Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Chap 360 - Meningtis, Encephalitis, Brain Abscess, Empyema
Caricato da
api-3704562100%(1)Il 100% ha trovato utile questo documento (1 voto)
1K visualizzazioni6 pagineBacterial meningitis is an acute purulent infection within the subarachnoid space. It may result to decreased consciousness, seizures, raised ICP and stroke. Lysis of bacteria with the subsequent release of cell wall components is the initial step in the induction of the inflammatory response.
Descrizione originale:
Titolo originale
chap 360 -- meningtis, encephalitis, brain abscess, empyema
Copyright
© Attribution Non-Commercial (BY-NC)
Formati disponibili
DOC, PDF, TXT o leggi online da Scribd
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoBacterial meningitis is an acute purulent infection within the subarachnoid space. It may result to decreased consciousness, seizures, raised ICP and stroke. Lysis of bacteria with the subsequent release of cell wall components is the initial step in the induction of the inflammatory response.
Copyright:
Attribution Non-Commercial (BY-NC)
Formati disponibili
Scarica in formato DOC, PDF, TXT o leggi online su Scribd
100%(1)Il 100% ha trovato utile questo documento (1 voto)
1K visualizzazioni6 pagineChap 360 - Meningtis, Encephalitis, Brain Abscess, Empyema
Caricato da
api-3704562Bacterial meningitis is an acute purulent infection within the subarachnoid space. It may result to decreased consciousness, seizures, raised ICP and stroke. Lysis of bacteria with the subsequent release of cell wall components is the initial step in the induction of the inflammatory response.
Copyright:
Attribution Non-Commercial (BY-NC)
Formati disponibili
Scarica in formato DOC, PDF, TXT o leggi online su Scribd
Sei sulla pagina 1di 6
CHAPTER 360: MENINGITIS, inflammatory reaction induced by
ENCEPHALITIS, BRAIN ABSCESS, the invading bacteria.
EMPYEMA • Lysis of bacteria with the
subsequent release of cell wall
• Prodrome of fever, headache are components into the subarachnoid
benign until altered consciousness, space is the initial step in the
focal neurologic deficits or seizures induction of the inflammatory
appear. response.
• Approach to the patient: first • Cytokine response is followed by
identify if infection is in the an increase in CSF protein
subarachnoid space. concentration and leukocystosis.
• Viral: encephalitis • Much of the pathophysiology of
• Bacterial/ fungal: cerebritis or bacterial meningitis is a direct
abscess consequence of elevated levels of
• Nuchal rigidity is the CSF cytokines and chemokines.
pathognomonic sign of meningeal TNF and IL1 act synergistically to
irritation. increase the permeability of the
• Kernigs’ sign blood brain barrier resulting in
vasogenic edema and the leakage
• Brudzinski’s sign
of serum proteins into the
• Failure of a patient suspected with subarachnoid space.
viral encephalitis to improve should • During the very early stages of
prompt reevaluation.
meningitis there is an increase in
• Bacterial meningitis is an acute cerebral blood flow followed by a
purulent infection within the decrease in blood flow and loss of
subarachnoid space. cerebrovascular autoregulation.
• Bacterial meningitis may result to • Combination of cytotoxic,
decreased consciousness, vasogenic and interstitial edema
seizures, raised ICP and stroke. lead to increased ICP and coma.
• Meningoencephalitis – the • Clinical presentation: clinical triad
parenchyma, meninges ad of meningitis: fever, headache and
subarachnoid nuchal rigidity.
• Bacterial meningitis is the most • Focal seizures may be due to focal
common form of suppurative CNS arterial ischemia, infarction, and
infection. cortical venous thrombosis with
• S. pneumoniae is the most hemorrhage or focal edema.
common cause in adults >20 • Generalized seizures or status
• N. meningitides is common in ages epilepticus may be due to
2-20 with petechial and purpuric hyponatremia and cerebral anoxia.
lesions. • Raised ICP is an expected
• Group B or S. agalactiae complication and is the major
predominates in neonates and cause of obtundation and coma.
