Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
FISCT
Caricato da
Nicole ThomsonDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
FISCT
Caricato da
Nicole ThomsonCopyright:
Formati disponibili
Journal of Gerontology: MEDICAL SCIENCES 1995, Vol. 50A. No.
6, M291-M297
Copyright 1995 by The Gerontological Society of America
A Cross-sectional Validation Study of the FICSIT Common Data Base Static Balance Measures
Jane E. Rossiter-Fornoff,1 Steven L. Wolf,2 Leslie I. Wolfson,3 David M. Buchner,4 and the FICSIT Group5
'Division of Biostatistics, Washington University School of Medicine, St. Louis, department of Rehabilitation Medicine, Emory University School of Medicine, Atlanta. 'Department of Neurology, University of Connecticut Health Center, Farmington. "Departments of Health Services and Medicine, University of Washington, and Seattle VA Medical Center. 5 See Acknowledgments.
Downloaded from http://biomedgerontology.oxfordjournals.org/ at Robert Gordon University on January 16, 2012
Background. Two simple balance scales comprising three or four familiar tests of static balance were developed, and their validity and reliability are described. The scales were such that the relative difficulties of the basic tests were taken into consideration. Methods. Using FICSIT data, Fisher's method was used to construct scales combining ability to maintain balance in parallel, semi-tandem, tandem, and one-legged stances. Reliability was inferred from the stability of the measure over 3-4 months. Construct validity was assessed by cross-sectional correlations. Results. Test-retest reliability (over 3-4 months) was good (r = .66). Validity of the FICSIT-3 scale was suggested by its low correlation with age, its moderate to high correlations with physical function measures, and three balance assessment systems. The FICSIT-4 scale discriminated balance over a wide range of health status; the three-test scale had a substantial ceiling effect in community samples. Conclusion. A balance scale was developed that appears to have acceptable reliability, validity, and discriminant ability.
postural sway and limits staCONCENTRATIONforonbalance has characterized ofmuch bility as proxies research (1-4). These measures are not yet used routinely in the clinic because the force-plate interfaces for measuring balance are expensive and not easily portable; the measures, however, are precise and objective. Some investigators have used functional performance tests which incorporate measures of balance to provide a measure of a subject's general mobility [e.g., the mobility score of the Fall Risk Index (5), up-and-go tests (6,7), the Physical Performance test (8)]. They may be performed almost anywhere and use familiar daily movements in assessing subjects, but they are not specific for balance. Other performance tests assess balance alone. Gabell and Simons (9) developed a measure, designed for use in elderly populations, that gives an aggregate profile of a subject's ability to balance under static, sagittal, and rotational stresses. As yet, there is little documentation of its reliability and validity. The functional reach test (10) requires subjects to reach as far forward as possible from a stationary base of support. The test needs only a yardstick attached to a wall, and is therefore cheap and simple to use, if not completely portable. The Berg scale (11) considers performance on 14 tasks. It is reliable, correlates well with global ratings provided by physicians, requires no special equipment, and takes 15-20 minutes to perform. The purpose of this study was to develop a composite measure of static balance status based on ability to maintain balance over a diminishing base of support. The maneuvers
require no specialized equipment and take little time to perform. We describe the construction of a composite balance measure, estimate its test-retest reliability, and assess its construct validity.
METHODS
Sample FICSIT (Frailty and Injuries: Cooperative Studies of Intervention Techniques) (12) was a series of eight linked but independent trials carried out at Portland, New Haven (Yale), Seattle, Atlanta, Iowa, Farmington, San Antonio, and Boston. The studies were designed to investigate the effects of a number of diverse interventions on different aspects of frailty in varied elderly populations. The FICSIT sites had different entrance and exclusion criteria (13-20). Consequently, some research subjects (from Farmington, Atlanta, and Seattle) were fairly healthy individuals, while others were very frail nursing home residents (San Antonio and Boston). Seven sites carried out randomized clinical trials; the other (Iowa) recruited community resident and nursing home subjects, and was a non-randomized feasibility study. The studies were linked through the collection of a common data base containing information collected on each subject by the different sites at baseline and follow-up (baseline only at Iowa), using common definitions and approaches to the data collection. This communality means that the studies can be analysed using meta-analytic techM291
M292
ROSSITER-FORNOFF ET AL.
