Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
NSCLCMA
Caricato da
api-26302710Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
NSCLCMA
Caricato da
api-26302710Copyright:
Formati disponibili
VOLUME 26 䡠 NUMBER 28 䡠 OCTOBER 1 2008
JOURNAL OF CLINICAL ONCOLOGY O R I G I N A L R E P O R T
Chemotherapy in Addition to Supportive Care Improves
Survival in Advanced Non–Small-Cell Lung Cancer: A
Systematic Review and Meta-Analysis of Individual Patient
Data From 16 Randomized Controlled Trials
NSCLC Meta-Analyses Collaborative Group
From the Clinical Trials Unit, Medical
Research Council, London, United King- A B S T R A C T
dom; and the Institut Gustave-Roussy,
Villejuif, France. Purpose
Since our individual patient data (IPD) meta-analysis (MA) of supportive care and chemotherapy for
Submitted April 24, 2008; accepted
May 27, 2008; published online ahead
non–small-cell lung cancer (NSCLC), published in 1995, many trials have been completed. An
of print at www.jco.org on August 4, updated, IPD MA has been carried out to assess newer regimens and determine conclusively the
2008. effect of chemotherapy.
Supported by UK Medical Research Methods
Council. Systematic searches for randomized controlled trials (RCTs) were undertaken, followed by central
Presented at 43rd Annual Meeting of collection, checking, and reanalysis of updated IPD. Results from RCTs were combined to
the American Society of Clinical Oncol- calculate individual and pooled hazard ratios (HRs).
ogy, Chicago, IL, June 1-5, 2007, and at
the World Conference on Lung Cancer,
Results
Seoul, South Korea, September 2-6,
Data were obtained from 2,714 patients from 16 RCTs. There were 1,293 deaths among 1,399
2007. patients assigned supportive care and chemotherapy and 1,240 among 1,315 assigned supportive
Authors’ disclosures of potential con-
care alone. Results showed a significant benefit of chemotherapy (HR, 0.77; 95% CI, 0.71 to 0.83;
flicts of interest and author contribu- P ⱕ .0001), equivalent to a relative increase in survival of 23% or an absolute improvement in
tions are found at the end of this survival of 9% at 12 months, increasing survival from 20% to 29%. There was no clear evidence
article. that this effect was influenced by the drugs used (P ⫽ .63) or whether they were used as single
Corresponding author: Sarah Burdett, agents or in combination (P ⫽ .40). Despite changes in patient demographics, the effect of
MSc, Medical Research Council Clinical chemotherapy in recent trials did not differ from those included previously (P ⫽ .77). There was
Trials Unit, 222 Euston Rd, London, no clear evidence of a difference or trend in the relative effect of chemotherapy across
NW1 2DA, United Kingdom; e-mail: patient subgroups.
sb@ctu.mrc.ac.uk.
Conclusion
© 2008 by American Society of Clinical
This MA of chemotherapy in the supportive care setting demonstrates conclusively that chemo-
Oncology
therapy improves overall survival in all patients with advanced NSCLC. Therefore, all patients who
0732-183X/08/2628-4617/$20.00
are fit enough and wish to receive chemotherapy should do so.
DOI: 10.1200/JCO.2008.17.7162
J Clin Oncol 26:4617-4625. © 2008 by American Society of Clinical Oncology
racic radiotherapy or combined chemoradiother-
INTRODUCTION
apy. The remaining 50% of patients, essentially
Worldwide, approximately 1.5 million new cases of those with metastatic disease or who are medically
lung cancer are diagnosed each year.1 Approxi- unfit, are treated palliatively.
mately 85% of these tumors are of non–small-cell Our previous meta-analysis6 based on individ-
histologicaltype,2 includingadenocarcinomas,squa- ual patient data (IPD) of more than 9,000 patients
mous cell, and large cell carcinomas. Non–small-cell from more than 50 randomized trials, concluded
lung cancer (NSCLC) is the main cause of death that despite previous scepticism and controversy,
from cancer,3 and 5-year survival across all stages of platinum-based chemotherapy has a role in treating
the disease is approximately 14%.4 patients with NSCLC. In particular, there was strong
Surgery is generally regarded as the best treat- evidence that for advanced disease, chemotherapy
ment option, but only approximately 30% of tu- given in addition to supportive care could prolong
mors are suitable for potentially curative resection.5 survival. Since the publication, a considerable num-
A further 20% of patients, usually those presenting ber of new trials exploring newer drugs and new
with locally advanced disease, undergo radical tho- modes of administration have been completed. To
© 2008 by American Society of Clinical Oncology 4617
Downloaded from jco.ascopubs.org by ALICIA HENAO URIBE on October 5, 2008 from 200.116.146.33.
Copyright © 2008 by the American Society of Clinical Oncology. All rights reserved.
Burdett et al
take account of the expanded evidence base and provide the most queries were resolved and the final database entries verified by the responsible
up-to-date and reliable assessment of the role of chemotherapy in trial investigator or statistician.
NSCLC, the NSCLC Collaborative Group has carried out an updated Definition of Outcomes
IPD meta-analysis that examines the role of chemotherapy in seven Overall survival was defined as the time from randomization until death
treatment comparisons.7 In the supportive care setting reported here, by any cause. Patients still alive were censored at the date of last follow-up or
we assessed the role of newer chemotherapy agents and assessed more date last known to be alive.
reliably the effect of chemotherapy in different subgroups of patients. Analysis
Analyses of outcomes, trial groups, and patient groups were (unless
otherwise stated) prespecified in the protocol and carried out on an intention
METHODS to-treat basis; that is, patients were analyzed according to their allocated treat-
ment, irrespective of whether they received that treatment. Analyses of all end
The aim was to assess the effect of supportive care and chemotherapy versus points were stratified by trial, and the log-rank expected number of deaths and
supportive care alone in advanced NSCLC. The meta-analysis followed a variance was used to calculate individual trial hazard ratios (HRs) and overall
detailed and prespecified protocol which set out the objectives, inclusion pooled HRs based on the fixed effect model.9 Thus, the times to death for
criteria for trials, data to be collected and analyses to be carried out. A copy of individual patients were used within trials to calculate the HR, representing the
the protocol is available on request (from S.B.). overall risk of an event for those patients allocated to supportive care and
chemotherapy compared with those allocated to supportive care alone. Results
Inclusion Criteria were also combined using the random effects model to assess the robustness of
To be included in the meta-analysis, trials had to be properly random- the results to the choice of meta-analysis model.
ized, have commenced accrual on or after January 1, 1965, and have completed To examine the potential impact of the treatments used, we predefined
accrual. Trials should have included patients with NSCLC who had received analyses that grouped trials by the type of the chemotherapy regimen used. For
either chemotherapy and supportive care or supportive care alone, that were these analyses, a pooled HR was calculated for each group of trials and for all
unsuitable for surgery or radical radiation therapy. Supportive care was de- trials together. As we specified that we would group those trials using
fined in the individual trials and may include palliative radiotherapy, antibiot- platinum-based chemotherapy with a vinca-alkaloid or etoposide separately
ics, corticosteroids, analgesics, antiemetics, transfusions, and psychosocial from those trials that did not use a vinca-alkaloid or etoposide, the Big Lung
support. Patients should have not received any previous chemotherapy or had Trial (BLT) trial10 was divided into two trials. BLT1 combined cisplatin with a
any prior malignancy. vinca-alkaloid and BLT2 did not use a vinca-alkaloid.
Identification of Trials The relative effects of chemotherapy in different subgroups of patients
To limit publication bias, we included all randomized trials, whether were investigated using similar stratified analyses. Analyses were performed for
published or unpublished. We carried out bibliographic searches of Medline each prespecified subgroup, for example, comparing the effect of treatment
and CancerLit using the Cochrane Collaboration optimal search strategy for and control for males and for females within each individual trial. These results
identifying randomized controlled trials.8 These were supplemented by were then combined to give overall HRs for males and for females. 2 tests for
searching the Cochrane Central Register of Controlled Trials, the abstracts interaction or trend were used to investigate whether there were any substan-
from relevant conferences, the reference lists of identified trials, the bibliogra- tial differences in the effect of chemotherapy between groups of trials or
phies of relevant books, and review articles. The National Cancer Institute subgroups of patients.