elderly >50 • Signs of increased ICP are:
• Listeria predominates in neonates
papilledema, dilated poorly reactive
and pregnant women due to pupils, 6th nerve palsies,
organisms in ready to eat foods decerebrate posturing and
• H. influenzae in unvaccinated Cushing’s reflex ( bradycardia,
children hypotension, irregular respirations)
• Staph aureus and CN-staph are • Most disastrous complication is
causes of infection following an cerebral herniation.
invasive neurosurgical procedure • Diagnosis: made by examination of
• Pathophysiology: Bacteria are able CSF
to avoid phagocytosis because of a • Classic CSF abnormalities:
polysaccharide capsule. leukocystosis (>100 cells),
• A critical event in the pathogenesis decreased glucose <2.2 mmol/L or
of bacterial meningitis is the serum glucose of <0.4, increased
protein concentration >0.45 g/L and Chemoprophylaxis with Rifampicin.
increased opening pressure >180 Rifampicin is CI in pregnant.
mmH2O • Pneumococcal meningitis:
• CSF latex agglutination test has a cephalosporin + vancomycin, MICs
specificity of 95-100% for S. > 0.5 ug/mL treat with cefotaxime
pneumoniae and N. meningitides, or ceftriaxone, MICs of >1 ug/mL
so a + test is virtually diagnostic of vancomycin
bacterial meningitis. • Patients with penicillin and
• Limulus amoebocyte lysate assay cephalosporin resistant strains of S.
is a rapid diagnostic test for the pneumoniae who don’t respond to
detection of gram – endotoxin in vancomycin may be given
CSF intraventricular vancomycin
• MRI is preferred than Ct because of • L. monocytogenes meningitis:
its superiority in demonstrating
ampicillin/ gentamicin. In penicillin
areas of cerebral edema and
allergic patients give cotrimoxazole
ischemia,
• Staphylococcal meningitis: nafcillin,
• Differential diagnosis: findings on
for MRSA use vancomycin
CSF studies, neuroimaging and
EEG distinguishes HSV • Gram – bacillary meningitis: 3rd gen
encephalitis from bacterial cephalosporins but with P.
meningitis aeruginosa use ceftazidime
• Viral CSF infections: lymphocytic • Adjunctive therapy:
pleocytosis with a normal glucose Dexamethasone
• Bacterial: PMN pleocytosis and • For increased ICP: elevate head to
hypoglycorrhachia 30-45 degrees, intubation,
• Subacutely evolving meningitis may hyperventilation and mannitol.
on occasion be considered as • Acute Viral Meningitis: fever,
differentia diagnosis of acute headache and meningeal irritation
meningitis. Principal causes include accompanied by arthralgia, malaise
M. tuberculosis, C. neoformans, H. and anorexia.
capsulatum, C. immitis and T. • Photophobia and pain on moving
pallidum the eyes.
• Treatment: bacterial meningitis is a • Kernig’s and brudzinski’s sign are
medical emergency. absent.
• Goal is to begin antibiotic therapy • Enteroviruses account for 75-90%
within 60 min. of aseptic meningitis.
• Ceftriaxone + vancomycin or • Laboratory Diagnosis of CSF:
Cefotaxime + vancomycin lymphocytic pleocytosis and slightly
• Cefepime has greater activity elevated protein concentration with
against Enterobacter and P. normal glucose.
aeruginosa • As a rule, lymphocytic pleocytosis
• Ampicillin to cover Listeria with a low glucose concentration
• In meningitis following should suggest fungal, listerial or
neurosurgical procedures: tuberculous meningitis.
vancomycin and ceftazidime • PCR – diagnostic procedure of
• Ceftazidime is the only choice
cephalosporin with adequate • HSV PCR- for recurrent episodes
activity against CNS infections with of aseptic meningitis
P. aeruginosa. • Oligoclonal bands can also be
• Meropenem is a carbapenem found in noninfectious neurologic
antibiotic that is highly active in diseases.
vitro against Listeria, P. aeruginosa • Enterovirus infection can have
and penicillin resistant exanthema, foot and mouth
pneumococci. disease, herpangina, pleurodynia,
• Meningococcal meningitis: Pen G, myopericarditis and hemorrhagic
if resistant Ceftriaxone.
conjunctivitis ( stigmata of • Laboratory: lymphocytic
enterovirus infection) pleocytosis, mildly elevated protein
• Arbovirus – bird deaths and normal glucose concentration.
