Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
NAFLD Current Concepts: Brief Communication
Caricato da
deepusebinDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
NAFLD Current Concepts: Brief Communication
Caricato da
deepusebinCopyright:
Formati disponibili
Viral Hepatitis Foundation Bangladesh
International Journal of Hepatology
Brief Communication
NAFLD current concepts
*Deepak Amarapurkar
Bombay Hospital & Medical Research Centre, Mumbai, India *Correspondence to Gastroenterologist and Hepatologist, Bombay Hospital & Medical Research Centre, D 401/402 Ameya Society, New Prabhadevi Road, Prabhadevi, Mumbai 400 0025 India. Fax: +91 22 24368623, E-mail: amarapurkar@gmail.com
Introduction
Fatty liver disease was defined as more than 5% of the hepatocytes containing fat or more than 5% of the liver weight due to fat. The term non alcoholic steatohepatitis (NASH) was developed by Ludwig in 1979 to describe an alcoholic like liver disease that develops in people who do not drink alcohol. 1. The pathological spectrum of Non Alcoholic Fatty Liver Disease (NAFLD) ranges from simple steatosis to steatohepatitis and cirrhosis.. 1-3 .The risk factors for the development of NASH were identified as metabolic syndrome, obesity, type II diabetes mellitus (T2 DM), and dyslipidemia. By the late 1990s, NASH was conceptualized as part of metabolic syndrome. 1-5 NAFLD is becoming a major public health problem due to the rising prevalence of obesity and T2DM worldwide.6 NAFLD/NASH are now considered to be common causes of chronic liver disease, and increasing indication of liver transplantation and a possible cause of hepatocellular carcinoma (HCC) 2 Natural history of NAFLD is quite variable. There are some inherent draw backs in studying natural history of NAFLD. 6,7 Firstly there is no definitive laboratory test for diagnosis. Various studies published have different definitions. Published series using serial biopsies for histological progression have limitation of short follow up and selection bias. While cohort studies examining clinical outcomes have remarkably varied definition of NAFLD and clinical outcome may be shadowed by other diseases. Due to these conflicting results many workers considered NAFLD as a medical curiosity.6-11. While others consider it as major cause of chronic liver disease with impending epidemic.12-16 Over the last 5 years there is addition of valuable information on NAFLD. NAFLD is considered as a liver manifestation of a generalized fat storage disorder (metabolic syndrome).17
NAFLD patients may have increased risk of cardiovascular events, extra hepatic malignancies as compared to liver related mortality. 12-16 NAFLD is histologically categorized into simple steatosis and steatohepatitis with dichotomous natural history. Relatively benign prognosis for steatosis while progressive liver disease leading to cirrhosis and hepatocellular carcinoma (HCC) has been predicted for steatohepatitis. 6, 10,18-22 . Unfortunately there is no good non invasive marker which separates steatosis from steatohepatitis and hence liver biopsy still remains gold standard for prognostication of NAFLD based on serial biopsies 20-23. Studies disease progression in NAFLD is a) In patients with simple steatosis progression to cirrhosis may occur in 4 to 5% over a period of 8 to 15 years while steatohepatitis can progress to cirrhosis in over 25% patients over similar follow up period. B) At initial biopsy 5 to 20% patients with NAFLD may have cirrhosis c) Once cirrhosis develops cumulative probability of complications and need for the transplantation and mortality is just the same as hepatitis C related cirrhosis. Risk for factors rapid progression in NAFLD are type II diabetes, obesity, older age and metabolic syndrome.24 NAFLD is important cause of cryptogenic cirrhosis and may not be appreciated on histology as with disease progression steatosis may disappear. Many studies have shown that cryptogenic cirrhotics have the same risk profile as NAFLD and higher incidence of NAFLD is noted in these patients after liver transplantation.25 NAFLD and cryptogenic cirrhosis have been shown to have increased risk of HCC. Risk factor for HCC in NAFLD are liver cirrhosis, type II diabetes, obesity, metabolic syndrome, insulin resistance, older age and male gender.26-27. Association of diabetes with cryptogenic cirrhosis and HCC is well established HCC arising from NASH related cirrhosis and NASH without significant fibrosis has been documented in several case reports. 28-36
45
International Journal of Hepatology
Viral Hepatitis Foundation Bangladesh
Clinical manifestations of NAFLD
NAFLD is a silent disease more than half of the patients are diagnosed accidentally without any symptoms. 25 to 50 %patients may complain of right upper quadrant pain and equal no of patients may complain of fatigue. Some patients can present directly with development cirrhosis and it complications. Majority of the patients have normal physical examination. 25-50% may have clinically identifiable hepatomegaly. Mild to modest ALT, AST elevation is found in 25-50% of patients, remaining patients have normal liver enzymes. 37-45 Approach to patients with NAFLD in clinical practice is as follows : Fatty Liver can be defined on ultrasonography characteristics as given below in day to day clinical practice 46-47 Ultrasonographic criteria: - Presence of 2 of the following 3 with or without elevated ALT - A) Bright hepatic echo texture as compared to kidney and spleen - B) Blurring of hepatic veins - C) Loss of deep echo- discontinuous diaphragm. Magnetic resonance spectroscopy and liver histology may be more accurate than ultrasound but their utility in daily clinical practice remains unclear.
c) Exclusion of other known etiologies of cirrhosis of liver.