Physicians Data Query clinical protocols, United Kingdom Coordinating Results are also presented as absolute differences at 1 year, calculated
Committee for Cancer Research trials register, and the Current Controlled using the overall HRs and the control arm event rate.11 CIs for absolute
Trials metaRegister of trials were also searched to identify unpublished and differences were calculated from the baseline event rate and the HR at the
ongoing trials. All trialists who took part in the meta-analysis were asked to 95% CI boundary values. 2 heterogeneity tests and the I2 statistic for
help to identify additional trials. Initially searches were completed for the inconsistency12 were used to assess statistical heterogeneity across trials. Sur-
period up to and including 2003. These were revised regularly to identify vival curves are presented as simple (nonstratified) Kaplan-Meier curves.13 All
further trials published by our final analyses in September 2007. Where there P values quoted are two sided.
was uncertainty about the eligibility of a trial or particular treatment arms Median follow-up was calculated by the reverse Kaplan-Meier method,
within a trial, this was discussed and resolved by consensus within the Project based on surviving patients and using censoring as the event.
Secretariat and International Advisory Group. We did not search for trials that
used long-term alkylating agents. These were included in the 1995 analyses,
but due to their antiquity, were not included in this update. RESULTS
Data Collection
For trials already included in the 1995 analyses, updated follow-up was A total of 19 potentially eligible trials that had used supportive care and
sought. Most of the trials previously provided mature data and we did not chemotherapy versus supportive care alone were identified. Data for
anticipate much additional information. However, some additional data were two trials14,15 were no longer available and for one trial,16 adequate
received and included in the new analyses. contact with the investigators could not be established.
For new trials, survival and baseline characteristics were sought for all Therefore, 16 trials that randomly assigned 2,714 patients were
patients randomly assigned into each trial. This included date of random- included (Table 1).10,17-29 These represent 84% of patients from all
ization, survival status, and date of last follow-up or death as well as
known randomized trials that compared supportive care and chemo-
information on date of birth, sex, performance status, tumor stage (TNM),
and histological type. therapy with supportive care alone and 65% more data than that
available in 1995. The 16 trials accrued between 32 to 447 patients.
Data Checking Characteristics of these trials are summarized in Table 1. Platinum-
A number of standard checks were applied to all new trials, including based chemotherapy was used in 12 trials (cisplatin in 11 and
checks for missing values and data validity and consistency across variables. To
assess the randomization integrity, we looked for unusual patterns in the
carboplatin in one25) and nonplatinum single agents (etoposide,
sequencing of allocation or imbalances in baseline characteristics between vinorelbine, gemcitabine, and paclitaxel) were used in four trials.
treatment arms. Follow-up of surviving patients was also assessed to ensure Patients’ characteristics for the 2,714 patients across all trials are
that it was balanced by treatment arm and as up-to-date as possible. Any presented in Table 2. Data for age and sex were provided for all trials.
4618 © 2008 by American Society of Clinical Oncology JOURNAL OF CLINICAL ONCOLOGY
Downloaded from jco.ascopubs.org by ALICIA HENAO URIBE on October 5, 2008 from 200.116.146.33.
Copyright © 2008 by the American Society of Clinical Oncology. All rights reserved.
Supportive Care and Chemotherapy in NSCLC
Table 1. Characteristics of Included Trials
Performance
No. of Maximum
Stage (%) Status (%) Histology (%) Age (%)
Inclusion Patients Chemotherapy Chemotherapy Dose No. of
Trial Period Accrued Used Per Cycle (mg/m2) Cycles I, II IIIa IIIb IV 0,1 ⱖ2 Squamous Adeno Other ⬍ 70 ⱖ 70
Using platinum ⫹
vinca-alkaloid/
etoposide
RLW 835117 1982-1986 167 Cisplatin 120 P/T 0 0 100 0 73 27 37 37 26 88 12
Vindesine 3
NCIC CTG BR518 1983-1986 150 Cisplatin 120 P/T 0 0 13 85 60 40 29 43 27 98 2
Vindesine 3
or
Cisplatin 40
Doxorubicin 40
Cyclophosphamide 400
Southampton17 1983-1986 32 Cisplatin 120 6 0 0 100 0 81 1 50 34 15 91 9
Vinblastine 3 15
NRH19 1983-1987 87 Cisplatin 70 4 0 2 0 48 60 40 40 39 21 89 11
Etoposide 100
20
Ancona 1 1985-1988 128 Cisplatin 80 P/T 0 0 41 59 88 12 NK NK NK 95 5
Cyclophosphamide 500
Epirubicin 50
alternating with
Methotrexate 30
Etoposide 200
Lomustine 70 (orally)
CEP-8522 1985-1988 49 Cisplatin 120 8 0 2 0 94 67 27 47 33 14 84 16
Vindesine 3 18
UCLA23 1984-1986 63 Cisplatin 120 P/T 0 0 0 100 67 10 40 54 6 63 11
Vinblastine 6
JLCSG25 1990-1995 48 Carboplatin 300 8 0ⴱ 0ⴱ 9ⴱ 91ⴱ NK NK NK NK NK 76 23
Etoposide 120 ⫻ 2
BLT110 1995-2001 477 Cisplatin 80 3 3 20 36 38 82 25 56 24 25 76 31
Vindesine 3⫻2
or
Cisplatin 80 3
Vinorelbine 30 ⫻ 2
or
Cisplatin 50 3
Mitomycin C 6
Vinblastine 6
Using other platinum
regimen
AOI-Udine21 1984-1986 102 Cisplatin 75 6 0 0 0 100 49 51 48 35 17 98 2
Mitomycin C 10
Cyclophophamide 400
MIC224 1988-1996 359 Cisplatin 50 4 NK NK NK NK 64 28 56 27 19 84 19
Mitomycin C 6
Ifosfamide 3 (g/m2)
BLT210 1995-2001 248 Cisplatin 50 3 2 30 30 36 71 19 46 22 19 56 33
Mitomycin C 6
Ifosfamide 3 (g/m2)
Using vinca-alkaloid/
etoposide only
Gwent 226 1982-1984 186 Etoposide 600 6 24 12 10 33 87 8 100 0 0 84 13
ELVIS27 1996-1997 161 Vinorelbine 30 ⫻ 2 6 0 1 15 60 63 21 36 29 26 ⬍1 84
Using anti-metabolic
agent only
Manchester 128 1994-1996 300 Gemcitabine 1,000 ⫻ 3 6 NK NK NK 40ⴱ 94 6 NK NK NK 69 31
Using taxane only
Manchester 229 1995-1997 157 Paclitaxel 200 P/T 0 0 45 55 81 19 47 29 20 66 34
NOTE. Totals may not add up to 100% due to missing/unknown data.
Abbreviations: Adeno, adenocarcinoma; NK, not known; P/T, until progression or toxicity; NCIC CTG, National Cancer Institute of Canada Clinical Trials Group; NRH,
Norwegian Radium Hospital; CEP-85, Cerce d’etudes pneumologiques; UCLA, University of California—Los Angeles; JLCSG, Joint Lung Cancer Study Group; BLT,
Big Lung Trial; AOI, Associazione Oncologia Italiana; MIC2, mitomycin, ifosfamide, and cisplatin; ELVIS, Elderly Lung Cancer Vinorebine Italian Study Group.
ⴱ
Information from publication not from data supplied.
www.jco.org © 2008 by American Society of Clinical Oncology 4619
Downloaded from jco.ascopubs.org by ALICIA HENAO URIBE on October 5, 2008 from 200.116.146.33.
Copyright © 2008 by the American Society of Clinical Oncology. All rights reserved.
Burdett et al
Table 2. Characteristics of Included Patients
Supportive Care Plus Chemotherapy Supportive Care Alone
Characteristic No. % No. %
Age, years
⬍ 60 509 36 448 34
60-64 259 19 236 18
65-69 274 20 272 21
⬎ 70 346 24 349 26
Unknown 11 ⬍1 10 ⬍1
Sex
Male 1,076 77 984 75
Female 313 22 322 24
Unknown 10 ⬍1 9 ⬍1
Histology
Adenocarcinoma 320 23 300 23
Squamous 605 43 554 42
Mixed 1 ⬍1 2 ⬍1
Large cell undifferentiated 96 7 73 5
NSC unspecified 22 1 36 3
Other 105 7 93 7
Unknown 39 3 40 3
Data not supplied 211 15 217 16
Stage
I 18 1 14 1
II 22 2 14 1
IIIa 92 7 106 8
IIIb 337 24 300 23
IV 508 36 466 35
Unknown 73 5 58 5
Data not supplied 349 25 357 27
Performance status
0 347 25 299 23
1 687 49 670 51
2 290 21 263 20
3 19 1 20 1
4 1 ⬍1 1 ⬍1
Unknown 33 2 36 2
Data not supplied 22 1 26 2
Abbreviation: NSC, non–small-cell.