niques, while avoiding many of the problems, usually associated with analyses such as selection bias, insufficient details in published manuscripts, and the reporting of different measures. Procedures To measure balance status most economically, FICSIT used tests requiring subjects to maintain three different stance tests without assistive devices (21). The time for which each stance could be maintained (1-10 seconds) was measured with a stopwatch. The stances were generally done in the presumed order of difficulty: first the parallel stance (Classic Romberg, with feet touching), followed by the semi-tandem stance (the preferred foot forward), and finishing with the tandem stance (Sharpen Romberg). At Iowa, subjects were not asked to attempt further tests once they had failed a test. The Seattle and Atlanta sites began with the semi-tandem stance. If this stance was held for 10 seconds, the subject then was presumed able to do the parallel stance and went on to attempt the tandem stance. At Seattle, 76 subjects did the tandem stance on the balance platform. Subjects at Seattle were also required to have their arms crossed; at the remaining sites, subjects were not so restricted. Some people refused to attempt a test or were unable to maintain their balance for 1 second. Others were excluded from taking the test if an investigator thought an attempt would be inadvisable. Rather than using three tests to express an individual's balance status, a single measure of balance, suitable for use over the whole range of the FICSIT populations was sought. There are several possible approaches to combining the tests, the simplest being the count of successfully completed tests or the sum of the recorded times. The former statistic is too crude to be useful, while the latter might be overinterpreted, as apparently substantial differences in scores could arise from rather trivial differences in test performances. Since most of the useful information in these data lies in whether an attempt was successful (evidenced by the small proportion of subjects who held the parallel or semi-tandem stance for between 1 and 9 seconds), we preferred to consider the three stance times as trichotomous variables (failed, incomplete attempt [1-9 sec] and completed [10 sec]). Further, the data appeared to follow a Guttman-type scale; therefore we constructed scales using the point in the series of stances at which a subject first failed to complete a test, as a means of taking the varying difficulty of the tests into account. The simplest approach to the association of a numerical scale with the composite variable assigning of consecutive integers to each level is often not the most satisfactory. Assumptions about the category order may not be correct; further, the distance between categories may not be equal. A preferable approach is to use Fisher's method of scoring (22), described below, to determine an appropriate scaling. The aim is to find the scaling that best linearizes the relationship between the scale, and one or more reference variables that are highly correlated with balance status. By this method, levels of the scale which correspond to similar values of the reference variables are assigned scores close to each other. Alternatively, if one level of the scale tended to
correspond to the extreme (high) values of the reference variables, then that level would be assigned a high score with a large difference between that level and the one below it. The ordering of the categories of the scale depends only on the data, not on our assumptions. SAS Procedure Transreg (23) was used to estimate the scaling. Ideally, the interval between two test occasions used to estimate the reliability of a scale would be brief, a few days only. However, the first retest occasion in these studies was at the end of the intervention periods (intervals of between 3 and 12 months). Since the interventions might have impacted subjects' balance status, we base the estimate of the reliability on the control group alone. However, since the intervals are lengthy, their balance status may have declined somewhat between test and retest. Inter-class (Pearson) correlations are therefore more appropriate estimates of reliability than the intraclass correlations, which require the assumption of no systematic change in balance status between the two test occasions. No other direct balance measures were collected as part of the FICSIT common data base. However, some variables were available which should correlate to a greater or lesser extent with balance. These included age, gait speed, stride length, the Sickness Impact Profile (SIP), ambulation, mobility, and body care and movement (BCM) subscales. The availability of these measures at baseline means that the concurrent criterion-related validity of the balance scale could be assessed by considering the size of the correlations between them. Three FICSIT sites (Seattle, Atlanta and Farmington) collected more sophisticated balance measures as part of their site-specific protocols. These were also used to assess the validity of the composite common data base balance measure. At Seattle, average radius (mm) of the center-ofpressure pattern with respect to the centroid; average sway path length (mm/sec); and average sway area (mmVsec) were measured using a Kistler multi-component force platform. Each parameter was measured twice in each stance; mean values are used here. Since a loss of balance during the test meant that no score could be obtained, the inverse of the parameters was assigned worst case scores of 0. Atlanta measured the antero-posterior displacement; differences in heel-toe pressure; and the dispersion index using the Chattecx Balance System (Chattecx Corporation, Chattanooga, TN). Each parameter was measured with arms crossed and uncrossed, and with the platform stationary and moving forward and backward. Farmington used a PRO 1 Balance Master to measure area of sway and the average radius from the center of pressure. The former parameter was measured with the platform stationary and moving, either forward and backward or from side to side.
