures in children are very common, it is important for nurses to understand the unique characteristics of the immature and developing
298
Journal of Pediatric Nursing, Vol 20, No 4 (August), 2005
EXTREMITY FRACTURES IN CHILDREN: WHEN IS IT AND EMERGENCY Table 1. Unique Characteristics of Fractures in Children
299
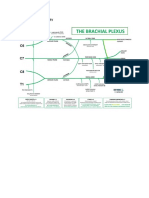
Anatomic Presence of growth plate/physis: The physis (growth plate) is the cartilage between the epiphysis, the most distal aspect of the long bones, and metaphysis, the growing portion of the long bones (Figure 1). Each long bone has at least two growth plates, one at each end. The growth plate will determine the future length and shape of the bones. The growth plate in a child is the weakest part of the bone and is frequently the site of injury during trauma. Fractures through the growth plate are most commonly described using the Salter Harris classification system (Salter, 1999). With this classification system, there is a progressive increase in physeal damage from Types I to VI fractures. Nursing care implications: Any growth plate injury should be referred for further evaluation and possible intervention. Delay in treatment, depending on the severity of the injury, can cause part or all of the bone to stop growing, resulting in shortening and/or angular deformity of the limb. The Salter Harris classification can assist prognostic information regarding the risk for permanent growth plate injury. Thicker and more elastic periosteum: The periosteum is the vascular sheath around bone that is responsible for the thickness of the bone. It helps to partially stabilize the bone when a fracture occurs. This allows many fractures to be treated with closed reduction and casting rather than surgery. Nursing care implications: Fractures in children are more stable than those in adults because of the thick periosteum. Therefore, fractures in children are often less displaced and do not require surgery as often as fractures in adults. For a stable fracture, splinting is usually adequate, but casting may be needed to decrease the childs activity level and provide comfort. Biomechanical Increased number of vascular canals and decreased mineral content: This increases the bones flexibility, allowing bones to buckle or bow rather than to break completely. Nursing care implications: The greater porosity of the bones causes greater flexibility in the bones of children leading to a bowing deformity, which is a unique fracture pattern seen primarily in children. If this fracture is untreated or undiagnosed, this could affect long-term motion in the affected extremity. Bone is weaker than ligaments and tendons: Ligamentous injury, or a sprain, is uncommon in the skeletally immature pediatric population. It is more common to sustain a growth plate/physis fracture. Nursing care implications: Fractures in children are more common than sprains and should be suspected if the child complains of pain at the growth plate even with a negative x-ray. Often, splinting or casting is necessary to decrease the childs activity level and provide comfort. Growth plates have not yet hardened into solid bone, therefore do not show up on x-ray. Physiological Rapid healing: Because of increased blood flow and cellular activity, nonunions or fractures that do not heal are rare in pediatrics. Nursing care implications: The younger the child, the more rapid the healing process. The closer the fracture is to the growth plate, the more rapid the healing process. Remodeling: In this process, bone is broken down and new bone is formed. Remodeling allows bones to straighten themselves out over time. Nursing care implications: Because children have a greater potential for remodeling (straightening out of the bones) than adults, perfect alignment of a fracture is not necessary for adequate healing and function. Data from England and Sundberg (1996), Lipp (1998), Mabrey and Fitch (1989), Musgrave and Mendelson (2002), and Ogden (1990).
skeletal system and how fractures in children differ from those of adults. Childrens bones are anatomically, biomechanically, and physiologically different from adults. An understanding of these differences will allow nurses to better identify and triage fractures of an urgent nature. Table 1 describes these unique differences of fractures and their nursing care implications. Figure 1 shows the normal anatomy of the wrist.
FRACTURES REQUIRING IMMEDIATE ATTENTION Several orthopedic injuries require emergent treatment and surgical intervention. Compartment syndrome with and without fracture, open fractures, fractures associated with vascular or nerve injuries, and irreducible joint dislocations are surgical emergencies. Delay in treatment can result in morbidity such as loss of limb function and infections such as osteomyelitis. The child should be referred immediately to a medical center that can provide pediatric orthopedic expertise. All of these surgical emergencies can be detected with a thorough history, physical assessment, and radiological findings (OCarroll, 2000). PHYSICAL ASSESSMENT Table 3 provides an overview of nonemergent and emergent physical assessment findings. bRed
COMMON EXTREMITY FRACTURES IN PEDIATRICS Table 2 describes the types of fractures seen in children (see Figures 2-5 for the anterior-posterior view of the fractures). Depending on history, physical assessment, and radiological findings, many of them do not require emergency orthopedic intervention.
300
DIFAZIO AND ATKINSON
Figure 2. Lateral view of a plastic or bowing deformity of the forearm.
