Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Ajish Akas Dexa
Caricato da
api-3827000Descrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Ajish Akas Dexa
Caricato da
api-3827000Copyright:
Formati disponibili
Department of Electronics and Communication
Government Engineering College, Thrissur
Seminar Report
2004
Dual Energy X-ray Absorptiometry
Presented by
Ajesh Kumar A.S.
S7 ECE
Roll No: 01-602
Dual Energy X-ray Absorptiometry 2 Seminar Report ‘04
ACKNOWLEDGMENT
I would like to thank everyone who helped to see this seminar to
completion. In particular, I would like to thank my seminar coordinator
Mrs. Muneera.C.R for her moral support and guidance to complete my
seminar on time. Also I would like to thank Mr. C. D. Anil Kumar for
his invaluable help and support.
I would like to take this opportunity to thank Prof. Indiradevi,
Head of the Department, Electronics & Communication Engineering for
her support and encouragement.
I express my gratitude to all my friends and classmates for their
support and help in this seminar.
GEC Thrissur Dept. of Electronics & Communication
Dual Energy X-ray Absorptiometry 3 Seminar Report ‘04
CONTENTS
Abstract 4
1. Introduction 5
2. Principles of Dual Energy X-ray Absorptiometry 6
2.1 Principal components of a DEXA system 6
2.2 Interaction of X-ray photon with physical matter 7
2.3 Mass attenuation coefficient (U) and
mass per unit area (M) of the absorber 9
2.4 Determination of Mass per unit area
of a homogeneous absorber 11
3. DEXA analysis of human body composition 13
3.1 Components of a human body 13
3.2 A model DEXA analysis 15
4. Actual DEXA calculation 17
4.1 The R value 17
4.2 Use of R value 18
5. Advantages of DEXA scanning 23
6. Conclusions 24
7. References 25
GEC Thrissur Dept. of Electronics & Communication
Dual Energy X-ray Absorptiometry 4 Seminar Report ‘04
ABSTRACT
The basic principles of Dual Energy X-ray Absorptiometry have been
discussed in this presentation. DEXA is a instrumental technique used to measure
bone mineral density (BMD), which is the widely accepted indicator of bone strength.
DEXA scanner is the most widely used modern electronic machine to diagnose the
disease osteoporosis, the thinning of bones. Human body being a heterogeneous
system, use of a dual energy, rather than single energy, X-ray source is necessary for
scanning. The interaction of the sample with the X-ray beams results in a reduction or
attenuation of the energy of the X-ray beam. The extent to which the photon energy
is attenuated is a function of the initial energy of the X-ray photon, the mass per unit
area (M) of the absorber material and the mass attenuation coefficient (U) of the
absorber. For a given absorber material, U (which is a measure of the degree of
attenuation) is a constant at any given photon energy.
U increases with the density of the absorber material and decreases with the
energy of the X-ray beam. U can be used to calculate the Mass per unit area (M) of a
homogenous absorber irradiated at a specific incident X-ray energy. The mass of
bone and soft tissue ‘below’ this square would represent the mass per unit area of the
absorber, viz., leg. For instance, if there are 100 grams of bone and soft tissue below
this square, the mass per unit area (M) would be 100 g/cm2. Knowledge of M of the
human body components, especially of bone, is important in determining the
possibility of osteoporosis. The calculations of M of the various components of the
body are discussed in detail.
From knowledge of mass attenuation coefficient (U) of the absorber and the
energy of the incident X-ray beam (E0) and of the emerging beam (E), we can
calculate M of a homogeneous absorber from the following relationship connecting
these properties.
GEC Thrissur Dept. of Electronics & Communication
Dual Energy X-ray Absorptiometry 5 Seminar Report ‘04
1. INTRODUCTION
Dual Energy X-ray Absorptiometry (DEXA) is an instrumental
technique used to measure bone mineral density (BMD) that includes the
hip and spine, compared to SXA (Single Energy X-ray Absorptiometry)
that measures only the wrist or heel bone. BMD is the widely accepted
indicator of bone strength.
DEXA (the whole body scanner) uses low dose x-rays to give us
information on bone content and density. It is currently the most widely
used machine in the clinical setting to diagnose the disease osteoporosis,
the thinning of bones.
