Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
53
Caricato da
davidmarkovic032Descrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
53
Caricato da
davidmarkovic032Copyright:
Formati disponibili
Ch03-X3706.
qxd
6/25/07
12:24 PM
Page 42
42 The Developing Human
Formation of the Bilaminar Embryonic Disc: Second Week
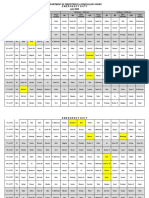
Completion of Implantation and Continuation of Embryonic Development Formation of the Amniotic Cavity, Embryonic Disc, and Umbilical Vesicle Development of the Chorionic Sac Implantation Sites of Blastocysts Summary of Implantation Summary of the Second Week Clinically Oriented Problems 43 44 45 45 48 51 53
42
Ch03-X3706.qxd
6/25/07
12:24 PM
Page 43
Formation of the Bilaminar Embryonic Disc: Second Week 43 Implantation of the blastocyst is completed during the second week. As this process occurs, morphologic changes in the embryoblast produce a bilaminar embryonic disc composed of epiblast and hypoblast (Fig. 3-1A). The embryonic disc gives rise to the germ layers that form all the tissues and organs of the embryo. Extraembryonic structures forming during the second week are the amniotic cavity, amnion, umbilical vesicle (yolk sac), connecting stalk, and chorionic sac.
Uterine gland Endometrial capillary
Syncytiotrophoblast
COMPLETION OF IMPLANTATION AND CONTINUATION OF EMBRYONIC DEVELOPMENT
Implantation of the blastocyst is completed by the end of the second week. It occurs during a restricted time period 6 to 10 days after ovulation. As the blastocyst implants (see Fig. 3-1), more trophoblast contacts the endometrium and differentiates into The cytotrophoblast, a layer of cells that is mitotically active and forms new cells that migrate into the increasing mass of syncytiotrophoblast, where they fuse and lose their cell membranes The syncytiotrophoblast, a rapidly expanding, multinucleated mass in which no cell boundaries are discernible The erosive syncytiotrophoblast invades the endometrial connective tissue, and the blastocyst slowly embeds itself in the endometrium. Syncytiotrophoblastic cells displace endometrial cells at the implantation site. The endometrial cells undergo apoptosis (programmed cell death), which facilitates the invasion. The molecular mechanisms of implantation involve synchronization between the invading blastocyst and a receptive endometrium. The microvilli of endometrial cells (pinopodes), cell adhesion molecules, cytokines, prostaglandins, homeobox genes, growth factors, and matrix metalloproteins play a role in making the endometrium receptive. The connective tissue cells around the implantation site accumulate glycogen and lipids and assume a polyhedral appearance. Some of these cellsdecidual cells degenerate adjacent to the penetrating syncytiotrophoblast. The syncytiotrophoblast engulfs these degenerating cells, providing a rich source of embryonic nutrition. The syncytiotrophoblast produces a hormonehuman chorionic gonadotrophin (hCG), which enters the maternal blood via lacunae (Latin, hollow cavities) in the syncytiotrophoblast (see Fig. 3-1C). hCG maintains the hormonal activity of the corpus luteum in the ovary during pregAmniotic cavity Epiblast Amnion Endometrial epithelium
Exocoelomic cavity Exocoelomic membrane
Cytotrophoblast Hypoblast
Syncytiotrophoblast Amnion Bilaminar embryonic disc Exocoelomic membrane Exocoelomic cavity
B
Cytotrophoblast
Amnion
Uterine gland
Maternal blood in lacunae
FIGURE 3-1. Implantation of a blastocyst in the endometrium. The
actual size of the conceptus is 0.1 mm, approximately the size of the period at the end of this sentence. A, Drawing of a section through a blastocyst partially implanted in the endometrium (approximately 8 days). Note the slitlike amniotic cavity. B, An enlarged three-dimensional sketch of a slightly older blastocyst after removal from the endometrium. Note the extensive syncytiotrophoblast at the embryonic pole (side of the blastocyst containing the embryonic disc). C, Drawing of a section through a blastocyst of approximately 9 days implanted in the endometrium. Note the lacunae appearing in the syncytiotrophoblast. The term yolk sac is a misnomer because it contains no yolk. Bilaminar embryonic disc
Primary umbilical vesicle (yolk sac)
Extraembryonic mesoderm
Endometrial epithelium
Ch03-X3706.qxd
6/25/07
12:24 PM
Page 44
44 The Developing Human nancy. The corpus luteum is an endocrine glandular structure that secretes estrogen and progesterone to maintain the pregnancy. Highly sensitive radioimmunoassays are available for detecting hCG and pregnancy and forms the basis for pregnancy tests. Enough hCG is produced by the syncytiotrophoblast at the end of the second week to give a positive pregnancy test, even though the woman is probably unaware that she is pregnant.
