Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Diseases
Caricato da
Erika DellosaCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Diseases
Caricato da
Erika DellosaCopyright:
Formati disponibili
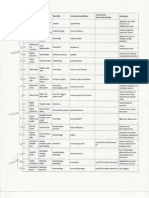
Disease Tuberculo sis Kochs Disease, Phthisis, Galloping consumptio n, TB
Causative agent Mycobacter ium tuberculosi s, M. bovis
MOT Droplet infection, Cows Milk containing Mycobacte rium bovis
Pathogno monic sign Hemopt ysis
Diagnosis AFB SMEAR Chest Xray Tuberculi n testing/ Mantoux Test
Specific s/sx
DOC DIRECTLY Observed Treatment Short Course (DOTS) RIPES
Nursing intervention 1. Diet- if with anorexiaSFF; high protein 2. Drugstrict compliance 3. Rest Contraindicat e: Chest Clapping (stimulates hemoptysis )
Prevention Immunizatio n BCG at birth 1 dose @ Right deltoid Proper disposal of nasopharyng eal secretion Covering of nose and mouth when coughing or sneezing Preventive: Proper disposal of nasopharyngeal secretions Covering of nose and mouth when sneezing and coughing (cough manners)
Pneumoni a
Pneumococ cus
droplet infection/i ndirect contact
Rusty or prune juice sputum
sputum exam chest x-ray
DIPHTHER IA
Coryneba cterium diptheriae or the Klebs-
Respirator y droplets
Formati on of pseudo membra ne
Nose and throat swab /culture
Fever, Dyspnea , Cyanosis Productive cough Chest pain aggravated by coughing Increase RR, shallow Stabbing chest pain when coughing In children: Nasal flaring Chest retraction Nasal Sero-sanguinos secretion with foul mousyodor
Procaine penicillin Less than 2 months = 200,000 IU 2-12 months = 400,000 IU 1-5 years = 800,000 IU
1. Mainte nance of proper airway 2. Relieve chest pain 3. Adequ ate nutrition 4. Preven t spread of infection by disposing secretions properly
1. antidiphtheria serum 2. AntibioticsPenicillin
1. Place the patient in CBR until 2 weeks after recovery
Immunizatio n-DPT at 6 weeks after birth at one month
Loeffler Bacillus
Schick Test Moloneys test
Nasopharyngeal Marked degree of toxemia Swollen lymph nodes Dysphagia Laryngeal Aphonia BOD, chest indrawing Croup
3. To prevent respiratory obstruction Tracheosto my
Pertussis Whooping cough
Hemophilu s pertusis, Bordetella pertusis
Nasophary ngeal secretions; Droplet
Bordet Gengou Agar plate
INFLUENZ A Flu
Myxovirus Influenza virus A, B, C
Droplet, contact with nasophary
Catarrhal Erythromycin -Colds, cough at , Penicillin night, fever,listlessne ss (balisa) Spasmodic/ Paroxysmal -5 to 10 forceful successive coughing w/c ends in a prolonged inspiratory phase or a whoop -Vomiting -Teary red eyes and protrusion of eyeballs Convulsion Convalescence - s/s subside and patient can recover a. Respiratory most common b. Intestinal c. Nervous
(to prevent myocarditis ) 2. Maintenanc e of proper airway 3. Small frequent feedings (soft) 4. Use ice collar to relieve pain 1. Complete bed rest 2. Prevent Aspiration 3. Application of abdominal binder
interval Cover of nose and mouth when sneezing and coughing Never kiss the patient
Immunizatio n - DPT Proper disposal of nasopharyngeal secretions
a. Adequate rest and good ventilation b. TSB
Annual vaccination for high risk people or for
ngeal secretions
c. Monitor vital signs d. Adequate nutrition Fever, body weakness or muscle pain, cough, sore throat, sore eyes, DOB Sudden onset of high grade fever Headaches/body aches Ist day- mild respiratory symptoms After 2 days- dry cough and respiratory difficulty Supportive treatment as needed (e.g. oxygen, fluids). >Empiric broad spectrum antibiotics also given against communityacquired pneumonia and atypical pneumonia a. Adequate rest and good ventilation b. TSB c. Monitor vital signs d. Adequate nutrition
individuals who wish to reduce chances of getting flu avoid migratory birds, Thorough cooking of poultry meat Containmen t Mask N95 Strict quarantine and isolation measures
Avian Influenza Bird flu, AI
Influenza A H5N1 virus
Direct contact with droppings of infected bird Person-toperson through respiratory droplets and direct contact with body fluids of a person with SARS.