• HSV meningitis- HSV2, Mollaret’s • Hemorrhagic encephalitis is seen in
meningitis HSV and Colorado tick fever virus.
• VZV meningitis: chickenpox and • CSF PCR is the primary diagnostic
shingles, acute cerebral ataxia. test for CNS infections caused by
• EBV infections may also produce CMV, EBV, and VZV.
aseptic meningitis characterized by • Demonstration of WNV IgM
atypical lymphocytosis in peripheral antibodies is diagnostic of WNV
blood. encephalitis.
• HIV meningitis: aseptic meningitis • Focal neurologic findings always
is a common manifestation. point to HSV as the etiologic agent.
• Mumps: orchitis, oophoritis, • Brain biopsy was once considered
parotitis and pancreatitis, also the gold standard.
elevations in serum lipase and • Differential Diagnosis: differentiate
amylase from vascular diseases, abscess,
• LCMV infection: exposure to house empyema, fungal, parasitic,
mice presenting with leucopenia, rickettsial, tuberculous infections,
thrombocytopenia or abnormal liver tumors, Reye’s syndrome, toxic
function tests. encephalopathy, subdural
• Treatment is symptomatic hematoma and SLE.
• Hyponatremia may develop due to • Primary amebic
inappropriate vasopressin secretion meningoencephalitis – Naegleria
(SIADH) fowleri
• Oral acyclovir may be of benefit in • Subacute or chronic granulomatous
meningitis caused by HSV, EBV or amebic meningoencephalitis –
VZV Acanthamoeba and Balamuthia
• Patients with HIV should be given • Raccoon exposure
HAART. • Bartonella sp- agents of cat scratch
• Vaccination is an effective method fever which is the most common
• Prognosis: prognosis for full bacterial infection mimicking viral
recovery from viral meningitis is encephalitis.
excellent. • Involvement of the inferomedial
• Viral encephalitis: involvement of frontotemporal regions of the brain
the brain parenchyma is present in HSV encephalitis.
• Involvement of the spinal cord is • If deep gray matter, basal ganglia
encephalomyelitis and thalamus are affected suspect
• Nerve root involvement is flaviviruses.
encephalomyeloradiculitis • Deaths in crows and corvid birds
• Confusion, altered level of are due to WNV.
consciousness, hallucinations, • Treatment: acyclovir is the
agitations, personality change, treatment for HSV.
behavioral disorders and a frankly • Ganciclovir and foscarnet are used
psychotic state is seen. for CMV related CNS infections.
• Focal findings include: ataxia, • Cidofovir if it doesn’t respond to
aphasia, hemiparesis Ganciclovir.
• Temperature dysregulation, • Side effects of Ganciclovir:
diabetes insipidus, SIADH granulocytopenia and
• Most common viruses causing thrombocytopenia, retinal
sporadic cases are HSV1, VZV and detachment.
enteroviruses. • IV Ribavarin for California
• Epidemics of encephalitis are encephalitis (Lacrosse) virus.
caused by arboviruses. • Side effect: hemolysis, anemia
• Subacute Meningitis: typically
manifest with unrelenting
headache, stiff neck, fever and • No therapy is available.
lethargy • Brain abscess – is a focal
• Common causative agents: M. suppurative infection within the
tuberculosis, C. neoformans, H brain parenchyma typically
capsulatum, C. immitis, T. pallidum. surrounded by a vascularized
• The most common pathogen capsule.
causing fungal encephalitis is C. • Caused by Toxoplasma,
neoformans. Aspergillus, Nocardia,
• T. pallidum invades the CNS in the Mycobacteria and C. neoformans
early course of the illness, affecting • Taenia solium in Latin America
cranial nerves VII & VIII. • Direct spread from a contiguous
• Culture remains to be the gold cranial site of infection such as
standard in the diagnosis of paranasal sinusitis, otitis media,
tuberculous meningitis mastoiditis or dental infection
• Eosinophils may be seen in C. • Otogenic abscesses usually in the
immitis meningitis. temporal lobe.