CASE STUDY An example of a fracture that requires emergent evaluation and intervention is illustrated in the following case. A 5-year-old male presents to the emergency department with his mother; his chief complaint is left elbow pain. While playing on the jungle gym earlier that day, he fell and landed on his outstretched left arm. He reported immediate pain to his left elbow and was unable to move it. He had visible swelling and deformity around the elbow. On examination, his vital signs were normal for age except for sinus tachycardia of 120 bpm. Swelling, bruising, and deformity were visualized slightly above the left elbow with no evidence of broken skin at the site of injury (Figure 6). Radial and brachial pulses were palpable. He had full sensation to light touch and intact motor function of his wrist, hand, and shoulder. He was tearful when his elbow was touched and refused attempts at flexion and extension. There were no other signs of external trauma. Figure 7 reveals a normal anterior-posterior x-ray of the elbow for purposes of comparison.
Figure 1. anatomy.
Anterior posterior view of the wrist: normal
flagsQ indicate emergency situations. Table 4 summarizes key nursing interventions that are required for situations that are considered emergent in nature. EDUCATIONAL NEEDS OF THE CHILD AND FAMILY Each family should receive instruction for assessing the neurovascular status of the distal extremity while in a splint or cast. They should also receive teaching on care of the splint or cast and care of the skin under and around the cast edges. If the child will be discharged with crutches or a walker, thorough instruction should be given on use and maintenance of the equipment, as well as weight-bearing status of the extremity. Table 5 lists some key points to address during teaching.
Table 2. Types of Fractures Seen in Children Plastic or bowing deformity: Significant bending without breaking may cause angular deformity of the bone (Figure 2). Buckle fracture: Compression injury with minimal cortical disruption. The cortex of the bone is the protective outer shell around the bone. These fractures are usually caused by axial loading in which the force is exerted parallel to the primary axis. Example: A child runs into a wall with his arm straight out all the force goes down the bone (Figure 3). Greenstick fracture: Incomplete fracture of the bone (Figure 4). Complete fracture: Bones become divided into two pieces: They often remain attached by the periosteum (Figure 5).
Figure 3.
Anteriorposterior view of a buckle fracture.
EXTREMITY FRACTURES IN CHILDREN: WHEN IS IT AND EMERGENCY Table 3. Physical Assessment
Parameter Lower Extremity Upper Extremity
301
Inspect Skin
Observe joint range of motion
Figure 4.
Anteriorposterior view of a greenstick fracture.
Anteriorposterior x-rays of the elbow revealed a Type III left supracondylar humeral fracture (Figure 8). Following emergency evaluation, he was taken to the operating room. He underwent a closed reduction with percutaneous pinning of his fracture (Figure 9). He was placed into a long arm cast, which was bivalved to accommodate anticipated swelling. The child spent the night in the hospital for pain management, arm elevation, and circulation, sensation, and motion assessment. The following day, an orthopedic nurse practitioner visited the child and his parents on the inpatient unit to reinforce the home care instructions, and provided
Discoloration Swelling Deformity Red flag Open wound Hip Decreased ability to flex, extend, abduct, adduct, or externally and internally rotate Knee Decreased ability to flex, extend, abduct, adduct, or internal and external rotation Ankle Decreased ability to dorsiflex, plantarflex, invert, or evert Phalanges Decreased ability to flex, extend, hyperflex, or hyperextend Red flag Incapable of any movement
Discoloration Swelling Deformity Red flag Open wound Shoulder Decreased ability to flex, extend, abduct, adduct, or externally and internally rotate Elbow Decreased ability to flex, extend, supinate, or pronate Wrist Decreased ability to flex, extend, ulnar deviate, or radial deviate Phalanges Decreased ability to flex, extend, hyperflex, or hyperextend Red flag Incapable of any movement
Palpate Pulses
Integrity of pulses Integrity of pulses Presence and strength Presence and strength distal to the injury distal to the injury (femoral, popliteal, pedal) (brachial, median, radial) Red flag Red flag Diminished or absent Diminished or absent pulse pulse Cool, cold, blue hue Cool, cold, blue hue distal to injury distal to injury Integrity of nerves Integrity of nerves Sensation to touch present Sensation to touch present Red flag Red flag Numbness, tingling, Numbness, tingling, and intermittent or and intermittent or complete paresthesia complete paresthesia Localized point Localized point tenderness; constant or tenderness; constant or intermittent rate pain by intermittent rate pain by approved pain scale approved pain scale Red flag Red flag Persistent pain, not Persistent pain, not relieved by analgesics relieved by analgesics
Describe Sensation
Pain
Data from Moloney-Harmon and Czerwinski (2003).
Figure 5.