RESULTS
Downloaded from http://biomedgerontology.oxfordjournals.org/ at Robert Gordon University on January 16, 2012
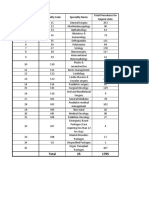
Distributions of the stance scores and other baseline characteristics of the eight study populations are shown in Table 1. The variation in the measures shows very clearly that Seattle, Atlanta, and Farmington recruited healthy subjects, whereas Iowa and the nursing home sites saw much frailer subjects. The nursing home populations had generally lower stance times than the community-dwelling populations. In
VALIDATION
OF FICSIT BALANCE
MEASURES
M293
Table 1. Baseline Characteristics of the FICSIT Populations Parallel Stance (p-s), Semi-Tandem Stance (st-s), Tandem Stance (t-s)
Community Resident Portland Number of subjects Age Gait speed Step length SIP* ambulation SIP mobility SIP BCM % Excellent health* % Poor health* Number with non-missing stance data parallel semi-tandem tandem Number (%) scoring 10 parallel semi-tandem tandem 1323 72.9 6.1 t 0.92 d 0 ? l t 0.55 d 0.12 10.7 d 13.6 t t 4.4 d 9.2 t 7.2 d 9.7 39.5 .5 1323 1321 1322 1285(97.1) 1239(93.8) 880 (66.6) Yale 301 78.4 5.3 0.46 + 0.16 0.33 + 0.08 22.7 14.3 12.3 15.6 Seattle 181 75.5 4.5 1.31 + 0.19 0.69 + 0.09 5.0 7.4 1.7 4.4 2.5 5.2 48.1 1.1 0 175 176 Atlanta 200 76.2 4.7 1.16 + 0.20 0.61 + 0.08 8.3 10.3 3.2 6.7 Iowa 150 79.0 10.4 0.45 + 0.27 0.30 + 0.13 30.4 18.5 26.8 21.9 31.1 20.3 Farmington 110 79.8 3.9 1.09 + 0.20 0.58 + 0.09 7.6 10.6 3.1 7.0 Nursing Home San Antonio 194 80.6 8.2 Boston 100 87.5 5.5
009 d: 0.13 0.46 0.22 0.10 d: 0.12 0.31 + 0 12 54.4 d 19.7 26.7 14.7 = 56.5 d 25.7 18.4 18.4 t 54.4 d 21.9 18.4 14.3 t 20.3 21.5 194 194 194 43 (22.2) 61(31.4) 10 (5.2) 25.4 7.0 72 73 71 50 (69.4) 46(63.0) 4 (5.6)
-t
18.3 9.0 296 299 297 277 (93.6) 245(81.9) 94(31.6)
t
55.5 1.0 0 200 200
t
46.6 0.0 110 110 108 109(99.1) 107 (97.2) 78 (72.2)
Downloaded from http://biomedgerontology.oxfordjournals.org/ at Robert Gordon University on January 16, 2012
t -t
119 97 89 80 (67.2) 53 (54.6) 28(31.5)
-t
172(98.3) 132 (75.0)
t
200(100.0) 162 (81.0)
FICSIT-3 Balance Scale (number in each category) p-s refused p-s failed p-s excluded Is < ps < 10s p-s = 10s + st-s refused + st-s failed + st-s excluded + Is < st-s < 10s p-s = 10s + st-s = 10s + t-s refused + t-s failed + t-s excluded + si < t-s < 10s 0 0 8 23 7 1 5 4 50 2 36 22 297 865 4 0 0 15 0 1 0 37 3 15 0 129 90 0 0 0 0 0 0 0 3 0 7 0 34 131 0 0 0 0 0 0 0 0 0 0 0 38 162 1 13 5 16 1 4 0 18 0 5 0 19 27 0 1 0 0 0 0 0 2 0 3 0 24 78 4 79 46 22 0 0 0 1 0 20 11 10 2 7 0 13 0 2 0 7 1 23 0
0.5 1.5
2.0
3.0
14 3
p-s = 10s, st-s = 10s, t-s = 10 4.0 =
Note: Scores assigned to the FICSIT-3 Balance Scale using Fisher's method of scoring. SIP = Sickness Impact Profile subscales. tData not collected. tSelf-reported status of general health.
this latter group, only the tandem stance test showed much sign of distinguishing between subjects. Self-selected gait speed was chosen as the reference variable because this measure was collected at all sites and was thought to be highly correlated with balance status. The time to first failure in the stance series would have 13 levels (listed in Table 1); however, certain combinations were rarely observed and therefore levels were collapsed together, leaving six, identified in Table 1 (the FICSIT-3 balance scale). Briefly, these are: 0 0.5 Subjects refused, failed or excluded from the parallel stance; Parallel stance held for less than 10 seconds;
1.5 2.0 3.0 4.0
Parallel stance held for 10 sec, semi-tandem stance for less than 10 sec; Parallel, semi-tandem stances held for 10 sec, refused, failed or excluded from tandem stance; Parallel, semi-tandem stances held for 10 sec, tandem stance for less than 10 sec; All three stances held for 10 sec.
