Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
NIH Public Access: Author Manuscript
Caricato da
HutsDMDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
NIH Public Access: Author Manuscript
Caricato da
HutsDMCopyright:
Formati disponibili
NIH Public Access
Author Manuscript
Brain Res. Author manuscript; available in PMC 2009 January 2.
Published in final edited form as: Brain Res. 2008 January 2; 1187: 4251.
NIH-PA Author Manuscript NIH-PA Author Manuscript NIH-PA Author Manuscript
Compatibility of human fetal neural stem cells with hydrogel biomaterials in vitro
Jason R. Thonhoff, Dianne I. Lou, Paivi M. Jordan, Xu Zhao, and Ping Wu* Department of Neuroscience and Cell Biology, University of Texas Medical Branch, Galveston, Texas 77555, USA
Abstract
Stroke and spinal cord or brain injury often result in cavity formation. Stem cell transplantation in combination with tissue engineering has the potential to fill such a cavity and replace lost neurons. Several hydrogels containing unique features particularly suitable for the delicate nervous system were tested by determining whether these materials were compatible with fetal human neural stem cells (hNSCs) in terms of toxicity and ability to support stem cell differentiation in vitro. The hydrogels examined were pluronic F127 (PF127), Matrigel and PuraMatrix. We found that PF127, in a gelated (30%) form, was toxic to hNSCs, and Matrigel, in a gelated (1-50%) form, prevented hNSCs normal capacity for neuronal differentiation. In contrast, PuraMatrix was the most optimal hydrogel for hNSCs, since it showed low toxicity when gelated (0.25%) and retained several crucial properties of hNSCs, including migration and neuronal differentiation. Further optimization and characterization of PuraMatrix is warranted to explore its full potential in assisting neural regeneration in vivo.
Keywords Stem cell; hydrogel; biocompatibility; scaffold; tissue engineering; neural differentiation
1. Introduction
An impediment to neural regeneration after injury is that a cavity often forms that lacks any structure to aid cellular replacement and differentiation. Thus, potential regeneration of neurons after transplantation of stem cells would undoubtedly be aided by being combined with appropriate biomaterials. The properties of an ideal biomaterial would include that it is biodegradable, non-toxic, provides a three-dimensional scaffold for developing tissue, can be vascularized due to its porous structure and elicits minimal immune responses (Holmes et al., 2000). Previously, rodent stem/progenitor cells have been seeded on scaffolds that meet some of these criteria and applied in cell-based therapies in animal models of neurotrauma (Vacanti et al., 2001; Lavik et al., 2002; Tate et al., 2002; Teng et al., 2002; Park et al., 2002; Bhang et al., 2007). However, hydrogel polymer scaffolds possess a further characteristic that may be advantageous in neural grafting in that they can be injected as a fluid into spinal cord or brain cavities and then polymerized in situ, thus conforming to the shape of the cavity caused by the
*Corresponding Author: Ping Wu, M.D., Ph.D., Department of Neuroscience and Cell Biology, University of Texas Medical Branch, Galveston, TX 77555-0620, Phone: 409-772-6414, Fax: 409-747-2187, Email: piwu@utmb.edu. Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Thonhoff et al.
Page 2
injury. The present study focuses on three hydrogels; pluronic F127 (PF127), Matrigel and PuraMatrix.
NIH-PA Author Manuscript NIH-PA Author Manuscript NIH-PA Author Manuscript 2. Results
PF127 is a nonionic surfactant composed of a block copolymer of propylene oxide and ethylene oxide. It gels at room temperature and has mostly been used in controlled-release drug delivery (Barichello et al., 1999; Desai and Blanchard, 2000; El Kamel, 2002; Wenzel et al., 2002). However, it has previously been applied as part of a scaffold for rat neural progenitor cells in a model of neurotrauma (Vacanti et al., 2001) and as a construct to support the growth and differentiation of lung progenitor cells (Cortiella et al., 2006). Matrigel is composed of basal membrane extract derived from Engelbreth-Holm-Swarm mouse sarcoma cells. It solidifies at room temperature forming a hydrogel. The extracellular matrix components in this hydrogel include laminin, collagen IV, entactin, nidogen and heparan sulfate proteoglycans. Growth factors such as TGF-, basic fibroblast growth factor, insulin-like growth factor-1 and tissue plasminogen activator are also present (Novikova et al., 2003; Kleinman and Martin, 2005). Matrigel has previously been used in neuronal culture and has been shown to stimulate neurite outgrowth in vitro (Tisay and Key, 1999; Novikova et al., 2006). PuraMatrix is a synthetic peptide hydrogel composed of ionic self-complementary oligopeptides similar to the EAK16 tandem repeats found in the yeast protein, zuotin. It is a 16-mer peptide with a repeating sequence of arginine, alanine, aspartate and alanine (RADARADARADARADA or RAD16) and has a composition of more than 99% water. The amphiphilic nature of PuraMatrix gives rise to the spontaneous assembly of a water-soluble -sheet structure in the presence of monovalent cations (Zhang et al., 1993; Zhang et al., 1995). This hydrogel has been shown to support cell attachment and proliferation (Zhang et al., 1995), formation of neurite outgrowth and active synapses (Holmes et al., 2000), and cell entrapment (Semino et al., 2004) and differentiation (Semino et al., 2003). None of these hydrogels have been assessed for biocompatibility with human fetal neural stem cells (hNSCs), a type of stem cell with self-renewing and multipotential differentiation properties as well as an origin most suitable for human transplantation. These cells proliferate in vitro in neurospheres, which consist of a heterogeneous population of neural stem cells and neural progenitors (Suslov et al., 2002). We have previously shown that mitogen-expanded and primed (Wu et al., 2002; Tarasenko et al., 2004) hNSCs become cholinergic motoneurons when grafted into acutely or chronically injured rat spinal cords (Gao et al., 2005; Tarasenko et al., 2007). However, grafted hNSCs showed limited survival rates and migrational capabilities within the injured cavity indicating the need for a scaffold support. In this study, we screened several scaffolding biomaterials and determined the optimal hydrogel based on its support of hNSC survival, differentiation and migration in vitro.
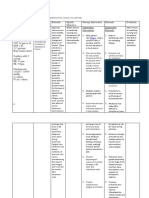
2.1. Survival and morphological characteristics of primed human neural stem cells after 2 days differentiation beneath hydrogels Cell survival is one of the critical parameters to determine whether a given material is biocompatible and suitable for hNSC tissue engineering. Therefore, we first assessed the survival of primed hNSCs through both morphological analyses and measurements of overall activity of mitochondrial dehydrogenases in live cells. After priming, hNSCs were exposed to hydrogels at different concentrations: PF127 (10-30%), Matrigel (1-50%) and PuraMatrix (0.25-1%).
Brain Res. Author manuscript; available in PMC 2009 January 2.
Thonhoff et al.
