Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
The Management of Postoperative Nausea and Vomiting in Elective Surgery Summary Points
Caricato da
Rebecca PiggottDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
The Management of Postoperative Nausea and Vomiting in Elective Surgery Summary Points
Caricato da
Rebecca PiggottCopyright:
Formati disponibili
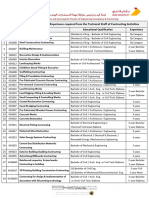
SP3 IFMSA Exchange 5th September 30th September Anaesthetics - Review of Modern Management 91017196 2004 words excluding
g in text references and textboxes
The Management of Postoperative Nausea and Vomiting in Elective Surgery Summary Points PONV has been reported in multiple studies to be present in 80 out of 100 surgical patients in the immediate post-operative period. The causes of PONV can be divided into surgical, anaesthetic and patient factors. The Apfel study decided that the most statistically important risk factors for PONV are being a woman, being a non-smoker, planned post-operative opioids and a history of motion sickness or previous PONV.
The use of prophylactic pharmacological agents is strongly debated and the best management incorporates a multi-modal prevention in order to improve the patient journey and improve cost-effectiveness.
The Management of Postoperative Nausea and Vomiting (PONV), is a high priority for every operating theatre. It has been reported that as many as 80 patients in 100 are affected by their surgical procedure and consequently either feel nauseous or vomit.i PONV can delay recovery room discharge by 47-61 minutes hence increases costs to healthcare providers due to the extra resources needed.ii Jenkins et al. found that avoiding PONV is one of the major priorities for day-case patients along with post-operative pain and discomfort experienced from the tracheal tube.iii This report will concentrate on the management of PONV within elective surgery and the many contributing factors that branch across the physiological, pharmacological and psychological realms and points are illustrated with a case report discussion.
SP3 IFMSA Exchange 5th September 30th September Anaesthetics - Review of Modern Management 91017196 2004 words excluding in text references and textboxes
Method The Cochrane database and PubMed search engine were searched for relevant papers using the key phrases such as PONV prophylaxis and management and core knowledge on the topic was found in the textbook Lees Synopsis of Anaesthesia. All papers were carefully reviewed with the date of publication in mind. A four week placement was also undertaken with the anaesthetic team of Policlinico di Modena, Italy, allowing for an appropriate case study to be identified. Verbal consent was gained from the patient for the case report and any identifying features have been removed. Lesson A multimodal protocol should be audited within a day surgery environment to establish individual patients risk and implement an appropriate treatment strategy for these planned procedures using education and pharmacological agents where necessary.
SP3 IFMSA Exchange 5th September 30th September Anaesthetics - Review of Modern Management 91017196 2004 words excluding in text references and textboxes
A Patients Story Mrs X, a 45 year old estate agent presented to the day surgery unit for excision of a peri-auricular tumour. She had no past medical history of note and was fit and healthy. At the age of 27 she underwent a total hysterectomy due to uncontrolled menorrhagia and had experienced some nausea associated with this surgery. She had no allergies. In this scenario, Mrs Xs airway was maintained using an endotracheal tube and mechanical ventilation using low-flow oxygen. Mrs X was given fentanyl and propofol 40mg for the induction of the general anaesthesia and kept on a maintenance infusion of remifentanyl and inhaled dexflurane as well as IV paracetamol for pain relief. This operation lasted 1 hour 40 minutes from the time of induction to extubation and no complications were experienced throughout this time. In the recovery suite the patient felt extremely nauseous and vomited twice. Within 20 minutes of the administration of ondansetron 8mg the nausea subsided. The patient recovered well after this incident with no further complaints and was discharged to the care of her husband. Physiology of PONV PONV is generally defined as nausea or vomiting that occurs within the first 24 hours following surgery.iv These feelings are stimulated by the vomiting centre located in lateral reticular formation of the medulla oblongata. The vomiting centre initiates a reflex after receiving information from neural pathways of the body, especially the chemoreceptor trigger zone as summarised in diagram A. These neural humoral responses are mediated by many different neurotransmitters including serotonin, dopamine, histamine and muscarinic transmitters and as a consequence of the increased stimulation of this pathway, a patient will frequently feel nauseous and vomit. PONV has also been linked with the more serious complications of dehydration and subsequent electrolyte imbalance, commonly that of sodium, as well as potential damage to the site of surgery. It is also difficult and
SP3 IFMSA Exchange 5th September 30th September Anaesthetics - Review of Modern Management 91017196 2004 words excluding in text references and textboxes
more costly to provide the patient with adequate pain relief orally and, as shown by a patient questionnaire, this negatively influences a patients journey.v
Diagram A Physiology of Emesis http://www.dcavm.org/05dec.html Risk Factors for PONV These can be systematically divided into those that are directly related to the patients demographic, surgical procedure and the anaesthetic agents chosen throughout their surgical journey.
