Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Historical Introduction of Regional Anesthesia
Caricato da
Suresh KumarDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Historical Introduction of Regional Anesthesia
Caricato da
Suresh KumarCopyright:
Formati disponibili
Introduction of Regional Anesthesia Early Attempts at Local Anesthesia
The first written account of the coca plant being used as a local anesthetic was by the Spanish Jesuit Bernabe Cobo (1582-1657), who chewed the plant Page | 1 to relieve a toothache and wrote about it in 1653. Albert Niemann (1834-1861) of Gttingen, Germany, who isolated the alkaloid from the dried leaves in 1856 gave the name cocaine to the active drug. Interest in cocaine in Europe and America was directed initially toward the central effects of the drug when taken systemically. Vasili von Anrep (1852-1918) was the first to remark on its local anesthetic properties, and after animal experiments, he suggested its use as a local anesthetic during surgery. This suggestion went unnoticed, and the drug remained a curiosity. A comprehensive pharmacology textbook from 1883 does not mention cocaine or the plant E. coca.
Sigmund Freud (1856-1939), a young house officer at the prestigious Allgemeines Krankenhaus in Vienna, had a unique interest in cocaine and tested the drug as a substitute for opioids on a colleague who was addicted to morphine. Although this research met with little success, he had also noticed its ability to produce numbness of the tongue and provided a small sample to his junior colleague Carl Koller (1858-1944), an intern who was interested in producing local anesthesia for operations on the eye. Koller had anticipated a career as a scientist in Vienna. He had taken up this question for his research project because the anesthetic methods of the time were highly unsatisfactory for ophthalmic surgery. General anesthetics presented numerous difficulties for the surgeon, and refrigeration anesthesia, although marginally successful for surgery on the extremities, was clearly inappropriate for the eye. Koller observed that after topical application of cocaine he was able to pinch and prick the cornea of dogs without discomfort to the animals. Self-experimentation confirmed complete analgesia of the corneal surface, and he proceeded to use the agent for superficial surgery on the eye.
Koller arranged to demonstrate the use of topical cocaine analgesia at the Ophthalmologic Congress in Heidelberg, Germany, on September 15, 1884. As the time for this presentation approached, he was unable to afford the travel expenses from Vienna, and a colleague from Trieste, Josef Brettauer Page | 2 (1835-1905), presented the three-page manuscript in his absence. The presentation and demonstration were followed by an enthusiastically favorable response. Priority for the discovery was briefly confounded by a report on topical cocaine analgesia at an ophthalmologic meeting in October 1884 by Leopold Koenigstein, who did not mention Koller's previous paper, and by other comments that Sigmund Freud had actually originated the idea of cocaine analgesia. Koenigstein later conceded full credit for the discovery to Koller, and Freud eventually rejected all claims to the idea of topical analgesia with cocaine, although many concede that with his earlier publication on the subject, he was instrumental in reviving interest in a drug that before 1884 was of no interest to pharmacologists. Koller's career in Vienna seemed secure, but a disagreement arose with another house officer in January 1885. The altercation escalated into a duel with sabers, an activity that was banned in Austria at that time. Koller emerged unscathed from the duel, but the offending party suffered two saber cuts to the face. After this episode, Koller became depressed and ultimately decided to leave Austria. He first immigrated to Holland and then settled in New York City in 1886. T here he built a successful private practice while continuing to contribute occasional clinical articles to the ophthalmologic literature. He died in New York City in 1944 after modestly receiving several awards for his seminal role in the development of local and regional anesthesia.