Page 3
Primed and differentiated hNSCs without hydrogel treatment showed many presumptive neurons based on morphology that appeared bright in phase-contrast microscopy and emitted processes (Fig. 1a). Further immunostaining studies confirmed their neuronal phenotype (Fig. 3). Similarly, 10% PF127 supported many phase-bright presumptive neurons (Fig. 1b) whereas more cells with a presumptive glial morphology were present in 20% PF127 (Fig. 1c). The presumptive glial cells exhibited large cell bodies and hypertrophied nuclei. 30% PF127 was toxic as fewer cells and more cellular debris were observed (Fig. 1d). A mix of presumptive neurons and glia were seen in 1% Matrigel (Fig. 1e). As the concentration of Matrigel increased, the number of presumptive glial cells increased (Fig. 1f-g). Little cellular debris was observed indicating that hNSCs survived well in Matrigel. A mix of presumptive neurons and glia were also present in 0.25% and 0.5% PuraMatrix (Fig. 1h-i). However, the concentrated PuraMatrix (1%) seemed to exert a toxic effect on the hNSCs as the cells seemed shrunken and degenerated (Fig. 1j). Cytotoxicity of these hydrogels was determined quantitatively using the WST-1 assay to evaluate mitochondrial enzymatic activities in viable cells. The viability of hNSCs decreased steadily as the concentration of PF127 and PuraMatrix increased. Surprisingly, however, Matrigel significantly decreased the viability of hNSCs at a 10% concentration (Fig. 2). 2.2. Differentiation capacity of primed human neural stem cells beneath Matrigel and PuraMatrix Another parameter of an optimal hydrogel is whether the material allows hNSCs to retain their natural differentiation capacity into both neurons and glial cells. To test the differentiation capacity, hNSCs were primed and allowed to differentiate in B27 alone as a control or in contact with 20% Matrigel or 0.25% PuraMatrix. The particular concentrations of Matrigel and PuraMatrix were selected based on their gelation capacity to support hNSCs after potential transplantation into the injured brain or spinal cord. PF127 was eliminated from this study, since it was too toxic to hNSCs at concentrations necessary for gelation. Differentiation of primed hNSCs in B27 medium, without hydrogel, showed a mix of both Tuj1+ neuronal cells (17.2 5.2%) and GFAP+ astroglial cells (27.6 9.5%) (Fig. 3a-d). Primed hNSCs differentiated in the presence of 20% Matrigel for 7 days showed primarily GFAP+ astroglial cells (95.3 3.6%) (Fig. 3e-h) with larger nuclei and cell bodies. Very few Tuj1+ neurons (4.7 3.6%) were present. The normal differentiation pattern seen in primed hNSCs (Fig. 3a-d) was retained in primed hNSCs that were differentiated in the presence of 0.25% PuraMatrix for 7 days (Tuj1: 17.3 4.2% and GFAP: 25.8 5.3%) (Fig. 3i-l). 2.3. Migration patterns and differentiation capacity of hNSC neurospheres embedded within PuraMatrix
NIH-PA Author Manuscript NIH-PA Author Manuscript NIH-PA Author Manuscript
Since PuraMatrix appeared to be the most optimal among the three hydrogels that were tested in terms of supporting the survival and differentiation capacity of hNSCs, we then asked whether hNSCs retained their migration capacity within PuraMatrix. We chose neurospheres rather than primed cells to address the migration issue, since the extensive migration of hNSCs that occurs during priming could prevent a full assessment of the cells migration capacity in PuraMatrix. Spheres, 4 days post-passage, were embedded within 0.25% PuraMatrix and allowed to differentiate for 7 days. Images were taken using a light microscope at 3.5 and 7 days to determine the extent of hNSC migration. NIS-Elements imaging software (Nikon Instruments, Inc., Melville, NY) was used to measure the migration distance of the cell that traveled furthest from the edge of each control sphere and sphere embedded within the PuraMatrix hydrogel. Some hNSCs were seen migrating from spheres 3.5 days post-embedding with an average furthest distance of 108.8 m 32.3 m (n=9) (Fig. 4c). After 7 days, a more extensive network of migrating cells was observed with an average furthest distance of 245.6 m 49.5 m (n=13) (Fig. 4d), although the distance of cell migration was much less than that
Brain Res. Author manuscript; available in PMC 2009 January 2.
Thonhoff et al.
Page 4
observed in medium without a hydrogel after only 3.5 days (670.8 m 17.5 m, n=8) (Fig. 4a). After 7 days in medium alone (Fig. 4b), a much higher proportion of migrating cells was observed from each sphere and many of these cells migrated further than the field of view at the lowest magnification in just a few days. We then asked whether hNSC neurospheres without priming retained their neuronal differentiation capacity in PuraMatrix, and compared the cell phenotypes to undifferentiated neurospheres. Immunostaining of sectioned spheres, which were cultured for 5 days in growth media and not seeded in PuraMatrix, showed heterogeneous populations with GFAP+ cells distributed evenly throughout the spheres and some Tuj1+ cells mainly in the center of spheres (Fig. 5a-e). Interestingly, spheres that were seeded in PuraMatrix and differentiated for 7 days in B27 revealed a concentration of GFAP+ cells on the outside regions of the spheres and an even distribution of Tuj1+ cells throughout (Fig. 5f-j).
NIH-PA Author Manuscript NIH-PA Author Manuscript NIH-PA Author Manuscript
3. Discussion
The major thesis of the present study was to determine an optimal hydrogel that was biocompatible with hNSCs and thus, could potentially be used in combination with stem cells to facilitate neural regeneration after stroke or traumatic injury. The data collected from the in vitro experiments revealed that PuraMatrix hydrogel was most compatible with hNSCs as it supported hNSC survival, differentiation and migration. Previously, poly(-hydroxy acid) polymers including poly(glycolic acid) (PGA), poly(lactic acid) (PLA) and their copolymers (PLGA) have been seeded with rodent stem/progenitor cells (Vacanti et al., 2001; Teng et al., 2002; Bhang et al., 2007; Gelain et al., 2007). It was unknown, though, whether these types of polymers were compatible with hNSCs. In an initial trial experiment, we found that hNSCs seeded and primed on PGA attached to and migrated along the PGA fibers (unpublished observation). However, PGA seemed to be particularly rigid and thus not suitable for transplantation into neural tissue as the rigid PGA fibers would need to be pressed, rather than injected into the cavity resulting from most neural injuries. An ideal biomaterial for neural transplantation would have the ability to be mixed with stem cells and injected into the cavity in a fluid form. Once in vivo, the biomaterial would solidify forming a three-dimensional matrix, in which the stem cells could migrate and form connections across the cavity. PF127, Matrigel and PuraMatrix hydrogels possessed this important characteristic. The biocompatibilities of PuraMatrix and Matrigel with rodent neural precursor cells were recently compared to other commonly used scaffolds including poly(-hydroxy acid) polymers (Gelain et al., 2007). Although some differences were observed in cell viability and differentiation capacity, the compatibilities of the hydrogel materials and other scaffolds were comparable. However, in our study, PF127 showed some toxicity to hNSCs at concentrations needed for in vivo gelation. Also, although more viable cells were found in the case of 10% PF127 hydrogel as compared to the control, this increase was not significant and may be attributed to cell plating variation. Furthermore, cell viability in 10% Matrigel was significantly decreased compared to the control whereas cells in 50% Matrigel had a much higher viability. This phenomenon observed under conditions of increasing concentrations of Matrigel likely involves a complex dynamic between cell toxicity (or inhibition of cell proliferation) and growth factor stimulation. The fact that hNSCs cultured with Matrigel become mainly astrocytes indicates a toxic effect of Matrigel on hNSC-derived neurons. This initial phase of neuronal death may then be followed by the proliferation of astrocytes that is stimulated by growth factors in the increasing concentration of Matrigel. Alternatively, Matrigel, a mixed basement membrane extract from mouse sarcoma cells containing various growth factors and molecules in addition to collagen and laminin, may inhibit the neuronal differentiation of
Brain Res. Author manuscript; available in PMC 2009 January 2.
Thonhoff et al.