Amnion Syncytiotrophoblast
Endometrial capillary
Lacunar network
FORMATION OF THE AMNIOTIC CAVITY, EMBRYONIC DISC, AND UMBILICAL VESICLE
As implantation of the blastocyst progresses, a small space appears in the embryoblast. This space is the primordium of the amniotic cavity (see Fig. 3-1A). Soon amniogenic (amnion-forming) cellsamnioblastsseparate from the epiblast and form the amnion, which encloses the amniotic cavity (see Fig. 3-1B and C). Concurrently, morphologic changes occur in the embryoblast that result in the formation of a flat, almost circular bilaminar plate of cells, the embryonic disc, consisting of two layers (Fig. 3-2A): Epiblast, the thicker layer, consisting of high columnar cells related to the amniotic cavity Hypoblast, consisting of small cuboidal cells adjacent to the exocoelomic cavity The epiblast forms the floor of the amniotic cavity and is continuous peripherally with the amnion. The hypoblast forms the roof of the exocoelomic cavity and is continuous with the thin exocoelomic membrane (see Fig. 3-1B). This membrane, together with the hypoblast, lines the primary umbilical vesicle. The embryonic disc now lies between the amniotic cavity and the umbilical vesicle (see Fig. 3-1C). Cells from the vesicle endoderm form a layer of connective tissue, the extraembryonic mesoderm (see Fig. 3-2A), which surrounds the amnion and umbilical vesicle. This mesoderm continues to form from cells that arise from the primitive streak (see Fig. 4-3). The umbilical vesicle and amniotic cavities make morphogenetic movements of the cells of the embryonic disc possible. As the amnion, embryonic disc, and primary umbilical vesicle form, isolated cavities lacunaeappear in the syncytiotrophoblast (see Figs. 3-1C and 3-2). The lacunae soon become lled with a mixture of maternal blood from ruptured endometrial capillaries and cellular debris from eroded uterine glands. The fluid in the lacunar spaces embryotroph (Greek, trophe, nourishment)passes to the embryonic disc by diffusion and provides nutritive material to the embryo. The communication of the eroded endometrial capillaries with the lacunae establishes the primordial uteroplacental circulation. When maternal blood flows into the lacunae, oxygen and nutritive substances are available to the embryo. Oxygenated blood passes into the lacunae from the spiral endometrial arteries, and poorly oxygenated blood is removed from them through the endometrial veins. The 10-day human conceptus (embryo and extraembryonic membranes) is completely embedded in the endometrium (see Fig. 3-2A). For approximately 2 days, there is a defect in
Epiblast Cytotrophoblast
Primary umbilical vesicle
Closing plug
Hypoblast
Extraembryonic mesoderm
Actual size of implanted blastocyst :
Eroded gland
Maternal blood
Lacunar network
Amniotic cavity Uterine gland
Extraembryonic coelomic space Extraembryonic endodermal lining of umbilical vesicle (yolk sac)
Embryonic disc
Cytotrophoblast
FIGURE 3-2. Implanted blastocysts. A, At 10 days; B, at 12 days.
This stage of development is characterized by communication of the blood-lled lacunar networks. Note in B that coelomic spaces have appeared in the extraembryonic mesoderm, forming the beginning of the extraembryonic coelom.
the endometrial epithelium that is lled by a closing plug, a brinous coagulum of blood. By day 12, an almost completely regenerated uterine epithelium covers the closing plug (see Fig. 3-2B). As the conceptus implants, the endometrial connective tissue cells undergo a transformation, the decidual reaction. After the cells swell because of the accumulation of glycogen and lipid in their cytoplasm, they are known as decidual cells. The primary function of the decidual reaction is to provide nutrition for the early embryo and an immunologically privileged site for the conceptus.
Ch03-X3706.qxd
6/25/07
12:24 PM
Page 45
Formation of the Bilaminar Embryonic Disc: Second Week 45 growth of these extensions is thought to be induced by the underlying extraembryonic somatic mesoderm. The cellular projections form primary chorionic villi, the rst stage in the development of the chorionic villi of the placenta. The extraembryonic coelom splits the extraembryonic mesoderm into two layers (see Fig. 3-5A and B): Extraembryonic somatic mesoderm, lining the trophoblast and covering the amnion Extraembryonic splanchnic mesoderm, surrounding the umbilical vesicle The extraembryonic somatic mesoderm and the two layers of trophoblast form the chorion (see Fig. 3-7B). The chorion forms the wall of the chorionic sac, within which the embryo and its amniotic sac and umbilical vesicle are suspended by the connecting stalk. The extraembryonic coelom is now called the chorionic cavity. The amniotic sac and the umbilical vesicle can be thought of as two balloons pressed together (at the site of embryonic disc) and suspended by a cord (connecting stalk) from the inside of a larger balloon (chorionic sac). Transvaginal ultrasonography (endovaginal sonography) is used for measuring the chorionic (gestational) sac diameter (Fig. 3-8). This measurement is valuable for evaluating early embryonic development and pregnancy outcome. The 14-day embryo still has the form of a flat bilaminar embryonic disc (see Fig. 3-9), but the hypoblastic cells in a localized area are now columnar and form a thickened circular areathe prechordal plate (see Fig. 3-5B and C), which indicates the future site of the mouth and an important organizer of the head region.