Severe Acute Respirator y Syndrome (SARS)
Corona virus, SARS CoV
GONORRH EA Gonococcu s (GC), Gonoclap, Jack, Gleet, Morning Drop
Direct contact with exudate via sexual contact transmissi on to the neonate during the passage through the birth canal
Neisseria gonorrhea
Positive gram stain smear of discharge or secretion Positive culture
Male - purulent discharge - pyuria - redness and edema of urinary meatus - protatitis - chronic-scar in epididymis -obstruct flow of sperms- sterility Female burning sensation upon urination if urinary meatus is involved - (+/-) of purulent discharge abscess formation in Bartholins/Ske nes glands
Tetracycline 500mg QID for 7 days Ceftriaxone for pregnant women Penicillin Other treatment for patients with coexisting chlamidial infection
SYPHILLIS Pox, Lues, Bad Blood Disease
Treponema pallidum
Sexual contact Blood transfusi on Placenta l transmis sion(5th mo of gestatio n)
VDRLvenereal disease researsh lab RPR- rapid plasma reagin test Fluorescen t Treponem al
Primary : chancre Secondary : condyloma lata, Mucous patches mouth, throat, cervix, patchy alopecia, moth eaten appearance, iritis, arthritic and bone pain
Penicillin G Newborn = 100,000 units/kg single IM dose Adult = 2.4 million units IM single dose
>Erythromyci n prophylaxis for ophthalmia neonatorum >Encourage follow up cultures in 4 to 7 days after treatment and again at 6 months >Teach importance of abstinence from sexual intercourse until cultures are negative >stress Importance to take full course of antibiotics >stress importance of treating partner too Patient Education Bed rest Aspirin Warn patient of Jarish Herxheimer reaction
Safe sex, Monogamous relationship
Antibody Absorption Test (FTA-ABS)
Latent stage Not infectious except to the fetus of the pregnant Tertiary syphilisGummas Itching, beefy red irritation, inflammation of the vaginal epithelium White, cheese-like, odorless discharge Patches of curdlike, cheesy material that adhere to the vaginal mucosa
CANDIDIA SIS Moniliasis
Candida albicans
CHLAMIDI AL INFECTIO N
Chlamydia trachomati s
Sexual contact
isolation of the organism in a tissue culture or
a. Pruritus in vagina b. Burning sensation in vagina
Nystatin vaginal suppositor y twice a day for 714 days vaginal douche of 2 tsp ordinary baking powder dissolved in 1 quart of warm water application of gentian violet to the vagina and perineum to prevent staining of undergarm ents Antibiotics: doxycyclin e and azithromyc in
1. Urge client to have sexual partner treated
serological complement fixation
c. Painful intercourse d. Pruritus of urethral infection in men e. Burning sensation during urination
TRICHOM ONIASIS
Trichomona s vaginalis
Sexual contact
Yellow green frothy vaginal discharge Burning and pruritus of vagina Dysuria, dyspareunia Usually asymptomatic in men ELISA screening test Western blot confirmato ry test CD4 T cell count (1000) Persistent fever within 1 month Chronic diarrhea Stunted growth 10 weight loss 6 minor Persistent cough Persistent genaralized lymphadenop
Metronidazol e (Flagyl) 250mg TID for 1 week.