Page 5
hNSCs. In any case, this observation is inconsistent with previous reports that showed neuronal differentiation and migration of neural stem/progenitor cells when placed on top of a surface coated with Matrigel (Katakowski et al., 2005; Flanagan et al., 2006). An apparent difference is that we placed hNSCs underneath the Matrigel. However, toxicity due to insufficient nutrient access is unlikely as both Matrigel and PuraMatrix at the concentrations we used have adequate pore sizes (approximately 2 m in 50% Matrigel and 0.05-0.2 m in 0.5% PuraMatrix) to allow medium infusion (Semino et al., 2003; Zaman et al., 2006). Whether toxicity in some conditions was due to the release of harmful or acidic byproducts during degradation is yet to be determined. Taken as a whole, Matrigel and PuraMatrix at gelating concentrations showed a lower toxicity than PF127 to hNSCs. Besides low cytotoxicity, an ideal biomaterial scaffold should allow the full differentiation capacity of hNSCs. Along this line, primed hNSCs mixed with Matrigel and PuraMatrix revealed different differentiation patterns. Almost every cell in Matrigel stained positively for GFAP, indicating either an astroglial or undifferentiated phenotype. In contrast, PuraMatrix supported both astroglial and neuronal differentiation in a similar pattern as the primed hNSC control group without a hydrogel. Interestingly, as the concentration of Matrigel was decreased, more Tuj1+ staining was observed, but the vast majority of cells were still GFAP+ (unpublished observation). This indicated that one or more components incorporated into the Matrigel prevented neuronal differentiation or survival. Another observation was that hNSCs mixed with Matrigel had larger nuclei. Hypertrophy of astrocytic nuclei has previously been described in activated astrocytes (Albrecht et al., 2002). Since Matrigel incorporates several growth factors and other extracellular matrix components, it is perceivable that one or more of these factors may be inducing the morphological change in the hNSC-derived astroglia. Our observation seems contradictory to the previous reports of a supporting role of Matrigel for neuronal differentiation and migration of human and rodent neural progenitor cells (Katakowski et al., 2005; Flanagan et al., 2006). The discrepancy may be due to the different concentrations of Matrigel used in these studies as we observed the most inhibition on neuronal formation from hNSCs when 50% Matrigel was used (total protein concentration of 10 mg/ ml), which is 60 and 18 times more concentrated than what were used in the previous neuronal differentiation (Flanagan, et al., 2006) and migration (Katakowski, et al., 2005) studies, respectively. While it is important to test markers for all three lineages when evaluating the differentiation capacity of hNSCs, oligodendrocytes expressing the O4 marker are undetectable in vitro until approximately 2-3 weeks post-differentiation using the priming and differentiation procedure described in these experiments (unpublished observation). Although the slow biodegradation of hydrogels is a necessity after transplantation in vivo, just a 7-day differentiation was chosen for this in vitro experiment to minimize hydrogel degradation due to a diluting effect caused by medium changes. A short-term differentiation allowed for the evaluation of differentiation during the critical period in which hNSCs were in direct contact with the hydrogel materials. Consequently, immunostaining for oligodendrocytes may be performed post-transplantation in vivo. Previously, we have shown that primed hNSCs have the capacity to differentiate into oligodendrocytes at least 3 months after transplantation (Tarasenko et al., 2007). Furthermore, the self-renewal property of hNSCs was not determined in this short-term in vitro study. With the purpose of replacing functional neural cells (neurons and glia), further in vivo studies are warranted to confirm that hNSCs mixed with PuraMatrix hydrogel do not form tumors after long-term transplantation. For transplantation, we routinely prime cells on a poly-D-lysine- and laminin-coated surface first and then collect cells for transplantation. This allows us to obtain neurons when the primed hNSCs are grafted into non-neurogenic areas in adult rats (Wu et al., 2002; Tarasenko et al., 2007). Collecting primed cells and embedding them within the hydrogels would most
NIH-PA Author Manuscript NIH-PA Author Manuscript NIH-PA Author Manuscript
Brain Res. Author manuscript; available in PMC 2009 January 2.
Thonhoff et al.
Page 6
appropriately mimic the environment that the cells would experience post-transplantation. However, when this particular experimental paradigm was attempted, too many cells were lost during the immunostaining process. Thus, in order to mimic the procedure of priming and grafting hNSCs to some extent while maintaining the capability to test differentiation through immunostaining, we added the hydrogels on top of the primed hNSCs, which were attached to poly-D-lysine- and laminin-coated glass coverslips. This method still allowed the hydrogels to interact with hNSCs during the differentiation process and mimicked the in vivo situation in that nutrients had to penetrate through the hydrogels to reach hNSCs. However, a limitation of this in vitro model was that the hNSCs were receiving cues from the coated coverslips as well as the hydrogels rather than solely the hydrogels. The effect of the extra cues in vitro compared to the condition post-transplantation is yet to be determined. Since a low concentration of PuraMatrix hydrogel showed sufficient gelling capability, low toxicity and supported a normal differentiation pattern, we next sought to determine the migration capability of hNSCs embedded as spheres within PuraMatrix. We found that hNSCs were able to migrate from spheres in gelated PuraMatrix. In vitro, hydrogels would be expected to physically impede migration to some extent (e.g., physically block the extension of neurites of a cell) when compared to controls without hydrogels. However, hydrogels may enhance migration capability across the injured cavity in vivo due to their ability to provide a threedimensional matrix scaffold suitable for cellular adhesion, migration and support. This migration capability of hNSCs through a PuraMatrix-formed scaffold will be important in terms of enhancing cell potentials to fill the cavity resulting from brain or spinal cord injuries.
NIH-PA Author Manuscript NIH-PA Author Manuscript NIH-PA Author Manuscript
4. Conclusion
The ultimate goal of the present study was to determine an optimal hydrogel that can form scaffolding for hNSC differentiation when placed in cavities in the damaged brain or spinal cord. Such a hydrogel should show low toxicity to hNSCs and the scaffold should permit hNSC adhesion, migration and differentiation. Among the three hydrogels tested in this study, PuraMatrix was most suitable for hNSC transplantation for the following reasons: 1) PuraMatrix showed low toxicity and suitable gelling capability at a low concentration, 2) Unlike PF127 and Matrigel, PuraMatrix did not require freezing temperatures to maintain a fluid form, but rather gelled upon salt incorporation, 3) PuraMatrix allowed a similar differentiation pattern to hNSCs primed in the absence of a hydrogel material and 4) PuraMatrix allowed hNSC migration.
5. Experimental Procedures
5.1. Hydrogels Hydrogels tested were pluronic F127 (PF127) (Sigma, St. Louis, MO), Matrigel (High Concentration, total protein concentrations of 18-22 mg/ml, BD Biosciences, Bedford, MA) and PuraMatrix (1% w/v amino acids, BD Biosciences). 5.2. Cell Culture Human fetal NSCs, line K048, were isolated from an 8-week fetal forebrain (Svendsen et al., 1998). Cells were cultured as neurospheres and passaged every 1011 days according to our previous description (Tarasenko et al., 2004). Growth media contained a basic medium supplemented with 20 ng/ml recombinant human epidermal growth factor (EGF) (R&D Systems, Minneapolis, MN), 20 ng/ml recombinant human basic fibroblast growth factor (bFGF) (R&D Systems), 5 g/ml heparin (Sigma), and 10 ng/ml recombinant human leukemia inhibitory factor (LIF) (Chemicon, Temecula, CA). The basic medium is serum-free defined medium containing DMEM (high glucose, L-glutamine)/Hams F12 (3:1) (Invitrogen/Gibco,
Brain Res. Author manuscript; available in PMC 2009 January 2.
Thonhoff et al.