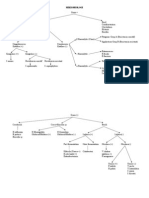
Regional Blocks
It was not obvious that cocaine would produce blockade of sensation if injected directly into peripheral nerves. In 1880, von Anrep had injected cocaine under the skin of his arm and discovered that it produced insensitivity, but this information did not attract Page | 3 attention. At least one Viennese surgeon, Anton Wlfler, first assistant to Theodore Billroth, had attempted hypodermic cocaine injections without producing analgesia and was convinced that it was effective only on the mucous membranes. The idea of injecting cocaine into nerve trunks is credited to William Halsted (1852-1922) and Alfred Hall, who began their injection experiments as early as 8 weeks after the Heidelberg announcement. Halsted and Hall had studied in Vienna during 1879 and 1880, but it is unlikely that they met Koller during those years because Koller did not finish his medical school training until 1882. During those years Koller was working on a paper about development of the mesoderm and had not developed his interest in cocaine. In 1884, Halsted was occasionally performing operations in the bedroom of his own house in New York City, and it was there that the two surgeons began their work on regional anesthesia. The first report of their success with injection appeared on December 6, 1884, in the New York Medical Journal in a letter written by Hall In this letter, Hall reported that they first injected 4% cocaine (15 mg) into the forearm and concluded that it blocked transmission in the cutaneous nerves because it provided analgesia below but not above the point of injection. They then injected 2 mL (80 mg) into the ulnar nerve at the elbow and produced a block of the entire ulnar distribution distal to the point of injection. Additional blocks were then performed on the brachial plexus and the infraorbital nerves, inferior dental nerves, and the sciatic nerve, all for operative surgery With these large doses, it is not surprising that constitutional symptoms developed. Hall described dizziness and nausea. Both Halsted and Hall became addicted to cocaine; Halsted lived with an occult cocaine or morphine addiction the
rest of his life. Hall took a position at Columbia University in New York City, but he later moved to Santa Barbara, California, where he died in 1924. Carl Schleich(1859-1922) introduced infiltration local anesthesia in 1892 as an alternative to direct injection of nerve trunks. His method was to infiltrate cocaine in dilute concentrations (0.01% to 0.2%) directly into subcutaneous tissues. James Leonard Corning(1855-1923), a neurologist from New York, observed that placing a tourniquet on the limb could prolong the analgesic effect of infiltration analgesia, and he reasoned that the tourniquet prevented the blood from removing cocaine from its active site. Heinrich F. Braun (1862-1934) achieved the same prolonged effect of cocaine by adding epinephrine to the solution and producing a chemical tourniquet. Braun became the pioneer of the new drug procaine, introduced in 1905 as a less toxic drug than cocaine. Braun's textbook, initially published in 1907, was one of the first devoted to regional anesthesia and went through eight editions, with the last one published in 1933. Although Halsted was the first to block the brachial plexus, he did not use a percutaneous technique. His method in 1884and that used by George Crile 13 years laterwas to surgically expose the roots and then inject each nerve directly. G. Hirschel produced the first percutaneous brachial plexus block in 1911 through an axillary approach The axillary brachial plexus block has been modified by several surgeons, including George Pitkin and R. H. de Jong, and remains a popular technique today. D. Kulenkampff introduced the supraclavicular brachial plexus block a few months after Hirschel described the axillary approach. Kulenkampff injected his own plexus with 10 mL of procaine at the midclavicular position, lateral to the subclavian artery, and achieved complete anesthesia of the arm.
Page | 4
Early reports indicated a frequent incidence of success with this block, but other practitioners soon reported complications such as pneumothorax and mediastinal emphysema. Several modifications of the supraclavicular block have emerged in an effort Page | 5 to avoid pneumothorax. Infraclavicular approaches to the brachial plexus were described by L. Bazy and V. Pauchet in 1917 and later popularized by P. Raj in 1973 In an attempt to approach the brachial plexus in the neck and thereby avoid pulmonary complications, M. Kappis in 1912 attempted to perform the block through a posterior paravertebral approach. Because of a high incidence of failures with the posterior approach, several investigators, including J. Etienne, V. Pauchet, and G. Pitkin, used various anterior approaches to the brachial plexus in the neck. In 1970, Alon P. Winnie introduced the interscalene brachial plexus block and emphasized that the scalene muscles are more accurate landmarks to the nerves than the subclavian artery or the midclavicular line is. The block has remained popular for operations on the shoulder and upper part of the arm; the nerves are located by paresthesias or direct nerve stimulation. Continuous infusion into the roots of the brachial plexus has been introduced and can provide long-lasting analgesia after operations on the arm and shoulder. A novel method of producing regional analgesia for operations on the extremities was described by August Bier (1861-1949) in 1908. Bier first exsanguinated the arm with an Esmarch wrap and, after placement of two tourniquets, injected a dilute solution of procaine intravenously. Analgesia was found to develop within minutes and persist until release of the tourniquet. The technique, known now as intravenous regional anesthesia, has been modified with new agents and remains a useful anesthetic technique for surgery on the extremities when a tourniquet is used. The development of regional anesthesia in the United States was accelerated with the arrival of Gaston Labat at the Mayo Clinic in 1924.