ACQUIRED IMMUNOD EFICIENCY SYNDROM E (AIDS)
HIV
blood 90% Sexual contact 0.1 to . 5% Sharps or needle 0.1 % to .5%
1. Mononucleo side Reverse Transcriptase Inhibitors (Azidothymidi ne , Zidovudine ,Lamivudine , Retrovir) 2. NonMNRTI
2. Emphasize the importance of long term drug therapy because of the pathogens unique life cycle, which make it difficult to eliminate Do not give metronidaz ole during the first trimester of pregnancy Sitz bath Acid douches (1 tablespoon of vinegar in 1L of water) Symptomatic A abstinence and B be faithful supportive C condom D dont use drug
athy Sarcoma Pharyngeal candidiasis Recurrent herpes zoster Progressive disseminated herpes simplex
Dideoxyinosi ne (Didanosine), Dideixycytidi ne ( Zalcitabine) 3. Protease inhibitors - Saquinavir, Indanavir, -Ritonavir,Nel finavir Monotherap y: Dapsone Multi drug therapy (MDT) (Treatment approach: depends on microorganis ms in skin lesions) a. Paucibacill ary: >Rifampici n once a month >Dapsone OD (6-9 mos) b. Multibacilla ry: >Rifampici n once a month >Dapsone OD(24-30 mos) >Lampren
Leprosy Hansens disease
Mycobacter ium leprae
Prolonged intimate skin to skin contact Droplet Infection
Skin smear test Skin lesion biopsy Lepromin skin test
1. Psychologi cal aspect of care 2. S kin care: -prevent injury 3. A ctive and passive exercise to avoid contracture s 4. Health education Dapsone: may increase the number of lesion also iritis, orchitis Lamprene: may cause skin discoloratio
e OD (2430 mos) (clofazimi ne) Measles Rubeola; First disease, Little red disease Paramyxovi rus droplet Koplik spots Clinical signs & symptoms 1. Pre-eruptive: > 3 Cs: Cough, coryza, conjunctivitis 2. Eruptive: > Koplik spots > Rashes Cephalocaudal maculopapular rash 3. Posteruptive: > fine branny desquamatio n 1. Pre-eruptive Forscheimer spots (fine red spots found on soft palate) 2. Eruptive > rashes exanthem maculopapul ar (smaller than measles) ; no desquamatio n nor pigmentation > enlargement of lymph Symptomatic
n, dryness and flakiness > Complete bed rest > Adequate nutrition > Increase fluid intake > Increase vitamin C & A > Keep patient warm & dry > darken the room 1. Immunization 0.5 ml SC deltoid Precaution: fever, mild rash MMR- given at 15 months - check for allergy to eggs 2. Proper disposal of nasal secretions
German Measles Rubella, 3 day measles, Third disease
Togavirus
droplet
Chicken pox Varicella; Bulutong
Varicella Zoster virus
Airborne
Clinical
HerpesZoster (Shingles)
Varicella zoster virus
Occurs in a partially immune individual due to a previous varicella infection
Clinical
nodes: suboccipital, post. Auricular, post. Cervical 1. Pre-eruptive > fever, headache, body malaise, muscle pain 2. Eruptive phase described as vesiculopustular, more abundant in covered parts of the body > unilocular appearance of lesions 3. Post-eruptive Superficial depigmented scars rashes are clustered, follows a nerve pathway (unilateral), itchy, painful
Symptomatic antiviral (acyclovir)
> prevention of secondary infection of the skin lesions > cut fingernails short & wash hands to minimize bacterial infections > isolation of patient > Cool soda bath/ baking soda paste reduce itchiness
> Immunization Varivax 2 doses in adult, 1 month interval 1 dose in child
Symptomatic > acyclovir (anti-viral) > KMnO4 A: astringent effect B: bactericidal > analgesics are necessary for weeks or even months after blisters
> use of mask, gown, proper disposal of nasopharynge al secretions
have dried up
RABIES Hydrophobi a, Lyssa, La Rage
Rhabdoviru s
Bite, abrasion or lick on a damaged skin or mucous membrane
Brain Biopsy negri bodies Virus culture and isolation Observat ion of dog for 10 days
