Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Iba 2
Caricato da
RPh Krishna Chandra JagritDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Iba 2
Caricato da
RPh Krishna Chandra JagritCopyright:
Formati disponibili
Iba lecture 1 Transcript
Relationship of metabolism of drugs to efficacy and safety of drugs depends extensively on drug metabolism 2 major phases of drug metabolism must be familiar with these 2 phases and the important enzymes that mediate these 2 phases Pharmacokinetics refers to what the body does to the drug ADME Pharmacodynamics is how the drug interacts with targets and receptors to bring about pharmacologic/therapeutic effects As you see in the chart, PD (what drugs do to the body depends on what body does to drug) metabolism is a major determinant of some of the PD responses in the body He is not going to ask us to remember specific drugs but occasionally will use specific drugs to demonstrate the important metabolic principles, these drugs he will expect us to be familiar with Acetaminophen /Tylenol ->will talk about a lot, really isnt the safest drug because of the way it is metabolized We are held accountable for recognizing the important functional groups that show up in drug molecules and should be familiar with how those fxnl groups are modified by drug metabolizing enzymes Will you give you a structure of drug..dont need to know name but should be able to tell him what metabolic pathway it will undergo (principles of drug metabolism) Single drug administered to an individual by 2 different routes For every therapeutic drug time course of changes in drug concentration in plasma Pharmacokinetics What route of administration is this? PO, what route is this? IV What do you call this phase? Absorption, then distribution, metabolism and distribution, now for every single drug there is a plasma concentration above which the drug will cause toxicity overdose in form of ADRs plasma concentrations should stay within therapeutic range, for most durgs and most people, when the plasma concentration reaches this level right here, associated with ADRs, overdose effects whereas if the plasma concentration stays below this range will not experience any therapeutic effects, no response below this therapeutic range what determines if a standard dose of a drug is metabolized too extensively or elminated too extensively chances are the plasma levels will not reach therapeutic levels whereas the metabolism of the same dose of drug in another individual is too slow, the drug will accumulate , in drugs that will not metabolize, this concentration will stay indefinitely, maintain plateau in body most take dose in regiments QD or BID, except for extended dose where you take one dose a day and then a constant amount is released to maintain a therapeutic drug concentration if drugs were not metabolized, w ill build up a cumulative level of drug toxicity most drugs are subject to metabolism, may be a few drugs that will not undergo metabolism, they are eliminated by excretion, but most drugs depend on metabolism prior to excretion
reason for metabolism is that most drugs are lipophilic the only way it can be excreted in urine, is to make the drug polar, to introduce a functional group total of 6 slides A-F, will talk about later in metabolism section? this is what happens to the drug when it gets into the cell metabolism of drugs are in the cell, there is very little metabolism of drugs outside of the cell there are many times the plasma that will metabolize the drug, but most of the drugs metabolizing enzymes are within the cell PK within the cell focusing on biotransformation the fate of the drug hepatic tissue liver is the major organ of drug metabolism, A substance could be a xenobiotic refers to therapeutic drugs, cosmetics, industrial chemicals, Unless he mentions Therapeutic drugs, assume that all of these compounds including some endogenous compounds (steroids, fatty acids, amino acids ) all can be metabolized by the same enzymes we will be discussing Like drugs, they can be taken up from the plasma into the cell and a lot of the very lipid soluble drugs will diffuse into the cell, whereas a lot of compounds depend on some kind of transport mechanism to be taken up. Mediatoreither active or regulated uptake of substance into cell Within the cell, the drug undergoes phase I metabolism comprises of oxidation, reduction, and hydrolysis. By Cyp 450 So the product, the first oxidation product is never sufficiently water soluble to enhance elimination so the need for Phase II If Phase I product is not sufficiently water soluble, couple an endogenous compound which is very polar so you can get a conjugation with metabolite product of Phase II conjugation metabolism is much more water soluble than product of phase I Phase 2 (catalyzed by transferases an enzyme that catalyzes conjugation reactions Phase 1 is catabolic metabolic reactions, whereas Phase 2 are synthetic metabolic Sometimes called Phase 3 is the export ( not really metabolism so the very polar metabolite formed within the cell canot passively pass through membrane series of transport processes that actively transport the conjugates from the cell Shown in red, that not all drugs will undergo the sequential phase1, phase2 a lot of drugs can undergo phase 2 without undergoing phase 1 What the drug will undergo depends on the functional groups on that molecule and if phase 2 enzymes recognizes the functional group and metabolizes it , itll conjugate that drug w/o phase 1 metabolism This is the interaction between PK and PDso thats the central drug compartment? And this is what determines the level of drug the central compartment determines the pharmacodynamic effects ??? For all PO drugs, the drug has to be absorbed and a lot of the absorption processes are mediated by transport proteins and active uptake of drug from oral administration GIT hepatic portal vein within the central compartment , with the excretion of the drug there is metabolism and distribution and excretion the balance of the 3 processes will determine the plasma level in blood Plasma level is what determines the level of drug that is present at the site of action , receptors, to determine the effects