Anteriorposterior view of a complete fracture.
them with a discharge instruction tool specific for supracondylar fracture. All questions were answered and a follow-up appointment was scheduled with the orthopedic surgeon. The nurse practitioner
302 Table 4. Nursing Care Interventions for Findings of an Emergent Nature
Issue/ Complication Intervention
DIFAZIO AND ATKINSON
Bleeding
Open fracture
Deformity
Swelling
Pain/anxiety Status change Procedure education
Discharge education
Control bleeding by applying pressure with a sterile dressing. Avoid hypovolemic shock by administering intravenous fluids and oxygen. Stabilize an impaled object; do not remove it. The wound should be irrigated with saline and covered with a sterile dressing to prevent infection. Tetanus prophylaxis should be administered if not up to date. Intravenous antibiotic therapy is indicated for open fractures. First-generation cephalosporins are usually used. Immobilize above and below the injury site in the most comfortable position with a splint. Do not attempt to straighten the limb or manipulate protruding bone. Apply and intermittently reapply cool packs to the injured area for up to 48 hours if needed. Elevate the extremity above the level of the heart. Initiate oral or intravenous analgesia as soon as possible. Frequently assess, document, and report the five Ps (pain, pallor, pulses, paresthesia, and paralysis). Preoperative or procedural sedation teaching for the child and family. Clearly explain all procedures to the child and family. Verbal and written family teaching for management at home.
on urgency, answering parents questions about the care of their child, and acting as a resource for the nonnursing appointment schedulers. Outside the ambulatory care setting, the nurse practitioners cross over to inpatient units and the emergency department to assist with education of both patients and the nurses. They work with interprofessional staff members on patient care plans and discharge/ follow-up plans, as well as contribute to staff education. Since 1996, the nurse practitioners have also helped to track and monitor patient care-related problems, such as poor communication and missed appointments. One problem that was identified was the lack of appropriate teaching and follow-up for children who were evaluated by the orthopedic
Table 5. Education
Teaching Point Suggested Intervention
Swelling
Itchy skin
Skin care
Data from Moloney-Harmon and Czerwinski (2003).
also gave the family contact information in the event of concerns or questions after discharge. ROLE OF ORTHOPEDIC NURSE PRACTITIONER ACROSS THE CONTINUUM OF CARE The role of the nurse practitioner within the department of orthopedic surgery at Childrens Hospital Boston began in 1997 and continues to evolve to meet the complex needs of the patients. Currently, there are five full-time nurse practitioners collaborating with 16 orthopedic surgeons. The nurse practitioners primarily work in the ambulatory setting. They complete all histories, physical assessments, and teaching on preoperative patients; they diagnose and treat children with common orthopedic disorders; they assist the orthopedic surgeons with the care of patients, such as patients with scoliosis, birth defects, and traumatic injuries. They are also responsible for telephone triage, which includes assisting with scheduling of patients based
Pain management
Equipment maintenance
When to call the doctor
Elevate the limb above the level of the heart. Apply cool packs. Have the child wiggle the fingers and toes hourly. Use a hair dryer on a cool, low setting to blow air into the cast. Use distraction. Never put anything into the cast to scratch, the skin may break and result in complications. Check the skin around the cast daily for open or irritated areas. Never use lotions or powders because they will soften and irritate the skin. Protect the cast form getting wet. When showering and bathing, cover the cast with a heavy plastic bag and waterproof tape. Use a hairdryer on cool to help dry a cast that is damp. Provide oral analgesia as directed. Decrease activity and elevate the extremity. Provide distraction. Check walkers and crutches daily for loose screws and fasten tightly. Check the grips and tips for worn out areas and replace if necessary. Survey the area in which the child will be using the equipment for safety hazards. Persistent numbness and tingling. Severe pain when moving fingers or toes. Extreme soreness or discoloration of fingers or toes. Coolness of the extremity in cast. Decreased ability to move fingers or toes. A bad smell or drainage from under the cast. Severe itching. Red, broken, or swollen skin around or under the cast. Cracked, split, or softened cast. Fever for more than a day.
EXTREMITY FRACTURES IN CHILDREN: WHEN IS IT AND EMERGENCY
303
Figure 6. Painful elbow after fall.
surgeons in the emergency department, so the nurse practitioners were charged with improving outcomes for orthopedic patients seen in the emergency department. The role of the orthopedic nurse practitioner expanded to include follow-up on patients who had been evaluated, treated, and discharged to home from the emergency department or admitted for surgery or observation. After a meeting with emergency department physicians, nurses, and support staff, an orthopedic patient logbook was developed to identify all orthopedic patients seen in the emergency department. The logbook includes patient demographics, diagnosis, treatment, and proposed follow-up plans. Patients are entered into the logbook by the orthopedic surgeon who sees the patient. The orthopedic nurse practitioners oriented the rotating orthopedic surgeons to the use of the logbook, and
Figure 8. Anteriorposterior view of a Type III supracondylar fracture of the humerus.
have frequent discussions with the surgeons to review patient teaching and follow-up plans. Each morning, a nurse practitioner reviews the logbook and calls all the patients who have been discharged to home. The purpose of these calls is to assure that families have a clear understanding of what occurred in the emergency department, to answer any further questions, and to schedule appropriate follow-up appointments. Many of the children with simple fractures or sprains are scheduled in the nurse practitioner clinic with physician coverage if necessary. Families have been
Figure 7. anatomy.
