Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Erythromycin - 10
Caricato da
irahclarissa18Descrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Erythromycin - 10
Caricato da
irahclarissa18Copyright:
Formati disponibili
ERYTHROMYCIN BASE Pharmacologic Category Antibiotic, Macrolide
Pertussis: Oral: 500 mg (base) every 6 hours for 14 days Preop bowel preparation: Oral: 1 g erythromycin base at 1, 2, and 11 PM on the day before surgery combined with mechanical cleansing of the large intestine and oral neomycin Dosing: Geriatric
Dosing: Adult Refer to adult dosing. Note: Due to differences in absorption, 400 mg erythromycin ethylsuccinate produces the same serum levels as 250 mg erythromycin base or stearate. Usual dosage range: Oral: Usual dosage range: Infants and Children: Base: 250-500 mg every 6-12 hours Oral: Indication-specific dosing: Bartonella sp infections (bacillary angiomatosis [BA], peliosis hepatis [PH]) (unlabeled use): Oral: 500 mg (base) 4 times/day for 3 months (BA) or 4 months (PH) Chancroid (unlabeled use): Oral: 500 mg (base) 3 times/day for 7 days; Note: Not a preferred agent; isolates with intermediate resistance have been documented (CDC, 2010) Gastrointestinal prokinetic (unlabeled use): I.V.: 200 mg initially followed by 250 mg (base) orally 3 times/day 30 minutes before meals. Lower dosages have been used in some trials. Granuloma inguinale (donovanosis) (unlabeled use): Oral: 500 mg (base) 4 times/day for 21 days (CDC, 2010) Legionnaires disease: Oral: 1.6-4 g (ethylsuccinate)/day or 1-4 g (base)/day in divided doses for 21 days. Note: No longer preferred therapy and only used in nonhospitalized patients. Lymphogranuloma venereum: Oral: 500 mg (base) 4 times/day for 21 days; Note: Preferred therapy for pregnant or lactating women (CDC, 2010) Nongonococcal urethritis (including coinfection with C. trachomatis): Oral: 500 mg (base) 4 times/day for 7 days or 800 mg (ethylsuccinate) 4 times/day for 7 days. Note: May use 250 mg (base) or 400 mg (ethylsuccinate) 4 times/day for 14 days if gastrointestinal intolerance. Base: 30-50 mg/kg/day in 2-4 divided doses; maximum: 2 g/day Ethylsuccinate: 30-50 mg/kg/day in 2-4 divided doses; maximum: 3.2 g/day Stearate: 30-50 mg/kg/day in 2-4 divided doses; maximum: 2 g/day Dosing: Pediatric Note: Due to differences in absorption, 400 mg erythromycin ethylsuccinate produces the same serum levels as 250 mg erythromycin base or stearate.
Indication-specific dosing: Infants and Children: Bartonella sp infections (bacillary angiomatosis [BA], peliosis hepatis [PH]) (unlabeled use): Oral: 40 mg/kg/day (ethylsuccinate) in 4 divided doses (maximum: 2 g/day) for 3 months (BA) or 4 months (PH) Chlamydial infection (C. trachomatis): Children <45 kg: Oral: 50 mg/kg/day (base or ethylsuccinate) in 4 divided doses for 14 days (CDC, 2010) Community-acquired pneumonia (CAP) (IDSA/PIDS, 2011): Infants >3 months and Children: Note: A beta-lactam antibiotic should be added if typical bacterial pneumonia cannot be ruled out. Presumed atypical (M. pneumoniae, C. pneumoniae, C. trachomatis) infection, mild atypical infection or step-down therapy (alternative to azithromycin): Oral: 10 mg/kg/dose every 6 hours
Moderate-to-severe atypical infection (alternative to azithromycin): I.V.: 5 mg/kg/dose every 6 hours Mild/moderate infection: Oral: 30-50 mg/kg/day in divided doses every 6-12 hours Pertussis: Oral: 40-50 mg/kg/day in 4 divided doses for 14 days; maximum 2 g/day (not preferred agent for infants <1 month due to IHPS) Pharyngitis, tonsillitis (streptococcal): Oral: 20 mg (base)/kg/day or 40 mg (ethylsuccinate)/kg/day in 2 divided doses for 10 days. Note: No longer preferred therapy due to increased organism resistance. Preop bowel preparation: Oral: 20 mg (base)/kg at 1, 2, and 11 PM on the day before surgery combined with mechanical cleansing of the large intestine and oral neomycin Severe infection: I.V.: 15-50 mg/kg/day; maximum: 4 g/day Dosing: Renal Impairment Slightly dialyzable (5% to 20%); supplemental dose is not necessary in hemo- or peritoneal dialysis or in continuous arteriovenous or venovenous hemofiltration. Use: Labeled Indications Treatment of susceptible bacterial infections including S. pyogenes, some S. pneumoniae, some S. aureus,M. pneumoniae, Legionella pneumophila, diphtheria, pertussis, Chlamydia, erythrasma, N. gonorrhoeae, E. histolytica, syphilis and nongonococcal urethritis, and Campylobacter gastroenteritis; used in conjunction with neomycin for decontaminating the bowel Use: Unlabeled/Investigational Treatment of gastroparesis, chancroid; preoperative gut sterilization Drug of Choice or Alternative for Disease/Syndrome(s) Acne Vulgaris Bronchitis Cervicitis Impetigo Pharyngitis Urethritis, Nongonococcal