SP3 IFMSA Exchange 5th September 30th September Anaesthetics - Review of Modern Management 91017196 2004 words excluding in text references and textboxes
Surgical factors are those which are often the most unavoidable and certain specialities are heavily linked with the incidence of PONV. The total duration of the operation is linked to the anaesthetic risk, which as seen in the chart above, is the most prominent group of risk factors. When discussing the type of surgery orthopaedic shoulder surgery, ophthalmic surgery and plastic surgery were grouped as higher risk with patients experiencing a six fold increase in PONV. Other specialities were also investigated and general orthopaedic, ENT and gynaecological surgery recorded a two to four fold increase in the incidence of PONV compared to the average surgical patient.vi Conversely, Apfel et al stated that the type of surgery was not a reliable component when predicting an increased risk. They did not include these factors in their scoring system when calculating PONV risk as they believed that these were influenced too heavily by the surgical cohort of a specific department, making it a non-independent factor.vii Hysterectomy exemplifies this theory. Whether performed abdominally or vaginally, hysterectomy is the most common type of gynaecological surgery performed. It is obvious that this surgery incurs higher risk of PONV due to the increased length of time the patient is under the influence of general anaesthesia (GA), opioid use and evidence also points towards the fact that being female is a significant predicting factor for PONV. It can therefore be concluded that the type of surgery cannot be reliably extracted as an independent risk factor from this situation. This seems a logical extrapolation made by Apfel et al. however it is also important to consider the whole patient when making decisions about clinical care and this information should not be totally dismissed. Anaesthesia proves the largest risk for PONV. According to McCracken et al, every 30 minutes that is spent under GA increases the risk by almost 60%.viii A balanced GA (an inhaled anaesthetic agent used in conjunction with intravenous medications) compared to total intravenous anaesthesia increases the risk of PONV by approximately 50%.ix Subsequently this approach is usually reserved for paediatric procedures and those patients whose intravenous access is poor. A volatile anaesthetic (one which is in a liquid state at room temperature and administered
SP3 IFMSA Exchange 5th September 30th September Anaesthetics - Review of Modern Management 91017196 2004 words excluding in text references and textboxes
through inhalation) doubles the risk of PONV compared to the actions of propofol and a high dose of the antidote to muscle relaxants used intra-operatively can also increase the likelihood of PONV.vii It is also considered a well-known fact that opioids, used in the control of post-operative pain relief, stimulate the vomiting reflex via D2 receptors in the dopaminergic pathway therefore increasing the incidence of PONV.xi Patient influenced risk factors are a mixture of the physiological and psychological, although as a group the majority are poorly understood. Most people have experienced nausea as a consequence of feeling scared or nervous. This, alongside a specific smell or sight, can lead individuals to become nauseous by stimulating higher cortical functions and there are no exceptions for surgery. It is interesting that if a patient has a pre-disposition to motion sickness or has previously experienced PONV, they too will be at higher risk of this occurring due to higher cortical functioning and the role of powerful memories. Surprisingly, the incidence of PONV does not follow a linear pattern when associated with age. Instead the figures peak when a patient reaches 6 and again at the age of 20 then declines into old age.x As emphasised forcefully on the Apfel Scoring system, it has been shown multiple times that females have triple the chance of experiencing PONV compared to males.vii Curiously enough, it has been recorded that smoking is of protective value to the patient and non-smokers are more likely to feel the effects of PONV. Management of PONV Number of Probability of PONV (%) 10 21 39 61 79
features Diagram B Apfel CC, Lr E, 0 Koivuranta M, Greim CA, Roewer N. 1 A simplified risk score for predicting 2 postoperative nausea and vomiting: 3 4 Conclusions from cross-validations between two centres. Anaesthesiology 1999; 91: 693-700.
SP3 IFMSA Exchange 5th September 30th September Anaesthetics - Review of Modern Management 91017196 2004 words excluding in text references and textboxes
The management of PONV is often ruled by the personal preference and experience of the anaesthetist in charge of the procedure. Anaesthetic drugs are often described as dirty drugs stimulating a range of potentially dangerous side-effects if given unnecessarily therefore a careful balance must always be made. Due to the potential reactions, the use of prophylactic antiemetics is not always a safe or cost-effective option. Suggested approaches to the management of PONV focus on all aspects of the care pathway and this report will now discuss the potential risks and benefits of those advocated. The proper assessment of risk would be according to an evidence-based system, as it is of great importance in recognising the patients who are more at risk of suffering from PONV. As seen in diagram B, the Apfel scoring system takes into account the most stastically important, independent features and evaluates the risk with a percentage score. 0-1 signifies a low risk, 2-3 moderate risk and equal to or greater than 4 signifies a high risk patients with whom there is more inclination to prescribe prophylactic anti-emetics alongside their surgical procedure. xi A generalised reduction of anaesthetic time and agents plays a major role in decreasing the incidence of PONV. The use of a local anaesthesia, wherever possible, is advocated as this very rarely causes a systemic upset like PONV. The use of propofol (an intravenous sedative) to maintain anaesthesia throughout the planned procedure, has the benefit of a short half-life; significantly decreasing time spent under sedation and it is also reported by Davies and Cashman to have modest anti-emetic qualities compared to other anaesthetic agents.xi Adequate oxygenation and hydration are also priorities for anaesthetists as these often precipitate symptoms. It is also recommended that care should be taken to avoid, if possible, the use of more volatile anaesthetics including nitrous oxide or neostigmine as they can be detrimental to post-operative recovery.xii The prophylactic use of anti-emetics in day surgery is an area of controversy. Recommended universally by the American College, the attitude in Great Britain and