ADME categorized as PK, and of course the concentration at the sites of the receptor trigger either beneficial effects or toxic/ADRs referred to as PD The amount of drugs that is present in the central compartment right here is determined by all of these processes and the resulting levels determine whether efficient, no effects, or toxic effects The PD responses depend on the PK Showed you this already, therapeutic range in which this black curve, toxic dose range by dotted line, and sub therapeutic by red dotted line Different people taking same dose of same drug metabolize at different rates, too rapidly and too slowly. Metabolism determines the plasma level: subtherapeutic, toxic, adequate Drug metabolism basic mechanisms and principles. Xenobiotics Greek , xeno is foreign to the body, anything the body does not make. All these cmpds are fair game for DMEs Drug metabolizing enzymes named because of how they were discovered, but were also found to be very effective in metabolizing endogenous compounds. In fact, these enzymes do not exist to metabolize chemicals, have very important homeostatic compounds, involved in the synthesis of steroid hormones, FA hormones and terminating the actions of hormones and neurotransmitters, so they have important physiological functions, it just happens that they have the right functions to metabolize they do not exist to metabolize the drugs. Many enzymes in fact are inducible, when you introduce chemicals to the body, homeostatic mechanisms is to try toget rid of these chemicals what these chemicals do is to stimulate the synthesis of enzymes to break down these chemicals so the body can get rid of them homeostatic function the metabolism of drugs is not always beneficial can lead to undesirable toxic effects a very new compound, never sure what metabolism will result exaggerated toxicity or .on the parent compound, or terminate the pharmacological actions of the drug this is basically what im showing here, what do the enzymes do to the drug depends on the structure of the drug, and where in the body metabolism takes place before the drug gets released, metabolism is always extensively studied to make sure that the drug is safe, that you dont form any toxic metabolites phenomenon called pharmacogenetics always people out there, outliers, people will metabolize the same drug in a very peculiar way and may experience effects not known in the general population what are the consequences of drug metabolism /biotransformation inactivation refers to terminating, rendering the drug pharmacologically inactive, all the drugs we take are pharmacologically active, would stay this way if there was not termination a lot of chemicals , toxic chemicals in the environment, pollutants, the metabolism(inactivation) of such compounds will terminate the toxicity metabolism can be bioactivation of either a therapeutic drug or an environmental chemical many pharmacological agents that are ineffective as crude drugs, as you get them from the shelf, theyre not pharmacologically active, they depend on the metabolism in the body to generate activity, some such cmpds are ineffective as crude/pure? Drugs Example is codeine codeine is an analgesic , but the pharmacologically active metabolite is actually morphine codeine has a slight analgesic effect, it is the morphine thats generated that accounts for the majority of the pharmacologically effects of codeine
acetaminophen analgesic, not narcotic, causes severe liver toxicity toxicity is due to a particular metabolite formed in the liver by DMEs drug activation/bioactivation can be caused by DMEs there isnt a single organ in the body that doesnt have these DMEs the liver is the, that why the liver is always reffered to as the organ of drug metabolism the highest in the liver?, and you do have some DMEs in extrahepatic tissue organs and tissues, some DMEs completely absent in the liver. liver has most of the DMEs but not all of them. 99.9% of DME activity is in the liver these are in decreasing amounts the GIT, some of the DMEs are found at levels in the intestine that are just about as high as in the liver the relevance of metabolism of drugs in extrahepatic organs toxicity some drugs are specifically toxic to some organs and not others some are toxic to the lung, and not to the liver, toxic to the brain, etc these toxic effects can result from the selective expression of enzymes involved in the metabolism of these drugs an enzyme that metabolizes drugs to toxic metabolites in the brain, even in selected neurons the level of metabolism is about 1% in the liver, but if the 1% is present in specific regions in the brain and only in selected cells can account for a lot of the toxicity the brain diseases are usually very localized within specific regions in the brain and within specific neurons > how basically these DMEs are distributed in region specific manner, in a cell-type specific manner p450 one of the cytp450 3a4 is very high in the GIT cell and also in the liver when you take a drug the intestinal cells metabolize it --. Get about 25%, lost 25% in the gut, so 75% survive will go into liver metabolizes another 50% so youre left with only 25% that survives into plasma and gets redistributed to the target organs metabolism from the GIT and then in the liver, into systemic circulation actually decreases the availability of the drug to reaches the plasma the first pass effect is what happens to a drug on its way from the GIT into the liver and then into systemic circulation 3a4 metabolizes 40% of the drugs, metabolism in the gut contributes significantly to the 1st pass effect whatever survives passes through the portal vein to the liver where most of the metabolism much lower fraction of what taken by PO whereas 1st pass is not significant from IV administration although IV introduce drugs into circulation the latency is a lot shorter in IV administered drugs compared to PO admin drugs because youre not going to need the time to absorb the drug to reach the plasma therapeutic level, almost instantaneously all the drugs you administer to central compartment through IV admin, will end up in the liver and get metabolized through the hepatic, IV drugs eventually do get metabolized the metabolism in the GIT and liver decrease the bioavailability of the drug Fraction of the administered drug that reaches central circulation Then of course another consequence ofdrug metabolism in extra hepatic tissues is that the metabolism in specific type of organs , they form toxic drugs that cause toxicity to those extrahepatic organs subcellular distributions subcellular fraction important ones we are concerned with o smooth ER 80% of all of the drugs are metabolized.