Drug of Choice or Alternative for Organism(s) Bartonella Species Bordetella pertussis Calymmatobacterium granulomatis Campylobacter jejuni Chlamydophila pneumoniae Chlamydophila psittaci Corynebacterium diphtheriae Corynebacterium Species, Other Than C. jeikeium Haemophilus ducreyi Legionella pneumophila Mycoplasma pneumoniae Rhodococcus Species Streptococcus agalactiae Streptococcus pyogenes Ureaplasma urealyticum
y y y y y y y y y y y y y y y
Administration: Oral Do not crush enteric coated drug product. GI upset, including diarrhea, is common. May be administered with food to decrease GI upset. Do not give with milk or acidic beverages. Dietary Considerations Drug may cause GI upset; may take with food. Some products may contain sodium. Storage Oral suspension: Granules: After mixing, store under refrigeration and use within 10 days. Powder: Erythromycin ethylsuccinate may be stored at room temperature if used within 14 days. Refrigerate to preserve taste. Medication Safety Issues
y y y y y y
Sound-alike/look-alike issues: Erythromycin may be confused with azithromycin, clarithromycin Eryc may be confused with Emcyt, Ery-Tab Contraindications Hypersensitivity to erythromycin, any macrolide antibiotics, or any component of the formulation Concomitant use with pimozide, cisapride, ergotamine or dihydroergotamine, terfenadine, astemizole
Infants: Use of erythromycin has been associated with infantile hypertrophic pyloric stenosis (IHPS); observe for non-bilious vomiting or irritability with feeding. Elderly: May be at increased risk of adverse events, including hearing loss and/or torsade de pointes when dosage 4 g/day, particularly if concurrent renal/hepatic impairment. Geriatric Considerations Dose does not need to be adjusted unless there is severe renal or hepatic impairment. Elderly may be at an increased risk for torsade de pointes, ototoxicity (particularly when dose is 4 g/day in conjunction with renal or hepatic impairment). Pregnancy Risk Factor
Warnings/Precautions B Concerns related to adverse effects: Pregnancy Considerations Altered cardiac conduction: Macrolides have been associated with rare QTc prolongation and ventricular arrhythmias, including torsade de pointes; use with caution in patients at risk of prolonged cardiac repolarization. Superinfection: Prolonged use may result in fungal or bacterial superinfection, including C. difficileassociated diarrhea (CDAD) and pseudomembranous colitis; CDAD has been observed >2 months postantibiotic treatment. Disease-related concerns: Hepatic impairment: Use with caution in patients with pre-existing liver disease; hepatic impairment, including hepatocellular and/or cholestatic hepatitis, with or without jaundice, has been observed. Discontinue if symptoms of malaise, nausea, vomiting, abdominal colic, and fever. Myasthenia gravis: Erythromycin has been associated with aggravation of weakness associated with myasthenia gravis. Concurrent drug therapy issues: Major inhibitor of CYP3A4: Use caution with any agents with substantial metabolism through the CYP3A4 pathway; high potential for drug interactions exists. Special populations: Adverse events were not observed in animal studies; therefore, erythromycin is classified as pregnancy category B. Erythromycin crosses the placenta and low concentrations are found in the fetal serum. No increased risk for congenital abnormalities has been documented, with the exception of a possible slight increase in risk for cardiovascular anomalies. Most studies do not support a link between prenatal exposure to erythromycin and pyloric stenosis in the neonate. In general, serum concentrations of erythromycin are lower in pregnant women. Erythromycin therapy in patients with preterm, premature rupture of membranes is associated with a range of health benefits to the neonate and long-term adverse events to the child have not been observed. However, maternal use of erythromycin in women with preterm labor, intact membranes, and no documented infection does not improve neonatal health and may have adverse effects in childhood (use is not recommended). Erythromycin is the antibiotic of choice for preterm premature rupture of membranes (with membrane rupture prior to 34 weeks gestation), the treatment of granuloma inguinale and lymphogranuloma venereum in pregnancy, and the treatment of or long-term suppression ofBartonella infection in HIV-infected pregnant patients. Erythromycin may be appropriate as an alternative agent for the prevention of group B streptococcal disease or the treatment of chlamydial infections in pregnant women (consult current guidelines). Lactation Enters breast milk/use caution (AAP considers compatible; AAP 2001 update pending) Breast-Feeding Considerations Erythromycin is excreted in breast milk; therefore, the manufacturer recommends that caution be exercised when administering erythromycin to breast-feeding women.