SP3 IFMSA Exchange 5th September 30th September Anaesthetics - Review of Modern Management 91017196 2004 words excluding in text references and textboxes
Italy is more modest. In a meta-analysis conducted in 2006 by Carlisle et al, 103 237 patient outcomes were compared in order to find the most suitable agent.xiii Outcomes were measured by the effect of the drug on nausea, vomiting, nausea or vomiting and rescue therapy (anti-emetic prescription on the basis of present symptoms). Of the 60 drugs tested, only 9 had a significant statistical effect on the objectified outcomes: cyclizine (H2 antagonist), dolasetron, ondansetron, granisetron, tropisetron and ramosetron (5-HT3 antagonists), dexamethasone (corticosteroid), metoclopramide and droperidol (D2 antagonists). The recommendation of the paper was also clear that these drugs were most effective when used in combination. If rescue therapy is required later on then it is thought that another pharmacological agent with a different mode of action should be used due to the previous treatments relative inefficacy. There have also been many studies comparing the effect of prophylaxis against a placebo. In one study, a comparison between the effects of dixyrazine vs. droperidol vs. placebo in 61 cases for ocular surgery was made. PONV occurred in 65% of cases treated with the placebo, dixyrazine 25% and droperidol 48%.xiv This has been replicated multiple times with many different combinations however due to cost effective measures it is more important that we concentrate on measuring the risks of a patient. Case Discussion Mrs X was operated on within the Otorhinolaryngology department. Although doubted, some research indicates that this type of surgery is twice as likely to be associated with PONV. Another factor that cannot be changed is the patients gender as being female is triples the likelihood of experiencing PONV. Alongside the female gender, the fact that Mrs X has had previous surgical experience of nausea and vomiting in adult life would suggest that there is a higher risk and many anaesthetists would advise the use of prophylactic anti-emetics. The Apfel total is now 2/4 and equates to a 39% chance of experiencing PONV. The usage of a balanced anaesthesia with opioids will only stand to increase the chances that this patient will experience nausea post-operatively and the anaesthetic risks could be minimised through selection of a suitable sedative to induce and maintain anaesthesia. I believe that propofol and remifentanyl were used advantageously for
SP3 IFMSA Exchange 5th September 30th September Anaesthetics - Review of Modern Management 91017196 2004 words excluding in text references and textboxes
a clean anaesthesia. Propofol is believed to possess some anti-emetic properties and remifentanyl has a short half-life, decreasing the duration of anaesthesia and ensuring that the patient wakes to a clear head and adequate oxygenation, decreasing the chance of PONV. However I believe that in this patients case an anti-emetic prophylaxis, potentially the least expensive histamine receptor antagonist cyclizine, could be used with good conscience. Conclusion This review calls for a clear protocol concerning the current management options for PONV, trialled and audited within an elective surgical environment in order to establish individual patients risk and implemented accordingly. Although this process is influenced by a great many factors of which we have little knowledge, more research should be undertaken with regards to use of antiemetic agents and when they prove most effective in the journey of a surgical patient. It is also imperative that the psychological well-being of a patient is not forgotten and by creating a calm environment and reducing anxiety we may see a reduction in the number of people affected by PONV, effecting future costs to the NHS and patient satisfaction.
Ongoing Research: Implementation Study of the Post-Operative Nausea and Vomiting Prediction Rule - This study evaluated the implementation of a prediction rule for postoperative nausea and vomiting changes physician behaviour, improves patient outcome and improves cost-effectiveness of treatment of postoperative nausea and vomiting. Accessed 03/10/2011. http://www.clinicaltrials.gov/ct2/show/NCT00293618? term=Post+operative+nausea+and+vomiting&rank=16
SP3 IFMSA Exchange 5th September 30th September Anaesthetics - Review of Modern Management 91017196 2004 words excluding in text references and textboxes
Patient Information: http://en.wikipedia.org/wiki/Postoperative_nausea_and_vomiting A quick overview of the topic with links to further reading for patients. http://www.patient.co.uk/doctor/Common-Post-Op-Complications-to-Look-OutFor.htm A summary of post-operative complications including PONV and possible treatments to reassure patients.
Additional Educational Resources: http://anesthesiologyinfo.com/articles/04252004.php A generalised overview of PONV including a detailed pharmacology report of all agents most commonly used to treat PONV. http://www.frca.co.uk/SectionContents.aspx?sectionid=113 This is a step by step guide from the Royal College of Anaesthetists that cover all angles up specialist level on the management of PONV. http://www.ponv.org/ An international team of researchers, concentrating on anaesthesia and designing new and innovative clinical trials around this subject.