• Cryptococcal polysaccharide • Cryptogenic abscesses are due to
antigen tests for cryptococcal dental infections.
meningitis is highly sensitive. • Enterobacteriaceae and P.
• Diagnosis of syphilic meningitis is aeruginosa are important causes of
made when a reactive treponemal abscesses associated with urinary
test is associated with lymphocytic sepsis.
pleocytosis. • Tetralogy of Fallot
• A negative CSF FTA ABS or MHA • Intact brain is resistant to
TP rules out neurosyphilis. infections; only in the presence of
• Treatment: initial therapy of ischemia, hypoxia and infarct will it
Rifampicin, isoniazid, pyrazinamide be able to be penetrated.
and ethambutol. • Early cerebritis – infiltrates
• Dexamethasone if with • Late cerebritis- pus formation
hydrocephalus.
• 3rd stage: is early capsule formation
• C. neoformans- amp B and
• Late capsule stage characterized
flucytosine
with a well formed necrotic center
• H. capsulatum- amp B and
• Marked gliosis will cause the
itraconazole
• C. immitis- IV amp B sequelae – seizures.
• Brain abscess presents as a mass.
• The most common complication of
• Triad: fever, focal Neurologic
fungal meningitis is hydrocephalus.
• Syphilitic meningitis is treated with deficits and fever
• Headache is the most common
aq. Pen G.
complaint.
• Chronic Encephalitis: Progressive
• Hemiparesis seen in frontal lobe
multifocal leukoencephalopathy is
pathologicaly characterized by lesion
multifocal areas of demyelination. • Dysphasia is seen in temporal lobe
• Astrocytes and oligoendrocytes are lesion
enlarged. • Nystagmus and ataxia are
• PCR analysis is diagnostic. cerebellar lesions.
• No therapy is available • MRI is used for diagnosis.
• Subacute Sclerosing • When fever is absent suspect
Panencephalitis: measles tumors.
• Treatment: Isoprinosine and • Treat with 3rd gen cephalosporins,
interferons ceftazidime for P. aeruginosa and
• Progressive Rubella vancomycin for staphylococci.
Panencephalitis: primarily affects • Non bacterial causes of infectious
males with congenital rubella focal cns lesions:
syndrome. neurocysticercosis is the most
common parasitic disease of the • 3rd gen cephalosporins+nafcillin or
CNS worldwide vancomycin+ metronidazole
• T. gondi from cat feces • Ceftazidime is used for
• Associated with resolution of the neurosurgical patients.
inflammatory response • Suppurative Thrombophlebitis- is
• Toxoplasma infection is usually septic venous thrombosis of cortical
asymptomatic. veins and sinuses
• MRI or CT scans. • Occur as a complication of bacterial
• Parenchymal calcifications and meningitis, SDE, epidural abscess.
scolex ca be visualized. • Superior sagittal sinus is the largest
• Albendazole and praziquantel. of the venous sinuses.
• CNS toxoplasmosis is treated with • Bacterial meningitis is a common
combination of sulfadiazine + predisposing condition for septic
pyrimethamine thrombosis of the superior sagittal
• Folinic acid to prevent sinus.
megaloblastic anemia • Thrombosis of the superior sagittal
• Clindamycin + pyrimethamine are sinus is often associated with
an alternative for patients who thrombosis of superior cortical
cannot tolerate sulfadiazine. veins and small parenchymal
• Subdural empyema – is a rare hemorrhages. Septic thrombosis of
disorder characterized by a the superior sagittal sinus with
collection of pus between the dura headache, fever, nausea, vomiting
and arachnoid membrane. and confusion and seizures.
• Sinusitits is the most common • There maybe a rapid development
predisposing condition and typically to stupor or coma.
involves the frontal sinuses. • Nuchal rigidity, Kernig’s and
• Young males are more affected. Brudzinski’s may be present.
• Also may develop as complication • Septic cavernous sinus thrombosis
of head trauma or neurosurgery presents with fever, headache
• Presents with fever and frontal and retroorbital pain and
progressively worsening headache diplopia.