The scores obtained using Fisher's method confirmed that subjects whose self-selected gait speed was slow failed earlier in the sequence of tests than others. For example, the relative scores indicate that subjects who did not complete the parallel stance are more similar to those who failed, refused, or were excluded from the test than to those who
M294
ROSSITER-FORNOFF ET AL.
completed it. The assigned scores indicate that the presumed ordering of test difficulty is correct, and that the variable spacing between levels provides more information about the relative balance status of different subjects than would assigning consecutive integers. Of the subjects who have data available for all three tests, few (3.7%) deviated from the Guttman ordering by completing a test after failing to complete an earlier one, or by partially completing a test having failed, refused, or been excluded from an earlier one. Table 1 clearly shows that while the balance scale may be useful in distinguishing among subjects at nursing home sites, and among more impaired community residents (New Haven and Iowa), there is a conspicuous ceiling effect at the sites recruiting from healthier populations (Seattle, Atlanta, and Farmington). Three sites Seattle, Atlanta and Farmington also collected one-legged stance times in a similar manner to the other stance times. A four-test version of the categorical balance scale could therefore be defined (the FICSIT-4 balance scale), using site-specific one-leg balance times in addition to the three common data base measures. Repeating the scoring using Fisher's method resulted in a seven-level test. These levels are: 0 0.5 1.5 2.0 3.0 4.0 5.0 Subjects refused, failed, or excluded from the parallel stance; Parallel stance held for less than 10 sec; Parallel stance held for 10 sec, semi-tandem stance for less than 10 sec; Parallel, semi-tandem stances held for 10 sec, refused, failed, or excluded from tandem stance; Parallel, semi-tandem stances held for 10 sec, tandem stance for less than 10 sec; Parallel, semi-tandem, and tandem held for 10 sec, one-legged stance held for less than 10 sec; All 4 stances held for 10 sec.
Reliability The within-site and overall estimates of reliability, with associated confidence intervals, are reported in Table 2. The observed correlations are only moderate to good, reflecting both the long intervals between test and retest and the statistical effect that an observed estimate of a correlation will be lower than the true correlation when the range of observed scores is restricted (24). The reliability estimates vary substantially between sites (between 0.25 and 0.74). The mean, weighted by sample size, is 0.45 (Table 2). When the sites with the longest test-retest times (Portland and Seattle) are excluded from this calculation, the estimate of the reliability is 0.66. Validity The concurrent criterion-related validity of the FICSIT-3 balance scale can be assessed by considering the size of the correlations between the scales and age, gait speed, stride length, the SIP ambulation, mobility, and BCM subscales at baseline (using both control and intervention subjects). These are shown in Table 3. There was good evidence of the content validity of the balance scale. First, Table 1 demonstrates that subjects resident in nursing homes were substantially worse at maintaining balance than those living in the community. Secondly, there were significant correlations between the balance scales and age, mean step length, and the SIP subscales (Table 3). At the community dwelling sites, age was modestly correlated with balance; there was less association at the nursing home sites. This is consistent with age-related disease, but not age per se, being a determinant of balance impairment. The measures of gait and the SIP subscales were moderately associated with the FICSIT-3 balance scale, with similar correlations being observed across all sites. The correlations between the same set of variables and the FICSIT-4 balance scale (at the three sites where onelegged stance times were collected) were also calculated. The correlations are mostly higher than those calculated with the FICSIT-3 scale. Finally, the correlations between the site-specific balance measures and the balance scales (Table 4) are also moderate. In general, the more challenging the conditions of the site-specific measures, the more highly
Downloaded from http://biomedgerontology.oxfordjournals.org/ at Robert Gordon University on January 16, 2012
The one-legged stance time was available on 296 subjects who had completed the first three stances. Of these, 149 (50.3%) did not complete the one-legged stance test, indicating that the ceiling effect is much less with the FICSIT-4 balance scale and that this scale might be useful in a wide range of elderly populations.
Table 2. Reliability Calculated Using Control Groups Only
Site Portland Yale Seattle Atlanta Farmington San Antonio Boston Pooledt Pooledt Time Between Test and Retest (Months) Number of Subjects Mean (SD) of Baseline Score 3.50(0.90) 2.81(1.09) 3.70 (0.56) 3.92 (0.27) 3.76 (0.44) 0.75(1.27) 1.53(0.92) Reliability* 95% CI .31-.45 .36-.64 -.16-.66 .37-.73 .33-.8S .64-.84 .44-.92 .44-.46 .62-.70
12 3-6 6 3.5 3.5 4 3
3-12
618 112 20 57 24 87 19 937 187
.38 .50 .25 .55 .59 .74 .68 .45 .66
3-4
Interclass (Pearson) correlations. tAverage of the site-specific reliability estimates, weighted using sample size.