Histology data were provided for 15 trials and performance status and Overall Survival
stage were supplied for 13 trials. Based on these available data, patients Survival analyses were based on 2,533 deaths and 2,714 patients
were mostly male, age between 60 and 70 years, with good perfor- from 16 trials. Figure 1 shows a highly statistically significant benefit of
mance status. Performance status was defined as good (WHO/Eastern chemotherapy on survival (HR, 0.77; 95% CI, 0.71 to 0.83; P ⬍ .0001)
Cooperative Oncology Group 0 or 1, Karnofsky 100 to 70) or poor translating to an absolute improvement of 9% at 12 months increasing
(WHO/Eastern Cooperative Oncology Group 2⫹, Karnofsky 60 survival from 20% to 29% or an absolute increase in median survival
or lower). of 1.5 months (from 4.5 months to 6 months). There was some
Of the stage data we received, 90% of patients had tumors that evidence of heterogeneity between the trials (P ⫽ .02; I2 ⫽ 47%).
were advanced (predominantly stage IIIb and IV). However, there was However, repeating the sensitivity analysis carried out in 1995,6 which
a small proportion (3%) of patients had stage I and II disease. This excluded the extreme results of CEP-8522 (49 patients) resulted in
appears to be because some trials10,26 did not restrict entry to advanced considerably lower heterogeneity (P ⫽ .275; I2 ⫽ 16%) with a similar
patients and these individuals were (presumably) randomly assigned effect of chemotherapy on overall survival (HR, 0.78; 95% CI, 0.72 to
because their condition precluded or the patient declined surgery or 0.85). Also, based on all trials, results using the random effects model
radical radiation therapy. were similar (HR, 0.75; 95% CI, 0.67 to 0.84; P ⬍ .0001). The survival
Most patients had squamous cell tumors (43%) or adenocarci- curve is shown in Figure 2.
nomas (23%), the proportion of these tumor types has not substan- There was no clear evidence of a difference in the effect of chem-
tially changed between 1995 and the current analysis. otherapy between chemotherapy types (Fig 1; P ⫽ .63) or between
The median follow-up for all surviving patients was 1 year 4 trials that used combination chemotherapy and those that used single
months (range, ⬍ 1 month to 9.5 years). agent chemotherapy (Table 3; P ⫽ .40).
4620 © 2008 by American Society of Clinical Oncology JOURNAL OF CLINICAL ONCOLOGY
Downloaded from jco.ascopubs.org by ALICIA HENAO URIBE on October 5, 2008 from 200.116.146.33.
Copyright © 2008 by the American Society of Clinical Oncology. All rights reserved.
Supportive Care and Chemotherapy in NSCLC
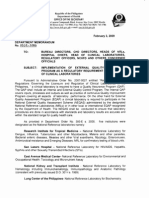
SC + CT SC alone
Trial Id. (no. events/no. entered) Hazard Ratio (fixed) 95% CI P value
Platinum + vinca alkaloid / etoposide
RLW 835117 84/86 80/81
NCIC CTG BR518 94/97 51/53
Southampton17 17/17 15/15
NRH19 44/44 40/43
Ancona 120 63/63 65/65
CEP-8522 23/25 21/24
UCLA23 31/32 30/31
BLT 110 222/237 233/240
JLCSG25 18/22 25/26
Subtotal 596/623 560/578 0.77 0.68 to 0.86 < .0001
Other platinum regimens
AOI-Udine21 52/52 50/50
MIC 224 177/179 179/180
BLT 210 123/127 119/121
Subtotal 352/358 348/351 0.73 0.63 to 0.85 < .0001
Vinca-alkaloid / etoposide only
Gwent226 96/111 67/75
ELVIS27 69/80 75/81
Subtotal 165/191 142/156 0.80 0.64 to 1.01 .057
Anti-metabolic agent only
Manchester 128 116/148 119/152
Subtotal 116/148 119/152 0.91 0.70 to 1.17 .466
Taxane only
Manchester 229 64/79 71/78
Subtotal 64/79 71/78 0.69 0.49 to 0.97 .032
Total 1,293/1,399 1,240/1,315 0.77 0.71 to 0.83 < .0001
0.0 0.5 1.0 1.5 2.0
SC + CT better SC alone better
Heterogeneity P = .02; I2 = 47; interaction P = .63
(Sensitivity analysis excluding CEP-85 heterogeneity P = .28; I2 = 16; interaction P = .62)
Fig 1. Hazard ratio plot of effect of chemotherapy on survival. Each trial is represented by a blue square, the center of which denotes the hazard ratio for that trial
with the horizontal lines showing the 99% and 95% CIs. The size of the square is directly proportional to amount of information in the trial. The red diamond gives the
overall hazard ratio for combined results of all trials; the center denotes the hazard ratio and the extremities the 95% CI. The yellow diamonds represent hazard ratios
for the trial groups; the center denotes the hazard ratio and the extremities the 95% CI. SC, supportive care; CT, chemotherapy; NCIC CTG, National Cancer Institute
of Canada Clinical Trials Group; NRH, Norwegian Radium Hospital; CEP-85, Cerce d’etudes pneumologiques; UCLA, University of California—Los Angeles; JLCSG, Joint
Lung Cancer Study Group; BLT, Big Lung Trial; AOI, Associazione Oncologia Italiana; MIC2, mitomycin, ifosfamide, and cisplatin; ELVIS, Elderly Lung Cancer Vinorebine
Italian Study Group.
Of the three trials that we could not include in these analyses, we noma or squamous cell histology. Despite these differences, there
could estimate a HR for survival30 for one trial16 of 207 patients. This was no evidence of a difference in effect of chemotherapy between
trial used single-agent docetaxel, had a reported P ⫽ .03 and gave a trials in the 1995 analysis and the recent trials (interaction P ⫽ .77)
very similar result (HR, 0.70; 95% CI, 0.51 to 0.95) to the included or between previous platinum-based trials and recent platinum-
trial29 that used a single-agent taxane (HR, 0.69; 95% CI, 0.49 to 0.97). based trials (interaction P ⫽ .64) (Table 3).
Since the 1995 meta-analysis, the patient demographic may
have changed, and so the effect of chemotherapy may also have Patient Subgroups
changed. Certainly, there was a higher proportion of patients older There was no clear evidence of a difference or trend in the relative
than 70 in the more recent trials, probably due to aging populations effect of chemotherapy in patient subgroups defined by age (P ⫽ .64),
and widening eligibility criteria, although all trials included pa- sex (P ⫽ .77), stage (P ⫽ .35), histology (P ⫽ .75), or performance
tients older than 70 years (Table 1). The median age of patients in status (P ⫽ .54; Fig 3). Furthermore, despite the difference in under-
the trials included since the 1995 analysis was higher (66 years old, lying survival by performance status, the absolute effect at 12 months
previously 61 years old), there were more women (28%, previously was fairly similar; 8% for performance status 0/Karnofsky 100 to 90
19%), and far more stage IIIa patients (16%, previously 3%). There (from 26% to 34%), 8% for 1/Karnofsky 80 to 70 (from 18% to 26%),
was no real change in the proportion of patients with adenocarci- and 6% for 2⫹/Karnofsky 60 or lower (from 8% to 14%).
www.jco.org © 2008 by American Society of Clinical Oncology 4621
Downloaded from jco.ascopubs.org by ALICIA HENAO URIBE on October 5, 2008 from 200.116.146.33.
Copyright © 2008 by the American Society of Clinical Oncology. All rights reserved.
Burdett et al
otherapy (P ⫽ .03) and another using vinorelbine27 is of borderline
1.0 Events Total significance (P ⫽ .06). The trial of single-agent docetaxel,16 that we
0.9 SC alone 1,240 1,315
0.8 SC + CT 1,293 1,399 could not include was also significantly in favor of chemotherapy
0.7 (P ⫽ .03).