Exclusion of other causes of liver diseases
a) Alcohol consumption <20 gm/d (men), and 10gm/d (women). b) Exclusion of HBV and HCV infections (HBsAg, AntiHCV). c) Exclusion of Wilson and Autoimmune liver disease using appropriate tools. d) Absence of ingestion of Indigenous treatment in recent past (6 months).
Who should be screened for NAFLD?
NAFLD screening is recommended for patients with diabetes, obesity, dyslipidemia, patients with unexplained elevation of transaminases. Ideal screening tool for NAFLD is ultrasound Patients who are accidentally diagnosed to have fatty liver on ultrasound should undergo evaluation for obesity, central obesity, dyslipidemia and glucose intolerance and metabolic syndrome.47 What should be minimal assessment for patients with NAFLD? Once a patient is found to have suspected NAFLD, further evaluation including clinical examination and baseline investigations should be done to confirm the diagnosis of NAFLD, identify any underlying metabolic disorder, exclude other disorders and make an assessment of disease severity. The assessment of NAFLD patients should include the following: A careful history and physical examination (specially look for drugs, surreptious alcohol abuse, use of complementary and alternative medicine) Hematological tests complete blood count including platelet count. Anthropometry Biochemical tests including liver function test, serum creatinine Serological and immunological tests including tests for hepatitis B & C, ANA, serum ceruloplasmin Metabolic tests including glucose tolerance test, lipid profile, Insulin sensitivity Abdominal ultrasound Optional tests: Abdominal CT scan, Liver biopsy, biomarkers for liver fibrosis
Defining NASH
Diagnosis of NASH should be based on liver histology. Liver biopsy should be done in patients with NFALD in whom suspicion of NASH is raised. Presence of high risk factors for progression of the liver disease. [BMI >23Kg/ m2 for Asians, Age >50 yrs, raised AST, type2 DM, raised TG >150mg/dl)]. Liver biopsy should be graded and staged.(AASLD composite criteria, Hepatology2003)12 Currently no imaging modalities can differentiate NASH from NAFLD but in future fibro scan and serological markers may be able to obviate the need of liver biopsy,
Defining NAFLD associated cirrhosis
a) Clinical, biochemical, imaging and endoscopic evidence of cirrhosis liver. b) Presence of at least 2 factors of metabolic syndrome.
46
Viral Hepatitis Foundation Bangladesh
International Journal of Hepatology
These tests have been divided in to those which are essential for minimal assessment and those which are optional 47 Liver biopsy: it should be considered in situations when there is a diagnostic uncertainty, to assess histological disease severity in patients suspected to have advanced fibrosis, and in those undergoing laparoscopy, cholecystectomy, or bariatric surgery
alcohol consumption no more than occasional drink a month.
What is risk of statins in patients with NAFLD?
Statins (HMG-CoA reductase inhibitors) are prescribed in patients with NAFLD to treat associated hyperlipidemia and for the prevention of cardiovascular disease. Statins have been found to be safe in patients with NAFLD even in the presence of raised liver enzymes: hence can be prescribed safely without frequent LFT monitoring. Patients with NAFLD should avoid crash diet, herbal medicines, cannabises and nicotine. Patients with NAFLD related cirrhosis should be vaccinated for hepatitis A & B and should be screened for hepatocellular carcinoma. Patients should be monitored for metabolic abnormalities like fasting blood sugar, lipid profile and clinical parameters like height, weight and waist circumference to follow up intervals depending upon the patients age, family history, extent of obesity and previous findings Cardiovascular disease is commoner than liver disease as a cause of death in patients with NAFLD because of increased cardiovascular risk factors like metabolic syndrome and its components (obesity, type 2 DM, hypertension dyslipidemia). Evaluation of cardiac risk in patients with NAFLD is highly recommended.