FIGURE 3-3. Photograph of the endometrial surface of the uterus,
showing the implantation site of the 12-day embryo shown in Figure 3-4. The implanted conceptus produces a small elevation (arrow) (8). (From Hertig AT, Rock J: Contrib Embryol Carnegie Inst 29:127, 1941. Courtesy of the Carnegie Institution of Washington.)
In a 12-day embryo, adjacent syncytiotrophoblastic lacunae have fused to form lacunar networks (see Fig. 3-2B), giving the syncytiotrophoblast a spongelike appearance. The lacunar networks, particularly obvious around the embryonic pole, are the primordia of the intervillous spaces of the placenta (see Chapter 7). The endometrial capillaries around the implanted embryo become congested and dilated to form sinusoids, thinwalled terminal vessels that are larger than ordinary capillaries. The syncytiotrophoblast erodes the sinusoids, and maternal blood flows freely into the lacunar networks. The trophoblast absorbs nutritive fluid from the lacunar networks, which is transferred to the embryo. Growth of the bilaminar embryonic disc is slow compared with growth of the trophoblast (see Figs. 3-1 and 3-2). The implanted 12-day embryo produces a minute elevation on the endometrial surface that protrudes into the uterine lumen (Figs. 3-3 and 3-4). As changes occur in the trophoblast and endometrium, the extraembryonic mesoderm increases and isolated extraembryonic coelomic spaces appear within it (see Figs. 3-2 and 3-4). These spaces rapidly fuse to form a large isolated cavity, the extraembryonic coelom (Fig. 3-5A). This fluid-lled cavity surrounds the amnion and umbilical vesicle, except where they are attached to the chorion by the connecting stalk. As the extraembryonic coelom forms, the primary umbilical vesicle decreases in size and a smaller secondary umbilical vesicle forms (see Fig. 3-5B). This smaller vesicle is formed by extraembryonic endodermal cells that migrate from the hypoblast inside the primary umbilical vesicle (Fig. 3-6). During formation of the secondary umbilical vesicle, a large part of the primary umbilical vesicle is pinched off (see Fig. 3-5B). The umbilical vesicle contains no yolk; however, it has important functions (e.g., it is the site of origin of primordial germ cells [see Chapter 12]). It may have a role in the selective transfer of nutrients to the embryo.
IMPLANTATION SITES OF BLASTOCYSTS
Implantation of blastocysts usually occurs in the endometrium of the uterus, superior in the body of the uterus, slightly more often on the posterior than on the anterior wall. Implantation of a blastocyst can be detected by ultrasonography and highly sensitive radioimmunoassays of hCG as early as the end of the second week.
EXTRAUTERINE IMPLANTATION
Blastocysts may implant outside the uterus. These implantations result in ectopic pregnancies; 95% to 98% of ectopic implantations occur in the uterine tubes, most often in the ampulla and isthmus (Figs. 3-10 to 3-12). The incidence of ectopic pregnancy has increased in most countries, ranging from 1 in 80 to 1 in 250 pregnancies, depending on the socioeconomic level of the population. In the United States, the frequency of ectopic pregnancy is approximately 2% of all pregnancies, and it is the main cause of maternal deaths during the rst trimester. A woman with a tubal pregnancy has signs and symptoms of pregnancy (e.g., misses her menstrual period). She may also experience abdominal pain
DEVELOPMENT OF THE CHORIONIC SAC
The end of the second week is characterized by the appearance of primary chorionic villi (Figs. 3-5 and 3-7). Proliferation of cytotrophoblastic cells produces cellular extensions that grow into the syncytiotrophoblast. The
Ch03-X3706.qxd
6/25/07
12:24 PM
Page 46
46 The Developing Human
Spongy layer
Endometrial glands
Endometrial blood vessels Compact layer Endometrial epithelium
Embryonic disc
Closing plug
Embryonic hypoblast
Embryonic epiblast
Amnion Lacunar network Cytotrophoblast SyncytioFIGURE 3-4. Implanted blastocyst. trophoblast A, Section through the implantation site of the 12-day embryo described in Figure 3-3. The embryo is Primary embedded supercially in the compact layer of the endometrium umbilical (30). B, Higher magnication of the vesicle conceptus and surrounding (yolk sac) endometrium (100). Lacunae containing maternal blood are visible in the syncytiotrophoblast. (From ExtraHertig AT, Rock J: Contrib Embryol embryonic Carnegie Inst 29:127, 1941. mesoderm Courtesy of the Carnegie Institution of Washington.)