McCracken G, Houston P, Lefebvre G. Guideline for the Management of Postoperative Nausea and Vomiting. JOGC 2008; 209: 600-607.
ii
Hirsch-J. "Impact of postoperative nausea and vomiting in the surgical setting". Anaesthesia. 1994. 49(Suppl):30-1.
iii
Jenkins K, Grady D, Wong J, Correa R, Armanious S, Chung F. Post-operative recovery: Day surgery patients preferences. Br J Anaesth 2001; 86: 272-4.
iv
McCracken G, Houston P, Lefebvre G. Guideline for the Management of Postoperative Nausea and Vomiting. JOGC 2008; 209: 600-607.
v
Collier J, Longmore M, Turmezei T, Mafi AR. Oxford Handbook of Clinical Specialities Eighth Edition. United States. Oxford University Press. 2009. 617.
vi
Lemos P, Jarrett P, Philip B. Day Surgery - Development and Practice. 2006. London: International Association for Ambulatory Surgery
vii
Apfel CC, Roewer N. Risk assessment of postoperative nausea and vomiting. Int Anesthesiol Clin 2003; 41:13-32
viii
McCracken G, Houston P, Lefebvre G. Guideline for the Management of Postoperative Nausea and Vomiting. JOGC 2008; 209: 600-607.
ix
Sneyd JR, Carr A, Byrom WD, Bilski AJ. A meta-analysis of nausea and vomiting following maintenance of anaesthesia with proprofol or inhalational agents. Eur J Anaesthesiol. 1998; 15:433-445.
x xi
Davies NJH and Cashman JN. Lees Synopsis of Anaesthesia. 13th Ed. Aug 2005, Butterworth-Heinemann.
xii
Lonie DS, Harper NJ. "Nitrous oxide anesthesia and vomiting". Anaesthesia. July 1996. 41:703-7
xiii
Carlisle J, Stevenson CA. Drugs for preventing postoperative nausea and vomiting. Cochrane Database of Systematic Reviews 2006, Issue 3. Art. No.: CD004125. DOI: 10.1002/14651858.CD004125.pub2.
xiv
Larsson S, Jonmarker C. Postoperative emesis after pediatric strabismus surgery: the effect of dixyrazine to droperidol. Acta Anesthesiol Scand. 1990. 34:227-30.
Potrebbero piacerti anche
- EVALUATION OF THE INFLUENCE OF TWO DIFFERENT SYSTEMS OF ANALGESIA AND THE NASOGASTRIC TUBE ON THE INCIDENCE OF POSTOPERATIVE NAUSEA AND VOMITING IN CARDIAC SURGERYDa EverandEVALUATION OF THE INFLUENCE OF TWO DIFFERENT SYSTEMS OF ANALGESIA AND THE NASOGASTRIC TUBE ON THE INCIDENCE OF POSTOPERATIVE NAUSEA AND VOMITING IN CARDIAC SURGERYNessuna valutazione finora
- Evidence-Based Management of Postoperative Nausea and Vomiting: A ReviewDocumento16 pagineEvidence-Based Management of Postoperative Nausea and Vomiting: A ReviewYaclinNessuna valutazione finora
- The Assessment of Risk Factors For Postoperative Nausea and VomitingDocumento5 pagineThe Assessment of Risk Factors For Postoperative Nausea and VomitingWiedya KristiantiNessuna valutazione finora
- Postoperative Nausea and VomitingDocumento45 paginePostoperative Nausea and Vomitingprem kotiNessuna valutazione finora
- Relationship Between The Incidence and Risk Factors of Postoperative Nausea and Vomiting in Patients With Intravenous Patient-Controlled AnalgesiaDocumento6 pagineRelationship Between The Incidence and Risk Factors of Postoperative Nausea and Vomiting in Patients With Intravenous Patient-Controlled AnalgesiaRandi KhampaiNessuna valutazione finora
- Moore RDocumento7 pagineMoore RElaine IllescasNessuna valutazione finora
- Acute Intraoperative Pulmonary Aspiration: SynopsisDocumento8 pagineAcute Intraoperative Pulmonary Aspiration: Synopsisibnu razzak laskarNessuna valutazione finora
- Acta Anaesthesiologica Taiwanica: Editorial ViewDocumento2 pagineActa Anaesthesiologica Taiwanica: Editorial ViewShuaib AhmedNessuna valutazione finora
- Acta Anaesthesiologica Taiwanica: Research PaperDocumento7 pagineActa Anaesthesiologica Taiwanica: Research PaperShuaib AhmedNessuna valutazione finora
- Postoperative Nausea and VomitingDocumento33 paginePostoperative Nausea and Vomitingferlina100% (1)
- Research Paper On Ventilator Associated PneumoniaDocumento8 pagineResearch Paper On Ventilator Associated PneumoniakwbfbzundNessuna valutazione finora
- Ncbi - Nlm.nih - Gov-Post-Op Urinary RetentionDocumento9 pagineNcbi - Nlm.nih - Gov-Post-Op Urinary RetentiondadupipaNessuna valutazione finora
- Post-Operative Nausea and VomitingDocumento8 paginePost-Operative Nausea and Vomitingika lindaNessuna valutazione finora
- 2011 - Preoperative Endoscopic Airway Examination (PEAE) Provides Superior Airway Information and May Reduce The Use of Unnecessary Awake Ion - MylenaDocumento6 pagine2011 - Preoperative Endoscopic Airway Examination (PEAE) Provides Superior Airway Information and May Reduce The Use of Unnecessary Awake Ion - MylenaMirella Andraous100% (1)
