Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Clin Pharm1
Caricato da
tho2793Descrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Clin Pharm1
Caricato da
tho2793Copyright:
Formati disponibili
Patient Assessment and the Pharmacist s Role in Patient Care MF Bacayo MS Evolution of Pharmacy Practice First stage (late
1850 s to early 1900 s) Major influence of this stage was the entrance of largescale drug manufacturing. The pharmacist was responsible for delivering pure, unadulterated medications and for providing good advice to the customers. As the pharmacy industry continued to grow, more and more medications were sold as prefabricated drug products rather than as medications that the pharmacist needed to compound.
Responsible provision of drug therapy for the purpose of achieving definite outcomes that improve a patient s quality of life These outcomes are (i) curing of a disease, (ii) eliminating or reducing of a patient s symptoms, (iii) arresting or slowing of a disease process, (iv) preventing a disease or symptoms. Philosophy (Pharmaceutical Care) A societal need for pharmacists to address drug-related problems A patient-centered approach to meet this need A practice based on caring about and for patients A responsibility for finding and responding to the patient s drug therapy problems. The central component of pharmaceutical care is caring about the patient. Having sincere concern for the patient and taking the time and effort to help that patient as a pharmacist and healthcare professional. The pharmacist will incorporate pharmaceutical care into his/her practice regardless of practice setting or potential obstacles. Is designed to complement existing patient care practices to make drug therapy more safe and effective. ASHP s five primary elements of pharmaceutical care:
Second Stage: (early 1900 s to mid 1960 s) Attention focused primarily on educational reform as the method to advance the profession. Very effective medications came on the market during the 1950 s, which increased the number of prescriptions being filled by 50%. APhA code of ethics from 1922 to 1969 prohibited the pharmacists from discussing the therapeutic effects or the composition of a prescription with a patient. (pharmacists were considered to be overeducated for a diminishing professional function).
Third Stage: (late 1960s to 1980s) The functions of the role expanded rapidly, increasing professional diversity. The pharmacist was beginning to provide new clinical services such as pharmacokinetics, drug information, and drug-use control. In 1969, APhA Code of Ethics allowed pharmacist to talk with patients about their medications, but the pharmacist s role continued to focus primarily on drugs and their delivery. Fourth Stage: (during the 1990s) This is the patient care stage, along with the concept of pharmaceutical care . Patient-centered care Pharmaceutical Care:
It is medication-related It is the care that is directly provided to the patient It is provided to produce definite outcomes These outcomes are intended to improve the patient s quality of life The provider (pharmacist) accepts personal responsibility for the outcomes. APhA principles delineate five key characteristics of pharmaceutical care: A professional relationship must be established and maintained. Patient-specific medical information must be collected, organized, recorded, and maintained. Patient-specific medical information must be evaluated and a drug therapy plan developed mutually with the patient.
APhA principles delineate five key characteristics of pharmaceutical care: The pharmacist assures that the patient has all supplies, information, and knowledge necessary to carry out the drug therapy plan. The pharmacist reviews, monitors, and modifies the therapeutic plan as necessary and appropriate, in concert with the patient and the healthcare team. Three Primary Responsibilities: To ensure that the patient s drug therapy is appropriately indicated, the most effective available, the safest possible, the most convenient to take, and the most economical. To identify, resolve, and prevent any drug therapy problems To ensure that the patient s therapeutic goals are met and that optimal health-related outcomes are attained. Drug Therapy Problems: Is any undesirable event experienced by the patient that involves drug therapy and that actually/potentially interferes with a desired patient outcome. Is a patient problem that is either caused by or may be treated with a drug. Cause a significant amount of morbidity and mortality. Common Drug Therapy Problems and their Causes:
Patients have all drug therapies necessary to resolve any untreated indications. Patient Care Process .. Patient Assessment: Is defined as the process through which pharmacist evaluates patient information both subjective and objective that was gathered from the patient and other sources and makes decisions regarding: (i) the health status of the pateint, (ii) drug therapy needs and problems; (iii) interventions that will resolve identified drug problems and prevent future problems; and (iv) follow-up to ensure that patient outcomes are being met. Pharmacotherapy Workup: This is a systematic, consistent process for patient data evaluation and assessment. This is a framework for organizing and evaluating patient specific data and should be used each time the pharmacist makes a drug therapy decision. This reflects the cognitive process involved with the patient assessment process. Logical questions regarding drug therapy needs: Does the patient have an appropriate indication for each of his/her drug therapies? Are these drug therapies the most effective for his/or her medical condition? Are the drug therapies causing any adverse /side effects?