Extraembryonic coelom
and tenderness because of distention of the uterine tube, abnormal bleeding, and irritation of the pelvic peritoneum (peritonitis). The pain may be confused with appendicitis if the pregnancy is in the right uterine tube. Ectopic pregnancies produce -human chorionic gonadotropin at a slower rate than normal pregnancies; consequently -human chorionic gonadotropin assays may give false-negative results if performed too early. Transvaginal ultrasonography is very helpful in the early detection of ectopic tubal pregnancies. There are several causes of tubal pregnancy, but they are often related to factors that delay or prevent
transport of the cleaving zygote to the uterus, for example, by mucosal adhesions in the uterine tube or from blockage of it that is caused by scarring resulting from pelvic inflammatory disease. Ectopic tubal pregnancies usually result in rupture of the uterine tube and hemorrhage into the peritoneal cavity during the rst 8 weeks, followed by death of the embryo. Tubal rupture and hemorrhage constitute a threat to the mothers life. The affected tube and conceptus are usually surgically removed (see Fig. 3-12). When blastocysts implant in the isthmus of the uterine tube (see Fig. 3-11D), the tube tends to
Ch03-X3706.qxd
6/25/07
12:24 PM
Page 47
Formation of the Bilaminar Embryonic Disc: Second Week 47
Extraembryonic Maternal somatic mesoderm sinusoid Lacunar network Primary chorionic villus
Endometrium
Chorion
Extraembryonic splanchnic mesoderm
Extraembryonic coelom
Primary umbilical vesicle (yolk sac)
Maternal blood
Primary chorionic villus
Connecting stalk
Secondary umbilical vesicle (yolk sac) Prechordal plate
rupture early because this narrow part of the tube is relatively unexpandable, and often with extensive bleeding, probably because of the rich anastomoses between ovarian and uterine vessels in this area. When blastocysts implant in the uterine (intramural) part of the tube (see Fig. 3-11E), they may develop beyond 8 weeks before expulsion occurs. When a uterine tubal pregnancy ruptures, it usually bleeds profusely. Blastocysts that implant in the ampulla or on mbriae of the uterine tube may be expelled into the peritoneal cavity where they commonly implant in the rectouterine pouch. In exceptional cases, an abdominal pregnancy may continue to full term and the fetus may be delivered alive through an abdominal incision. Usually, however, the placenta attaches to abdominal organs (Fig. 3-11G) and causes considerable intraperitoneal bleeding. Abdominal pregnancy increases the risk of maternal death from hemorrhage by a factor of 90 when compared with intrauterine pregnancy, and seven times more than that for tubal pregnancy. In very unusual cases, an abdominal conceptus dies and is not detected; the fetus becomes calcied, forming a stone fetuslithopedion (Greek, lithos, stone, + paidion, child). Simultaneous intrauterine and extrauterine pregnancies are unusual, occurring approximately 1 in 7000. The ectopic pregnancy is masked initially by the presence of the uterine pregnancy. Usually the ectopic pregnancy can be terminated by surgical removal of the involved uterine tube without interfering with the intrauterine pregnancy (see Fig. 3-12). Cervical implantations are unusual (see Fig. 3-11); in some cases, the placenta becomes rmly attached to brous and muscular tissues of the cervix, often resulting in bleeding and requiring subsequent surgical intervention, such as hysterectomy (excision of uterus).
Remnant of primary umbilical vesicle
Endometrial epithelium
Extraembryonic somatic mesoderm
Amnion
Epiblast
Hypoblast
FIGURE 3-5. Drawings of sections through implanted human
Bilaminar embryonic disc Prechordal plate embryos, based mainly on Hertig and colleagues (1956). Observe that (1) the defect in the endometrial epithelium has disappeared; (2) a small secondary umbilical vesicle has formed; (3) a large cavity, the extraembryonic coelom, now surrounds the umbilical vesicle and amnion, except where the amnion is attached to the chorion by the connecting stalk; and (4) the extraembryonic coelom splits the extraembryonic mesoderm into two layers: extraembryonic somatic mesoderm lining the trophoblast and covering the amnion and the extraembryonic splanchnic mesoderm around the umbilical vesicle. A, At 13 days, illustrating the decrease in relative size of the primary umbilical vesicle and the early appearance of primary chorionic villi. B, At 14 days, showing the newly formed secondary umbilical vesicle and the location of the prechordal plate in its roof. C, Detail of the prechordal plate outlined in B.
Ch03-X3706.qxd
6/25/07
12:24 PM
Page 48
48 The Developing Human
Ectoderm of amnion
Extraembryonic mesoderm Epiblast Embryonic ectoderm Embryonic mesoderm
Primitive streak (see Chapter 4)
Notochordal process
Bilaminar embryonic disc
Embryonic endoderm
Endoderm of umbilical vesicle
Extraembryonic mesoderm
Hypoblast
FIGURE 3-6. Origin of embryonic tissues. The colors in the boxes are used in drawings of sections of conceptuses.