- Nonoperating Room Anesthesia Anesthesia in The Gastrointestinal SuiteDocumento16 pagineNonoperating Room Anesthesia Anesthesia in The Gastrointestinal SuiteGustavo ParedesNessuna valutazione finora
- Anestesia - Cardiovascular - Luna OrtizDocumento11 pagineAnestesia - Cardiovascular - Luna OrtizWeimar Andres Bonilla MosqueraNessuna valutazione finora
- 2019 Curr Op Dez TIVA AmbDocumento5 pagine2019 Curr Op Dez TIVA AmbjaquelinemiyakeNessuna valutazione finora
- 29th International Symposium On Intensive Care and Emergency MedicineDocumento209 pagine29th International Symposium On Intensive Care and Emergency MedicineYOGINessuna valutazione finora
- ExtubationDocumento7 pagineExtubationbalab2311Nessuna valutazione finora
- Acta Anaesthesiologica Taiwanica: Research PaperDocumento6 pagineActa Anaesthesiologica Taiwanica: Research PaperStela MpNessuna valutazione finora
- Prospective External Validation of A Predictive Score For Postoperative Pulmonary ComplicationDocumento13 pagineProspective External Validation of A Predictive Score For Postoperative Pulmonary ComplicationAthziri GallardoNessuna valutazione finora
- Intravenous Acetaminophen: A Study of Effectiveness of Practice of Intraoperative Administration in Children Undergoing AdenotonsillectomyDocumento6 pagineIntravenous Acetaminophen: A Study of Effectiveness of Practice of Intraoperative Administration in Children Undergoing Adenotonsillectomyjoions gilberth oppiesNessuna valutazione finora
- 08 AE 5585 Crespo IngDocumento3 pagine08 AE 5585 Crespo Ingcarlosalayon2Nessuna valutazione finora
- PIIS0007091221004359Documento7 paginePIIS0007091221004359luisfernandoamaya89Nessuna valutazione finora
- Postoperative Nausea and Vomiting at A Tertiary Care Hospital in North-Western TanzaniaDocumento9 paginePostoperative Nausea and Vomiting at A Tertiary Care Hospital in North-Western TanzaniaAsfaw NurhussenNessuna valutazione finora
- Postoperative Nausea and VomitingDocumento20 paginePostoperative Nausea and VomitingfraolNessuna valutazione finora
- 2 5373127936972950922Documento6 pagine2 5373127936972950922teguh sNessuna valutazione finora
- JurnalDocumento6 pagineJurnalFitri Aesthetic centerNessuna valutazione finora
- Pneumonia Research PaperDocumento5 paginePneumonia Research Paperhbzqwpulg100% (1)
- Ventilator Associated Pneumonia ThesisDocumento8 pagineVentilator Associated Pneumonia Thesisannapagejackson100% (2)
- German S3 Guidelines: Anal Abscess and Fistula (Second Revised Version)Documento55 pagineGerman S3 Guidelines: Anal Abscess and Fistula (Second Revised Version)Bunga AmiliaNessuna valutazione finora
- US Pulmón para Manejo de Atelectasias PerioperatoriasDocumento11 pagineUS Pulmón para Manejo de Atelectasias PerioperatoriasJURAGOMANessuna valutazione finora
- Perioperative Antibiotic Use in Sleep Surgery: Clinical RelevanceDocumento10 paginePerioperative Antibiotic Use in Sleep Surgery: Clinical RelevanceBRENDA VANESSA TREVIZO ESTRADANessuna valutazione finora
- Farmako 44Documento11 pagineFarmako 44dev darma karinggaNessuna valutazione finora
- Recent Thesis Topics in AnaesthesiaDocumento4 pagineRecent Thesis Topics in Anaesthesialbbzfoxff100% (2)
- Prehospital Ultrasound Imaging Improves Management of Abdominal TraumaDocumento5 paginePrehospital Ultrasound Imaging Improves Management of Abdominal TraumaAhmad Hasbi Al-MuzakyNessuna valutazione finora
- Acta Anaesthesiol Scand 2021 Johansson Early Post OperativeDocumento11 pagineActa Anaesthesiol Scand 2021 Johansson Early Post OperativetasyadelizaNessuna valutazione finora
- Effect of Smoking On Intraoperative Sputum and Postoperative Pulmonary Complication in Minor Surgical PatientsDocumento7 pagineEffect of Smoking On Intraoperative Sputum and Postoperative Pulmonary Complication in Minor Surgical PatientsfellaniellaNessuna valutazione finora
- Lateral ColposuspentionDocumento24 pagineLateral ColposuspentionMohammad QuayyumNessuna valutazione finora
- (2018) - Flujo Inspiratorio Máximo Como Predictor de Traqueotomía.Documento4 pagine(2018) - Flujo Inspiratorio Máximo Como Predictor de Traqueotomía.luribe662Nessuna valutazione finora
- A Retrospective Study of Success, Failure, and Time Needed To Perform Awake IntubationDocumento10 pagineA Retrospective Study of Success, Failure, and Time Needed To Perform Awake IntubationAinun RamadaniNessuna valutazione finora