Anteriorposterior view of the elbow: normal
Figure 9. Anteriorposterior view of a supracondylar fracture of the humerus after a closed reduction and percutaneous pinning.
304
DIFAZIO AND ATKINSON
very receptive to the telephone follow-up and nurse practitioner care. For admitted patients, the nurse practitioner visits the child in the hospital and assists with care plan development and discharge planning and teaching. The nurse practitioner also participates in daily inpatient rounds, which include nursing, child life, social work, physical therapy, and the discharge planning coordinator. The emergency department follow-up has been very successful. Parents have expressed gratitude for the follow-up service; the number of incoming calls from parents asking questions about care of their child has decreased; and the number of inappropriately scheduled appointments has decreased. This role extension has freed up appointment space for other children, and it has assured safe follow-up for emergency department patients. Not every hospital has the resources to implement this type of nurse practitioner-sponsored program. This information was included to illustrate the efficiency and effectiveness of using advanced practice nurses to improve care outcomes for this pediatric patient population. The primary purpose, however, was to illustrate some important underlying concepts of this article. When children have fractures, they are brought to emergency departments. Whether the fractures are simple or complex, whether they require
surgical intervention or not, fractures produce a great deal of anxiety and concern. Our experience as nurse practitioners caring for this population has shown that problems occur when there is lack of sufficient education and follow-up to allay concern and to decrease anxiety. Nurses are in an ideal situation to use their knowledge of fractures, physical assessment skills, and basic intervention skills to effectively educate and inform parents (and patients) about the injury. It is inevitable that children with fractures will require nursing intervention. What nurses say and do can make a significant difference. CONCLUSION Musculoskeletal injury is a leading cause of emergency department use and disability among children (Buckley et al., 1994). It is important for nurses to obtain a thorough history focusing on the mechanism of injury, to understand the unique characteristics of the immature, developing skeletal system, and to recognize common fractures. Early identification of clinical signs of emergent injuries can expedite definitive treatment. Prompt nursing interventions, accompanied by thoughtful explanations and appropriate education can help alleviate unnecessary fear and concern.
REFERENCES
Beaty, J., & Kasser, J. (2001). Rockwood and Wilkins fractures in children (5th ed.). Philadelphia: Lippincott Williams & Wilkins. Buckley, S. L., Gotschall, C., & Robertson, W., et al. (1994). The relationships of skeletal injuries with trauma score, injury severity score, length of hospital stay, hospital charges, and mortality in children admitted to a regional pediatric trauma center. Journal of Pediatric Orthopedics, 14, 449 453. England, S. P., & Sundberg, S. (1996). Management of common pediatric fractures. Pediatric Clinics of North America, 43, 991 997. Kay, R., & Matthys, G. (2001). Pediatric ankle fractures: Evaluation and treatment. Journal of the American Academy of Orthopaedic Surgeons, 9, 268 278. Lipp, E. (1998). Athletic physeal injury in children and adolescents. Orthopaedic, 17 22. Mabrey, J., & Fitch, R. (1989). Plastic deformation in pediatric fractures: Mechanism and treatment. Journal of Pediatric Orthopaedics, 9, 310 314. Moloney-Harmon, P. A., & Czerwinski, S. J. (2003). Nursing care of the pediatric trauma patient. St. Louis, MO: ElsevierSaunders. Musgrave, D., & Mendelson, S. (2002). Pediatric orthopedic trauma: Principles in management. Critical Care Medicine, 30, 431 443. OCarroll, B. M. (2000). Principles of basic trauma nursing (1st ed.). South Easton, MA: Western Schools Press. Ogden, J. A. (1990). Injury to the immature skeleton. In R. Touloukian, (Ed.) Pediatric trauma. New York: Wiley (2nd ed., pp. 518). Salter, R. (1999). Disorders and injuries of the musculoskeletal system (3rd ed.). Baltimore, MD: Williams & Wilkins. Worlokc, P., & Stower, M. (1988). Fracture patterns in Nottingham children. Journal of Pediatric Orthopedics, 6, 656 660.