Invasive stagenumbness on site, flu like symptoms, marked insomnia, restless, irritable, apprehensive , with slight photosensitiv ity. Excitement stageaerophobia, hydrophobia, px fears water due to laryngospas m, difficulty in swallowing, photosensitiv ity Paralytic stageparalysis
A. Active 1. verorab : 0.50 cc/vial (IM) Site: Deltoid or Vastus lateralis 2. Purified duck embryo IM deltoid or SubQ OD for 14 days 1. Lyssavac N 2. Lyssavac plain B. Passive immunization : > Given up to 7 days after being bitten, >Deep IM at buttocks area >Single dose >Animal Serum (ERIG) equine rabies immunoglobu lin Eg. ARS (antirabies serum); HyperRAB 0.2cc/kg BW
Provid e a dim & quiet environme nt Room should be away from sub-utility rooms (area for washing: avoid sound of water) Restrai n patient even before aggressive behavior sets in Wear protective barriers
Immuniz ation of animals All animals should be caged or chained Stay away from stray animals
>Human serum (HRIG) human rabies immunoglobu lin E.g. Rabuman; Imogam 0.133 cc/Kg BW POLIOMYE LITIS Infantile paralysis, Heinemedin disease Legio Debelitans 1. Type 1 - L.D. Brunhilde 2. Type 2 - L.D. Lansing 3. Type 3- L.D. Leon 1. Fecal oral route 2. Droplets Lumbar Puncture protein content of CSF is increase: (+) Pandys test EMG Muscle Stool exam. done 10 days after infection Invasive stage or abortive stage Abdominal pain, anorexia, nausea, vomiting, diarrhea, constipationpayers patches Pre- paralytic stage Involvement of the CNS but w/out paralysis Char. by TRIPOD POSITION Haynes sign: Pokers sign: Paralytic Stage FLACCID PARALYSIS Masseter muscle trismus or lockjaw Facial musclePatient is treated symptomatic ally Bedrest Use hot compress for spasm PROM when pain and spasms are gone In case of respiratory paralysis, px is placed in mechanica l ventilator called iron lung machine. Immunization OPV or Sabin(3doses @ 6wks with 1 month interval) Salk - IM Avoid mode of transmission droplet a. Proper disposal of secretions b. Proper handling of food c. Handwashing
TETANUS Lockjaw
Clostridiu m tetani
Acquired thru wound (any kind of wound)
1. ATSantibodies -Prepare epinephrine and
Dim light, quiet environment Minimal and gentle
Immunization (DPT, Tetanus toxoid)
laceration, burn, bite, umbilical stump
risus sardonicus or sardonic grin Muscle of spineopisthotonus or arching of the back Respiratory muscledyspnea and chest heaviness Abdominal muscleabdominal rigidity(1st) Extremity musclesstiffness of extremities
corticosteroid in cases of delayed hypersensitiv ity reaction 2. ABPenicillin 3. muscle relaxant (DiazephamValium)
handling of patient Protect patient from injury Provide px comfort Always have padded tongue depressor Watch for urinary retention Wound Care: Washing with antiseptic Thin dressing Debride necrotic tissues
Clean wound immediately
MENINGITI Fungal S meningiti sCryptococ cal meningiti s Meningoc occal meningiti smeningoc oxemia or spotted feverNeisseria meningiti s
Respirator y droplet
Lumbar tap or Lumbar puncture Secure consent Fetal position during; flat on bed after Increase WBC; increase protein; decrease sugar
Clinical Manifestation s: 1. Meningococc emia - Fever, chills, N/V, malaise, headache Rashes, petechia, or blotchy purpuric lesion appear Waterhouse Friederichsen syndrome (+) shock and rashes
Antimicrobi al agent Rifampicin, Penicillin, Chloramphe nicol Steroidsantiinflamm atory agent Osmotic diuretics mannitol to reduce CSF fluid Anticonvuls ants Dilantin
(symptomatic and supportive) Promote rest and safety Monitor VS and neurologic status Fever provide TSB Convulsion s protect from injury
Proper disposing of tissues used for nasopharen geal secretions ( in plastic bags) Covering of nose and mouth when coughing and sneezing.