Labat had learned regional anesthetic methods from the French authority on injection techniques, Victor Pauchet (1869-1936), and expanded on his work while in Rochester, Minnesota. Labat founded the American Society of Regional Anesthesia and was active Page | 6 during its formative years. John Lundy adopted many of the regional techniques introduced by Labat at the Mayo Clinic and continued their use after Labat relocated to Bellevue Hospital in New York City. Labat's 1922 textbook was one of the first English texts on regional anesthesia and has been followed by several authoritative works on the subject. Labat's influence was also evident in New York City, where Emery A. Rovenstine (1895-1960), his successor as Chairman of the Department of Anesthesiology at Bellevue Hospital, established the first chronic pain clinic. The commitment of anesthesiologists to chronic pain therapy arose as a natural sequel to their emerging expertise in neuraxial and peripheral nerve blocks. Chronic pain clinics today are often modeled after the multidisciplinary clinic established by John J. Bonica (1917-1994) at the University of Washington in Seattle The continued success of regional anesthetic techniques can be partially credited to ultrasound techniques for localization of the nerves and also to improved local anesthetics with lower toxicity and longer duration of action. Cocaine was highly toxic, addictive, and of short duration. Procaine was synthesized in 1905 by Alfred Einhorn (1856-1917) and was the most commonly used agent until 1932, when tetracaine, a longer-acting agent, became available. Lidocaine, introduced in 1948 by Torsten Gordh(1907-), had several advantages, including lower toxicity and intermediate duration of action, and it is still widely used. Other local anesthetics include chloroprocaine (introduced in 1952), mepivacaine (1957), and bupivacaine (1963). Concern about therapyresistant cardiovascular toxicity with bupivacaine led to introduction of the newer agents ropivacaine (1996) and levobupivacaine. Bupivacaine, ropivacaine, and levobupivacaine are popular agents in low concentration for
control of postoperative pain and for obstetric anesthesia because of their long duration of action.
Neuraxial Block and Acute Pain Service
The first neuraxial block was performed 8 months after the demonstration in Heidelberg of the local anesthetic properties of cocaine James Leonard Corning (1855-1923) was a neurologist who had learned of the action of cocaine possibly from observation of Halsted's work in New York City. Corning was interested to know whether the blood could carry cocaine to the spinal cord, similar to what had been demonstrated to occur after the injection of strychnine between the spinous processes. On October 12, 1885, Corning injected a total of 120 mg of cocaine between the T11 and T12 spinous processes in a 45-year-old man and obtained loss of sensation of the legs and perineum. He concluded that this proved cocaine's action on the spinal cord and suggested its use in certain cases of spinal spasticity and for operations on the genitourinary system. The consensus is that Corning produced an epidural injection of the drug because 120 mg (60 mg initially and then 60 mg 8 minutes later) of intrathecal cocaine would be expected to produce a total spinal anesthetic or a block extending into the cervical dermatomes. It is not surprising that Corning's method of neuraxial blockade was not repeated because the technique of consistently injecting into the epidural space had not yet been described. If any investigators had attempted to repeat the Corning experiment with the dose that he used, it might have ended in disaster and thereby have delayed the development of neuraxial blockade by several years.
Spinal Analgesia
Page | 7
In Kiel, Germany, during the last decade of the 19th century, preparations were being made for the next major advance in anesthetic practice. At the Kiel University Medical School, Friederich von Esmarch (1823-1908) was the senior surgeon and August Bier one of the junior surgeons. Heinrich I. Quincke (1842-1922) was the leading internist in Kiel and had already contributed several useful clinical observations, among them the Quincke pulse and Quincke edema, to the medical literature.
In 1891, Quincke observed that the dural sac, described by Domenico Cotugno (1736-1822) in 1787, could be punctured by inserting a needle between the lumbar spinous processes. This procedure, independently reported by Walter Wynter (1860-1945) of Leeds, England, in the same year, at first was a curiosity without any real Page | 8 purpose. Quincke unsuccessfully attempted to treat hydrocephalus by draining fluid from the dural sac. Microscopic examination of the fluid did have some diagnostic value in cases of inflammation of the central nervous system. On August 15, 1898, August Bier and his assistant August Hildebrandt (18681854) used the Quincke method of entering the intrathecal space and injected between 5 and 15 mg of cocaine to produce spinal anesthesia in six cases for operations on the lower part of the body. They also reported the results of spinal anesthesia given to each other in what has become one of the classic clinical papers in medical literature. Bier thought that it would not replace general anesthesia because of the severity of side effects such as nausea, vomiting, dizziness, and headache. He proposed that these undesirable side effects were caused by escape of cerebrospinal fluid from the dural sac. The method whereby Bier arrived at the correct intrathecal dose of cocaine on the first attempt remains a mystery. After Bier's report, interest in spinal anesthesia spread rapidly. J. B. Seldowitsch successfully provided spinal anesthesia in St. Petersburg on May 11, 1899; Frederick Dudley Tait (1862-1918) and Guido Caglieri (18711951) in San Francisco on October 26, 1899; Theodore Tuffier in Paris on November 9, 1899; and Rudolph Matas (18601957) in New Orleans on November 10, 1899. By one report, more than 1000 manuscripts relating to spinal anesthesia had been published within 2 years of the original paper by Bier. Not all researchers agreed on the technique and indications for spinal anesthesia. Tait and Caglieri suggested the use of cervical intrathecal injections for operating on the upper extremities.