- Pelvic Organ Prolapse After Laparoscopic Hysterectomy Compared With Vaginal Hysterectomy: The POP-UP StudyDocumento10 paginePelvic Organ Prolapse After Laparoscopic Hysterectomy Compared With Vaginal Hysterectomy: The POP-UP Studymuhammadnurul asmiNessuna valutazione finora
- Postoperative Nausea and Vomiting: Retrospective Comparative Statistical StudyDocumento19 paginePostoperative Nausea and Vomiting: Retrospective Comparative Statistical StudyIJAR JOURNALNessuna valutazione finora
- 158 Nausea - Vomiting ScaleDocumento9 pagine158 Nausea - Vomiting ScaleMas Indra ShuNessuna valutazione finora
- 03 WeilbachDocumento3 pagine03 WeilbachAmalia Sholihah MukhtarNessuna valutazione finora
- Evidence-Based Analysis of Risk Factors For Postoperative Nausea and VomitingDocumento12 pagineEvidence-Based Analysis of Risk Factors For Postoperative Nausea and Vomitingdwi maudy maulidiyahNessuna valutazione finora
- Thesis UrologyDocumento5 pagineThesis Urologydeepjonesmanchester100% (2)
- Ramgolam2018 PDFDocumento10 pagineRamgolam2018 PDFmortazaqNessuna valutazione finora
- Meconium-Stained Amniotic Fluid: A Risk Factor For Postpartum HemorrhageDocumento5 pagineMeconium-Stained Amniotic Fluid: A Risk Factor For Postpartum HemorrhagelaniNessuna valutazione finora
- Anaesthesia For Adenotonsillectomy: An Update: Indian J Anaesth 10.4103/0019-5049.199855Documento14 pagineAnaesthesia For Adenotonsillectomy: An Update: Indian J Anaesth 10.4103/0019-5049.199855Nazwa AlhadarNessuna valutazione finora
- Strobel 2015Documento9 pagineStrobel 2015Prasad NeelamNessuna valutazione finora
- Non-Invasive Positive Pressure Ventilation in Acute Respiratory Failure: Providing Competent CareDocumento9 pagineNon-Invasive Positive Pressure Ventilation in Acute Respiratory Failure: Providing Competent CareAndana TrisaviNessuna valutazione finora
- Jove 87 50687aDocumento15 pagineJove 87 50687aSaúlNessuna valutazione finora
- VAP in ICU ReviewDocumento8 pagineVAP in ICU ReviewAdam KurniaNessuna valutazione finora
- 1 s2.0 S0733862722000384 MainDocumento13 pagine1 s2.0 S0733862722000384 Maincoca12451Nessuna valutazione finora
- Overview of Total Intravenous Anesthesia in ChildrenDocumento12 pagineOverview of Total Intravenous Anesthesia in ChildrenJosibel OcantoNessuna valutazione finora
- Literature Review of PneumothoraxDocumento4 pagineLiterature Review of Pneumothoraxc5e83cmh100% (1)
- A Retrospective Study of Success, Failure, and Time Needed To Perform Awake IntubationDocumento10 pagineA Retrospective Study of Success, Failure, and Time Needed To Perform Awake IntubationnadaNessuna valutazione finora
- Secuencia de Intubación RápidaDocumento16 pagineSecuencia de Intubación Rápidaalis_maNessuna valutazione finora
- A Prospective Study: Clinical Paper OrthognaDocumento12 pagineA Prospective Study: Clinical Paper OrthognamfahrizaNessuna valutazione finora
- Stopping by Woods On A Snowy EveningDocumento9 pagineStopping by Woods On A Snowy EveningJulia Garces100% (2)
- MA 106: Linear Algebra Tutorial 1: Prof. B.V. Limaye IIT DharwadDocumento4 pagineMA 106: Linear Algebra Tutorial 1: Prof. B.V. Limaye IIT Dharwadamar BaroniaNessuna valutazione finora
- Book Index The Art of Heavy TransportDocumento6 pagineBook Index The Art of Heavy TransportHermon Pakpahan50% (2)
- Assessment of Diabetic FootDocumento7 pagineAssessment of Diabetic FootChathiya Banu KrishenanNessuna valutazione finora
- GBJ0232 - en GLX 3101 T2Documento43 pagineGBJ0232 - en GLX 3101 T2mnbvqwert100% (2)
- 5 Contracting Activity and Technical Staff RequirementsDocumento2 pagine5 Contracting Activity and Technical Staff RequirementsDaniyar KussainovNessuna valutazione finora
- ARK - Intel® Core™ I3-370m Processor (3M Cache, 2Documento3 pagineARK - Intel® Core™ I3-370m Processor (3M Cache, 2Delzi Guindra AdriNessuna valutazione finora
- Anderson, Poul - Flandry 02 - A Circus of HellsDocumento110 pagineAnderson, Poul - Flandry 02 - A Circus of Hellsgosai83Nessuna valutazione finora
- 3M Novec 1230 Fire Protection Fluid FAQDocumento8 pagine3M Novec 1230 Fire Protection Fluid FAQEden CansonNessuna valutazione finora
- Haldex-Barnes 2-Stage Pump For Log SplittersDocumento2 pagineHaldex-Barnes 2-Stage Pump For Log SplittersPer Akkamaan AgessonNessuna valutazione finora