o Cytoplasm conjugating enzymes are distributed. Some DMEs are found
exclusively in mitochondria
o Some of the nucleus, but the is not important to metabolism?
The ER enzymes catalyze mostly phase I metabolism, but they do also catalyze conjugation reactions the particular enzymes of phase I is classified as a mixed function oxidase enzyme system that cytp450 is the most important component of the mixed function oxidase systems These systems are localized in the smooth ER the enzymes of the SER are very important in industry enzymes are studied from human tissues, animal tissues so we always have SER in a test tube in vitro, and when you isolate them, the ER is frequently referred to as microsomes as isolated in test tubes homogenize the organ and centrifugation steps you can separate the structures Take these different fractions and find out about their drug metabolizing activity we found that the the ER is the richest in terms of metabolism about 80% of all the therapeutically useful drugs So this is the process series of centrifugations until you get the ? Microsomes what we use for the study of metabolism DMEs exclusive to SER
Potrebbero piacerti anche
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5795)
- Matrimonial Resume CVDocumento3 pagineMatrimonial Resume CVRPh Krishna Chandra Jagrit76% (37)
- Matrimonial Resume CVDocumento3 pagineMatrimonial Resume CVRPh Krishna Chandra Jagrit76% (37)
- Matrimonial Resume CVDocumento3 pagineMatrimonial Resume CVRPh Krishna Chandra Jagrit76% (37)
- About MeningiomaDocumento5 pagineAbout MeningiomaRPh Krishna Chandra JagritNessuna valutazione finora
- Mantras - English - KundaliniDocumento7 pagineMantras - English - KundaliniRPh Krishna Chandra JagritNessuna valutazione finora
- 6th Central Pay Commission Salary CalculatorDocumento15 pagine6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- MantrasDocumento24 pagineMantrasg_gaurishankar@rediffmail.com100% (4)
- Martial Arts - Bruce Lee's Training SecretsDocumento3 pagineMartial Arts - Bruce Lee's Training Secretsbrogan91% (34)
- Krav Maga Pressure Points - Military Hand To Hand Combat GuideDocumento27 pagineKrav Maga Pressure Points - Military Hand To Hand Combat Guidebrogan98% (135)
- HTML-XHTML Tag SheDocumento6 pagineHTML-XHTML Tag SheabcjohnNessuna valutazione finora
- General Pharmacology MCQDocumento6 pagineGeneral Pharmacology MCQShrikant ThakurNessuna valutazione finora
- About This Tutorial: Version HistoryDocumento328 pagineAbout This Tutorial: Version HistoryKate CorralesNessuna valutazione finora
- Martial Arts - Bruce Lee's Speed TrainingDocumento4 pagineMartial Arts - Bruce Lee's Speed Trainingbrogan97% (33)
- Super Fast Mental Math - Vedic Math HistoryDocumento51 pagineSuper Fast Mental Math - Vedic Math Historyvedicmath98% (41)
- Web DesigningDocumento638 pagineWeb DesigningRPh Krishna Chandra JagritNessuna valutazione finora
- Introduction in Human AnatomyDocumento60 pagineIntroduction in Human AnatomyRPh Krishna Chandra JagritNessuna valutazione finora
- Math Olympiad Problems Collection-V1Documento97 pagineMath Olympiad Problems Collection-V1RPh Krishna Chandra Jagrit100% (1)
- Tally 9.2 NotesDocumento1.918 pagineTally 9.2 NotesRamesh75% (4)
- Medicinal PlantsDocumento29 pagineMedicinal PlantsGANESH KUMAR JELLANessuna valutazione finora
- Curriculum VitaeDocumento2 pagineCurriculum VitaeRPh Krishna Chandra JagritNessuna valutazione finora