Due to the low concentrations in human milk, minimal toxicity would be expected in the nursing infant. One case report and a cohort study raise the possibility for a connection with pyloric stenosis in neonates exposed to erythromycin via breast milk and an alternative antibiotic may be preferred for breast-feeding mothers of infants in this age group. Nondose-related effects could include modification of bowel flora. Pregnancy & Lactation, In-Depth
Substrate of CYP2B6 (minor), CYP3A4 (major), P-glycoprotein; Note: Assignment of Major/Minor substrate status based on clinically relevant drug interaction potential; Inhibits CYP3A4 (moderate), Pglycoprotein Drug Interactions Alfentanil: Macrolide Antibiotics may decrease the metabolism of Alfentanil. Risk D: Consider therapy modification Alfuzosin: May enhance the QTc-prolonging effect of QTc-Prolonging Agents. Risk C: Monitor therapy Antifungal Agents (Azole Derivatives, Systemic): Macrolide Antibiotics may decrease the metabolism of Antifungal Agents (Azole Derivatives, Systemic). Antifungal Agents (Azole Derivatives, Systemic) may decrease the metabolism of Macrolide Antibiotics. Risk D: Consider therapy modification Antineoplastic Agents (Vinca Alkaloids): Macrolide Antibiotics may increase the serum concentration of Antineoplastic Agents (Vinca Alkaloids). Macrolides may also increase the distribution of Vinca Alkaloids into certain cells and/or tissues. Management: Consider an alternative to using a macrolide antibiotic when possible in order to avoid the potential for increased vinca alkaloid toxicity. Risk D: Consider therapy modification Artemether: May enhance the QTc-prolonging effect of QTc-Prolonging Agents. Risk X: Avoid combination BCG: Antibiotics may diminish the therapeutic effect of BCG. Risk X: Avoid combination Benzodiazepines (metabolized by oxidation): Macrolide Antibiotics may decrease the metabolism of Benzodiazepines (metabolized by oxidation).Risk D: Consider therapy modification Budesonide (Systemic, Oral Inhalation): CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Budesonide (Systemic, Oral Inhalation). Management: Consider reducing the oral budesonide dose when used together with a CYP3A4 inhibitor. This interaction is likely less severe with orally inhaled budesonide. Monitor patients closely for signs/symptoms of corticosteroid excess. Risk D: Consider therapy modification BusPIRone: Macrolide Antibiotics may decrease the metabolism of BusPIRone. Risk D: Consider therapy modification Calcium Channel Blockers: Macrolide Antibiotics may decrease the metabolism of Calcium Channel Blockers. Management: Consider using a noninteracting macrolide. Monitor for increased therapeutic effects of calcium channel blockers if an interacting macrolide antibiotic is initiated, or decreased effects if a macrolide is discontinued. Exceptions: Clevidipine. Risk D: Consider therapy modification
Erythromycin (Systemic) in Pregnancy & Lactation
Adverse Reactions Frequency not defined. Incidence may vary with formulation. Cardiovascular: QTc prolongation, torsade de pointes, ventricular arrhythmia, ventricular tachycardia Central nervous system: Seizure Dermatologic: Erythema multiforme, pruritus, rash, Stevens-Johnson syndrome, toxic epidermal necrolysis Gastrointestinal: Abdominal pain, anorexia, diarrhea, infantile hypertrophic pyloric stenosis, nausea, oral candidiasis, pancreatitis, pseudomembranous colitis, vomiting Hepatic: Cholestatic jaundice (most common with estolate), hepatitis, liver function tests abnormal Local: Phlebitis at the injection site, thrombophlebitis Neuromuscular & skeletal: Weakness Otic: Hearing loss Miscellaneous: Allergic reactions, anaphylaxis, hypersensitivity reactions, interstitial nephritis, urticaria Allergy and Idiosyncratic Reactions Macrolide Allergy
Metabolism/Transport Effects
CarBAMazepine: Macrolide Antibiotics may decrease the metabolism of CarBAMazepine. Risk D: Consider therapy modification Cardiac Glycosides: Macrolide Antibiotics may increase the serum concentration of Cardiac Glycosides. Risk D: Consider therapy modification Chloroquine: May enhance the QTc-prolonging effect of QTc-Prolonging Agents. Risk C: Monitor therapy Cilostazol: Macrolide Antibiotics may decrease the metabolism of Cilostazol. Risk D: Consider therapy modification Ciprofloxacin: May enhance the QTc-prolonging effect of QTc-Prolonging Agents. Risk C: Monitor therapy Ciprofloxacin (Systemic): May enhance the QTc-prolonging effect of QTc-Prolonging Agents. Risk C: Monitor therapy Cisapride: Macrolide