Page 7
Grand Island, NY), 15 mM HEPES (Sigma), 1.5% D-glucose (Sigma), 67 I.U./ml/67 g/ml penicillin/streptomycin (Cellgro, Herndon, VA), 25 g/ml bovine insulin (Sigma), 100 g/ml human transferrin (Sigma), 100 M putrescine (Sigma), 20 nM progesterone (Sigma), 30 nM sodium selenite (Sigma) and 2 mM L-glutamine (Sigma). Cells were incubated at 37C with 8.5% CO2 to maintain pH 7.4-7.5. 5.3. Cell priming and differentiation Priming was performed by plating hNSCs (passage # 15-32) either in 96-well plates for the WST-1 assay or onto German glass coverslips (Carolina Biological Supply, Burlington, NC) in 24-well plates for immunostaining. The plates and coverslips were pre-coated with 0.01% poly-D-lysine (PDL) (Sigma) in calcium and magnesium free Dulbeccos phosphate-buffered saline (dPBS) (Cellgro) for at least 1 hr at 37C and then 0.5 g/cm2 of laminin (LMN) (Invitrogen/Gibco) in dPBS overnight at 37C. Spheres, 3-4 days post-passage, were plated onto PDL/LMN-coated areas at 1 104 cells/0.28 cm2 for the WST-1 assay or 2 105 cells/ 1.8 cm2 for immunostaining in the basic medium supplemented with 10 ng/ml bFGF, 2.5 g/ ml heparin and 1g/ml LMN for 5 days. Half of the medium was changed after 2 days. After 5 days in priming medium, 80% of the medium was changed to a B27 medium containing DMEM/Hams F12 (3:1), 15 mM HEPES, 1.5% D-glucose, 67 I.U./ml/67 g/ml penicillin/ streptomycin and B27 (Invitrogen/GIBCO) to allow for differentiation. When cells were mixed with PF127 or Matrigel, the hydrogels were diluted with B27 medium to the appropriate concentration and then added on top of the primed hNSCs after the priming medium was removed. After solidification of these hydrogels, additional B27 medium was added to avoid cellular desiccation. PuraMatrix was first diluted to the appropriate concentration with 10% sucrose and then added on top of the primed hNSCs after removal of the priming medium. B27 medium was immediately added to initiate solidification of the PuraMatrix and to avoid cellular desiccation. Cells in B27 medium were maintained at 37C with 5% CO2 to maintain pH 7.4-7.5. When cells were allowed to differentiate longer than 2 days, half of the B27 medium was changed every 3-4 days. 5.4. WST-1 assay Cell viability was assessed using WST-1 (Roche, Indianapolis, IN). Mitochondrial dehydrogenases in live cells cleave WST-1, a tetrazolium salt, into a colorimetric product, formazan, which was assayed to determine the amount of viable cells. Spheres were plated in a 96-well plate at approximately 1 104 cells/0.28 cm2 and primed for 5 days. Priming medium was then removed and PF127 (10, 20, 30%), Matrigel (1, 10, 50%) and PuraMatrix (0.25, 0.5 and 1%) (n=7/group) were added on top of the primed hNSCs for 2 days. Another group of primed hNSCs was changed to just B27 medium for 2 days to serve as a priming control. After 2 days, the WST-1 reagent was incubated at a dilution of 1:10 for 1.5 hrs. The absorbance of the formazan produced by the metabolically active cells in each sample was measured at a wavelength of 450 nm with a 630 nm reference using an ELx800uv Universal Microplate Reader (Biotek Instruments, Inc., Winooski, VT). Absorbance readings were normalized against control wells with medium alone. A one-way ANOVA and Dunnett multiplecomparisons test was used to compare each hydrogel group to the priming control group. A p value less than 0.05 was considered statistically significant. Data were expressed as means S.E.M. Statistical analyses were done using GraphPad Prism Version 4 software (GraphPad Software, Inc., San Diego, CA). 5.5. Immunofluorescent staining Four-day spheres that were allowed to differentiate in PuraMatrix for 7 days and 5-day spheres were embedded in Optical Cutting Temperature (O.C.T.) medium (Tissue-Tek, Tokyo, Japan) and sectioned on a Leica CM1900 cryostat (Meyer Instruments, Houston, TX) into 15 m
NIH-PA Author Manuscript NIH-PA Author Manuscript NIH-PA Author Manuscript
Brain Res. Author manuscript; available in PMC 2009 January 2.
Thonhoff et al.
Page 8
sections. These sections along with cells that were primed and then differentiated in Matrigel, PuraMatrix or B27 medium alone for 7 days were fixed for 20 min with 4% paraformaldehyde in phosphate-buffered saline (PBS) at room temperature and rinsed three times with 0.1 M PBS pH 7.4. Cells were then permeablized for 1 hr at room temperature with 0.25% Triton X-100 (Sigma) and treated with 0.3% bovine serum albumin (BSA) (Sigma) with 5% normal goat serum (NGS) in Tris-buffered saline (TBS) pH 7.4 to block nonspecific bindings. Primary antibodies were diluted in 0.1% Triton X-0.3% BSA/TBS to the following working concentrations: neuronal class III -tubulin (TuJ1) 1:5,000 (Babco, Berkeley, CA) and glial fibrillary acidic protein (GFAP) 1:1,000 (Chemicon). Cells were incubated with primary antibodies overnight at 4C and rinsed with TBS prior to the addition of the secondary antibody. Alexafluor 488-conjugated secondary goat anti-mouse and 568-conjugated goat anti-rabbit antibodies (Molecular Probes, Eugene, OR) were both diluted 1:300 in 0.1% Triton X-0.3% BSA/TBS and added to cells for 3 hrs at room temperature in the dark. Cells were then washed with TBS and cell nuclei were counterstained with 1 g/ml DAPI (Sigma) in TBS for 5 min at room temperature in the dark. Glass coverslips with cells were mounted onto glass slides and microscope coverglass (Fisher Scientific, Pittsburgh, PA) was mounted onto sectioned neurospheres with Fluoromount-G (Fisher, Fair Lawn, NJ). Fluorescent images were taken on a Nikon Eclipse 80i epifluorescent microscope.
Acknowledgements The authors thank the contributions from Drs. Joan Nichols and Joaquin Cortiella for critical scientific discussion and providing PGA and PF127. The authors also thank the technical assistance from Tiffany J. Dunn and the critical review by Dr. Richard Coggeshall. Sponsorship: Supported by the National Institute of Neurological Disorders and Stroke (NS046025), the Coalition for Brain Injury Research, the TIRR Foundation and the John S. Dunn Research Foundation.
NIH-PA Author Manuscript NIH-PA Author Manuscript NIH-PA Author Manuscript
References
Albrecht PJ, Dahl JP, Stoltzfus OK, Levenson R, Levison SW. Ciliary neurotrophic factor activates spinal cord astrocytes, stimulating their production and release of fibroblast growth factor-2, to increase motor neuron survival. Exp Neurol 2002;173:4662. [PubMed: 11771938] Barichello JM, Morishita M, Takayama K, Nagai T. Absorption of insulin from pluronic F-127 gels following subcutaneous administration in rats. Int J Pharm 1999;184:189198. [PubMed: 10387948] Bhang SH, Lim JS, Choi CY, Kwon YK, Kim BS. The behavior of neural stem cells on biodegradable synthetic polymers. J Biomater Sci Polym Ed 2007;18:223239. [PubMed: 17323855] Cortiella J, Nichols JE, Kojima K, Bonassar LJ, Dargon P, Roy AK, Vacant MP, Niles JA, Vacanti CA. Tissue-engineered lung: An in vivo and in vitro comparison of polyglycolic acid and pluronic F-127 hydrogel/somatic lung progenitor cell constructs to support tissue growth. Tissue Eng 2006;12:1213 1225. [PubMed: 16771635] Desai SD, Blanchard J. Pluronic F127-based ocular delivery system containing biodegradable polyisobutylcyanoacrylate nanocapsules of pilocarpine. Drug Deliv 2000;7:201207. [PubMed: 11195426] El Kamel AH. In vitro and in vivo evaluation of pluronic F127-based ocular delivery system for timolol maleate. Int J Pharm 2002;241:4755. [PubMed: 12086720] Flanagan LA, Rebaza LM, Derzic S, Schwartz PH, Monuki ES. Regulation of human neural precursor cells by laminin and integrins. J Neurosci Res 2006;83:845856. [PubMed: 16477652] Gao J, Coggeshall RE, Tarasenko YI, Wu P. Human neural stem cell-derived cholinergic neurons innervate muscle in motoneuron deficient adult rats. Neuroscience 2005;131:257262. [PubMed: 15708470] Gelain F, Lomander A, Vescovi AL, Zhang S. Systematic studies of a self-assembling peptide nanofiber scaffold with other scaffolds. J Nanosci Nanotechnol 2007;7:424434. [PubMed: 17450774]
Brain Res. Author manuscript; available in PMC 2009 January 2.
Thonhoff et al.