Management of NAFLD
All patients diagnosed to have NAFLD after evaluation should be treated for abnormalities if present e.g. diabetes, and dyslipidemia and glucose intolerance. In case of doubt of severity of liver disease, patients should undergo liver biopsy. In the absence of diabetes and dyslipidemia but presence of NASH on histology, with abnormal glucose tolerance tests or presence of insulin resistance should be considered for treatment with insulin sensitizers. Treatment modalities are still evolving and no drug has been proved useful in the treatment of NAFLD in the absence of predisposing conditions. Currently life style modifications including dietary restrictions and exercise should be recommended as cornerstone of the therapy. The general recommendations for the diet are individualized to achieve energy deficit of 500 to 1000 kcal per day depending on the patients BMI, reduced saturated fat and total fat less than 30% of the total energy intake, reduced refined sugars and increase soluble fiber intake. Physical activities recommended 60 minutes per day at least 3 days a week and progressively increase the exercise to five times a week. Pharmacological and surgical methods of weight loss should be used in morbidly obese patients or moderately obese patients with significant risk factors.46-47 Bariatric surgery for the weight loss has been shown to be effective in improving NASH. Some preliminary data shows efficacy of metformin and glitazones in improving liver histology in patients with non diabetic NASH but still their routine use cannot be recommended at present. Various cytoprotective drugs like UDCA, antioxidants like vitamin E, probiotics, anti TNF alpha agents like pentoxiphylene, antifibortic drugs like losartan have been used in some preliminary studies but there is no evidence for their use in clinical practice. 46,47,48
References
1. Ludwig J, Viggiano TR, McGill DB, Oh BJ. Nonalcoholic steatohepatitis: Mayo Clinic experiences with a hitherto unnamed disease. Mayo Clin Proc 1980;55:4348. Bacon BR, Farahvash MJ, Janney CG, Neuschwander Tetri BA. Nonalcoholic steatohepatitis: an expanded clinical entity. Gastroenterology 1994;107:11039. Angulo P. Nonalcoholic fatty liver disease. N Engl J Med 2002;16:122131. Chitturi S, Abeygunasekera S, Farrell GC, Holmes-Walker J, Hui JM, Fung C, et al. NASH and insulin resistance: insulin hypersecretion and specific association with the insulin resistance syndrome. Hepatology 2002;35:3739. Yoon KH, Lee JH, Kim JW, Cho JH, Ko SH, Zimmet P, San HY. Epidemic obesity and type 2 diabetes in Asia. Lancet 2006;368:16818. Ratziu V, Poynard T, Assessing the outcome of Nonalcoholic steatohepatitis ? Its Time to Get Serious. Hepatology 2006;44:802-5. Day CP. Natural history of NAFLD: Remarkably benign in the absence of cirrhosis. Gastroenterology 2005;129:375-78.
2.
3. 4.
5.
6.
What are dos and donts for patients with NAFLD?
We should advise our patients with NAFLD to limit their
7.
47
International Journal of Hepatology
8. 9. Thomas v Harish K Are we overestimating the risks of NASH? Gastroenterology 2006;130:1015-16 author reply 1016-17. Loannou GN The natural history of NAFLD impressively unimpressive. Gastroenterology 2005;129:1805. Gastroenterology
Viral Hepatitis Foundation Bangladesh
Cryptogenic Cirrhosis and hepatocellular carcinoma. Chapter in International update on Hepatology, Ed Ramon Bataller, Permanyer Publication 2007. 26. Caldwell SH, Crespo DM Kang HS AL Qsaimi AM. Obesity and hepatocellular carcinoma Gastroenterology 2004;127:S97-103. 27. Qian Y and Fan JG. Obesity, fatty liver and liver cancer Hepatobiliary Pancreat Dis Int 2005;4:173-77. 28. Yoshioka Y, Hashimoto E, Yatsuji S et al Nonalcoholic steatohepatitis: cirrhosis, hepatocellular carcinoma, and burnt-out NASH J Gastroenterol 2004; 39: 1215-18. one case report. 29. Mori S, Yamasaki T, Sakaida T et al. Hepatocellular carcinoma with nonalcoholic steatohepatitis J Gastroenterol 2004;39:391-96 one Case Report. 30. Ikeda H, Suzzuki M, Takashi H, et al. Hepatocellular carcinoma with silent and cirrhotic non-alcoholic steatohepatitis, accompanying ectopic liver tissue attached to gallbladder Pathol Int 2006; 56:4045. one case report. 31. Shimada M, Hashimoto E, Taniai M et al. Hepatocellular carcinoma in patients with non-alcoholic steatohepatitis. J Hepatol 2002;37:154-60. six case reports. 32. Orikasa H, Ohyama R. Tsuka N et al. Lipid-rich clear-cell hepatocellular carcinoma arising in non-alcoholic steatohepatitis in a patient with diabetes mellitus J Submicrosc Cyto Pathol 2001;33:195-200. One case report. 33. Zen Y, Katayananaqi K, Tsuneyama K, et al. Hepatocellular carcinoma arising in non-alcoholic steatohepatitis Pathol Int 2001; 51:127-131. One case report. 34. Bullock RE, Zaitoun AM, Aithal GP et al. Association of non-alcoholic steatohepatitis without significant fibrosis with hepatocellular carcinoma J Hepatol 2004;41:685-86. Two case reports. 35. Ichikawa T, et al. J Gastroenterol Hepatol 2006;21: 1865-66. one without significant fibrosis, the other with some bridging fibrosis. 36. Hasizume H, et al. Euro Gastroenterol Hepatol 2007;19:827-34. six pts with cirrhosis, and 3 with mild fibrosis 37. Amarapurkar D, Amarapurkar A : Nonalcoholic Steatohepatitis : Clinicopathological Profiles, JAPI 2000;48:311-313. 38. Agarwal SR, Malhotra V, Sakhuja P, Sarin S, Clinical biochemical and histological profile of nonalcoholic steatohepatitis. Ind. J Gastroenterol 2001:20:183-186. 39. Amarapurkar D Das HS Chronic Liver Disease in diabetes mellitus. Trop Gastroenterol 2002;23:3-5. 40. Amarapurkar D, Patel N. Prevalence of Clinical Spectrum and natural history of nonalcoholic steatohepatitis with normal alanine aminotransferase values . Trop Gastroenterol 2004:25:130-134. 41. Madan K, Batra Y, Gupta SD, Chander B, Rajan KD, Tewatia MS, Panda SK, Acharya SK, Non alcoholic fatty liver disease may not be a severe disease at presentation among ASIAN INDIANS> World J Gastroenterol 2006;12:3400-05.
