Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Case Study of Public Private Partnership in Uttarakhand State-Verma Surabhi, Garg Shilpa
Caricato da
eletsonlineDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Case Study of Public Private Partnership in Uttarakhand State-Verma Surabhi, Garg Shilpa
Caricato da
eletsonlineCopyright:
Formati disponibili
This papei was submitteu foi eW0RLBF0R0N confeience Page
CASL S1UD CI U8LIC kIVA1L Ak1NLkSnI IN U11AkAknAND S1A1L
Authors: Verma Surabhi; Garg Shilpa
Background:
%he origin oI PPP is since last three decades. Since 1990 onwards , PPP is an essential Iinancing
tool and has grown in all developed and developing economies. As such there is no single
deIinition Ior PPP. Every country`s approach to meet its policy objectives. It is a contractual
partnership between public and private sector to deliver services traditionally the domain oI
public sector Iinancing, designing ,implementing and operating inIrastructure Iacilities/service.
According to WHO,PPP is a means to bring together a set oI actors Ior the common goal oI
improving the health oI the population based on mutually agreeable goals and principals.WHO
deIined health sector reIorms and included 'collaboration with the private sector as one oI the
strategies in health reIorms. Other strategies are alternative Iinancing,institutional management
and public sector reIorms. %he two partners involved are public sector which may involve
national government, district administration, local government bodies,state universities and
research organization. %he private partner can be commercial Ior proIit enterprises, Development
Iocused organization,co-operative societies, community based organizations and proIessional
organizations.%here are various models involved in PPP which are common in various Iields like
social marketing,lease voucher system,subsidies ,jointventures and technology demos. However
,some oI the key types encountered in healthsectors are Contracting out, Service contracts,
Management contracts, Construction, maintenance, and equipment contracts Hybrid contracts
(e.g., large I% inIrastructure and service contracts, Leases,Concessions Backed by government
,guarantees/other Iiscal incentives, Supported by government or third party purchase contracts,
Free-standing ,Private Financing Initiatives and Other types, typically without government
guarantees, including: Divestiture/privatization,Free entry and a Iew others. Partnering with the
private sector carries the potential Ior meaningIul beneIits to begained Ior the public partner and
the health sector.
This papei was submitteu foi eW0RLBF0R0N confeience Page
dvantages and disadvantages:
Potential beneIits can include reduced government spending (e.g., eliminating large up-Iront
investments oI scarce public Iunds), greater eIIiciency by design/build with Iinancing single
entity responsible Ior design,build Iinance and O $M, better healthcare management (e.g., oI
hospital services and inIrastructure, leveraging technical or management expertise in
collaboration with private clan(e.g.,innovative methods, perIormance-based monitoring and
incentives),optimum allocation oI risk and management, value Ior money Ior the tax-
payer,speedy eIIicient and cost eIIective competitive public service delivery and spurring
technology transIer, all oI which can lead to quality improvements.However ,PPP has to Iace
many ethical ,operational and process related challenges with regard to global norms and
principals,Impartiality in health,global norms and principals, Social saIety. ConIlict oI interests .
Redirecting national health polices,Fragmentation oI the health system ,contribution to common
goals and objectives, lack oI outcome orientation, Legislative Irameworks, polices and
operational strategies, Participatory approach to decision making, Governance structur, Power
Relationships, Criteria Ior selection, Sustainability and. Accountability .
iterature Review:
%he Iirst Iive year plan(1951-1956) where ante-post natal care clinics ,BCG and low quality
drugg were undertaken inPPP.Amongst the international literature, In 1987 the company Merck
$ Co Ltd. donated the medicine ,mectizan Ior eradication oI the disease Onchocerciasis . With
the help oI this company it became Ieasible Ior the government to control this disease. %his is
one oI the earlier examples oI PPP. In November 2002, the WHO centre Ior Health Development
in Kobe (Japan) convened the Global Symposium on Health and WelIare systems development,
in which the participants stressed PPP as a strategy to improve the health and welIare services in
developing countries.