Page 9
Holmes TC, de Lacalle S, Su X, Liu GS, Rich A, Zhang SG. Extensive neurite outgrowth and active synapse formation on self-assembling peptide scaffolds. Proc Natl Acad Sci USA 2000;97:6728 6733. [PubMed: 10841570] Katakowski M, Zhang Z, deCarvalho AC, Chopp M. EphB2 induces proliferation and promotes a neuronal fate in adult subventricular neural precursor cells. Neurosci Lett 2005;385:204209. [PubMed: 15970380] Kleinman HK, Martin GR. Matrigel: Basement membrane matrix with biological activity. Semin Cancer Biol 2005;15:378386. [PubMed: 15975825] Lavik E, Teng YD, Snyder E, Langer R. Seeding neural stem cells on scaffolds of PGA, PLA, and their copolymers. Methods Mol Biol 2002;198:8997. [PubMed: 11951644] Novikova LN, Novikov LN, Kellerth JO. Biopolymers and biodegradable smart implants for tissue regeneration after spinal cord injury. Curr Opin Neurol 2003;16:711715. [PubMed: 14624081] Novikova LN, Mosahebi A, Wiberg M, Terenghi G, Kellerth JO, Novikov LN. Alginate hydrogel and matrigel as potential cell carriers for neurotransplantation. J Biomed Mater Res A 2006;77A:242 252. [PubMed: 16392134] Park KI, Teng YD, Snyder EY. The injured brain interacts reciprocally with neural stem cells supported by scaffolds to reconstitute lost tissue. Nat Biotechnol 2002;20:11111117. [PubMed: 12379868] Semino CE, Merok JR, Crane GG, Panagiotakos G, Zhang SG. Functional differentiation of hepatocytelike spheroid structures from putative liver progenitor cells in three-dimensional peptide scaffolds. Differentiation 2003;71:262270. [PubMed: 12823227] Semino CE, Kasahara J, Hayashi Y, Zhang SG. Entrapment of migrating hippocampal neural cells in three-dimensional peptide nanofiber scaffold. Tissue Eng 2004;10:643655. [PubMed: 15165480] Suslov ON, Kukekov VG, Ignatova TN, Steindler DA. Neural stem cell heterogeneity demonstrated by molecular phenotyping of clonal neurospheres. Proc Natl Acad Sci USA 2002;99:1450614511. [PubMed: 12381788] Svendsen CN, ter Borg MG, Armstrong RJ, Rosser AE, Chandran S, Ostenfeld T, Caldwell MA. A new method for the rapid and long term growth of human neural precursor cells. J Neurosci Methods 1998;85:141152. [PubMed: 9874150] Tarasenko YI, Yu YJ, Jordan PM, Bottenstein J, Wu P. Effect of growth factors on proliferation and phenotypic differentiation of human fetal neural stem cells. J Neurosci Res 2004;78:625636. [PubMed: 15490463] Tarasenko YI, Gao J, Nie L, Johnson KM, Grady JJ, Hulsebosch CE, McAdoo DJ, Wu P. Human fetal neural stem cells grafted into contusion-injured rat spinal cords improve behavior. J Neurosci Res 2007;85:4757. [PubMed: 17075895] Tate MC, Shear DA, Hoffman SW, Stein DG, Archer DR, LaPlaca MC. Fibronectin promotes survival and migration of primary neural stem cells transplanted into the traumatically injured mouse brain. Cell Transplant 2002;11:283295. [PubMed: 12075994] Teng YD, Lavik EB, Qu XL, Park KI, Ourednik J, Zurakowski D, Langer R, Snyder EY. Functional recovery following traumatic spinal cord injury mediated by a unique polymer scaffold seeded with neural stem cells. Proc Natl Acad Sci USA 2002;99:30243029. [PubMed: 11867737] Tisay KT, Key B. The extracellular matrix modulates olfactory neurite outgrowth on ensheathing cells. J Neurosci 1999;19:98909899. [PubMed: 10559398] Vacanti MP, Leonard JL, Dore B, Bonassar LJ, Cao Y, Stachelek SJ, Vacanti JP, OConnell F, Yu CS, Farwell AP, Vacanti CA. Tissue-engineered spinal cord. Transplant Proc 2001;33:592598. [PubMed: 11266974] Wenzel JG, Balaji KS, Koushik K, Navarre C, Duran SH, Rahe CH, Kompella UB. Pluronic F127 gel formulations of deslorelin and GnRH reduce drug degradation and sustain drug release and effect in cattle. J Control Release 2002;85:5159. [PubMed: 12480311] Wu P, Tarasenko YI, Gu YP, Huang LY, Coggeshall RE, Yu YJ. Region-specific generation of cholinergic neurons from fetal human neural stem cells grafted in adult rat. Nat Neurosci 2002;5:12711278. [PubMed: 12426573] Zaman MH, Trapani LM, Siemeski A, MacKellar D, Gong HY, Kamm RD, Wells A, Lauffenburger DA, Matsudaira P. Migration of tumor cells in 3D matrices is governed by matrix stiffness along with
NIH-PA Author Manuscript NIH-PA Author Manuscript NIH-PA Author Manuscript
Brain Res. Author manuscript; available in PMC 2009 January 2.
Thonhoff et al.
Page 10
cell-matrix adhesion and proteolysis. Proc Natl Acad Sci USA 2006;103:1088910894. [PubMed: 16832052] Zhang SG, Holmes T, Lockshin C, Rich A. Spontaneous assembly of a self-complementary oligopeptide to form a stable macroscopic membrane. Proc Natl Acad Sci USA 1993;90:33343338. [PubMed: 7682699] Zhang SG, Holmes TC, Dipersio CM, Hynes RO, Su X, Rich A. Self-complementary oligopeptide matrices support mammalian-cell attachment. Biomaterials 1995;16:13851393. [PubMed: 8590765]
NIH-PA Author Manuscript NIH-PA Author Manuscript NIH-PA Author Manuscript
Brain Res. Author manuscript; available in PMC 2009 January 2.
Thonhoff et al.
Page 11
NIH-PA Author Manuscript NIH-PA Author Manuscript
Fig. 1.
Cytotoxicity and morphological characteristics of human neural stem cells in hydrogels. Phasecontrast images of human neural stem cells primed for five days and then differentiated for two days in the absence of a hydrogel (control) (a), 10% PF127 (b), 20% PF127 (c), 30% PF127 (d), 1% Matrigel (e), 10% Matrigel (f), 50% Matrigel (g), 0.25% PuraMatrix (h), 0.5% PuraMatrix (i) and 1% PuraMatrix (j). Scale bar = 20 m.
NIH-PA Author Manuscript
Brain Res. Author manuscript; available in PMC 2009 January 2.
Thonhoff et al.
Page 12
NIH-PA Author Manuscript NIH-PA Author Manuscript NIH-PA Author Manuscript
Brain Res. Author manuscript; available in PMC 2009 January 2.
Fig. 2.
Viability of human neural stem cells beneath hydrogels. WST-1 assay on human neural stem cells primed for five days and then differentiated for two days in the absence of a hydrogel (control), PF127 (10-30%), Matrigel (1-50%) and PuraMatrix (0.25-1%). PF = PF127, MG = Matrigel and PM = PuraMatrix. A reference absorbance at 630 nm was taken and subtracted from the absorbance at 450 nm for each sample. *p < 0.05 compared to the control group.
Thonhoff et al.
Page 13
NIH-PA Author Manuscript NIH-PA Author Manuscript NIH-PA Author Manuscript
Brain Res. Author manuscript; available in PMC 2009 January 2.
Fig. 3.
Differentiation capacity of human neural stem cells beneath Matrigel and PuraMatrix. Immunofluorescent images of human neural stem cells primed for five days and then differentiated for seven days in the absence of a hydrogel (control, a-d); in contact with 20% Matrigel (e-h); and in contact with 0.25% PuraMatrix (i-l). DAPI (a, e and i), GFAP (b, f and j), Tuj1 (c, g and k) and overlay (d, h and l). Scale bar = 20 m.
Thonhoff et al.
Page 14
NIH-PA Author Manuscript
Fig. 4.
Migration capacity of human neural stem cells embedded as neurospheres after seven days within PuraMatrix. Phase-contrast images of human neural stem cell neurospheres seeded without a hydrogel for 3.5 days (a) and 7 days (b) and within 0.25% PuraMatrix for 3.5 days (c) and 7 days (d). A much higher proportion of migrating cells was observed from each sphere after 7 days in medium alone compared to 3.5 days. Scale bar = 20 m.
NIH-PA Author Manuscript NIH-PA Author Manuscript
Brain Res. Author manuscript; available in PMC 2009 January 2.
Thonhoff et al.
Page 15
NIH-PA Author Manuscript NIH-PA Author Manuscript NIH-PA Author Manuscript
Fig. 5.