TELAAH JURNAL Extremity Fractures in Children: When Is It an Emergency? A. JUDUL Fraktur ekstremitas pada Anak: Ketika Apakah itu Darurat? B. INDENTIFIKASI MASALAH
1. PENDAHULUAN Depresi adalah dipandang sebagai konstelasi depresi gejala dengan fokus khusus pada respon afektif. Ini gejala bisa meningkat untuk disfungsi parah, sehingga peningkatan bunuh diri potensial (Ownsworth & Oei, 1998). Gejala depresi mungkin mewakili konstruk demoralisasi, diyakini untuk menemani parah fisik dan psikologis penyakit, dan berkaitan dengan
keputusasaan, kesedihan, dan rendah diri (Breslau & Davis, 1986). Ketika dibandingkan dengan orang dengan kondisi medis kronis, orang hanya dengan gejala depresi secara bermakna lebih gangguan dalam fungsi sosial. Efek aditif adalah melaporkan ketika orang sakit medis juga memiliki depresi gejala (Wells et al, 1989.).
2. TOPIK PERMASALAHAN Untuk menguji apakah stres kronis, keterkaitan interpersonal, dan beban kognitif bisa menjelaskan depresi setelah cedera otak traumatis, traumatic brain injury (TBI).
3. IDENTIFIKASI MASALAH Stres kronis setelah cedera dan rasa memiliki adalah prediktor kuat pascacedera depresi dan variabel setuju untuk intervensi oleh perawat dalam kesehatan masyarakat, neurologis pusat, atau klinik rehabilitasi. Studi masa depan diperlukan untuk memeriksa bagaimana variabel-variabel ini berubah dari waktu ke waktu selama proses pemulihan. Variable-variabel tersebut yaitu Stres dan Gejala depresi setelah cidera, Keterkaitan Interpersonal dan Depresi, Beban kognitif dan Gejala depresi . Hipotesis yang diuji: Hipotesis 1: Postinjury stres kronis dan pasca-TBI gejala depresi berhubungan positif.
Hipotesis 2: Keterkaitan interpersonal (akal postinjury dari depresi memiliki dan dukungan sosial) dan pasca-TBI gejala yang berbanding terbalik terkait. Hipotesis 3 : Kognitif beban pemrosesan kecepatan dan akurasi dan pasca-TBI gejala depresi positif. Metode: Selama tatap muka wawancara, informasi demografis, dan perkiraan diperoleh dari keparahan cedera otak dan peserta menyelesaikan tes kognitif mengarahkan perhatian dan ingatan jangka pendek, tanggapan terhadap stres skala persepsi, interpersonal.
C. HASIL PENELITIAN Demografis profil. Sampel ini didominasi (91,7%) Kaukasia. Tiga puluh enam (48%) adalah perempuan dan 39 (52%) adalah laki-laki. Hampir 91% dipekerjakan sebelum cedera. Usia rata-rata adalah 37,4 tahun (SD = 12,10, kisaran 19-60). Tiga puluh enam persen tidak pernah menikah, 40% sudah menikah, dan 20% bercerai, dipisahkan, atau janda. Empat persen hidup dengan lainnya yang signifikan. Sepertiga memiliki pendapatan rumah tangga tahunan lebih dari $ 75.000 dan 14,7% memiliki pendapatan tahunan kurang dari $ 15.000. Tiga belas persen sebelumnya telah dirawat karena masalah alkohol atau narkoba. Enam puluh lima persen dinilai status kesehatan mereka saat ini baik untuk yang sangat baik. Empat puluh satu persen memakai antidepresan diresepkan, tetapi tidak ada data dikumpulkan pada obat, dosis, dan durasi. Hampir 7% melaporkan tidak memiliki resep diisi untuk antidepresan. Dua puluh persen melaporkan gangguan kejiwaan preinjury, seperti kecemasan atau depresi, 8% mengatakan mereka telah brpikiran untuk bunuh diri sebelum cedera, dan 16% memiliki cedera kepala sebelumnya. Keparahan cedera kepala. Pada tanggal pengujian, 30 korban yang selamat dalam waktu 7 bulan dari cedera mereka, dan 45 adalah antara 7-25 bulan sejak tanggal cedera. Jumlah yang sama yang selamat memiliki tingkat ringan dan sedang cedera. Rata-rata durasi Post Trauma Amnesia (PTA) adalah 7,65 hari (SD = 8,92, rentang 0-45 hari). Sedikit lebih dari 48% memiliki hasil CT abnormal , menunjukkan perdarahan kecil, hematoma, atau kontusio. Lokasi yang tepat dari luka tidak tercatat. Hampir 71% melaporkan bahwa kecelakaan kendaraan bermotor adalah mekanisme cedera dan 64% melaporkan durasi ketidaksadaran akan singkat menjadi kurang dari satu jam. Ukuran gejala depresi. Para Neurobehavioral Functioning Inventory depression subscale (NFI-D) dan Center for Epidemiological Studies Depression Scale (CES-D) sangat berkorelasi (r =. 85, p <0,00, satu-sisi). Menggunakan