10. Tarantino G Is NAFLD an incidentaloma? 2006;130:1014-15.
11. Charlton M Cirrhosis and liver failure in non alcoholic fatty liver disease: Molehill or Mountain ? Hepatology 2008;47:1431-33. 12. Matteoni CA, Younossi ZM, Gramlich T, Boparai N Chang Liu Y, Mc Cullough AJ. Nonalcoholic fatty liver disease : a spectrum of clinical and pathological severity Gastroenterology 1999;116:141319. 13. Targher G, Bertolini L, Poli F et al Nonalcoholic fatty liver disease and risk of future cardiovascular events among type 2 diabetic patients. Diabetes 2005;54:3541-6. 14. Ekstedt M, Franzen LE, mathiesen UL et al Long term follow up of patients with NAFLD and elevated liver enzymes. Hepatology 2006;44:865-73. 15. Adams LA, Lymp JF, St Sauver J et al The natural history of nonalcoholic fatty liver disease a population based cohort study. Gastroenterology 2005;129:113-21. 16. Sanyal AJ, Banas C, Sargeant C et al Similarities and differences in outcome of cirrhosis due to nonalcoholic steatohepatitis and hepatitis C. Hepatology 2006;43:682-89. 17. Marchesini G, Bugianesi E, Forlani G et a. Non alcoholic fatty liver disease. Steatohepatitis, and the metabolic syndrome. Hepatology 2003:37;917-23. 18. Adams LA, Sanderson S, Lindor KD, Angulo P. The histological course of nonalcoholic fatty liver disease; a longitudinal study of 103 patients with sequential liver biopsies. J Hepatol 2005;42:132-8. 19. Fassio E, Alvarez E, Dominguez N, Landeira G, Longo C. Natural history of nonalcoholic steatohepatitis; A longitudinal study of repeat liver biopsies. Hepatology 2004;40:820-6. 20. Harrison Sa, Torgerson S, Hayashi PH. The natural history of nonalcoholic fatty liver disease: a clinical histopathological study. Am J Gastroenterol 2003;98:2042-7. 21. Hui AY, Wong VW, Chan HL, Liew CT, Chan IL, Chan FK, Sung JJ. Histological progression of non-alcoholic fatty liver disease in Chinese patients. Aliment Pharmacol Ther 2005;21:407-13. 22. Ong JP, Younossi ZM, Epidemiology and natural history of NAFLD and NASH Clin Liver Dis 2007:11:1-16. 23. Liou I, Kowdley KV Natural history of nonalcoholic statohepatitis. J Clin Gastroenterol 2006;40:Suppl1;S11-16. 24. Fan JG, Saibana T , Chitturi S, Kim BI, Sung JJY, Chuttaputti A & Asia Pacfic Working Party of NAFLD. What are the risk factors and settings for non-alcoholic fatty liver disease in Asia Pacific? J Gastroenterol & Hepatol 2007;22:794-800. 25. Caldwell SH, OLIVEIRA CPMS, de Lima VMR, Park SH. NASH,
48
Viral Hepatitis Foundation Bangladesh
42. Duseja A, DAs A, Das R, Dhiman RK, Chawla Y, Bhansali A, Kalra N. The clinicopathological profile of Indian patients with nonalcoholic fatty liver disease (NAFLD) is different from that in the West. Dig Dis Sci. 2007;52:2368-74. 43. Singh DK, Sakhuja P, Malhotra V, Gondal V, Sarin SK. Independent Predictors of steatohepatitis and fibrosis in Asian Indian Patients with non alcoholic steatohepatitis. Dig Dis Sci 2008;53:1967-76. 44. Duseja A, Nanda M, DAS A Das R Bhansali A, Chawla Y. Prevalence of obesity, diabetes mellitus and hyperlipidemia in patients with cryptogenic liver cirrhosis. Trop Gastroenterol 2004;25;15-17. 45. Amarapurkar DN, Patel ND, Kamani P. Impact of Diabetes mellitus on outcome of HCC. Annals of Hepatology 2008;7:148-151.