Differentiation capacity of human neural stem cell neurospheres embedded within PuraMatrix. Immunofluorescent images of human neural stem cell neurospheres five days after passage (control) (a-e); and neurospheres differentiated within 0.25% PuraMatrix for seven days (f-j). DAPI (a and f), GFAP (b and g), Tuj1 (c and h) and overlay in a low magnification (d and i). Insets in d and i are shown in a high magnification in e and j, respectively. Scale bars = 20 m.
Brain Res. Author manuscript; available in PMC 2009 January 2.
Potrebbero piacerti anche
- Neurotoxicology and Teratology: Full Length ArticleDocumento7 pagineNeurotoxicology and Teratology: Full Length ArticlepasomagaNessuna valutazione finora
- Carbajal BEcellsDocumento9 pagineCarbajal BEcellsPatySA2Nessuna valutazione finora
- Inexhaustible Hair-Cell Regeneration in Young and Aged ZebrafishDocumento7 pagineInexhaustible Hair-Cell Regeneration in Young and Aged ZebrafishSaifuddin HaswareNessuna valutazione finora
- Stemcells 2006-0409Documento9 pagineStemcells 2006-0409dupuytrenNessuna valutazione finora
- 2011 BakirciogluDocumento13 pagine2011 BakirciogluMestrado EducacaoNessuna valutazione finora
- Evaluation of The Susceptibility of Neurons Anticancer DrugsDocumento6 pagineEvaluation of The Susceptibility of Neurons Anticancer DrugsLisbeth AlmNessuna valutazione finora
- Afafsaggw EscleDocumento7 pagineAfafsaggw EscleStephanie DuncanNessuna valutazione finora
- Joa 235 432Documento20 pagineJoa 235 432ElCanaldeSaadNessuna valutazione finora
- Neurobiology of Disease: E.N. Mangano, S. Peters, D. Litteljohn, R. So, C. Bethune, J. Bobyn, M. Clarke, S. HayleyDocumento14 pagineNeurobiology of Disease: E.N. Mangano, S. Peters, D. Litteljohn, R. So, C. Bethune, J. Bobyn, M. Clarke, S. HayleyShawn HayleyNessuna valutazione finora
- Articulo Neuro 1Documento12 pagineArticulo Neuro 1Victor CuellarNessuna valutazione finora
- Des Car GableDocumento10 pagineDes Car GableDago CastilloNessuna valutazione finora
- Genes Dev. 2015 Quesnel Vallières 746 59Documento15 pagineGenes Dev. 2015 Quesnel Vallières 746 59Misael G JordanNessuna valutazione finora
- 10.1007@s10571 020 00988 yDocumento8 pagine10.1007@s10571 020 00988 yKelvincarlx MorghanNessuna valutazione finora
- Changes in Hippocampal Neurogenesis Throughout Early 2015 Neurobiology of ADocumento15 pagineChanges in Hippocampal Neurogenesis Throughout Early 2015 Neurobiology of AErik J. Vallejo FonsecaNessuna valutazione finora
- Antibody Appears To Attack Cancer Cells, Leaving Other Cells UnscathedDocumento13 pagineAntibody Appears To Attack Cancer Cells, Leaving Other Cells UnscathedAnonymous EdgflnjcNessuna valutazione finora
- Yi_et_al-Glia 2017Documento19 pagineYi_et_al-Glia 2017Daniela HenríquezNessuna valutazione finora
- Learn. Mem.-2009-Jessberger-147-54llDocumento9 pagineLearn. Mem.-2009-Jessberger-147-54llJean Pierre Chastre LuzaNessuna valutazione finora
- The Blood Brain and Other Neural Barriers Methods in Molec Bio 0686 S Nag Humana 2011 WWDocumento591 pagineThe Blood Brain and Other Neural Barriers Methods in Molec Bio 0686 S Nag Humana 2011 WWAlexandr TrotskyNessuna valutazione finora
- Forebrain Engraftment by Human Glial Progenitor Cells Enhances Synaptic Plasticity and Learning in Adult MiceDocumento22 pagineForebrain Engraftment by Human Glial Progenitor Cells Enhances Synaptic Plasticity and Learning in Adult MiceAylin Lidsay Feria GNessuna valutazione finora
- Essay - Nanou - Discuss New Cancer Treatment Approach - Biol - Basics - Psychol - 2021 - Fall PDFDocumento9 pagineEssay - Nanou - Discuss New Cancer Treatment Approach - Biol - Basics - Psychol - 2021 - Fall PDFMaria NaNessuna valutazione finora
- Ref 5Documento11 pagineRef 5Tiago BaraNessuna valutazione finora
- Cerebral Dopamine Neurotrophic Factor Regulates Multiple Neuronal Subtypes and BehaviorDocumento19 pagineCerebral Dopamine Neurotrophic Factor Regulates Multiple Neuronal Subtypes and BehaviorCONSTANZA TERESA BERNA ARAYANessuna valutazione finora
- Chapter 17 - Endocrine Systems - 2020 - The Zebrafish in Biomedical ResearchDocumento15 pagineChapter 17 - Endocrine Systems - 2020 - The Zebrafish in Biomedical ResearchNicolas BaronNessuna valutazione finora
- Neun, A Neuronal Specific Nuclear Protein in VertebratesDocumento11 pagineNeun, A Neuronal Specific Nuclear Protein in VertebratesAditya KhemkaNessuna valutazione finora
- Reversing A Model of Parkinson's Disease With in Situ Converted Nigral NeuronsDocumento49 pagineReversing A Model of Parkinson's Disease With in Situ Converted Nigral NeuronsPablo OrdazNessuna valutazione finora
- Ramesh 2018Documento11 pagineRamesh 2018Ricardo MedinaNessuna valutazione finora
- Interneurons in The Developing Human Neocortex: Nada Zecevic, Frances Hu, Igor JakovcevskiDocumento16 pagineInterneurons in The Developing Human Neocortex: Nada Zecevic, Frances Hu, Igor JakovcevskiFrontiersNessuna valutazione finora
- Mechanisms of Disease: What Factors Limit The Success of Peripheral Nerve Regeneration in Humans?Documento7 pagineMechanisms of Disease: What Factors Limit The Success of Peripheral Nerve Regeneration in Humans?balab2311Nessuna valutazione finora
- 9732 FullDocumento10 pagine9732 FullDaniel Isaac Castillo HidalgoNessuna valutazione finora
- AlzehimerDocumento13 pagineAlzehimerFrancisco SalgadoNessuna valutazione finora
- Mouse Brain Proteome CGPDocumento30 pagineMouse Brain Proteome CGPChristina MountakiNessuna valutazione finora
- Currie, 2016 PDFDocumento18 pagineCurrie, 2016 PDF22gaefNessuna valutazione finora
- Generation and Characterization of A Mouse/human Chimeric Antibody Directed Against Extracellular Matrix Protein TenascinDocumento11 pagineGeneration and Characterization of A Mouse/human Chimeric Antibody Directed Against Extracellular Matrix Protein TenascinSayda DhaouadiNessuna valutazione finora
- Journal Pbio 3002242Documento37 pagineJournal Pbio 3002242Raymundo Lopez NNessuna valutazione finora
- Ajpcell 00166 2015Documento22 pagineAjpcell 00166 2015JasonNessuna valutazione finora
- P53 Aggregation, Interactions With Tau, and Impaired DNA Damage Response in Alzheimer 'S DiseaseDocumento21 pagineP53 Aggregation, Interactions With Tau, and Impaired DNA Damage Response in Alzheimer 'S DiseaseMazhar HussainNessuna valutazione finora
- Biochimica Et Biophysica Acta: Valerie C. Fleisch, Brittany Fraser, W. Ted AllisonDocumento17 pagineBiochimica Et Biophysica Acta: Valerie C. Fleisch, Brittany Fraser, W. Ted AllisonArvian DarmawanNessuna valutazione finora
- 401 2018 Article 1868Documento16 pagine401 2018 Article 1868Valen EstevezNessuna valutazione finora