diterbitkan CES-D norma (Radloff, 1977), 36% dari sampel ini memiliki skor yang tidak berada dalam kisaran depresi dan 20% memiliki nilai CES-D> 30,5. Rata-rata skor depresi pada CES-D dan NFID tidak berbeda secara signifikan dengan usia, jenis kelamin, diagnosis psikiatri preinjury atau mencoba bunuh diri, tingkat ringan dibandingkan sedang cedera, atau sebelumnya TBI. Peserta mengambil antidepresan rata-rata memiliki tingkat depresi yang lebih tinggi secara signifikan pada CES-D dan NFI-D (t = 2,92, p =. 005 dan t = 3,05, p =. 003). Karena NFI-D divalidasi dengan sampel TBI, ini adalah variabel hasil untuk analisis berikut. Hipotesis 1. Pemeriksaan hubungan antara stres dan gejala depresi postinjury itu mengungkapkan. Stres Postinjury saja membantu menjelaskan 54% dari varians [R 2 =. 55; Disesuaikan R 2 =. 54, F = 87,72 (1,73), p =. 00]. Selain itu, hubungan linear positif dan signifikan yang ditemukan antara Jurnal Stres kronis Triwulan Ketiga Keperawatan Beasiswa 2002 225 waktu sejak gejala cedera, stres postinjury, dan depresi [R 2 =. 64, Disesuaikan R 2 =. 63, F = 63,73 ( 2, 72), p =. 00]. Hipotesis 2. Postinjury rasa memiliki itu berbanding terbalik dengan gejala depresi dan menjelaskan 54% dari varians dalam pasca TBI gejala depresi, F = 87,72, (1,73), p =. 00. Ketika waktu sejak cedera ditambahkan ke model, 58% dari varians dijelaskan, F = 52,23, (2, 72), p =. 00. Variabel-variabel yang tidak terpengaruh oleh usia, gender, atau tingkat keparahan cedera. Dukungan sosial berkorelasi dengan gejala depresi dan merupakan variabel penjelas yang signifikan dalam model regresi sederhana, R2 =. 17 (1,73), F = 15,43, p =. 00. Namun, ketika waktu sejak cedera dan rasa memiliki yang dimasukkan dengan dukungan sosial (Lihat Gambar 1.1), itu tidak lagi signifikan. Hipotesis 3. Skor pada baterai tes kognitif perhatian diarahkan dan memori jangka pendek tidak menjelaskan variasi yang signifikan dalam depresi. Gejala depresi juga tidak dijelaskan oleh waktu untuk menyelesaikan tes ini, dan tingkat kesalahan atau waktu untuk menyelesaikan baterai tidak berkorelasi dengan tindakan keparahan cedera kepala, stres yang dirasakan, atau salah mengukur gejala depresi. Namun, kombinasi dari bagian pengakuan visual dan bagian diketik pada tes Delayed Recognition Word Span (DRWS) menghasilkan beberapa temuan yang signifikan. Bila kedua tes memori jangka pendek itu dijumlahkan, jelas hubungan signifikan yang ditemukan antara skor dan gejala depresi, R 2 =. 19, Disesuaikan R 2 =. 17, F = 8,60 (2, 72), p =. 00. Ketika variabel ini ditambahkan ke model, hubungan ini tidak akan terpengaruh oleh usia atau tingkat keparahan cedera. Namun, saat ini mengukur kognitif dijumlahkan
disertakan dengan PSS dan waktu sejak cedera, tes dijumlahkan tidak lagi membantu menjelaskan pasca TBI gejala depresi.
D. ANALISA HASIL PENELITIAN Penelitian ini mengunakan uji statistik regresi dan didapatkan hasil sebagai berikut
Gambar 1.1 Tabel hasil penelitian
Relasi memiliki arti jika nilai p <0,05 dan ada pengaruh jika nilai p <0,05. Pada tabel di atas terlihat bahwa dukungan sosial tidak menjadi pengaruh bagi gejala depresi pada postinjury rasa milik, dukungan sosial, stres persepsi, dan waktu karena cedera. Nilai r2 semakin besar nilai tersebut maka model semakin baik. Jika nilai mendekati 1 maka model regresi semakin baik. Nilai r2 mempunyai karakteristik diantaranya: 1) selalu positif, 2) Nilai r2 maksimal sebesar 1. Jika Nilai r2 sebesar 1 akan mempunyai arti kesesuaian yang sempurna, dan pada tabel ini niai r2 >1 maka hasilnya baik. Penelitian ini menunjukkan variabel tertentu yang terkait dengan pasca TBI depresi, dan ini adalah kerangka awal untuk studi masa depan. Dirasakan postinjury stres dan rasa milik membantu menjelaskan hampir 75% dari varians dalam gejala depresi dan keduanya mungkin akan setuju untuk intervensi oleh perawat yang terlibat dalam pelayanan masyarakat untuk orang pulih dari TBI. Studi membutuhkan dengan menggunakan sampel yang lebih besar untuk menentukan bagaimana depresi, stres, dan perubahan keterkaitan antarpribadi selama pemulihan dan re-integrasi proses.