W. Morton reported success with total spinal anesthesia after lumbar puncture for operations on all parts of the body. Thomas Jonnesco reported no adverse effects from 398 spinal anesthetics administered between vertebrae at the thoracic and lumbar levels with a Page | 9 novocaine and strychnine mixture. Jonnesco called the method general spinal anesthesia. Remarkably, in his series there were 14 operations on the skull, 45 on the face, and 25 on the neck. In 1909, Bier claimed that to be successful with spinal anesthesia, the anesthetist should inject the solution only at body temperature and that tropacocaine was preferable to cocaine. The early reports of cocaine spinal anesthesia mentioned that after injection, patients frequently became restless and excitable, often exhibiting a significant rise in body temperature. One of the first physicians to specialize in anesthesia, S. Ormond Goldan, maintained accurate anesthesia records from several cases of spinal anesthesia with cocaine His records reveal a typical increase in heart rate, pupil size, and body temperature after cocaine spinal anesthesia. Matas reasoned that these effects were secondary to an action of cocaine on the central nervous system. He learned that mixing 1.5 mg of morphine with cocaine was useful in mitigating these symptoms. I n his 1900 report on spinal anesthesia, he regarded a mixture of cocaine and morphine as his standard agent. This report by Matas appears to be among the first attempts to use spinal opioids to enhance neuraxial analgesia. The Japanese anesthesiologist Otojiro Kitagawa (1864-1922) used intrathecal morphine (10 mg) in the same year to treat the chronic painful conditions of two patients. It is not surprising that serious complications from the spinal technique were soon observed. F. Gumprecht reported 15 cases of sudden death from lumbar puncture in 1900.
Several investigators observed respiratory arrest after high spinal injections. After the introduction of routine blood pressure measurements by Cushing in 1903, it was observed that severe hypotension could occur after spinal anesthesia. The scientific study of spinal anesthesia began within a few years after its introduction. Investigations were undertaken by Arthur E. Barker (1850-1916) to determine factors involved in spread of the local anesthetic within the subarachnoid space. Barker advised meticulous sterile technique and introduced the use of dextrose to produce hyperbaric solutions. His emphasis on gravity as an essential determinant of local anesthetic spread remains an important facet of the spinal technique today. Several researchers reported the dangers of total spinal anesthesia. Gaston Labat and George P. Pitkin contributed clinical observations that improved the safety of spinal anesthesia. A widely publicized malpractice trial in 1953 had a negative impact on the use of spinal anesthesia. Albert Woolley and Cecil Roe were healthy subjects who received dibucaine spinal anesthetics on the same day in 1947 at the Chesterfield Royal Hospital in England. Permanent painful spastic paraparesis developed in both patients. Although the cause of the paresis was inconclusive, it was thought that the injuries were caused by contamination of the spinal solution by phenol, in which the dibucaine ampules had been immersed for sterilization. The Wooley and Roe case was followed by other reports of paralysis after spinal anesthesia. However, in 1954, a reassuring study of 10,098 spinal anesthetics with only 71 minor neuropathies, most unrelated to the block itself, was published in a widely circulated medical journal. Spinal anesthesia then re-emerged as a safe anesthetic method, provided that attention was directed to meticulous technique.
Page | 10
Consideration has been given to a syndrome characterized by transient paresthesias after lidocaine spinal anesthesia. However, with the introduction of disposable spinal kits and improved techniques, the spinal route of drug administration is now firmly established. Research is continuing on new drugs and methods of delivery. Reports of cauda equina syndrome after the introduction of lidocaine through spinal microcatheters emphasize the importance of careful clinical observations when new methods of spinal delivery are introduced. Postdural puncture headache was an annoying problem for the first practitioners and their patients. The exact cause of this reaction was not agreed on for several years. As late as 1924, Labat had suggested removal of cerebrospinal fluid for the treatment of spinal headache. However, an extensive study by Leroy D. Vandam (1914-2004) and Robert Dripps (1911-1974) confirmed Bier's original suggestion that leakage of cerebrospinal fluid through the dural rent was the causative factor. The use of small-diameter spinal needles has decreased the incidence of spinal headache after spinal anesthesia. However, inadvertent dural puncture with larger needles can sometimes occur during the placement of epidural catheters. An innovative treatment of headache after dural puncture, the epidural blood patch, was suggested by James B. Gormley in 1960 and further described by Anthony J. DiGiovanni and Burdett S. Dunbar in 1970. The blood patch has been reported to be successful in a high percentage of cases and has withstood the test of time as an effective treatment of this condition.