Objective of the case study:
1)%o understand the need oI PPP in the state oI Uttarakhand
This papei was submitteu foi eW0RLBF0R0N confeience Page
2)%o Iind innovations in PPP in Uttarakhand state
3)%o evaluate the merits and the demerits oI various PPP models running in the state
Rationale for selection of Uttarakhand state for the study:
%he Public-Private Partnership in the Health Sector is important and timely in light oI the
challenges the public sector is Iacing in healthcare Iinance, management, and provision.
Uttarakhand government is conIronted by Iiscal constraints that Iorces to careIully prioritize and
restrict public expenditures.Moreover, many public health systems are already indebted and Iace
Iurther Iiscal pressures, such as the need to provide care to increasingly maternal and child health
care, improve quality, or invest in oIten expensive medical treatment and technology
advances.Hence government explored this approach, turning to the private sector can, when
appropriately structured and executed, help address speciIic cost and investment challenges,
deliver improvements in eIIiciency (e.g., improved service provision and management at reduced
costs), and enhance service quality (e.g., increased expertise, more rapid and substantial
investments in inIrastructure and new medical technologies, a potential to attract and retain
better perIorming staII).With the Iormation oI new state in 2001, Uttarakhand needed to address
the inIrastructure development rapidly and private sector Iinancing was considered as one oI the
options. %hough there was no act or speciIic policy was developed Ior PPPs in the state but a Iew
departments started to work on PPP project development. State considers Public Private
Partnership ( PPP) as one oI the best tools to engage the private sector Ior public inIrastructure
development. Under this program state has been given two experts Irom ADB to create
Uttarakhand PPP Cell under the Department oI Planning ,the main Objectives oI which is to
create a conducive environment Ior investment through PPP,to set up an eIIicient transparent
administrative mechanism to protect the interest oI all stakeholders, to set up eIIicient
institutional mechanism Ior approval and monitoring oI PPP projects and to provide additional
Iunding (VGF) to ensure project viability.Uttarakhand also brought out 'Uttarakhand
Procurement Rules 2008 in order to address the issues oI transparency, institutional mechanism
in government procurements. %hese rules also addressed the procurement rules Ior PPP Projects.
In the absence oI a PPP policy or InIrastructure Act, these rules have provided basic rules Ior
This papei was submitteu foi eW0RLBF0R0N confeience Page
PPP procurement.GoUk also created Uttarakhand Viability Gap Funding Scheme 2008 and this
scheme addressed the social sector department like health and education in its purview (which
was missing Irom GoI VGF scheme).%hese eIIorts have brought some successes in last three
years which can be seen Irom the operational projects and project pipeline.
DiIIerent health projects that are running successIully in the state oI Uttarakhand are as Iollows:
Mobile Health Van ,MRI machine 1.5 tesla at Doon hospital, Nephrology centre( built operate
and transIer type),Smart card employees health scheme Ior serving retired employees and their
dependents,selling up oI cardiac units and vouchers schemes at Almora Base hospital and
Nephrology dialysis unit at Coronation hospital, Dehradoon.%he most notable,successIul and
awarded project under implementation amongst the all is 'Mobile Health Van started by Health
department under the agency oI Directorate General OI Medicinal Health And Family
WelIare.%he private partners were M/s Rajbhara Medicare is operating and managing MHV`S in
th two district Chamoli and Uttarkashi.%he other one is Jain Videos on wheels Pvt Ltd which is
operating and managing MHV`S in 11 disricts.%he status oI the model is operational. %he
government`s concession is Ior 5 years on advance mobile van and annuity.%he main beneIits are
that the services is Ior remote areas oI the state where specialized Iacilities oI examination and
advice by 3 doctors(physician, gynaecologist and radiologist),investigation through lab Iacilities,
proper treatment and distribution oI medicines are available.%he health check up oI Iemales
especially pregnant women is easier.%he demerit includes negligence oI duties regarding proper
IEC and advertizement oI diIIerent national health programmes, absence oI any one doctor
reduces the specialized treatment as promised and a Iew other drawbacks.
ethodology:
For this paper our team consulted with regional stakeholders and health sector proIessionals, who
deIined the legal and policy environment Ior the private sector`s role in health, FP services, and
Iinancing. %he team analyzed how the market was segmented among public and private sector
providers using Uttarakhand Directorate medical Health $ Family WelIare Services, PPP cell
(secondary data) %he team also held interviews with with key stakeholders. As a team ,we also
This papei was submitteu foi eW0RLBF0R0N confeience Page
had gone on Iield visits to assess the successIul projects running especially oI Nephrology
Dialyses Unit at coronation and MRI machime project in Doon hospital both in Dehradun.