Antibiotics may decrease the metabolism of Cisapride. Risk X: Avoid combination Clopidogrel: Macrolide Antibiotics may diminish the therapeutic effect of Clopidogrel. Risk C: Monitor therapy CloZAPine: Macrolide Antibiotics may decrease the metabolism of CloZAPine. Risk D: Consider therapy modification Colchicine: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Colchicine. Colchicine distribution into certain tissues (e.g., brain) may also be increased. Management: Colchicine is contraindicated in patients with impaired renal or hepatic function who are also receiving a p-glycoprotein inhibitor. In those with normal renal and hepatic function, reduce colchicine dose as directed. Risk D: Consider therapy modification Conivaptan: May increase the serum concentration of CYP3A4 Substrates. Risk X: Avoid combination Corticosteroids (Systemic): Macrolide Antibiotics may decrease the metabolism of Corticosteroids (Systemic). Risk D: Consider therapy modification CycloSPORINE: Macrolide Antibiotics may decrease the metabolism of CycloSPORINE. Risk C: Monitor therapy CycloSPORINE (Systemic): Macrolide Antibiotics may decrease the metabolism of CycloSPORINE (Systemic). Risk C: Monitor therapy CYP3A4 Inducers (Strong): May increase the metabolism of CYP3A4 Substrates. Risk C: Monitor therapy
CYP3A4 Inhibitors (Moderate): May decrease the metabolism of CYP3A4 Substrates. Risk C: Monitor therapy CYP3A4 Inhibitors (Strong): May decrease the metabolism of CYP3A4 Substrates. Risk D: Consider therapy modification CYP3A4 Substrates: CYP3A4 Inhibitors (Moderate) may decrease the metabolism of CYP3A4 Substrates. Risk C: Monitor therapy Dabigatran Etexilate: P-glycoprotein/ABCB1 Inhibitors may increase serum concentrations of the active metabolite(s) of Dabigatran Etexilate. Management: Dabigatran dose reductions may be needed. Specific recommendations vary considerably according to US vs Canadian labeling, specific P-gp inhibitor, renal function, and indication for dabigatran treatment. Refer to full monograph or dabigatran labeling. Risk D: Consider therapy modification Deferasirox: May decrease the serum concentration of CYP3A4 Substrates. Risk C: Monitor therapy Disopyramide: Macrolide Antibiotics may enhance the QTc-prolonging effect of Disopyramide. Macrolide Antibiotics may decrease the metabolism of Disopyramide. Risk X: Avoid combination Dronedarone: QTc-Prolonging Agents may enhance the QTc-prolonging effect of Dronedarone. Risk X: Avoid combination Eletriptan: Macrolide Antibiotics may decrease the metabolism of Eletriptan. Risk D: Consider therapy modification Eplerenone: Macrolide Antibiotics may decrease the metabolism of Eplerenone. Risk C: Monitor therapy Ergot Derivatives: Macrolide Antibiotics may enhance the adverse/toxic effect of Ergot Derivatives. Specifically leading the development of ergotism. Exceptions: Cabergoline. Risk D: Consider therapy modification Etravirine: May decrease the serum concentration of Macrolide Antibiotics. Clarithromycin AUC is reduced and levels of the active metabolite (14-hydroxy-clarithromycin) are modestly increased. Management: For the treatment of Mycobacterium avium complex, consider changing to alternative agent, such as azithromycin. Risk D: Consider therapy modification Everolimus: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Everolimus. Management: Everolimus dose reductions are required for patients being treated for subependymal giant cell astrocytoma or renal cell carcinoma. See prescribing information for specific dose adjustment and monitoring recommendations. Risk D: Consider therapy modification FentaNYL: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of FentaNYL. Management: Monitor patients extra closely for several days following initiation of the combination,
and fentanyl dosage reductions should be made as appropriate. Risk D: Consider therapy modification Fexofenadine: Erythromycin (Systemic) may increase the serum concentration of Fexofenadine. Risk C: Monitor therapy Gadobutrol: May enhance the QTc-prolonging effect of QTc-Prolonging Agents. Risk D: Consider therapy modification HMG-CoA Reductase Inhibitors: Macrolide Antibiotics may decrease the metabolism of HMG-CoA Reductase Inhibitors. Management: Avoid lovastatin or simvastatin with erythro-, clarithro-, or telithromycin. Limit pitavastatin to a 1 mg/day maximum adult dose with erythromycin. Atorvastatin dose adjustments may be required. Increase monitoring for toxicity with any such combination. Exceptions: Fluvastatin; Pravastatin; Rosuvastatin. Risk D: Consider therapy modification Indacaterol: May enhance the QTc-prolonging effect of QTc-Prolonging Agents. Risk C: Monitor therapy Lincosamide Antibiotics: May diminish the therapeutic effect of Erythromycin (Systemic). Risk X: Avoid combination Lumefantrine: May enhance the QTc-prolonging effect of QTc-Prolonging Agents. Risk X: Avoid combination Lurasidone: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Lurasidone. Risk D: Consider therapy modification Nilotinib: May enhance the QTc-prolonging effect of QTc-Prolonging Agents. Risk X: Avoid combination P-glycoprotein/ABCB1 Inducers: May decrease the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inducers may also further limit the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Risk C: Monitor therapy P-glycoprotein/ABCB1 Inhibitors: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inhibitors may also enhance the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, Tlymphocytes, testes, etc.). Risk C: Monitor therapy P-glycoprotein/ABCB1 Substrates: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inhibitors may also enhance the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Risk C: Monitor therapy
Pimecrolimus: CYP3A4 Inhibitors (Moderate) may decrease the metabolism of Pimecrolimus. Risk C: Monitor therapy Pimozide: Macrolide Antibiotics may enhance the QTc-prolonging effect of Pimozide. Macrolide Antibiotics may decrease the metabolism of Pimozide. QTc prolongation is a risk. Risk X: Avoid combination Pimozide: QTc-Prolonging Agents may enhance the QTc-prolonging effect of Pimozide. Risk X: Avoid combination QTc-Prolonging Agents: May enhance the adverse/toxic effect of other QTc-Prolonging Agents. Their effects can be additive, causing life-threatening ventricular arrhythmias. Risk D: Consider therapy modification QUEtiapine: May enhance the QTc-prolonging effect of QTc-Prolonging Agents. Risk X: Avoid combination QuiNIDine: Macrolide Antibiotics may decrease the metabolism of QuiNIDine. Risk D: Consider therapy modification QuiNINE: Macrolide Antibiotics may increase the serum concentration of QuiNINE. Risk X: Avoid combination QuiNINE: QTc-Prolonging Agents may enhance the QTc-prolonging effect of QuiNINE. QuiNINE may enhance the QTc-prolonging effect of QTc-Prolonging Agents. Risk X: Avoid combination Repaglinide: Macrolide Antibiotics may increase the serum concentration of Repaglinide. Risk C: Monitor therapy Rifamycin Derivatives: Macrolide Antibiotics may decrease the metabolism of Rifamycin Derivatives. Exceptions: Rifapentine. Risk D: Consider therapy modification Rivaroxaban: Erythromycin (Systemic) may increase the serum concentration of Rivaroxaban. Risk C: Monitor therapy Rivaroxaban: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Rivaroxaban. Risk C: Monitor therapy Salmeterol: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Salmeterol. Risk C: Monitor therapy Selective Serotonin Reuptake Inhibitors: Macrolide Antibiotics may decrease the metabolism of Selective Serotonin Reuptake Inhibitors.Exceptions: FluvoxaMINE; PARoxetine. Risk C: Monitor therapy
Silodosin: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Silodosin. Risk X: Avoid combination Sirolimus: Macrolide Antibiotics may decrease the metabolism of Sirolimus. Risk D: Consider therapy modification Tacrolimus: Macrolide Antibiotics may increase the serum concentration of Tacrolimus. Risk C: Monitor therapy Tacrolimus (Systemic): Macrolide Antibiotics may increase the serum concentration of Tacrolimus (Systemic). Risk C: Monitor therapy Tacrolimus (Topical): Macrolide Antibiotics may increase the serum concentration of Tacrolimus (Topical). Risk C: Monitor therapy Temsirolimus: Macrolide Antibiotics may enhance the adverse/toxic effect of Temsirolimus. Levels of sirolimus, the active metabolite, may be increased, likely due to inhibition of CYP-mediated metabolism. Risk D: Consider therapy modification Terfenadine: Macrolide Antibiotics may enhance the QTc-prolonging effect of Terfenadine. Macrolide Antibiotics may increase the serum concentration of Terfenadine. Risk X: Avoid combination Tetrabenazine: QTc-Prolonging Agents may enhance the QTc-prolonging effect of Tetrabenazine. Risk X: Avoid combination Theophylline Derivatives: Macrolide Antibiotics may decrease the metabolism of Theophylline Derivatives. Exceptions: Dyphylline. Risk D: Consider therapy modification Thioridazine: QTc-Prolonging Agents may enhance the QTc-prolonging effect of Thioridazine. Risk X: Avoid combination Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates. Risk