- General KnowledgeDocumento141 pagineGeneral KnowledgeRAVI KUMAR83% (12)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Pharmacists Role Clinical Pharmacokinetic MonitoringDocumento2 paginePharmacists Role Clinical Pharmacokinetic MonitoringauliaNessuna valutazione finora
- Hard HPMC CapsulesDocumento3 pagineHard HPMC CapsulesnaturalcapsulesNessuna valutazione finora
- Syllabus For Pharmacy (PGQP24) : Pharmaceutics-I (Introduction To Pharmaceutics)Documento9 pagineSyllabus For Pharmacy (PGQP24) : Pharmaceutics-I (Introduction To Pharmaceutics)Huba ZehraNessuna valutazione finora
- Update Pasang Flash Sale Minggu Iii SD Iv Januari 2022Documento9 pagineUpdate Pasang Flash Sale Minggu Iii SD Iv Januari 2022riskaNessuna valutazione finora
- Modelo UnidadesDocumento64 pagineModelo UnidadesRafael MagalhãesNessuna valutazione finora
- Daftar PustakaDocumento16 pagineDaftar PustakaDestrie CindyNessuna valutazione finora
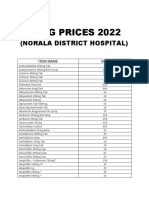
- Drug Prices 2022Documento11 pagineDrug Prices 2022NDH PHARMACYNessuna valutazione finora
- RectalDocumento32 pagineRectalYoga SutrisnoNessuna valutazione finora
- 保健中心藥品清單Documento2 pagine保健中心藥品清單台大家醫部總醫師Nessuna valutazione finora
- Pkpdcon Programme FinalDocumento2 paginePkpdcon Programme FinalSivanantham KrishnamoorthiNessuna valutazione finora
- Sample Internship Training Plan TemplateDocumento127 pagineSample Internship Training Plan TemplatenadivataniaNessuna valutazione finora
- Regulatory Affairs What Is It 1702454611Documento63 pagineRegulatory Affairs What Is It 1702454611bastawroussamerNessuna valutazione finora
- Acetaminophen Toxicity in ChildrenDocumento5 pagineAcetaminophen Toxicity in Childrendaniascl9527Nessuna valutazione finora
- NO Nama Obat Satuan Jumlah Harga Tanggal ED BatchDocumento4 pagineNO Nama Obat Satuan Jumlah Harga Tanggal ED BatchDiah WidianingtyasNessuna valutazione finora
- 368371Documento10 pagine368371Ashraf Uddin AhmedNessuna valutazione finora
- DAFTAR OBAT DAN PBF (Karunia Farma TGR)Documento2 pagineDAFTAR OBAT DAN PBF (Karunia Farma TGR)mincutttNessuna valutazione finora
- Clinical Research ICRIDocumento37 pagineClinical Research ICRIanu87scorpNessuna valutazione finora
- Pharmacy Technician CVDocumento2 paginePharmacy Technician CVOliaNessuna valutazione finora
- Pharmacovigilance Directive English 2020Documento26 paginePharmacovigilance Directive English 2020Zelalem KetemaNessuna valutazione finora
- What Is 21 CFR Part 11Documento26 pagineWhat Is 21 CFR Part 11chemtabNessuna valutazione finora
- Cerenia Combo PI May2012Documento2 pagineCerenia Combo PI May2012wvhvet100% (1)
- Stock 18 Feb 20Documento29 pagineStock 18 Feb 20alfath ramaNessuna valutazione finora
- Aplikasi Apotek Fadilah FarmaDocumento75 pagineAplikasi Apotek Fadilah FarmaRama RakanataNessuna valutazione finora
- Lasa High Alert FarmasiDocumento10 pagineLasa High Alert FarmasiUlfa ErviliaNessuna valutazione finora
- MicromedextwoDocumento60 pagineMicromedextwoDaniel Martínez SilvaNessuna valutazione finora
- Administering Oral Medication (Print)Documento5 pagineAdministering Oral Medication (Print)Binoy Serino100% (1)
- Simcyp PBPK V23 2024 Final v2Documento5 pagineSimcyp PBPK V23 2024 Final v2backup.data.drive.03Nessuna valutazione finora
- Drug Study PyrazinamideDocumento1 paginaDrug Study PyrazinamideEphraim MaravillaNessuna valutazione finora
- Pharmaceutical Science 2014Documento10 paginePharmaceutical Science 2014Mihai CojocaruNessuna valutazione finora
- An Overview On Fast Disintegrating Sublingual Tablets 945-2760-1-PBDocumento11 pagineAn Overview On Fast Disintegrating Sublingual Tablets 945-2760-1-PBQasim AkhtarNessuna valutazione finora