VALIDATION OF FICSIT BALANCE MEASURES
M295
Table 3. Correlations (and Associated 95% Confidence Intervals) of the Common Data Base FICSIT-3 Scale With Validating Common Data Base Measures
Community Resident Portland Number of subjects 1320 Yale 294 Seattle 175 Atlanta 200 Iowa 112 Farmington 108 Nursing Home San Antonio 194 Boston 72 -0.25 (-0.25,-0.24) 0.38 (0.37,0.38) -0.35 (-0.35,-0.34) -0.32 (-0.32,-0.32) -0.37 (-0.37,-0.37) Pooled
Correlations with FICSIT-3 scale -0.24 -0.22 -0.44 -0.24 -0.19 0.17 Age -0.28 -0.18 (-0.29,-0.19) (-0.39,-0.17) (-0.38,-0.10) (-0.35,-0.09) (-0.37,-0.01) (-0.59,-0.29) (-0.31,-0.03) (-0.40,0.04) 0.58 Step length 0.41 0.18 0.26 0.31 0.43 0.36 0.63 (0.04,0.32) (0.46,0.70) (0.24,0.62) (0.31,0.51) (0.13,0.39) (0.14,0.48) (0.55,0.71) (0.31,0.41) -0.06 -0.27 -0.41 SIP* ambulation -0.29 -0.13 -0.17 -0.43 -0.36 (-0.47,-0.39) (_0.46,-0.26) (-0.21,0.09) (-0.40,-0.14) (-0.57,-0.25) (_0.47,-0.11) (-0.26,0.01) (-0.55,-0.13) -0.34 -0.11 -0.23 -0.34 -0.34 SIP mobility -0.18 -0.38 -0.29 (-0.43,-0.33) (-0.39,-0.19) (-0.26,0.05) (-0.36,-0.10) (-0.51,-0.17) (-0.51,-0.19) (-0.32,-0.04) (-0.55,-0.13) -0.10 -0.24 -0.41 -0.49 -0.28 S1PBCM (_O.45(_o.37) (-0.25,0.05) (-0.63,-0.35) (-0.41,-0.15) (-0.46,-0.02) SIP = Sickness Impact Profile.
Downloaded from http://biomedgerontology.oxfordjournals.org/ at Robert Gordon University on January 16, 2012
Table 4. Magnitudes of the Pearson Correlations Between Quantitative Measures of Static Balance and the FICSIT Balance Scales
FICSIT-3 Scale Quantitative Measure Seattle I/path length I/average radius from COP 1/area of sway Atlanta Square root AP displacement Absolute difference in heel/toe pressure Dispersion index Square root AP displacement Absolute difference in heel/toe pressure Dispersion index Farmington Log area of sway Log average radius from COP Log area of sway Log area of sway *AP: Antero-posterior. tML: Medio-lateral. Condition tandem stanceleft foot forward n 174 174 174 105 110 110 105 110 110 108 79 40 35 Correlation 0.30 0.34 0.29 0.25 0.29 0.14 0.36 0.31 0.16 0.39 0.12 0.36 0.25 95% CI (0.33,0.57) (0.38,0.60) (0.29,0.53) (0.10,0.46) (0.21,0.53) (-0.01,0.35) (0.57,0.25) (0.21,0.53) (0.00,0.36) (0.22,0.54) (-0.09,0.34) (0.11,0.65) (0.11,0.67) n 96 96 96 105 110 110 105 110 110 90 79 37 34 FICSIT-4 Scale Correlation 0.46 0.52 0.45 0.35 0.35 0.19 0.39 0.31 0.18 0.46 0.10 0.45 0.25 95% CI
arms crossed
platform moving
platform stationary AP motion* ML motion!
correlated the measures are with the balance scale (in these relatively fit subjects). Again, bigger correlations are usually observed with the FICSIT-4 scale than with the FICSIT-3 scale (Table 4).
DISCUSSION
The FICSIT-3 scale is a measure of static balance, or the ability to maintain posture over a restricted base of support. For useful measurement, the most important requirements of any test are reliability (consistency of results) and validity, the extent to which an instrument measures what it is intended to measure. Briefly, the balance scale had good stability when retested after a period of several months. It showed good construct validity both with FICSIT common data base data and balance platform parameters.
It was not possible to use FICSIT data to measure reliability of the balance scale directly. Rather, we have inferred good reliability from the estimates of reliability calculated with long intervals between test and retest. Using control subjects, reliability of the measure was estimated as 0.66 over a test-retest interval of 3 to 4 months. While moderate, this correlation provides good evidence that the FICSIT-3 balance scale is reliable in a general population, since it has been reduced by the range restriction at the sites, and the long test-retest interval. Unsurprisingly, subjects residing in long-term care facilities have poorer balance than those who reside in the community. Similarly, sites which aimed to recruit frail subjects demonstrated worse balance scores than sites with a healthier sample. Thus, over the 8 sites there was a fairly
M296
ROSSITER-FORNOFF ET AL.