GEC Thrissur Dept. of Electronics & Communication
Dual Energy X-ray Absorptiometry 6 Seminar Report ‘04
2. PRINCIPLES OF DUAL ENERGY X-RAY
ABSORPTIOMETRY
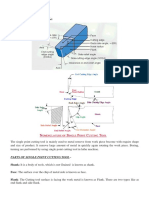
2.1 Principal components of a DEXA system
A typical DEXA system is shown in the figure.
Figure 1. The DEXA system
The DEXA scanner consists of the following basic components:
1. Source of X-rays
2. The sample space
3. The detector
A block diagram of the instrument is shown below as Figure 2. Two separate
beams of X-rays of known energies (E0,1 and E0,2) produced at the source are passed
through a desired absorber material (sample)-usually human body- positioned in the
sample space (DEXA table). The sample interacts with the incident beams altering
their energies to E1 and E2. The detector determines the energies (E1 and E2) of the
emerging beams of X-radiation. A data acquisition and control unit manipulates the
data. The operation of this electronic machine is fully controlled by a computer
system.
GEC Thrissur Dept. of Electronics & Communication
Dual Energy X-ray Absorptiometry 7 Seminar Report ‘04
Figure 2. The principal components of DEXA system
We will understand the working principle of DEXA by first considering the
interaction of a single beam of X-Rays with matter.
2.2 Interaction of X-ray photon with physical matter
When a beam of X-rays is allowed to pass through an absorber material, the
X-ray photons interact with the electrons of the material in 2 different ways.
a. The photon knocks the weakly bound outer orbit electron giving up some of
its energy to the electron and gets deflected (scattered) from its path. The scattered
photon has a lower energy and hence a longer wavelength than the incident photon.
This is Compton scattering (Figure 3a).
GEC Thrissur Dept. of Electronics & Communication
Dual Energy X-ray Absorptiometry 8 Seminar Report ‘04
Figure 3a. Compton effect
b. The photon collides with more tightly bound orbit electron giving up all its
energy to the electron and the photon ceases to exist. This is photoelectric collision
(Figure 3b).
Figure 3b. Photoelectric effect
GEC Thrissur Dept. of Electronics & Communication
Dual Energy X-ray Absorptiometry 9 Seminar Report ‘04
Both these interactions result in a reduction or attenuation of the energy of the
X-ray beam. In fact, the incident photon energy is exponentially reduced or
attenuated as it passes through the absorber (see Figure 4).
Figure 4. Attenuation of X-Ray energy by the interaction of the absorber.
2.3 Mass attenuation coefficient (U) and mass per unit area
(M) of the absorber
The extent to which the photon energy is attenuated is a function of the initial
energy of the X-ray photon, the mass per unit area (M) of the absorber material and
the mass attenuation coefficient (U) of the absorber. For a given absorber material,
U (which is a measure of the degree of attenuation) is a constant at any given photon
energy. For instance, at an incident photon energy of 40 keV, A for hydrogen is
0.3458 cm2/g; at an incident photon energy of 70 keV, it is 0.3175 cm2/g. The mass
attenuation coefficients of some absorber elements are given below for two photon
energies for examination:
GEC Thrissur Dept. of Electronics & Communication
Dual Energy X-ray Absorptiometry 10 Seminar Report ‘04
Table 1 : Mass attenuation coefficients of some elements.
Element Atomic number U (cm2/g)
40 keV 70 keV
H 1 0.3458 0.3175
C 6 0.2047 0.1678
N 7 0.2246 0.1722
O 8 0.2533 0.1788
Na 11 0.3851 0.2022
Mg 15 0.4704 0.2244
P 15 0.7784 0.2839
S 16 0.9509 0.3258
Cl 18 1.1000 0.3491
K 19 1.4840 0.4297
Ca 20 1.7920 0.5059
From the table it is clear, that
(a) U increases with atomic number of the element. In other words, higher atomic
number elements attenuate the X-ray beam to a greater degree than lower atomic
number elements.
(b) The lower energy beam is always attenuated to a greater degree than the
higher energy beam.
U can be used to calculate the Mass per unit area (M) of a homogenous
absorber irradiated at a specific incident X-ray energy.