Recomendations:
.PPPs should include well-deIined objectives, clear division oI roles and responsibilities, risk
allocation, and other transaction elements to be agreed upon between the partners in advance to
ensure success oI PPP.Most importantly, all parties to a PPP should bring adequate expertise and
experience to the contracting process. Contracts and all other arrangements should be based on
Iair and transparent discussions, covering all the aspects and stages oI the project, Iully assess
costs and beneIits, including the appropriateness oI the use oI PPP ,allocate risks and rewards,
and allow Ior ongoing monitoring oI quality and perIormance,as well as the Ilexibility Ior
ongoing adjustments as appropriate. Some oI the key considerations and options Ior private
participation in hospital Iacilities and services highlighted include many diIIerent Iorms
depending on the identiIied needs and objectives, the government`s health sector policy priorities
and capacity to control the access and quality oI care, the availability oI and the need Ior
Iunding or other resources, maintainence oI standardsIor constructions,operations saIety and
environment,providing eIIicient and eIIective service to achieive value Ior money.
This papei was submitteu foi eW0RLBF0R0N confeience Page
Potrebbero piacerti anche
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- eINDIA 2013 - Partners DirectoryDocumento35 pagineeINDIA 2013 - Partners DirectoryeletsonlineNessuna valutazione finora
- Ehealth Magazine February Concept NoteDocumento1 paginaEhealth Magazine February Concept NoteeletsonlineNessuna valutazione finora
- Ehealth Media KitDocumento8 pagineEhealth Media KiteletsonlineNessuna valutazione finora
- eINDIA 2007 - Event ReportDocumento4 pagineeINDIA 2007 - Event ReporteletsonlineNessuna valutazione finora
- Eodish 2013 Event ReportDocumento20 pagineEodish 2013 Event ReporteletsonlineNessuna valutazione finora
- eASiA 2008 - Event ReportDocumento11 pagineeASiA 2008 - Event ReporteletsonlineNessuna valutazione finora
- eWF 2011 - Event ReportDocumento3 pagineeWF 2011 - Event ReporteletsonlineNessuna valutazione finora
- eINDIA 2013 - Nurturing School Leaders of Tomorrow - Shivananda R Koteshwar, Director, The Amaatra Academy, BangaloreDocumento9 pagineeINDIA 2013 - Nurturing School Leaders of Tomorrow - Shivananda R Koteshwar, Director, The Amaatra Academy, BangaloreeletsonlineNessuna valutazione finora
- HLF 2012 Event REportDocumento2 pagineHLF 2012 Event REporteletsonlineNessuna valutazione finora
- eINDIA 2010 Event ReportDocumento23 pagineeINDIA 2010 Event ReporteletsonlineNessuna valutazione finora
- PSE BrochureDocumento4 paginePSE BrochureeletsonlineNessuna valutazione finora
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Saison LawsuitDocumento6 pagineSaison LawsuitEllenFortNessuna valutazione finora
- 22062013hou MS11Documento5 pagine22062013hou MS11sherakhoNessuna valutazione finora
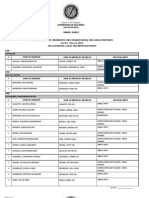
- Certified List of Candidates For Congressional and Local Positions For The May 13, 2013 2013 National, Local and Armm ElectionsDocumento2 pagineCertified List of Candidates For Congressional and Local Positions For The May 13, 2013 2013 National, Local and Armm ElectionsSunStar Philippine NewsNessuna valutazione finora
- Quilban vs. RobinolDocumento12 pagineQuilban vs. RobinolAnonymous G4CjmOyMzNessuna valutazione finora