- Functional Differences and Similarities in Activated Peripheral Blood Mononuclear Cells by Lipopolysaccharide or Phytohemagglutinin Stimulation Between Human and Cynomolgus Monkeys PDFDocumento25 pagineFunctional Differences and Similarities in Activated Peripheral Blood Mononuclear Cells by Lipopolysaccharide or Phytohemagglutinin Stimulation Between Human and Cynomolgus Monkeys PDFLluis GomezNessuna valutazione finora
- 2012 Theneuroprotectiveroleof TERTviaanantiapoptoticDocumento6 pagine2012 Theneuroprotectiveroleof TERTviaanantiapoptoticLoic MCNessuna valutazione finora
- Deciphering Stem Cell From Apical Papilla– MDocumento17 pagineDeciphering Stem Cell From Apical Papilla– Matif nawazNessuna valutazione finora
- Lee 2008Documento14 pagineLee 2008Laura Duarte RojasNessuna valutazione finora
- 1 s2.0 S0168165623000123 MainDocumento10 pagine1 s2.0 S0168165623000123 MainLauren Caluya LañoNessuna valutazione finora
- Mitochondrial Regulation in Pluripotent Stem Cells ReviewDocumento8 pagineMitochondrial Regulation in Pluripotent Stem Cells ReviewSamile AmorimNessuna valutazione finora
- Fendo 12 719843Documento17 pagineFendo 12 719843asdNessuna valutazione finora
- Chemically Induced Reprogramming of Somatic Cells To Pluripotent Stem Cells and Neural CellsDocumento13 pagineChemically Induced Reprogramming of Somatic Cells To Pluripotent Stem Cells and Neural CellsnembutalNessuna valutazione finora
- Multifunctionalized Hydrogels Foster HNSC MaturatiDocumento10 pagineMultifunctionalized Hydrogels Foster HNSC Maturatiandrey cardozoNessuna valutazione finora
- Nafisa HDocumento17 pagineNafisa Hiromini uthmanNessuna valutazione finora
- B-Regenerative Medicine 2023Documento11 pagineB-Regenerative Medicine 2023pnom43582Nessuna valutazione finora
- Dkk1 mediates MPP+-induced neurotoxicity in PC12 cellsDocumento8 pagineDkk1 mediates MPP+-induced neurotoxicity in PC12 cellsShawnNessuna valutazione finora
- Genome Res.-2013-Alföldi-1063-8Documento7 pagineGenome Res.-2013-Alföldi-1063-8Yamile A Rodríguez RiascosNessuna valutazione finora
- 6142 FullDocumento12 pagine6142 FullAmol MundeNessuna valutazione finora
- Emb Oj 2009327 ADocumento14 pagineEmb Oj 2009327 Athemoonwalker2014Nessuna valutazione finora
- Prospects For Human Gene TherapyDocumento17 pagineProspects For Human Gene TherapyAijaz AhmadNessuna valutazione finora
- Neuroanatomic Connectivity of the Human Ascending ArousalDocumento16 pagineNeuroanatomic Connectivity of the Human Ascending ArousalBritany SantanaNessuna valutazione finora
- Aggregating Brain Cell Cultures For Neurotoxicological StudiesDocumento24 pagineAggregating Brain Cell Cultures For Neurotoxicological Studiesmarej312Nessuna valutazione finora
- NAP ZNDocumento9 pagineNAP ZNancuta.lupaescuNessuna valutazione finora
- tmp7286 TMPDocumento15 paginetmp7286 TMPFrontiersNessuna valutazione finora
- 2021.04.19.440397v1.full طارقDocumento35 pagine2021.04.19.440397v1.full طارقTareq aliNessuna valutazione finora
- Tissue Engineering and Regeneration in Dentistry: Current StrategiesDa EverandTissue Engineering and Regeneration in Dentistry: Current StrategiesRachel J. WaddingtonNessuna valutazione finora
- S.Shelah and D.H.Fremlin - Pointwise Compact and Stable Sets of Measurable FunctionsDocumento16 pagineS.Shelah and D.H.Fremlin - Pointwise Compact and Stable Sets of Measurable FunctionsHutsDMNessuna valutazione finora
- Saharon Shelah - Vive La Difference II. The Ax-Kochen Isomorphism TheoremDocumento30 pagineSaharon Shelah - Vive La Difference II. The Ax-Kochen Isomorphism TheoremHutsDMNessuna valutazione finora
- Steven Givant and Saharon Shelah - Universal Theories Categorical in Power and Kappa-Generated ModelsDocumento22 pagineSteven Givant and Saharon Shelah - Universal Theories Categorical in Power and Kappa-Generated ModelsHutsDMNessuna valutazione finora
- Ankiewicz, S.Shelah and P.Zbierski - On Closed P-Sets With CCC in The Space OmegaDocumento6 pagineAnkiewicz, S.Shelah and P.Zbierski - On Closed P-Sets With CCC in The Space OmegaHutsDMNessuna valutazione finora
- Thomas Jech and Saharon Shelah - A Partition Theorem For Pairs of Finite SetsDocumento10 pagineThomas Jech and Saharon Shelah - A Partition Theorem For Pairs of Finite SetsHutsDMNessuna valutazione finora
- Uri Abraham and Saharon Shelah - A Delta 2-2 Well-Order of The Reals and Incompactness of L (Q MM)Documento49 pagineUri Abraham and Saharon Shelah - A Delta 2-2 Well-Order of The Reals and Incompactness of L (Q MM)HutsDMNessuna valutazione finora
- Saharon Shelah - Borel Whitehead GroupsDocumento14 pagineSaharon Shelah - Borel Whitehead GroupsHutsDMNessuna valutazione finora
- Saharon Shelah - Factor Quotient, Uncountable Boolean Algebras, Number of Endomorphism and WidthDocumento17 pagineSaharon Shelah - Factor Quotient, Uncountable Boolean Algebras, Number of Endomorphism and WidthHutsDMNessuna valutazione finora
- Saharon Shelah - Characterizing An - Epsilon Saturated Model of Superstable NDOP Theories by Its L, - Epsilon TheoryDocumento61 pagineSaharon Shelah - Characterizing An - Epsilon Saturated Model of Superstable NDOP Theories by Its L, - Epsilon TheoryHutsDMNessuna valutazione finora
- Saharon Shelah - Cardinal Arithmetic For SkepticsDocumento15 pagineSaharon Shelah - Cardinal Arithmetic For SkepticsHutsDMNessuna valutazione finora
- Alan H. Mekler and Saharon Shelah - The Canary TreeDocumento10 pagineAlan H. Mekler and Saharon Shelah - The Canary TreeHutsDMNessuna valutazione finora
- Saharon Shelah - Categoricity For Abstract Classes With AmalgamationDocumento82 pagineSaharon Shelah - Categoricity For Abstract Classes With AmalgamationHutsDMNessuna valutazione finora
- Thomas Jech and Saharon Shelah - A Note On Canonical FunctionsDocumento6 pagineThomas Jech and Saharon Shelah - A Note On Canonical FunctionsHutsDMNessuna valutazione finora
- Thomas Jech and Saharon Shelah - Full Reflection of Stationary Sets Below Aleph-OmegaDocumento13 pagineThomas Jech and Saharon Shelah - Full Reflection of Stationary Sets Below Aleph-OmegaHutsDMNessuna valutazione finora
- J. Baldwin and S. Shelah - Abstract Classes With Few Models Have 'Homogeneous-Universal' ModelsDocumento29 pagineJ. Baldwin and S. Shelah - Abstract Classes With Few Models Have 'Homogeneous-Universal' ModelsHutsDMNessuna valutazione finora
- Saharon Shelah - On Spectrum of Kappa-Resplendent ModelsDocumento28 pagineSaharon Shelah - On Spectrum of Kappa-Resplendent ModelsHutsDMNessuna valutazione finora
- Akihiro Kanamori and Saharon Shelah - Complete Quotient Boolean AlgebrasDocumento19 pagineAkihiro Kanamori and Saharon Shelah - Complete Quotient Boolean AlgebrasHutsDMNessuna valutazione finora
- Thomas Jech and Saharon Shelah - On A Conjecture of Tarski On Products of CardinalsDocumento8 pagineThomas Jech and Saharon Shelah - On A Conjecture of Tarski On Products of CardinalsHutsDMNessuna valutazione finora