- Manual of Sensorless Brushless Motor Speed Controller: Pentium SeriesDocumento4 pagineManual of Sensorless Brushless Motor Speed Controller: Pentium Seriesfosavo5839Nessuna valutazione finora
- EXCEL For Pump DesignDocumento2 pagineEXCEL For Pump Designkad-7Nessuna valutazione finora
- Regression Analysis Random Motors ProjectDocumento22 pagineRegression Analysis Random Motors ProjectPrateek AgrawalNessuna valutazione finora
- Diagnosis of TrypanosomiasisDocumento82 pagineDiagnosis of TrypanosomiasisDrVijayata Choudhary100% (1)
- VavDocumento8 pagineVavkprasad_56900Nessuna valutazione finora
- Pusheen With Donut: Light Grey, Dark Grey, Brown, RoséDocumento13 paginePusheen With Donut: Light Grey, Dark Grey, Brown, RosémafaldasNessuna valutazione finora
- Eco Exercise 3answer Ans 1Documento8 pagineEco Exercise 3answer Ans 1Glory PrintingNessuna valutazione finora
- Integration ConceptDocumento34 pagineIntegration ConceptJANELLA ALVAREZNessuna valutazione finora
- The 10 Most Famousfilipino Artists and Their MasterworksDocumento3 pagineThe 10 Most Famousfilipino Artists and Their MasterworksGina MagtibayNessuna valutazione finora
- Hashimoto's Thyroiditis: Veena RedkarDocumento10 pagineHashimoto's Thyroiditis: Veena RedkarSan RedkarNessuna valutazione finora
- Youth Camp Registration Form-2022Documento1 paginaYouth Camp Registration Form-2022FlerkNessuna valutazione finora
- Types of Loads Considered For Design of BridgeDocumento45 pagineTypes of Loads Considered For Design of BridgeAbhishek100% (1)
- Ujian 1 THN 4Documento13 pagineUjian 1 THN 4Che Shuk ShukaNessuna valutazione finora
- Chillers VoltasDocumento4 pagineChillers Voltasanil shuklaNessuna valutazione finora
- Beastlikebalsam - Muscle BuildingDocumento10 pagineBeastlikebalsam - Muscle BuildingBalsam LaaroussiNessuna valutazione finora
- Recruitment and Selection in Canada 7Th by Catano Wiesner Full ChapterDocumento22 pagineRecruitment and Selection in Canada 7Th by Catano Wiesner Full Chaptermary.jauregui841100% (51)
- Islam and Civilization (Analysis Study On The History of Civilization in Islam) Muhammad Hifdil IslamDocumento18 pagineIslam and Civilization (Analysis Study On The History of Civilization in Islam) Muhammad Hifdil IslamLoveth KonniaNessuna valutazione finora
- MSDS DowthermDocumento4 pagineMSDS DowthermfebriantabbyNessuna valutazione finora
- Joby Aviation - Analyst Day PresentationDocumento100 pagineJoby Aviation - Analyst Day PresentationIan TanNessuna valutazione finora
- Model Detailed Project Report: Animal Feed Making UnitDocumento19 pagineModel Detailed Project Report: Animal Feed Making UnitShashi ShekharNessuna valutazione finora
- An Autobiography of Trauma: A Healing JourneyDa EverandAn Autobiography of Trauma: A Healing JourneyValutazione: 5 su 5 stelle5/5 (2)
- Summary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisDa EverandSummary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisValutazione: 4 su 5 stelle4/5 (9)
- The Complex PTSD Workbook: A Mind-Body Approach to Regaining Emotional Control & Becoming WholeDa EverandThe Complex PTSD Workbook: A Mind-Body Approach to Regaining Emotional Control & Becoming WholeValutazione: 4.5 su 5 stelle4.5/5 (49)
- My Grandmother's Hands: Racialized Trauma and the Pathway to Mending Our Hearts and BodiesDa EverandMy Grandmother's Hands: Racialized Trauma and the Pathway to Mending Our Hearts and BodiesValutazione: 5 su 5 stelle5/5 (70)
- Rewire Your Anxious Brain: How to Use the Neuroscience of Fear to End Anxiety, Panic, and WorryDa EverandRewire Your Anxious Brain: How to Use the Neuroscience of Fear to End Anxiety, Panic, and WorryValutazione: 4.5 su 5 stelle4.5/5 (157)
- The Upward Spiral: Using Neuroscience to Reverse the Course of Depression, One Small Change at a TimeDa EverandThe Upward Spiral: Using Neuroscience to Reverse the Course of Depression, One Small Change at a TimeValutazione: 4.5 su 5 stelle4.5/5 (140)
- Summary of The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma by Bessel van der Kolk MDDa EverandSummary of The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma by Bessel van der Kolk MDValutazione: 4.5 su 5 stelle4.5/5 (167)
- Vagus Nerve: A Complete Self Help Guide to Stimulate and Activate Vagal Tone — A Self Healing Exercises to Reduce Chronic Illness, PTSD, Anxiety, Inflammation, Depression, Trauma, and AngerDa EverandVagus Nerve: A Complete Self Help Guide to Stimulate and Activate Vagal Tone — A Self Healing Exercises to Reduce Chronic Illness, PTSD, Anxiety, Inflammation, Depression, Trauma, and AngerValutazione: 4.5 su 5 stelle4.5/5 (16)