SUMMARY OF IMPLANTATION
Implantation of the blastocyst begins at the end of the rst week and is completed by the end of the second week. The cellular and molecular events relating to implantation are complex. It involves a receptive endometrium and hormonal factors, such as estrogen, progesterone, prolactin, as well as cell adhesion molecules, growth factors, and HOX genes, Implantation may be summarized as follows: The zona pellucida degenerates (day 5). Its disappearance results from enlargement of the blastocyst and degeneration caused by enzymatic lysis. The lytic enzymes are released from the acrosomes of the sperms that surround and partially penetrate the zona pellucida. The blastocyst adheres to the endometrial epithelium (day 6). The trophoblast differentiates into two layers: the syncytiotrophoblast and cytotrophoblast (day 7). The syncytiotrophoblast erodes endometrial tissues, and the blastocyst starts to embed in the endometrium (day 8). Blood-lled lacunae appear in the syncytiotrophoblast (day 9). The blastocyst sinks beneath the endometrial epithelium, and the defect is lled by a closing plug (day 10).
Lacunar networks form by fusion of adjacent lacunae (days 10 and 11). The syncytiotrophoblast erodes endometrial blood vessels, allowing maternal blood to seep in and out of lacunar networks, thereby establishing a uteroplacental circulation (days 11 and 12). The defect in the endometrial epithelium is repaired (days 12 and 13). Primary chorionic villi develop (days 13 and 14).
PLACENTA PREVIA
Implantation of a blastocyst in the inferior segment of the uterus near the internal os results in placenta previa, a placenta that partially or completely covers the os (see Fig. 3-11). Placenta previa may cause bleeding because of premature separation of the placenta during pregnancy or at delivery of the fetus (see Chapter 7).
SPONTANEOUS ABORTION
OF
EMBRYOS
Most spontaneous abortions of embryos occur during the rst 3 weeks. Sporadic and recurrent
Ch03-X3706.qxd
6/25/07
12:24 PM
Page 49
Formation of the Bilaminar Embryonic Disc: Second Week 49
Maternal blood Trophoblastic lacunar network Extraembryonic somatic mesoderm Primary chorionic villus Syncytiotrophoblast
Cytotrophoblastic core
Chorionic sac
Embryo Chorionic cavity
FIGURE 3-7. A, Detail of the section (outlined in B) of the wall of the chorionic sac. B, Sketch of a 14-day conceptus illustrating the chorionic sac and the shaggy appearance of it created by the primary chorionic villi. C, Drawing of a transverse section through a primary chorionic villus.
FIGURE 3-8. Endovaginal sonogram of an early chorionic (gestational)
sac. The mean gestational sac diameter is determined by adding the three orthogonal dimensions (length, depth, and width) and dividing by 3. (From Laing FC, Frates MC: Ultrasound evaluation during the rst trimester of pregnancy. In Callen PW [ed]: Ultrasonography in Obstetrics and Gynecology, 4th ed. Philadelphia, WB Saunders, 2000.)
spontaneous abortions are two of the most common gynecologic problems. The frequency of early abortions is difcult to establish because they often occur before a woman is aware that she is pregnant. An abortion occurring several days after the rst missed period is very likely to be mistaken for a delayed menstruation. Detection of a conceptus in the menses (menstrual blood) is very difcult because of its small size. Study of most early spontaneous abortions resulting from medical problems reveals abnormal conceptuses. More than 50% of all known spontaneous abortions result from chromosomal abnormalities. The higher incidence of early abortions in older women probably results from the increasing frequency of nondisjunction during oogenesis (see Chapter 2). It has been estimated that from 30% to 50% of all zygotes never develop into blastocysts and implant. Failure of blastocysts to implant may result from a poorly developed endometrium; however, in many cases, there are probably lethal chromosomal abnormalities in the embryo. There is a higher incidence of spontaneous abortion of fetuses with neural tube defects, cleft lip, and cleft palate.
Ch03-X3706.qxd
6/25/07
12:24 PM
Page 50
50 The Developing Human
Decidua basalis
Lacunar network
Maternal blood
Embryonic disc
Connecting stalk and amnion Umbilical vesicle (yolk sac)
Extraembryonic coelom Chorion and chorionic villi Endometrial epithelium
Lacunar network containing maternal blood Trophoblast
Connecting stalk Amniotic cavity Amnion Epiblast Hypoblast Bilaminar embryonic disc
Secondary umbilical vesicle
Wall of umbilical vesicle
Extraembryonic coelom (primordium of chorionic cavity)
B
FIGURE 3-9. Photomicrographs of longitudinal sections of an implanted embryo at Carnegie stage 6, approximately 14 days. Note the large size
of the extraembryonic coelom. A, Low-power view (18). B, High-power view (95). The embryo is represented by the bilaminar embryonic disc composed of epiblast and hypoblast. (From Nishimura H [ed]: Atlas of Human Prenatal Histology. Tokyo, Igaku-Shoin, 1983.)