C: Monitor therapy Topotecan: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Topotecan. Risk X: Avoid combination Toremifene: QTc-Prolonging Agents may enhance the QTc-prolonging effect of Toremifene. The risk for potentially dangerous arrhythmias may be increased. Risk X: Avoid combination Typhoid Vaccine: Antibiotics may diminish the therapeutic effect of Typhoid Vaccine. Only the live attenuated Ty21a strain is affected. Management: Vaccination with live attenuated typhoid vaccine (Ty21a) should be avoided in patients being treated with systemic antibacterial agents. Use of this vaccine should be postponed until at least 24 hours after cessation of antibacterial agents. Risk D: Consider therapy modification
Vandetanib: QTc-Prolonging Agents may enhance the arrhythmogenic effect of Vandetanib. Risk X: Avoid combination Vemurafenib: QTc-Prolonging Agents may enhance the QTc-prolonging effect of Vemurafenib. Risk X: Avoid combination Vitamin K Antagonists (eg, warfarin): Macrolide Antibiotics may increase the serum concentration of Vitamin K Antagonists. Risk C: Monitor therapy Zafirlukast: Erythromycin (Systemic) may decrease the serum concentration of Zafirlukast. Risk C: Monitor therapy Ziprasidone: QTc-Prolonging Agents may enhance the QTc-prolonging effect of Ziprasidone. The risk of a severe arrhythmia may be increased.Risk X: Avoid combination Zopiclone: Macrolide Antibiotics may increase the serum concentration of Zopiclone. Risk D: Consider therapy modification Ethanol/Nutrition/Herb Interactions Ethanol: Avoid ethanol (may decrease absorption of erythromycin or enhance ethanol effects). Food: Erythromycin serum levels may be altered if taken with food (formulation-dependent). Herb/Nutraceutical: St John's wort may decrease erythromycin levels. Test Interactions False-positive urinary catecholamines, 17-hydroxycorticosteroids and 17-ketosteroids Nursing: Physical Assessment/Monitoring Assess results of culture and sensitivity tests and patient's previous allergy history prior to therapy. Monitoring: Lab Tests Perform culture and sensitivity studies prior to initiating drug therapy. Patient Education
Tablets/capsules: Take around-the-clock, with a full glass of water (not juice or milk); may take with food to reduce GI upset. Do not chew or crush extended release capsules or tablets. Avoid alcohol (may cause adverse response). May cause nausea, vomiting, or mouth sores. Report immediately any unusual malaise, nausea, vomiting, abdominal colic, or fever; skin rash or itching; easy bruising or bleeding; vaginal itching or discharge; watery or bloody diarrhea; yellowing of skin or eyes, pale stool or dark urine; persistent diarrhea; white plaques, sores, or fuzziness in mouth; or any change in hearing. Dosage Forms Excipient information presented when available (limited, particularly for generics); consult specific product labeling. Capsule, delayed release, enteric coated pellets, oral, as base: 250 mg
Erythrocin: 250 mg [contains potassium 5 mg (0.1 mEq)/tablet, sodium 56.7 mg (2.5 mEq)/tablet] Erythrocin: 500 mg [sodium free; contains potassium 7 mg (0.2 mEq)/tablet] Tablet, delayed release, enteric coated, oral, as base: Ery-Tab: 250 mg [contains sodium 8.3 mg (0.4 mEq)/tablet] Ery-Tab: 333 mg [contains sodium 11.2 mg (0.5 mEq)/tablet] Ery-Tab: 500 mg [contains sodium 16.7 mg (0.7 mEq)/tablet] Tablet, polymer coated particles, oral, as base:
Granules for suspension, oral, as ethylsuccinate [strength expressed as base]: PCE: 333 mg [contains sodium 0.5 mg (0.02mEq)/tablet] E.E.S.: 200 mg/5 mL (200 mL) [contains sodium 25.9 mg (1.1 mEq)/5 mL; cherry flavor] PCE: 500 mg [dye free, sodium free] E.E.S.: 200 mg/5 mL (100 mL) [contains sodium 25.9 mg (1.1 mEq)/5 mL; cherry flavor] Mechanism of Action Injection, powder for reconstitution, as lactobionate [strength expressed as base]: Erythrocin Lactobionate-I.V.: 500 mg Powder, for prescription compounding: Erythro-RX: USP: 100% (50 g) Powder for suspension, oral, as ethylsuccinate [strength expressed as base]: Distribution: EryPed: 200 mg/5 mL (100 mL) [contains sodium 117.5 mg (5.1 mEq)/5 mL; fruit flavor] Relative diffusion from blood into CSF: Minimal even with inflammation EryPed: 400 mg/5 mL (100 mL) [contains sodium 117.5 mg (5.1 mEq)/5 mL; banana flavor] CSF:blood level ratio: Normal meninges: 2% to 13%; Inflamed meninges: 7% to 25% Tablet, oral, as base: 250 mg, 500 mg Protein binding: Base: 73% to 81% Tablet, oral, as ethylsuccinate [strength expressed as base]: 400 mg Metabolism: Demethylation primarily via hepatic CYP3A4 E.E.S.: 400 mg [contains potassium 10 mg (0.3 mEq)/tablet, sodium 47 mg (2 mEq)/tablet] Half-life elimination: Peak: 1.5-2 hours; End-stage renal disease: 5-6 hours Tablet, oral, as stearate [strength expressed as base]: Inhibits RNA-dependent protein synthesis at the chain elongation step; binds to the 50S ribosomal subunit resulting in blockage of transpeptidation Pharmacodynamics/Kinetics Absorption: Oral: Variable but better with salt forms than with base form; 18% to 45%; ethylsuccinate may be better absorbed with food