A homogeneous material is any single material for which U is known at a
specific incident X-ray photon energy. This can be an element, a compound, or a
solution, as given below.
GEC Thrissur Dept. of Electronics & Communication
Dual Energy X-ray Absorptiometry 11 Seminar Report ‘04
Table 2: Mass attenuation coefficients of some homogeneous absorber materials.
Component U
40 keV 70 keV
Ca 1.7920 0.5059
Water 0.2636 0.1942
Protein 0.2363 0.1831
Fat(Oleic acid) 0.2273 0.1872
Bone mineral 0.9039 0.3159
2.4 Determination of Mass per unit area of a homogeneous
absorber
When X-rays scan a 3-dimensional absorber such as a human being, it
produces a 2-dimensional flat image. Let us consider the X-ray image of a human leg.
Figure 5. X-ray image of a human leg. The square mark on the image represents an
area of 1 cm2
This is a flat 2-dimensional image of a real 3-dimensional leg. The image is
made up of many small “picture elements” or “pixels”. Each pixel is uniform and
represents a ‘snap shot’ taken during the X-ray scan. Let us now consider a square of
GEC Thrissur Dept. of Electronics & Communication
Dual Energy X-ray Absorptiometry 12 Seminar Report ‘04
area 1cm2 on the image. The mass of bone and soft tissue ‘below’ this square would
represent the mass per unit area of the absorber, viz., leg. For instance, if there are
100 grams of bone and soft tissue below this square, the mass per unit area (M) would
be 100 g/cm2.
Knowledge of M of the human body components, especially of bone, is
important in determining the possibility of osteoporosis.
Calculation of M:
From a knowledge of mass attenuation coefficient (U ) of the absorber and the
energy of the incident X-ray beam (E0) and of the emerging beam (E), we can
calculate M of a homogeneous absorber from the following relationship connecting
these properties.
ln ( E0 / E ) = U x M
M = ln ( E0 / E ) / U
For instance, let us consider that we allow a 40 keV X-ray beam to pass
through the absorber bone mineral, whose U value is 0.9039 cm2/g (see Table 2).
Some of the energy will be lost due to Compton scattering and photoelectric effect.
Let the emerging X-ray beam be attenuated to 10 keV. Then, the mass per unit area
of this homogeneous absorber, bone mineral, is given by
M = ln (40/10) / 0.9039
= ( ln 4 ) / 0.9039
= 1.534 g /cm2
Thus using a single X-ray beam we are able to determine the mass of bone
mineral in our sample.
Unfortunately, a human body is not a homogeneous absorber since there
are several different components in the body, such as fat, lean tissue, and bone.
A single X-ray beam cannot differentiate among these different components. For this
we must utilize a “dual energy X-ray” beam.
GEC Thrissur Dept. of Electronics & Communication
Dual Energy X-ray Absorptiometry 13 Seminar Report ‘04
3. DEXA ANALYSIS OF HUMAN BODY
COMPOSITION
While a mono energetic X-ray source is capable of measuring the areal density
of a homogeneous absorber, a dual energy X-ray source is required to determine the
areal densities of up to two components of an absorber. Before we discuss the DEXA
body composition analysis, let us have a look at the various components of human
body.
3.1 Components of a human body
Bone mineral
Non-bone mineral
Glycogen
Proteins
Water
Fat
The sum of all these make up the body weight. These 6 components can be
conveniently grouped into a 2-component system: Soft tissue mass and Bone
mineral mass. Here soft tissue mass includes all the non-bone mass (items 2 to 6)
made up of lean tissue mass (items 2 to 5) and fat tissue mass (item 6).
In areas that contain no bone, the soft tissue component can be divided into its
own 2-component model consisting of Fat soft tissue and Lean soft tissue. By
considering the body to be made up of a series of 2-component systems, DEXA can
analyze each 2-component system separately and then combine the results for a
complete body composition analysis.