Ch03-X3706.qxd
6/25/07
12:24 PM
Page 51
Formation of the Bilaminar Embryonic Disc: Second Week 51
Embryo and extraembryonic membranes Isthmus Site of ectopic tubal pregnancy
Ampulla
FIGURE 3-10. A, Frontal section of the uterus and left uterine tube, illustrating an ectopic pregnancy in the ampulla of the tube. B, Ectopic tubal
pregnancy. This axial sonogram through the left adnexa (placenta and extraembryonic membranes) of a 6-week pregnant patient shows a small chorionic or gestational sac (arrow) in the left uterine tube with prominent vascularity in its periphery. This is characteristic of an ectopic tubal pregnancy. The incidence of tubal pregnancy ranges from 1 in 80 to 1 in 250 pregnancies. Most ectopic implantations (95% to 97%) occur in the uterine tube, usually in the isthmus or ampulla. (Courtesy of E.A. Lyons, MD, Professor of Radiology and Obstetrics and Gynecology, Health Sciences Centre, University of Manitoba, Winnipeg, Manitoba, Canada.)
INHIBITION
OF IMPLANTATION
SUMMARY OF THE SECOND WEEK
The administration of relatively large doses of progestins and/or estrogens (morning-after pills) for several days, beginning shortly after unprotected sexual intercourse, usually does not prevent fertilization but often prevents implantation of the blastocyst. A high dose of diethylstilbestrol, given daily for 5 to 6 days, may also accelerate passage of the cleaving zygote along the uterine tube. Normally, the endometrium progresses to the secretory phase of the menstrual cycle as the zygote forms, undergoes cleavage, and enters the uterus. The large amount of estrogen disturbs the normal balance between estrogen and progesterone that is necessary for preparation of the endometrium for implantation. An intrauterine device inserted into the uterus through the vagina and cervix usually interferes with implantation by causing a local inflammatory reaction. Some intrauterine devices contain progesterone that is slowly released and interferes with the development of the endometrium so that implantation does not usually occur.
Rapid proliferation and differentiation of the trophoblast occurs as the blastocyst completes its implantation in the endometrium. The endometrial changes resulting from the adaptation of these tissues in preparation for implantation are known as the decidual reaction. Concurrently, the primary umbilical vesicle (yolk sac) forms and extraembryonic mesoderm develops. The extraembryonic coelom forms from spaces that develop in the extraembryonic mesoderm. The coelom later becomes the chorionic cavity. The primary umbilical vesicle becomes smaller and gradually disappears as the secondary umbilical vesicle develops. The amniotic cavity appears as a space between the cytotrophoblast and the embryoblast. The embryoblast differentiates into a bilaminar embryonic disc consisting of epiblast, related to the amniotic cavity, and hypoblast, adjacent to the blastocyst cavity. The prechordal plate develops as a localized thickening of the hypoblast, which indicates the future
Ch03-X3706.qxd
6/25/07
12:24 PM
Page 52
52 The Developing Human
Intestine
D E
Mesentery
X
A H
Ovary
Implantation at internal os
Cervical implantation
FIGURE 3-11. Implantation sites of blastocysts. The usual site in the posterior wall of the uterus is indicated by an X. The approximate order of frequency of ectopic implantations is indicated alphabetically (A, most common, H, least common). A to F, tubal pregnancies; G, abdominal pregnancy; H, ovarian pregnancy. Tubal pregnancies are the most common type of ectopic pregnancy. Although appropriately included with uterine pregnancy sites, a cervical pregnancy is often considered to be an ectopic pregnancy.
Uterine tube Chorionic sac
A
Embryo
FIGURE 3-12. A tubal pregnancy. A, The uterine tube has been surgically removed and sectioned to show the conceptus implanted in the
mucous membrane (3). B, Enlarged photograph of the normal-appearing 4-week embryo (13). (Courtesy of Professor Jean Hay [retired], Department of Anatomy and Cell Science, University of Manitoba, Winnipeg, Manitoba, Canada.)
Ch03-X3706.qxd
6/25/07
12:24 PM
Page 53
Formation of the Bilaminar Embryonic Disc: Second Week 53 cranial region of the embryo and the future site of the mouth; the prechordal plate is also an important organizer of the head region. What would the physician likely tell her? Can women over 40 have normal babies? What tests and diagnostic techniques would likely be performed? Discussion of these problems appears at the back of the book.
CLINICALLY ORIENTED PROBLEMS CASE 3-1
A 22-year-old woman who complained of a severe chest cold was sent for a radiograph of her thorax. Is it advisable to examine a healthy females chest radiographically during the last week of her menstrual cycle? Are birth defects likely to develop in her conceptus if she happens to be pregnant?