Probability
0.6 In 1998, a meta-analysis that compared single agent and com-
0.5 bination chemotherapy in advanced NSCLC31 found that while the
0.4 response rate for patients receiving combination chemotherapy
0.3
was improved, overall survival was not significantly better. There
0.2
0.1 was also increased toxicity associated with combination chemo-
therapy. Similarly, this meta-analysis suggests no difference in
0 3 6 9 12 15 18 21 24 effect between trials using single-agent and combination chemo-
Time (months) therapy, however, our observation is an indirect comparison. Two
Patients at risk more recent literature-based meta-analyses32,33 both reported that
SC alone 1,315 884 552 363 231 161 107 77 55
SC + CT 1,399 1,052 779 519 349 233 165 115 91 two agents were more beneficial than one, but that three agents
were no more beneficial than two.33 It is important to remember
Fig 2. Simple (nonstratified) Kaplan-Meier curve for survival by treatment. SC,
supportive care; CT, chemotherapy. however, that these observations are based on indirect compari-
sons and the power to detect any differences is limited. Thus, this
conclusion should be interpreted with caution.
A number of trials have been completed or are still ongoing
DISCUSSION which compare newer agents, such as docetaxel and gemcitabine, in
combination or as single agents. One completed trial34 of carboplatin
Based on 16 trials and 2,714 patients, this systematic review and and paclitaxel versus paclitaxel alone suggested that although there
meta-analysis includes 65% more data than that available in 1995 was no evidence of a difference in effect between the treatments,
and represents the most comprehensive and reliable review of combination chemotherapy could be an option for those able to
chemotherapy in the supportive care setting. Results demonstrate a tolerate a more aggressive treatment.
substantial benefit of chemotherapy for advanced NSCLC, im- In the 1995 analysis, the platinum-based trials showed a 27%
proving survival by 9% at 12 months and median survival by 1.5
reduction in the risk of death equivalent to an increase in median
months. The benefit seen in new trials is consistent with that seen
survival of 1.5 months. This led to discussion about the impact on
previously, despite changes in the lung cancer population and drug
quality of life and whether the adverse effects of chemotherapy
regimens used over time.
were worthwhile for this relatively small increase in survival. At
We now have substantially more power to look at the effect of
chemotherapy in different groups of patients and can be more confi- that time, only two22,23 of the included trials had tried to measure
dent on these results than in 1995. Both the relative and absolute quality of life and both had failed to do so successfully. Although we
benefits of chemotherapy are remarkably consistent across patient did not collect quality of life data, three trials using platinum-based
subgroups, notably with benefits irrespective of age and perfor- chemotherapy10,24,25one using vinorelbine,27 one using gemcitab-
mance status. ine,28 and one using paclitaxel,29 which have been included since
In our meta-analysis, the effectiveness of newer drugs such as 1995, assessed quality of life. Of the trials we could not include, one
vinorelbine, paclitaxel, and gemcitabine, used as single agents ap- trial of docetaxel16 and one of platinum-based chemotherapy14
pears to be similar to that of platinum-based chemotherapy com- also assessed quality of life. All reported that quality of life was
bined with older agents, such as vindesine and mitomycin C, either no worse or improved for those patients receiving chemo-
potentially offering a greater range of treatment options and can- therapy. This suggests that platinum-based regimens and newer
didates for future trials. However, individually only one trial using agents could offer both improved survival and possibly better
single-agent paclitaxel29 is statistically significant in favor of chem- quality of life.
Table 3. Exploratory Analysis of the Effect of Chemotherapy on Survival
Trial Group No. of Trials No. of Patients Hazard Ratio 95% CI P P for Interaction
Period of trials (all trials) .77
All trials included in 1995 9 964 0.76 0.66 to 0.87 .0006
All trials included since 1995 6 1,750 0.77 0.70 to 0.86 ⬍ .0001
Period of trials (platinum-based trials) .64
Platinum-based trials included in 1995 8 778 0.73 0.63 to 0.85 ⬍ .0001
Platinum-based trials included since 1995 3 1,132 0.77 0.68 to 0.86 ⬍ .0001
Chemotherapy type (all trials) .40
Combination chemotherapy 11 1,910 0.75 0.68 to 0.83 ⬍ .0001
Single-agent chemotherapy 4 804 0.81 0.70 to 0.95 .008
4622 © 2008 by American Society of Clinical Oncology JOURNAL OF CLINICAL ONCOLOGY
Downloaded from jco.ascopubs.org by ALICIA HENAO URIBE on October 5, 2008 from 200.116.146.33.
Copyright © 2008 by the American Society of Clinical Oncology. All rights reserved.
Supportive Care and Chemotherapy in NSCLC
SC+CT SC alone
(no. events/no. entered) Hazard Ratio (fixed)
Age
< 60 429/456 368/382
60-64 275/299 267/289
Trend P = .64
65-69 243/268 253/267
≥ 70 336/365 344/367
Sex
Male 997/1,076 933/984
Female 287/313 301/322 Interaction P = .77
Stage
I & II 37/40 27/28
IIIa 86/92 101/106
IIIb 313/337 289/300 Trend P = .35
IV 477/508 451/466
Fig 3. Effect of chemotherapy on sur-
Histology
vival by age, sex, stage, histology, and
performance status.
Adenocarcinoma 302/320 295/300
Squamous cell 567/605 532/554
Interaction P = .75
Other 214/224 194/204
Performance Status
Good 946/1034 904/969
Interaction P = .54
Poor 298/310 279/284
Exploratory Analysis
Performance Status (WHO or Karnofsky)
0 or 100-90 310/347 273/299
1 or 80-70 636/687 631/670
Trend P = .76
2+ or ≤ 60 298/310 279/284
0.0 0.5 1.0 1.5 2.0
SC + CT better SC alone better
The current meta-analysis suggests that we do not need another quality of life. Therefore, all patients who are fit enough and wish to
trial of supportive care alone versus supportive care and chemother- receive chemotherapy, should do so.
apy. What we do need are more trials comparing third generation
chemotherapy combinations, doses, and duration, and also further
AUTHORS’ DISCLOSURES OF POTENTIAL CONFLICTS
research on toxicity and adverse effects. Recent trials have shown the OF INTEREST
efficacy of epidermal growth factor receptor tyrosine kinase inhibitors
in patients with advanced cancer35 who have relapsed after first-line Although all authors completed the disclosure declaration, the following
chemotherapy and so future trials may also exploit these encourag- author(s) indicated a financial or other interest that is relevant to the subject
ing developments. matter under consideration in this article. Certain relationships marked
This meta-analysis demonstrates conclusively that chemothera- with a “U” are those for which no compensation was received; those
relationships marked with a “C” were compensated. For a detailed
py increases overall survival for all types of patients with advanced
description of the disclosure categories, or for more information about
NSCLC and that there should be no change in the treatment para- ASCO’s conflict of interest policy, please refer to the Author Disclosure
digm. Evidence from trials that collected quality of life data also sug- Declaration and the Disclosures of Potential Conflicts of Interest section in
gests that this approach is unlikely to be detrimental to the patients’ Information for Contributors.
www.jco.org © 2008 by American Society of Clinical Oncology 4623
Downloaded from jco.ascopubs.org by ALICIA HENAO URIBE on October 5, 2008 from 200.116.146.33.
Copyright © 2008 by the American Society of Clinical Oncology. All rights reserved.
Burdett et al
Employment or Leadership Position: Thierry Le Chevalier, Collection and assembly of data: S. Burdett, L. Stewart
GlaxoSmithKline (U) Consultant or Advisory Role: None Stock Data analysis and interpretation: R. Arriagada, A. Auperin, D. Bell,
Ownership: None Honoraria: Richard Stephens, Pierre Fabre Oncology S. Burdett, G. Cartei, Y. Cormier, M. Cullen, P. Ganz, C. Gridelli,
Research Funding: Max Parmar, UK Medical Research Council; J. Higgins, D. Johnson, S. Kaasa, T. Le Chevalier, C. Le Pechoux,
Jean-Pierre Pignon, Sanofi-aventis; Richard Stephens, UK Medical M. Parmar, J.P. Pignon, E. Quoix, E. Rapp, L. Seymour, R. Souhami,
Research Council Expert Testimony: None Other Remuneration: None S. Spiro, R. Stephens, L. Stewart, N. Thatcher, J. Tierney, D.