GEC Thrissur Dept. of Electronics & Communication
Dual Energy X-ray Absorptiometry 14 Seminar Report ‘04
Thus, when the dual energy X-ray beams are over a position of the body that
contains no bone, DEXA can analyze the area for the 2 components, fat tissue mass
and lean tissue mass. When the dual energy X-ray beams are over a position of the
body that does contain bone, DEXA can analyse the area for the 2 components, soft
tissue mass (fat and lean combined) and bone mineral mass. The fat and lean
components of the bone-containing areas can then be deducted by a method that we
shall discuss. This way, the human body can be regarded as consisting of 3
principal components viz., fat mass, lean mass and bone mass (see Figure 6) and
these 3 components can be estimated by a 2-component technique using dual
energy X-rays.
Figure 6. Human body composition
GEC Thrissur Dept. of Electronics & Communication
Dual Energy X-ray Absorptiometry 15 Seminar Report ‘04
3.2 A model of DEXA analysis
For convenience, we shall reduce the human example into a block of tissue
containg the 3 components we are interested in. The left half of the block represents
an area of tissue containg only soft tissue (fat + lean). The right half represents an
area of tissue that contains both soft tissue and bone (see Figure 7).
Figure 7. A block of tissue
As the dual energy X-ray beams pass through the “soft-tissue only” region, the
mass of the 2 components, fat tissue and lean tissue, can be determined. Similarly, as
the dual energy X-ray beams scan through the “bone + soft-tissue” region, the mass of
its 2 components, bone mineral and soft tissue, can be determined.
The composition of the soft tissue over the bone is nearly the same as the
composition of the soft tissue in the no-bone area. For instance, if the total soft
tissue mass of the “soft tissue only” area is 10g and it contains 2g fat (known from
scan), then we have the following results:
GEC Thrissur Dept. of Electronics & Communication
Dual Energy X-ray Absorptiometry 16 Seminar Report ‘04
No-Bone area
% Fat = 2 x 100 /10 = 20
∴ % Lean = 100 – 20 = 80
This composition of the soft tissue in the “no-bone” area is assumed to be the
composition of the soft tissue in the “bone” area also. Thus,
Bone area
Fat mass = 2g
∴ % Fat = 2 x 100 /10 = 20
∴ % Lean = 100 – 20 = 80
If the total mass of the soft tissue in the bone area is 5g (known from the scan),
then the fat mass of this area can now be calculated as
Bone area
% fat = 20
soft tissue mass (from scan) = 5g
∴ fat mass = 5 x 20/100 = 1g
∴ lean mass = 5 – 1 = 4g
(Bone mass is also known from the scan)
We have thus understood how 3 components of the body can be determined
using a technique that can only measure 2 components at one time. We shall now
attempt to understand how DEXA actually measures bone, fat and lean mass.
GEC Thrissur Dept. of Electronics & Communication
Dual Energy X-ray Absorptiometry 17 Seminar Report ‘04
4. ACTUAL DEXA CALCULATION
4.1 The R-value
To understand this, we need to define a new term, namely R-value. R-value is
simply the ratio of the low-energy attenuation coefficient to the high-energy
attenuation coefficient. Let us return to Tables 1 and 2 to calculate the R values of
some homogeneous absorbers. We get a column of R-values for these absorbers in
relation to the 40 and 70 keV X-rays (see Tables 3 and 4 generated from Tables 1 and
2).
Table 3 : R values of some elements.
Element Atomic number U (cm2/g) R-value
40 keV 70 keV
H 1 0.3458 0.3175 1.0891
C 6 0.2047 0.1678 1.2199
N 7 0.2246 0.1722 1.3043
O 8 0.2533 0.1788 1.4167
Na 11 0.3851 0.2022 1.9045
Mg 15 0.4704 0.2244 2.0963
P 15 0.7784 0.2839 2.7418
S 16 0.9509 0.3258 2.9187
Cl 18 1.1000 0.3491 3.1600
K 19 1.4840 0.4297 3.4536
Ca 20 1.7920 0.5059 3.5422
GEC Thrissur Dept. of Electronics & Communication
Dual Energy X-ray Absorptiometry 18 Seminar Report ‘04
Table 4: R-values of some homogeneous absorber materials.
Component U R-value
40 keV 70 keV
Ca 1.7920 0.5059 3.5422
Water 0.2636 0.1942 1.3574
Protein 0.2363 0.1831 1.2906
Fat(Oleic acid) 0.2273 0.1872 1.2136
Bone mineral 0.9039 0.3159 2.8613
For absorbers composed of more than one component, the R-value is a
function of mass attenuation coefficient of each component as well as the mass
fraction of each component.