Blood Culture
Symptoms of meningeal irritation 1. nuchal rigidity 2. increase ICP 3. altered LOC 4. convulsive seizures Kernigs sign brudzinskis sign Opistothonus
JAPANESE ENCEPHAL ITIS Brain fever
Arbovirus
Mosquito bite (Culex)
Lumbar puncture EEG
Clinical Manifestati ons- s/s Altered LOC lethargic Fever, chills and vomiting Convulsion Signs of neurologic damage
patient is treated symptomatic ally
Typhoid Fever Enteric fever
Salmonell a typhosa
Fecal-oral route ingestion of contamina ted food and water Source of Infection: 5 Fs
Rose Spots
Blood culturedone during prodromal stage Widal Test antibody test Becomes
1. Prodromal Stage-Fever, dull headache, abdominal pain, nausea and vomiting, diarrhea or constipation. 2. Fastidial/Pyre xial Stage-
Antibiotic: Chloramphen icol 100mg/kg in 4 doses for 14 days (side effect is bone marrow depression)
(symptomatic and supportive) Promote rest and safety Monitor VS and neurologic status Fever provide TSB Convulsions protect from injury 1. Maintenanc e of fluid and electrolyte imbalance - Proper regulation of IVF - Adequate fluids
- eradicate mosquito thru DOH program
CDT Immunizati on-adults: 0.5 cc IM deltoid -children: <10 years old 0.25cc IM deltoid *6 months immunity
Feces, Finger, Food, Flies, Fomites
positive on the 2nd week Typhidot Stool culture done on the 2nd week
3 Clinical Features of Typhoid Presence of Rose Spots (abdomen and chest)only symptom specific to typhoid Ladderlike fever Splenomegal y 3.Defervescenc e Stage a. Intestinal Hemorrhages -melena, hematochezi a b. Intestinal Perforationperitonitis - Sudden, severe, abdominal pain, persistence of fever, rigid abdomen 4.Lysis/Convale scence- s/s will subside
- Assess for the sign of dehydration 2. Maintenanc e of nutrition - High calorie, low residue diet - Do not give milk which can lead to increase acidity and diarrhea 3. Isolation of patients
Vivotif- in capsule form - 3 doses: 1 hour before meal q other day - 3 years immunity Protect / Purify water supplies Proper excreta disposal Hand washing Proper preparatio n and handling of food Avoid eating fresh and uncooked vegetables and fruits in endemic areas Do not put anything in your mouth
Leptospir osis(orang e eye) Mud fever, Swamp fever, Canicola fever, Weils Disease, Swine herds Disease, IcteroHemorrhagi a
Leptospira interrogans spirochetes
Can be transmitt ed by the semen of infected animal Skin penetrati on, ingestion of infected or carcasse s of either wild or domestic animals
Dysentery
1.