1. Unneccessary drug therapy 2. Wrong drug 3. Dose too low 4. Dose too high 5. Adverse drug reaction Patient Assessment: 6. Nonadherence 7. Additional drug therapy Actions of Pharmacist (drug therapy problems): Patients have appropriate indication for every drug they are taking. Patient s drug therapy is effective. Patient s drug therapy is safe. Patients can comply with drug therapy and other aspects of their care plan. Is the process through which pharmacist evaluates patient information that was gathered from the patient and other sources and makes decisions regarding: 1. Health status of the patient 2. Drug therapy needs and problems 3. Interventions that will resolve identified drug problems and prevent future problems. 4. Follow-up to ensure that patient outcomes are met. Patient Assessment Questions: Is the patient able and willing to comply with the drug therapies? Is each of the patient s medical problems/symptoms/complaints being treated with drug therapy (if appropriate)?
Are any of the patient s complaints/symptoms or abnormal objective/physical findings caused by drug therapy? (consider possible adverse effects of drug therapy). What are the other possible causes of the patient s complaints/symptoms or abnormal objective/physical findings? (consider other medical conditions) Patient Assessment Questions: Are each of the medications appropriately indicated? (appropriate medical condition for each drug) Are each of the medications the most efficacious and safest possible? (for the medical condition, for the patient (age, gender, renal and liver function, weight, and other medical conditions)) Patient Assessment Questions: Is the patient experiencing any adverse effects from the drug therapy? (if yes, can any of the ADE be resolved?) Are there any drug interactions that will impair efficacy or safety? ( consider prescription and non-prescription, are there any drug-food, drug-laboratory test interactions) Patient Assessment Questions: Is the patient able to follow the drug regimen? (does the patient understand how to appropriately take the medications?; can the patient afford the drug therapy?) Does the patient need additional drug therapy for an untreated indication? Synergism with current therapy? prophylaxis Documentation: Provides a permanent record of patient information. Provides a permanent record and evidence of patient care acitivities by the pharmacist. Communicates essential information to other pharmacists and healthcare professionals. Serves as a legal record of patient care that was provided. Provides evidence of patient interventions and medication therapy management services for reimbursement. Characteristic of useful documentation: Information that is neat, organized, and able to be found quickly. Information that is easily understandable, so that any healthcare professional can determine what the
problems were, what actions were taken, and what follow-up is needed. Accurate subjective and objective information. An assessment of the patient information, focusing on drug therapy problems. A plan to resolve any problems that were identified. A therapeutic monitoring plan for future follow-up to ensure that any problems are resolved and that patient outcomes are met. SOAP Note: The most common-and universally recognized-format for documenting patient information in the healthcare system. Subjective, Objective, Assessment, and Plan Subjective section: Includes information that is given by the patient, family members, significant others, or caregivers. Complaints/symptoms or reason for the visit from the patient in his or her own words (chief complaint) Recent history that pertains to those symptoms (history of present illnes) Past medical history Medication history, including adherence and adverse effects (from the pateint) Allergies, social and/or family history. Review of systems Objective section: Vital signs Physical findings or physical examination (if possible) Laboratory test result s Serum drug concentrations Various diagnostic test results Computerized medication profile with refill information Assessment section: Involves critical thinking and analysis by the pharmacist. The pharmacist analyzes the subjective and objective information and determines the health-status of the patient.