• Headache is the most common • Classic signs are ptosis, proptosis,
complaint chemosis and extraocular
• Contralateral hemiparesis and dysmotility due to deficits of cranial
hemiplegia is the most common nerves II, IV and VI, hyperesthesia
focal Neurologic deficit. of the 5th nerve and decreased
• MRI or CT scan. CT may show a corneal reflex, papilledema.
crescent shaped hypodensity over • Headache and earache are the
one or both hemispheres. most frequent symptoms of
• SDE is a medical emergency. transverse sinus thrombosis. it may
• Burr-hole drainage or craniotomy is also present with Gradinego’s
syndrome ( facial pain ).
the management.
• Sigmoid sinus and internal jugular
• 3rd gen cephalosporins and vein thrombosis may present with
vancomycin and metronidazole. neck pain.
• Epidural abscess- is a suppurative • Cerebral angiography for definitive
infection occurring in the potential diagnosis.
space between the inner skull table • Septic venous sinus thrombosis is
and dura. treated with antibiotics and
• Develops as a complication of hydration.
craniotomy or infectious from an • Dose adjusted heparin
area with osteomyelitis.
• Aseptic venous sinus thrombosis
• Staph is usually the etiologic agent.
through urokinase therapy, rTPa
• MRI is the procedure of choice. and IV heparin.
• Neurosurgical drainage is
indicated.
Liz IIIB
Potrebbero piacerti anche
- Gender SensitivityDocumento10 pagineGender Sensitivityapi-3704562100% (10)
- SURGERYDocumento36 pagineSURGERYapi-3704562Nessuna valutazione finora
- PulmoconDocumento64 paginePulmoconapi-3704562100% (1)
- Gender SensitivityDocumento2 pagineGender Sensitivityapi-370456296% (26)
- Dr. JTG Presentation (Diarrheas)Documento33 pagineDr. JTG Presentation (Diarrheas)api-3704562Nessuna valutazione finora
- Kaplan Community EpidemDocumento3 pagineKaplan Community Epidemapi-3704562Nessuna valutazione finora
- Vasculitis SyndromesDocumento9 pagineVasculitis Syndromesapi-3704562Nessuna valutazione finora
- PlasticischwartsDocumento3 paginePlasticischwartsapi-3704562Nessuna valutazione finora
- Neurosurgery Case 1Documento111 pagineNeurosurgery Case 1api-3704562Nessuna valutazione finora
- SLE SummaryDocumento5 pagineSLE Summaryapi-3704562100% (1)
- CHAPTER 127 MENINGOCOCCAL INFECTIONS SummaryDocumento3 pagineCHAPTER 127 MENINGOCOCCAL INFECTIONS Summaryapi-3704562Nessuna valutazione finora
- HUMAN HERPES VIRUS Types 6Documento1 paginaHUMAN HERPES VIRUS Types 6api-3704562100% (1)
- Psych AdjustmentDocumento2 paginePsych Adjustmentapi-3704562Nessuna valutazione finora
- Bacterial and Viral MeningitisDocumento12 pagineBacterial and Viral Meningitisapi-3704562Nessuna valutazione finora
- Ringkasan MeningitisDocumento2 pagineRingkasan Meningitisd17oNessuna valutazione finora
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Sheet PilesDocumento5 pagineSheet PilesolcayuzNessuna valutazione finora
- Duterte Vs SandiganbayanDocumento17 pagineDuterte Vs SandiganbayanAnonymous KvztB3Nessuna valutazione finora
- Cover Letter For Lettings Negotiator JobDocumento9 pagineCover Letter For Lettings Negotiator Jobsun1g0gujyp2100% (1)
- Notice: Constable (Driver) - Male in Delhi Police Examination, 2022Documento50 pagineNotice: Constable (Driver) - Male in Delhi Police Examination, 2022intzar aliNessuna valutazione finora
- Simple Past and Past Continuous Notes and ExercisesDocumento5 pagineSimple Past and Past Continuous Notes and ExercisesConstantina KouverianosNessuna valutazione finora