Page | 11
Epidural Analgesia
Jean Enthuse Sicard (1872-1929) and Fernand Cathelin (1873-1945) independently introduced cocaine through the sacral hiatus in 1901, thereby becoming the first practitioners of caudal (epidural) anesthesia.
Sicard was a neurologist and used the technique to treat sciatica and tabes, but Cathelin used the technique for surgical anesthesia. Arthur Lwen(1876-1958), a pupil of Heinrich Braun (1862-1934) and an early proponent of regional anesthesia, successfully used caudal anesthesia Page | 12 with large volumes of procaine for pelvic surgery. It soon became apparent that caudal anesthesia was sufficient for operations on the perineum, but the drug would have to be deposited into the epidural space at higher levels if the surgeon anticipated operating on the abdomen or thorax. Initial attempts to provide epidural anesthesia through needles placed at higher levels were unsuccessful. B. Heile published an extensive study of the epidural space in 1913, but the focus of his final report was on the treatment of neurologic conditions with epidural injections. His unique approach was to enter the epidural space through the intervertebral foramina (a technique that has recently been revived). Tuffier was aware of the need for entry at higher levels but was unable to perfect a reliable technique for lumbar or thoracic epidural injections. In 1921, Fidel Pags(1886-1923), a Spanish military surgeon, devised a technique to introduce epidural procaine at all levels of the neuraxis. His method was to use a blunt needle and then feel and hear entry of the needle through the ligamentum flavum. His report of 43 cases of lumbar and thoracic epidural anesthesia represents a landmark article that went unnoticed because of its publication in an obscure medical journal. Pags died in an automobile accident soon after his report on epidural analgesia, and no students at the time had learned his technique. Pags had the idea of producing segmental anesthesia through epidural injections, thereby avoiding some of the side effects of complete neuraxial blockade, which occurred after high subarachnoid administration of local anesthetics. He provided the anesthetics himself and then performed the operations, noting that much time was saved with the epidural technique as compared
with general anesthesia. Of the 43 cases, it appears that one subject experienced total spinal anesthesia but survived after assisted ventilation. Achille Mario Dogliotti (1897-1966) described epidural injections of local anesthetics in 1931, apparently without previous knowledge of the work of Page | 13 Pags. Dogliotti performed extensive studies to determine the spread of solutions within the epidural and paravertebral space after injection. His work launched one of the most valuable techniques in the modern practice of anesthesiology. An important innovation was Dogliotti's method of identification of the epidural space. His 1939 textbook illustrates the use of continuous pressure on the plunger of a saline-filled syringe as the needle is advanced through the ligamentous structures. In contrast to the methods of Corning and Pags, the Dogliotti technique was reproducible and easily learned. Dogliotti also observed the extent and duration of analgesia after injection into various spinal interspaces. Initial acceptance of epidural analgesia was slow to develop in North America, although it gained early acceptance in Europe and South America. Gutierrez of Argentina became an enthusiastic advocate for the epidural method and collected valuable data on a large series of successful epidural anesthesia. He also developed the hanging drop sign, which is still used by some anesthesiologists to identify the epidural space. Dogliotti's anesthesia textbook was translated into English in 1939 and contained an extensive chapter on epidural analgesia. Textbooks by American authors several years later contained only a short description of the technique and considered it a novelty practiced only by those with special expertise. There were some early practitioners of epidural anesthesia in North America.
Charles B. Odom of New Orleans published 285 cases of lumbar epidural anesthesia in 1936 and introduced the concept of a test dose to detect intrathecal injection. In Odom's series there was one death attributed to the poor condition of the patient. John R. Harger and coworkers of Cook County Hospital in Chicago Page | 14 reported 1000 cases without a fatality when using single injections of 45 to 50 mL of 2% procaine. Oral Crawford and colleagues reported more than 600 cases of thoracic epidural analgesia for thoracic surgery in 1951, with two deaths. One major limitation of the neuraxial techniques was the short duration of action of procaine. Bier experimented with the addition of rubber and latex to the spinal anesthetic solution in an attempt to prolong the duration of blockade These ideas were not expanded on because of complications or lack of effect. To deal with the same problem, William T. Lemmon (1896-1974) used a 17gauge, malleable, silver needle that was connected through a hole in the operating room table to rubber tubing and a syringe. Injections could then be made at intervals to maintain the spinal block for several hours. Edward B. Tuohy(1908-1959) used a ureteral catheter threaded through a large Huber-tipped spinal needle to provide continuous spinal anesthesia. The Tuohy needle, a simple modification of the Huber needle, was used by him to thread the catheter into the subarachnoid space. Beginning in 1947, Manuel Martinez Curbelo of Havana, Cuba, used the Tuohy needle and a small ureteral catheter to provide continuous lumbar epidural analgesia. He reported 59 successful cases, and in one patient the catheter remained in place for 4 postoperative days with intermittent injections of local anesthetic. Caudal anesthesia experienced a resurgence in popularity after the report by W. B. Edwards and Robert A. Hingson (1918-1996) in 1942 that analgesia for labor and delivery could be achieved with caudal injections of tetracaine through a malleable needle left in situ within the sacral canal.