Time to peak, serum: Base: 4 hours; Ethylsuccinate: 0.5-2.5 hours; delayed with food due to differences in absorption Excretion: Primarily feces; urine (2% to 15% as unchanged drug) Pharmacogenomic Genes of Interest
HMG-CoA reductase inhibitors, also known as the statins, effectively decrease the hepatic cholesterol biosynthesis resulting in the reduction of blood LDL-cholesterol concentrations. The AUC of atorvastatin (Lipitor) was increased 33% by erythromycin administration. Combination of erythromycin and lovastatin (Mevacor) has been associated with rhabdomyolysis (Ayanian, et al). The mechanism of erythromycin is inhibiting the CYP3A4 metabolism of atorvastatin, lovastatin, and cerivastatin. Simvastatin (Zocor) would likely be affected in a similar manner by the coadministration of erythromycin. Clarithromycin (Biaxin) may exert a similar effect as erythromycin on atorvastatin, lovastatin, cerivastatin, and simvastatin. Effects on Dental Treatment Key adverse event(s) related to dental treatment: Oral candidiasis. Effects on Bleeding
y y y y
ATP-Binding Cassette, Sub-Family B, Member 1 Cardiac Potassium Ion Channels Cardiac Sodium Channel CYP3A4
Dental Use No information available to require special precautions Alternative to penicillin VK for treatment of orofacial infections Dental Usual Dosing Local Anesthetic/Vasoconstrictor Precautions Treatment of orofacial infections: Adults: Oral: Erythromycin is one of the drugs confirmed to prolong the QT interval and is accepted as having a risk of causing torsade de pointes. In terms of epinephrine, it is not known what effect vasoconstrictors in the local anesthetic regimen will have in patients with a known history of congenital prolonged QT interval or in patients taking any medication that prolongs the QT interval. Until more information is obtained, it is suggested that the clinician consult with the physician prior to the use of a vasoconstrictor in suspected patients, and that the vasoconstrictor (epinephrine, mepivacaine and levonordefrin [Carbocaine 2% with Neo-Cobefrin]) be used with caution. See Dental Health Professional Considerations. Dental Health Professional Considerations Erythromycin is known to prolong the QT interval. The QT interval is measured as the time and distance between the Q point of the QRS complex and the end of the T wave in the ECG tracing. After adjustment for heart rate, the QT interval is defined as prolonged if it is more than 450 msec in men and 460 msec in women. A long QT syndrome was first described in the 1950s and 60s as a congenital syndrome involving QT interval prolongation and syncope and sudden death. Some of the congenital long QT syndromes were characterized by a peculiar electrocardiographic appearance of the QRS complex involving a premature atria beat followed by a pause, then a subsequent sinus beat showing marked QT prolongation and deformity. This type of cardiac arrhythmia was originally termed torsade de pointes (translated from the French as twisting of the points). Erythromycin is considered as having a risk of causing torsade de pointes. Since it is not known what effect vasoconstrictors in the local anesthetic regimen will have in patients with a known history of congenital prolonged QT interval or in patients taking any medication that prolongs the QT interval, a medical consult is suggested. Base: 250-500 mg every 6-12 hours Ethylsuccinate: 400-800 mg every 6-12 hours Mental Health: Effects on Mental Status Macrolides have been reported to cause nightmares, confusion, anxiety, and mood lability Mental Health: Effects on Psychiatric Treatment Contraindicated with pimozide; may increase concentration of bromocriptine, carbamazepine, and triazolam Cardiovascular Considerations Erythromycin, when used with drugs that affect the QT interval (eg, cisapride, quinidine) or when administered to patients with a prolonged QT interval, may further increase the QT interval and the risk of torsade de pointes (proarrhythmias).