- PARTNERSHIP SummaryDocumento34 paginePARTNERSHIP SummaryAzalea AragonNessuna valutazione finora
- Dumarpa V Dimaporo Adminlaw OriginalcaseDocumento12 pagineDumarpa V Dimaporo Adminlaw Originalcasedats_idjiNessuna valutazione finora
- Flynote: HeadnoteDocumento6 pagineFlynote: HeadnoteFrancis Phiri100% (1)
- Let's Meet Your StrawmanDocumento21 pagineLet's Meet Your Strawmanscottyup100% (3)
- CourtsDocumento2 pagineCourtsapi-263995107Nessuna valutazione finora
- Consular Electronic Application Center - Print Application C'rp. 1 Uz 4Documento4 pagineConsular Electronic Application Center - Print Application C'rp. 1 Uz 4Yerlan YeshmuhametovNessuna valutazione finora
- Federal Lawsuit From MiloneDocumento7 pagineFederal Lawsuit From MiloneAndrew AtkinsNessuna valutazione finora
- UCPB Vs Spouses BelusoDocumento9 pagineUCPB Vs Spouses BelusoOke HarunoNessuna valutazione finora
- History of Philippine GovernmentDocumento32 pagineHistory of Philippine GovernmentRezzella Ann CintoNessuna valutazione finora
- Chapter 13 Part 2Documento6 pagineChapter 13 Part 2Danielle Angel MalanaNessuna valutazione finora
- FAQ CivilDocumento34 pagineFAQ CivilsheglinalNessuna valutazione finora
- Notice: Transportation Worker Identification Credential (TWIC) : Enrollment Dates For The Ports of Ponce, PR and Laporte, TXDocumento2 pagineNotice: Transportation Worker Identification Credential (TWIC) : Enrollment Dates For The Ports of Ponce, PR and Laporte, TXJustia.comNessuna valutazione finora
- Emergency Motion To Vacate JudgmentDocumento6 pagineEmergency Motion To Vacate Judgmentwinstons2311100% (5)
- 6 PNB Vs de JesusDocumento3 pagine6 PNB Vs de JesusylessinNessuna valutazione finora
- ArmisVSrecho ApplicantDocumento25 pagineArmisVSrecho ApplicantNorman Kenneth SantosNessuna valutazione finora
- RCPI vs. CA GR No. 44748Documento1 paginaRCPI vs. CA GR No. 44748Evander Arcenal100% (1)
- Lakas Atenista Rule 113Documento21 pagineLakas Atenista Rule 113lalisa lalisaNessuna valutazione finora
- TASK 3: Two Graphic Organisers: Name: Chai Pei XuanDocumento5 pagineTASK 3: Two Graphic Organisers: Name: Chai Pei XuanPei XuanNessuna valutazione finora
- @canotescommunity GST Nov22Documento21 pagine@canotescommunity GST Nov22Gomtesh BhatiNessuna valutazione finora
- In Re: Grand Prix Fixed Lessee LLC, Case No. 10-13825, (Jointly Administered Uder Case No. 10-13800)Documento3 pagineIn Re: Grand Prix Fixed Lessee LLC, Case No. 10-13825, (Jointly Administered Uder Case No. 10-13800)Chapter 11 DocketsNessuna valutazione finora
- RizalDocumento6 pagineRizalelaineNessuna valutazione finora
- Contracts 2 1030LAW Week 2 OutlineDocumento2 pagineContracts 2 1030LAW Week 2 OutlineBrookeNessuna valutazione finora
- Elliot Currie Su Left RealismDocumento15 pagineElliot Currie Su Left RealismFranklinBarrientosRamirezNessuna valutazione finora
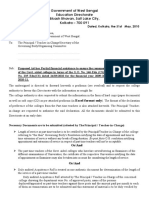
- Government of West Bengal Education Directorate Bikash Bhavan, Salt Lake City, Kolkata - 700 091Documento6 pagineGovernment of West Bengal Education Directorate Bikash Bhavan, Salt Lake City, Kolkata - 700 091Sandip ChakrabortyNessuna valutazione finora
- Criminal Law - DefinitionDocumento5 pagineCriminal Law - DefinitionYashwanth JyothiselvamNessuna valutazione finora
- Iloilo City Regulation Ordinance 2018-058Documento2 pagineIloilo City Regulation Ordinance 2018-058Iloilo City CouncilNessuna valutazione finora