International Journal of Hepatology
46. Amarapurkar DN Approach to NAFLD in India in Non Alcoholic Fatty Liver Disease ECAB clinical update Gastroenterology Hepatology Eds Khanna S Elsevier New Delhi 2010 pp 57-75. 47. Asia Working Party on NAFLD: Executive Summary Guidelines for the assessment and management of Non-Alcoholic Fatty Liver Disease in the Asia-Pacific Region. J Gastroenterol Hepatol 2007;22:7757. 48. George J, Farrell GC. Practical approach to the diagnosis and management of people with fatty liver diseases. In: Farrell GC, Hall P, George J, McCullough AJ, eds. Fatty Liver Disease: NASH and Related Disorders Malden, MA: Blackwell, 2005:18193.
Brief Communication
Rationality and designing immune therapy against chronic hepatitis B virus infection
*Sheikh Mohammad Fazle Akbar1, Mamun-Al-Mahtab2, Sakirul Islam Khan3
1
Department of Medical Sciences, Toshiba General Hospital, Tokyo, Japan, 2Department of Hepatology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh, 3Department of Animal Science, Bangladesh Agricultural University, Mymensingh, Bangladesh *Correspondence to Principal Investigator, Department of Medical Sciences, Toshiba General Hospital, Tokyo, Japan E-mail: sheikh.akbar@toshiba.co.jp
Hepatitis B virus (HBV)-induced chronic hepatitis B (CHB) and subsequent complications (liver cirrhosis and hepatocellular carcinoma) represent major threats to human health worldwide. About 370 million people are chronically infected with the HBV worldwide. Several antiviral drugs are now used in patients with CHB, however, a welldesigned study for a National Institutes of Health (NIH, USA) consensus development conference that analyzed all randomized clinical trials with antiviral drugs in CHB patients from 1989 to 2008 have shown that no single drug treatment improved ultimate clinical outcomes or all intermediate outcomes of CHB, although improvements of some intermediate outcomes have been seen. However, adverse events during antiviral treatment occurred in about 50% patients. In addition, patients taking antiviral drugs should be periodically checked for viral, biochemical and immunological aspects of the HBV before, during and after cessation of therapy. However, the health care delivery system of developing country is unable to accomplish these. In this situation, mutant HBV may spread in community that may cause a devastating outcome.
The concept of immune therapy originated due to better understandings of pathogenesis of CHB and inefficacy of commercially-available antiviral drugs. Host immunity plays a pivotal role during induction, maintenance, and progression of liver damages in these patients. Again, the replication of the HBV can be minimized by host immune response. Thus, proper manipulation of host immunity may have therapeutic implications. Now, controversy remains about the design immune therapy in CHB patients. Studies have revealed that non antigen-specific immune modulators (gamma-interferon, interleukins, and growth factors) that upregulate or down regulate host immunity do not seem to be able stand the test of time as a better therapeutic endeavor in CHB patients (2). A new mode of immune therapeutic strategy surfaced in early 1990s in which hepatitis B vaccine containing HBsAg were used as a therapeutic vaccine for containment of HBV and reduction of liver damages by inducing HBV-specific immune responses in CHB patients. To optimize the therapeutic regimen, vaccine therapy was applied in murine model of HBV carrier state, HBV transgenic mice (HBV
49
Potrebbero piacerti anche
- DM No. 2022-0287 Updated Moa and Tor PRDPDocumento8 pagineDM No. 2022-0287 Updated Moa and Tor PRDPDRMC Infirmary100% (1)
- Evaluation and Management of Obesity-Related Nonalcoholic Fatty Liver DiseaseDocumento10 pagineEvaluation and Management of Obesity-Related Nonalcoholic Fatty Liver DiseaseVíctor V MayoralNessuna valutazione finora
- WHS PR Symposium - Non-Alcoholic Fatty Liver DiseaseDocumento63 pagineWHS PR Symposium - Non-Alcoholic Fatty Liver DiseaseWomen's Health SocietyNessuna valutazione finora
- DAFTAR PUSTAKA CHFDocumento39 pagineDAFTAR PUSTAKA CHFiganuryantiNessuna valutazione finora
- Thesis Protocol: DNB General MedicineDocumento30 pagineThesis Protocol: DNB General Medicinegattu santoshNessuna valutazione finora
- Fatty Liver and MSDocumento16 pagineFatty Liver and MSAljon Anies100% (1)