Their report was widely publicized, and within months the technique was adopted by several hospitals. Although caudal epidural injections had been used for obstetric analgesia for many years, it became apparent that the lumbar approach to the epidural space was more consistent, and it eventually replaced the caudal approach. Page | 15 Beginning in 1960, coincident with its rising popularity in obstetric anesthesia, the epidural method was taken up by several practitioners in North America. Philip R. Bromage and John J. Bonica performed several studies on epidural dose-response relationships and the hemodynamic changes that followed initiation of the block. Textbooks soon followed that introduced epidural analgesia into the operating room Although Dogliotti thought that general anesthesia was contraindicated after the initiation of epidural blockade, Massey Dawkins (1905-1975), Philip R. Bromage, and later Michael Cousins] discussed the advantages of providing general anesthesia during prolonged surgery while extending epidural analgesia throughout the surgical procedure and into the postoperative period. Although lumbar epidurals were widely used for postoperative pain relief, problems with ambulation and inadequate analgesia led to the current practice of placing epidural catheters between the appropriate interspaces to provide selective antinociception along the surgical incision site. A report in 1979 by J. Wang and associates demonstrated long-lasting analgesia from the intrathecal administration of morphine in eight patients with cancer pain. This clinical study had firm groundwork from previous basic studies on the spinal effects of opioids in animals. In 1976, Yaksh and Rudy reported that intrathecal morphine produced spinal analgesia in rats. Duggan and North demonstrated evidence of spinal analgesia after iontophoretic application of morphine into the dorsal horn region of the spinal cords of animals. Autoradiographic studies demonstrated a high density of opioid receptors in the substantia gelatinosa of the spinal cord.
The use of spinal opioids spread rapidly after the initial report by Wang and coworkers. Samii and colleagues confirmed that selective opioid spinal analgesia occurs in humans. Cousins and associates noticed that 1 to 2 mg of intrathecal morphine injected into the thoracic intrathecal region relieved the pain of breast or lung cancer for more than 24 hours. Behar and collaborators reported epidural opioid therapy in 1979. The explosive interest in neuraxial opioids that followed these reports was equal to the enthusiasm after the initial report of cocaine spinal anesthesia. The use of epidural catheters to provide long-lasting pain relief after surgery led to the formation of acute pain services. With special attention to drug concentrations and rates of infusion, patients were able to recuperate without pain and ambulate on the first postoperative day, even after extensive thoracic, abdominal, and orthopedic operations. The special advantage of epidural opioids was the synergistic effect that they exhibited with local anesthetics, which allowed a marked decrease in the dose of both drugs to achieve the same level of analgesia
Page | 16
MILLERS 7TH E
Potrebbero piacerti anche
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- Panic DisorderDocumento50 paginePanic Disorderheshm300020001790100% (3)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Labour Analgesia - Recent ConceptsDocumento18 pagineLabour Analgesia - Recent ConceptsSuresh KumarNessuna valutazione finora
- Anaesthetic Management of Ihd Patients For Non Cardiac SurgeryDocumento18 pagineAnaesthetic Management of Ihd Patients For Non Cardiac SurgerySuresh KumarNessuna valutazione finora
- Portal HypertensionDocumento25 paginePortal HypertensionJainab SiddiquiNessuna valutazione finora
- Alleviating Cancer PainDocumento9 pagineAlleviating Cancer PainSuresh KumarNessuna valutazione finora