4.2 Use of R-value
Using R-value, we can determine the mass fraction of each component in a 2-
component system, if we also know the mass attenuation coefficients of each
component. In fact, the R-value for soft tissue (made up of fat and lean) is linearly
related to the amount of fat in the tissue. It decreases with increase in the fat content
(see Figure ).
Let us now consider a DEXA scanning experiment using a low-energy X-ray
beam of energy 40 keV and a high-energy X-ray beam of energy 70 keV. The
sample used is the block of tissue considered earlier. The DEXA detectors measure
the energies of the attenuated X-ray beams emerging from the sample.
Let us first scan through the “soft tissue (ST) only” area. The energy of the 40
keV beam has been attenuated to 0.358 keV and that of 70 keV to 2.291 keV. Now
scan the bone (B) area. The energy of the 40 keV beam has been attenuated to 0.080
keV and that of 70 keV to 1.960 keV. The data collected may be represented as
shown below:
GEC Thrissur Dept. of Electronics & Communication
Dual Energy X-ray Absorptiometry 19 Seminar Report ‘04
40 70
E0 = 40 keV E0 = 70 keV
40 70
EST = 0.358 keV EST = 2.291 keV
40 70
EB = 0.080 keV EB = 1.960 keV
We have now collected all the necessary DEXA data to determine the
composition of our tissue block. We need to know the mass attenuation coefficients
and R-values for fat tissue (F), lean tissue (L) and bone (B). These are known from
experiments and are given below.
40
UF = 0.23 cm2/g 70
UF = 0.19 cm2/g RF = 1.211
40
UL = 0.27 cm2/g 70
UL = 0.19 cm2/g RL = 1.421
40
UB = 1.00 cm2/g 70
UB = 0.32 cm2/g RB = 3.125
We also need to know the mass attenuation coefficients and R-value for soft
tissue (ST). These values will vary from subject to subject. (Recall the variation of
soft tissue R value with the amount of fat in the subject.) So we have to determine
them from our experimental results by the following procedure.
Calculation of RST:
We know,
ln ( E0 / E ) = U x M
Thus for 40 keV X-ray we have
ln ( 40E0 / 40E ) = 40
U x M
Similarly, for 40 keV X-ray we have
ln ( 70E0 / 70E ) = 70
U x M
GEC Thrissur Dept. of Electronics & Communication
Dual Energy X-ray Absorptiometry 20 Seminar Report ‘04
Note that M, the mass per unit area of the tissue will not change with the
energy of the radiation. Applying these equations for calculating the R value of the
soft tissue, we obtain
ln ( 40E0 / 40EST ) 40
UST x MST 40
UST
----------------- = ----------------- = ------ = RST
ln ( 70E0 / 70EST ) 70
UST x MST 70
UST
Thus, substituting the known values on the LHS, we can cal culate the value of
RST.
ln ( 40E0 / 40EST ) ln ( 40 / 0.358 )
RST = ----------------- = ------------------
ln ( 70E0 / 70EST ) ln ( 70 / 2.291 )
= 1.379
We can now calculate the % Lean content of the soft tissue from the equation
% Lean = [(RST – RF) / (RL – RF)] x 100 = [(1.379-1.211) / (1.421-1.211)] x 100
= [0.168/ 0.21] x 100
= 80
∴% Fat = 20
40 70
Calculation of UST and UST :
40
UST = (Lean fraction) x 40UL + (Fat fraction) x 40UF
70
UST = (Lean fraction) x 70UL + (Fat fraction) x 70UF
Substituting our experimental data, we obtain
40
UST = 0.262 cm2/g
70
UST = 0.19 cm2/g
GEC Thrissur Dept. of Electronics & Communication
Dual Energy X-ray Absorptiometry 21 Seminar Report ‘04
The summary of data so far developed
From DEXA scan
40 70
E0 = 40 keV E0 = 70 keV
40 70
EST = 0.358 keV EST = 2.291 keV
40 70
EB = 0.080 keV EB = 1.960 keV
Experimentally known and calculated values
40
UF = 0.23 cm2/g 70
UF = 0.19 cm2/g RF = 1.211
40 2 70 2
UL = 0.27 cm /g UL = 0.19 cm /g RL = 1.421
40 2 70 2