Tummarello, J. van Meerbeeck, C. Williams, I. Williamson
AUTHOR CONTRIBUTIONS Manuscript writing: R. Arriagada, A. Auperin, S. Burdett, J. Higgins,
D. Johnson, T. Le Chevalier, C. Le Pechoux, M. Parmar, J.P. Pignon,
Conception and design: R. Arriagada, A. Auperin, S. Burdett, J. Higgins, R. Souhami, R. Stephens, L. Stewart, J. Tierney, J. van Meerbeeck
D. Johnson, T. Le Chevalier, C. Le Pechoux, M. Parmar, J.P. Pignon, Final approval of manuscript: R. Arriagada, A. Auperin, D. Bell,
R. Souhami, R. Stephens, L. Stewart, J. Tierney, J.P. van Meerbeeck S. Burdett, G. Cartei, Y. Cormier, M. Cullen, P. Ganz, C. Gridelli,
Administrative support: S. Burdett J. Higgins, D. Johnson, S. Kaasa, T. Le Chevalier, C. Le Pechoux,
Provision of study materials or patients: D. Bell, G. Cartei, Y. Cormier, M. Parmar, J.P. Pignon, E. Quoix, E. Rapp, L. Seymour, R. Souhami,
M. Cullen, P. Ganz, C. Gridelli, S. Kaasa, E. Quoix, E. Rapp, L. Seymour, S. Spiro, S. Spiro, R. Stephens, L. Stewart, N. Thatcher, J. Tierney, D.
R. Stephens, N. Thatcher, D. Tummarello, C. Williams, I. Williamson Tummarello, J. van Meerbeeck, C. Williams, I. Williamson
cancer: Best supportive care (BSC) versus BSC plus 25. Helsing M, Bergman B, Thaning L, et al:
REFERENCES chemotherapy. Lung Cancer 24:17-24, 1999 Quality of life and survival in patients with advanced
15. Gasparini S, Farabollini B, Isidori P, et al: non-small cell lung cancer receiving supportive care
1. Parkin DM, Bray F, Ferlay J, et al: Global Lonidamine, chemotherapy (cisplatin and etoposide) plus chemotherapy with carboplatin and etoposide
cancer statistics, 2002. CA Cancer J Clin 55:74-108, and chemotherapy plus lonidamine vs the best or supportive care only. A multicentre randomised
2005 supportive care in the treatment of advanced non- phase III trial. Eur J Cancer 34:1036-1044, 1998
2. Visbal AL, Leighl NB, Feld R, et al: Adjuvant small cell lung cancer (NSCLC): Preliminary results 26. Anderson G, Payne H: Response rate and
chemotherapy for early stage non-small cell lung of a randomised study. Lung Cancer 7:A383, 1991 toxicity of etoposide (VP-16) in squamous carcinoma
cancer. Chest 128:2933-2943, 2005 16. Roszkowski K, Pluzanska A, Krzakowski M, et of the lung: Report from the Lung Cancer Treatment
3. World Health Organization: Global cancer rates al: A multicenter, randomized, phase III study of Study Group. Semin Oncol 12:21-22, 1985 (suppl 2)
could increase by 50% to 15 million by 2020. http:// docetaxel plus best supportive care versus best 27. Elderly Lung Cancer Vinorelbine Italian Study
www . who . int / mediacentre / news / releases/2003/ supportive care in chemotherapy-naı̈ve patients with Group: Effect of vinorelbine on quality of life and
pr27/en/ metastatic or non-resectable localized non-small cell survival of elderly patients with advanced non-small
4. Greenlee RT, Murray T, Bolden S, et al: Can- lung cancer. Lung Cancer 27:145-157, 2000 cell lung cancer. J Natl Cancer Inst 91:66-72, 1999
cer Statistics, 2000. CA Cancer J Clin 50:7-33, 2000 17. Woods RL, Williams CJ, Levi J, et al: A 28. Anderson H, Hopwood P, Stephens RJ, et al:
5. Rudd R: Chemotherapy in the treatment of randomised trial of cisplatin and vindesine versus Gemcitabine plus best supportive care (BSC) vs BSC
non-small cell lung cancer. Respiratory Disease in supportive care only in advanced non-small cell lung in inoperable non-small cell lung cancer: A random-
Practice 7:12-14, 1991 cancer. Br J Cancer 61:608-611, 1990 ized trial with quality of life as the primary outcome.
6. Non-Small Cell Lung Cancer Collaborative 18. Rapp E, Pater JL, Willan A, et al: Chemother- Br J Cancer 83: 447-453, 2000
Group: Chemotherapy in non-small cell lung cancer: apy can prolong survival in patients with advanced 29. Ranson M, Davidson N, Nicolson M, et al:
A meta-analysis using updated data on individual non-small cell lung cancer: Report of a Canadian Randomized trial of paclitaxel plus supportive care
patients from 52 randomised clinical trials. BMJ multicenter randomized trial. J Clin Oncol 6:633-641, versus supportive care for patients with advanced
311:899-909, 1995 1988 non-small cell lung cancer. J Natl Cancer Inst 92:
7. Burdett S, Pignon JP, Stewart L: Chemother- 19. Kaasa S, Lund E, Thorud E, et al: Symptomatic 1074-1080, 2000
apy in non-small cell lung cancer: An update of an treatment versus combination chemotherapy for 30. Parmar MKB, Torri V, Stewart L: Extracting
IPD meta-analysis. J Thorac Cardiovasc Surg 129: patients with extensive non-small cell lung cancer. summary statistics to perform meta-analyses of the
1205, 2005 Cancer 67:2443-2447, 1991 published literature for survival endpoints. Stat Med
8. Dickersin K, Scherer R, Lefebvre C: Identify- 20. Cellerino R, Tummarello D, Guidi F, et al: A 17:2815-2834, 1998
ing relevant studies for systematic reviews. BMJ randomized trial of alternating chemotherapy versus 31. Lilenbaum RC, Langenberg P, Dickersin K:
309:1286-1291, 1994 best supportive care in advanced non-small cell lung Single agent versus combination chemotherapy in
9. Yusuf S, Peto R, Lewis J, et al: Beta blockade cancer. J Clin Oncol 9:1453-1461, 1991 patients with advanced non-small cell lung carci-
during and after myocardial infarction: An overview 21. Cartei G, Cartei F, Cantone A, et al: Cisplatin- noma. Cancer 82:116-126, 1998
of the randomized trials. Prog Cardiovasc Dis 27: cyclophosphamide-mitomycin combination chemo- 32. Hotta K, Matsuo K, Ueoka H, et al: Addition of
335-371, 1985 therapy with supportive care versus supportive care platinum compounds to a new agent in patients with
10. Spiro SG, Rudd RM, Souhami RL, et al: Chem- alone for treatment of metastatic non-small cell lung advanced non-small cell lung cancer: A literature
otherapy versus supportive care in advanced non- cancer. J Natl Cancer Inst 85:794-800, 1993 based meta-analysis of randomised trials. Ann Oncol
small cell lung cancer: Improved survival without 22. Quoix É, Dietemann A, Charbonneau J, et al: 15:1782-1789, 2004
detriment to quality of life. Thorax 59:828-836, 2004 Is cisplatinum-based chemotherapy useful in dis- 33. Delbaldo C, Michiels S, Syz N, et al: Benefits
11. Parmar MKB, Machin D: Survival Analysis: A seminated non–small-cell lung cancer? Report of a of adding a drug to a single-agent or a 2-agent
Practical Approach. Chichester, John Wiley and French multicenter randomized trial [in French]. Bull chemotherapy regimen in advanced non-small cell
Sons Ltd, 1995 Cancer 78:341-346, 1991 lung cancer. JAMA 292:470-484, 2004
12. Higgins JPT, Thompson SG, Deeks JJ, et al: 23. Ganz PA, Figlin RA, Haskell CM, et al: Sup- 34. Lilenbaum RC, Herndon JE II, List MA, et al:
Measuring inconsistency in meta-analyses. BMJ portive care versus supportive care and combination Single agent versus combination chemotherapy in
327:557-560, 2003 chemotherapy in metastatic non-small cell lung can- advanced non-small cell lung cancer: The Cancer
13. Kaplan EL, Meier P: Nonparametric estima- cer. Does chemotherapy make a difference? Cancer and Leukemia Group B (study 9730). J Clin Oncol
tion from incomplete observation. Journal of the 63:1271-1278, 1989 23:190 196, 2005
American Statistical Association 53:457-481, 1958 24. Cullen MH, Billingham LJ, Woodroffe CM, et 35. Gridelli C, Bareschino MA, Schettino C, et al:
14. Thongprasert S, Sanguanmitra P, Juthapan al: Mitomycin, ifosfamide and cisplatin in resectable Erlotinib in non-small cell lung cancer treatment:
W, et al: Relationship between quality of life and non-small cell lung: Effects on survival and quality of Current status and future development. The Oncol-
clinical outcomes in advanced non-small cell lung life. J Clin Oncol 17:3188-3194, 1999 ogist 12:840-849, 2007
■ ■ ■
4624 © 2008 by American Society of Clinical Oncology JOURNAL OF CLINICAL ONCOLOGY
Downloaded from jco.ascopubs.org by ALICIA HENAO URIBE on October 5, 2008 from 200.116.146.33.