- Cardiovascular Dynamics PhysiolabDocumento55 pagineCardiovascular Dynamics PhysiolabJaninepacia100% (1)
- Giovanni Maciocia Menorrhagia NotesDocumento22 pagineGiovanni Maciocia Menorrhagia Noteshihi12100% (5)
- Nursing Care Plan Ineffective Breathing Pattern Hepatic MassDocumento2 pagineNursing Care Plan Ineffective Breathing Pattern Hepatic MassRheegell Ellar-Fuertes100% (3)
- GO S For Tamilnadu DoctorsDocumento160 pagineGO S For Tamilnadu DoctorsSuresh KumarNessuna valutazione finora
- Cerebral Protection What Is New ?Documento11 pagineCerebral Protection What Is New ?Suresh Kumar100% (1)
- Spinal Anesthesia For Caeserian Section: Comparison of 5.0% Lignocaine and 0.5% BupivacaineDocumento4 pagineSpinal Anesthesia For Caeserian Section: Comparison of 5.0% Lignocaine and 0.5% BupivacaineSuresh KumarNessuna valutazione finora
- Local Anaesthetic AgentsDocumento21 pagineLocal Anaesthetic AgentsSuresh KumarNessuna valutazione finora
- Medico-Legal Issues in AnaesthesiaDocumento2 pagineMedico-Legal Issues in AnaesthesiaSuresh KumarNessuna valutazione finora
- Day Care AnesthesiaDocumento4 pagineDay Care AnesthesiaSuresh KumarNessuna valutazione finora
- Ventilator Associated Pneumonia (Vap)Documento11 pagineVentilator Associated Pneumonia (Vap)Suresh KumarNessuna valutazione finora
- Anaesthetic Management of Blunt Chest TraumaDocumento11 pagineAnaesthetic Management of Blunt Chest TraumaSuresh KumarNessuna valutazione finora
- Anaesthesia in The Gastrointestinal Endoscopy SuiteDocumento3 pagineAnaesthesia in The Gastrointestinal Endoscopy SuiteSuresh KumarNessuna valutazione finora
- Anaesthesia Care Beyond Operating Rooms: Newer Opportunities & Challenges.Documento8 pagineAnaesthesia Care Beyond Operating Rooms: Newer Opportunities & Challenges.Suresh Kumar100% (1)
- Controversial Issues in NeuroanaesthesiaDocumento12 pagineControversial Issues in NeuroanaesthesiaSuresh KumarNessuna valutazione finora
- Surgical Patients at Risk For Renal FailureDocumento35 pagineSurgical Patients at Risk For Renal FailureSuresh KumarNessuna valutazione finora
- Perioperative Management of A Patient With Left Ventricular FailureDocumento6 paginePerioperative Management of A Patient With Left Ventricular FailureSuresh KumarNessuna valutazione finora
- Muscle Relaxants in Current PracticeDocumento6 pagineMuscle Relaxants in Current PracticeSuresh KumarNessuna valutazione finora
- Pre-Operative Cardio-Pulmonary Exercise Testing (Cpet)Documento14 paginePre-Operative Cardio-Pulmonary Exercise Testing (Cpet)Suresh KumarNessuna valutazione finora
- Role of The Anaesthesiologists in The Management of BurnsDocumento12 pagineRole of The Anaesthesiologists in The Management of BurnsSuresh KumarNessuna valutazione finora
- Anesthesia For Fetal SurgeryDocumento8 pagineAnesthesia For Fetal SurgerySuresh KumarNessuna valutazione finora
- Anaesthetic Management of Bleeding Obstetric PatientDocumento10 pagineAnaesthetic Management of Bleeding Obstetric PatientSuresh KumarNessuna valutazione finora
- Anaesthesia For Bleeding TonsilDocumento6 pagineAnaesthesia For Bleeding TonsilSave MedicalEducation Save HealthCareNessuna valutazione finora
- Depth of Anesthesia & MonitoringDocumento2 pagineDepth of Anesthesia & MonitoringSuresh KumarNessuna valutazione finora
- Preoperative Anaesthetic Risk Assessment and Risk Reduction Before SurgeryDocumento17 paginePreoperative Anaesthetic Risk Assessment and Risk Reduction Before SurgerySuresh KumarNessuna valutazione finora
- Anaesthesia Breathing SystemsDocumento15 pagineAnaesthesia Breathing SystemsSuresh KumarNessuna valutazione finora
- Anaesthetic Management of Patients With Pacemakers and Implantable Cardioverter Defibrillator.Documento16 pagineAnaesthetic Management of Patients With Pacemakers and Implantable Cardioverter Defibrillator.Suresh KumarNessuna valutazione finora