Bacil
lary Dysenter yShigellosi s 2. Viole nt Dysentery - Cholera 3. Amo
Fecal oral route
Cholera: RICE WATER STOOL
BLOOD septic stage EXAMINAT high fever ION 4-7 days, >LATheadache, Leptospir N/V, a abdominal Agglutinat pain, joint ion Test pain, >LAATrespiratory Leptospir distress a Antigen- Immune or Antibody toxic stageTest with or Liver without function jaundice- 4-30 test. BUN days CREATINE o Anicteric low grade fever, meningeal manifestation (convulsion, disorientation) Icteric (Weils syndrome) jaundice, hemorrhages, hepatomegaly , renal involvement (RF) Stool Examinati onamoebiasi s Rectal Swab for cholera and shigellosis
Antibiotics: penicillin, doxycycline,T etracycline (not given to < 8 yrs old and pregnant women) ***Do not give calciumrich foods (tetracycline binds with calcium) Prophylaxisdoxy 100 mg p.o q12 x 7 days
1. Sympt omatic and supportiv e 2. Monito r urine output
Eradicate rats Avoid wading in contaminate d pool of water/ swamps
Shigellosis: Cotrimoxazole, ciprofloxacin Cholera: Cotrimoxazole, Tetracycline Amoebiasis:
Control of fever Maintenanc e of fluid and electrolyte balance Oral Rehydratio n Salt (ORS)
CDT Vaccine (Cholera/Dys entery/Typh oid) 6 months immunity given only on outbreaks. Personal hygiene -
ebic Dysentery Amoebiasi s
Metronidazol e
o NaCl, Sodium Bicarbonat e, Potassium Chloride, Glucose
Schistoso miasis Snail fever, Bilharziasis, Blood fluke
Schistoso ma japonicum , S. mansoni, S. hematobi um
Parotitis Mumps
Paramyxovi rus
penetratio n of free swimming fork-tailed cercaria, ingestion of contamina ted water Sources of infection Feces of infected person Dogs, pigs, carabao s, monkey s and wild rats tiny snail called Oncome lania quadrasi Droplet or by direct contact with saliva of infected
Stool exam look for egg of parasite, kato katz technique o Blood exam COPT (circumov al precipitin test) o ELISA
1. swimmer s itch 2. Low grade Fever, myalgia and cough 3. Dysentery like symptoms 4. Emaciatio ns from chronic disease 5. Hepatom egaly, splenomegaly, lymphadenop athy
given early at the course of disease Praziquant el (Biltricide) = 30 mg/kg BID Fuadin IM OR IV
handwashin g Environment sanitation boiling of water, protect food from flies Snail Control (Oncomelani a quadrasi) use of molluscides Environment al Sanitation proper disposal of excretion
Clinical
a. Prodromal: Headache, fever, malaise b. Acute phase:
1. Place patient on CBR until swelling subside
MMR vaccine given on 1518 months (1dose)
person
Swelling of the salivary glands leading to difficulty in swallowing and chewing; + earache peaks at two days and stays up to 10 days
DENGUE Dandy Fever, Break bone fever
ArthropodBorne virus (arbovirus) belonging to the family Flaviviridae 4 serotypes (DENV1, 2, 3, 4)
Vectors: Aedes aegypti Aedes albopict us- tiger mosquit o Culex fatigans
1. Grade I - High grade fever (3-5 days) - Headache, peri-orbital pain - Joint & bone pain - Abdominal pain - Nausea & vomiting - Petechial formation Hermans sign generalized flushing of
Symtomatic and supportive 1. Oral fluids and electrolyte 2. Antipyreti cs (dont use aspirin) 3. Platelet transfusio n 4. Convulsio ns Dilantin
2. Wear fitted supporter to prevent pulling gravity in testes 3. Soft, bland diet 4. Hot or cold application over parotid gland to relieve pain 5. Patient should be excluded from school/work for 9 days after onset Watch for bleeding: Nosebleed cold compress over forehead Melena cold compress over stomach area, avoid eating dark colored foods