wide distribution of scores. With the FICSIT-3 scale, subjects resident in long-term care facilities are evenly distributed throughout the range of scores, while communityresiding subjects are clustered at the high end of the range, suggesting a ceiling on their scores. To obviate this effect, a fourth item, one-legged standing time, can be added to the measure, resulting in less clustering at the highest score in these community enrollment sites. Improvement in discrimination at the lower end of the scale might be obtained by the addition of a comfortable stance. Age, measures of gait, and the SIP subscales were variably, but generally highly significantly correlated with the balance scales, suggesting validity for these measures. Since each site's study population was restricted in some way (by recruiting among nursing home residents, or by excluding people unable to cope with demanding interventions) the observed correlations are based on a reduced range of scores. Consequently, we observe smaller correlations than would be seen in the general population. Thus, the moderate correlations observed here, over a number of narrow ranges of scores, provide strong evidence of validity. The balance scales were also compared with high-tech, site-specific measures of static balance. There was a robust correlation between the FICSIT-3 scale and the measures of static balance; for the most challenging site-specific measures the correlation was larger still when using the FICSIT-4 scale. We cannot refute the value of measurement tools described by other investigators (5-11) to measure static balance. Nevertheless, these approaches often have significant time or equipment requirements. In contrast, the FICSIT balance scales require only a watch, are simple and quick to perform, and have a wide range of scores allowing use in both frail and robust older persons. While these studies were not intended to assess reliability and validity, they provide evidence that the FICSIT-3 scale is a reliable and valid quantitative measure of static balance. Where the population is healthy, the addition of the one-legged stance to the FICSIT battery of stance tests provides useful further discrimination. The FICSIT balance scales are potentially useful assessment tools.
ACKNOWLEDGMENTS
Emory University School of Medicine (UOJ AG09J24), Department of Rehabilitation Medicine: Steven L. Wolf, PhD, FAPTA, Nancy G. Kutner, PhD, Robert C. Green, MD, Elizabeth McNeely, PhD, Carol Coogler, PT, DSc. Hebrew Rehabilitation Centerfor Aged, Harvard Medical School, USDA Human Nutrition Research Center on Aging (UOJ AG09078): Maria A. Fiatarone, MD, Evelyn F. O'Neill, CTRS, Nancy Doyle Ryan, Diet T, Karen M. Clements, MPH, Lewis A. Lipsitz, MD, Joseph J. Kehayias, PhD, Susan B. Roberts, PhD, William J. Evans, PhD. University of Iowa, Iowa State University (UOJ AG09J23): Robert Wallace, MD, Jo Ellen Ross, MA, Jeffrey C. Huston, PhD, Carolyn J. Kundel, PhD, Michael S. Sellberg, BS. Department of Neurology, University of Connecticut Health Center (U01 AG09096): Leslie I. Wolfson, MD, Robert H. Whipple, MA, Paula M. Amerman, RN, MSN, James O. Judge, MD, Carol A. Derby, PhD, Mary B. King, MD. NIAINCNR: Evan C. Hadley, MD, AshleshaTamboli, MD, PhD, Marcia G. Ory, PhD, MPH, Sharlene Weiss, PhD, RN. Centers for Disease Control and Prevention: Richard W. Sattin, MD.
REFERENCES
Downloaded from http://biomedgerontology.oxfordjournals.org/ at Robert Gordon University on January 16, 2012
Address correspondence to Dr. Jane Rossiter-Fornoff, Division of Family Health, Illinois Department of Public Health, 535 West Jefferson, Springfield, IL 62761. The FICSIT Group consists of: Division of Biostatistics, Washington University School of Medicine (UOJAG09098):). Philip Miller, AB, Michael A. Province, PhD, Kenneth B. Schechtman, PhD, Cynthia L. Arfken, PhD, Jane E. Rossiter-Fornoff, DPhil. Centerfor Health Research, Kaiser Permanente, Northwest Region (UOJ AG09089): Mark C. Hornbrook, PhD, Victor J. Stevens, PhD, Darlene J. Wingfield, MPA, PT, Mervyn R. Greenlick, PhD. Program on Aging, Yale University School of Medicine (U01AG09087): Mary E. Tinetti, MD, Dorothy I. Baker, PhD, RNC, Elizabeth B. Claus, PhD, Ralph I. Horwitz, MD. Department of Health Sciences, University of Washington (U01 AG09095): David M. Buchner, MD, MPH, Edward H. Wagner, MD, MPH, Barbara J. de Lateur, MD, M. Elaine Cress, PhD, Robert Wee, MMSE, Itamar B. Abrass, MD, Peter Esselman, MD, Tony Marguerita, MD. Geriatric Research, Education, and Clinical Center, Audie L. Murphy Veterans Hospital (U01 AG09117): Cynthia D. Murlow, MD, Meghan B. Gerety, MD, John E. Cornell, PhD, Louis A. DeNino, PhD, Deanna Kanten, RN.