UB = 1.00 cm /g UB = 0.32 cm /g RB = 3.125
40 2 70 2
UST = 0.262 cm /g UST = 0.19 cm /g RST = 1.379
Calculation of areal densities of the components :
Bone mineral density (MB):
It is calculated using the equation,
ln ( 40E0/ 40EB ) - RST x ln ( 70E0 / 70EB )
MB = ------------------------------------------------
40 70
UB - UB x RST
On substituting the valures we obtain
MB = 2.30 g / cm2
Soft tissue density (MST), Lean tissue density (ML) and Fat tissue density (MF) over
the bone:
This is calculated using the expression
ln ( 40E0/ 40EB ) - RB x ln ( 70E0 / 70EB )
MST = ------------------------------------------------
40 70
UST - UST x RB
= 14.95 g/ cm2
We now assume that the composition of this soft tissue in the bone area is
approximately equal to that of the adjacent soft tissue in the no-bone area:
GEC Thrissur Dept. of Electronics & Communication
Dual Energy X-ray Absorptiometry 22 Seminar Report ‘04
% Lean of ST (No-bone area) = 80
% Fat of ST (No-bone area) = 20
So,
% Lean of ST (Bone area) = 80
% Lean of Fat (Bone area) = 20
∴ML (Bone area) = 14.95 x 0.80 = 11.96 g/ cm2
MF (Bone area) = 14.95 x 0.20 = 2.99 g/ cm2
Soft tissue density (MST), Lean tissue density (ML) and Fat tissue density (MF) in the
no- bone area:
Finally, we calculate the areal densities of the Lean and Fat tissue fractions of
the “ST only” area using the same above formulas.
ML (No-Bone area) = 18 x 0.80 = 14.4 g/ cm2
MF (No-Bone area) = 18 x 0.20 = 3.6 g/ cm2
If we sum all the areal densities that we have calculated, we would obtain an
accurate measurement of the total weight of our tissue block:
MB = 2.3 g / cm2
ML (Bone area) = 11.96 g / cm2
MF (Bone area) = 2.99 g / cm2
ML (No-Bone area) = 14.4 g / cm2
MF (No-Bone area) = 3.6 g / cm2
------------------------------------------------
Total tissue weight = 35.25 g / cm2
Evidently, these are tedious calculations to do by hand. We have just shown
the calculations with respect to one tissue. In reality, a very large number of tissues
are to be scanned and then the results are to be consolidated. A computer is
absolutely necessary to achieve this. In fact the technician operates the DEXA
apparatus from a PC. After completing the scan, the data are analysed using the PC as
well. It is possible to divide the scanned image into various regions of interest (ROI’s)
by properly positioning the cut lines. The DEXA software then analyzes each of the
ROI’s and generates a report of the composition of each of the ROI’s , as well as the
whole body analysis.
GEC Thrissur Dept. of Electronics & Communication
Dual Energy X-ray Absorptiometry 23 Seminar Report ‘04
5. ADVANTAGES OF DEXA SCANNING
Dual Energy X-ray Absortiometry, or DEXA scanning, is currently the most
widely used method to measure bone mineral density. For the test, a patient lies down
on an examining table, and the scanner rapidly directs x-ray energy from two
different sources towards the bone being examined. The X-ray source and the
detector move in a coordinated rectilinear pattern over the patient. The mineral
density of the patient’s bone weakens, or prolongs the transmission of these two
sources of x-ray energy through a filter onto a counter in a degree related to the
amount of bone mass present. The greater the bone mineral density, the greater the
signal picked up by the photon counter. The use of the two different x-ray energy
sources rather than more traditional radioisotope studies (such that would be used for
a bone scan) greatly improves the precision and accuracy of the measurements. The
DEXA images of hip and spine are shown below.