- Tomek Bartoszynski, Haim Judah and Saharon Shelah - The Cichon DiagramDocumento24 pagineTomek Bartoszynski, Haim Judah and Saharon Shelah - The Cichon DiagramHutsDMNessuna valutazione finora
- Saharon Shelah and Joel Spencer - Can You Feel The Double JumpDocumento15 pagineSaharon Shelah and Joel Spencer - Can You Feel The Double JumpHutsDMNessuna valutazione finora
- Saharon Shelah, Heikki Tuuri and Jouko Vaananen - On The Number of Automorphisms of Uncountable ModelsDocumento20 pagineSaharon Shelah, Heikki Tuuri and Jouko Vaananen - On The Number of Automorphisms of Uncountable ModelsHutsDMNessuna valutazione finora
- Thomas Jech and Saharon Shelah - Full Reflection of Stationary Sets at Regular CardinalsDocumento16 pagineThomas Jech and Saharon Shelah - Full Reflection of Stationary Sets at Regular CardinalsHutsDMNessuna valutazione finora
- Alan H. Mekler and Saharon Shelah - Some Compact Logics - Results in ZFCDocumento33 pagineAlan H. Mekler and Saharon Shelah - Some Compact Logics - Results in ZFCHutsDMNessuna valutazione finora
- Alan H. Mekler and Saharon Shelah - Almost Free AlgebrasDocumento23 pagineAlan H. Mekler and Saharon Shelah - Almost Free AlgebrasHutsDMNessuna valutazione finora
- Haim Judah, Andrzej RosÃlanowski and Saharon Shelah - Examples For Souslin ForcingDocumento26 pagineHaim Judah, Andrzej RosÃlanowski and Saharon Shelah - Examples For Souslin ForcingHutsDMNessuna valutazione finora
- J. Baldwin and S. Shelah - The Primal Framework II: SmoothnessDocumento41 pagineJ. Baldwin and S. Shelah - The Primal Framework II: SmoothnessHutsDMNessuna valutazione finora
- S. Shelah and L. Soukup - On The Number of Non-Isomorphic SubgraphsDocumento25 pagineS. Shelah and L. Soukup - On The Number of Non-Isomorphic SubgraphsHutsDMNessuna valutazione finora
- P. Komjath and S. Shelah - On Taylor's ProblemDocumento7 pagineP. Komjath and S. Shelah - On Taylor's ProblemHutsDMNessuna valutazione finora
- Saharon Shelah and Oren Kolman - Categoricity of Theories in L-Kappa-Omega, When Kappa Is A Measurable Cardinal - Part 1Documento40 pagineSaharon Shelah and Oren Kolman - Categoricity of Theories in L-Kappa-Omega, When Kappa Is A Measurable Cardinal - Part 1HutsDMNessuna valutazione finora
- Saharon Shelah and Lee J. Stanley - A Combinatorial Forcing For Coding The Universe by A Real When There Are No SharpsDocumento76 pagineSaharon Shelah and Lee J. Stanley - A Combinatorial Forcing For Coding The Universe by A Real When There Are No SharpsHutsDMNessuna valutazione finora
- Antenatal Care and High Risk PregnancyDocumento76 pagineAntenatal Care and High Risk PregnancyLouis EkaputraNessuna valutazione finora
- TOG Assessment of The Infertile MaleDocumento9 pagineTOG Assessment of The Infertile MaleMarNessuna valutazione finora
- NonClassical MHC Class I PDFDocumento12 pagineNonClassical MHC Class I PDFRobMarvinNessuna valutazione finora
- PEMERIKSAAAN LABORATORIUM KELAINAN THYROIDDocumento12 paginePEMERIKSAAAN LABORATORIUM KELAINAN THYROIDBonitavanyNessuna valutazione finora
- Building On Success: A Bright Future For Peptide TherapeuticsDocumento7 pagineBuilding On Success: A Bright Future For Peptide TherapeuticsDiana PachónNessuna valutazione finora
- Biliary Atresia Copy LNGDocumento10 pagineBiliary Atresia Copy LNGlloraoNessuna valutazione finora
- Biopolymer Research Trends PDFDocumento236 pagineBiopolymer Research Trends PDFsrijitkhanNessuna valutazione finora
- DermatologyDocumento121 pagineDermatologyjimisurgon83100% (4)
- Evolution of Vertebrate Eyes - How Vision EvolvedDocumento14 pagineEvolution of Vertebrate Eyes - How Vision Evolvedlurolu1060Nessuna valutazione finora
- Dendrimers: Synthesis, Applications, and Properties: Nanoreview Open AccessDocumento10 pagineDendrimers: Synthesis, Applications, and Properties: Nanoreview Open AccessIonut StirbescuNessuna valutazione finora
- Toxicological Evaluation PDFDocumento291 pagineToxicological Evaluation PDFMaría SolórzanoNessuna valutazione finora
- Quantitative Analysis of The Substrate Specificity of Human Rhinovirus 3C Protease and Exploration of Its Substrate Recognition MechanismsDocumento14 pagineQuantitative Analysis of The Substrate Specificity of Human Rhinovirus 3C Protease and Exploration of Its Substrate Recognition MechanismsLuís MiguelNessuna valutazione finora
- Evolution - A Golden GuideDocumento164 pagineEvolution - A Golden GuideKenneth83% (12)
- Microbiology NotesDocumento3 pagineMicrobiology NotesAthena Huynh100% (1)
- Part 25: Muscle Chapter 216: The Muscular DystrophiesDocumento73 paginePart 25: Muscle Chapter 216: The Muscular DystrophiesVane100% (1)
- Normal Bone Anatomy and PhysiologyDocumento9 pagineNormal Bone Anatomy and PhysiologyElsa GonçalvesNessuna valutazione finora
- Journal Reading - TLR9 Expression Correlates with Cytokine Levels in SLE PatientsDocumento48 pagineJournal Reading - TLR9 Expression Correlates with Cytokine Levels in SLE PatientsEdwin DarmawanNessuna valutazione finora
- Genetically Modified Bacteria Treat Digestive DiseaseDocumento6 pagineGenetically Modified Bacteria Treat Digestive DiseaseRutba SafdarNessuna valutazione finora
- Horseshoe Crab For Medical Science by Dr. Anil ChatterjiDocumento42 pagineHorseshoe Crab For Medical Science by Dr. Anil ChatterjiDr Bugs TanNessuna valutazione finora
- 22 Respiratory SystemDocumento99 pagine22 Respiratory SystemvanderphysNessuna valutazione finora
- Evolution Biology IntroductionDocumento22 pagineEvolution Biology IntroductionConstance Viloria100% (1)
- NCP - FatigueDocumento3 pagineNCP - Fatigueitsmeaya100% (1)
- BlastulaDocumento4 pagineBlastulaCyanDesNessuna valutazione finora
- 2021 ASO Biology Exam Part 1Documento20 pagine2021 ASO Biology Exam Part 1Joshua DeathNessuna valutazione finora
- Triple Negative Breast Cancer: Understanding The Molecular, Biologic, and Clinical CharacteristicsDocumento24 pagineTriple Negative Breast Cancer: Understanding The Molecular, Biologic, and Clinical Characteristicsleeann_swenson100% (1)
- Biotechnology: Quarter 3 - Module 2: Genetic ManipulationDocumento24 pagineBiotechnology: Quarter 3 - Module 2: Genetic ManipulationJohn Mark Laurio82% (17)
- Nursing Care of The Client With CancerDocumento15 pagineNursing Care of The Client With CancerAlvin M Alcayno0% (1)
- 2005 January SN 1,4 Mark SchemeDocumento28 pagine2005 January SN 1,4 Mark Schememmgdumbo1230% (1)
- Study Guide For The Psychiatry NBME Content Exam AKA The Psychiatry Shelf Exam!Documento2 pagineStudy Guide For The Psychiatry NBME Content Exam AKA The Psychiatry Shelf Exam!DoriNessuna valutazione finora
- IAL Biol WBI05 Jan18 Scientific ArticleDocumento8 pagineIAL Biol WBI05 Jan18 Scientific ArticleMoeez AkramNessuna valutazione finora