- Rapid Weight Loss Hypnosis: How to Lose Weight with Self-Hypnosis, Positive Affirmations, Guided Meditations, and Hypnotherapy to Stop Emotional Eating, Food Addiction, Binge Eating and MoreDa EverandRapid Weight Loss Hypnosis: How to Lose Weight with Self-Hypnosis, Positive Affirmations, Guided Meditations, and Hypnotherapy to Stop Emotional Eating, Food Addiction, Binge Eating and MoreValutazione: 5 su 5 stelle5/5 (17)
- The Worry Trick: How Your Brain Tricks You into Expecting the Worst and What You Can Do About ItDa EverandThe Worry Trick: How Your Brain Tricks You into Expecting the Worst and What You Can Do About ItValutazione: 4.5 su 5 stelle4.5/5 (107)
- Somatic Therapy Workbook: A Step-by-Step Guide to Experiencing Greater Mind-Body ConnectionDa EverandSomatic Therapy Workbook: A Step-by-Step Guide to Experiencing Greater Mind-Body ConnectionNessuna valutazione finora
- Don't Panic: Taking Control of Anxiety AttacksDa EverandDon't Panic: Taking Control of Anxiety AttacksValutazione: 4 su 5 stelle4/5 (12)
- BORDERLINE PERSONALITY DISORDER: Help Yourself and Help Others. Articulate Guide to BPD. Tools and Techniques to Control Emotions, Anger, and Mood Swings. Save All Your Relationships and Yourself. NEW VERSIONDa EverandBORDERLINE PERSONALITY DISORDER: Help Yourself and Help Others. Articulate Guide to BPD. Tools and Techniques to Control Emotions, Anger, and Mood Swings. Save All Your Relationships and Yourself. NEW VERSIONValutazione: 4.5 su 5 stelle4.5/5 (24)
- Brain Inflamed: Uncovering the Hidden Causes of Anxiety, Depression, and Other Mood Disorders in Adolescents and TeensDa EverandBrain Inflamed: Uncovering the Hidden Causes of Anxiety, Depression, and Other Mood Disorders in Adolescents and TeensValutazione: 5 su 5 stelle5/5 (2)
- Summary: No Bad Parts: Healing Trauma and Restoring Wholeness with the Internal Family Systems Model by Richard C. Schwartz PhD & Alanis Morissette: Key Takeaways, Summary & AnalysisDa EverandSummary: No Bad Parts: Healing Trauma and Restoring Wholeness with the Internal Family Systems Model by Richard C. Schwartz PhD & Alanis Morissette: Key Takeaways, Summary & AnalysisValutazione: 5 su 5 stelle5/5 (5)
- Binaural Beats: Activation of pineal gland – Stress reduction – Meditation – Brainwave entrainment – Deep relaxationDa EverandBinaural Beats: Activation of pineal gland – Stress reduction – Meditation – Brainwave entrainment – Deep relaxationValutazione: 5 su 5 stelle5/5 (9)
- A Profession Without Reason: The Crisis of Contemporary Psychiatry—Untangled and Solved by Spinoza, Freethinking, and Radical EnlightenmentDa EverandA Profession Without Reason: The Crisis of Contemporary Psychiatry—Untangled and Solved by Spinoza, Freethinking, and Radical EnlightenmentNessuna valutazione finora
- Critical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsDa EverandCritical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsValutazione: 4.5 su 5 stelle4.5/5 (39)
- Heal the Body, Heal the Mind: A Somatic Approach to Moving Beyond TraumaDa EverandHeal the Body, Heal the Mind: A Somatic Approach to Moving Beyond TraumaValutazione: 4.5 su 5 stelle4.5/5 (56)
- Winning the War in Your Mind: Change Your Thinking, Change Your LifeDa EverandWinning the War in Your Mind: Change Your Thinking, Change Your LifeValutazione: 5 su 5 stelle5/5 (558)
- Redefining Anxiety: What It Is, What It Isn't, and How to Get Your Life BackDa EverandRedefining Anxiety: What It Is, What It Isn't, and How to Get Your Life BackValutazione: 4.5 su 5 stelle4.5/5 (152)
- When Religion Hurts You: Healing from Religious Trauma and the Impact of High-Control ReligionDa EverandWhen Religion Hurts You: Healing from Religious Trauma and the Impact of High-Control ReligionValutazione: 4 su 5 stelle4/5 (11)
- I Don't Want to Talk About It: Overcoming the Secret Legacy of Male DepressionDa EverandI Don't Want to Talk About It: Overcoming the Secret Legacy of Male DepressionValutazione: 4.5 su 5 stelle4.5/5 (106)
- Feel the Fear… and Do It Anyway: Dynamic Techniques for Turning Fear, Indecision, and Anger into Power, Action, and LoveDa EverandFeel the Fear… and Do It Anyway: Dynamic Techniques for Turning Fear, Indecision, and Anger into Power, Action, and LoveValutazione: 4 su 5 stelle4/5 (250)