E. SARAN 1. KELEBIHAN a) Setiap penjelasan dicantumkan nama penulis dari penelitian sebelumnya
sehingga bisa digunakan sebagai sumber pendukung dari data tersebut. b) Metode penelitian dijelaskan secara detail, mulai dari cara pencarian sampel hingga mendapatkan hasil akhir penelitian. c) Hasil penelitian dalam jurnal ini kemudian dibandingkan dengan hasil penelitian dari jurnal lain yang masih berkaitan lingkup penelitiannya, sehingga akan lebih memperkuat hasil penelitian dulu dan sekarang. d) Setiap sampel yang digunakan juga diteliti dan dijelaskan keadaan mereka secara umum, seperti usia, jenis kelamin, status perkawinan, pekerjaan, status kesehatan dan lain-lain.
2. KEKURANGAN a) Masih ada perdebatan atau teori yang berbeda dari setiap penulis dan belum saling melengkapi. b) Ada beberapa singkatan kata yang belum dijelaskan apa maknanya. c) Tidak semua orang mengetahui arti dari simbol, istilah dan cara perhitungan data statistik yang digunakan dalam penelitian tersebut, contohnya r, p, dan lain-lain. d) Peran perawat hanya dijelaskan secara garis besar saja, tidak secara mendetail setiap langkah dan cara yang harus dilakukan oleh seorang perawat dalam kondisi pasien depresi pasca TBI.
F. APLIKASI PADA PELAYANAN KEPERAWATAN DI INDONESIA Jurnal ini membahas bagaimana depresi, stres, dan perubahan keterkaitan antar pribadi selama proses pemulihan dan proses re-integrasi pada pasien postinjury TBI. Dari jurnal ini diketahui bahwa faktor pemberat pertama pada mereka dengan postinjury TBI adalah psikososial yang terganggu sehingga menimbulkan depresi, stres, kemudian berdampak pada hilangnya fungsi sosial di masyarakat. Jurnal ini dapat diaplikasikan di Indonesia. Jurnal ini menjelaskan mengenai bagaimana seorang perawat berperan dalam menilai atau
memperkirakan keparahan cidera otak dengan menggunakan metode pengukuran tradisional menggunakan PTA, Gasglow Coma Scale skor (GCS), dan durasi ketidaksadaran. Selain berperan menilai tingkat keparahan cedera otak, perawat memberi panduan kepada anggota keluarga untuk menilai durasi PTA. Di Luar Negeri untuk mendeteksi tingkat keparahan cidera otak bisa menggunakan GCS, PTA dan durasi ketidaksaran loss of consciousness (LOC). Di Indonesia sudah menerapkan sistem seperti ini. Namun dalam memperkirakan
keparahan cidera otak perawat cenderung menggunakan metode dengan GCS skor karena dinilai lebih akurat daripada metode lain. Namun dalam hal ini, perawat sering mengalami kesulitan dalam menilai GCS skor karena perilaku klien dinilai ambigu pada saat pemeriksaan. Dalam keadaan postinjury cidera kepala TBI, perawat berperan besar dalam proses pemulihan. Tingkat stress atau depresi akibat postinjury dan rasa ingin membaur mempunyai potensi besar untuk disetujuinya intervensi perawat dalam proses pemulihan pasien dengan trauma cidera otak. Perawat berperan untuk mengelola stress yang terkait dengan proses pemulihan dan membantu mereka untuk memperkuat ketrampilan atau peran sosial di masyarakat dengan memberikan dukungan sosial pada mereka dengan postinjury cidera otak.
G. REFRENSI
Breslau, N., & Davis, G. (1986). Chronic stress and major depression. Archives of General Psychiatry, 43(4), 309-314.
Esther Bay, Bonnie M. Hagerty, Reg A. Williams, Ned Kirsch, Brenda Gillespie. (2002). Chronic Stress, Sense of Belonging, and Depression Among Survivors of Traumatic Brain Injury. Journal of nursing scholarship : Sigma theta tau international. 34:3, 221-226.
Ownsworth, T., & Oei, T. (1998). Depression after traumatic brain injury: conceptualization and treatment considerations. Brain Injury, 12(9), 735-751.
Wells, K., Stewart, A., Hays, R., Burnam, A., Rogers, W., Daniels, M., et al. (1989). The functioning and well-being of depressed patients. JAMA, 262(7), 914-919.