Copyright © 2008 by the American Society of Clinical Oncology. All rights reserved.
Supportive Care and Chemotherapy in NSCLC
Acknowledgment
The NSCLC Meta-Analyses Collaborative Group (composition below) thanks all patients who took part in the trials and contributed to this
research. The meta-analysis would not have been possible without their participation or without the collaborating institutions that provided their
trial data.
The meta-analysis was funded by the United Kingdom Medical Research Council.
NSCLC Meta-Analyses Collaborative Group
Project Management Group
Medical Research Council (MRC) Clinical Trials Unit, London, United Kingdom
S. Burdett, R. Stephens, L. Stewart, J. Tierney
Institut Gustave-Roussy, Villejuif, France
A. Auperin, T. Le Chevalier, C. Le Pechoux, J.P. Pignon
International Advisory Group
R. Arriagada, Karolinska Institutet, Stockholm, Sweden and Institut Gustave-Roussy, Villejuif, France
J. Higgins, MRC Biostatistics Unit, Cambridge, United Kingdom
D. Johnson, Vanderbilt-Ingram Cancer Center, Nashville, TN
J. van Meerbeeck, University Hospital, Ghent, Belgium
M. Parmar, MRC Clinical Trials Unit, London, United Kingdom
R. Souhami, Cancer Research United Kingdom, London, United Kingdom
Collaborators who supplied individual patient data
D. Bell, Royal North Shore Hospital, St Leonards, New South Wales, Australia
G. Cartei, International Academy of Environmental Sciences, Venice, Italy
Y. Cormier, Hospital Laval, Sainte-Foy, Quebec, Canada
M. Cullen, Queen Elizabeth Hospital, Birmingham, United Kingdom
P. Ganz, Schools of Medicine and Public Health, University of California, Los Angeles, Los Angeles, CA
C. Gridelli, SG Moscati Hospital, Avellino, Italy
S. Kaasa, University Hospital, Trondheim, Norway
E. Quoix, Service de Pneumologie, Strasbourg, France
E. Rapp (Retired), University of California-Los Angeles, Tom Baker Cancer Centre, Calgary, Alberta, Canada
L. Seymour, National Cancer Institute of Canada Clinical Trials Group, Queens University, Kingston, Ontario, Canada
S. Spiro, University College Hospital, London, United Kingdom
N. Thatcher, Christie Hospital, Manchester, United Kingdom
D. Tummarello, Universita Delgi Studi de Ancona, Ancona, Italy
C. Williams, Bristol Hematology and Oncology Centre, Bristol, United Kingdom
I. Williamson, Newport Chest Clinic, Newport, United Kingdom
www.jco.org © 2008 by American Society of Clinical Oncology 4625
Downloaded from jco.ascopubs.org by ALICIA HENAO URIBE on October 5, 2008 from 200.116.146.33.
Copyright © 2008 by the American Society of Clinical Oncology. All rights reserved.
Potrebbero piacerti anche
- The Secret of The House WTDocumento22 pagineThe Secret of The House WTPetr -50% (2)
- Rreinforcement Pad Leak Test ProcedureDocumento5 pagineRreinforcement Pad Leak Test ProcedureAmin Thabet100% (2)
- Beethoven Piano Sonata Op. 57 N. 23Documento29 pagineBeethoven Piano Sonata Op. 57 N. 23GiancarloNessuna valutazione finora
- EO On Ban of Fireworks (Integrated)Documento2 pagineEO On Ban of Fireworks (Integrated)Mario Roldan Jr.Nessuna valutazione finora
- Mufon Ufo JournalDocumento21 pagineMufon Ufo JournalSAB78Nessuna valutazione finora
- HR Policy For Hotel IndustriesDocumento5 pagineHR Policy For Hotel IndustriesHR Forum India78% (9)
- Fundamentals of Fast SwimmingDocumento9 pagineFundamentals of Fast SwimmingTorcay Ulucay100% (1)
- Siemens MV Gas Insulated Switch GearDocumento14 pagineSiemens MV Gas Insulated Switch GearSajesh Thykoodan T VNessuna valutazione finora
- Cot 1 Vital SignsDocumento22 pagineCot 1 Vital Signscristine g. magatNessuna valutazione finora
- BCM Continuous ImprovementDocumento22 pagineBCM Continuous ImprovementnikoNessuna valutazione finora
- Neoadjuvant Chemoradiotherapy Followed by Surgery VersusDocumento15 pagineNeoadjuvant Chemoradiotherapy Followed by Surgery VersusRaul Matute MartinNessuna valutazione finora
- MR23002 D Part Submission Warrant PSWDocumento1 paginaMR23002 D Part Submission Warrant PSWRafik FafikNessuna valutazione finora
- CPCNP MTXDocumento9 pagineCPCNP MTXMary CogolloNessuna valutazione finora
- Cisplatin-Based Adjuvant Chemotherapy in Patients With Completely Resected Non-Small-Cell Lung CancerDocumento10 pagineCisplatin-Based Adjuvant Chemotherapy in Patients With Completely Resected Non-Small-Cell Lung CancerSouvik SahaNessuna valutazione finora
- Palliative Chemotherapy For Advanced Colorectal Cancer Systemati 2000Documento5 paginePalliative Chemotherapy For Advanced Colorectal Cancer Systemati 2000Wiro SablengNessuna valutazione finora
- A Genomic StrategyDocumento11 pagineA Genomic StrategyAmirahShalehaNessuna valutazione finora
- Prediction Model For Shortterm Mortality After Palliative Therapy For Patients Having Advanced Cancer - A Cohort Study From Routine Electronic Medical DataDocumento10 paginePrediction Model For Shortterm Mortality After Palliative Therapy For Patients Having Advanced Cancer - A Cohort Study From Routine Electronic Medical DataHollis LukNessuna valutazione finora
- NeutropeniaDocumento17 pagineNeutropeniaassajadda lizikriNessuna valutazione finora
- 10 Anos Cross Trial Jco2021Documento11 pagine10 Anos Cross Trial Jco2021alomeletyNessuna valutazione finora
- Concurrent Cisplatin, Etoposide, and Chest Radiotherapy in Pathologic Stage IIIB Non-Small-Cell Lung CancerDocumento7 pagineConcurrent Cisplatin, Etoposide, and Chest Radiotherapy in Pathologic Stage IIIB Non-Small-Cell Lung Cancerdurgesh kumarNessuna valutazione finora
- Treatment of The Elderly When Cure Is The GoalDocumento8 pagineTreatment of The Elderly When Cure Is The GoalCatia AraujoNessuna valutazione finora
- Nejmoa 1112088Documento11 pagineNejmoa 1112088Med MedNessuna valutazione finora
- Review: Second Consensus On Medical Treatment of Metastatic Breast CancerDocumento11 pagineReview: Second Consensus On Medical Treatment of Metastatic Breast Cancermohit.was.singhNessuna valutazione finora
- Clinical Impact of External Radiotherapy in Non-Metastatic Esophageal Cancer According To Histopathological SubtypeDocumento12 pagineClinical Impact of External Radiotherapy in Non-Metastatic Esophageal Cancer According To Histopathological SubtypesilviailieNessuna valutazione finora
- Landoni 2019Documento12 pagineLandoni 2019t88frb5kqrNessuna valutazione finora
- First-Line Treatment of Metastatic Renal Cell Carcinoma: A Systematic Review and Network Meta-AnalysisDocumento8 pagineFirst-Line Treatment of Metastatic Renal Cell Carcinoma: A Systematic Review and Network Meta-AnalysisDr. Alexandre SatoNessuna valutazione finora
- Farmakopunktur Pada KankerDocumento15 pagineFarmakopunktur Pada KankerYoshua ViventiusNessuna valutazione finora
- 2021 Consolidation Theraphy in Esophageal CancerDocumento6 pagine2021 Consolidation Theraphy in Esophageal CancerykommNessuna valutazione finora
- JournalReading ONKO JeffriSyaputraDocumento17 pagineJournalReading ONKO JeffriSyaputraYarman War officialNessuna valutazione finora