- Kolehiyo NG Lungsod NG Lipa: College of Teacher EducationDocumento3 pagineKolehiyo NG Lungsod NG Lipa: College of Teacher EducationPrincess LopezNessuna valutazione finora
- Queen of Hearts Rules - FinalDocumento3 pagineQueen of Hearts Rules - FinalAudrey ErwinNessuna valutazione finora
- Hellwalker: "What Terrors Do You Think I Have Not Already Seen?"Documento2 pagineHellwalker: "What Terrors Do You Think I Have Not Already Seen?"mpotatoNessuna valutazione finora
- Symptoms: Generalized Anxiety Disorder (GAD)Documento3 pagineSymptoms: Generalized Anxiety Disorder (GAD)Nur WahyudiantoNessuna valutazione finora
- Improving Downstream Processes To Recover Tartaric AcidDocumento10 pagineImproving Downstream Processes To Recover Tartaric AcidFabio CastellanosNessuna valutazione finora
- MagmatismDocumento12 pagineMagmatismVea Patricia Angelo100% (1)
- ICTSAS601 Student Assessment Tasks 2020Documento30 pagineICTSAS601 Student Assessment Tasks 2020Lok SewaNessuna valutazione finora
- Consortium of National Law Universities: Provisional 3rd List - CLAT 2020 - PGDocumento3 pagineConsortium of National Law Universities: Provisional 3rd List - CLAT 2020 - PGSom Dutt VyasNessuna valutazione finora
- Lifeline® Specialty: Fire Resistant QFCI Cable: Fire Resistant, Flame Retardant Halogen-Free Loose Tube - QFCI/O/RM-JMDocumento2 pagineLifeline® Specialty: Fire Resistant QFCI Cable: Fire Resistant, Flame Retardant Halogen-Free Loose Tube - QFCI/O/RM-JMkevinwz1989Nessuna valutazione finora
- CRM Final22222222222Documento26 pagineCRM Final22222222222Manraj SinghNessuna valutazione finora
- Amt 3103 - Prelim - Module 1Documento17 pagineAmt 3103 - Prelim - Module 1kim shinNessuna valutazione finora
- Grope Assignment 1Documento5 pagineGrope Assignment 1SELAM ANessuna valutazione finora
- Karak Rules - EN - Print PDFDocumento8 pagineKarak Rules - EN - Print PDFWesley TeixeiraNessuna valutazione finora
- Iluminadores y DipolosDocumento9 pagineIluminadores y DipolosRamonNessuna valutazione finora
- PS4 ListDocumento67 paginePS4 ListAnonymous yNw1VyHNessuna valutazione finora
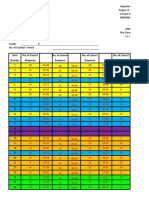
- Pea RubricDocumento4 paginePea Rubricapi-297637167Nessuna valutazione finora
- ANSI-ISA-S5.4-1991 - Instrument Loop DiagramsDocumento22 pagineANSI-ISA-S5.4-1991 - Instrument Loop DiagramsCarlos Poveda100% (2)
- The Rise of Political Fact CheckingDocumento17 pagineThe Rise of Political Fact CheckingGlennKesslerWPNessuna valutazione finora
- Health and Hatha Yoga by Swami Sivananda CompressDocumento356 pagineHealth and Hatha Yoga by Swami Sivananda CompressLama Fera with Yachna JainNessuna valutazione finora
- Annals of The B Hand 014369 MBPDocumento326 pagineAnnals of The B Hand 014369 MBPPmsakda HemthepNessuna valutazione finora
- Filehost - CIA - Mind Control Techniques - (Ebook 197602 .TXT) (TEC@NZ)Documento52 pagineFilehost - CIA - Mind Control Techniques - (Ebook 197602 .TXT) (TEC@NZ)razvan_9100% (1)
- Proposal For Real Estate Asset Management and Brokerage ServicesDocumento2 pagineProposal For Real Estate Asset Management and Brokerage ServicesTed McKinnonNessuna valutazione finora
- 5g-core-guide-building-a-new-world Переход от лте к 5г английскийDocumento13 pagine5g-core-guide-building-a-new-world Переход от лте к 5г английскийmashaNessuna valutazione finora
- Item AnalysisDocumento7 pagineItem AnalysisJeff LestinoNessuna valutazione finora
- Notice: Grant and Cooperative Agreement Awards: Public Housing Neighborhood Networks ProgramDocumento3 pagineNotice: Grant and Cooperative Agreement Awards: Public Housing Neighborhood Networks ProgramJustia.comNessuna valutazione finora