If the problem is identified for the first time, adding a notation of newly identified is helpful. resolved , worsened , or stable (follow-up assessment or re-evaluation) This section provides the basis or rationale for the plan section. Plan section: Involves actions that were-or need to be-taken to resolve any problems that have been identified. Sufficient details need to be included, without being too lengthy, so that future pharmacist or other healthcare professionals can easily understand what took place during the patient encounter and what follow-up actions are necessary. Case study 1 Jb is a 74-year old man who comes to the pharmacy for a refill of his antihypertensive medication, atenolol. As he approaches the pharmacy counter, he loses his balance slightly, but catches himself on the counter. The pharmacist asks, Are you okay, Joe? the patient answers, Oh, yes, I m fine. I just stumbled a little. I do that often these days. I need a refill of my blood pressure medicine. the pharmacist pulls up Joe s drug therapy profile on the computer screen and asks, what s the name of the medication? the patient answers, I need my atenolol. Assessment of the Patient: Pharmacist: so how long have you been having problems with your balance? Joe: oh, it s not a problem. I ve just been a little lightheaded the past couple of weeks. I guess it s just old age. Pharmacist: how is your energy level? Joe: I don t do a whole lot anymore, so I guess I don t need much energy at my age. Pharmacist: how have you been feeling otherwise? Have you been having any other problems? Joe: no, otherwise I feel okay Pharmacist: I notice in your profile that you just started taking the atenolol 2 weeks ago. How have you been taking it? Joe: I take it with breakfast and supper. Just like my other blood pressure medicine. Pharmacist: actually, you should be taking it just once a day. why don t you have a seat over here and let me check your blood pressure and heart rate. They could be
too low from the atenolol, and that could be causing your light-headedness and low energy. Joe s heart rate is 48bpm, bp is 114/72 and 112/70 mm Hg. Pharmacist: your heart rate and blood pressure are lower than they should be. I think this is probably because you are taking the atenolol twice a day rather than once a day, and this is probably causing the light-headedness and decreased energy. I ll go ahead and get the refill for you, but make sure that you take it just once a day. Joe: okay, I guess I never paid attention to it. I just figured it was the same as the other medicine I m taking. From now on, I ll take it with my breakfast. Pharmacist: that would be fine. I also want you to come back in a week so that I can re-check your BP and HR and see if you re feeling better. Joe: that sounds like a good idea to me. Thanks for taking the time to check into this. Patient Care Plan: Patient name: JB Date: 9/8/08 Medical problems: hypertension Current medications: atenolol 25 mg (one tablet once daily), captopril 12.5 mg (one tablet twice a day) Subjective data: comes in for atenolol refill. C/O occasional ligh-theadedness, decreased energy level, and loss of balance over the past 2 weeks. No other C/O. currently taking the atenolol twice a day for the past two weeks. Objective data: saw patient lose his balance on the way to the pharmacy counter. heart rate: 48 bpm blood pressure: 114/72, 112/70 mm Hg Assessment: bradycardia and hypotension-new onsetprobably caused by nonadherence to the atenolol. Plan: instructed patient to take the atenolol once a day with breakfast and captopril twice a day as hehas been doing. follow-up in 1 week to re-check heart rate and blood pressure. If still low, call the physician and see about possibly D/C the atenolol. Questions: Briefly describe the concept of pharmaceutical care.
What are the pharmacist s primary responsibilities in providing pharmaceutical care to patients? Briefly describe how the concept of patient assessment is intertwined with the pharmacist s role in patient care. Case study 2: MG is a 48-year old woman going through menopause. She comes to the pharmacy for a refill on her Premarin, which she has been taking for 6 months now. The pharmacist often chats with MG about her children, but she seems distracted today. When the pharmacist asks MG if everything is all right, MG asks if she can speak to the pharmacist in private. The pharmacist invites MG into the patient consultation room.
Thanks for listening .
Potrebbero piacerti anche
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Cost-Effective Analysis of The Combination Therapies, Losartan + Hydrochlorothiazide and Bisoprolol + Hydrochlorothiazide For HypertensionDocumento1 paginaCost-Effective Analysis of The Combination Therapies, Losartan + Hydrochlorothiazide and Bisoprolol + Hydrochlorothiazide For Hypertensiontho2793Nessuna valutazione finora
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Graph For AEDDocumento1 paginaGraph For AEDtho2793Nessuna valutazione finora