Many patients cannot tolerate erythromycin because of abdominal pain and nausea; the mechanism of this adverse effect appears to be the motilin agonistic properties of erythromycin in the GI tract. For these patients, clindamycin is indicated as the alternative antibiotic for treatment of orofacial infections.
Potrebbero piacerti anche
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- Vocations The New Midheaven Extension ProcessDocumento266 pagineVocations The New Midheaven Extension ProcessMiss M.100% (24)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Why File A Ucc1Documento10 pagineWhy File A Ucc1kbarn389100% (4)
- Course Projects PDFDocumento1 paginaCourse Projects PDFsanjog kshetriNessuna valutazione finora
- AcousticsDocumento122 pagineAcousticsEclipse YuNessuna valutazione finora
- N50-200H-CC Operation and Maintenance Manual 961220 Bytes 01Documento94 pagineN50-200H-CC Operation and Maintenance Manual 961220 Bytes 01ANDRESNessuna valutazione finora
- UnixDocumento251 pagineUnixAnkush AgarwalNessuna valutazione finora
- Endometab Exam 2018Documento8 pagineEndometab Exam 2018teabagmanNessuna valutazione finora
- Pricing of A Revolutionary ProductDocumento22 paginePricing of A Revolutionary ProductiluvparixitNessuna valutazione finora
- En 50124 1 2001Documento62 pagineEn 50124 1 2001Vivek Kumar BhandariNessuna valutazione finora
- Buildingawinningsalesforce WP DdiDocumento14 pagineBuildingawinningsalesforce WP DdiMawaheb ContractingNessuna valutazione finora
- Industrial Machine and ControlsDocumento31 pagineIndustrial Machine and ControlsCarol Soi100% (4)
- SEC CS Spice Money LTDDocumento2 pagineSEC CS Spice Money LTDJulian SofiaNessuna valutazione finora
- Mixing and Agitation 93851 - 10 ADocumento19 pagineMixing and Agitation 93851 - 10 Aakarcz6731Nessuna valutazione finora
- Technical Data Sheet TR24-3-T USDocumento2 pagineTechnical Data Sheet TR24-3-T USDiogo CNessuna valutazione finora
- LS01 ServiceDocumento53 pagineLS01 ServicehutandreiNessuna valutazione finora
- ULANGAN HARIAN Mapel Bahasa InggrisDocumento14 pagineULANGAN HARIAN Mapel Bahasa Inggrisfatima zahraNessuna valutazione finora
- Metalcor - 1.4507 - Alloy - F255 - Uranus 52N - S32520Documento1 paginaMetalcor - 1.4507 - Alloy - F255 - Uranus 52N - S32520NitinNessuna valutazione finora
- Electric Vehicles PresentationDocumento10 pagineElectric Vehicles PresentationVIBHU CHANDRANSH BHANOT100% (1)
- Avid Final ProjectDocumento2 pagineAvid Final Projectapi-286463817Nessuna valutazione finora
- Rubric For Aet570 BenchmarkDocumento4 pagineRubric For Aet570 Benchmarkapi-255765082Nessuna valutazione finora
- Bachelors - Harvest Moon Animal ParadeDocumento12 pagineBachelors - Harvest Moon Animal ParaderikaNessuna valutazione finora
- De DusterDocumento6 pagineDe DusterArstNessuna valutazione finora
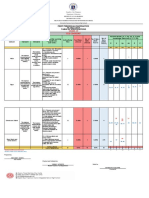
- Revised Final Quarter 1 Tos-Rbt-Sy-2022-2023 Tle-Cookery 10Documento6 pagineRevised Final Quarter 1 Tos-Rbt-Sy-2022-2023 Tle-Cookery 10May Ann GuintoNessuna valutazione finora
- Brochure International ConferenceDocumento6 pagineBrochure International ConferenceAnubhav Sharma sf 12Nessuna valutazione finora
- Internal Analysis: Pertemuan KeDocumento15 pagineInternal Analysis: Pertemuan Kekintan utamiNessuna valutazione finora
- Q4 Music 6 Module 2Documento15 pagineQ4 Music 6 Module 2Dan Paolo AlbintoNessuna valutazione finora
- Automated Dish Washer v1.1Documento21 pagineAutomated Dish Washer v1.1Anonymous XXCCYAEY6M67% (3)
- Bluestar Annual Report 2021-22Documento302 pagineBluestar Annual Report 2021-22Kunal PohaniNessuna valutazione finora
- Functions: Var S AddDocumento13 pagineFunctions: Var S AddRevati MenghaniNessuna valutazione finora