1. Lichtenstein MJ, Burger MC, Shields SL, Shiavi RG. Comparison of biomechanics platform measures of balance and videotaped measures of gait with a clinical mobility scale in elderly women. J Gerontol Med Sci 1990;45:M49-54. 2. Lord SR, Clark RD, Webster IW. Postural stability and associated physiological factors in a population of aged persons. J Gerontol Med Sci 1991;46:M69-76. 3. Maki BE, Holliday PJ, Topper AK. Fear of falling and postural performance in the elderly. J Gerontol Med Sci 1991 ;46:M12331. 4. Murray MP, Seireg AA, Sepic SB. Normal postural stability and steadiness: quantitative assessment. J Bone Joint Surg 1975;57-A: 510-6. 5. Tinetti ME. Performance-oriented assessment of mobility problems in elderly patients. J Am Geriatr Soc 1986;34:119-26. 6. Mathias S, Nayak USL, Isaacs B. Balance in elderly patients: the getup and go test. Arch Phys Med Rehab 1986;67:387-9. 7. Podsiadlo D, Richardson S. The timed "Up & Go": a test of basic mobility for frail elderly persons. J Am Geriatr Soc 1991 ;39:142-8. 8. Reuben DB, Siu AL. An objective measure of physical function of elderly outpatients: the physical performance test. J Am Geriatr Soc 1990;38:l 105-12. 9. Gabell A, Simons MA. Balance coding. Physiotherapy 1983;68:286-8. 10. Duncan PW, Weiner DK, Chandler J, Studenski S. Functional reach: a new clinical measure of balance. J Gerontol Med Sci 1990;45:M192-7. 11. Berg K, Wood-Dauphinee S, Williams JI, Gayton D. Measuring balance in the elderly: preliminary development of an instrument. Physiotherapy Canada 1989;41:304-l 1. 12. Ory MG, Schechtman KB, Miller JP, et al. Frailty and injuries in later life: the FICSIT trials. J Am Geriatr Soc 1993;41:283-96. 13. Hornbrook MC, Stevens VJ, Wingfield DJ. Seniors' program for injury control and education. J Am Geriatr Soc 1993;41:30914. 14. Tinetti ME, Baker DI, Garrett PA, Gottschalk M, Koch ML, Horwitz RI. Yale FICSIT: risk factor abatement strategy for fall prevention. J Am Geriatr Soc 1993;41:315-20. 15. Buchner DM, Cress ME, Wagner EH, de Lateur BJ, Price R, Abrass IB. The Seattle FICSIT/MOVEIT study: the effect of exercise on gait and balance in older adults. J Am Geriatr Soc 1993;41:321-5. 16. Mulrow CD, Gerety MB, Kanten D, DeNino LA, Cornell JE. Effects of physical therapy on functional status of nursing home residents. J Am Geriatr Soc 1993;41:326-8. 17. Wolf SL, Kutmer NG, Green RC, McNeely E. The Atlanta FICSIT study: two exercise interventions to reduce frailty in elders. J Am Geriatr Soc 1993 ;41:329-32. 18. Fiatarone MA, O'Neill EF, Doyle N, et al. The Boston FICSIT study: the effects of resistance training and nutritional supplementation on physical frailty in the oldest old. J Am Geriatr Soc 1993;41:333-7. 19. Wallace RB, Ross JE, Houston JC, Kundel C, Woodworth G. Iowa FICSIT trial: the feasibility of elderly wearing a hip joint protective garment to reduce hip fractures. J Am Geriatr Soc 1993;41:338-40. 20. Wolfson LI, Whipple R, Judge J, Amerman P, Derby C, King M. Training balance and strength in the elderly to improve function. J /Km Geriatr Soc 1993,41:340-3.
VALIDATION OF FICSIT BALANCE MEASURES
M297
21. Buchner DM, Hornbrook MC, Kutner NG, et al. Development of the common data base for the FICSIT trials. J Am Geriatr Soc 1993;41:297-308. 22. Fisher R. Statistical methods for research workers (11th edition), Edinburgh: Oliver and Boyd Press; 1938:289-95. 23. SAS Institute Inc. SAS/STAT user's guide, version 6, fourth ed., vol. 2. Cary, NC: SAS Institute Inc; 1989:1511-611.