References and Suggested Reading
Attar E: Endocrinology of ectopic pregnancy. Obstet Gynecol Clin N Am 31:779, 2004. Bianchi DW, Wilkins-Haug LE, Enders AC, Hay ED: Origin of extraembryonic mesoderm in experimental animals: relevance to chorionic mosaicism in humans. Am J Med Genet 46:542, 1993. Bukulmez O, Arici A: Luteal phase defect: Myth or reality. Obstet Gynecol Clin N Am 31:727. 2004. Cadkin AV, McAlpin J: The decidua-chorionic sac: A reliable sonographic indicator of intrauterine pregnancy prior to detection of a fetal pole. J Ultrasound Med 3:539, 1984. Coulam CB, Faulk WP, McIntyre JA: Spontaneous and recurrent abortions. In Quilligan EJ, Zuspan FP (eds): Current Therapy in Obstetrics and Gynecology, Vol 3. Philadelphia, WB Saunders, 1990. Dickey RP, Gasser R, Olar TT, et al: Relationship of initial chorionic sac diameter to abortion and abortus karyotype based on new growth curves for the 16 to 49 post-ovulation day. Hum Reprod 9:559, 1994. Enders AC, King BF: Formation and differentiation of extraembryonic mesoderm in the rhesus monkey. Am J Anat 181:327, 1988. Hertig AT, Rock J: Two human ova of the pre-villous stage, having a development age of about seven and nine days respectively. Contrib Embryol Carnegie Inst 31:65, 1945. Hertig AT, Rock J: Two human ova of the pre-villous stage, having a developmental age of about eight and nine days, respectively. Contrib Embryol Carnegie Inst 33:169, 1949. Hertig AT, Rock J, Adams EC: A description of 34 human ova within the rst seventeen days of development. Am J Anat 98:435, 1956. Hertig AT, Rock J, Adams EC, Menkin MC: Thirty-four fertilized human ova, good, bad, and indifferent, recovered from 210 women of known fertility. Pediatrics 23:202, 1959. Kodaman PH, Taylor HS: Hormonal regulation of implantation. Obstet Gynecol Clin N Am 31:745, 2004. Lessey BA: The role of the endometrium during embryo implantation. Human Reprod 15(Suppl 6):39, 2000. Levine D: Ectopic pregnancy. In Callen PW (ed): Ultrasonography in Obstetrics and Gynecology, 4th ed. Philadelphia, WB Saunders, 2000. Lindsay DJ, Lovett IS, Lyons EA, et al: Endovaginal sonography: Yolk sac diameter and shape as a predictor of pregnancy outcome in the rst trimester. Radiology 183:115, 1992. Lipscomb GH: Ectopic pregnancy. In Copeland LJ, Jarrell JF (eds): Textbook of Gynecology, 4th ed. Philadelphia, WB Saunders, 2000. Luckett WP: The origin of extraembryonic mesoderm in the early human and rhesus monkey embryos. Anat Rec 169:369, 1971. Luckett WP: Origin and differentiation of the yolk sac and extraembryonic mesoderm in presomite human and rhesus monkey embryos. Am J Anat 152:59, 1978. Nogales FF (ed): The Human Yolk Sac and Yolk Sac Tumors. New York, Springer-Verlag, 1993. Sen C, Yayla M: Chromosomal abnormalities of the embryo. In Kurjak A, Chervenak FA, Carrera JM (eds): The Embryo as a Patient. New York, Parthenon Publishing Group, 2001. Streeter GL: Developmental horizons in human embryos. Description of age group XI, 13 to 20 somites, and age group XII, 21 to 29 somites. Contrib Embryol Carnegie Inst 30:211, 1942.
CASE 3-2
A woman who was sexually assaulted during her fertile period was given large doses of estrogen twice for 1 day to interrupt a possible pregnancy. If fertilization had occurred, what do you think would be the mechanism of action of this hormone? What do lay people call this type of medical treatment? Is this what the media refer to as the abortion pill? If not, explain the method of action of the hormone treatment. How early can a pregnancy be detected?
CASE 3-3
A 23-year-old woman consulted her physician about severe right lower abdominal pain. She said that she had missed two menstrual periods. A diagnosis of ectopic pregnancy was made. What techniques might be used to enable this diagnosis to be made? What is the most likely site of the extrauterine gestation? How do you think the physician would likely treat the condition?
CASE 3-4
A 30-year-old woman had an appendectomy toward the end of her menstrual cycle; 81/2 months later, she had a child with a congenital anomaly of the brain. Could the surgery have produced this childs congenital anomaly? What is the basis for your views?
CASE 3-5
A 42-year-old woman nally became pregnant after many years of trying to conceive. She was concerned about the development of her baby.