- Fluid Resuscitation in TraumaDocumento17 pagineFluid Resuscitation in TraumaSuresh Kumar100% (1)
- Analysis of Arterial Blood GasesDocumento17 pagineAnalysis of Arterial Blood GasesSuresh KumarNessuna valutazione finora
- Basic Physics Applied To AnaesthesiologyDocumento10 pagineBasic Physics Applied To AnaesthesiologySuresh KumarNessuna valutazione finora
- Pulmonary Function Test in Pre Anaesthetic EvaluationDocumento10 paginePulmonary Function Test in Pre Anaesthetic EvaluationSuresh KumarNessuna valutazione finora
- Midterms Psyc LecDocumento14 pagineMidterms Psyc LecMiden AlbanoNessuna valutazione finora
- Rle Requirements Wardspcl Area NCP DSDocumento3 pagineRle Requirements Wardspcl Area NCP DSAzhly AntenorNessuna valutazione finora
- Mathis Et. Al. Intraoperative MV & PPCDocumento17 pagineMathis Et. Al. Intraoperative MV & PPCJun HungNessuna valutazione finora
- The Management of Patients With Acute Myocardial Infarction: Pocket GuidelinesDocumento22 pagineThe Management of Patients With Acute Myocardial Infarction: Pocket GuidelinesAhmad Yuliandri MustopaNessuna valutazione finora
- Applied Pharmacology For The Dental Hygienist 7th Edition Haveles Solutions ManualDocumento24 pagineApplied Pharmacology For The Dental Hygienist 7th Edition Haveles Solutions ManualJosephCraiggmax100% (50)
- Diagnosis of Typhoid FeverDocumento5 pagineDiagnosis of Typhoid FeverpeterjongNessuna valutazione finora
- EZCare Clinic Now Offers ADD or ADHD Treatment. Diagnostic Exam For New Patients and Prescription Refills Available Today.Documento3 pagineEZCare Clinic Now Offers ADD or ADHD Treatment. Diagnostic Exam For New Patients and Prescription Refills Available Today.PR.comNessuna valutazione finora
- Safety Seal Certification ChecklistDocumento2 pagineSafety Seal Certification ChecklistKathlynn Joy de GuiaNessuna valutazione finora
- Fluid Balance Case StudyDocumento9 pagineFluid Balance Case StudyAna BienneNessuna valutazione finora
- Literature ReviewDocumento8 pagineLiterature Reviewapi-550033018Nessuna valutazione finora
- Mikrobiologi DiagramDocumento2 pagineMikrobiologi Diagrampuguh89Nessuna valutazione finora
- Discuss Ethical and Cultural Consideration in DiagnosisDocumento2 pagineDiscuss Ethical and Cultural Consideration in DiagnosisJames Harlow0% (1)
- Chapter 43 - Thrombocytopenia and ThrombocytosisDocumento6 pagineChapter 43 - Thrombocytopenia and ThrombocytosisNathaniel SimNessuna valutazione finora
- Tonsillitis, Tonsillectomy and Adenoidectomy: - Literature ReadingDocumento52 pagineTonsillitis, Tonsillectomy and Adenoidectomy: - Literature ReadingdestiNessuna valutazione finora
- Student Notes Animals in ReserchDocumento14 pagineStudent Notes Animals in ReserchKayla ZunigaNessuna valutazione finora
- Cardiovascular Examination: Preparation of The PatientDocumento4 pagineCardiovascular Examination: Preparation of The PatientLolla SinwarNessuna valutazione finora
- HR Policy ManualDocumento34 pagineHR Policy Manualshamna AbdullaNessuna valutazione finora
- Basic Principles of Periodontal SurgeryDocumento100 pagineBasic Principles of Periodontal SurgerySandip Ladani100% (2)
- Pe Lesson 1 LifestyleDocumento17 paginePe Lesson 1 LifestyleKeil San PedroNessuna valutazione finora
- 701 1941 1 SMDocumento6 pagine701 1941 1 SMANNISA DAMAYANTINessuna valutazione finora
- dm2020 0202 PDFDocumento6 paginedm2020 0202 PDFcode4saleNessuna valutazione finora
- Epworth Sleepiness ScaleDocumento1 paginaEpworth Sleepiness ScaleSridhar ReddyNessuna valutazione finora
- Gender M F Marital Status: Rizal Medical CenterDocumento21 pagineGender M F Marital Status: Rizal Medical CentermaKitten08Nessuna valutazione finora
- PEMENANG PENAWARAN OBAT - PT. Novell Pharmaceutical LaboratoriesDocumento28 paginePEMENANG PENAWARAN OBAT - PT. Novell Pharmaceutical LaboratoriesRikoNessuna valutazione finora
- Megan Fobar - Case Study AbstractDocumento2 pagineMegan Fobar - Case Study Abstractapi-288109471Nessuna valutazione finora