- Estudio CarmenaDocumento11 pagineEstudio CarmenaAlfredo BalcázarNessuna valutazione finora
- Neoadjuvant Chemotherapy Vs Upfront Surgery For Gastric Signet Ring Cell Carcinoma A Retrospective, Propensity Score-Matched StudyDocumento11 pagineNeoadjuvant Chemotherapy Vs Upfront Surgery For Gastric Signet Ring Cell Carcinoma A Retrospective, Propensity Score-Matched StudyLITTLESWEETKILLERNessuna valutazione finora
- wenzel2005Documento8 paginewenzel2005cikox21848Nessuna valutazione finora
- 1857 FullDocumento6 pagine1857 FullTahniat AishaNessuna valutazione finora
- The Role of Surgery in The Palliative Care of Cancer A Retrospective Analysis of 22 YearsDocumento6 pagineThe Role of Surgery in The Palliative Care of Cancer A Retrospective Analysis of 22 YearsAthenaeum Scientific PublishersNessuna valutazione finora
- The Pattern of Antimicrobial Use For Palliative Care In-Patients During The Last Week of LifeDocumento4 pagineThe Pattern of Antimicrobial Use For Palliative Care In-Patients During The Last Week of Lifem1k0eNessuna valutazione finora
- Systemic Therapy For Advanced Appendiceal Adenocarcinoma: An Analysis From The NCCN Oncology Outcomes Database For Colorectal CancerDocumento8 pagineSystemic Therapy For Advanced Appendiceal Adenocarcinoma: An Analysis From The NCCN Oncology Outcomes Database For Colorectal Canceralberto cabelloNessuna valutazione finora
- Prognostic Factors in Nasopharyngeal Carcinoma With Synchronous Liver Metastasis: A Retrospective Study For The Management of TreatmentDocumento7 paginePrognostic Factors in Nasopharyngeal Carcinoma With Synchronous Liver Metastasis: A Retrospective Study For The Management of TreatmentChairul Nurdin AzaliNessuna valutazione finora
- Neoadjuvant Chemotherapy Versus Neoadjuvant Chemoradiotherapy For Cancer of The Esophagus or The Gastroesophageal Junction A Meta-Analysis Based On Clinical TrialsDocumento19 pagineNeoadjuvant Chemotherapy Versus Neoadjuvant Chemoradiotherapy For Cancer of The Esophagus or The Gastroesophageal Junction A Meta-Analysis Based On Clinical TrialsChendil VNessuna valutazione finora
- CANCER UPDATE Clinical Stem Cell Document - Alex Mou & Ryan TangDocumento7 pagineCANCER UPDATE Clinical Stem Cell Document - Alex Mou & Ryan Tangalexmou2008Nessuna valutazione finora
- Jurnal Divisi OnkologiDocumento19 pagineJurnal Divisi OnkologiAtika PusparaniNessuna valutazione finora
- Ournal of Linical Ncology: PurposeDocumento7 pagineOurnal of Linical Ncology: PurposeIvor Wiguna Hartanto WilopoNessuna valutazione finora
- Walk 2020Documento19 pagineWalk 2020Marcus ShawNessuna valutazione finora
- MeduloblastomaDocumento7 pagineMeduloblastomasilvia erfanNessuna valutazione finora
- Pembrolizumab For Previously TreatedDocumento11 paginePembrolizumab For Previously Treatedalex.losadaNessuna valutazione finora
- Immunotherapy and Biomarker Testing in Recurrent and Metastatic Head and Neck Cancers: ASCO GuidelineDocumento17 pagineImmunotherapy and Biomarker Testing in Recurrent and Metastatic Head and Neck Cancers: ASCO GuidelineDrDeepak MittalNessuna valutazione finora
- Lung Stereotactic Ablative Body Radiotheray SABR - Patient o - 2019 - ClinicalDocumento1 paginaLung Stereotactic Ablative Body Radiotheray SABR - Patient o - 2019 - ClinicalSENessuna valutazione finora
- AsdasdDocumento10 pagineAsdasdAdhi PratamaNessuna valutazione finora
- Aoun 2015Documento10 pagineAoun 2015skribekbenjaminNessuna valutazione finora
- Cancers 14 02775Documento22 pagineCancers 14 02775SiscaNessuna valutazione finora
- Jco 2007 14Documento13 pagineJco 2007 14api-3821924100% (2)
- The Comparison of Surgery and Chemo-Radio Therapy in Locally Recurrent Colorectal CancerDocumento4 pagineThe Comparison of Surgery and Chemo-Radio Therapy in Locally Recurrent Colorectal CancerInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- Debiri 1Documento12 pagineDebiri 1paquidermo85Nessuna valutazione finora
- (583950958) Journal Leucopenia Treatment Effiicacy NPCDocumento8 pagine(583950958) Journal Leucopenia Treatment Effiicacy NPCDaniel HoseaNessuna valutazione finora
- Clin Cancer Res-2010-Tabchy-Evaluation of A 30-Gene Paclitaxel, Fluorouracil, Doxorubicin, and Cyclophosphamide Chemotherapy Response Predictor in A Multicenter Randomized Trial in Breast CancerDocumento11 pagineClin Cancer Res-2010-Tabchy-Evaluation of A 30-Gene Paclitaxel, Fluorouracil, Doxorubicin, and Cyclophosphamide Chemotherapy Response Predictor in A Multicenter Randomized Trial in Breast CancerOncology FatmawatiNessuna valutazione finora
- UntitledDocumento26 pagineUntitledAounAbdellahNessuna valutazione finora
- TCA-12-2161Documento9 pagineTCA-12-2161hafidisara05Nessuna valutazione finora
- Kanker TumorDocumento11 pagineKanker TumorRENTI NOVITANessuna valutazione finora
- 10.12921 cmst.2006.12.02.143-147 MoczkoDocumento5 pagine10.12921 cmst.2006.12.02.143-147 Moczkoshital shermaleNessuna valutazione finora
- Neadyuvancia Cancer de Pene 1Documento5 pagineNeadyuvancia Cancer de Pene 1Ivan Perez NestaresNessuna valutazione finora
- Grothey 2004Documento6 pagineGrothey 2004api-26302710Nessuna valutazione finora
- Immunotherapy Expands Lung Cancer Treatment Options - National Cancer InstituteDocumento4 pagineImmunotherapy Expands Lung Cancer Treatment Options - National Cancer InstitutePongwirat ChantasoontornNessuna valutazione finora
- Desktop IiiDocumento9 pagineDesktop IiihenryNessuna valutazione finora
- 127 FullDocumento19 pagine127 FullKai ParaneeNessuna valutazione finora
- Asco GCSF 2015Documento16 pagineAsco GCSF 2015Alvy SyukrieNessuna valutazione finora
- BJU International - 2021 - Ravi - Optimal Pathological Response After Neoadjuvant Chemotherapy For Muscle Invasive BladderDocumento8 pagineBJU International - 2021 - Ravi - Optimal Pathological Response After Neoadjuvant Chemotherapy For Muscle Invasive BladderMajdNessuna valutazione finora
- 1 s2.0 S1083879111002916 MainDocumento8 pagine1 s2.0 S1083879111002916 MainNunungTriwahyuniNessuna valutazione finora
- Eighth Edition of The AJCC Cancer Staging Manual: Breast CancerDocumento3 pagineEighth Edition of The AJCC Cancer Staging Manual: Breast CancerRamona PalalogosNessuna valutazione finora
- Allen2021 Article ChemotherapyVersusChemotherapyDocumento8 pagineAllen2021 Article ChemotherapyVersusChemotherapyXavier QuinteroNessuna valutazione finora
- 1094 FullDocumento6 pagine1094 FullGuido ABNessuna valutazione finora
- Essentail Drugs For Cancer PIIS0923753419571502Documento6 pagineEssentail Drugs For Cancer PIIS0923753419571502Wadood Md ZahedNessuna valutazione finora
- Clinical Applications of Nuclear Medicine Targeted TherapyDa EverandClinical Applications of Nuclear Medicine Targeted TherapyEmilio BombardieriNessuna valutazione finora
- Post ASCO2009Documento51 paginePost ASCO2009api-26302710Nessuna valutazione finora
- CLAGDocumento8 pagineCLAGapi-26302710Nessuna valutazione finora