DEXA scanning has become the most widely used method for measuring bone
mineral density for several reasons. When compared with radiographic absortiometry
or single energy x-ray absortiometry, DEXA scanning more precisely documents
small changes in bone mass and is also more flexible since it can be used to examine
GEC Thrissur Dept. of Electronics & Communication
Dual Energy X-ray Absorptiometry 24 Seminar Report ‘04
both the spine and the extremities. A scan of the spine, hip or the total body requires
only one, two or four minutes respectively. Qualitative computed tomography (QCT)
is the only technique that can directly measure bone density and volume but can
distinguish trabecular from cortical bone. DEXA scanning is less expensive, exposes
the patient to less radiation and is more sensitive and accurate at measuring subtle
changes in bone density over time or in response to drug therapy than is QCT.
6. CONCLUSIONS
DEXA is the most commonly used modern technique to determine the bone
density and hence the bone strength. The DEXA results help to predict the patient’s
risk factors for osteoporosis. It is a fast, accurate, and less expensive technique. It
exposes the patient to fewer amounts of radiations. So the risk is reduced to a great
extend.
Studies using DEXA scanning have shown that women with osteoporosis have
substantially lower bone density measurements than normal, age-matched women.
Bone mineral density is widely accepted as a good indicator of bone strength. Thus
low values can be compared against standard bone density measurements and help
predict a patient’s risk for fracture based upon the DEXA scan measurements.
GEC Thrissur Dept. of Electronics & Communication
Dual Energy X-ray Absorptiometry 25 Seminar Report ‘04
7. REFERENCES
1. Pietrobelli, A., et al., Am J. Physiol., 271: E941 – E951
(1996)
2. Phoenix 5’s Prostate Cancer Glossary, 2002
3. Genant HK et al. Review Noninvasive assessment of bone
mineral and structure, J Bone Miner Res. 11, 707-730, 1996.
GEC Thrissur Dept. of Electronics & Communication
Potrebbero piacerti anche
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- 6th Central Pay Commission Salary CalculatorDocumento15 pagine6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- Electrician Mostly Asked MCQ For RRB ALP PDFDocumento32 pagineElectrician Mostly Asked MCQ For RRB ALP PDFSajid Faniband100% (1)
- Aci435 PDFDocumento89 pagineAci435 PDFVasanthapragash NadarajhaNessuna valutazione finora
- Parts of Single Point Cutting ToolDocumento8 pagineParts of Single Point Cutting ToolMukesh sutharNessuna valutazione finora
- Mechanics of Rotor Spinning MachinesDocumento283 pagineMechanics of Rotor Spinning MachinesFelipe Melgarejo75% (4)
- MD VI Shaft DesignDocumento11 pagineMD VI Shaft DesignShatendra SahuNessuna valutazione finora
- Polyamide 610 KasarDocumento8 paginePolyamide 610 KasarAlison BurksNessuna valutazione finora
- MRI Lecture NotesDocumento33 pagineMRI Lecture NotesArungoud PoshalaNessuna valutazione finora
- 77-7 Sliding BearingDocumento11 pagine77-7 Sliding Bearingrip111176100% (1)
- Sujith - Digital Light ProcessingDocumento43 pagineSujith - Digital Light Processingapi-3827000100% (3)
- Subin S B (Virtual Keyboard)Documento36 pagineSubin S B (Virtual Keyboard)yuben josephNessuna valutazione finora
- Ushashi SMSDocumento22 pagineUshashi SMSapi-3827000Nessuna valutazione finora
- Shyam Ac Performance of Nano ElectronicsDocumento30 pagineShyam Ac Performance of Nano Electronicsapi-3827000100% (1)
- SUBIN K M Freespace Laser CommunicationsDocumento31 pagineSUBIN K M Freespace Laser Communicationsapi-3827000100% (3)
- Sreerekha (FinFET)Documento38 pagineSreerekha (FinFET)yuben josephNessuna valutazione finora
- Sreerekha (FinFET)Documento38 pagineSreerekha (FinFET)yuben josephNessuna valutazione finora