Potrebbero piacerti anche
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Anatomy - & - Physiology Cheat SheetDocumento2 pagineAnatomy - & - Physiology Cheat SheetAlaka69% (16)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (120)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Rock Climbing 6 Week Workout Plan - Adventure SchoolDocumento21 pagineRock Climbing 6 Week Workout Plan - Adventure SchoolYusuf TosunNessuna valutazione finora
- Cervical Total Disc Replacement: Long-Term OutcomesDocumento12 pagineCervical Total Disc Replacement: Long-Term OutcomesKyle RobinNessuna valutazione finora
- Metacarpal FractureDocumento45 pagineMetacarpal FractureJinnasit TeeNessuna valutazione finora
- First Aid - Dance Related Injuries Gr9Documento31 pagineFirst Aid - Dance Related Injuries Gr9Jai UniraNessuna valutazione finora
- Universal Hip DistractorDocumento4 pagineUniversal Hip Distractorapi-19808945Nessuna valutazione finora
- Hallux ValgusDocumento16 pagineHallux ValgusucssNessuna valutazione finora
- Knee Interventions ProjectDocumento3 pagineKnee Interventions Projectapi-670980669Nessuna valutazione finora
- 5 Vertical Jump SecretsDocumento4 pagine5 Vertical Jump SecretsBrito KevinNessuna valutazione finora
- New Roods ApprochDocumento50 pagineNew Roods ApprochMonicca GV100% (1)
- Mat ActivitiesDocumento20 pagineMat Activitiesmuthuu60% (5)
- FractureDocumento13 pagineFractureLadylyn BrazaNessuna valutazione finora
- Principles of Radiographic Interpretation: Submitted By:-Saikat Kumar Kundu MVSC 2 Year ID-54187Documento104 paginePrinciples of Radiographic Interpretation: Submitted By:-Saikat Kumar Kundu MVSC 2 Year ID-54187Praney SlathiaNessuna valutazione finora
- Brachial Plexus Notes11.13Documento11 pagineBrachial Plexus Notes11.13cpNessuna valutazione finora
- Ankle FracturesDocumento9 pagineAnkle FracturesUmar Dion SiraidNessuna valutazione finora
- AmputationDocumento40 pagineAmputationAmruth KhNessuna valutazione finora
- AHS 131 Lecture 4 MusclesDocumento60 pagineAHS 131 Lecture 4 MusclesBikash MainaliNessuna valutazione finora
- 4037.1-GLBL-En Persona OsseoTi Keel Tibia Ordering Information - FINALDocumento20 pagine4037.1-GLBL-En Persona OsseoTi Keel Tibia Ordering Information - FINALValaMelkorNessuna valutazione finora
- Orthopaedic Surgery Essentials Series Hand and WristDocumento275 pagineOrthopaedic Surgery Essentials Series Hand and Wristskyofclouds1100% (2)
- 16-Clinical Anatomy of The Upper LimbDocumento27 pagine16-Clinical Anatomy of The Upper LimbAlapati Vinod KumarNessuna valutazione finora
- Distal Radius Fractures (Broken Wrist) - OrthoInfo - AAOSDocumento4 pagineDistal Radius Fractures (Broken Wrist) - OrthoInfo - AAOSmuhammad iqbal mahfuzhNessuna valutazione finora
- F Muscular System MDocumento32 pagineF Muscular System MFitzgerald PachecoNessuna valutazione finora
- Abdominal Wall - HoDocumento71 pagineAbdominal Wall - HoMekuriya BeregaNessuna valutazione finora
- Non Locomotor Exercise CompilationDocumento10 pagineNon Locomotor Exercise Compilation22105346Nessuna valutazione finora
- A& P NotesDocumento178 pagineA& P NotesJSeashark100% (3)
- Shoulder Guidelines AdhesiveCapsulitis JOSPT May 2013 PDFDocumento31 pagineShoulder Guidelines AdhesiveCapsulitis JOSPT May 2013 PDFRulyNessuna valutazione finora
- Subclavian ArteryDocumento8 pagineSubclavian ArteryPatalie HettihewaNessuna valutazione finora
- Proximal Hamstring Tendinopathy Expert Physiotherapists' Perspectives On Diagnosis, Management and PreventionDocumento9 pagineProximal Hamstring Tendinopathy Expert Physiotherapists' Perspectives On Diagnosis, Management and PreventionAlberto Saura RodríguezNessuna valutazione finora
- Knee Ligament InjuriesDocumento5 pagineKnee Ligament InjuriesNijin XmxNessuna valutazione finora
- CASE REPORT Hip DislocationDocumento42 pagineCASE REPORT Hip DislocationvereriNessuna valutazione finora