Proper covering of mouth and nose when coughing and sneezing
DOH CLEAN Program C hemically treated mosquito nets L arvae eating fish E nvironmental sanitation (4pm habit) A ntimosquito soaps (basil, citronel) N atural mosquito repellants (neem tree,
MALARIA Ague, King of Tropical Diseases
Plasmodiu m
1. Malarial Smear 2. Quantitati ve Buffy Coat (QBC)rapid test for malaria
the skin 2. Grade II signs & symptoms of grade I + bleeding - Epistaxis - GI bleeding - Gum bleeding 3. Grade III grade II + circulatory failure - Cold, clammy skin - Altered VS decreased BP, rapid, weak pulse, increased RR 4. Grade IV grade III + hypovolemic shock 1. Cold stage - Chilling manifestation s (10-15 mins) nursing responsibility : provide warmth to patient 2. Hot stage Characterized by fever, headache, abdominal pain &
Gingival bleeding offer ice chips, use soft bristle toothbrus h Hematem esis - NPO Observe for signs of shock
eucalyptus, oregano)
Anti-malarial agents -Chloroquine (drug of Choice) -Quinineneurologic toxicity, muscular twitching, delirium, convulsion -Primaquine -Fansidar
Keep patient comfortabl e with dry, warm clothes, replace fluid loss. Monitor V/S Diet high calories, vitamins and minerals Fluid and
1. Advise malaria chemoprophy laxis when travelling to malaria endemic areas 2. Limit dusk to dawn exposure, 3. wear protective clothing 4. sleep under mosquito nets
vomiting - Lasts for 4-6 hours Nursing responsibility : lower body temperature 3. Diaphoretic stage Excessive sweating/ feeling of weakness due to the past stages px underwent
electrolyte 5. use topical s balance repellents
Potrebbero piacerti anche
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- FEU NRMF Admission FormDocumento2 pagineFEU NRMF Admission FormMea Faye DinoNessuna valutazione finora
- Maternal and Child Health NursingDocumento2 pagineMaternal and Child Health NursingErika DellosaNessuna valutazione finora
- Pathophysiology of ALL DiagramDocumento3 paginePathophysiology of ALL DiagramErika DellosaNessuna valutazione finora
- Falls in ElderlyDocumento8 pagineFalls in ElderlyErika DellosaNessuna valutazione finora
- Professional Regulatory Board of Nursing: The "Commision"Documento15 pagineProfessional Regulatory Board of Nursing: The "Commision"Erika DellosaNessuna valutazione finora
- Professional Regulatory Board of Nursing: The "Commision"Documento15 pagineProfessional Regulatory Board of Nursing: The "Commision"Erika DellosaNessuna valutazione finora
- CA ReportDocumento20 pagineCA ReportErika DellosaNessuna valutazione finora
- Med SchoolsDocumento2 pagineMed SchoolsErika DellosaNessuna valutazione finora
- Renal DisordersDocumento24 pagineRenal DisordersErika Dellosa100% (2)
- PsychDocumento23 paginePsychErika DellosaNessuna valutazione finora
- Orem Nursing TheoryDocumento2 pagineOrem Nursing TheoryErika DellosaNessuna valutazione finora
- SYPHILIS Annual TechDocumento41 pagineSYPHILIS Annual TechkimotosanNessuna valutazione finora
- Clinical Pathology and Medical Laboratory: Indonesian Journal ofDocumento6 pagineClinical Pathology and Medical Laboratory: Indonesian Journal ofIma PratiwiNessuna valutazione finora
- Dental Management of The Patient With HIVAIDS 2002Documento6 pagineDental Management of The Patient With HIVAIDS 2002drkameshNessuna valutazione finora
- John CarnevaleDocumento8 pagineJohn Carnevaleapi-209693106Nessuna valutazione finora
- Vector ControlDocumento11 pagineVector ControlMayuri Vohra100% (1)
- The National Health SituationDocumento167 pagineThe National Health SituationCes AriaNessuna valutazione finora