24. HunterJE, Schmidt FL. Methods of meta-analysis: correcting error and bias in research findings. Newbury Park, CA: Sage Publications, 1990:125-32. Received September 21, 1994 Accepted April 28, 1995
Downloaded from http://biomedgerontology.oxfordjournals.org/ at Robert Gordon University on January 16, 2012
NOTICE TO AUTHORS
Beginning January 1, 1996
Manuscripts for the Journal of Gerontology: Medical Sciences Should Be Sent to
William B. Ershler, MD Institute on Aging, University of Wisconsin GRECC, Madison VA Medical Center 2500 Overlook Terrace (11G) Madison, WI53705
Potrebbero piacerti anche
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- ENT Summery TABLEDocumento19 pagineENT Summery TABLEtaliya. shvetzNessuna valutazione finora
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5795)
- Case Study: MYXEDEMATOUS COMADocumento5 pagineCase Study: MYXEDEMATOUS COMAjisooNessuna valutazione finora
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- A Mini Project Report On "Issues Challenge and Application of Emerging Technologies in The Pharmaceutical Industry"Documento42 pagineA Mini Project Report On "Issues Challenge and Application of Emerging Technologies in The Pharmaceutical Industry"Raja Medical StoreNessuna valutazione finora
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Quality Management in The Imaging Sciences 5th Edition Papp Test BankDocumento35 pagineQuality Management in The Imaging Sciences 5th Edition Papp Test Bankmisdateholinessaubzt6100% (22)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Airway Problems in PACUDocumento35 pagineAirway Problems in PACUIndrani HemantkumarNessuna valutazione finora
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- Faculty 363 Histotechnique Lectures - 2Documento27 pagineFaculty 363 Histotechnique Lectures - 2einsteinspy100% (1)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- MYDRIATICDocumento6 pagineMYDRIATICManik BashaNessuna valutazione finora
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Stratification in The Cox Model: Patrick BrehenyDocumento20 pagineStratification in The Cox Model: Patrick BrehenyRaiJúniorNessuna valutazione finora
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Orthotic/Prosthetic Referral Form: Dispensing RX: Please Evaluate and Treat Patient With The Following DeviceDocumento1 paginaOrthotic/Prosthetic Referral Form: Dispensing RX: Please Evaluate and Treat Patient With The Following DeviceKelly Roberts WiggenNessuna valutazione finora
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- FirstAid SlidesDocumento62 pagineFirstAid Slidessamihamaideh100% (1)
- Junkyard Dog (16) : B A R S W L I C ESS I/D AC CM MoveDocumento2 pagineJunkyard Dog (16) : B A R S W L I C ESS I/D AC CM MoveLeonnardo CruzNessuna valutazione finora
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- ANATOM 64 Clarity SpecificationsDocumento6 pagineANATOM 64 Clarity SpecificationsVixiMerahNessuna valutazione finora
- The Secrets To Gaining Muscle Mass Fast by Anthony Ellis PDFDocumento125 pagineThe Secrets To Gaining Muscle Mass Fast by Anthony Ellis PDFVishal DokaniaNessuna valutazione finora
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- All PackageRates (ABPMJAY) PDFDocumento300 pagineAll PackageRates (ABPMJAY) PDFSumit Soni0% (1)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The PRISMAFLEX System: Making Possible PersonalDocumento12 pagineThe PRISMAFLEX System: Making Possible PersonalluisfulaNessuna valutazione finora
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- RNI For Malaysians-SummaryDocumento2 pagineRNI For Malaysians-SummaryAimi Hannani100% (1)
- ZtPyrBpzMK Naskah Publikasi PDFDocumento17 pagineZtPyrBpzMK Naskah Publikasi PDFFathiya FarhaniNessuna valutazione finora
- Ethics and The Pharmaceutical Industry PDFDocumento2 pagineEthics and The Pharmaceutical Industry PDFDonaldNessuna valutazione finora
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Malaria Treatment 2013Documento75 pagineMalaria Treatment 2013Rheinny IndrieNessuna valutazione finora
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Accidental AddictsDocumento6 pagineThe Accidental AddictsnorthandsouthnzNessuna valutazione finora
- Ancondroplasia DwarfismDocumento10 pagineAncondroplasia DwarfismjordandeanNessuna valutazione finora
- Biomagnetic Bracelet Biolife IndiaDocumento61 pagineBiomagnetic Bracelet Biolife Indiasagarkumar11Nessuna valutazione finora
- Medical Needs Fatiguing The Descrpit Social CcienceDocumento11 pagineMedical Needs Fatiguing The Descrpit Social Ccienceicicle900Nessuna valutazione finora
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Pneumonia FinalDocumento2 paginePneumonia FinalMMW MNessuna valutazione finora
- Public Notice20oct2014124416 PDFDocumento73 paginePublic Notice20oct2014124416 PDFLeticia RileyNessuna valutazione finora
- Red Eye: Education Session SevenDocumento20 pagineRed Eye: Education Session SevenHendry SetiawanNessuna valutazione finora
- Anatomy & Physiology Unit 1Documento29 pagineAnatomy & Physiology Unit 1Priyanjali SainiNessuna valutazione finora
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Regulatory Compliance Pharmacy Manager in Tampa FL Resume John HawesDocumento2 pagineRegulatory Compliance Pharmacy Manager in Tampa FL Resume John HawesJohnHawesNessuna valutazione finora
- PranoyDocumento24 paginePranoySupriyo ChatterjeeNessuna valutazione finora
- Emr Policy and ProcedureDocumento7 pagineEmr Policy and Procedureapi-267965870Nessuna valutazione finora
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)