- Anand 4G WirelessDocumento31 pagineAnand 4G Wirelessapi-3827000100% (6)
- Girish TeleportationDocumento26 pagineGirish Teleportationapi-3827000100% (3)
- Sanjay - High Performance DSP ArchitecturesDocumento38 pagineSanjay - High Performance DSP Architecturesapi-3827000Nessuna valutazione finora
- Arun OFDMDocumento42 pagineArun OFDMapi-3827000Nessuna valutazione finora
- 64 Bit ComputingDocumento18 pagine64 Bit ComputingAshish MadaanNessuna valutazione finora
- Quadrics Interconnection NetworkDocumento24 pagineQuadrics Interconnection Networkapi-3827000100% (1)
- Voice MorphingDocumento31 pagineVoice Morphingapi-382700092% (13)
- Prasanna (Code Division Duplex Ing)Documento30 paginePrasanna (Code Division Duplex Ing)yuben josephNessuna valutazione finora
- Wireless FidelityDocumento22 pagineWireless Fidelitymuraliraj_sNessuna valutazione finora
- Wireless Local LoopDocumento8 pagineWireless Local Loopapi-3827000100% (1)
- Surround SystemsDocumento24 pagineSurround Systemsapi-3827000Nessuna valutazione finora
- Tele ImmersionDocumento20 pagineTele Immersionapi-3827000100% (8)
- Polymer MemoryDocumento27 paginePolymer Memoryapi-3827000100% (4)
- ProblemsDocumento32 pagineProblemsjosiedabatosNessuna valutazione finora
- AngularDocumento57 pagineAngularThomas Edoche EdocheNessuna valutazione finora
- 3 Marks PDFDocumento62 pagine3 Marks PDFNithin Aadhav.SNessuna valutazione finora
- Lecture 03Documento25 pagineLecture 03Magdalena SiahaanNessuna valutazione finora
- Classical Field TheoryDocumento35 pagineClassical Field TheorySagar JCNessuna valutazione finora
- Miniature Aluminum Electrolytic Capacitors: SeriesDocumento7 pagineMiniature Aluminum Electrolytic Capacitors: SeriesLaurentiu IacobNessuna valutazione finora
- ASCO 327 Solenoid Valves ATEX IECEx Certified For Hazardous Areas2Documento4 pagineASCO 327 Solenoid Valves ATEX IECEx Certified For Hazardous Areas2harishNessuna valutazione finora
- Higgs Lecture NotesDocumento48 pagineHiggs Lecture Noteszcapg17Nessuna valutazione finora
- ChainDocumento2 pagineChainmyusuf_engineerNessuna valutazione finora
- Effect of Structure-Directing Agent On AlPO4-n Synthesis From Aluminum DrossDocumento5 pagineEffect of Structure-Directing Agent On AlPO4-n Synthesis From Aluminum DrossXantos YulianNessuna valutazione finora
- 4 - Rate Laws and Stoichiometry - StuDocumento62 pagine4 - Rate Laws and Stoichiometry - StuTiệp MatícNessuna valutazione finora
- Drying Introduction, DefinationDocumento15 pagineDrying Introduction, DefinationChintan ModiNessuna valutazione finora
- Effect of Fly Ash and Silica Fume On Concrete": Submitted byDocumento19 pagineEffect of Fly Ash and Silica Fume On Concrete": Submitted bysushil kumarNessuna valutazione finora
- Engg Mechanics Question Bank UNIT-1Documento10 pagineEngg Mechanics Question Bank UNIT-1Thiyagarajan GurusamyNessuna valutazione finora
- MAAE 3202 Mid Term Assignment 2014Documento11 pagineMAAE 3202 Mid Term Assignment 2014Moustafa SohdyNessuna valutazione finora
- Pharmaceutical Chemistry Answer Key Blue PacopDocumento30 paginePharmaceutical Chemistry Answer Key Blue PacopJeannie UyNessuna valutazione finora
- 1-7 Manufacturing BasicsDocumento29 pagine1-7 Manufacturing BasicsFaNg KupthammasarnNessuna valutazione finora
- VibrationDocumento15 pagineVibrationCma WeyhNessuna valutazione finora
- Part 32 Welding RelatedDocumento8 paginePart 32 Welding Relatedravindra_jivaniNessuna valutazione finora
- Chemistry Form Three Q&a1Documento110 pagineChemistry Form Three Q&a1MajaningumbaoNessuna valutazione finora
- 83 WorksheetDocumento2 pagine83 WorksheetRishabh DhaulakhandiNessuna valutazione finora
- Mini Projek Meriam BuluhDocumento6 pagineMini Projek Meriam BuluheizharNessuna valutazione finora