- Imci Chart Booklet Up DateDocumento6 pagineImci Chart Booklet Up DateifyejinkeonyeNessuna valutazione finora
- Syllabus Hiv AidsDocumento3 pagineSyllabus Hiv Aidsniketut alit arminiNessuna valutazione finora
- Antifungal AntibioticsDocumento16 pagineAntifungal AntibioticsLyadelou FortuNessuna valutazione finora
- Standard Operating Procedures Manual For The Management of TheDocumento114 pagineStandard Operating Procedures Manual For The Management of TheHarry GaiyaNessuna valutazione finora
- An Accident With A Gates Glidden Drill in Endodontic PracticeDocumento2 pagineAn Accident With A Gates Glidden Drill in Endodontic PracticeahujasurajNessuna valutazione finora
- Dermatology Written Exam 2007Documento6 pagineDermatology Written Exam 2007Abdullah Matar BadranNessuna valutazione finora
- Bisexual Invisibility:: Impacts and RecommendationsDocumento47 pagineBisexual Invisibility:: Impacts and RecommendationsprideinutahNessuna valutazione finora
- Family Life, Reproductive Health, and Population Education:: Information Series On School HealthDocumento90 pagineFamily Life, Reproductive Health, and Population Education:: Information Series On School HealthChris McIverNessuna valutazione finora
- Cambridge A As Level Biology Mark Scheme 2 Winter 2007Documento5 pagineCambridge A As Level Biology Mark Scheme 2 Winter 2007rasNessuna valutazione finora
- Bpjs NovemberDocumento219 pagineBpjs NovemberAnonymous KSvPjR2DNessuna valutazione finora
- Plot 126, Solent Avenue, Tel: (+256) 771256301 Mbuya, Kampala, Uganda P. O. Box 8379Documento7 paginePlot 126, Solent Avenue, Tel: (+256) 771256301 Mbuya, Kampala, Uganda P. O. Box 8379George LumiisaNessuna valutazione finora
- Pictures of Six Sexual Transmitted InfectionDocumento6 paginePictures of Six Sexual Transmitted InfectionDavia ColmanNessuna valutazione finora
- Health Is Very Important in Our Daily LivesDocumento2 pagineHealth Is Very Important in Our Daily LivesFit RINessuna valutazione finora
- The Miracle of Q RAK CultivationDocumento308 pagineThe Miracle of Q RAK CultivationRafyta100% (4)
- Internship Plan Surakshya Karki University of North Carolina GreensboroDocumento13 pagineInternship Plan Surakshya Karki University of North Carolina Greensboroapi-310446292Nessuna valutazione finora
- HIV Related Policies and Guidelines Issuances: Training On HIV Counseling and Testing and Facility-Based HIV ScreeningDocumento77 pagineHIV Related Policies and Guidelines Issuances: Training On HIV Counseling and Testing and Facility-Based HIV ScreeningJovania B.Nessuna valutazione finora
- NSTP Project ProposalDocumento3 pagineNSTP Project ProposalIris FuedanNessuna valutazione finora
- NYCAHN Is Now VOCAL New York!Documento3 pagineNYCAHN Is Now VOCAL New York!VOCAL-NYNessuna valutazione finora
- An Approach To Fever Throught Boger BoenninghausenDocumento10 pagineAn Approach To Fever Throught Boger BoenninghausenHomoeopathic Pulse100% (2)
- Pregestational ConditionsDocumento46 paginePregestational ConditionsSheryl M. Ablao50% (2)
- Chronic Viral HepatitisDocumento66 pagineChronic Viral HepatitisSuresh KadliNessuna valutazione finora
- Annual Report 2009 10Documento189 pagineAnnual Report 2009 10tkhalifaNessuna valutazione finora
- History OsteomielitisDocumento4 pagineHistory OsteomielitisMuhammad Hamka Maha PutraNessuna valutazione finora
- Ppg-Gdch-Nur-53 Abbreviations and SymbolsDocumento13 paginePpg-Gdch-Nur-53 Abbreviations and SymbolsKenny JosefNessuna valutazione finora