Potrebbero piacerti anche
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Secondary Amenorrhea Testing AlgorithmDocumento1 paginaSecondary Amenorrhea Testing AlgorithmpolygoneNessuna valutazione finora
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Recent Advancement in Infertility ManagementDocumento18 pagineRecent Advancement in Infertility ManagementFarheen khan100% (2)
- Fertility and SubfertilityDocumento95 pagineFertility and SubfertilitydidiNessuna valutazione finora
- LESSON PLAN For COTDocumento5 pagineLESSON PLAN For COTMerrie Anne Pascual BagsicNessuna valutazione finora
- InfertilityDocumento10 pagineInfertilityits_piks7256Nessuna valutazione finora
- A Study To Assess The Effectiveness of Structured Teaching Programme On Pregnancy Induced Hypertension Among Antenatal Mothers in Selected Areas of RaichurDocumento19 pagineA Study To Assess The Effectiveness of Structured Teaching Programme On Pregnancy Induced Hypertension Among Antenatal Mothers in Selected Areas of Raichursanvar soniNessuna valutazione finora
- Chlamydia SlidesDocumento63 pagineChlamydia Slideslia primasari100% (1)
- Responsible Parenthood and Reproductive Health:: Family PlanningDocumento37 pagineResponsible Parenthood and Reproductive Health:: Family PlanningalyssaNessuna valutazione finora
- M Vanguardia-McnpDocumento11 pagineM Vanguardia-Mcnpmark OrpillaNessuna valutazione finora
- Management of Bleeding in Early PregnancyDocumento44 pagineManagement of Bleeding in Early PregnancyOyedele OluwaseunNessuna valutazione finora
- Department of Education: Learning Activity Sheet in Science 6Documento4 pagineDepartment of Education: Learning Activity Sheet in Science 6Tampok ES (Region III - Bulacan)Nessuna valutazione finora
- Pretest and PosttestDocumento3 paginePretest and PosttestMarissa FontanilNessuna valutazione finora
- New Estrogen and ProgesteroneDocumento39 pagineNew Estrogen and ProgesteroneWegrimel AriegaraNessuna valutazione finora
- 75 - PDFsam - GOMELLA 14Documento18 pagine75 - PDFsam - GOMELLA 14Chago MencosNessuna valutazione finora
- The Breasts Do Become Sensitive and Some Women DoDocumento14 pagineThe Breasts Do Become Sensitive and Some Women DoJaymih Santos AbasoloNessuna valutazione finora
- DR Case Pres Updated 1Documento30 pagineDR Case Pres Updated 1Ethan NamoNessuna valutazione finora
- Maternal and Child Nursing - Antenatal Practice Test With Answers and RationaleDocumento31 pagineMaternal and Child Nursing - Antenatal Practice Test With Answers and Rationalegelean payodNessuna valutazione finora
- Anatomy and Physiology: Patient P / Room No. 415 - 1Documento3 pagineAnatomy and Physiology: Patient P / Room No. 415 - 1Julianne B. Dela Cruz100% (1)
- Telaah JurnalDocumento5 pagineTelaah JurnalMade Angga DiningratNessuna valutazione finora
- RMS Senior B WangayaDocumento11 pagineRMS Senior B Wangayaimamsantos1191Nessuna valutazione finora
- guigoz milk - ស្វែងរក GoogleDocumento1 paginaguigoz milk - ស្វែងរក Googlelammei6868Nessuna valutazione finora
- Molar PregnancyDocumento15 pagineMolar Pregnancyapi-3705046Nessuna valutazione finora
- Newborn AssessmentDocumento3 pagineNewborn AssessmentMimie CaliNessuna valutazione finora
- Subamniotic Hematoma: Case Report and Review of LiteratureDocumento3 pagineSubamniotic Hematoma: Case Report and Review of LiteratureIJAR JOURNALNessuna valutazione finora
- Research Proposal o NishaDocumento14 pagineResearch Proposal o NishaNishaThakuri100% (1)
- Week 3 - MenstruationDocumento10 pagineWeek 3 - MenstruationTEDDY BEAR PRODUCTIONNessuna valutazione finora
- Department of Obstetrics & Gynecology-Wwrc Emergency Duty July 2020Documento3 pagineDepartment of Obstetrics & Gynecology-Wwrc Emergency Duty July 2020noorNessuna valutazione finora
- Evaluation of The Endometrium For Malignant or Premalignant DiseaseDocumento10 pagineEvaluation of The Endometrium For Malignant or Premalignant Diseasenautilus81Nessuna valutazione finora
- Obstetric Haemorrhage: EsmoeDocumento40 pagineObstetric Haemorrhage: EsmoePoonam RanaNessuna valutazione finora
- In-Vitro Fertilisation (Ivf) in Singapore: Charges and Success RatesDocumento4 pagineIn-Vitro Fertilisation (Ivf) in Singapore: Charges and Success RatesLászló ÉvaNessuna valutazione finora