- Dummy TablesDocumento2 pagineDummy Tablestho2793100% (1)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Drug Incompatibilities and InteractionDocumento3 pagineDrug Incompatibilities and Interactiontho27930% (1)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Clin PharmDocumento5 pagineClin Pharmtho2793Nessuna valutazione finora
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Curriculum VitaeDocumento4 pagineCurriculum Vitaetho2793Nessuna valutazione finora
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Blooms TaxonomyDocumento2 pagineBlooms Taxonomytho2793Nessuna valutazione finora
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- ChloroformDocumento2 pagineChloroformtho2793Nessuna valutazione finora
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Capsule ProposalDocumento6 pagineCapsule Proposaltho2793Nessuna valutazione finora
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- BibliographyDocumento3 pagineBibliographytho2793Nessuna valutazione finora
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
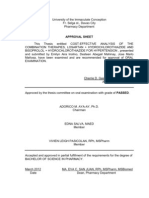
- Approval SheetDocumento1 paginaApproval Sheettho2793Nessuna valutazione finora
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Company Law Handout 3Documento10 pagineCompany Law Handout 3nicoleclleeNessuna valutazione finora
- MSEA News, Jan-Feb 2014Documento20 pagineMSEA News, Jan-Feb 2014Justin HinkleyNessuna valutazione finora
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- Standard Cost EstimatesDocumento12 pagineStandard Cost EstimatesMasroon ẨśầŕNessuna valutazione finora
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Adjectives With Cork English TeacherDocumento19 pagineAdjectives With Cork English TeacherAlisa PichkoNessuna valutazione finora
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Chapter 1 Hospital and Clinical Pharmacy Choplete PDF Notes D.Pharma 2nd Notes PDF NoteskartsDocumento7 pagineChapter 1 Hospital and Clinical Pharmacy Choplete PDF Notes D.Pharma 2nd Notes PDF NoteskartsDrx Brajendra LodhiNessuna valutazione finora
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- SVPWM PDFDocumento5 pagineSVPWM PDFmauricetappaNessuna valutazione finora
- VoIP Testing With TEMS InvestigationDocumento20 pagineVoIP Testing With TEMS Investigationquantum3510Nessuna valutazione finora
- Nasoya FoodsDocumento2 pagineNasoya Foodsanamta100% (1)
- Qa-St User and Service ManualDocumento46 pagineQa-St User and Service ManualNelson Hurtado LopezNessuna valutazione finora
- Brush Seal Application As Replacement of Labyrinth SealsDocumento15 pagineBrush Seal Application As Replacement of Labyrinth SealsGeorge J AlukkalNessuna valutazione finora
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- SPIE Oil & Gas Services: Pressure VesselsDocumento56 pagineSPIE Oil & Gas Services: Pressure VesselsSadashiw PatilNessuna valutazione finora
- Usha Unit 1 GuideDocumento2 pagineUsha Unit 1 Guideapi-348847924Nessuna valutazione finora
- Immovable Sale-Purchase (Land) ContractDocumento6 pagineImmovable Sale-Purchase (Land) ContractMeta GoNessuna valutazione finora
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Developments in Prepress Technology (PDFDrive)Documento62 pagineDevelopments in Prepress Technology (PDFDrive)Sur VelanNessuna valutazione finora
- Medical Devices RegulationsDocumento59 pagineMedical Devices RegulationsPablo CzNessuna valutazione finora
- TATA Power - DDL:ConfidentialDocumento15 pagineTATA Power - DDL:ConfidentialkarunakaranNessuna valutazione finora
- WWW - Manaresults.co - In: Internet of ThingsDocumento3 pagineWWW - Manaresults.co - In: Internet of Thingsbabudurga700Nessuna valutazione finora
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (120)
- Computer System Sevicing NC Ii: SectorDocumento44 pagineComputer System Sevicing NC Ii: SectorJess QuizzaganNessuna valutazione finora
- Manual Generador KohlerDocumento72 pagineManual Generador KohlerEdrazGonzalezNessuna valutazione finora
- G JaxDocumento4 pagineG Jaxlevin696Nessuna valutazione finora
- Prepositions Below by in On To of Above at Between From/toDocumento2 paginePrepositions Below by in On To of Above at Between From/toVille VianNessuna valutazione finora
- Central Banking and Monetary PolicyDocumento13 pagineCentral Banking and Monetary PolicyLuisaNessuna valutazione finora
- OOPS Notes For 3rd Sem ALL ChaptersDocumento62 pagineOOPS Notes For 3rd Sem ALL Chaptersabhishek singh83% (6)
- Province of Camarines Sur vs. CADocumento8 pagineProvince of Camarines Sur vs. CACrisDBNessuna valutazione finora
- Mayor Breanna Lungo-Koehn StatementDocumento2 pagineMayor Breanna Lungo-Koehn StatementNell CoakleyNessuna valutazione finora
- 254 AssignmentDocumento3 pagine254 AssignmentSavera Mizan ShuptiNessuna valutazione finora
- Risk and Uncertainty in Estimating and TenderingDocumento16 pagineRisk and Uncertainty in Estimating and TenderingHaneefa ChNessuna valutazione finora
- BBCVDocumento6 pagineBBCVSanthosh PgNessuna valutazione finora
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Catalogue of The Herbert Allen Collection of English PorcelainDocumento298 pagineCatalogue of The Herbert Allen Collection of English PorcelainPuiu Vasile ChiojdoiuNessuna valutazione finora
- Deshidratador Serie MDQDocumento4 pagineDeshidratador Serie MDQDAIRONessuna valutazione finora