- Piis001650852200628x PDFDocumento12 paginePiis001650852200628x PDFAriana HurtadoNessuna valutazione finora
- 1.Dr. Hussnain Ali Shah GROWING ISSUES OF NAFLD Sri Lanka 2017Documento27 pagine1.Dr. Hussnain Ali Shah GROWING ISSUES OF NAFLD Sri Lanka 2017Hussain AliNessuna valutazione finora
- IntJMedPublicHealth32111-7924347 220043Documento0 pagineIntJMedPublicHealth32111-7924347 220043budi_26690Nessuna valutazione finora
- NafldDocumento30 pagineNafldprabhatguyNessuna valutazione finora
- Nonalcoholic Fatty Liver - StatPearls - NCBI Bookshelf PDFDocumento6 pagineNonalcoholic Fatty Liver - StatPearls - NCBI Bookshelf PDFMr BrewokNessuna valutazione finora
- Gut and Liver NASH Inflammatory DisorderDocumento23 pagineGut and Liver NASH Inflammatory Disordershiv_chitturi1295Nessuna valutazione finora
- Management of Nonalcoholic Fatty Liver Disease in Patients With Type 2 Diabetes: A Call To ActionDocumento12 pagineManagement of Nonalcoholic Fatty Liver Disease in Patients With Type 2 Diabetes: A Call To ActionNur ArafahNessuna valutazione finora
- A Clinical Overview of Non-Alcoholic Fatty Liver Disease A GuideDocumento12 pagineA Clinical Overview of Non-Alcoholic Fatty Liver Disease A GuideAnindya RosmaNessuna valutazione finora
- Hígado Graso No AlcohólicoDocumento16 pagineHígado Graso No AlcohólicoAntonio Martinez GarciaNessuna valutazione finora
- Preamble: Podcast Interview: - Also Available On ItunesDocumento18 paginePreamble: Podcast Interview: - Also Available On ItuneswawanpecelNessuna valutazione finora
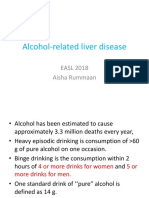
- Alcohol Related Liver Disease Rev.01Documento71 pagineAlcohol Related Liver Disease Rev.01rummaan17100% (1)
- Watanabe2015 - Article - Evidence-basedClinicalPracticeDocumento14 pagineWatanabe2015 - Article - Evidence-basedClinicalPracticemariam.husseinjNessuna valutazione finora
- Diagnosis Nafld 2016Documento15 pagineDiagnosis Nafld 2016AfifMaulanaFirmansyahNessuna valutazione finora
- The Epidemiology of Non-Alcoholic Fatty Liver Disease: Stefano BellentaniDocumento4 pagineThe Epidemiology of Non-Alcoholic Fatty Liver Disease: Stefano BellentaniPrabjot SehmiNessuna valutazione finora
- Lipid and Glucose Profile in Non-Alcoholic Fatty Liver Disease: A Hospital Based StudyDocumento8 pagineLipid and Glucose Profile in Non-Alcoholic Fatty Liver Disease: A Hospital Based StudyijasrjournalNessuna valutazione finora
- Non-Alcoholic Fatty Liver DiseaseDocumento15 pagineNon-Alcoholic Fatty Liver DiseaseKurnia pralisaNessuna valutazione finora
- Nonalcoholic Fatty Liver Disease (Nafld) Challenge To DiagnosisDocumento31 pagineNonalcoholic Fatty Liver Disease (Nafld) Challenge To DiagnosisMohamed NaguibNessuna valutazione finora
- Epidemia HgnaDocumento8 pagineEpidemia HgnaAntonio Alexis Bustos TorresNessuna valutazione finora
- 1 s2.0 S0261561422002874 MainDocumento12 pagine1 s2.0 S0261561422002874 Maindr. Nur'aini HasanNessuna valutazione finora
- NAFLD HarrisonDocumento2 pagineNAFLD HarrisonJesly CharliesNessuna valutazione finora
- NAFLD in DM Banjarmasin Edit NEWDocumento74 pagineNAFLD in DM Banjarmasin Edit NEWZayed NorwantoNessuna valutazione finora
- Complete Resolution of Nonalcoholic Fatty LiverDocumento32 pagineComplete Resolution of Nonalcoholic Fatty LiverRegir KurNessuna valutazione finora
- Evaluation Prognosis Patients CirrhosisDocumento13 pagineEvaluation Prognosis Patients Cirrhosisdini yuhelfiNessuna valutazione finora
- Journal Pre-Proof: GastroenterologyDocumento22 pagineJournal Pre-Proof: GastroenterologyntnquynhproNessuna valutazione finora
- Histopathology of Nonalcoholic Fatty Liver Disease - Nonalcoholic SteatohepatitisDocumento18 pagineHistopathology of Nonalcoholic Fatty Liver Disease - Nonalcoholic SteatohepatitisLaia BertranNessuna valutazione finora
- Management of Liver CirrhosisDocumento7 pagineManagement of Liver Cirrhosispet_trinNessuna valutazione finora
- Journal of Internal Medicine - 2022 - Paternostro - Current Treatment of Non Alcoholic Fatty Liver DiseaseDocumento15 pagineJournal of Internal Medicine - 2022 - Paternostro - Current Treatment of Non Alcoholic Fatty Liver DiseaseHunny BunnyNessuna valutazione finora
- Art 3 Non-Alcoholic Fatty Liver Disease ADocumento10 pagineArt 3 Non-Alcoholic Fatty Liver Disease AAlexsander SarmientoNessuna valutazione finora