- Vorinostat CTCLLandmark Study 02Documento7 pagineVorinostat CTCLLandmark Study 02api-26302710Nessuna valutazione finora
- Everolimus RCCDocumento8 pagineEverolimus RCCapi-26302710Nessuna valutazione finora
- Ncologist: R I FDADocumento7 pagineNcologist: R I FDAapi-26302710Nessuna valutazione finora
- Terapia Sistémica en Carcinoma Metastásico de Colon Y Recto: Mauricio Lema Medina MDDocumento14 pagineTerapia Sistémica en Carcinoma Metastásico de Colon Y Recto: Mauricio Lema Medina MDapi-26302710Nessuna valutazione finora
- PACCE01Documento9 paginePACCE01api-26302710Nessuna valutazione finora
- GCis in Bladder Cancer 2006Documento5 pagineGCis in Bladder Cancer 2006api-26302710Nessuna valutazione finora
- Terapia Sistémica en Carcinoma Metastásico de Colon Y Recto: Mauricio Lema Medina MDDocumento14 pagineTerapia Sistémica en Carcinoma Metastásico de Colon Y Recto: Mauricio Lema Medina MDapi-26302710Nessuna valutazione finora
- Mycosis Fungoides and Sézary Syndrome: SeminarDocumento13 pagineMycosis Fungoides and Sézary Syndrome: Seminarapi-26302710Nessuna valutazione finora
- Adjuvant Imatinib GISTDocumento8 pagineAdjuvant Imatinib GISTapi-26302710Nessuna valutazione finora
- Nature 07762Documento6 pagineNature 07762api-26302710Nessuna valutazione finora
- For Refractory Cutaneous T-Cell Lymphoma (CTCL) Phase 2 Trial of Oral Vorinostat (Suberoylanilide Hydroxamic Acid, SAHA)Documento10 pagineFor Refractory Cutaneous T-Cell Lymphoma (CTCL) Phase 2 Trial of Oral Vorinostat (Suberoylanilide Hydroxamic Acid, SAHA)api-26302710Nessuna valutazione finora
- Nature 07485Documento7 pagineNature 07485api-26302710Nessuna valutazione finora
- Nature 07567Documento7 pagineNature 07567api-26302710Nessuna valutazione finora
- Letters: Regulation of ERBB2 by Oestrogen receptor-PAX2 Determines Response To TamoxifenDocumento6 pagineLetters: Regulation of ERBB2 by Oestrogen receptor-PAX2 Determines Response To Tamoxifenapi-26302710Nessuna valutazione finora
- Letters: Carcinoma-Produced Factors Activate Myeloid Cells Through TLR2 To Stimulate MetastasisDocumento6 pagineLetters: Carcinoma-Produced Factors Activate Myeloid Cells Through TLR2 To Stimulate Metastasisapi-26302710Nessuna valutazione finora
- Nature 07423Documento7 pagineNature 07423api-26302710Nessuna valutazione finora
- Nature 07385Documento8 pagineNature 07385api-26302710Nessuna valutazione finora
- IL2 in MRCCDocumento9 pagineIL2 in MRCCapi-26302710Nessuna valutazione finora
- Letters: Epigenetic Silencing of Tumour Suppressor Gene p15 by Its Antisense RNADocumento6 pagineLetters: Epigenetic Silencing of Tumour Suppressor Gene p15 by Its Antisense RNAapi-26302710Nessuna valutazione finora
- Guidelines Interleukin-2 For Safe AdministrationDocumento7 pagineGuidelines Interleukin-2 For Safe Administrationapi-26302710Nessuna valutazione finora
- EditorialDocumento1 paginaEditorialapi-26302710Nessuna valutazione finora
- Ncologist: T C O D O F SDocumento12 pagineNcologist: T C O D O F Sapi-26302710Nessuna valutazione finora
- CaScreening2009 01Documento16 pagineCaScreening2009 01api-26302710Nessuna valutazione finora
- Aldesleukin For Injection RX Only: DescriptionDocumento16 pagineAldesleukin For Injection RX Only: Descriptionapi-26302710Nessuna valutazione finora
- Proleukin Melanoma Evidencia en 270 Pacientes Con Dosis AltasDocumento12 pagineProleukin Melanoma Evidencia en 270 Pacientes Con Dosis Altasapi-26302710Nessuna valutazione finora
- Guias para Administrar en Forma Segura Altas Dosis de Interleukina 2007Documento2 pagineGuias para Administrar en Forma Segura Altas Dosis de Interleukina 2007api-26302710Nessuna valutazione finora
- Neo Adjuvant CTin LACervical CancerDocumento10 pagineNeo Adjuvant CTin LACervical Cancerapi-26302710Nessuna valutazione finora
- Akshaya Trust NgoDocumento24 pagineAkshaya Trust NgodushyantNessuna valutazione finora
- MLS 321 Aubf M6u2 Other Metabolic Diseases V2122Documento7 pagineMLS 321 Aubf M6u2 Other Metabolic Diseases V2122proximusNessuna valutazione finora
- Apc 8x Install Config Guide - rn0 - LT - enDocumento162 pagineApc 8x Install Config Guide - rn0 - LT - enOney Enrique Mendez MercadoNessuna valutazione finora
- Gate Installation ReportDocumento3 pagineGate Installation ReportKumar AbhishekNessuna valutazione finora
- Vturn-NP16 NP20Documento12 pagineVturn-NP16 NP20José Adalberto Caraballo Lorenzo0% (1)
- High-pressure dryers for PET bottle production and industrial applicationsDocumento3 pagineHigh-pressure dryers for PET bottle production and industrial applicationsAnonymous 6VCG1YRdNessuna valutazione finora
- Philippines implements external quality assessment for clinical labsDocumento2 paginePhilippines implements external quality assessment for clinical labsKimberly PeranteNessuna valutazione finora
- Characteristics of Uveitis Presenting For The First Time in The Elderly Analysis of 91 Patients in A Tertiary CenterDocumento9 pagineCharacteristics of Uveitis Presenting For The First Time in The Elderly Analysis of 91 Patients in A Tertiary CenterFrancescFranquesaNessuna valutazione finora
- PERSONS Finals Reviewer Chi 0809Documento153 paginePERSONS Finals Reviewer Chi 0809Erika Angela GalceranNessuna valutazione finora
- TA-Ingles IX - UAPDocumento10 pagineTA-Ingles IX - UAPmanuel brennerNessuna valutazione finora
- Ensure Even Preload with Proper Tightening Tools and SequenceDocumento2 pagineEnsure Even Preload with Proper Tightening Tools and SequenceMachineryengNessuna valutazione finora
- Request For Review FormDocumento11 pagineRequest For Review FormJoel MillerNessuna valutazione finora
- M-LVDT: Microminiature Displacement SensorDocumento2 pagineM-LVDT: Microminiature Displacement Sensormahdi mohammadiNessuna valutazione finora
- Micdak BackgroundDocumento3 pagineMicdak Backgroundappiah ernestNessuna valutazione finora
- Notice: Use of Segways® and Similar Devices by Individuals With A Mobility Impairment in GSA-Controlled Federal FacilitiesDocumento2 pagineNotice: Use of Segways® and Similar Devices by Individuals With A Mobility Impairment in GSA-Controlled Federal FacilitiesJustia.comNessuna valutazione finora
- Measure BlowingDocumento52 pagineMeasure BlowingLos Ángeles Customs GarageNessuna valutazione finora
- Aplikasi Berbagai Jenis Media Dan ZPT Terhadap Aklimatisasi Anggrek VandaDocumento15 pagineAplikasi Berbagai Jenis Media Dan ZPT Terhadap Aklimatisasi Anggrek VandaSihonoNessuna valutazione finora
- AYUSHMAN BHARAT Operationalizing Health and Wellness CentresDocumento34 pagineAYUSHMAN BHARAT Operationalizing Health and Wellness CentresDr. Sachendra Raj100% (1)
- Position paper-MUNUCCLE 2022: Refugees) Des États !Documento2 paginePosition paper-MUNUCCLE 2022: Refugees) Des États !matNessuna valutazione finora
- Jounce Therapeutics Company Events and Start DatesDocumento48 pagineJounce Therapeutics Company Events and Start DatesEquity NestNessuna valutazione finora