- The Role of Long Non-Coding Rnas (Lncrnas) in The Development and Progression of Fibrosis Associated With Nonalcoholic Fatty Liver Disease (Nafld)Documento15 pagineThe Role of Long Non-Coding Rnas (Lncrnas) in The Development and Progression of Fibrosis Associated With Nonalcoholic Fatty Liver Disease (Nafld)Dindin GarciaNessuna valutazione finora
- Nafld: DR. Shatdal Chaudhary MDDocumento42 pagineNafld: DR. Shatdal Chaudhary MDWaqar AhmedNessuna valutazione finora
- HIgado GrasoDocumento6 pagineHIgado GrasoWilson Suarez VenturaNessuna valutazione finora
- Advances in Understanding The Progression of Non-Alcoholic Fatty Liver Disease To Non-Alcoholic Steatohepatitis: A Comprehensive ReviewDocumento7 pagineAdvances in Understanding The Progression of Non-Alcoholic Fatty Liver Disease To Non-Alcoholic Steatohepatitis: A Comprehensive ReviewInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- DR T Dinesh Guide DR Baba YelkeDocumento27 pagineDR T Dinesh Guide DR Baba YelkeDinesh AshwinNessuna valutazione finora
- Isolated Hepatic SarcoidosisDocumento6 pagineIsolated Hepatic Sarcoidosiskabal321Nessuna valutazione finora
- Acute Alcoholic HepatitisDocumento18 pagineAcute Alcoholic HepatitisMariana NavarroNessuna valutazione finora
- Predisposing Conditions, Management and Prevention of Chronic Kidney DiseaseDocumento52 paginePredisposing Conditions, Management and Prevention of Chronic Kidney DiseaseSaad MotawéaNessuna valutazione finora
- Ald & MasldDocumento19 pagineAld & MasldAli SafaaNessuna valutazione finora
- Cause, Pathogenesis, and Treatment of Nonalcoholic SteatohepatitisDocumento10 pagineCause, Pathogenesis, and Treatment of Nonalcoholic SteatohepatitisGabriel VargasNessuna valutazione finora
- JCTH 10 0979Documento7 pagineJCTH 10 0979Svt Mscofficial2Nessuna valutazione finora
- Part 9. Approach To Chronic Kidney Disease Using These GuidelinesDocumento8 paginePart 9. Approach To Chronic Kidney Disease Using These GuidelinesSudjarwo AntonNessuna valutazione finora
- Metabolic-Associatedfatty Liverdiseaseanddiabetes: A Double WhammyDocumento16 pagineMetabolic-Associatedfatty Liverdiseaseanddiabetes: A Double WhammyFarjana NajninNessuna valutazione finora
- Specific Nursing Care Rendered in Hepatic Encephalopathy Contemporary Review and New Clinical Insights 2167 1168 1000264Documento7 pagineSpecific Nursing Care Rendered in Hepatic Encephalopathy Contemporary Review and New Clinical Insights 2167 1168 1000264zeljko_vlaisavl4859Nessuna valutazione finora
- Performance of Non-Invasive Models of Fibrosis in Predicting Mild To Moderate Fibrosis in Patients With Non-Alcoholic Fatty Liver DiseaseDocumento8 paginePerformance of Non-Invasive Models of Fibrosis in Predicting Mild To Moderate Fibrosis in Patients With Non-Alcoholic Fatty Liver DiseaseChausarPutraBenagilNessuna valutazione finora
- Commentary: Gamma Glutamyl Transferase: A Novel Cardiovascular Outfit For An Old Liver TestDocumento4 pagineCommentary: Gamma Glutamyl Transferase: A Novel Cardiovascular Outfit For An Old Liver TestPrasanna BabuNessuna valutazione finora
- Mechanism of NAFLD Dev & Therapeutic Strategies - Arun SanyalDocumento15 pagineMechanism of NAFLD Dev & Therapeutic Strategies - Arun SanyalParul SoodNessuna valutazione finora
- Articol RJMEDocumento6 pagineArticol RJMELigia Ariana BancuNessuna valutazione finora
- Non-Invasive Diagnosis of NASH and NAFLDDocumento17 pagineNon-Invasive Diagnosis of NASH and NAFLDRaeni Dwi PutriNessuna valutazione finora
- Summary. Nonalcoholic Fatty Liver (NAFL) or Nonalcoholic Fatty Liver DiseaseDocumento43 pagineSummary. Nonalcoholic Fatty Liver (NAFL) or Nonalcoholic Fatty Liver DiseaseAngga Julyananda PradanaNessuna valutazione finora
- Endocrino Diabet Metabol - 2020 - Hernandez Roman - The Role of Noninvasive Biomarkers in Diagnosis and RiskDocumento9 pagineEndocrino Diabet Metabol - 2020 - Hernandez Roman - The Role of Noninvasive Biomarkers in Diagnosis and Riskhoria_minea5905Nessuna valutazione finora
- Radiologic Evaluation of Nonalcoholic Fatty Liver DiseaseDocumento12 pagineRadiologic Evaluation of Nonalcoholic Fatty Liver DiseasePuputNessuna valutazione finora
- Piis0021915019301169 PDFDocumento9 paginePiis0021915019301169 PDFWickedSilverNessuna valutazione finora
- 7cholestatic Liver DiseaseDocumento9 pagine7cholestatic Liver DiseaseDaniel Fernando LozanoNessuna valutazione finora
- Hepatology Communications - 2022 - Vieira Barbosa - Fibrosis 4 Index As An Independent Predictor of Mortality andDocumento15 pagineHepatology Communications - 2022 - Vieira Barbosa - Fibrosis 4 Index As An Independent Predictor of Mortality andjim.palmarbNessuna valutazione finora
- Ahmed Ali - CKDDocumento20 pagineAhmed Ali - CKDAhmed AliNessuna valutazione finora
- Non-Alcoholic Fatty Liver Disease: A Practical GuideDa EverandNon-Alcoholic Fatty Liver Disease: A Practical GuideGeoffrey C. FarrellNessuna valutazione finora
- Jurisprudence Direct Exam of Expert WitnessDocumento9 pagineJurisprudence Direct Exam of Expert WitnessxquisiteDNessuna valutazione finora
- PEBC Qualifying Exam References and Resources ListDocumento5 paginePEBC Qualifying Exam References and Resources ListAnkit ShahNessuna valutazione finora
- Activity 1Documento2 pagineActivity 1cherrielNessuna valutazione finora
- Consolidated Guidelines OnDocumento594 pagineConsolidated Guidelines OnRICHARD EDUARDO FERNANDEZ SAENZNessuna valutazione finora
- MWF Community Resource Guide - Atlanta - 2014Documento32 pagineMWF Community Resource Guide - Atlanta - 2014MuslimWellnessNessuna valutazione finora
- Artifact 1Documento15 pagineArtifact 1api-420188600Nessuna valutazione finora
- Physical Education Cambridge Progression Test P1 - ST6 (2022)Documento14 paginePhysical Education Cambridge Progression Test P1 - ST6 (2022)Givemore MuromboNessuna valutazione finora
- Babe 2Documento17 pagineBabe 2Sathish SizzyNessuna valutazione finora
- Treatment and Prevention of LeptospirosisDocumento7 pagineTreatment and Prevention of LeptospirosisSherry FeliciaNessuna valutazione finora
- Somatoform Disorders FinalDocumento28 pagineSomatoform Disorders Finalapi-281484882Nessuna valutazione finora
- Agujero MacularDocumento39 pagineAgujero MacularKate CastañoNessuna valutazione finora
- Cognitive - Behavioural Strategies in Crisis InterventionDocumento3 pagineCognitive - Behavioural Strategies in Crisis InterventionHugo Gonzalez EnriquezNessuna valutazione finora
- Carmen Best Background InformationDocumento15 pagineCarmen Best Background InformationKING 5 NewsNessuna valutazione finora
- Renal Drug StudyDocumento3 pagineRenal Drug StudyRiva OlarteNessuna valutazione finora
- RRR PosterDocumento1 paginaRRR Posterndaru GreenNessuna valutazione finora
- Bhutan, Keeping PromisesDocumento44 pagineBhutan, Keeping Promisesstevens106Nessuna valutazione finora
- Do's and Dont's in Writing Research QuestionsDocumento2 pagineDo's and Dont's in Writing Research QuestionsLisandrea BrownNessuna valutazione finora
- Posts Advertisement With The Closing Date 15 June 2023 - KZN RegionDocumento24 paginePosts Advertisement With The Closing Date 15 June 2023 - KZN RegionNtobeko LihasiNessuna valutazione finora
- Diabetes and Its Management: Rohit ThanageDocumento10 pagineDiabetes and Its Management: Rohit ThanageRohit ThanageNessuna valutazione finora
- Disaster ManagementDocumento21 pagineDisaster ManagementLokesh Ravi TejaNessuna valutazione finora
- Hse Plan 3Documento14 pagineHse Plan 3YcRij SeYerNessuna valutazione finora
- Safety Quize 2014 With AnsDocumento7 pagineSafety Quize 2014 With AnsMANOUJ GOELNessuna valutazione finora
- Soal PAS BIG Xi, SMT 3, OnlineDocumento10 pagineSoal PAS BIG Xi, SMT 3, OnlineRivaldi Lukman HakimNessuna valutazione finora
- Doctor's Appointment Portal: Project Report OnDocumento62 pagineDoctor's Appointment Portal: Project Report OnheamNessuna valutazione finora
- SMR August 19 (Rengat - Tembilahan, Sect 2) PDFDocumento28 pagineSMR August 19 (Rengat - Tembilahan, Sect 2) PDFDoo PLTGUNessuna valutazione finora
- Medical Emergencies in Dental Practice: A Review: July 2016Documento18 pagineMedical Emergencies in Dental Practice: A Review: July 2016AnushkaNessuna valutazione finora
- VSO Our Side of The Story Uganda - Full ReportDocumento68 pagineVSO Our Side of The Story Uganda - Full ReportVSONessuna valutazione finora
- Information Booklet 1 PDFDocumento40 pagineInformation Booklet 1 PDFVandana RanaNessuna valutazione finora
- Negative Impact of Social Media: A Qualitative Inquiry Towards Student of Arellano University Jose Rizal CampusDocumento30 pagineNegative Impact of Social Media: A Qualitative Inquiry Towards Student of Arellano University Jose Rizal Campusisabel ysaNessuna valutazione finora